Abstract
Placement of retrievable inferior vena cava filters has seen rapid growth since their introduction into clinical practice. When retrieved, these devices offer the notional benefit of temporary protection from pulmonary embolism related to lower extremity deep venous thrombosis, and mitigation of filter-related deep venous thrombosis. When promptly removed after the indication for mechanical prophylaxis is no longer present, standard endovascular retrieval techniques are frequently successful. However, the majority of these devices are left in place for extended periods of time, which has been associated with greater device-related complications when left in situ, and failure of standard techniques when retrieval is attempted. The development of advanced retrieval techniques has had a positive impact on retrieval of these embedded devices. In this article, technical considerations in the retrieval of such devices, with an emphasis on advanced techniques to facilitate retrieval of embedded devices, are discussed.
Keywords: retrievable inferior vena cava filters, advanced retrieval techniques, interventional radiology
Objectives: Upon completion of this article, the reader will be able to describe the basic utility of retrievable inferior vena cava filters and assess advanced techniques and when they are most effective for filter retrieval.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Venous thromboembolism (VTE) presents a significant burden on the health care system, resulting in high rates of morbidity and mortality as well as several million dollars annually in health care costs.1 Inferior vena cava filters (IVCFs) are utilized in patients with VTE in whom anticoagulation has failed or is contraindicated, as well as for prophylaxis from VTE. Prior prospective studies have demonstrated that while permanent IVCFs are effective in preventing pulmonary embolism (PE), they are associated with an increased risk of lower extremity deep venous thrombosis (DVT).2 3 Retrievable inferior vena cava filters (rIVCFs) were developed to protect against PE and to allow removal once the timeframe for indicated use has passed, thereby mitigating the risk of filter-related DVT.
Though designed to be removed when no longer indicated, the majority of filters are left in place for prolonged periods of time, if not permanently.4 5 Studies have demonstrated that prolonged dwell time for rIVCF is not only more likely to be subject to greater device-related complications but also likely to fail retrieval with standard techniques.6 7 Findings such as these have prompted the United States Food and Drug Administration (FDA) to issue a safety communication in 2014, recommending that all rIVCFs be removed as soon as protection from PE is no longer needed.8
Impediments to Removal of Retrievable IVC Filters
Poor clinical follow-up of patients with rIVCF impedes retrieval of devices that are no longer indicated. Several studies have confirmed this theory, with reported retrieval rates as low as 8.5%.9 The development of dedicated service lines for patients with these devices have positively impacted retrieval rates, with one study reporting an increase in retrieval rates from 29 to 60% after the establishment of a dedicated IVC filter service.10
Prior studies have identified prolonged rIVCF dwell time as a negative predictor for successful retrieval. Dwell times of 90 days and 6 months have been separately reported as being significantly associated with retrieval failure.11 12 Findings from studies like these have led to the perception that prolonged dwell time rIVCFs should be left in situ due to the likelihood of procedural failure and the theoretical risk of vascular injury.
The development of advanced retrieval techniques has positively impacted filter retrieval, particularly of embedded devices with prolonged dwell times. Studies have demonstrated that advanced techniques are more likely to be necessary to retrieve filters with prolonged dwell time, but can do so very effectively.13 These techniques have effectively removed the “time limit” on filter retrieval. A series of 648 retrievals confirms this notion, demonstrating that filter removal can be performed regardless of filter dwell time with a success rate of 97% or more when advanced endovascular techniques are employed.14 In this series, there was a strong positive association with filter dwell time and the need for advanced filter techniques. Despite the complex nature of some of these advanced retrieval procedures, reported complication rates were low and were not associated with filter dwell time.14
Filter Removal Techniques
Most rIVCFs employ a conical design, including the Denali, G2X/G2, Eclipse, Meridian, Recovery (all Bard Peripheral Vascular Inc., Tempe, AZ); Celect, Gunther Tulip (both Cook Medical Inc., Bloomington, IN); ALN (ALN Implants Chirurgicaux, Ghisonaccia, France); and Option/Option Elite (Argon Medical Devices, Plano, TX). These devices are designed to be retrieved via an internal jugular venous access. The OptEase (Cordis Corp., Miami Lakes, FL) has a nonconical polyhedron design and is designed to be retrieved from a femoral venous approach. A relative newcomer to the market, the Crux (Volcano Corp., San Diego, CA), has a helical design with hooks on both the caudal and cranial aspects of the filter, allowing retrieval from either a jugular or femoral approach.
Standard Retrieval Techniques
Most rIVCFs have a hook that facilitates retrieval utilizing an endovascular snare, with the majority of devices designed for retrieval from jugular venous access (Fig. 1). Older devices (particularly the Bard G2 and Recovery) have a smooth bushing at the apex, designed to be retrieved with a proprietary retrieval cone device. Individual manufacturers offer retrieval kits for their specific device, but all use the common mechanism of an endovascular snare to capture the filter by its hook, and a sheath to facilitate coaxial collapse of the filter and disengagement from the caval wall. In the authors' experience, proprietary kits are not necessary.
Fig. 1.
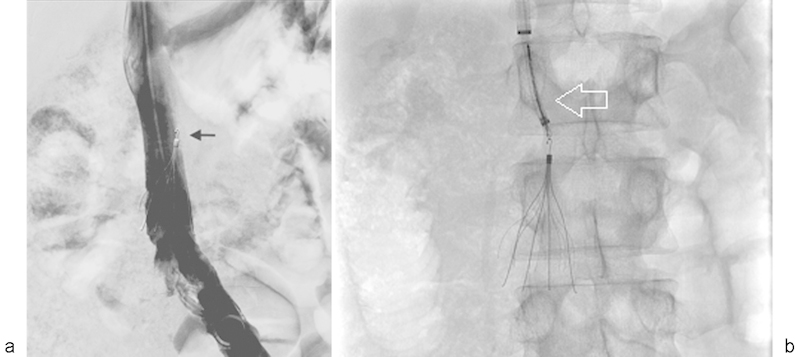
Curved sheath use for retrieval of tilted, nonembedded filters. (a) Filter hook is significantly tilted from the central axis of the inferior vena cava (arrow). (b) Curved inner sheath (white arrow) provides greater directionality to enable successful snaring of the filter hook.
The authors' approach to standard filter retrieval begins with a pigtail flush catheter, which is introduced over a wire caudal to the filter. Care is taken not to entangle the wire or catheter in the filter. After inferior vena cavography is performed to assess for in situ filter thrombus, coaxial sheaths are placed immediately cephalad to the filter. A standard endovascular snare is used to capture the filter hook; once captured, the filter is collapsed within the sheath while gentle counter traction is applied via the snare.
Advanced Retrieval Techniques
Standard filter removal can fail for a variety of reasons, including filter tilt, encasement of the filter hook in the IVC wall by a fibrin cap, incorporation of filter elements into the caval wall, significant extracaval perforation of filter elements, and filter fracture. In these cases, advanced retrieval techniques have been employed to successfully remove the rIVCF.
When filters are tilted significantly, standard straight sheaths and snare devices are often unable to capture the filter hook successfully. The use of a curved inner sheath can add directionality and facilitate successful snaring of a hook that is significantly deviated from the central axis of the IVC (Fig. 1). This technique is most useful when the filter hook is not embedded and no fibrin cap has formed. In the authors' practice, a Flexor sheath with Ansel 2 modification (Cook Medical Inc.) is used.
A rIVCF with an embedded tip or hook presents a significant challenge during retrieval. Several techniques have been described as an approach to this problem; however, two techniques that are most used in the authors' practice are highlighted here. These techniques are the loop snare and use of rigid endobronchial forceps.
The loop snare method was originally described where a reverse curve catheter was guided through the filter struts as a locus of support, and a hydrophilic wire was passed through the catheter and advanced cephalad.15 The wire is snared and externalized via the jugular access to provide counter-traction while the filter is coaxially collapsed into the sheath and removed. The concern with this technique is the potential for filter fracture, given the large forces exerted over a small area where the loop wire is engaged. Instead, the authors developed a modified loop wire technique that also addresses the fibrin cap. Rather than passing the catheter through the filter struts, the reverse curve catheter is used to engage the cap at the filter apex; the looped hydrophilic wire then creates a loop through the fibrin cap.16 Applied counter-tension allows coaxial collapse of the filter and disruption of the fibrin cap, subsequently allowing for filter removal with standard snare techniques (Fig. 2).
Fig. 2.
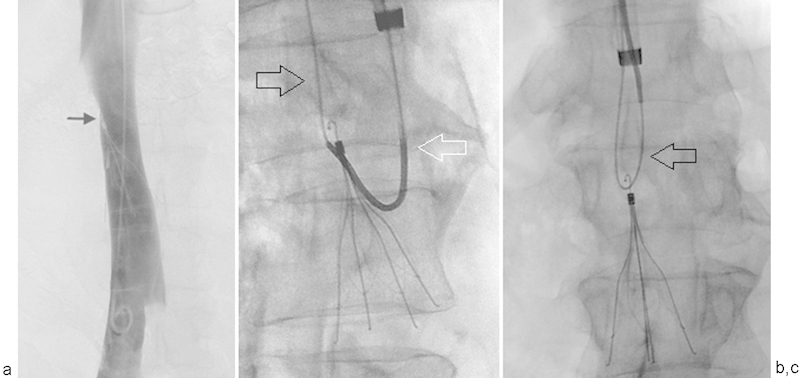
Loop wire capture of fibrin cap. (a) Digital subtraction cavography demonstrates filter hook abutting the right lateral caval wall with suggestion of fibrin cap formation (arrow). Standard techniques failed to remove this device. (b) Reverse curve catheter (white arrow) utilized to engage fibrin cap. Hydrophilic wire (black arrow) is advanced cranially and captured with snare device. (c) Loop wire successfully engaged on fibrin cap. Note that no portion of the wire (arrow) is through the filter struts.
Rigid endobronchial forceps are used for dissection of fibrin encasing the filter apex, thus exposing the hook for filter capture via forceps or snare and subsequently allowing collapse and removal of the filter17 (Fig. 3). These forceps are usually malleable, and can be adjusted to achieve optimum curvature to reach a tilted, embedded filter apex. The interventional radiologist must be alert to potential adverse events when using this device, as excess curvature of the instrument or applied force can cause significant patient discomfort from distention of the IVC. Furthermore, IVC wall rupture is possible when the caval wall is grasped rather than the fibrin obscuring the hook. With sufficient operator experience, however, these devices can be employed safely. In their reports, Stavropoulos et al and Avery et al report filter retrieval success rates of 95 and 85%, respectively, both reporting no major adverse events.17 18
Fig. 3.
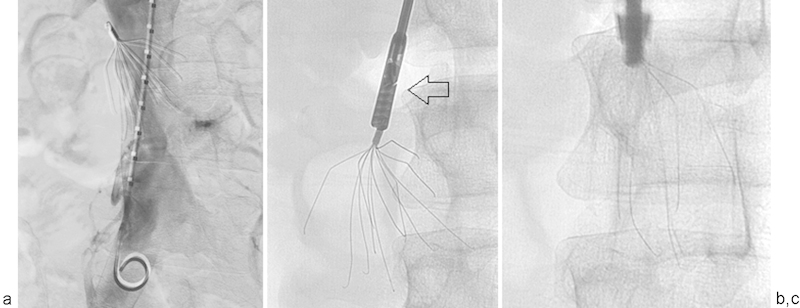
Endobronchial forceps in IVC filter retrieval. (a) Digital subtraction cavogram demonstrates embedded hook and multiple penetrated struts. (b) Rigid endobronchial forceps (arrow) utilized to dissect fibrin off of hook and capture filter hook/apex. (c) Successfully captured filter can then be collapsed in sheath.
In some cases, a filter hook can be successfully captured, but the rIVCF cannot be collapsed within the sheath despite exertion of large forces. This typically occurs when there is incorporation of the filter struts into the wall. Laser extraction sheaths originally designed for pacemaker lead extraction have been successfully used to photothermally ablate the fibrin encasing the filter struts into the caval wall (Fig. 4), allowing filter removal without having to exert large and potentially hazardous forces during the retrieval procedure.19 The CVX-300 Excimer laser system utilizes 12, 14, and 16F, 50-cm-long sheaths that are introduced via a larger outer sheath. Photothermal ablation frees the filter from caval wall attachment, allowing it to be collapsed and retrieved through the outer sheath. When used, the laser sheath is highly successful, with Kuo and Cupp reporting a 98% technical retrieval success rate using this technique.19 It is important to note that control of the filter apex/hook is required to successfully employ photothermal laser ablation; indeed, it is common in the authors' practice that other techniques must be employed to free the filter apex prior to using the laser sheath.
Fig. 4.
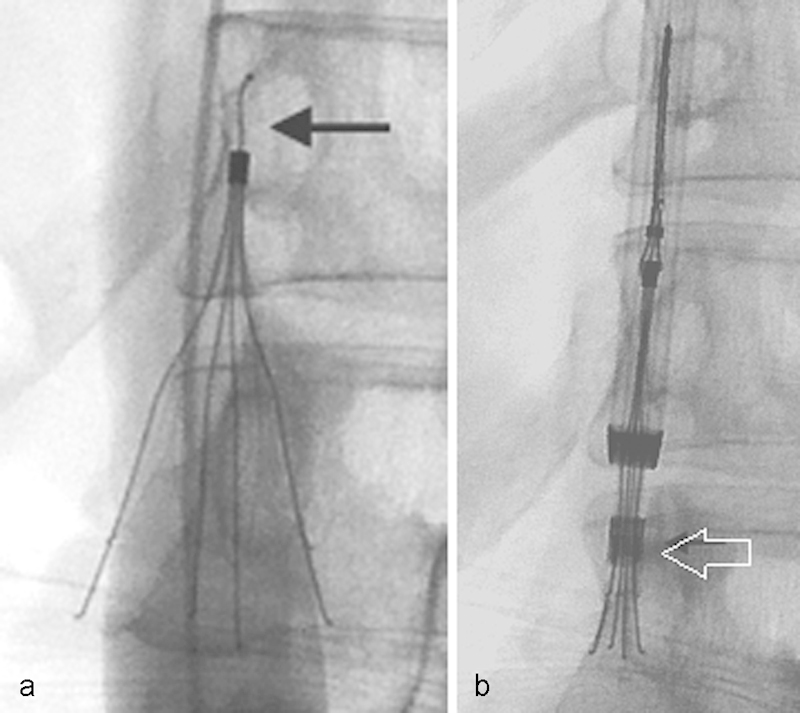
Photothermal laser ablation for embedded IVC filter struts. (a) Cavogram demonstrates that lower portion of filter struts is penetrated. Note that the hook is straightened from prior filter retrieval attempt (arrow). (b) After snare capture of filter apex, the laser sheath (arrow) is sequentially activated to enable ablation of fibrin, thus enabling filter removal.
Conclusion
Retrievable inferior vena cava filters remain an important option in providing temporary protection from PE in patients who cannot receive anticoagulation. With the continued growth in the use of these devices, clinical follow-up and surveillance of patients with these devices take a heightened importance, particularly in light of device-related complications that appear to increase with prolonged filter dwell time. Proper employment of the advanced retrieval techniques described here fosters the safe removal of the majority of devices, regardless of filter dwell time. In accordance with the FDA safety communication, removal should be considered in all patients in whom the rIVCF is no longer indicated.
References
- 1.Geerts W H, Bergqvist D, Pineo G F. et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133(6):381–453. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 2.Decousus H, Leizorovicz A, Parent F. et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338(7):409–415. doi: 10.1056/NEJM199802123380701. [DOI] [PubMed] [Google Scholar]
- 3.Group P S; PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study Circulation 20051123416–422. [DOI] [PubMed] [Google Scholar]
- 4.Smouse B, Johar A. Is market growth of vena cava filters justified? Endovasc Today. 2010;2010:74–77. [Google Scholar]
- 5.Helling T S, Kaswan S, Miller S L, Tretter J F. Practice patterns in the use of retrievable inferior vena cava filters in a trauma population: a single-center experience. J Trauma. 2009;67(6):1293–1296. doi: 10.1097/TA.0b013e3181b0637a. [DOI] [PubMed] [Google Scholar]
- 6.Andreoli J M, Lewandowski R J, Vogelzang R L, Ryu R K. Comparison of complication rates associated with permanent and retrievable inferior vena cava filters: a review of the MAUDE database. J Vasc Interv Radiol. 2014;25(8):1181–1185. doi: 10.1016/j.jvir.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Marquess J S, Burke C T, Beecham A H. et al. Factors associated with failed retrieval of the Günther Tulip inferior vena cava filter. J Vasc Interv Radiol. 2008;19(9):1321–1327. doi: 10.1016/j.jvir.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Health C for D and R. Safety Communications - Removing Retrievable Inferior Vena Cava Filters Initial Communication [Internet]. Available at: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm221676.htm; Accessed December 2015
- 9.Sarosiek S, Crowther M, Sloan J M. Indications, complications, and management of inferior vena cava filters: the experience in 952 patients at an academic hospital with a level I trauma center. JAMA Intern Med. 2013;173(7):513–517. doi: 10.1001/jamainternmed.2013.343. [DOI] [PubMed] [Google Scholar]
- 10.Minocha J, Idakoji I, Riaz A. et al. Improving inferior vena cava filter retrieval rates: impact of a dedicated inferior vena cava filter clinic. J Vasc Interv Radiol. 2010;21(12):1847–1851. doi: 10.1016/j.jvir.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Geisbüsch P, Benenati J F, Peña C S. et al. Retrievable inferior vena cava filters: factors that affect retrieval success. Cardiovasc Intervent Radiol. 2012;35(5):1059–1065. doi: 10.1007/s00270-011-0268-x. [DOI] [PubMed] [Google Scholar]
- 12.Rosenthal D, Wellons E D, Hancock S M, Burkett A B. Retrievability of the Günther Tulip vena cava filter after dwell times longer than 180 days in patients with multiple trauma. J Endovasc Ther. 2007;14(3):406–410. doi: 10.1583/06-2045.1. [DOI] [PubMed] [Google Scholar]
- 13.Al-Hakim R Kee S T Olinger K Lee E W Moriarty J M McWilliams J P Inferior vena cava filter retrieval: effectiveness and complications of routine and advanced techniques J Vasc Interv Radiol 2014256933–939., quiz 940 [DOI] [PubMed] [Google Scholar]
- 14.Desai K R, Lewandowski R J, Salem R. et al. Retrieval of inferior vena cava filters with prolonged dwell time: a single-center experience in 648 retrieval procedures. JAMA Intern Med. 2015;175(9):1572–1574. doi: 10.1001/jamainternmed.2015.2561. [DOI] [PubMed] [Google Scholar]
- 15.Rubenstein L, Chun A K, Chew M, Binkert C A. Loop-snare technique for difficult inferior vena cava filter retrievals. J Vasc Interv Radiol. 2007;18(10):1315–1318. doi: 10.1016/j.jvir.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Esparaz A M, Ryu R K, Gupta R, Resnick S A, Salem R, Lewandowski R J. Fibrin cap disruption: an adjunctive technique for inferior vena cava filter retrieval. J Vasc Interv Radiol. 2012;23(9):1233–1235. doi: 10.1016/j.jvir.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Stavropoulos S W, Dixon R G, Burke C T. et al. Embedded inferior vena cava filter removal: use of endobronchial forceps. J Vasc Interv Radiol. 2008;19(9):1297–1301. doi: 10.1016/j.jvir.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 18.Avery A, Stephens M, Redmond K, Harper J. Initial experience using the rigid forceps technique to remove wall-embedded IVC filters. J Med Imaging Radiat Oncol. 2015;59(3):306–311. doi: 10.1111/1754-9485.12299. [DOI] [PubMed] [Google Scholar]
- 19.Kuo W T, Cupp J S. The excimer laser sheath technique for embedded inferior vena cava filter removal. J Vasc Interv Radiol. 2010;21(12):1896–1899. doi: 10.1016/j.jvir.2010.08.013. [DOI] [PubMed] [Google Scholar]


