Abstract
Introduction Preservation of the temporal branches of the facial nerve during anterolateral craniotomies is important. Damaging it can inflict undesirable cosmetic defects to the patient. The supraorbital trans-eyebrow approach (SOTE) is a versatile keyhole craniotomy but still has a high rate of frontalis muscle (FM) palsy.
Objective Anatomical study to implement the interfascial dissection during the SOTE to preserve the nerves to the FM.
Methods Slight modification of the standard technique of the SOTE was performed in 6 cadaveric specimens (12 sides).
Results Distal rami to the FM were exposed. The standard “u—shape” incision of the FM can cross over the nerves. Alternatively, an “l-shape” incision was performed until the superior temporal line (STL). An interfascial dissection was performed near to the STL and the interfascial fat pad was used as a protective layer for the nerves.
Conclusion Various pathologies can be addressed with the SOTE. In the majority of the cases the cosmetic results are good, but FM palsy remains a drawback of this approach. The interfascial dissection may be used in an attempt to prevent frontalis rami palsy.
Keywords: supraorbital trans-eyebrow approach, interfascial dissection, frontalis muscle palsy, nerve protection
Introduction
Concerns in preserving the temporal branches (TB) of the facial nerve during anterolateral craniotomies should be in mind since the soft tissue dissection can pose risks to the nerve. Damage to these nerves can inflict undesirable cosmetic defects to the patient due to weakness of the frontalis, oculi, orbicularis, and corrugator supercilii muscles.1 2 3
To prevent TB injuries, Yasargil et al proposed the interfascial dissection,4 which reduced frontalis muscles (FM) palsy incidence.2 5
The TB when above the zygomatic arc commonly gives three main rami: the auricularis (posterior), frontalis (middle), and orbicularis (anterior)3 4 6 of which the latter two have clinical importance because it innervates the frontalis and orbicularis muscles, respectively. This article will address more attention to the frontalis rami (FR) that innervates the FM. Those rami runs in the loosen areolar tissue below the galea,2 7 8 thus a subgaleal dissection plan can put the nerves in jeopardy. Anastomosis between the TB can be encountered in up to 75% of the cases,7 9 10 11 and this is a very important feature that will be discussed further in this article.
In the past two decades the neurosurgical approaches have turned into a tendency of minimally invasiveness. Smaller skin incision and keyhole craniotomies have been used to address different pathologies including vascular and skull base lesion12 13 14 15 16 17 that once was only approached using the conventional routes. The supraorbital trans-eyebrow approach (SOTE) offers this advantage in selected cases, but an expressive number of patients experience transitory or even permanent FM palsy, although this is mentioned only in a few reports14 18 19 and even less specifies how to try to prevent FR injury.19
This study has the objective to propose a modification of the surgical technique during the soft tissue dissection to protect the FR when performing a SOTE to decrease FM palsy during this approach.
Material and Methods
Six cadaveric formalin-fixed heads with intravascular colored silicone (Science Care, Phoenix, Arizona, United States) obtained from the Neuroanatomy Laboratory of the University of Pittsburgh Medical Center was used. In all, 12 sides a SOTE approach was performed following the same steps. The mean distance from the lateral cantus of the eye to the last FR crossing the superior temporal line (STL) was measured.
Results
Technique Description
A 5 cm skin incision was performed in the superior edge of the eyebrow. The skin incision was slight bigger than in a live patient, because the tissue loses its elasticity after being fixed in formalin (Fig. 1A). The dissections were performed using a surgical microscope to perform the dissection of the supraorbital branches in the medial portion of the incision and the terminal branches of the FR running in the loose areolar tissue of the subgaleal space (Fig. 1D) until it reaches the frontalis muscle in the lateral portion of the approach (Fig. 1B, C). Instead of doing a u-shape cut of the frontalis and temporal muscles doing a single flap as suggested in the majority of the descriptions (white and red symbols in Fig. 1B),12 14 15 19 20 21 initially an l-shape cut was performed (white arrows in Fig. 1B), to avoid cutting over the FR exposed (Fig. 1E) and at the same time preserving the main trunk of the supraorbital nerve and the majority of its branches. The horizontal cut was performed immediately posterior to the last FR dissected in a mean distance of 31.3 mm (range, 27–35 mm, standard deviation, 2.7mm) superior and posterior to the lateral cantus of the eye (green arrow in Fig. 1B). The horizontal cut was done from medial to lateral through the STL, disconnecting the superficial from the deep layers of the temporal fascia (Fig. 1E), since both layers join together in this region7 with the interfascial fat pad in between them Fig. 2A. The myofascial flap was detached from the bone together with the periosteum in the medial portion of the STL and separated from the deep layer of the temporal fascial in the lateral portion of the STL (Fig. 2A, B). Notice that the superficial layer of the temporal fascial lateral to the STL is continuous with the “pericranium flap” (frontalis muscle), medial to the STL (Fig. 2A, B). In all cases, the interfascial fat pad could be observed, although the difference in the thickness happens. When the retraction of the flap was maximum but not yet enough to expose the keyhole (blue arrow in Fig. 2B), a straight cut pointing toward the zygomatic arc, slight under the skin, but running away from the direction of the most posterior FR was performed (Fig. 2C) to mobilize further anterior the flap and better expose the keyhole (Fig. 2D, E).
Fig. 1.
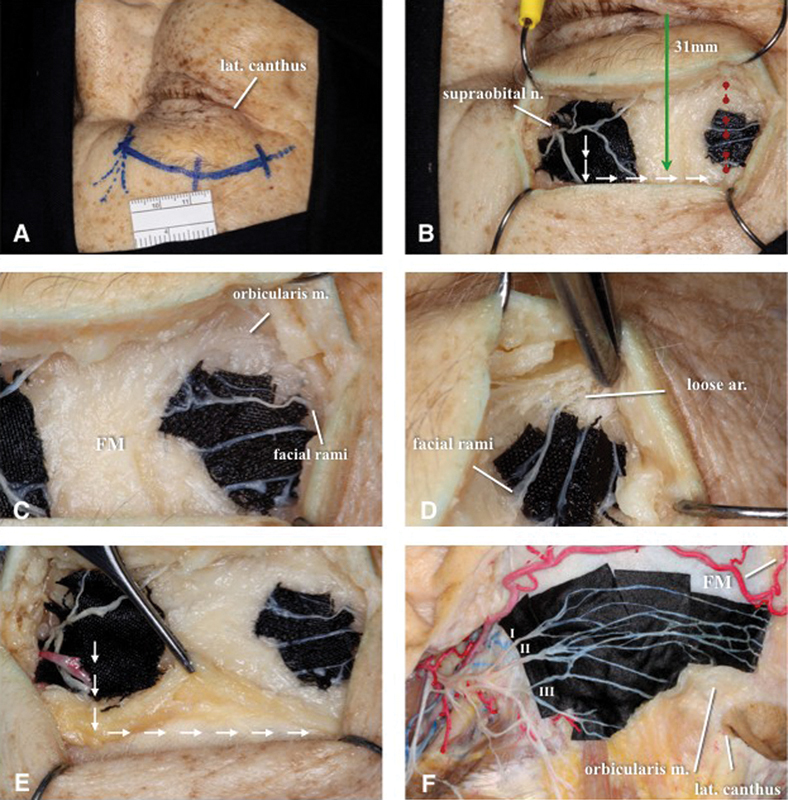
Supraorbital nerve branches and FR of temporal branches of the facial never exposure. (A) A 5 cm skin incision lateral to the supraorbital notch. (B) Supraorbital nerve and FR exposure. Note that the myofascial flap will begin with an “l-shape” cut with the horizontal cut starting in a mean distance of 31.3 mm superior and posterior the lateral cantus of the eye (green arrow). If the cut is performed through the STL (red dots) the FR may be injured. (C) Distal nerve terminations of FR with the FM. Fibers from the orbitalis muscles can be seen with different direction when compared with the FM. (D) Loose areolar tissue in the subgaleal space, where the FR runs. (E) “l-shape” myofascial flap being detached from the bone. The cut is carried on from medial to lateral passing through the STL and reaching the superficial layer of the temporal fascia. (F) Facial nerve exposure (different specimen), demonstrating nervous supply of the orbicularis and occipito-frontalis muscles by auricularis/posterior (I), frontalis/medial (II) and orbicularis/anterior (III) facial branches. Note the extent of connections between the respective branches. FM, frontalis muscle; FR, frontalis rami; STL, superior temporal line.
Fig. 2.
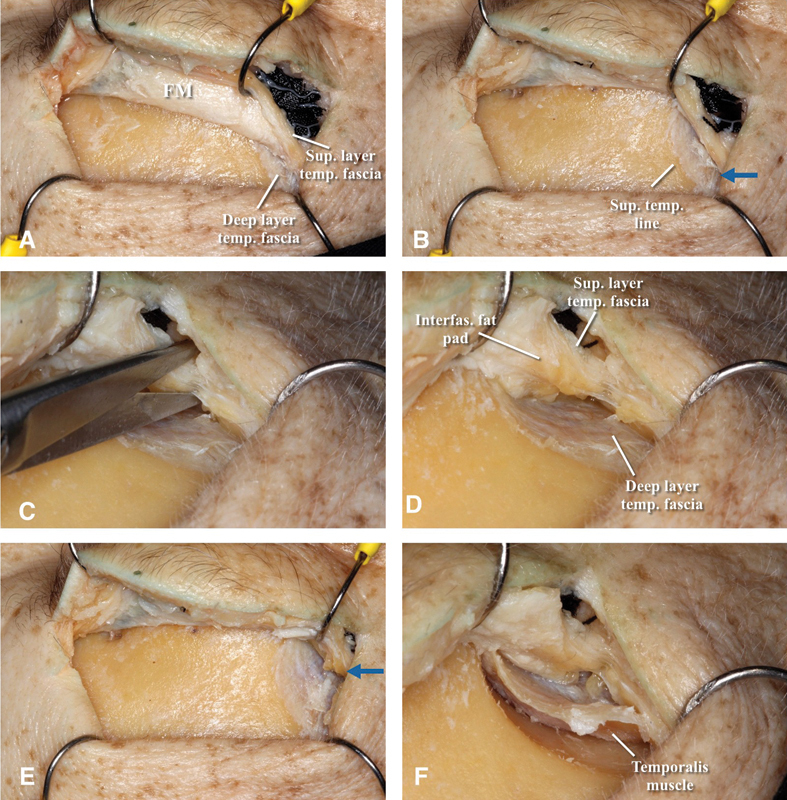
Interfascial dissection steps from medial to lateral. (A) Myofascial flap reflected anteriorly along with the STF, exposing the deep layer of the temporal fascia. (B) Maximum retraction of the myofascial flap. Blue arrow showing the point where the cut of the STF along with the interfascial fat pad should be done to keep mobilizing the STF and fat pad anteriorly. (C) Cutting the STF along with the interfascial fat pad. (D) View showing layers lateral to the STL, specially the interfascial fat pad that will protect the FR. (E) Flap retraction after interfascial dissection. Note that further anterior retraction is achieved. (F) Temporal muscle detached from the STL exposing the keyhole region. STF, superficial layer of the temporal fascia; STL, superior temporal line.
The interfascial fat pad could now be better visualized and was used to protect the FR when placing the retractor.
This is a modification of the most usual description that makes the cut along the STL directing it toward the zygomatic process of the frontal bone.15 18 19 22 By doing so enough space is created to detach the temporal muscle from the keyhole region (Figs. 2F and 3A) and a MacCarty keyhole can be drilled. From now on a small one-piece frontoorbital craniotomy (Fig. 4A) following the standard steps was performed (Fig. 3C–F). The size and type of bone removal may vary with the pathology in question. The dura was opened with a u-shape incision (Fig. 4B). A rigid 4 mm zero-degree view endoscope was used to dissect the supra- and infrachiasmatic cisterns, sellar and suprasellar region, including the vascular supply (Fig. 4C).
Fig. 3.
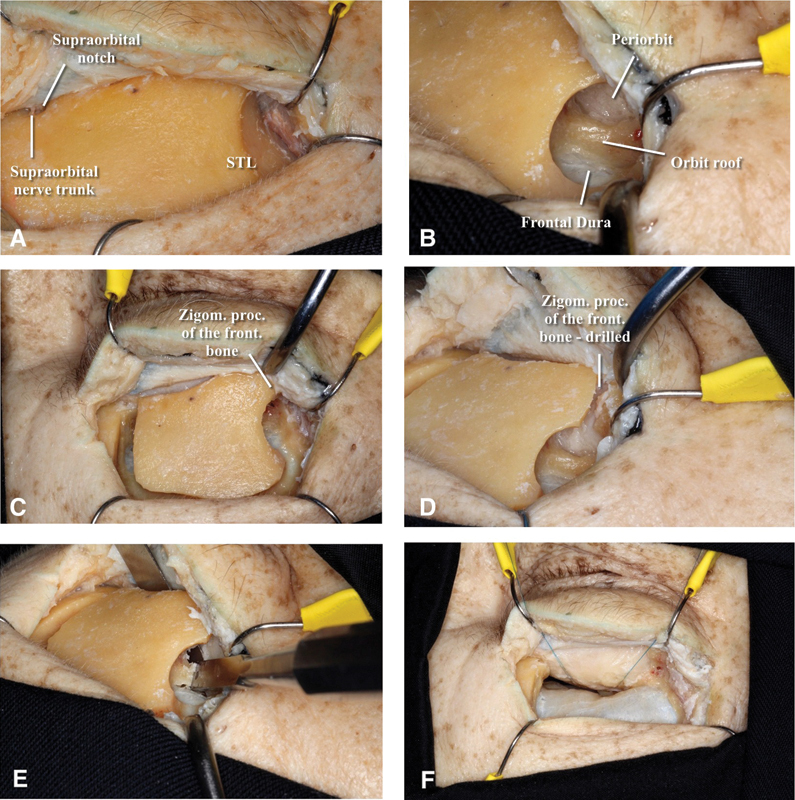
(A–E) Stepwise frontoorbital craniotomy. (A) Keyhole region exposed lateral to the STL and under the detached temporal muscle. (B) MacCarty keyhole exposing the periorbit and the frontal dura separated by the orbital roof. (C) Osteotomies from the MacCarty keyhole following a u-shape line until the orbital rim lateral to the supraorbital notch. (D) Zygomatic process of the frontal bone drilled. (E) Chisel being used to cut though the orbital roof—note the protection of the periorbit with a spatula. (F) Sutures being used to retract the periorbit to gain more inferior space. STL, superior temporal line.
Fig. 4.
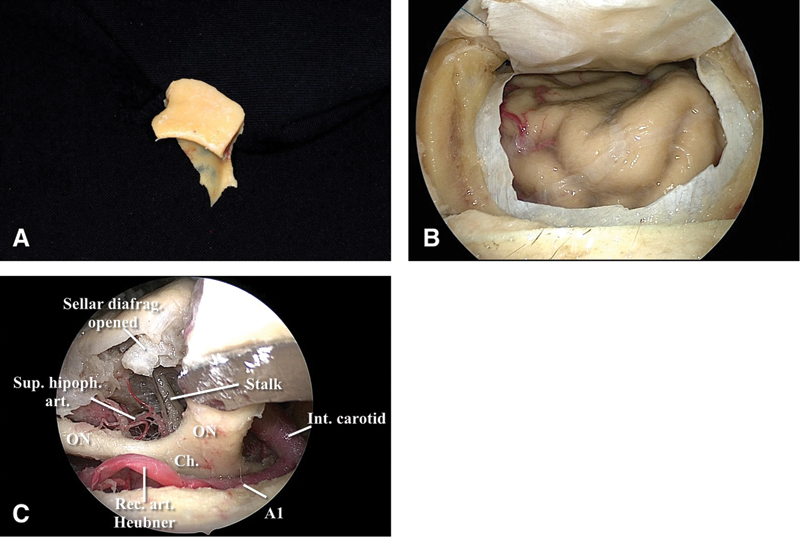
(A) Frontoorbital bone flap in one piece. (B) Dural opening. (C) Dissection of the suprachiasmatic cistern showing the right A1 segment of the anterior cerebral artery and the right recurrent artery of Heubner. The superior portion of the carotid cistern can be opened exposing the internal carotid bifurcation. ON and optic chiasm can be gently mobilized in other to further exposure. Dissecting the infrachiasmatic cistern, the superior hypophyseal artery and it branches comes in to view and care must be taken to avoid injury. Opening the seller diaphragm, the connection between the stalk and the pituitary gland can be seen. ON, optic nerves.
Discussion
There is not a consensus on the terminology to be adopted when naming the branches of the facial nerve above the zygomatic arch and the temporal fascial layers. Although some authors proposed unification of the nomenclature by doing excellent reviews about it,1 8 9 this issue still remains controversial. Thus, we have used in this article the same terminology used by Poblete et al7 because it is more common in the neurosurgical literature and surgical practice.
The SOTE is a tailored minimally invasive skull base approach that can safely address various pathologies including tumors (meningiomas, craniopharingiomas) and vascular abnormalities.14 21
The cosmetic results of this approach are very favorable in the majority of the cases, but the risk of frontalis muscle palsy due to an injury of the FR remains a serious drawback to a supraorbital keyhole approach as a minimally invasive surgical technique.
The literature provides many reports, surgical technique and anatomical dissections of the SOTE approach, including different osteotomies and emphasizing the importance of avoiding supraorbital nerve injury,14 15 16 18 19 23 24 but quite a few mentioned that the FR can be at risk during the soft tissue exposure12 13 22 and almost no one explored a solution to protect the FR. Reisch et al14 reported that the FR did not cross the surgical field, but in the same article showed that 5.5% of the cases that underwent SOTE experienced FM palsy. Later the same author reported another series of SOTE with 5.6% of nerve palsy, being 3.5% temporary and 2.1% permanent palsies. Park et al 19 did a preoperative percutaneous mapping of the trajectory of the FR which can be very useful in attempting to preserve the nerve, but did not implement a surgical modification to try to avoid nerve lesion, using the same c-shape flap described elsewhere. Perhaps that was why that study reported 22% of FM transitory palsy.
The transitory palsy can be a result of an anatomical “protection,” since anastomosis above the zygomatic arc between the anterior, middle, and posterior rami of the TB can be encountered in up to 75% of the cases.7 9 10 11 This anatomical feature could be the explanation that neurotmesis, and not neuropraxia, of one or more TB may result in spontaneous functional recovery following initial facial nerve injury. This theory has already been explored elsewhere in the setting of conventional anterolateral craniotomies.9 25
Conclusion
SOTE is a useful approach when dealing with anterior skull base pathologies. Although the majority of the cases have a good aesthetic result, there is still a high rate of frontalis muscle palsy, permanent or transitory. This can be due to FR retraction or even injury when the soft tissue dissection is performed through the STL. To minimize this, percutaneous nerve mapping19 and a slight modification of the surgical technique which implements the interfascial dissection can lead to lower FM palsy rates. This technique is feasible and further studies in living patients should be performed.
References
- 1.Babakurban S T, Cakmak O, Kendir S, Elhan A, Quatela V C. Temporal branch of the facial nerve and its relationship to fascial layers. Arch Facial Plast Surg. 2010;12(1):16–23. doi: 10.1001/archfacial.2009.96. [DOI] [PubMed] [Google Scholar]
- 2.Ammirati M Spallone A Ma J Cheatham M Becker D An anatomicosurgical study of the temporal branch of the facial nerve Neurosurgery 19933361038–1043., discussion 1044 [DOI] [PubMed] [Google Scholar]
- 3.Coscarella E, Vishteh A G, Spetzler R F, Seoane E, Zabramski J M. Subfascial and submuscular methods of temporal muscle dissection and their relationship to the frontal branch of the facial nerve. Technical note. J Neurosurg. 2000;92(5):877–880. doi: 10.3171/jns.2000.92.5.0877. [DOI] [PubMed] [Google Scholar]
- 4.Yaşargil M G, Reichman M V, Kubik S. Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg. 1987;67(3):463–466. doi: 10.3171/jns.1987.67.3.0463. [DOI] [PubMed] [Google Scholar]
- 5.Ammirati M, Spallone A, Ma J, Cheatham M, Becker D. Preservation of the temporal branch of the facial nerve in pterional-transzygomatic craniotomy. Acta Neurochir (Wien) 1994;128(1–4):163–165. doi: 10.1007/BF01400667. [DOI] [PubMed] [Google Scholar]
- 6.Spiriev T, Poulsgaard L, Fugleholm K. Techniques for Preservation of the Frontotemporal Branch of Facial Nerve during Orbitozygomatic Approaches. J Neurol Surg B Skull Base. 2015;76(3):189–194. doi: 10.1055/s-0034-1396599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poblete T, Jiang X, Komune N, Matsushima K, Rhoton A L Jr. Preservation of the nerves to the frontalis muscle during pterional craniotomy. J Neurosurg. 2015;122(6):1274–1282. doi: 10.3171/2014.10.JNS142061. [DOI] [PubMed] [Google Scholar]
- 8.Davidge K M van Furth W R Agur A Cusimano M Naming the soft tissue layers of the temporoparietal region: unifying anatomic terminology across surgical disciplines Neurosurgery 201067(3, Suppl Operative):ons120–ons129., discussion ons129–ons130 [DOI] [PubMed] [Google Scholar]
- 9.Krayenbühl N Isolan G R Hafez A Yaşargil M G The relationship of the fronto-temporal branches of the facial nerve to the fascias of the temporal region: a literature review applied to practical anatomical dissection Neurosurg Rev 20073018–15., discussion 15 [DOI] [PubMed] [Google Scholar]
- 10.Bernstein L, Nelson R H. Surgical anatomy of the extraparotid distribution of the facial nerve. Arch Otolaryngol. 1984;110(3):177–183. doi: 10.1001/archotol.1984.00800290041009. [DOI] [PubMed] [Google Scholar]
- 11.Ishikawa Y. An anatomical study on the distribution of the temporal branch of the facial nerve. J Craniomaxillofac Surg. 1990;18(7):287–292. doi: 10.1016/s1010-5182(05)80533-5. [DOI] [PubMed] [Google Scholar]
- 12.Fernandes Y B Maitrot D Kehrli P Tella O I Jr Ramina R Borges G Supraorbital eyebrow approach to skull base lesions Arq Neuropsiquiatr 200260(2-A):246–250. [DOI] [PubMed] [Google Scholar]
- 13.Fernandes Y B, Maitrot D, Kehrli P. Supraorbital minicraniotomy. Skull Base Surg. 1997;7(2):65–68. doi: 10.1055/s-2008-1058610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reisch R Perneczky A Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision Neurosurgery 200557(4, Suppl):242–255., discussion 242–255 [DOI] [PubMed] [Google Scholar]
- 15.Reisch R, Marcus H J, Kockro R A, Ulrich N H. The supraorbital keyhole approach: how I do it. Acta Neurochir (Wien) 2015;157(6):979–983. doi: 10.1007/s00701-015-2424-6. [DOI] [PubMed] [Google Scholar]
- 16.Adawi M M, Abdelbaky A M. Validity of the lateral supraorbital approach as a minimally invasive corridor for orbital lesions. World Neurosurg. 2015;84(3):766–771. doi: 10.1016/j.wneu.2015.04.058. [DOI] [PubMed] [Google Scholar]
- 17.Igressa A, Pechlivanis I, Weber F. et al. Endoscope-assisted keyhole surgery via an eyebrow incision for removal of large meningiomas of the anterior and middle cranial fossa. Clin Neurol Neurosurg. 2015;129:27–33. doi: 10.1016/j.clineuro.2014.11.024. [DOI] [PubMed] [Google Scholar]
- 18.Reisch R, Marcus H J, Hugelshofer M, Koechlin N O, Stadie A, Kockro R A. Patients' cosmetic satisfaction, pain, and functional outcomes after supraorbital craniotomy through an eyebrow incision. J Neurosurg. 2014;121(3):730–734. doi: 10.3171/2014.4.JNS13787. [DOI] [PubMed] [Google Scholar]
- 19.Park J, Jung T-D, Kang D-H, Lee S-H. Preoperative percutaneous mapping of the frontal branch of the facial nerve to assess the risk of frontalis muscle palsy after a supraorbital keyhole approach. J Neurosurg. 2013;118(5):1114–1119. doi: 10.3171/2013.1.JNS121525. [DOI] [PubMed] [Google Scholar]
- 20.Reisch R Fischer G Stadie A Kockro R Cesnulis E Hopf N The supraorbital endoscopic approach for aneurysms World Neurosurg 201482(6, Suppl):S130–S137. [DOI] [PubMed] [Google Scholar]
- 21.Ormond D R, Hadjipanayis C G. The Supraorbital Keyhole Craniotomy through an Eyebrow Incision: Its Origins and Evolution. Minim Invasive Surg. 2013;2013:296469. doi: 10.1155/2013/296469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dare A O, Landi M K, Lopes D K, Grand W. Eyebrow incision for combined orbital osteotomy and supraorbital minicraniotomy: application to aneurysms of the anterior circulation. Technical note. J Neurosurg. 2001;95(4):714–718. doi: 10.3171/jns.2001.95.4.0714. [DOI] [PubMed] [Google Scholar]
- 23.Tatarli N, Ceylan D, Şeker A, Solmaz B, Çavdar S, Kiliç T. The Supraorbital Keyhole Approach. J Craniofac Surg. 2015;26(5):1663–1667. doi: 10.1097/SCS.0000000000001650. [DOI] [PubMed] [Google Scholar]
- 24.Kurbanov A Sanders-Taylor C Keller J T Andaluz N Zuccarello M The extended transorbital craniotomy: an anatomic study Neurosurgery 201511202338–344., discussion 344 [DOI] [PubMed] [Google Scholar]
- 25.Gosain A K Sewall S R Yousif N J The temporal branch of the facial nerve: how reliably can we predict its path? Plast Reconstr Surg 19979951224–1233., discussion 1234–1236 [DOI] [PubMed] [Google Scholar]


