Abstract
We conducted a systematic review to evaluate the burden of late vitamin K deficiency bleeding (VKDB) and the effect of vitamin K prophylaxis on the incidence of VKDB. We searched MEDLINE and other electronic databases, and included all observational studies including population surveys as well as randomized controlled trials (RCT). The median (interquartile range) burden of late VKDB was 35 (10.5 to 80) per 100 000 live births in infants who had not received prophylaxis at birth; the burden was much higher in low- and middle-income countries as compared with high-income countries-80 (72 to 80) vs 8.8 (5.8 to 17.8) per 100 000 live births. Two randomized trials evaluated the effect of intramuscular (IM) prophylaxis on the risk of classical VKDB. Although one trial reported a significant reduction in the incidence of any bleeding (relative risk (RR) 0.73, 95% confidence interval (CI) 0.56 to 0.96) and moderate to severe bleeding (RR 0.19, 0.08 to 0.46; number needed to treat (NNT) 74, 47 to 177), the other trial demonstrated a significant reduction in the risk of secondary bleeding after circumcision in male neonates (RR 0.18, CI 0.08 to 0.42; NNT 9, 6 to 15). No RCTs evaluated the effect of vitamin K prophylaxis on late VKDB. Data from four surveillance studies indicate that the use of IM/subcutaneous vitamin K prophylaxis could significantly reduce the risk of late VKDB when compared with no prophylaxis (pooled RR 0.02; 95% CI 0.00 to 0.10). When compared with IM prophylaxis, a single oral dose of vitamin K increased the risk of VKDB (RR 24.5; 95% CI 7.4 to 81.0) but multiple oral doses did not (RR 3.64; CI 0.82 to 16.3). There is low-quality evidence from observational studies that routine IM administration of 1 mg of vitamin K at birth reduces the incidence of late VKDB during infancy. Given the high risk of mortality and morbidity in infants with late VKDB, it seems appropriate to administer IM vitamin K prophylaxis to all neonates at birth. Future studies should compare the efficacy and safety of multiple oral doses with IM vitamin K and also evaluate the optimal dose of vitamin K in preterm neonates.
Introduction
Vitamin K is essential for the γ-carboxylation of glutamic acid residues of coagulant factors II, VII, IX and X. Deficiency of vitamin K leads to inadequate activity of these factors, resulting in bleeding. As opposed to adults, neonates have reduced stores of vitamin K at birth owing to insufficient placental transfer.1 This is compounded by deficient vitamin K content in breast milk2 resulting in higher levels of proteins induced in the absence of vitamin K in breastfed neonates.3
Vitamin K deficiency bleeding (VKDB) is usually categorized into three major groups based on the age of onset: early (first 24 h of life), classical (second to seventh day) and late (2 to 12 weeks of life). Although early VKDB is due to placental transfer of maternal drugs that inhibit vitamin K activity, the classical form occurs because of the low intake via breast milk. Late VKDB is often linked to malabsorption secondary to liver disease and poor intake of vitamin K. Intracranial bleeding (30 to 60%) is the predominant manifestation of late onset VKDB, whereas bleeding from the gastrointestinal tract and/or umbilicus is the usual presenting feature in classical disease.4 The high rates of mortality and morbidity following VKDB—particularly late VKDB—raised a call for an effective preventive strategy in the early 1900s.
A large study published in The Lancet in the 1940s showed a fivefold reduction in death from hemorrhage in infants who were given 1 mg of vitamin K3 (menadione) at delivery. The results generated a huge interest in routine vitamin K prophylaxis.5 With the introduction of the natural, fat-soluble vitamin K1 (phylloquionone) in place of synthetic vitamin K3 (that was associated with increased risk of hemolysis and kernicterus), most countries started using routine prophylaxis.6
However, the strategy of routine prophylaxis is not free of any pitfalls. The usual prophylactic dose (1 mg) is ~1000 times more than the daily requirement. Experimental studies have shown increased sister chromatid exchange in lymphocyte suspensions and mutagenic activity at such high concentrations. Also, intramuscular (IM) administration can cause local trauma, injury to vessels and nerves, abscesses and muscle hematoma. Not surprisingly, some countries are reluctant about universal prophylaxis and instead practice selective prophylaxis to at-risk neonates only.
Given the lack of consensus, the WHO (World Health Organization) did not make a universal recommendation on routine vitamin K prophylaxis in the first edition of its Pocket book of hospital care for children.7 Instead, it advised health providers to follow their respective national guidelines to decide the need for prophylaxis.7 In 2010, WHO reviewed the available evidence on key questions including routine vitamin K prophylaxis to update the recommendations in the second edition of its Pocket book of hospital care for children.8 As a part of this process, we conducted the present systematic review to synthesize the evidence on the need for and efficacy of vitamin K prophylaxis at birth.
Methods
Objectives and outcomes
The two major objectives of this review were to evaluate: (1) the burden of VKDB by estimating the incidence of late VKDB in infants who did not receive vitamin K prophylaxis at birth; and (2) the effect of vitamin K prophylaxis on the incidence of classical and late VKDB in neonates and infants up to 1 year of age.
Types of studies
For objective 1, we included prospective and retrospective cohort studies as well as cross-sectional surveys; for objective 2, we included randomized controlled trials and ecological/nationwide surveillance studies. Studies from both high-income and low- and middle-income countries (LMICs) were considered for inclusion in the review.
Types of participants
Studies reporting data on neonates and infants up to the age of 1 year were eligible for inclusion.
Types of interventions
Intervention (for objective 2): administration of vitamin K in the first 24 h after birth, irrespective of the route (oral/IM), dose (single/multiple) or preparation (K1/K2/K3 and mixed micellar preparation).
Control: placebo or no prophylaxis.
Outcomes and their definitions
The outcomes of interest were the incidence of classical and late VKDB in the neonatal period and infancy, respectively. VKDB was defined as any bleeding that occurred due to inadequate activity of vitamin K-dependent coagulation factors (diagnosed by prolonged prothrombin time but normal fibrinogen level and platelet count) and was correctable by replacement of vitamin K. Classic VKDB referred to VKDB occurring between 2 and 7 days of life while late VKDB referred to VKDB occurring after the first week of life up to 1 year of age.
Search methods for identification of studies
We initially searched electronic bibliographic databases including MEDLINE, Embase, Cochrane CENTRAL, Web of Science, CINAHL, IndMed and the clinical trials website (www.clinicaltrials.gov) up to September 2009. We used the following search terms for searching Medline: (Newborn OR infan* OR neonat*) AND (vitamin K prophylaxis). Similar terms were used for searching the other databases. No language restrictions were used. We later updated the search in December 2013. Owing to practical reasons we could only update the search in MEDLINE, Cochrane CENTRAL and IndMed.
Related conference proceedings—for example, Pediatric Academic Societies annual meetings for the years 2000 to 2013—were also searched for relevant abstracts. For further identification of ongoing trials, the website www.clinicaltrials.gov was searched.
We scanned the title and abstract of the retrieved citations to exclude those that were obviously irrelevant. We retrieved the full text of the remaining studies to identify relevant articles. The search strategy is summarized in the Supplementary Information (Supplementary Table 1).
Data extraction
Data extraction was carried out using a pre-designed data extraction form pilot-tested by the review authors (MJS, PK and RA). We extracted information on the study setting (country, type of population and socioeconomic status), study intervention (type of conventional treatment, description of vitamin K used-including dose and frequency), sample size, length of follow-up, randomization procedure, allocation concealment, risk of bias and outcomes as listed above.
For dichotomous outcomes, the total number of participants for each group and the number of participants experiencing an event were extracted. Three review authors (MJS, PK and AC) independently assessed the methodological quality of the selected studies. Quality assessment of the randomized trials was undertaken using the standard criteria of allocation concealment, blinding and completeness of follow-up (classified as yes, no or unclear). Disagreements between the authors were resolved by consensus.
Statistical analysis
For the first objective, data from the available studies were tabulated to obtain the median incidence of VKDB in LMICs and high-income countries. We intended to pool the incidence if the relevant data were available. For objective 2, meta-analysis of the studies with complete data was carried out using Stata 11.2 (StataCorp, College Station, TX, USA). We used the fixed effects model for meta-analysis. For categorical outcomes, the relative risk (RR) and 95% confidence interval (CI) are reported. For significant findings, the number needed to treat (NNT) was calculated along with 95% CIs.
Results
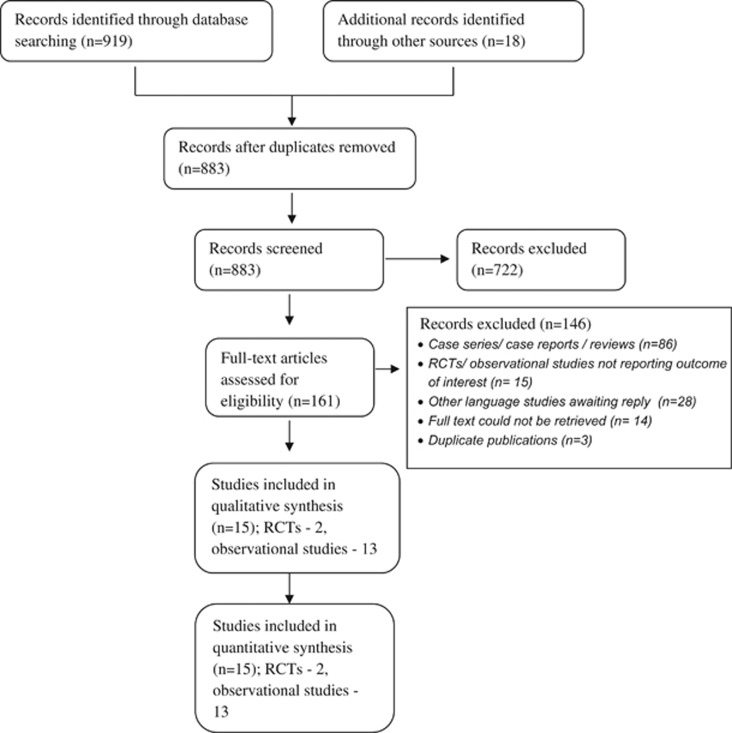
A total of 883 citations were retrieved, of which 722 were excluded after screening the title/abstract. Of the remaining 161 citations, 15 were found to be eligible for inclusion in the review (Figure 1).
Figure 1.
Flow chart depicting the selection of studies included in the review. RCT, randomized control trial.
Burden of late VKDB in populations that did not receive vitamin K prophylaxis
Table 1 lists the studies that provided data on the incidence of VKDB in infants who did not receive vitamin K prophylaxis at birth. Almost all of the studies listed were surveillance studies in which different hospitals were requested to report on cases of hemorrhage disease of the newborn admitted during the study period.
Table 1. Burden of late VKDB in the population.
| Study | Country | Period of study | Method of data collection | Incidence per 100 000 live births (95% CI) |
|---|---|---|---|---|
| Khanjanasthiti et al.22 | Thailand | 1977–1978 | Not known | 80 |
| Nagao and Nakayama23 a | Japan | 1978–1989 | Nationwide hospital study | 25 |
| Hanawa et al.11 | Japan | 1981–1983 | Large pediatric hospital survey | 10.5 (7.0–15.0) |
| Ungchusak et al.24 | Thailand | 1983 | Nationwide hospital survey | 35 |
| von Kries13 b | Germany | 1988–1989 | Pediatric hospital survey | 7.2 (3.5–13.3) |
| McNinch and Tripp14 | British Isles | 1988–1990 | Pediatrician-based surveillance | 4.4 (2.0–8.4) |
| Chuansumrit et al.15 | Thailand | 1981–1984 | Nationwide hospital survey | 72.0 |
| Newton-Sánchez et al.25 a | Mexico | 1997–2000 | Retrospective study in a level 3 hospital, data of which are extrapolated to population (average annual live births in the state) | 80 |
| Zhou et al.26 a | China | 2002c | Survey of five districts and six counties in Shandong Province (using stratified cluster sampling) | 327 (overall including classical VKDB) |
Abbreviations: CI, confidence interval; VKDB, vitamin K deficiency bleeding.
Status of vitamin K prophylaxis not mentioned clearly in the original study.
The published study reported all forms of VKDB–data provided here on late VKDB are from the review by von Kries.13
Full text could not be retrieved; refers to the year of publication.
Table 2 summarizes the estimated burden of late VKDB in different settings. The median interquartile range burden in the absence of any prophylaxis is 35 (10.5 to 80) per 100 000 live births; the median burden in LMIC and high-income countries is 80 (72 to 80) and 8.8 (5.8 to 17.8) per 100 000 live births, respectively.
Table 2. Median burden of late VKDB in different settings.
| Setting | Median incidence (per 100 000 live births) | Interquartile range |
|---|---|---|
| Overalla | 35 | 10.5–80 |
| LMICs | 80 | 72–80 |
| High-income countries | 8.8 | 5.8–17.8 |
Abbreviations: LMICs, low- and middle-income countries; VKDB, vitamin K deficiency bleeding.
Irrespective of the country and prophylaxis status.
Effect of vitamin K prophylaxis on classical VKDB
Only two trials9, 10 on vitamin K prophylaxis included classical hemorrhage disease of the newborn as one of the pre-defined outcome variables (Table 3). Sutherland et al. used two different dosage regimes of vitamin K3 (100 mcg and 5 mg) and compared them with placebo. Enrolled neonates were either breast- or formula-fed and were followed-up for the occurrence of bleeding until discharge from the hospital (usually the fourth or fifth day of life). There was a significant reduction in the incidence of any bleeding (RR 0.73; 95% CI 0.56 to 0.96) as well as moderate to severe bleeding (RR 0.19; 0.08 to 0.46; NNT 74, 47 to 177) following vitamin K prophylaxis (Table 3). In the study by Vietti et al. vitamin K1 (5 mg IM) was administered to male neonates born on even-numbered days during a trial period of 3 months. There was a significant reduction in the incidence of secondary bleeding after circumcision in neonates who received vitamin K prophylaxis (RR 0.18, 0.08 to 0.42; NNT 9, 6 to 15). The results of the two studies could not be pooled because of the different nature of the outcomes (spontaneous bleeding vs post-circumcision bleeding).
Table 3. Effect of vitamin K prophylaxis on classic VKDB/HDN.
| Study, design and level of evidence | Participants | Comparison groups | Outcome measure | Effect measure (95% CI) |
|---|---|---|---|---|
| Sutherland et al.9 RCT | Full-term infants weighing 2260 g (5 lbs) or more; both breast and formula fed | Three groups: IM 100 mcg vitamin K3 (n=1132); IM 5 mg vitamin K3 (n=1063); placebo (normal saline; n=1143) | Minor bleeding (no local measures), moderate (innocuous sites requiring local measures) and severe (significant location such as central nervous system) bleeding | Any bleeding: RR 0.73 (0.56, 0.96) RD −0.02 (−0.038, −0.002) NNT 50 (26–479) moderate to severe bleeding: RR 0.19 (0.08, 0.46) RD −0.01 (−0.02, −0.006) NNT 74 (47–177) |
| Vietti et al.10 Quasi-RCT | Male infants for whom circumcision was performed on mothers' request | Two groups: IM 5 mg vitamin K3; no prophylaxis | Secondary bleeding after circumcision | RR 0.18 (0.08, 0.42) RD −0.11 (−0.16, −0.07) NNT 9 (6–15) |
Abbreviations: HDN, hemorrhage disease of the newborn; IM, intramuscular; NNT, number needed to treat; RCT, randomized controlled trials; RD, risk difference; RR, relative risk; VKDB, vitamin K deficiency bleeding.
Note: Sutherland's study used two dosage regimes–100 mcg and 5 mg of vitamin K3; the data from these two groups are combined for the purpose of this review.
Effect of vitamin K prophylaxis on late VKDB
We did not find any randomized or quasi-randomized trials that evaluated the effect of vitamin K prophylaxis on the incidence of late VKDB. Therefore, we used data from nationwide surveys conducted in four countries to estimate the effect (Table 4) of vitamin K prophylaxis.
Table 4. Incidence of late VKDB/HDN in the population.
| Study, year of study | Country, method | Route and dose of vitamin K in vitamin K prophylaxis group | Incidence in vitamin K prophylaxis group (per 100 000 live births; 95% CI) | Incidence in no prophylaxis group (per 100 000 live births; 95% CI) | RR (95% CI) |
|---|---|---|---|---|---|
| Hanawa et al.,11 1981–1985 Takahashi et al.,12 1999–2004 | Japan; large pediatric hospital survey 1981 (first) 1985 (second) 1985–1988 (third) 1988–1990 (fourth) | Not clear in first survey; in later surveys: oral (days 1, 7 and 28) | 2.8 (2.0–3.8) 1.9 (1.2–3.0) | 10.5 (7.0–15.0)a | — |
| von Kriesb,13 1988–1989 | Germany; pediatric hospital survey | Oral: 1–2 mg IM or SC: 1 mg | IM: 0.25 (0.3–1.3) oral: 1.4 (0.2–5.2) | 7.2 (3.5–13.3) | IM/SC vs no: 0.03 (0.004–0.25) oral vs no: 0.2 (0.04–0.91) |
| McNinch and Tripp,14 1988–1990 | British Isles; pediatrician-based surveillance | Oral: 1–2 mg IM: 1 mg | IM: 0 (0–0.4) oral: 1.5 (0.6–3.2) | 4.4 (2.0–8.4) | IM/SC vs no: 0.01 (0.001–0.21) oral vs no: 0.35 (0.13–0.93) |
| Chuansumrit et al.,15 1981–1995 | Thailand; nationwide hospital survey: 1981–1984 1988–1995 | 2 mg orally for normal infants and 0.5–1 mg IM for sick neonates | 4.2–7.8 | 72.0 | Not available |
Abbreviations: CI, confidence interval; HDN, hemorrhage disease of the newborn; IM, intramuscular; RR, relative risk; SC, subcutaneous; VKDB, vitamin K deficiency bleeding.
Full text could not be retrieved; refers to the year of publication.
The published study reported all forms of VKDB–data provided here (on late VKDB) are from the review by von Kries.13
A total of five nationwide surveys on VKDB were conducted in Japan over a period of 20 years from 1981 to 2004.11, 12 It is not clear whether the neonates received routine vitamin K prophylaxis at the time of the first survey, but almost all neonates received prophylactic vitamin K during the subsequent surveys. The incidence of VKDB declined nearly four times from 10.5 per 100 000 live births in the first survey to 2.8 (95% CI 2.0 to 3.8) per 100 000 by 1988 (third survey), and further to 1.9 (1.2 to 3.0) per 100 000 live births by the fifth survey.12
von Kries evaluated the efficacy of vitamin K prophylaxis in prevention of VKDB in early infancy during a 15-month period between 1988 and 1989.13 The number of cases of VKDB and exposure to vitamin K prophylaxis were collected by a questionnaire sent to all pediatric hospitals in then West Germany; the population denominators were collected by a survey of all obstetric hospitals. Response rates were 85 and 68% from pediatric and obstetric hospitals, respectively. About 56% of the hospitals employed single parenteral prophylaxis (1 mg IM or subcutaneous), 19% used oral prophylaxis (1 to 2 mg given as a single dose at birth) and 19% did not give any prophylaxis. No data were available for 7% of hospitals. Thirteen cases of VKDB in early infancy were confirmed (10, 1 and 2 in no prophylaxis, parenteral and oral prophylaxis groups, respectively). IM vitamin K reduced the risk of late VKDB by ~97% while prophylaxis by the oral route reduced the risk by 80% (Table 4). In a study by McNinch and Tripp, cases of VKDB were enrolled over 2 years from 1988 to 1990 by means of the report card system of the British Paediatric Surveillance Unit.14 Birth data were obtained from the Office of Population Censuses and Surveys and from the Central Statistics Office. Out of the 27 infants with VKDB, 20 did not receive any prophylaxis while the other seven received oral prophylaxis. Ten infants developed intracranial bleeding. None of the infants who received IM prophylaxis developed VKDB. The RR of late VKDB in infants who received IM vitamin K prophylaxis as compared with those who did not receive prophylaxis was 0.01 (95% CI 0.001 to 0.21); the corresponding RR in infants receiving oral prophylaxis was 0.35 (0.13 to 0.93).14
In the Thailand surveillance study reported by Chuansumrit et al., two time periods were studied—1981 to 1984 when no prophylaxis was routinely used, and between 1988 and 1995 when most neonates were supplemented (2 mg orally for normal and 0.5 to 1 mg IM for sick neonates). The response rates in the survey were 58.2 and 67%, respectively, for the two time periods. VKDB (total n= 830) was reported mainly in exclusively breastfed infants (92%) who did not receive vitamin K prophylaxis at birth (90%). The incidence of VKDB significantly declined from 72 per 100 000 live births in the earlier time period to 4.2 to 7.8 per 100 000 live births in the later period.15 The incidence of intracranial hemorrhage was high (82%) as was the case fatality rate (24%).
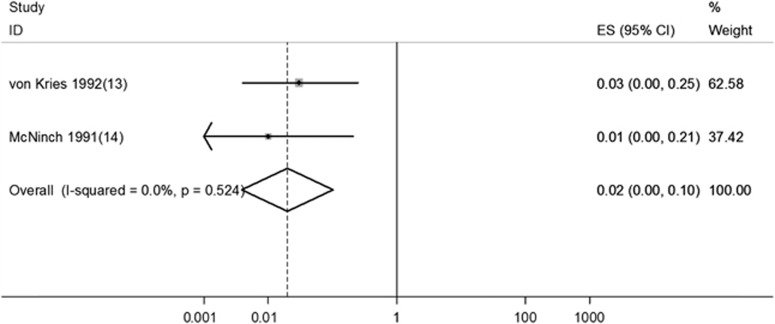
Pooled analysis of the two studies from Germany and the United Kingdom showed a significant reduction in the incidence of late VKDB following IM vitamin K prophylaxis (Figure 2).
Figure 2.
Effect of intramuscular vitamin K prophylaxis on late vitamin K deficiency bleeding. ES, effect size; ID, identification.
Discussion
The current review attempts to answer an important area of uncertainty in the routine care of all neonates at birth. The major findings of the review are: (1) a significant burden of late VKDB—particularly in LMICs—in the absence of routine vitamin K prophylaxis; and (2) the huge benefits observed on the incidence of late VKDB following routine prophylaxis at birth. Although the quality of evidence for the latter is low because of the lack of randomized controlled trials, the finding has major implications for policy-making.
The burden of late VKDB is significant in the absence of vitamin K prophylaxis at birth. Given the high risk of mortality and adverse neurodevelopmental outcomes in the survivors—22 and 25% to 67%, respectively, in one study from Thailand16—the burden assumes importance from a public health point of view. The reported incidence did vary widely in the included studies, possibly because of the different settings—LMICs vs high-income countries (Table 1). The median (interquartile range) incidence in the former was found to be almost 10 times than that of the latter—80 (72 to 80) vs 8.8 (5.8 to 17.8) per 100 000 live births (Table 2). Interestingly, the difference between the two settings persists even with the introduction of vitamin K prophylaxis, the magnitude of difference being almost the same (6 vs 0.76 per 100 000 live births; Supplementary Table 2). The possible reasons for this discrepancy are the differences in ethnicity, seasonality and latitude (higher incidence in summer-tropical countries are likely to have a higher incidence), and exclusive breastfeeding rates (owing to low vitamin K content in breast milk as opposed to formula and maternal nutritional status).13
We did not find any randomized trial evaluating the effect of routine prophylaxis at birth on the incidence of late VKDB. The only two available randomized trials on IM vitamin K vs placebo at birth examined the effect on classical VKDB. Both of them were conducted in the 1960s, used IM vitamin K3 for prophylaxis, and demonstrated a significant reduction in the incidence of bleeding of any severity in the first week of life (Table 3).9, 10 A few other randomized trials compared either a single oral dose of vitamin K with placebo or oral with IM route of vitamin K, but none of them assessed clinical bleeding.
The effect of vitamin K on late VKDB is currently available from only four surveillance studies. The pooled effect of the two studies with complete data demonstrated a 98% reduction (95% CI 90 to 100%) in the incidence of late VKDB following IM vitamin K prophylaxis (Figure 2). Assuming the control risk to be 80 per 100 000 live births (median incidence in LMICs), the NNT to prevent one additional case of major clinical bleeding in infancy due to vitamin K deficiency would be 1275 (95% CI 1042 to 1667). Admittedly, the NNT is not small but the easy availability of the drug, ease of administration (single dose at birth that does not involve additional visits for the family or health providers), low cost17 and the apparent lack of major adverse effects (see below) tilt the balance in favor of universal prophylaxis at birth. Assuming a cost of US$ 1.00 per injectable dose, Victora and Van Haecke estimated that saving one disability-adjusted life year would cost US$ 52 and US$ 133 in high- and intermediate-incidence scenarios, respectively.17 As per a World Bank report that classifies interventions costing under $100 per disability-adjusted life year as cost-effective,18 IM vitamin K prophylaxis would be cost-effective in high-incidence scenarios, that is, incidence of 72 or more per 100 000 live births.
Between the two routes of administration of vitamin K, IM route was found to be more beneficial than the oral route in the two studies from Germany and the United Kingdom. The reported RRs for IM and oral routes were 0.03 and 0.2, respectively, in the former study13 and 0.01 and 0.35, respectively, in the latter study.14 The disadvantage of oral vitamin K may possibly be due to poor absorption and a shorter duration of effect. Indeed, multiple oral doses of vitamin K seemed to offer an advantage over a single oral dose. For example, in the British surveillance study, a significantly higher risk of VKDB was observed in infants receiving a single dose of oral vitamin K than in those receiving IM prophylaxis at birth (RR 24.53; 95% CI 7.4 to 81); no such difference was found in infants receiving multiple oral doses extending beyond the first week of life (RR 3.64; 0.82 to 16.3).19 The Cochrane review also found no evidence of a difference between the oral and IM route in effects on biochemical indices of coagulation status.20 As compared with IM prophylaxis, multiple oral doses are cheaper and do not have the theoretical risk of mutagenicity.17, 21 However, they are not easily available in many LMICs.
Strengths and limitations
We have attempted to systematically review and synthesize the available evidence on the burden of VKDB and the effects of vitamin K prophylaxis on the incidence of VKDB. Unlike the Cochrane review, we included observational studies to evaluate the effects of routine prophylaxis so that policy-makers and other stakeholders may make an informed decision. We focused on only the outcomes of public health interest such as major bleeding, and not on biochemical parameters such as vitamin K levels.
This review has major limitations. First, we did not evaluate the safety of the intervention. Although later studies did not confirm the association between IM vitamin K prophylaxis and the risk of childhood cancer, the theoretical possibility of mutagenicity cannot be excluded. Second, the evidence for an effect on late VKDB is available only from surveillance studies. Because of the low response rates in many of these surveys, the actual incidence of late VKDB may have been underestimated.
Implications for policy-makers
With significant benefits observed in the incidence of VKDB, policy-makers and other stakeholders are likely to give a high value to the routine administration of IM vitamin K (1 mg) at birth. The WHO also now recommends routine prophylaxis in all resource-restricted countries.8
Implications for researchers
There is a definite need to evaluate the efficacy of using smaller doses (between 100 and 1000 mcg) of IM vitamin K in preterm infants. In addition, the effect of multiple oral doses vs IM vitamin K in term neonates needs to be evaluated systematically.
Conclusions
There is low-quality evidence from observational studies that routine IM administration of 1 mg of vitamin K at birth reduces the incidence of late VKDB during infancy. Given the high risk of mortality and morbidity in infants with late VKDB, it seems advisable to administer IM vitamin K prophylaxis to all neonates at birth. Future studies should compare the efficacy and safety of multiple oral doses with IM vitamin K and also evaluate the optimal dose of vitamin K in preterm neonates.
Acknowledgments
We acknowledge Dr Sushil Kumar for help in searching the various databases. The Department of Maternal, Newborn, Child and Adolescent Health and Development, World Health Organization, Geneva, Switzerland funded this review.
Author contributions
MJS developed the study protocol, extracted data, did the statistical analysis and wrote the manuscript. AC, AT and PK applied the search strategy, retrieved the articles and extracted data. AC also helped in writing the manuscript. RA supervised data extraction and helped in statistical analysis. VKP guided development of the protocol, supervised data extraction and modified the manuscript. MJS and VKP act as the guarantors of the paper.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Journal of Perinatology website (http://www.nature.com/jp).
Supplementary Material
References
- Shearer MJ. Vitamin K metabolism and nutriture. Blood Rev 1992; 6(2): 92–104. [DOI] [PubMed] [Google Scholar]
- Van Hasselt PM, de Koning TJ, Kvist N, de Vries E, Lundin CR, Berger R et al. Prevention of vitamin K deficiency bleeding in breastfed infants: lessons from the Dutch and Danish biliary atresia registries. Pediatrics 2008; 121(4): e857–e863. [DOI] [PubMed] [Google Scholar]
- Widdershoven J, Lambert W, Motohara K, Monnens L, de Leenheer A, Matsuda I et al. Plasma concentrations of vitamin K1 and PIVKA-II in bottle-fed and breast-fed infants with and without vitamin K prophylaxis at birth. Eur J Pediatr 1988; 148(2):139–142. [DOI] [PubMed] [Google Scholar]
- Sutor AH. Vitamin K deficiency bleeding in infants and children. Semin Thromb Hemost 1995; 21: 317–329. [DOI] [PubMed] [Google Scholar]
- Lehmann J. Vitamin K as a prophylactic in 13,000 babies. Lancet 1944; i: 493–494. [Google Scholar]
- American Academy of PediatricsCommittee on Nutrition. Vitamin K compounds and the water soluble analogues. Pediatrics 1961; 28: 7. [Google Scholar]
- WHOPocket Book of Hospital Care for Children: Guidelines for the management of Common Illnesses with Limited Resources. WHO: Geneva, 2005. [Google Scholar]
- WHOPocket Book of Hospital Care for Children: Guidelines for the Management of Common Illnesses with Limited Resources. 2nd edn. WHO: Geneva, 2013. [Google Scholar]
- Sutherland JM, Glueck HI, Gleser G. Hemorrhagic disease of the newborn. Breast feeding as a necessary factor in the pathogenesis. Am J Dis Child 1967; 113(5): 524–533. [DOI] [PubMed] [Google Scholar]
- Vietti TJ, Murphy TP, James JA, Pritchard JA. Observations on the prophylactic use of vitamin K in the newborn infant. J Pediatr 1960; 56: 343–346. [DOI] [PubMed] [Google Scholar]
- Hanawa Y, Maki M, Murata B, Matsuyama E, Yamamoto Y, Nagao T et al. The second nation-wide survey in Japan of vitamin K deficiency in infancy. Eur J Pediatr 1988; 147(5): 472–477. [DOI] [PubMed] [Google Scholar]
- Takahashi D, Shirahata A, Itoh S, Takahashi Y, Nishiguchi T, Matsuda Y. Vitamin K prophylaxis and late vitamin K deficiency bleeding in infants: fifth nationwide survey in Japan. Pediatr Int 2011; 53(6): 897–901. [DOI] [PubMed] [Google Scholar]
- von Kries R. Vitamin K prophylaxis–a useful public health measure? Paediatr Perinat Epidemiol 1992; 6(1): 7–13. [DOI] [PubMed] [Google Scholar]
- McNinch AW, Tripp JH. Haemorrhagic disease of the newborn in the British Isles: two year prospective study. BMJ 1991; 303(6810): 1105–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuansumrit A, Isarangkura P, Hathirat P. Vitamin K deficiency bleeding in Thailand: a 32-year history. Southeast Asian J Trop Med Public Health 1998; 29(3): 649–654. [PubMed] [Google Scholar]
- Isarangkura PB, Chuamsumrit A, Hathirat P. Idiopathic vitamin K deficiency in infants: its roles in infant morbidity and childhood handicaps. Thromb Haemost 1989; 62: 363. [Google Scholar]
- Victora CG, Van Haecke P. Vitamin K prophylaxis in less developed countries: policy issues and relevance to breastfeeding promotion. Am J Public Health 1998; 88(2): 203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World BankWorld Development Report 1993. Investing in Health. Oxford University Press Inc.: New York, NY, USA, 1993. [Google Scholar]
- Busfield A, Samuel R, McNinch A, Tripp JH. Vitamin K deficiency bleeding after NICE guidance and withdrawal of Konakion Neonatal: British Paediatric Surveillance Unit study, 2006-2008. Arch Dis Child 2013; 98(1): 41–47. [DOI] [PubMed] [Google Scholar]
- Puckett RM, Offringa M. Prophylactic vitamin K for vitamin K deficiency bleeding in neonates. Cochrane Database Syst Rev 2000; (4): CD002776. [DOI] [PMC free article] [PubMed]
- Sutor AH, von Kries R, Cornelissen EA, McNinch AW, Andrew M. Vitamin K deficiency bleeding (VKDB) in infancy. ISTH Pediatric/Perinatal Subcommittee. International Society on Thrombosis and Haemostasis. Thromb Haemost 1999; 81(3): 456–461. [PubMed] [Google Scholar]
- Khanjanasthiti P, Benchakarn V, Saksawad A, Khantanaphar S, Posayanond P. Perinatal problems in rural Thailand. J Trop Pediatr 1984; 30(2): 72–78. [DOI] [PubMed] [Google Scholar]
- Nagao T, Nakayama K. Vitamin K deficiency in infancy in Japan. Pediatrics 1984; 74(2): 315–316. [PubMed] [Google Scholar]
- Ungchusak K, Tishyadhigama S, Choprapawon C, Sawadiwutipong W, Varintarawat S. Incidence of idiopathic vitamin K deficiency in infants: a national, hospital based, survey in Thailand, 1983. J Med Assoc Thai 1988; 71(8): 417–421. [PubMed] [Google Scholar]
- Newton-Sánchez OA, Basurto-Celaya G, Richardson V, Belkind-Gerson J. Re-emergence of hemorrhagic disease in newborns. Implications for its prevention. Salud Pública Méx 2002; 44(1): 57–59. [PubMed] [Google Scholar]
- Zhou F, He S, Wang X. An epidemiological study on vitamin K deficiency bleeding in infants under six months. Zhonghua Yu Fang Yi Xue Za Zhi 2002; 36(5): 305–307. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.