Abstract
Recurrent deep venous thrombosis and inferior vena cava (IVC) thrombosis are well-described complications following IVC filter placement. IVC thrombosis ranges in severity of clinical presentation, but can lead to significant morbidity and mortality with incidence rates depending on patient population and type of filter used. Endovascular therapies such as catheter-directed thrombolysis, mechanical thrombectomy, balloon venoplasty, and stenting are safe and effective in restoration of venous patency.
Keywords: inferior vena cava filter, IVC thrombosis, deep venous thrombosis, interventional radiology, thrombectomy, thrombolysis
Objectives: Upon completion of this article, the reader will be able to identify the risk of deep vein thrombosis and IVC thrombosis due to IVC filter placement and describe the workup and management of these complications.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Inferior vena cava filters (IVCFs) are an important alternative for treatment of deep vein thrombosis (DVT) in cases where pharmacologic anticoagulation is contraindicated or ineffective.1 2 However, while IVCFs are effective in decreasing the incidence of pulmonary embolism (PE), they are associated with long-term risks including increased risk or DVT and IVC thrombosis.3 4
Inferior Vena Cava–associated Deep Venous Thrombosis
Recurrent DVT is a well-known complication of IVCF use. The randomized, controlled Prevention du Risque d'Embolie Pulmonaire par Interruption Cave (PREPIC) study demonstrated an 8.5% cumulative incidence of DVT 1 year after permanent IVCF placement. At 2 years, the incidence was 20.8% and at 8 years it was 35.7%.3 4 The incidence of DVT after 2 years and after 8 years was significantly higher in the filter group compared with the nonfilter group.
Heterogeneity in the length of follow-up and patient populations within different studies makes it difficult to compare DVT rate among filter types. However, a review of several case series suggested that among permanent filters, DVT may be more common with the stainless steel Greenfield filter.5 Rates of DVT with retrievable IVCFs range in the literature from 0.8 to 18%.5 6 7 The highest rates reported were with the ALN (ALN International Inc., Bormes les Mimosas, France) and Option filters (Argon Medical Devices Inc., Athens, TX). In a prospective study by Mismetti et al, 15.2% of patients experienced DVT after ALN filter placement, 84% of which occurred during the first 3 months.8 Johnson et al demonstrated a DVT rate of 18% in a prospective study utilizing the Option filter.9
Filter-Associated Inferior Vena Cava Thrombosis
IVC thrombosis is a less common complication, but has potentially serious consequences. The severity of IVC thrombosis can range from small, clinically insignificant thrombus to clot extending into the lower extremities and even complete caval occlusion. IVC thrombus decreases filter patency, impairs lower extremity venous return, and can ultimately lead to stasis. Depending on clot burden, patients may be asymptomatic or go on to develop postthrombotic syndrome, debilitating lower extremity pain and edema, venous claudication, and stasis ulcers.10 Recurrent PE may develop secondary to thrombus propagation above the filter or via collateral vessels bypassing the IVC filter. Cases of renal failure secondary to propagation into the renal veins have been reported.11
The incidence of symptomatic and asymptomatic IVC occlusion varies significantly in the literature and depends on the study population and type of filter used. For permanent filters, rates of IVC thrombosis range from 1.6 up to 33%.3 4 7 12 13 14 15 16 17 In the PREPIC study, symptomatic IVC thrombosis was seen in 13% of filter recipients after 8 years of follow-up.3 The incidence of IVC thrombus further varies by filter type, as significantly higher rates of IVC thrombus have been reported for the TrapEase filter (Cordis Corporation, Bridgewater, NJ) when compared with other permanent filters.14 15 A prospective observational study of patients with VenaTech filters (B. Braun/VenaTech, Evanston, IL) demonstrated IVC thrombosis in 33% of patients after 9 years of follow-up.13
IVC thrombosis may be due to entrapment of emboli within the filter, extension of DVT from the lower extremities, or in situ thrombosis due to the intrinsic thrombogenicity of the device. Filter design may play a role in higher rates of IVC thrombosis. TrapEase has been shown to exhibit more flow disturbance than the Greenfield filter due to its more pronounced slant angle, which causes venous stagnation zone formation and partial clot entrapment.18 19
Among retrievable IVCFs, the incidence of IVC thrombosis ranges from 0.6 to 8%.6 14 One review found the lowest rates among Celect filters (Cook, Bloomington, IN) at 0.6% and the highest among Option filters at 8%.6 It should be noted that, in contrast to permanent filters, no long-term prospective studies exist evaluating safety and efficacy among retrievable IVCFs; mean follow-up in studies of retrievable IVCFs is generally less than 1 year. Furthermore, retrievable IVCFs are more commonly placed for prophylaxis,5 and such patients may be at lower risk for thrombotic complications than a patient who has already developed DVT or PE. Thus, the apparent lower rates of DVT and IVC thrombosis among retrievable IVCFs may be attributable to shorter follow-up times and patient factors, rather than true differences in performance compared with permanent devices.
Diagnosis of DVT and IVC Thrombosis
When recurrent DVT or IVC thrombosis is suspected clinically, ultrasound (US) with Doppler is generally the first modality used for diagnosis. While sensitivity for lower extremity DVT is high, US can be limited in the evaluation of the common iliac veins and IVC, particularly in obese patients, in those with severe lower extremity edema, and following orthopedic surgery.20 In circumstances where US is limited, computed tomography (CT) venography is an alternative that can be rapidly obtained. CT venography is useful in defining the extent of clot burden and other incidental findings (Fig. 1A). Disadvantages of CT include the use of ionizing radiation and the need for iodinated contrast, which may not be feasible in patients with poor renal function. For these patients, MRI utilizing steady-state free precession pulse sequences can be used to evaluate the vasculature without gadolinium administration.21
Fig. 1.
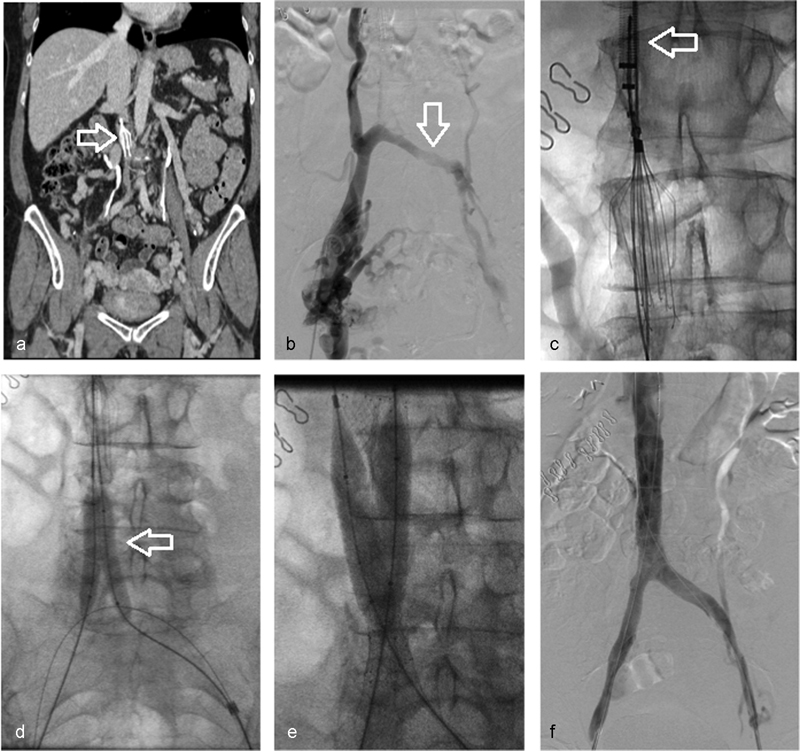
Successful balloon venoplasty and stenting in a 58-year-old woman with chronic thrombosis of the inferior vena cava and bilateral iliac veins after Denali filter (Bard Peripheral Vascular, Tempe, AZ) placement. (a) CT venogram demonstrating occlusion of the IVC and opacification of multiple venous collaterals (arrow—IVC filter). (b) Venography confirms occlusion of the left external iliac vein with mature collaterals draining across the pelvis and into the IVC via lumbar veni collaterals (arrow). (c) Via internal jugular access, an endovascular snare was utilized to capture the filter hook. The filter was then coaxially collapsed in the sheaths (arrow). (d) Sequential 8-mm balloon angioplasty (arrow) of the iliac veins and IVC was performed from each access. (e) 14 mm × 80 mm self-expanding stents were deployed into the IVC immediately cranial to the prior location of the filter. (f) Completion venography demonstrating flow through the stented segments (arrows) without evidence of residual flow-limiting lesion.
Management of Inferior Vena Cava Thrombosis
Pharmacologic anticoagulation, when clinically feasible, remains the mainstay of treatment for recurrent DVT with or without IVC thrombosis. However, anticoagulation may have little effect on regression or resolution of IVCF thrombus or a decrease in the occurrence of PE in patients with IVCFs.22
Early studies describing the use of endovascular therapies for DVT/IVC thrombosis found relatively higher rates of technical failure, residual thrombus, and bleeding complications among patients with IVCFs.23 24 25 26 However, these reports involved very small numbers of patients with IVC thrombus attributable to IVC filtration. Vedantham et al published the largest study to date addressing the use of endovascular therapy to treat IVC thrombosis in patients with IVCFs.27 The authors evaluated endovascular methods, specifically catheter-directed therapy (CDT) with or without mechanical thrombectomy (MT), balloon angioplasty, and stent placement. They reported these techniques to be safe and effective in the short term with a success rate that was comparable to that reported for iliofemoral DVT therapy. The rate of major bleeding was comparable to rates reported in other DVT thrombolysis studies.
Catheter-Directed Therapy and Mechanical Thrombectomy
Catheter-directed therapy enables a localized delivery of thrombolytic agents directly into the thrombus, which may facilitate restoration of venous patency without the increased risk of bleeding complications. CDT has been demonstrated to be effective in reestablishing venous patency in patients with acute iliofemoral DVT, with early clinical success rates of 80 to 85%.28 The choice of thrombolytic agent and the dose used remains variable between institutions. Typically, tPA (Genentech, San Francisco, CA) or urokinase (Abbott Laboratories, Chicago, IL) are used.
Adding MT to CDT can improve thrombus removal and aid in lysis of residual clot.29 30 31 Several devices exist to perform MT. The AngioJet rheolytic thrombectomy system (Boston Scientific, Marlborough, MA) utilizes high-velocity, high-pressure saline jets for thrombus dissolution and aspiration. The EKOS system (EKOS, Bothell, WA) employs low-energy, high-frequency US to aid in thrombectomy. The Trellis device (Bacchus Vascular Inc, Santa Clara, CA) with rotating sinusoidal dispersion wires has been used in this setting; however, it is no longer commercially available.31 Follow-up venography should be performed after CDT, as residual clot may indicate subacute thrombus requiring further thrombolysis or chronic thrombus which may be resistant to CDT.
Technical success and achievement of venous patency may depend on the timing of intervention after symptom onset. Acute clot responds more favorably to CDT and MT than chronic, organized thrombus. Many patients treated for IVCF thrombosis, particularly those with chronic symptoms, may show significant residual clot after thrombolysis.
Balloon Venoplasty and Stent Placement
In patients with chronic IVC thrombosis, balloon angioplasty with primary stent placement may be the best endovascular option (Fig. 1). Neglén et al found stenting across an obstructed IVCF to be safe, with patency rates similar to those without an IVCF in place.32 While thrombolytic infusion prior to stent placement may enable a larger venous diameter to be achieved, it may not be warranted unless there is evidence of acute thrombus.27 After stent placement, an antiplatelet regimen is generally initiated, though this practice varies and no consensus recommendations exist.
Technical Considerations
An IVCF can present significant technical challenges when attempting to restore venous patency. The presence of the filter can lead to difficulty with guidewire recanalization and passage of catheters. Most of the experience in the literature with respect to endovascular treatment of IVCF-related thrombosis is in the setting of permanent IVCFs. However, over the past several years, an increasing proportion of filters being placed are retrievable.33 In cases of IVC recanalization due to thrombosis related to a retrievable IVCF, fracture or deformation during intervention could result in filter failure or predisposition to recurrent thrombosis. Therefore, filter removal should be considered, even if a new filter needs to be placed. IVCFs present within a chronically occluded vena cava or those that have been deformed during intervention may be difficult to remove and utilization of adjunctive techniques for removal may be necessary.34
Conclusion
Recurrent DVT and IVC thrombosis are well-recognized complications following IVCF placement that may lead to significant morbidity and mortality. Endovascular therapies such as CDT, MT, balloon venoplasty, and stenting are safe and effective in restoration of venous patency.
References
- 1.Geerts W H Bergqvist D Pineo G F et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest 2008133(6, Suppl):381S–453S. [DOI] [PubMed] [Google Scholar]
- 2.Kaufman J A, Kinney T B, Streiff M B. et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol. 2006;17(3):449–459. doi: 10.1097/01.rvi.0000203418-39769.0d. [DOI] [PubMed] [Google Scholar]
- 3.PREPIC Study Group . Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. 2005;112(3):416–422. doi: 10.1161/CIRCULATIONAHA.104.512834. [DOI] [PubMed] [Google Scholar]
- 4.Decousus H, Leizorovicz A, Parent F. et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338(7):409–415. doi: 10.1056/NEJM199802123380701. [DOI] [PubMed] [Google Scholar]
- 5.Rajasekhar A, Streiff M B. Vena cava filters for management of venous thromboembolism: a clinical review. Blood Rev. 2013;27(5):225–241. doi: 10.1016/j.blre.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Angel L F, Tapson V, Galgon R E, Restrepo M I, Kaufman J. Systematic review of the use of retrievable inferior vena cava filters. J Vasc Interv Radiol. 2011;22(11):1522–1.53E6. doi: 10.1016/j.jvir.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 7.Sella D M, Oldenburg W A. Complications of inferior vena cava filters. Semin Vasc Surg. 2013;26(1):23–28. doi: 10.1053/j.semvascsurg.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Mismetti P, Rivron-Guillot K, Quenet S. et al. A prospective long-term study of 220 patients with a retrievable vena cava filter for secondary prevention of venous thromboembolism. Chest. 2007;131(1):223–229. doi: 10.1378/chest.06-0631. [DOI] [PubMed] [Google Scholar]
- 9.Johnson M S, Nemcek A A Jr, Benenati J F. et al. The safety and effectiveness of the retrievable option inferior vena cava filter: a United States prospective multicenter clinical study. J Vasc Interv Radiol. 2010;21(8):1173–1184. doi: 10.1016/j.jvir.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Fox M A, Kahn S R. Postthrombotic syndrome in relation to vena cava filter placement: a systematic review. J Vasc Interv Radiol. 2008;19(7):981–985. doi: 10.1016/j.jvir.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 11.Marcy P Y, Magné N, Frenay M, Bruneton J N. Renal failure secondary to thrombotic complications of suprarenal inferior vena cava filter in cancer patients. Cardiovasc Intervent Radiol. 2001;24(4):257–259. doi: 10.1007/s00270-001-0015-9. [DOI] [PubMed] [Google Scholar]
- 12.Caplin D M Nikolic B Kalva S P Ganguli S Saad W E Zuckerman D A; Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism J Vasc Interv Radiol 201122111499–1506. [DOI] [PubMed] [Google Scholar]
- 13.Crochet D P, Brunel P, Trogrlic S, Grossetëte R, Auget J L, Dary C. Long-term follow-up of Vena Tech-LGM filter: predictors and frequency of caval occlusion. J Vasc Interv Radiol. 1999;10(2, Pt 1):137–142. doi: 10.1016/s1051-0443(99)70455-0. [DOI] [PubMed] [Google Scholar]
- 14.Nazzal M, Chan E, Nazzal M. et al. Complications related to inferior vena cava filters: a single-center experience. Ann Vasc Surg. 2010;24(4):480–486. doi: 10.1016/j.avsg.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Usoh F, Hingorani A, Ascher E. et al. Prospective randomized study comparing the clinical outcomes between inferior vena cava Greenfield and TrapEase filters. J Vasc Surg. 2010;52(2):394–399. doi: 10.1016/j.jvs.2010.02.280. [DOI] [PubMed] [Google Scholar]
- 16.Schutzer R, Ascher E, Hingorani A, Jacob T, Kallakuri S. Preliminary results of the new 6F TrapEase inferior vena cava filter. Ann Vasc Surg. 2003;17(1):103–106. doi: 10.1007/s10016-001-0328-9. [DOI] [PubMed] [Google Scholar]
- 17.Hajduk B, Tomkowski W Z, Malek G, Davidson B L. Vena cava filter occlusion and venous thromboembolism risk in persistently anticoagulated patients: a prospective, observational cohort study. Chest. 2010;137(4):877–882. doi: 10.1378/chest.09-1533. [DOI] [PubMed] [Google Scholar]
- 18.Harlal A, Ojha M, Johnston K W. Vena cava filter performance based on hemodynamics and reported thrombosis and pulmonary embolism patterns. J Vasc Interv Radiol. 2007;18(1, Pt 1):103–115. doi: 10.1016/j.jvir.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 19.Leask R L, Johnston K W, Ojha M. Hemodynamic effects of clot entrapment in the TrapEase inferior vena cava filter. J Vasc Interv Radiol. 2004;15(5):485–490. doi: 10.1097/01.rvi.0000124941.58200.85. [DOI] [PubMed] [Google Scholar]
- 20.Gaitini D. Current approaches and controversial issues in the diagnosis of deep vein thrombosis via duplex Doppler ultrasound. J Clin Ultrasound. 2006;34(6):289–297. doi: 10.1002/jcu.20236. [DOI] [PubMed] [Google Scholar]
- 21.Lindquist C M, Karlicki F, Lawrence P, Strzelczyk J, Pawlyshyn N, Kirkpatrick I D. Utility of balanced steady-state free precession MR venography in the diagnosis of lower extremity deep venous thrombosis. AJR Am J Roentgenol. 2010;194(5):1357–1364. doi: 10.2214/AJR.09.3552. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad I, Yeddula K, Wicky S, Kalva S P. Clinical sequelae of thrombus in an inferior vena cava filter. Cardiovasc Intervent Radiol. 2010;33(2):285–289. doi: 10.1007/s00270-009-9664-x. [DOI] [PubMed] [Google Scholar]
- 23.Angle J F, Matsumoto A H, Al Shammari M, Hagspiel K D, Spinosa D J, Humphries J E. Transcatheter regional urokinase therapy in the management of inferior vena cava thrombosis. J Vasc Interv Radiol. 1998;9(6):917–925. doi: 10.1016/s1051-0443(98)70422-1. [DOI] [PubMed] [Google Scholar]
- 24.Hansen M E, Miller G L III, Starks K C. Pulse-spray thrombolysis of inferior vena cava thrombosis complicating filter placement. Cardiovasc Intervent Radiol. 1994;17(1):38–40. doi: 10.1007/BF01102071. [DOI] [PubMed] [Google Scholar]
- 25.Ryu R K, Durham J D, Kumpe D A. Transcatheter venous thrombolysis—pitfalls and pratfalls: a case discussion of indications, technique, and alternatives. J Vasc Interv Radiol. 1997;8(6):1005–1010. doi: 10.1016/s1051-0443(97)70702-4. [DOI] [PubMed] [Google Scholar]
- 26.Tarry W C, Makhoul R G, Tisnado J, Posner M P, Sobel M, Lee H M. Catheter-directed thrombolysis following vena cava filtration for severe deep venous thrombosis. Ann Vasc Surg. 1994;8(6):583–590. doi: 10.1007/BF02017416. [DOI] [PubMed] [Google Scholar]
- 27.Vedantham S, Vesely T M, Parti N. et al. Endovascular recanalization of the thrombosed filter-bearing inferior vena cava. J Vasc Interv Radiol. 2003;14(7):893–903. doi: 10.1097/01.rvi.0000083842.97061.c9. [DOI] [PubMed] [Google Scholar]
- 28.Mewissen M W, Seabrook G R, Meissner M H, Cynamon J, Labropoulos N, Haughton S H. Catheter-directed thrombolysis for lower extremity deep venous thrombosis: report of a national multicenter registry. Radiology. 1999;211(1):39–49. doi: 10.1148/radiology.211.1.r99ap4739. [DOI] [PubMed] [Google Scholar]
- 29.Comerota A J The ATTRACT trial: rationale for early intervention for iliofemoral DVT Perspect Vasc Surg Endovasc Ther 2009214221–224., quiz 224–225 [DOI] [PubMed] [Google Scholar]
- 30.Poon W L, Luk S H, Yam K Y, Lee A C. Mechanical thrombectomy in inferior vena cava thrombosis after caval filter placement: a report of three cases. Cardiovasc Intervent Radiol. 2002;25(5):440–443. doi: 10.1007/s00270-002-1921-1. [DOI] [PubMed] [Google Scholar]
- 31.McLafferty R B. Endovascular management of deep venous thrombosis. Perspect Vasc Surg Endovasc Ther. 2008;20(1):87–91. doi: 10.1177/1531003507313304. [DOI] [PubMed] [Google Scholar]
- 32.Neglén P, Oglesbee M, Olivier J, Raju S. Stenting of chronically obstructed inferior vena cava filters. J Vasc Surg. 2011;54(1):153–161. doi: 10.1016/j.jvs.2010.11.117. [DOI] [PubMed] [Google Scholar]
- 33.Smouse B, Johar A. Endovascular Today; 2010. Is market growth of vena cava filters justified? pp. 74–77. [Google Scholar]
- 34.Pellerin O, Barral F G, Lions C, Novelli L, Beregi J P, Sapoval M. Early and late retrieval of the ALN removable vena cava filter: results from a multicenter study. Cardiovasc Intervent Radiol. 2008;31(5):889–896. doi: 10.1007/s00270-008-9357-x. [DOI] [PubMed] [Google Scholar]


