Abstract
Hypotonia in a newborn presents a diagnostic challenge for clinicians. It is an important clinical feature that may indicate an underlying systemic illness or neurological problem at the level of the central or peripheral nervous system. It is important to know the different presentations of hypotonia and to have the knowledge of the diagnostic work up which requires multidisciplinary assessment and input and the prognostic implications of these disorders. This review article presents a structured approach highlighting initial assessment, examination, and management of a neonate with generalized hypotonia.
Keywords: Floppy neonate, hypotonia, structured approach
Introduction
Hypotonia in a newborn poses a diagnostic challenge for neonatologists and pediatricians, as it is a clinical sign suggestive of both benign and serious conditions. The differential diagnosis for neonatal hypotonia is extensive and a methodical approach helps in localizing the problem to a specific region of the nervous system and formulating a differential diagnosis. Most of these neonates need prolonged mechanical ventilation, and diagnosing the underlying cause helps plan the management and inform the parents about the prognosis. This review article presents a structured approach highlighting initial assessment, examination, and management of a neonate with generalized hypotonia.
Important Aspects in History and Examination
Prenatal, neonatal, and perinatal history
The list of differential diagnosis of hypotonia in neonates is long, but a good history will narrow the possibilities. A detailed family history may be very helpful: A family history of neuromuscular disease needs to be elicited; a history of repeated abortions may suggest a variety of disorders with prenatal onset, developmental delay (a chromosomal abnormality), delayed motor milestones (a congenital myopathy), and premature death (metabolic or muscle disease).[1]
Details of pregnancy, delivery, and postnatal period are important. Prenatal risk factors include parental age, consanguinity, a history of drug or teratogen exposure, maternal diseases (diabetes/epilepsy), reduced fetal movements, polyhydramnios, and breech presentation. History of congenital infections - toxoplasmosis, rubella, cytomegalovirus, herpes simplex, and any history of pre- or post-natal insult increase the likelihood of central nervous system (CNS) dysfunction as the underlying cause of hypotonia.[2] It is also important to evaluate the mother for muscle weakness and myotonia.[3]
Meticulous documentation of any delivery complications, perinatal birth trauma, low Apgar scores, and time of onset of the hypotonia should be done. A detailed history regarding the degree of weakness and its progression should be recorded.
An abnormal fetal presentation and a shortened umbilical cord indicate poor fetal movement and may point toward neuromuscular disorder.[2] Neonates who need mechanical ventilation soon after birth have significant muscle weakness. Inborn error of metabolism should be considered in neonates who are born with normal pregnancy and delivery who later on develop hypotonia after a period of normality.[4]
Clinical examination
Clinical examination is the key in narrowing the differential diagnosis. The physical examination should include the assessment of relevant clinical signs including a detailed neurologic evaluation and an assessment for dysmorphic features.[5,6] The presence of congenital malformations in other organ systems and dysmorphic features indicates a possible syndromic diagnosis. Important conditions to rule out are trisomy 21 where hypotonia is associated with short stature,[7] characteristic facies and cardiac anomalies,[8] and Prader–Willi syndrome where hypotonia is associated with characteristic facial features, reduced deep tendon reflexes, feeding difficulties, and hypogonadism.[9]
It is important to determine whether the baby has low tone with or without weakness. Tone is defined as resistance of muscle to stretch, therefore babies with hypotonia have decreased resistance on passive stretching.[5] On the other hand, weakness is decreased muscle strength or power.[6] Lack of spontaneous movement in a baby suggests weakness. Most hypotonic neonates demonstrate a characteristic frog-legged posture-full abduction and external rotation of the legs as well as a flaccid extension of the arms.[1] Other signs of hypotonia include head lag, slip-through on vertical suspension, and draping on ventral suspension.
Weakness can be assessed by the cry, facial expressions, sucking and Moro's reflex, antigravity movements, and respiratory effort. It is important to evaluate the distribution and progression of weakness in differentiating the causes of neonatal hypotonia.
Physical examination of parents may also provide useful cues as babies with congenital myotonic dystrophy have severe hypotonia and examining mother may reveal the features of myotonia. Likewise, neonatal myasthenia may be suspected if mother displays fatigability of eyelids on upward gaze and fatigability of arms with sustained forward extension.[1]
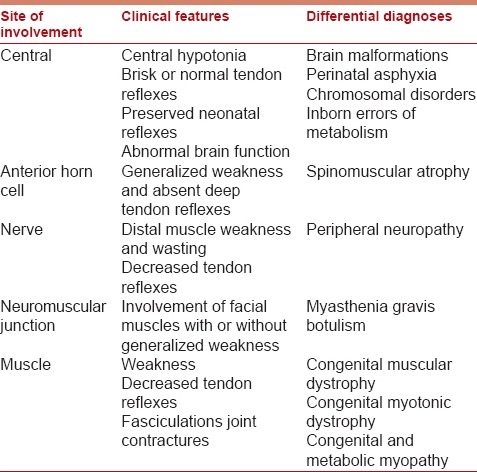
The major task in the evaluation of a hypotonic neonate is to determine the anatomic level of the pathology; whether it is central or peripheral in origin. The pattern of weakness and muscle involvement may help to localize the involved region in the nervous system [Table 1].
Table 1.
Clinical Features of Central Hypotonia
These hypotonic neonates show signs of abnormal consciousness, seizures, apneas, abnormal posturing, and feeding difficulties. Muscle power is relatively preserved and axial weakness is a significant clinical feature. The tendon reflexes are normal or hyperactive, and there is no evidence of muscle fasciculations.[10] Diminished or absent tendon reflexes point toward lower motor neuron lesion and brisk reflexes indicate CNS dysfunctions.[1]
Tight fisting of the hands, which do not open spontaneously, and in which the thumbs are enclosed by the other fingers or adducted across the palmar surface, and adduction of the thighs such that the legs are crossed when the infant is held in vertical suspension (scissoring) may be evidence of spasticity.[11]
Postural reflexes are generally preserved in infants with cerebral hypotonia despite a paucity of spontaneous movements. In some acute encephalopathies, the Moro reflex may be exaggerated.[11]
Clinical Features of Peripheral Hypotonia
Babies with anterior horn cell disease usually have sparing of extra-ocular muscles while the disorders of neuromuscular junctions may have ptosis and extra-ocular muscle weakness.[6] These infants appear more alert in comparison to those with CNS involvement. There is weakness in the antigravity limb muscles along with diminished or absent reflexes. They can have deformities of bones or joints (arthrogryposis).[2] Fasciculations, often observed in the tongue, are often very difficult to distinguish from normal random tongue movements. Postural reflexes are absent or diminished, and limbs that lack voluntary movement also cannot move reflexively.
Investigations
Appropriate use of investigations is necessary to establish a specific etiologic diagnosis and should be guided by the history and physical examination. We suggest a systematic approach based on the tests currently utilized in the evaluation of infants with hypotonia. Clinical details and relevant diagnostic tests are discussed in conjunction with specific disorders.
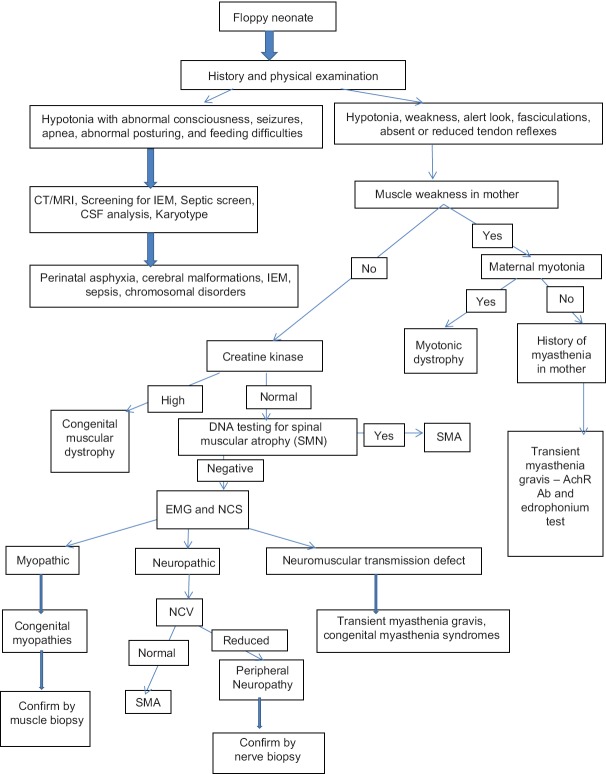
Here is a list of investigations for neonates with hypotonia (a schematic approach to the diagnosis of neonatal hypotonia is shown in Figure 1).
Figure 1.
Evaluation of a neonate with generalized hypotonia.[2,5,10,19] CT: Computed tomography, MRI: Magnetic resonance imaging, IEM: Inborn errors of metabolism, CSF: Cerebrospinal fluid, NCV: Nerve conduction velocity, SMA: Spinal muscular atrophy, NCS: Nerve conduction study
Neuroimaging
In babies with features of central hypotonia, neuroimaging is a valuable tool for diagnosis. Cranial and spinal neuroimaging (computed tomography/magnetic resonance imaging) studies are helpful in the identification of structural malformations, neuronal migration defects, brain stem and cerebellar abnormalities, and can identify features suggestive of mitochondrial abnormalities and metabolic diseases.
Genetic studies
These tests should be chosen according to the clinical presentation of the infants. The karyotype will disclose any genetic defects such as chromosomal duplications, deletions, trisomies such as Down syndrome (Trisomy 21), and disorders of genetic imprinting such as Prader Willi syndrome. Molecular genetic tests may also help in the diagnosis of spinal muscular atrophy (SMA) (deletion of SMN gene)[12,13] and myotonic dystrophy (trinucleotide repeats).[14]
Blood investigations
Blood investigations including full blood count, electrolytes, and inflammatory markers are important to rule out systemic disorders causing hypotonia including sepsis and dyselectrolytemias. Muscle enzymes (creatine kinase [CK] assay) are helpful in diagnosing muscle disorders such as congenital muscular dystrophies, metabolic myopathies, and some forms of the congenital myopathies. The blood for CK measurement should be obtained before performing the electromyography or muscle biopsy, as these procedures may cause false elevation of CK levels. The CK and iso-enzyme levels may be increased 10-fold for up to 1 week following normal vaginal delivery (presumably due to muscle trauma). The CK may be even higher in the context of acidosis (e.g., severely asphyxiated newborns).[11] Other biochemical investigations (e.g., serum lactate and carnitine levels) may be required in specific circumstances.
Chest X-ray
A chest radiograph may demonstrate enlarged cardiac shadows indicating cardiomyopathy or thin ribs, related to reduced fetal respiratory movements. The latter observation is a useful clue to antenatal onset of neuromuscular disease. An enlarged heart on chest X-ray may suggest Pompe disease.
Lumbar puncture
Cerebrospinal fluid (CSF) analysis is important to rule out neuroinfections. Markedly, increased protein concentration in CSF may indicate peripheral neuropathy or specific degenerative conditions.
Screening for inborn errors of metabolism
If the clinical picture suggests multisystem involvement, screening should be done for inborn errors of metabolism.[4]
Electrophysiological studies
Nerve conduction and electromyogram studies are useful in the assessment of disorders affecting the lower motor unit. Electromyography[15] is very helpful in establishing the diagnosis of SMA and disorders of the neuromuscular junction (botulism and congenital forms of myasthenia gravis).
Nerve conduction studies are consistent and reliable after 32 weeks of gestation.[11] Nerve conduction velocities may be very slow or unrecordable in congenital peripheral neuropathies. Nerve conduction studies and electromyography are also useful in diagnosing hereditary motor sensory neuropathies and in differentiating axonal disorders from demyelinating conditions.[16,17] Slow nerve conduction velocity and conduction block favor peripheral nerve involvement.
Muscle and nerve biopsies
These investigations should be considered, even if the electrophysiological studies are normal.[18] Muscle biopsy with immunohistochemical staining and electron microscopy is the method of choice for differentiating myopathies and muscular dystrophies, although it is more invasive. If biopsy shows specific abnormalities, it can be an essential part of the diagnostic evaluation in the newborn to guide subsequent DNA molecular diagnostic studies.
What is the Management of this Clinical Presentation?
Hypotonia is an important clinical presentation at birth or in the first few days of life. A specific diagnosis can help tailor the management and explain the prognosis to parents.
It is very important to continue supportive care with regards to feeding and respiration. Most of these hypotonic neonates need prolonged mechanical ventilation. Regular physiotherapy is needed to aid the clearance of respiratory secretions and will prevent limb contractures. It is vital to aggressively treat any respiratory infections. Feeding should be initiated by nasogastric tube and gastrostomy may be needed for few babies. Weight should be closely monitored as excessive weight gain can worsen existing muscle weakness.
Children with neuromuscular disorders need attention if they require anesthesia. Muscle relaxants should only be used if necessary as they have a more prolonged effect in these children. They are also susceptible to malignant hyperthermia and implicating agents should be avoided.[20]
It is important to ensure multidisciplinary follow-up for neonates with neuromuscular disorders. Follow-up should be arranged with neurologist and respiratory team, and an appointment with the geneticist for genetic counseling should be offered.
If there are symptoms and signs of severe neuromuscular involvement at birth (with respiratory insufficiency, lack of swallowing, cough, and tendon reflexes), the prognosis is very poor. Such a presentation should lead to timely ethical discussions as well as parental counseling and to the consideration of early extubation. In babies with hypotonia who survive the neonatal period, it is important to have detailed discussions sensitively with parents regarding the appropriateness of cardiopulmonary resuscitation in the event of cardiac arrest or acute respiratory failure.
Conclusion
The list of differential diagnoses for floppiness in the neonatal age group is extensive. However, most of these neonates have distinctive features in their family history, history at presentation, and their physical examination that can help differentiate them into central and peripheral disorders, and sometimes can lead to specific diagnoses within these groups. As there are frequent implications for future pregnancies, and specific treatments are available in a few disorders, we should strive for an accurate diagnosis in these neonates.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Leyenaar J, Camfield P, Camfield C. A schematic approach to hypotonia in infancy. Paediatr Child Health. 2005;10:397–400. doi: 10.1093/pch/10.7.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prasad AN, Prasad C. The floppy infant: Contribution of genetic and metabolic disorders. Brain Dev. 2003;25:457–76. doi: 10.1016/s0387-7604(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 3.Dubowitz V, editor. Muscle Disorders in Childhood. 2nd ed. London: WB Saunders Company; 1995. The floppy infant syndrome; pp. 457–72. [Google Scholar]
- 4.Tein I. Neonatal metabolic myopathies. Semin Perinatol. 1999;23:125–51. doi: 10.1016/s0146-0005(99)80046-9. [DOI] [PubMed] [Google Scholar]
- 5.Fenichel GM, editor. Clinical Pediatric Neurology: A Signs and Symptoms Approach. 4th ed. Philadelphia: WB Saunders Company; 2001. The hypotonic infant; pp. 149–69. [Google Scholar]
- 6.Crawford TO. Clinical evaluation of the floppy infant. Pediatr Ann. 1992;21:348–54. doi: 10.3928/0090-4481-19920601-06. [DOI] [PubMed] [Google Scholar]
- 7.Morris AF, Vaughan SE, Vaccaro P. Measurements of neuromuscular tone and strength in Down's syndrome children. J Ment Defic Res. 1982;26(Pt 1):41–6. doi: 10.1111/j.1365-2788.1982.tb00127.x. [DOI] [PubMed] [Google Scholar]
- 8.Rogers PT, Coleman M. New York: Dekker; 1992. Medical Care in Down Syndrome. [Google Scholar]
- 9.Cassidy SB, Schwartz S, Miller JL, Driscoll DJ. Prader-Willi syndrome. Genet Med. 2012;14:10–26. doi: 10.1038/gim.0b013e31822bead0. [DOI] [PubMed] [Google Scholar]
- 10.Paro-Panjan D, Neubauer D. Congenital hypotonia: Is there an algorithm? J Child Neurol. 2004;19:439–42. doi: 10.1177/088307380401900608. [DOI] [PubMed] [Google Scholar]
- 11.Hill A. Neonatal hypotonia. In: Maria BL, editor. Current Management in Child Neurology. 3rd ed. Hamilton: B C Decker Inc; 2005. pp. 529–34. [Google Scholar]
- 12.Vitali T, Sossi V, Tiziano F, Zappata S, Giuli A, Paravatou-Petsotas M, et al. Detection of the survival motor neuron (SMN) genes by FISH: Further evidence for a role for SMN2 in the modulation of disease severity in SMA patients. Hum Mol Genet. 1999;8:2525–32. doi: 10.1093/hmg/8.13.2525. [DOI] [PubMed] [Google Scholar]
- 13.Lefebvre S, Bürglen L, Frézal J, Munnich A, Melki J. The role of the SMN gene in proximal spinal muscular atrophy. Hum Mol Genet. 1998;7:1531–6. doi: 10.1093/hmg/7.10.1531. [DOI] [PubMed] [Google Scholar]
- 14.Kamsteeg EJ, Kress W, Catalli C, Hertz JM, Witsch-Baumgartner M, Buckley MF, et al. Best practice guidelines and recommendations on the molecular diagnosis of myotonic dystrophy types 1 and 2. Eur J Hum Genet. 2012;20:1203–8. doi: 10.1038/ejhg.2012.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.David WS, Jones HR., Jr Electromyography and biopsy correlation with suggested protocol for evaluation of the floppy infant. Muscle Nerve. 1994;17:424–30. doi: 10.1002/mus.880170410. [DOI] [PubMed] [Google Scholar]
- 16.Renault F. The role of electrodiagnostic studies in the diagnosis of hypotonia in infancy. Rev Med Liege. 2004;59(Suppl 1):190–7. [PubMed] [Google Scholar]
- 17.Russell JW, Afifi AK, Ross MA. Predictive value of electromyography in diagnosis and prognosis of the hypotonic infant. J Child Neurol. 1992;7:387–91. doi: 10.1177/088307389200700410. [DOI] [PubMed] [Google Scholar]
- 18.Richer LP, Shevell MI, Miller SP. Diagnostic profile of neonatal hypotonia: An 11-year study. Pediatr Neurol. 2001;25:32–7. doi: 10.1016/s0887-8994(01)00277-6. [DOI] [PubMed] [Google Scholar]
- 19.Hahn JS, Henry M, Hudgins L, Madan A. Congenital hypomyelination neuropathy in a newborn infant: Unusual cause of diaphragmatic and vocal cord paralyses. Pediatrics. 2001;108:E95. doi: 10.1542/peds.108.5.e95. [DOI] [PubMed] [Google Scholar]
- 20.Wedel DJ. Malignant hyperthermia and neuromuscular disease. Neuromuscul Disord. 1992;2:157–64. doi: 10.1016/0960-8966(92)90001-m. [DOI] [PubMed] [Google Scholar]