Abstract
Objective To assess the risk of pulmonary embolism, ischaemic stroke, and myocardial infarction associated with combined oral contraceptives according to dose of oestrogen (ethinylestradiol) and progestogen.
Design Observational cohort study.
Setting Data from the French national health insurance database linked with data from the French national hospital discharge database.
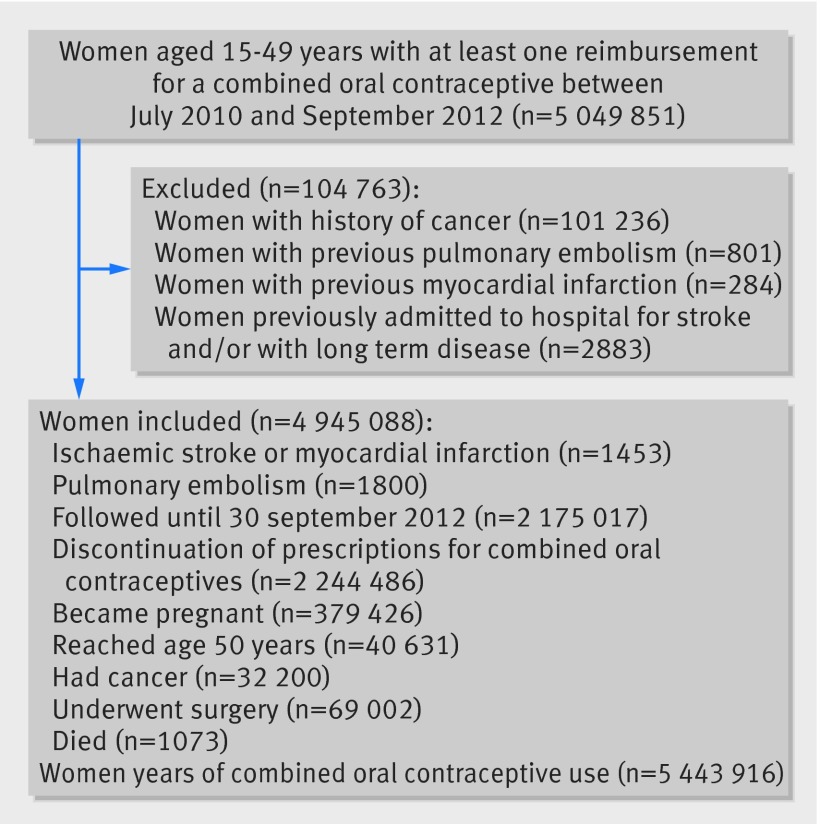
Participants 4 945 088 women aged 15-49 years, living in France, with at least one reimbursement for oral contraceptives and no previous hospital admission for cancer, pulmonary embolism, ischaemic stroke, or myocardial infarction, between July 2010 and September 2012.
Main outcome measures Relative and absolute risks of first pulmonary embolism, ischaemic stroke, and myocardial infarction.
Results The cohort generated 5 443 916 women years of oral contraceptive use, and 3253 events were observed: 1800 pulmonary embolisms (33 per 100 000 women years), 1046 ischaemic strokes (19 per 100 000 women years), and 407 myocardial infarctions (7 per 100 000 women years). After adjustment for progestogen and risk factors, the relative risks for women using low dose oestrogen (20 µg v 30-40 µg) were 0.75 (95% confidence interval 0.67 to 0.85) for pulmonary embolism, 0.82 (0.70 to 0.96) for ischaemic stroke, and 0.56 (0.39 to 0.79) for myocardial infarction. After adjustment for oestrogen dose and risk factors, desogestrel and gestodene were associated with statistically significantly higher relative risks for pulmonary embolism (2.16, 1.93 to 2.41 and 1.63, 1.34 to 1.97, respectively) compared with levonorgestrel. Levonorgestrel combined with 20 µg oestrogen was associated with a statistically significantly lower risk than levonorgestrel with 30-40 µg oestrogen for each of the three serious adverse events.
Conclusions For the same dose of oestrogen, desogestrel and gestodene were associated with statistically significantly higher risks of pulmonary embolism but not arterial thromboembolism compared with levonorgestrel. For the same type of progestogen, an oestrogen dose of 20 µg versus 30-40 µg was associated with lower risks of pulmonary embolism, ischaemic stroke, and myocardial infarction.
Introduction
About 104 million women worldwide use oral contraceptives.1 In most countries various types of pills are available, and studies have shown an increased risk of venous thromboembolism with the use of combined oral contraceptives.2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 This risk differs according to type of progestogen and decreases with both duration of use and decreasing oestrogen dose.
The optimal choice of oral contraceptives must also take into account the risks of stroke and myocardial infarction. Few studies have examined this relation, and those that are available have reported conflicting results.19 20 21 22 23 24 25 26 27 28 29 30 31 The impact and magnitude of the arterial risk according to dose of oestrogen (ethinylestradiol, 20 µg v 30-40 µg) have not been established for all progestogens. In France, eight combinations were available and reimbursed by national health insurance during the study period (table 1). They differed according to type of progestogen (norethisterone, levonorgestrel, desogestrel, gestodene, norgestrel) and dose of oestrogen (20 µg to 50 µg).
Table 1.
List of combined oral contraceptives reimbursed by French national health insurance
| Combined oral contraceptive | Generation of progestogen | Introduction to market | Start of reimbursement by health insurance | |
|---|---|---|---|---|
| Progestogen type | Oestrogen* dose | |||
| Norethisterone | 35 µg | First | 1982 | June 1984 |
| Norgestrel | 50 µg | Second | 1973 | February 1975 |
| Levonorgestrel | 30-40 µg | Second | 1974 | May 1976 |
| Levonorgestrel | 20 µg | Second | Apr-10 | April 2010 |
| Desogestrel | 30 µg | Third | 1984 | September 2009 |
| Desogestrel | 20 µg | Third | 1988 | January 2010 |
| Gestodene | 30 µg | Third | 1988 | November 2010 |
| Gestodene | 20 µg | Third | 1995 | November 2010 |
*Ethinylestradiol.
We assessed, under real life conditions in France, the absolute and relative risk of pulmonary embolism, ischaemic stroke, and myocardial infarction associated with the eight reimbursed oral contraceptives (including levonorgestrel with 20 µg oestrogen) according to type of progestogen and dose of oestrogen. The objective was to identify the combination associated with the lowest risk of venous and arterial thromboembolism.
Methods
This study was based on an observational historical population cohort comprising all women aged 15-49 years, living in France, with at least one reimbursement for oral contraceptives between July 2010 and September 2012.
Data source
We identified women in the French national health insurance database (SNIIRAM) linked to the French hospital discharge database (Programme de Médicalisation des Systèmes d’Information, PMSI) by a unique anonymous number on each woman’s health insurance smart card. SNIIRAM covers the entire French population (65.3 million inhabitants, including 14.8 million women of childbearing age) and contains exhaustive data on all reimbursements for health related expenditures,32 33 including medicinal products and outpatient medical and nursing care prescribed or performed by healthcare professionals, as well as demographic data such as age, sex, area of residence (postcode), vital status, and complementary universal health insurance (free access to healthcare for people with an annual income <50% of the poverty threshold, corresponding to 4.8 million inhabitants in France and including 1.2 million women aged 15-49 years). The medical indication for outpatient reimbursements is not available, but the patient’s status for 100% reimbursement of care related to a severe and costly long term disease is recorded and coded according to ICD-10 (international classification of diseases, 10th revision). The date of disease onset is available in the database for each patient with a long term disease (for example, cancer, diabetes, ischaemic heart disease).
PMSI provides detailed medical information on all admissions to French public and private hospitals, including dates of hospital admission and hospital discharge, discharge diagnosis ICD-10 codes, and medical procedures during the hospital stay. These data are used in the French diagnosis related groups.
Study population and follow-up
All women aged 15 to 49 years and registered in the French national health system were eligible for inclusion. As this study was designed to assess the risk of first pulmonary embolism, stroke, or myocardial infarction, we excluded women with a history of pulmonary embolism (hospital discharge since 2006, ICD-10 codes: I26), ischaemic stroke (hospital discharge since 2006 or long term disease diagnosis, ICD-10: I63-64), myocardial infarction (hospital discharge since 2006, ICD-10: I21, I22), and cancer and neoplastic disease (hospital discharge since 2006 or long term disease diagnosis, ICD-10 codes: C00-C97 and D00-D48) before the date of study entry. Follow-up started from the first reimbursement for oral contraceptives by French national health insurance between July 2010 and September 2012, and ended at the time of the first of the following events: discontinuation of oral contraceptives, hospital discharge for pulmonary embolism or ischaemic stroke or myocardial infarction, onset of pregnancy, age 50, hospital discharge for cancer, hospital discharge after orthopaedic surgery to the leg or gynaecological surgery, death, or 30 September 2012 (see supplementary tables 1 and 2).
Pregnancies that ended before September 2012 were identified by hospital stays for birth or abortion (diagnosis and/or medical procedure) or by reimbursement of non-hospital medical abortion. We excluded women from the study at the estimated date of onset of pregnancy. To avoid attributing the well known excess risk of thromboembolism post partum to oral contraceptives use, and because the effective start of oral contraception after birth is uncertain, women with a first reimbursement for oral contraceptives occurring less than two months after delivery or abortion were entered into the cohort two months after the end of pregnancy.
Definition of oral contraceptive use
Data on oral contraceptive use was collected from records for reimbursement. We categorised drug use by combinations of progestogen and oestrogen (ethinylestradiol) doses. Eight combinations with 26 brand names are reimbursed in France (table 1), and oral contraceptives are dispensed by pharmacists to women for a maximum authorised period of three months. This maximum dispensing period was observed in 99.2% of cases in our cohort. To assess the specific effects of each progestogen and each oestrogen dose on outcome, we also studied the various combinations of oral contraceptives. We considered women who switched to another dose of oestrogen or switched progestogen to have changed drug group during follow-up. The period for use of oral contraceptives ranged from the date of first dispensing until the date of the next dispensing. We defined the discontinuation of treatment as more than three consecutive months without filling a prescription for oral contraceptives after the period covered by the last prescription. In this case, use of oral contraceptives ended three months after the period covered by the last prescription.
Outcomes
During follow-up we assessed hospital admissions for pulmonary embolism (ICD-10 code: I26), stroke (ICD-10 codes: I63 with the exception of I63.6, I64), or myocardial infarction when initial management was specified by the medical staff (ICD-10 codes: I21.0 to 4, I21.9 plus indication of initial management). We also assessed the composite endpoint of hospital admission for pulmonary embolism, stroke, or myocardial infarction.
Confounding factors
In the database we identified potential baseline confounding factors known or likely to be related to cardiovascular events: age at study entry, complementary universal health insurance, deprivation index of participant’s area of residence calculated from socioeconomic data for 2009,34 consultation with a gynaecologist (at least one in the previous year), hypertension treated by antihypertensive drugs, and diabetes defined by at least two prescriptions of antidiabetic drugs in the previous 12 months or long term disease for diabetes. Data on smoking status were absent from the database, but some information about medical care related to tobacco use was present: a hospital discharge diagnosis related to tobacco use since 2006 (ICD-10 codes F17, Z71.6 and Z72.0) or dispensing of nicotine replacement therapy since 2009.
Because the proportion of women with diabetes or hypertension or treated for smoking cessation was small (<2% each), we combined these three factors in a single composite indicator of “contraindication or need for precautions for use” of oral contraceptives.
Statistical analysis
We calculated crude and age standardised incidence rates for pulmonary embolism, stroke, and myocardial infarction per 100 000 women years for the eight progestogen and oestrogen combinations and for progestogen and oestrogen dose groups. Poisson regression was used to calculate the adjusted relative risk estimates of outcome rates with the various combined oral contraceptives. We also estimated relative risks by stratification according to oestrogen dose (30-40 µg or 20 µg). Lack of fit and over-dispersion were assessed by Pearson and deviance statistics. Interactions with age were tested and, when statistically significant, we carried out subgroup analyses when compatible with the number of events in each drug use group. For all analyses, we considered the type of oral contraceptives most commonly prescribed (that is, 30 µg dose of oestrogen and levonorgestrel as progestogen) to be the reference group for drug use. We performed a secondary analysis in the subgroup of new users after pregnancy: postpartum women in whom pregnancy had ended less than six months (and more than two months) before study entry. Stratified analyses were performed according to consultation with a gynaecologist, complementary universal health insurance, oestrogen dose for progestogen type, and progestogen type for oestrogen dose.
We conducted several sensitivity analyses: for one we used a more specific definition of outcomes—confirmation that women who had not died 30 days after the event of interest had at least two prescriptions during the following four months (oral anticoagulant treatment after hospital admission for pulmonary embolism, antiplatelet agent after stroke, a combination of at least two drugs among antiplatelet agent, β blocking agents, statin, angiotensin converting enzyme (ACE) inhibitor, or angiotensin receptor blocker (ARB) after myocardial infarction). For the other sensitivity analyses we used censoring of drug use just after the end of the period covered by the last dispensing, one month after, and women who did not switch drugs.
We considered P values of less than 0.05 to be statically significant. Statistical analyses were performed with SAS 9.3 software (SAS Institute, Cary, NC).
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for recruitment, design, or implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community, although the French National Agency for Medicines and Health Products Safety (http://ansm.sante.fr/var/ansm_site/storage/original/application/69261368479ccbb39b5a909842e4b4cc.pdf) and French National Health Insurance (www.ameli.fr/l-assurance-maladie/statistiques-et-publications/etudes-en-sante-publique/etudes-pharmaco-epidemiologiques/risques-sous-contraceptif-oral-combine.php) disseminate key findings from studies on their websites.
Results
After exclusion and censoring of data (figure 1), the study cohort comprised 4 945 088 women with 5 443 916 women years of oral contraceptive use.
Fig 1 Flow of participants through study
The mean age of the women was 28.0 years (standard deviation 8.7 years) and almost 34% of the women used an oral contraceptive containing 20 µg oestrogen. The four oral contraceptive combinations most commonly used were levonorgestrel with 30-40 µg oestrogen (58.3% of women), levonorgestrel with 20 µg oestrogen (15.3%), desogestrel with 20 µg oestrogen (13.9%), and desogestrel with 30 µg oestrogen (13.2%). Specific participant characteristics were associated with each combination (table 2): younger women used levonorgestrel with 20 µg oestrogen and desogestrel with 30 µg oestrogen (mean age 25.3 and 25.7 years, respectively, with almost one third of women aged 15-19 years); women from higher socioeconomic groups used desogestrel with 20 µg oestrogen and gestodene with 20 and 30 µg oestrogen; women with a higher cardiovascular risk used levonorgestrel with 30-40 µg oestrogen, norethisterone with 35 µg oestrogen, and norgestrel with 50 µg oestrogen. Follow-up by a gynaecologist varied considerably according to the oral contraceptive used, from 33.5% (levonorgestrel with 30-40 µg oestrogen) to 61.3% (gestodene with 20 µg oestrogen). The distribution of oral contraceptives used by women post partum and the distribution of antimigraine drugs use according to oral contraceptive groups were also similar (table 2).
Table 2.
Characteristics of women using oral contraceptives before entry to cohort. Values are numbers (percentages) unless stated otherwise
| Characteristics | Progestogen type and oestrogen* dose | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Norethisterone+35 µg | Levonorgestrel | Norgestrel+50 µg | Desogestrel | Gestodene | |||||
| 20 µg | 30-40 µg | 20 µg | 30 µg | 20 µg | 30 µg | ||||
| No of women | 81 051 | 759 868 | 2 882 313 | 71 172 | 688 220 | 651 656 | 237 788 | 164 196 | 4 945 088 |
| Women years | 92 645 | 565 763 | 3 185 593 | 46 966 | 672 826 | 583 706 | 185 209 | 111 208 | 5 443 916 |
| Median (interquartile range) age (years) | 32 (24 to 40) | 23 (18 to 31) | 27 (21 to 35) | 30 (24 to 38) | 27 (21 to 35) | 24 (19 to 31) | 29 (23 to 36) | 30 (23 to 37) | 27 (21 to 34) |
| Mean (SD) age (years) | 32.0 (9.2) | 25.3 (8.3) | 28.5 (8.6) | 30.9 (8.6) | 28.3 (8.7) | 25.7 (8.5) | 30.1 (8.3) | 30.5 (8.5) | 28.0 (8.7) |
| Age group (years): | |||||||||
| 15-19 | 7658 (10.4) | 191 305 (32.5) | 450 176 (16.2) | 5406 (9.8) | 107 859 (18.4) | 170 982 (30.8) | 17 908 (9.4) | 12 238 (10.7) | 963 532 (19.5) |
| 20-24 | 12 032 (16.3) | 130 352 (22.1) | 652 423 (23.4) | 9676 (17.5) | 124 533 (21.2) | 126 883 (22.9) | 38 993 (20.6) | 21 046 (18.4) | 1 115 938 (22.6) |
| 25-29 | 11 372 (15.4) | 96 483 (16.4) | 550 163 (19.8) | 10 482 (19.0) | 111 352 (19.0) | 89 154 (16.1) | 40 476 (21.3) | 21 435 (18.7) | 930 917 (18.8) |
| 30-34 | 10 160 (13.8) | 74 283 (12.6) | 416 190 (15.0) | 9899 (18.0) | 90 593 (15.5) | 67 880 (12.2) | 35 722 (18.8) | 20 943 (18.3) | 725 670 (14.7) |
| 35-39 | 12 928 (17.5) | 51 445 (8.7) | 335 619 (12.1) | 9186 (16.7) | 75 467 (12.9) | 51 382 (9.3) | 26 541 (14.0) | 19 415 (17.0) | 581 983 (11.8) |
| 40-44 | 12 790 (17.4) | 31 060 (5.3) | 236 797 (8.5) | 6591 (12.0) | 49 331 (8.4) | 31 969 (5.8) | 18 124 (9.6) | 12 391 (10.8) | 399 053 (8.1) |
| 45-49 | 6730 (9.1) | 13 933 (2.4) | 141 200 (5.1) | 3895 (7.1) | 27 149 (4.6) | 16 092 (2.9) | 11 937 (6.3) | 7059 (6.2) | 227 995 (4.6) |
| Complementary universal health insurance† | 9944 (13.5) | 67 383 (11.4) | 402 822 (14.5) | 9846 (17.9) | 37 723 (6.4) | 62 963 (11.4) | 6084 (3.2) | 4744 (4.1) | 601 509 (12.2) |
| Ecological deprivation index (fifths): | |||||||||
| First fifth (least deprived) | 7030 (9.5) | 78 381 (13.3) | 295 723 (10.6) | 6859 (12.4) | 99 818 (17.0) | 79 077 (14.3) | 33 163 (17.5) | 24 012 (21.0) | 624 063 (12.6) |
| Second fifth | 9714 (13.2) | 95 149 (16.2) | 409 213 (14.7) | 7936 (14.4) | 98 016 (16.7) | 86 462 (15.6) | 32 772 (17.3) | 19 468 (17.0) | 758 730 (15.3) |
| Third fifth | 10 952 (14.9) | 93 373 (15.9) | 443 178 (15.9) | 8637 (15.7) | 89 544 (15.3) | 85 363 (15.4) | 29 206 (15.4) | 16 451 (14.4) | 776 704 (15.7) |
| Fourth fifth | 12 440 (16.9) | 91 752 (15.6) | 496 400 (17.8) | 9590 (17.4) | 83 676 (14.3) | 84 636 (15.3) | 27 667 (14.6) | 15 250 (13.3) | 821 411 (16.6) |
| Fifth fifth (most deprived) | 15 119 (20.5) | 91 064 (15.5) | 584 337 (21.0) | 12 117 (22.0) | 80 075 (13.7) | 89 704 (16.2) | 23 162 (12.2) | 13 616 (11.9) | 909 194 (18.4) |
| Missing data | 18 415 (25.0) | 139 142 (23.6) | 553 717 (19.9) | 9 996 (18.1) | 135 155 (23.1) | 129 100 (23.3) | 43 731 (23.1) | 25 730 (22.5) | 1 054 986 (21.3) |
| Medical history: | |||||||||
| Diabetes | 605 (0.8) | 3203 (0.5) | 20 672 (0.7) | 674 (1.2) | 3102 (0.5) | 2691 (0.5) | 937 (0.5) | 503 (0.4) | 32 387 (0.7) |
| Hypertensive agents | 2211 (3.0) | 1954 (0.3) | 47 204 (1.7) | 1139 (2.1) | 6199 (1.1) | 4538 (0.8) | 55 (0.0) | 25 (0.0) | 63 325 (1.3) |
| Smoking cessation treatment | 1982 (2.7) | 13 954 (2.4) | 88 548 (3.2) | 2545 (4.6) | 13 080 (2.2) | 12 870 (2.3) | 4217 (2.2) | 2348 (2.1) | 139 544 (2.8) |
| Diabetes and/or antihypertension and/or smoking cessation treatment | 4582 (6.2) | 18 797 (3.2) | 151 064 (5.4) | 4187 (7.6) | 21 886 (3.7) | 19 663 (3.5) | 5181 (2.7) | 2856 (2.5) | 228 216 (4.6) |
| Antimigraine drugs | 1982 (2.7) | 8651 (1.5) | 53 151 (1.9) | 1514 (2.7) | 11 304 (1.9) | 9634 (1.7) | 4136 (2.2) | 2253 (2.0) | 92 625 (1.9) |
| Private gynaecologist | 24 000 (32.6) | 295 002 (50.1) | 932 674 (33.5) | 27 969 (50.7) | 359 579 (61.3) | 274 715 (49.6) | 100 325 (52.9) | 70 150 (61.3) | 2 084 414 (42.2) |
| Post-partum period | 5898 (8.0) | 88 917 (15.1) | 321 358 (11.5) | 11 048 (20.0) | 62 088 (10.6) | 58 373 (10.5) | 16 185 (8.5) | 10 997 (9.6) | 574 864 (11.6) |
*Ethinylestradiol.
†Free access to healthcare for people with an annual income <50% of poverty threshold.
A total of 1800 pulmonary embolisms, 1046 ischaemic strokes, 407 myocardial infarctions, and 3253 composite events were observed during the study period. The respective absolute risk rates were 33, 19, 7, and 60 per 100 000 women years of oral contraceptive use.
Women aged more than 35 years accounted for 26.1% of all oral contraceptive use and 56.7% of serious adverse events. Women with the lowest socioeconomic status presented a 1.4-fold, 1.5-fold, and 2.5-fold higher risk of pulmonary embolism, stroke, and myocardial infarction, respectively (see supplementary table 3).
After adjustment for progestogen and risk factors, the relative risks for women using low dose oestrogen (20 µg v 30-40 µg) were 0.75 (95% confidence interval 0.67 to 0.85) for pulmonary embolism, 0.82 (0.70 to 0.96) for ischaemic stroke, and 0.56 (0.39 to 0.79) for myocardial infarction (table 3). Using a low dose of oestrogen was inversely associated with pulmonary embolism for all three progestogens, although the association did not reach statistical significance among gestodene users (table 4). After adjustment for risk factors and oestrogen dose, desogestrel and gestodene were associated with statistically significantly higher relative risks of pulmonary embolism: 2.16 (1.93 to 2.41) and 1.63 (1.34 to 1.97), respectively, compared with levonorgestrel. Desogestrel and gestodene were also associated with a significantly higher risk for the composite endpoint of pulmonary embolism, stroke, or myocardial infarction: 1.59 (1.45 to 1.74) and 1.24 (1.06 to 1.46), respectively (table 3). The associations between pulmonary embolism and progestogens provided similar results across strata of oestrogen dose (table 5). The crude and standardised rates of the events of interest and the effect of adjustment on the various confounders are shown (see supplementary tables 4 to 8).
Table 3.
Incidence rates and adjusted relative risks of pulmonary embolism, ischaemic stroke, and myocardial infarction according to type of oral contraceptives
| Variables | No of women years | Pulmonary embolism | Ischaemic stroke | Myocardial infarction | Composite event | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of events* | Crude incidence rate* | Adjusted relative risk† (95% CI) | No of events* | Crude incidence rate* | Adjusted relative risk† (95% CI) | No of events* | Crude incidence rate* | Adjusted relative risk† (95% CI) | No of events* | Crude incidence rate* | Adjusted relative risk† (95% CI) | |||||
| Oestrogen‡ dose: | ||||||||||||||||
| 20 µg | 1 423 797 | 454 | 31.9 | 0.75 (0.67 to 0.85) | 193 | 13.6 | 0.82 (0.70 to 0.96) | 44 | 3.1 | 0.56 (0.39 to 0.79) | 691 | 48.5 | 0.74 (0.67 to 0.82) | |||
| 30-40 µg | 3 880 507 | 1,300 | 33.5 | 1 | 800 | 20.6 | 1 | 333 | 8.6 | 1 | 2,433 | 62.7 | 1 | |||
| Progestogen type: | ||||||||||||||||
| Levonorgestrel | 3 751 356 | 1,048 | 27.9 | 1 | 761 | 20.3 | 1 | 314 | 8.4 | 1 | 2,123 | 56.6 | 1 | |||
| Desogestrel | 1 256 531 | 589 | 46.9 | 2.16 (1.93 to 2.41) | 179 | 14.2 | 0.96 (0.82 to 1.12) | 55 | 4.4 | 1.01, (0.73 to 1.39) | 823 | 65.5 | 1.59 (1.45 to 1.74) | |||
| Gestodene | 296 416 | 117 | 39.5 | 1.63 (1.34 to 1.97) | 53 | 17.9 | 0.96 (0.74 to 1.23) | 8 | 2.7 | 0.49 (0.22 to 0.94) | 178 | 60.1 | 1.24 (1.06 to 1.46) | |||
| Oral contraceptive type: | ||||||||||||||||
| Norethisterone 35 | 92 645 | 19 | 20.5 | 0.56 (0.35 to 0.83) | 25 | 27.0 | 0.85 (0.58 to 1.19) | 14 | 15.1 | 0.97 (0.54 to 1.60) | 58 | 62.6 | 0.75 (0.58 to 0.96) | |||
| Levonorgestrel 20 | 565 763 | 98 | 17.3 | 0.73 (0.60 to 0.89) | 56 | 9.9 | 0.68 (0.53 to 0.86) | 8 | 1.4 | 0.28 (0.13 to 0.53) | 162 | 28.6 | 0.65 (0.55 to 0.76) | |||
| Levonorgestrel 30/40 | 3 185 593 | 950 | 29.8 | 1 | 705 | 22.1 | 1 | 306 | 9.6 | 1 | 1,961 | 61.6 | 1 | |||
| Norgestrel 50 | 46 966 | 27 | 57.5 | 1.66 (1.14 to 2.34) | 28 | 59.6 | 2.13 (1.50 to 2.94) | 16 | 34.1 | 2.50 (1.45 to 3.99) | 71 | 151.2 | 2.00 (1.57 to 2.51) | |||
| Desogestrel 20 | 672 825 | 285 | 42.4 | 1.60 (1.41 to 1.82) | 109 | 16.2 | 0.88 (0.73 to 1.06) | 32 | 4.8 | 0.71 (0.48 to 1.02) | 426 | 63.3 | 1.22 (1.10 to 1.35) | |||
| Desogestrel 30 | 583 706 | 304 | 52.1 | 2.18 (1.93 to 2.47) | 70 | 12.0 | 0.80 (0.64 to 0.99) | 23 | 3.9 | 0.75 (0.48 to 1.12) | 397 | 68.0 | 1.52 (1.36 to 1.69) | |||
| Gestodene 20 | 185 208 | 71 | 38.3 | 1.34 (1.06 to 1.67) | 28 | 15.1 | 0.72 (0.50 to 0.99) | 4 | 2.2 | 0.28 (0.09 to 0.66) | 103 | 55.6 | 0.97 (0.79 to 1.17) | |||
| Gestodene 30 | 111 207 | 46 | 41.4 | 1.43 (1.07 to 1.87) | 25 | 22.5 | 1.04 (0.71 to 1.46) | 4 | 3.6 | 0.45 (0.14 to 1.05) | 75 | 67.4 | 1.15 (0.91 to 1.43) | |||
*Number of events/100 000 women years.
†Adjusted for age, complementary universal health insurance, medical risk factors, gynaecological visit during previous year, type of progestogen (for dose of oestrogen), and dose of oestrogen (for type of progestogen)
‡Ethinylestradiol.
Table 4.
Adjusted relative risks of pulmonary embolism according to oestrogen dose stratified by type of progestogen
| Progestogen | Oestrogen* 20 µg | Oestrogen* 30-40 µg | |||
|---|---|---|---|---|---|
| No of events | Adjusted relative risk† (95% CI) | No of events | Adjusted relative risk† (95% CI) | ||
| Levonorgestrel | 98 | 0.74 (0.59 to 0.91) | 950 | 1 | |
| Desogestrel | 285 | 0.75 (0.63 to 0.88) | 304 | 1 | |
| Gestodene | 71 | 0.94 (0.68 to 1.29) | 46 | 1 | |
No significant interaction between progestogen and oestrogen dose.
*Ethinylestradiol.
†Adjusted for age, complementary universal health insurance, medical risk factors, and gynaecological visit during previous year.
Table 5.
Adjusted relative risks of pulmonary embolism according to type of progestogen stratified by oestrogen dose
| Oestrogen* dose | Levonorgestrel | Desogestrel | Gestodene | |||||
|---|---|---|---|---|---|---|---|---|
| No of events | Adjusted relative risk† (95% CI) | No of events | Adjusted relative risk† (95% CI) | No of events | Adjusted relative risk† (95% CI) | |||
| 20 µg | 98 | 1 | 285 | 2.30 (1.86 to 2.86) | 71 | 1.96 (1.47 to 2.61) | ||
| 30-40 µg | 950 | 1 | 304 | 2.19 (1.93 to 2.48) | 46 | 1.41 (1.05 to 1.84) | ||
No significant interaction between progestogen and oestrogen dose.
*Ethinylestradiol.
†Adjusted for age, complementary universal health insurance, medical risk factors, and gynaecological visit during previous year.
Analysis of women post partum (two months to six months after delivery) also indicated a lower risk with using the 20 µg dose of oestrogen compared with 30-40 µg for pulmonary embolism (0.65, 0.44 to 0.94) and for arterial events (ischaemic stroke or myocardial infarction) (0.36, 0.20 to 0.62). The adjusted relative risk of pulmonary embolism for desogestrel and gestodene (reference levonorgestrel) was 2.16 (1.52 to 3.03) and 1.49 (0.64 to 2.99), respectively (see supplementary table 9). Analyses stratified according to consultation with a gynaecologist and complementary universal health insurance provided similar results (see supplementary tables 10).
Several sensitivity analyses were performed. The first used a definition of endpoints confirmed by drug treatments prescribed after the event of interest (for example, anticoagulants after pulmonary embolism) (see supplementary table 11). Other sensitivity analyses used censoring of exposure just after the end of the period covered by the last dispensing and one month after (see supplementary tables 12 and 13). The analysis confined to women who did not switch drugs during follow-up was also performed (see supplementary table 14). These analyses demonstrated similar results for pulmonary embolism and arterial risk.
Discussion
In this population based cohort study, levonorgestrel with 20 µg of oestrogen was associated with a statistically significantly lower risk of pulmonary embolism, ischaemic stroke, and myocardial infarction than levonorgestrel with 30-40 µg of oestrogen. For the same type of progestogen, using an oestrogen dose of 20 µg compared with 30-40 µg was associated with a lower risk of pulmonary embolism (by 25%), ischaemic stroke (by 18%), and myocardial infarction (by 44%). Desogestrel and gestodene were associated with 2.2-fold and 1.6-fold statistically significantly higher risks of pulmonary embolism compared with levonorgestrel. In contrast, the observed arterial vascular risks did not differ according to the type of progestogen used. Levonorgestrel with 20 µg of oestrogen was globally associated with a lower risk of the composite endpoint of hospital admission for pulmonary embolism, stroke, or myocardial infarction compared with the other oral contraceptive combinations tested.
Comparison with other studies
Most authors have observed a dose-effect relation with oestrogen, higher doses being associated with an increased risk of venous thromboembolism. Lidegaard and colleagues12 showed that desogestrel or gestodene combined with 20 µg of oestrogen was associated with 23% and 17% lower relative risks of venous thromboembolism compared with the same progestogens combined with 30 µg of oestrogen. Van Hylckama and colleagues7 reported a higher risk of venous thromboembolism for oral contraceptives containing 50 µg of oestrogen compared with 30 µg of oestrogen (odds ratio 1.9, 1.1 to 3.4), and no statistically significant difference for risk with oral contraceptives containing 20 µg of oestrogen (0.8, 0.5 to 1.2). A similar trend has been shown for oral contraceptives with higher doses of oestrogen (50-100 µg).35 36 37
In the present study, after adjustment for the type of progestogen, we observed a statistically significant reduction in the risk of pulmonary embolism by about 25% with the 20 µg dose compared with 30-40 µg dose. A similar tendency was found for risk of venous thromboembolism with desogestrel and gestodene, but not with levonorgestrel.15 Finally, the analysis by Lidegaard and colleagues31 showed that oral contraceptives with 20 µg, 30-40 µg, and 50 µg of oestrogen were associated with relative risks of myocardial infarction of 1.40 (95% confidence interval 1.07 to 1.81), 1.88 (1.66 to 2.13), and 3.73 (2.78 to 5.00), respectively (P<0.001 for trend). We also observed a statistically significantly lower risk for the 20 µg dose compared with 30-40 µg doses (adjusted relative risk 0.56, 95% confidence interval 0.39 to 0.79), in line with the results reported previously.31
Similarly, the relative risk of pulmonary embolism was 2.16 (1.93 to 2.41) for desogestrel and 1.63 (1.34 to 1.97) for gestodene compared with levonorgestrel. These relative risks were similar to those reported for risk of venous thromboembolism by Lidegaard and colleagues (2.2, 1.7 to 2.3 and 2.1, 1.6 to 2.8)12; by van Hylckama and colleagues (2.0, 1.4 to 2.8 and 1.6, 1.0 to 2.4)7; in the meta-analysis by Stegeman and colleagues (1.8, 1.4 to 2.2 and 1.5, 1.2 to 2.0)15; and by Vinogradova and colleagues18 (1.8, 1.5 to 2.1 and 1.5, 1.2 to 1.9).
The effect of age on the events of interest in this study is in line with those reported in the literature, supporting the validity of our reported results. For example, the 3.6-fold increased risk of venous thromboembolism with age (45-49 years v 15-19 years) calculated in by Lidegaard and colleagues8 was close to the risk of pulmonary embolism calculated in our study (4.1-fold). Similarly, the risks of ischaemic stroke and myocardial infarction with age (45-49 years v 15-19 years) were the same in the two studies: 20 and 100, according to Lidegaard and colleagues31 and 21 and 106 in our study.
Strengths and limitations of this study
These results were shown with a high statistical power based on 5.4 million women years of combined oral contraceptive use, allowing us to observe more than 3200 serious events (pulmonary embolism, ischaemic stroke, or myocardial infarction) in this study. However, the number of events was low for some subgroups, particularly the number of myocardial infarctions among women treated with gestodene and levonorgestrel with 20 µg of oestrogen. These results therefore need to be interpreted cautiously, and further studies are necessary to confirm the present results. The follow-up period was also relatively short (maximum of two years and three months), which limits the bias associated with changing diagnostic procedures and health system management of the three events of interest, and eliminated the potential time trend bias. However, certain diseases may take longer to manifest, particularly ischaemic stroke and myocardial infarction. The availability of levonorgestrel with 20 µg of oestrogen on the French market in April 2010, with more than 650 000 women years in our cohort, allowed us to calculate arterial and venous thromboembolic risk under real conditions of use. A possible indication bias was limited by adopting September 2012 as the end date for inclusion in the study, owing to the publication of a practice guideline for doctors in October and November 2012.38
This study was based on two databases (SNIIRAM and PMSI) with completely independent data collection. The search for a possible increased risk of hospital admission among women reimbursed for oral contraceptives was therefore performed by using both health insurance reimbursement data related to pharmacy purchases of oral contraceptives and inhospital diagnoses.
Information on reimbursement of medicinal products is exhaustively collected on a regular basis by entering the specific bar code for each medicinal product reimbursed. Patients are identified by their personal smart card, and daily teletransmission by pharmacists to the French national health insurance network avoided the recall or recording bias often associated with retrospective case-control studies.
Data on hospital stay is systematically recorded in PMSI (French hospital discharge database), as each hospital doctor in France is required to complete this information after a patient is admitted to hospital.39 Doctors specialised in these hospital codes collect, validate, and transmit all structured and coded medical information from the hospital to paying and controlling bodies. PMSI is used to determine the cost of each hospital stay. Retrospective linking between the two databases, based on independent data collection, therefore theoretically excludes the possibility of a differential observation bias on hospital management diagnoses of pulmonary embolism or arterial thromboembolic events according to outpatient prescribed and dispensed use of oral contraceptives. Validation of cases is essential in this type of observational study. A validation study of cases of pulmonary embolism in 25 French hospitals found that the sensitivity of the ICD-10 diagnostic code for pulmonary embolism in the PMSI was 88.9% (95% confidence interval 85.6 to 92.2).40 Our analysis of anticoagulant treatment on discharge from hospital (89% of cases filled at least two prescriptions, with an average of more than five prescriptions, for anticoagulants during the four months after hospital admission) confirmed the validity of this criterion. The authors of a validation study of cases of stroke based on the PMSI compared with the stroke registry reported a sensitivity of 77.1% (95% confidence interval 74.2 to 80) and a positive predictive value of 69.2.41 However, an improvement was observed over time, with a sensitivity of 82.9% and positive predictive value of 81.2% in 2008, the last year of the study. A classic difficulty in observational studies on stroke concerns interpretation of the I64 code (stroke, not specified as haemorrhage or infarction). This code made a limited contribution to the present study, as it represented only 102 of the 1046 ischaemic strokes compared with 944 of I63 codes (with the exception of I63.6).
The initial management of myocardial infarction has a specific code in the French hospital discharge database based on ICD-10 to distinguish initial management from a prevalent case by means of a mandatory additional digit. As this code has a major impact on the cost of hospital stay, the initial management of myocardial infarction seems to be associated with a relatively low risk of error, especially in young participants. We also observed that more than 94% of women in this study received outpatient post-infarction treatment comprising at least two treatment groups from among statins, β blockers, angiotensin converting enzyme inhibitors/sartans, and platelet aggregation inhibitors.
However, our study has several limitations. The first concerns the absence of the start date for use of combined oral contraceptives and the concept of new user or switch from another product not reimbursed by French national health insurance. Indeed, the incidence of venous thromboembolism is increased during the initial phase of oral contraceptives use, particularly during the first three months and the first year.12 An adjustment for the length of oral contraceptives use would be necessary to take this variable into account. Lidegaard and colleagues, who performed this adjustment, observed a slight reduction in the relative risk for new products, but the global results remained unchanged. If this factor had a major impact, it would have primarily concerned levonorgestrel with 20 µg oestrogen, the product most recently released onto the French market, for which the risk of pulmonary embolism would possibly be overestimated, although we observed a lower risk than with the other drug combinations. The frequently reported argument that third generation oral contraceptives such as gestodene, desogestrel that have been released onto the market more recently and therefore correspond to newer users, would lead to bias,42 can no longer be justified more than 25 years after the release of these oral contraceptives in France. The relative stability of the market shares of the various oral contraceptives other than levonorgestrel with 20 µg oestrogen in France between July 2010 and September 2012 is an argument in favour of the validity of our estimates. Another element concerns the analysis in the post-partum setting, in which all women of the cohort initiated use of oral contraceptives after the pregnancy. The results of this subgroup analysis were similar to those of the main analysis for desogestrel compared with levonorgestrel as reference.
In contrast, to our knowledge the duration of use had no impact on the risk of myocardial infarction and ischaemic stroke—the other two events of interest in the study.
Among the limitations related to the study design, we failed to take into account women who may have died from a venous or arterial thromboembolic event before admission to hospital. This limitation could introduce a bias if women experiencing a thromboembolic event while taking a combined oral contraceptive with 20 µg of oestrogen died more rapidly and before admission to hospital compared with women taking one with 30-40 µg of oestrogen, which seems unlikely.
Potential for confounding by indication is a another limitation of the present study, as we did not take into account some factors known to increase the risk of venous or arterial thrombosis and which may therefore influence a doctor’s choice of oral contraceptives, such as body mass index and family predisposition. However, doctors preferentially prescribed levonorgestrel to the most economically underprivileged women and women with diabetes, two factors associated with higher body mass index. In the present study these two factors would underestimate the risk of pulmonary embolism associated with the other progestogens such as desogestrel and gestodene. The same argument could apply to women with a family predisposition, who would be prescribed oral contraceptives associated with a lower risk. Data on smoking, a major risk factor for arterial thrombosis, but with a low impact on the risk of venous thromboembolism,43 were only partially available and limited to situations of medically assisted smoking cessation. Again, the population most concerned by smoking was that using levonorgestrel, an argument in favour of underestimation of the risk associated with the other oral contraceptive combinations. Furthermore, analyses adjusted for smoking in previous published studies did not modify, or only marginally modified, the results.7 31
Finally, another limitation of this study was the failure to include oral contraceptives not reimbursed by French national health insurance, such as drospirenone for which discordant result have been previously reported.7 8 9 10 11 12 18 44 Based on data derived from declarations of annual sales by drug companies to the French National Agency for Medicines and Health Products Safety, we estimated that our study sample comprised about two thirds of all women receiving a third generation oral contraceptive and all women receiving a first or second generation oral contraceptive. Limiting our study to women using oral contraceptives reimbursed by French national health insurance has the advantage of improving the comparability of women within the sample, as it has been largely shown in the literature that the choice of method of contraception is related to women’s socioeconomic status as well as financial imperatives.45
Lastly, only pulmonary embolism was considered as an outcome of deep vein thrombosis, although use of oral contraceptives increases the risk of all forms of deep vein thrombosis.8 Indeed, acute diagnoses can be determined only for hospital related events in the present databases, and the frequency of deep vein thrombosis, of which not all cases involve hospital admission, would have been seriously underestimated.
Conclusions
Women using an oral contraceptive with 20 µg of oestrogen had a lower risk of pulmonary embolism and serious arterial thromboembolic events than women using an oral contraceptive with 30-40 µg oestrogen. We also found that use of an oral contraceptive containing levonorgestrel was associated with a 50% lower risk of pulmonary embolism compared with using an oral contraceptive with a third generation progestogen. The combination of levonorgestrel and 20 µg of oestrogen was the combination associated with the lowest incidence of serious adverse events. Under real conditions of use, among 100 000 women using a combined oral contraceptive for one year an estimated 33 will experience pulmonary embolism, 19 ischaemic stroke, and seven myocardial infarction. For each woman, it is necessary to determine the most appropriate contraceptive method in terms of acceptability and risk. A risk reduction strategy should be based on limitation of use of oral contraceptives associated with the highest risk to decrease the incidence of pulmonary embolism46 and arterial thromboembolic events among young women.
What is already known on this topic
Use of combined oral contraceptives increases the risk of pulmonary embolism
A dose related effect of oestrogen (ethinylestradiol) has been observed for the progestogens gestodene, desogestrel, and levonorgestrel, with higher doses associated with a higher risk of venous thromboembolism
The use of oral contraceptives is also associated with an increased risk of ischaemic stroke and myocardial infarction
What this study adds
For the same progestogen, using an oestrogen dose of 20 µg compared with 30-40 µg was associated with lower risks of pulmonary embolism, ischaemic stroke, and myocardial infarction
Oral contraceptives containing levonorgestrel with 20 µg of oestrogen was the combination associated with the overall lowest risk of pulmonary embolism and arterial thromboembolism
Web Extra.
Extra material supplied by author
Web appendix: Supplementary information
We thank Anthony Saul for English revision of the manuscript.
Contributors: This study was conducted at the official request of the French Ministry of Health. MZ, PR, FA, and AW had the idea for the study. AW and MZ conceived the study design. AW planned the study and drafted the manuscript. MD performed data management. MD and PB did the statistical analyses. AW and MZ were responsible for management of the project and oversaw the study. All authors contributed to the interpretation of the data, revised the manuscript, and approved the final manuscript. AW and MD are the guarantors.
Funding: This research was funded by the French National Health Insurance Fund (CNAMTS) and the French National Agency for Medicines and Health Products Safety (ANSM). AW, MD, PB, JR, PR, and FA are employees of the French National Health Insurance Fund, MZ and FR of the French National Agency for Medicines and Health Products Safety. The present paper represents the opinions of the authors and does not necessarily reflect the position of their employers.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study was approved by the French data protection agency Commission Nationale de l'Informatique et des Libertés (regulatory decision DE-2011-078).
Data sharing: No additional data available.
Transparency: The lead author affirms that this manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1.Compiled by Earth Policy Institute from U.N. Population Division. World Contraceptive Use 2011, wall chart, February 2011. www.google.fr/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0CCMQFjAA&url=http%3A%2F%2Fwww.earth-policy.org%2Fdatacenter%2Fxls%2Fhighlights26_all.xls&ei=FZ0WVKPMOdTvaKXzgqgP&usg=AFQjCNF10wNQtG2aoPUgkK9YRymHRxb5cw&sig2=ZpqOHEY2CTVVkIA9WUrS4Q&bvm=bv.75097201,d.d2s
- 2.Vandenbroucke JP, Koster T, Briët E, Reitsma PH, Bertina RM, Rosendaal FR. Increased risk of venous thrombosis in oral-contraceptive users who are carriers of factor V Leiden mutation. Lancet 1994;344:1453-7. 10.1016/S0140-6736(94)90286-0 pmid:7968118. [DOI] [PubMed] [Google Scholar]
- 3.Thorogood M, Mann J, Murphy M, Vessey M. Risk factors for fatal venous thromboembolism in young women: a case-control study. Int J Epidemiol 1992;21:48-52. 10.1093/ije/21.1.48 pmid:1544757. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Venous thromboembolic disease and combined oral contraceptives: results of international multicentre case-control study. Lancet 1995;346:1575-82. 10.1016/S0140-6736(95)91926-0 pmid:7500748. [DOI] [PubMed] [Google Scholar]
- 5.Farmer RD, Lawrenson RA, Thompson CR, Kennedy JG, Hambleton IR. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet 1997;349:83-8. 10.1016/S0140-6736(96)07496-X pmid:8996419. [DOI] [PubMed] [Google Scholar]
- 6.Parkin L, Skegg DCG, Wilson M, Herbison GP, Paul C. Oral contraceptives and fatal pulmonary embolism. Lancet 2000;355:2133-4. 10.1016/S0140-6736(00)02382-5 pmid:10902629. [DOI] [PubMed] [Google Scholar]
- 7.van Hylckama Vlieg A, Helmerhorst FM, Vandenbroucke JP, Doggen CJ, Rosendaal FR. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ 2009;339:b2921 10.1136/bmj.b2921 pmid:19679614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lidegaard Ø, Løkkegaard E, Svendsen AL, Agger C. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ 2009;339:b2890 10.1136/bmj.b2890 pmid:19679613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dinger J, Assmann A, Möhner S, Minh TD. Risk of venous thromboembolism and the use of dienogest- and drospirenone-containing oral contraceptives: results from a German case-control study. J Fam Plann Reprod Health Care 2010;36:123-9. 10.1783/147118910791749416 pmid:20659364. [DOI] [PubMed] [Google Scholar]
- 10.Parkin L, Sharples K, Hernandez RK, Jick SS. Risk of venous thromboembolism in users of oral contraceptives containing drospirenone or levonorgestrel: nested case-control study based on UK General Practice Research Database. BMJ 2011;342:d2139 10.1136/bmj.d2139 pmid:21511804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jick SS, Hernandez RK. Risk of non-fatal venous thromboembolism in women using oral contraceptives containing drospirenone compared with women using oral contraceptives containing levonorgestrel: case-control study using United States claims data. BMJ 2011;342:d2151 10.1136/bmj.d2151 pmid:21511805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lidegaard Ø, Nielsen LH, Skovlund CW, Skjeldestad FE, Løkkegaard E. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ 2011;343:d6423 10.1136/bmj.d6423 pmid:22027398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Food and Drug Administration Office of Surveillance and Epidemiology. Combined hormonal contraceptives (CHCs) and the risk of cardiovascular disease endpoints (http://www.fda.gov/downloads/Drugs/DrugSafety/UCM277384.pdf).
- 14.Gronich N, Lavi I, Rennert G. Higher risk of venous thrombosis associated with drospirenone-containing oral contraceptives: a population-based cohort study. CMAJ 2011;183:E1319-25. 10.1503/cmaj.110463 pmid:22065352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stegeman BH, de Bastos M, Rosendaal FR, et al. Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis. BMJ 2013;347:f5298 10.1136/bmj.f5298 pmid:24030561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunn N. Oral contraceptives and venous thromboembolism. BMJ 2009;339:b3164 10.1136/bmj.b3164 pmid:19679617. [DOI] [PubMed] [Google Scholar]
- 17.Bitzer J, Amy JJ, Beerthuizen R, et al. Statement on combined hormonal contraceptives containing third- or fourth-generation progestogens or cyproterone acetate, and the associated risk of thromboembolism. J Fam Plann Reprod Health Care 2013;39:156-9. 10.1136/jfprhc-2013-100624 pmid:23585363. [DOI] [PubMed] [Google Scholar]
- 18.Vinogradova Y, Coupland C, Hippisley-Cox J. Use of combined oral contraceptives and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases. BMJ 2015;350:h2135 10.1136/bmj.h2135 pmid:26013557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poulter NR, Chang CL, Farley TM, Marmot MG, Meirik O. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Effect on stroke of different progestagens in low oestrogen dose oral contraceptives. Lancet 1999;354:301-2. 10.1016/S0140-6736(99)01013-2 pmid:10440309. [DOI] [PubMed] [Google Scholar]
- 20.Heinemann LAJ, Lewis MA, Spitzer WO, Thorogood M, Guggenmoos-Holzmann I, Bruppacher R. Transnational Research Group on Oral Contraceptives and the Health of Young Women. Thromboembolic stroke in young women. A European case-control study on oral contraceptives. Contraception 1998;57:29-37. 10.1016/S0010-7824(97)00204-7 pmid:9554248. [DOI] [PubMed] [Google Scholar]
- 21.Lidegaard Ø, Kreiner S. Contraceptives and cerebral thrombosis: a five-year national case-control study. Contraception 2002;65:197-205. 10.1016/S0010-7824(01)00306-7 pmid:11929641. [DOI] [PubMed] [Google Scholar]
- 22.Stampfer MJ, Willett WC, Colditz GA, Speizer FE, Hennekens CH. A prospective study of past use of oral contraceptive agents and risk of cardiovascular diseases. N Engl J Med 1988;319:1313-7. 10.1056/NEJM198811173192004 pmid:3185634. [DOI] [PubMed] [Google Scholar]
- 23.Lewis MA, Heinemann LAJ, Spitzer WO, MacRae KD, Bruppacher R. The use of oral contraceptives and the occurrence of acute myocardial infarction in young women. Results from the Transnational Study on Oral Contraceptives and the Health of Young Women. Contraception 1997;56:129-40. 10.1016/S0010-7824(97)00118-2 pmid:9347202. [DOI] [PubMed] [Google Scholar]
- 24.Poulter NR, Chang CL, Farley TMM, Kelaghan J, Meirik O, Marmot MG. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Acute myocardial infarction and combined oral contraceptives: results of an international multicentre case-control study. Lancet 1997;349:1202-9. 10.1016/S0140-6736(97)02358-1 pmid:9130941. [DOI] [PubMed] [Google Scholar]
- 25.Sidney S, Siscovick DS, Petitti DB, et al. Myocardial infarction and use of low-dose oral contraceptives: a pooled analysis of 2 US studies. Circulation 1998;98:1058-63. 10.1161/01.CIR.98.11.1058 pmid:9736591. [DOI] [PubMed] [Google Scholar]
- 26.Dunn N, Thorogood M, Faragher B, et al. Oral contraceptives and myocardial infarction: results of the MICA case-control study. BMJ 1999;318:1579-83. 10.1136/bmj.318.7198.1579 pmid:10364115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dunn NR, Arscott A, Thorogood M. The relationship between use of oral contraceptives and myocardial infarction in young women with fatal outcome, compared to those who survive: results from the MICA case-control study. Contraception 2001;63:65-9. 10.1016/S0010-7824(01)00172-X pmid:11292469. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg L, Palmer JR, Rao RS, Shapiro S. Low-dose oral contraceptive use and the risk of myocardial infarction. Arch Intern Med 2001;161:1065-70. 10.1001/archinte.161.8.1065 pmid:11322840. [DOI] [PubMed] [Google Scholar]
- 29.Tanis BC, van den Bosch MA, Kemmeren JM, et al. Oral contraceptives and the risk of myocardial infarction. N Engl J Med 2001;345:1787-93. 10.1056/NEJMoa003216 pmid:11752354. [DOI] [PubMed] [Google Scholar]
- 30.Margolis KL, Adami HO, Luo J, Ye W, Weiderpass E. A prospective study of oral contraceptive use and risk of myocardial infarction among Swedish women. Fertil Steril 2007;88:310-6. 10.1016/j.fertnstert.2006.11.206 pmid:17624338. [DOI] [PubMed] [Google Scholar]
- 31.Lidegaard Ø, Løkkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 2012;366:2257-66. 10.1056/NEJMoa1111840 pmid:22693997. [DOI] [PubMed] [Google Scholar]
- 32.Tuppin P, de Roquefeuil L, Weill A, Ricordeau P, Merlière Y. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique 2010;58:286-90. 10.1016/j.respe.2010.04.005 pmid:20598822. [DOI] [PubMed] [Google Scholar]
- 33.Moulis G, Lapeyre-Mestre M, Palmaro A, Pugnet G, Montastruc JL, Sailler L. French health insurance databases: What interest for medical research?Rev Med Interne 2015;36:411-7. 10.1016/j.revmed.2014.11.009 pmid:25547954. [DOI] [PubMed] [Google Scholar]
- 34.Rey G, Jougla E, Fouillet A, Hémon D. Ecological association between a deprivation index and mortality in France over the period 1997 - 2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health 2009;9:33 10.1186/1471-2458-9-33 pmid:19161613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vessey M, Mant D, Smith A, Yeates D. Oral contraceptives and venous thromboembolism: findings in a large prospective study. Br Med J (Clin Res Ed) 1986;292:526 10.1136/bmj.292.6519.526 pmid:3081157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bloemenkamp KW, Rosendaal FR, Helmerhorst FM, Büller HR, Vandenbroucke JP. Enhancement by factor V Leiden mutation of risk of deep-vein thrombosis associated with oral contraceptives containing a third-generation progestagen. Lancet 1995;346:1593-6. 10.1016/S0140-6736(95)91929-5 pmid:7500751. [DOI] [PubMed] [Google Scholar]
- 37.Gerstman BB, Piper JM, Tomita DK, Ferguson WJ, Stadel BV, Lundin FE. Oral contraceptive estrogen dose and the risk of deep venous thromboembolic disease. Am J Epidemiol 1991;133:32-7.pmid:1983896. [DOI] [PubMed] [Google Scholar]
- 38.Haute Autorité de Santé. Correct use of medicinal products: Combined oral contraceptives: prefer 1st or 2nd generation pills. November 2012. www.hassante.fr/portail/upload/docs/application/pdf/2012-12/contraceptis_oraux_3_g_fiche_bum.pdf
- 39.French Ministry of Labour. Employment and Health. Guide to the methodology of production of information on medical activity and billing in medicine, surgery, obstetrics and dentistry. Official Bulletin No. 2011/6 b. Special issue. June 2011. www.sante.gouv.fr/IMG/pdf/sts_20110006_0001_p000.pdf
- 40.Casez P, Labarère J, Sevestre MA, et al. ICD-10 hospital discharge diagnosis codes were sensitive for identifying pulmonary embolism but not deep vein thrombosis. J Clin Epidemiol 2010;63:790-7. 10.1016/j.jclinepi.2009.09.002 pmid:19959332. [DOI] [PubMed] [Google Scholar]
- 41.Aboa-Eboulé C, Mengue D, Benzenine E, et al. How accurate is the reporting of stroke in hospital discharge data? A pilot validation study using a population-based stroke registry as control. J Neurol 2013;260:605-13. 10.1007/s00415-012-6686-0 pmid:23076827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suissa S, Spitzer WO, Rainville B, Cusson J, Lewis M, Heinemann L. Recurrent use of newer oral contraceptives and the risk of venous thromboembolism. Hum Reprod 2000;15:817-21. 10.1093/humrep/15.4.817 pmid:10739826. [DOI] [PubMed] [Google Scholar]
- 43.Zhang G, Xu X, Su W, Xu Q. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health 2014;45:736-45.pmid:24974658. [PubMed] [Google Scholar]
- 44.Dinger JC, Heinemann LA, Kühl-Habich D. The safety of a drospirenone-containing oral contraceptive: final results from the European Active Surveillance Study on oral contraceptives based on 142,475 women-years of observation. Contraception 2007;75:344-54. 10.1016/j.contraception.2006.12.019 pmid:17434015. [DOI] [PubMed] [Google Scholar]
- 45.Bajos N, Bohet A, Le Guen M, Moreau C. Fecond Survey Team. Contraception in France: new context, new practices?Popul Soc (Paris) 2012;492 www.ined.fr/fichier/t_publication/1606/publi_pdf2_pesa492.pdf. [Google Scholar]
- 46.Tricotel A, Collin C, Zureik M. Impact of the sharp changes in the use of contraception in 2013 on the risk of pulmonary embolism in France. J Thromb Haemost 2015;13:1576-80. 10.1111/jth.13053 pmid:26179493. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary information