Abstract
We expressed the wild-type rplC and mutated rplC (Cys154Arg) genes, respectively, in Mycobacterium tuberculosis H37Ra and H37Rv in an attempt to delineate the role of rplC (Cys154Arg) regarding oxazolidinone resistance. An increase of the MICs of linezolid (LZD) and sutezolid (PNU-100480, PNU) against the recombinant mycobacteria with overexpressed rplC mutation (Cys154Arg) was found, suggesting the rplC gene is a determinant of bacillary susceptibilities to LZD and PNU.
TEXT
Currently, global control of tuberculosis (TB) is faced with the formidable challenge of worsening scenarios of drug-resistant disease, notably multidrug-resistant tuberculosis (MDR-TB), with bacillary resistance to at least rifampin and isoniazid, and extensively drug-resistant tuberculosis (XDR-TB), with additional resistance to fluoroquinolone(s) and second-line injectable agent(s) (1). Linezolid (LZD) has been widely used for the treatment of complicated MDR-TB and XDR-TB, improving the outcome of patients (2–5). Sutezolid (PNU-100480, PNU), a new congener of the same class, has also entered phase IIB TB treatment trials (http://www.newtbdrugs.org/project.php?id=135) after showing very good activity in the mouse TB model (6) and in the human whole-blood bactericidal system (7, 8).
Richter and colleagues (9) first reported on LZD-resistant clinical isolates of Mycobacterium tuberculosis with a 4- to 8-fold rise of the MICs from the susceptibility level of ≤1 μg/ml (10, 11). Whole-genome sequencing identified a point mutation, T460C (Cys154Arg), in the rplC gene that might constitute a putative marker for LZD resistance in M. tuberculosis (12). The rplC gene encodes the ribosomal protein L3 located in the S10 operon of the Escherichia coli chromosome, encoding 11 ribosomal proteins (13). The main part of L3 is positioned on the surface of the 50S ribosomal subunit, but a branched loop extends close to the peptidyl transferase center, the binding site for many different ribosomal antibiotics (14). Until now, the mechanisms of LZD resistance in M. tuberculosis were not yet fully unraveled because the association of rplC Cys154Arg mutation with LZD and PNU in M. tuberculosis was not confirmed by molecular genetic methods. Herein, we constructed recombinant strains to determine whether rplC Cys154Arg mutation would result in resistances to LZD and PNU in M. tuberculosis.
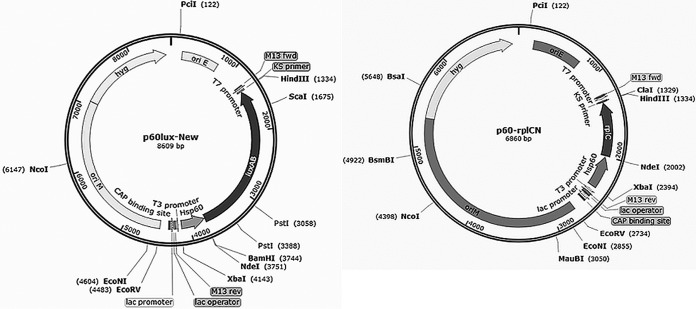
The oxazolidinone susceptibilities were evaluated on Middlebrook 7H11 medium (Difco). The rplC gene is preceded by an upstream rpsJ gene, and a putative promoter was identified (Fig. 1A); hence, primers rplCf and rplCr (Table 1) for amplification of the promoter-rpsJ-rplC fragment (Fig. 1A) were designed with EcoRI and XbaI restriction sites at the 5′ terminals, respectively, and the fragment was cloned into the integrative plasmid pMH94A between EcoRI and XbaI sites to create pLZD-N (Fig. 2; Table 2). The rplC in the construct pLZD-N was confirmed by DNA sequencing (BGI, Shenzhen, China). We further induced a point mutation of the rlpC gene at T460C (Cys154Arg) in pLZD-N creating the plasmid pLZD-NM (Generay Biotech, Shanghai, China) (Table 2). The rplC and rplC Cys154Arg genes were amplified by PCR from pLZD-N and PLZD-NM plasmids, respectively, using the oligonucleotide primers (rplC-F and rplC-R; Table 2) of the rplC open reading frame only, and were cloned into the NdeI-HindIII sites of an extrachromosomal plasmid p60luxN (15) under the control of a strong promoter, Hsp60, to yield p60-rplCN (Fig. 3) and p60-rplcNM. The four plasmids pLZD-N, pLZD-NM, p60-rplCN, and p60-rplcNM were transformed into wild-type M. tuberculosis (H37Rv and H37Ra) through electroporation as described previously (16). Positive selection was confirmed by PCR amplification of the kanamycin (KAN)-resistant marker gene (KANr) in pLZD-N and pLZD-NM using primers kan-r and kan-f or PCR of the hygromycin-resistant marker gene (hyg) in p60-rplCN and p60-rplcNM using primers hyg-r and hyg-f (Table 1). The MICs of recombinant and wild-type bacteria against LZD and PNU were determined by the classical agar plate method (17). We observed no changes in the MICs of LZD and PNU against the two recombinant strains containing integrative pLZD-N and pLZD-NM, comparing to their parental strains (Table 3). However, 4- and 2-fold increments in LZD and PNU MICs, respectively, were observed in M. tuberculosis H37Ra and M. tuberculosis H37Rv containing p60-rplcNM, but no MIC changes were observed in the strain containing p60-rplCN.
FIG 1.

Diagrammatic illustration of the position of rplC gene (A) and its predicted promoter and the position of Ts red in pLZD-luc (B).
TABLE 1.
DNA primers and fragments used in this study
| Primer | Nucleotide sequence (5′–3′) |
|---|---|
| Kan-f | ATGAGCCATATTCAACGGGA |
| Kan-r | TTAGAAAAACTCATCGAGCA |
| rplCf | GTGAATTCCTGACGGACGAGACCA |
| rplCr | CTTCTAGACGCAGCCATCACTTCT |
| tsrF | GGTGGTACCATGGAAGACGCCAAAAAC |
| tsrR | GCTCTAGATTACAATTTGGACTTTCC |
| rplC-F | GGGAATTCCATATGGCACGAAAGGGCATTC |
| rplC-R | CCCAAGCTT TCACTTCTCACCTCGTTTG |
| hyg-f | GTGACACAAGAATCCCTG |
| hyg-r | TCAGGCGCCGGGGGCGGTG |
FIG 2.
Integrative plasmid pMH94A and pLZD-N. oriE, origin region in E. coli; KANr, kanamycin-resistant gene from Tn9O3; bla, ampicillin-resistant gene; rplC, gene from M. tuberculosis H37Rv.
TABLE 2.
Bacterial strains and plasmids used in this study
| Strain/plasmid | Relevant characteristic(s) | Source or reference |
|---|---|---|
| pMH94 | pUC119 carrying KANr from Tn9O3 and attp-int cassette from L5 mycobacteriophage at SalI-SalI | 17 |
| pMH94A | pMH94 containing apramycin-resistant gene (Apr) gene at KpnI sites | This study |
| pLZD-N | pMH94A containing M. tuberculosis natural promoter-rpsJ-rplC gene at EcoRI-XbaI sites | This study |
| pLZD-NM | Mutated rplC CYS154ARG gene in pLZD-N | This study |
| pN60-RIK | Plasmid containing the Ts red | Unpublished |
| pLZD-luc | pLZD-N and pLZD-NM plasmids containing the Ts red firefly luciferase gene | This study |
| p60luxN | Containing the strong promoter Hsp60, origins of replication for E. coli and mycobacteria and hygromycin-resistant gene (hyg) | 15 |
| p60-rplcN | p60luxN inserted the rplC wild-type gene at NdeI-HindIII sites | This study |
| p60-rplcNM | p60luxN containing the mutated rplC CYS154ARG gene at NdeI-HindIII sites. | This study |
| E. coli DH5α | General-purpose cloning strain; F− [ϕ80d lacZΔM15] ΔD(lacZYA-argF)U169 deoR recA1 endA1 hsdR17 glnV44 thi-1 gyrA96 relA | 17 |
| M. tuberculosis H37Rv | A widely used virulent laboratory M. tuberculosis strain, ATCC 27294 | 16 |
| M. tuberculosis H37Ra | A widely used avirulent laboratory M. tuberculosis strain | This study |
| M. tuberculosis H37Rv::pLZD-N | M. tuberculosis H37Rv containing pLZD-N | This study |
| M. tuberculosis H37Rv::pLZD-NM | M. tuberculosis H37Rv containing pLZD-NM | This study |
| M. tuberculosis H37Ra::pLZD-N | M. tuberculosis H37Ra containing pLZD-N | This study |
| M. tuberculosis H37Ra::pLZD-NM | M. tuberculosis H37Ra containing pLZD-NM | This study |
| M. tuberculosis H37Rv::p60-rplCN | M. tuberculosis H37Rv containing p60-rplCN | This study |
| M. tuberculosis H37Rv::p60-rplCNM | M. tuberculosis H37Rv containing p60-rplCNM | This study |
| M. tuberculosis H37Ra::p60-rplCN | M. tuberculosis H37Ra containing p60-rplCN | This study |
| M. tuberculosis H37Ra::p60-rplCNM | M. tuberculosis H37Ra containing p60-rplCNM | This study |
| M. tuberculosis H37Ra::pN60-RIK | M. tuberculosis H37Ra containing pN60-RIK | This study |
| M. tuberculosis H37Ra::pLZD-luc | M. tuberculosis H37Ra containing pLZD-luc | This study |
FIG 3.
Plasmids p60luxN and p60-rplcN. oriE, origin region in E. coli; oriM, origin region in mycobacteria; hyg, hygromycin-resistant gene; rplC and rplC (CYS154ARG), genes from pLZD-N and PLZD-NM plasmids, respectively.
TABLE 3.
MICs of LZD and PNU for wild-type and recombinant M. tuberculosis strains
| M. tuberculosis strain | MIC (μg/ml) |
|
|---|---|---|
| LZD | PNU | |
| H37Rv | 1.0 | 0.25 |
| H37Rv::pLZD-N | 1.0 | 0.25 |
| H37Rv::pLZD-NM | 1.0 | 0.25 |
| H37Rv::p60-rplCN | 1.0 | 0.25 |
| H37Rv::p60-rplCNM | 4.0 | 0.5 |
| H37Ra | 1.0 | 0.25 |
| H37Ra::pLZD-N | 1.0 | 0.25 |
| H37Ra::pLZD-NM | 1.0 | 0.25 |
| H37Ra::p60-rplCN | 1.0 | 0.25 |
| H37Ra::p60-rplCNM | 4.0 | 0.5 |
We investigated whether the rplC gene expression level influenced oxazolidinone resistance. A reporter thermostable red firefly luciferase gene (Ts red) (18, 19) was introduced into pLZD-N by exploiting the KpnI and XbaI restriction sites inside the rplC gene (primers tsrF and tsrR; Table 1) to obtain plasmid pLZD-luc. The Ts red was fused with 9 amino acids of RplC at its N terminal (Fig. 1B). In the presence of the d-Luciferin (BBI Life Sciences), the E. coli strains containing pN60-RIK and pLZD-Luc (Table 2) produced strong light, which meant the fused luciferase was functional (Table 4). The 2 plasmids were transformed into M. tuberculosis H37Ra as previously described (16), and the KAN-resistant colonies were selected after confirmation of the resistant marker genes by PCR. The luciferase activities of the recombinant bacteria were measured using d-Luciferin bioluminescent assays (Table 4). M. tuberculosis H37Ra::pN60-RIK produced at least a 25-fold stronger light than M. tuberculosis H37Ra::pLZD-luc (Table 4). The light produced by M. tuberculosis H37Ra::pLZD-luc was weak, only about 2-fold greater than the background reading (Table 4). Our data suggest that the rplC-rplC (Cys154Arg) integrated into M. tuberculosis can be expressed but at a low level. Given that the mutations of 50S ribosomal protein L3 (rplC encoded) may alter the structure of the adjacent LZD binding site in the peptidyl transferase center (14), an excessive amount of the mutated L3 protein will be required to titrate out the drug-binding sites. It has also been reported that integration of a single-copy target gene (with mutation) in mycobacteria failed to induce resistance that was otherwise conferred with the multicopy plasmid (20). Therefore, the low level of expression may explain why integration of the rplC (Cys154Arg) gene in M. tuberculosis H37Ra::pLZD-NM failed to induce resistance to LZD and PNU, as the number of gene copies and/or the level of gene expression are important determinants of the resistance phenotype.
TABLE 4.
Detection of the firefly luciferase activity
| Detection | E. coli containing pN60-RIK | E. coli containing pLZD-luc | M. tuberculosis H37Ra containing pN60-RIK | Control: M. tuberculosis H37Ra containing pLZD-luc without luciferin | M. tuberculosis H37Ra containing pLZD-luc with luciferin |
|---|---|---|---|---|---|
| RLUa | >1,700,000 | >1,000,000 | >5,000 | 52.50 ± 7.41 | 145.3 ± 30.42b |
Mean relative light unit ± standard error of mean from 4 independent measurements.
P = 0.025 < 0.05 compared with luciferin-free control.
Zhang et al. (21) recently found 3 LZD-resistant M. tuberculosis strains with the TGC460CGC mutation and one strain with the CAC463GAC mutation, indicating Cys154Arg and His155Asp amino acid substitutions, respectively. However, we found that the sequence of 457- to 468-bp of rplC gene was GGATGTGCCACG (460T was underlined and 462T and 465C were boxed) and the TGC460CGC and CAC463GAC mutations in the rplC gene in their report (21) may be TGT(Cys)462TGC(Cys) and GCC(Ala)465GCA(Ala). If so, they do not result in any amino acid substitution. Until now, rplC (Cys154Arg) has been shown to cause resistance to all the congeners of the oxazolidinone class, and the mutated sequence is the only one found in this gene (22).
In conclusion, we have verified by molecular genetics that the mutation Cys154Arg in rplC can cause resistance to LZD and PNU oxazolidinone. Our findings, therefore, concur with Beckert et al. (12) that the Cys154Arg mutation in the rplC gene possibly plays a major role in LZD resistance in M. tuberculosis in clinical isolates. As shown elsewhere, the equivalent mutation N149R in E. coli L3 protein also increased the MIC from 8 to 32 μg/ml (14). We hence propose further work to establish a novel, rapid, and high-throughput drug-screening model for undertaking such oxazolidinone resistance using the autoluminescent M. tuberculosis (16, 23) overexpressing rplC (Cys154Arg). Our data support that the Cys154Arg mutation in rplC may be considered one of the markers for oxazolidinone resistance in clinical M. tuberculosis isolates.
ACKNOWLEDGMENTS
Pfizer is gratefully acknowledged for providing LZD and PNU powder for the susceptibility testing.
We declare no conflicts of interest.
Funding Statement
This work was supported by the One Hundred Talents Program of the Chinese Academy of Sciences (category A, to T.Z.), by the Key Program of the Chinese Academy of Sciences (KJZD-EW-L02), by the National Natural Science Foundation of China (81572037), by the Key Project Grant (2015SKLRD-K01) and the Open Project Grant (2014SKLRD-O06) from the State Key Lab of Respiratory Disease, Guangzhou Institute of Respiratory Disease, First Affiliated Hospital of Guangzhou Medical University, by the Chinese Academy of Sciences-Commonwealth Scientific and Industrial Research Organization Joint Grant (154144KYSB20150045), and partially by the Guangzhou Municipal Industry and Research Collaborative Innovation Program (201508020248) and Guangzhou Municipal Clinical Medical Center Program (155700012).
REFERENCES
- 1.World Health Organization. 2014. Global tuberculosis report. World Health Organization, Geneva, Switzerland: http://www.who.int/tb/publications/global_report/en/. [Google Scholar]
- 2.Migliori GB, Eker B, Richardson MD, Sotgiu G, Zellweger JP, Skrahina A, Ortmann J, Girardi E, Hoffmann H, Besozzi G, Bevilacqua N, Kirsten D, Centis R, Lange C. 2009. A retrospective TBNET assessment of linezolid safety, tolerability and efficacy in multidrug-resistant tuberculosis. Eur Respir J 34:387–393. doi: 10.1183/09031936.00009509. [DOI] [PubMed] [Google Scholar]
- 3.Udwadia ZF, Sen T, Moharil G. 2010. Assessment of linezolid efficacy and safety in MDR- and XDR-TB: an Indian perspective. Eur Respir J 35:936–938. doi: 10.1183/09031936.00132009. [DOI] [PubMed] [Google Scholar]
- 4.Lee M, Lee J, Carroll MW, Choi H, Min S, Song T, Via LE, Goldfeder LC, Kang E, Jin B, Park H, Kwak H, Kim H, Jeon HS, Jeong I, Joh JS, Chen RY, Olivier KN, Shaw PA, Follmann D, Song SD, Lee JK, Lee D, Kim CT, Dartois V, Park SK, Cho SN, Barry CE III. 2012. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N Engl J Med 367:1508–1518. doi: 10.1056/NEJMoa1201964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang KC, Yew WW, Tam CM, Leung CC. 2013. WHO group 5 drugs and difficult multidrug-resistant tuberculosis: a systematic review with cohort analysis and meta-analysis. Antimicrob Agents Chemother 57:4097–4104. doi: 10.1128/AAC.00120-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams KN, Stover CK, Zhu T, Tasneen R, Tyagi S, Grosset JH, Nuermberger EL. 2009. Promising antituberculosis activity of the oxazolidinone PNU-100480 relative to that of linezolid in a murine model. Antimicrob Agents Chemother 53:1314–1319. doi: 10.1128/AAC.01182-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallis RS, Jakubiec WM, Kumar V, Silvia AM, Paige D, Dimitrova D, Li X, Ladutko L, Campbell S, Friedland G, Mitton-Fry M, Miller PF. 2010. Pharmacokinetics and whole-blood bactericidal activity against Mycobacterium tuberculosis of single doses of PNU-100480 in healthy volunteers. J Infect Dis 202:745–751. doi: 10.1086/655471. [DOI] [PubMed] [Google Scholar]
- 8.Wallis RS, Dawson R, Friedrich SO, Venter A, Paige D, Zhu T, Silvia A, Gobey J, Ellery C, Zhang Y, Eisenach K, Miller P, Diacon AH. 2014. Mycobactericidal activity of sutezolid (PNU-100480) in sputum (EBA) and blood (WBA) of patients with pulmonary tuberculosis. PLoS One 9:e94462. doi: 10.1371/journal.pone.0094462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richter E, Rüsch-Gerdes S, Hillemann D. 2007. First linezolid-resistant clinical isolates of Mycobacterium tuberculosis. Antimicrob Agents Chemother 51:1534–1536. doi: 10.1128/AAC.01113-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodríguez JC, Cebrián L, López M, Ruiz M, Jiménez I, Royo G. 2004. Mutant prevention concentration: comparison of fluoroquinolones and linezolid with Mycobacterium tuberculosis. J Antimicrob Chemother 53:441–444. doi: 10.1093/jac/dkh119. [DOI] [PubMed] [Google Scholar]
- 11.Ahmed I, Jabeen K, Inayat R, Hasan R. 2013. Susceptibility testing of extensively drug-resistant and pre-extensively drug-resistant Mycobacterium tuberculosis against levofloxacin, linezolid, and amoxicillin-clavulanate. Antimicrob Agents Chemother 57:2522–2525. doi: 10.1128/AAC.02020-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beckert P, Hillemann D, Kohl TA, Kalinowski J, Richter E, Niemann S, Feuerriegel S. 2012. rplC T460C identified as a dominant mutation in linezolid-resistant Mycobacterium tuberculosis strains. Antimicrob Agents Chemother 56:2743–2745. doi: 10.1128/AAC.06227-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yates JL, Nomura M. 1980. Escherichia coli ribosomal protein L4 is a feedback regulatory protein. Cell 21:517–522. doi: 10.1016/0092-8674(80)90489-4. [DOI] [PubMed] [Google Scholar]
- 14.Klitgaard RN, Ntokou E, Nørgaard K, Biltoft D, Hansen LH, Trædholm NM, Kongsted J, Vester B. 2015. Mutations in the bacterial ribosomal protein L3 and their association with antibiotic resistance. Antimicrob Agents Chemother 59:3518–3528. doi: 10.1128/AAC.00179-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu T, Wang B, Guo J, Zhou Y, Julius M, Njire M, Cao Y, Wu T, Liu Z, Wang C, Xu Y, Zhang T. 2015. Role of folP1 and folP2 genes in the action of sulfamethoxazole and trimethoprim against mycobacteria. J Microbiol Biotechnol 25:1559–1567. doi: 10.4014/jmb.1503.03053. [DOI] [PubMed] [Google Scholar]
- 16.Zhang T, Li SY, Nuermberger EL. 2012. Autoluminescent Mycobacterium tuberculosis for rapid, real-time, non-invasive assessment of drug and vaccine efficacy. PLoS One 7:e29774. doi: 10.1371/journal.pone.0029774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang T, Bishai WR, Grosset JH, Nuermberger EL. 2010. Rapid assessment of antibacterial activity against Mycobacterium ulcerans by using recombinant luminescent strains. Antimicrob Agents Chemother 54:2806–2813. doi: 10.1128/AAC.00400-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fujii H, Noda K, Asami Y, Kuroda A, Sakata M, Tokida A. 2007. Increase in bioluminescence intensity of firefly luciferase using genetic modification. Anal Biochem 366:131–136. doi: 10.1016/j.ab.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 19.Branchini BR, Ablamsky DM, Murtiashaw MH, Uzasci L, Fraga H, Southworth TL. 2007. Thermostable red and green light-producing firefly luciferase mutants for bioluminescent reporter applications. Anal Biochem 361:253–262. doi: 10.1016/j.ab.2006.10.043. [DOI] [PubMed] [Google Scholar]
- 20.Zimhony O, Cox JS, Welch JT, Vilchèze C, Jacobs WR Jr. 2000. Pyrazinamide inhibits the eukaryotic-like fatty acid synthetase I (FASI) of Mycobacterium tuberculosis. Nat Med 6:1043–1047. doi: 10.1038/79558. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Z, Pang Y, Wang Y, Liu C, Zhao Y. 2014. Beijing genotype of Mycobacterium tuberculosis is significantly associated with linezolid resistance in multidrug-resistant and extensively drug-resistant tuberculosis in China. Int J Antimicrob Agents 43:231–235. doi: 10.1016/j.ijantimicag.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Balasubramanian V, Solapure S, Iyer H, Ghosh A, Sharma S, Kaur P, Deepthi R, Subbulakshmi V, Ramya V, Ramachandran V, Balganesh M, Wright L, Melnick D, Butler SL, Sambandamurthy VK. 2014. Bactericidal activity and mechanism of action of AZD5847, a novel oxazolidinone for treatment of tuberculosis. Antimicrob Agents Chemother 58:495–502. doi: 10.1128/AAC.01903-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang F, Njire MM, Liu J, Wu T, Wang B, Liu T, Cao Y, Liu Z, Wan J, Tu Z, Tan Y, Tan S, Zhang T. 2015. Engineering more stable, selectable marker-free autoluminescent mycobacteria by one step. PLoS One 10:e0119341. doi: 10.1371/journal.pone.0119341. [DOI] [PMC free article] [PubMed] [Google Scholar]