Abstract
Inferior vena cava filters have been placed in patients for decades for protection against pulmonary embolism. The widespread use of filters has dramatically increased owing at least in part to the approval of retrievable vena cava filters. Retrievable filters have the potential to protect against pulmonary embolism and then be retrieved once no longer needed to avoid potential long-term complications. There are several retrievable vena cava filters available for use. This article discusses the different filter designs as well as the published data on these available filters. When selecting a filter for use, it is important to consider the potential short-term complications and the filters' window for retrieval. Understanding potential long-term complications is also critical, as these devices are approved for permanent placement and many filters are not retrieved. Finally, this article will address research into new designs that may be the future of vena cava filtration.
Keywords: inferior vena cava filter, pulmonary embolism, deep venous thrombosis, venous thromboembolic event, interventional radiology
Objectives: Upon completion of this article, the reader will be able to identify the available IVC filter designs, efficacy, and outcomes.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Endovascular interruption of the inferior vena cava (IVC) for the prevention of pulmonary embolism (PE) has been utilized for over four decades, but retrievable vena cava filters are considerably more recent. The United States Food and Drug Administration (FDA) first approved percutaneous retrieval of three existing permanent vena cava filters in 2003 and 2004 without modifications of the indications for placement.1 This approval gave physicians the option of either removing IVC filters once the risk of PE had passed or leaving the device in place permanently. While permanent IVC filters have been shown in a prospective, randomized controlled trial to decrease PE, long-term use is associated with an increased risk of deep venous thrombosis (DVT).2 3 Retrievable filters would presumably offer the same benefit of protection against PE without the long-term risks, although this remains to be proven.
Despite the lack of high-quality evidence, the use of IVC filters has dramatically increased over time.4 5 Many retrievable filters, however, are not retrieved for a variety of reasons. In addition to thrombotic complications, there are numerous reports of filter fracture, migration, and penetration/perforation for both permanent and retrievable filters, with the majority of complications associated with chronic use.6 7 8 This article will review the design and data of retrievable IVC filters currently available, and assess what the future filter design may hold.
Filter Design
The first three IVC filters approved for retrieval were the Günther Tulip (Cook, Bloomington, IN), the Recovery (Bard; Tempe, AZ), and the OptEase (Cordis, Fremont, CA).9 The Tulip and the Recovery have conical designs, while the OptEase has a double basket design like its predecessor designed for permanent placement, the TrapEase filter (Cordis). The Tulip and OptEase filters remain on the market, while Bard has since developed multiple iterations of the Recovery and currently offers the Denali filter.
The majority of IVC filters on the market offer a conical design, including the aforementioned Günther Tulip and Denali as well as the ALN filter (ALN Implants Chirurgicaux; Ghisonaccia, France), Celect Platinum (Cook), and Option Elite (Argon Medical Devices, Plano, TX) (Table 1, Fig. 1). The Celect Platinum filter is a minor variant of the previously offered Celect filter, designed to increase visibility with platinum markers and specially designed anchors on the filters feet. The Celect filter was a modification of the Günther Tulip filter, and was created to improve retrievability in which the secondary legs do not contact and overlap the primary legs as with the Tulip filter. The Option Elite filter is a variant of the Option filter and offers an over-the-wire delivery system to aid with centering the filter. The Denali and Celect Platinum filters have two levels of filtration with legs of differing lengths. While the ALN filter has two levels of struts, all legs differ slightly in length to prevent entanglement during delivery. Additionally, the ALN filter now offers a design with a cranial hook allowing retrieval with the end users' choice of snares. Introducer sheath sizes for these filters range from 5F for the Option Elite to 8.4F for the Denali; all filters can be placed from a jugular or femoral approach.
Table 1. Retrievable IVC filters currently available in the United States.
| Filter (manufacturer) | Material | Design | Introducer sheath | Maximum IVC diameter | Placement approach | Retrieval approach |
|---|---|---|---|---|---|---|
| Conical designs | ||||||
| ALN (ALN Implants Chirurgicaux, Ghisonaccia, France) | Stainless steel | Six shorter anchoring struts with hooks, three longer centering struts; all struts differ in length; new design with cranial hook | 7F | 32 mm | Jugular, brachial, femoral | Jugular |
| Celect Platinum (Cook, Bloomington, IN) | Cobalt–chromium alloy | Four legs with anchors and platinum markers on feet, eight shorter stabilizing wires | 7F | 30 mm | Jugular, femoral | Jugular |
| Denali (Bard, Tempe, AZ) | Nickel–titanium alloy | Six legs with anchors, six upper arms | 8.4F | 28 mm | Jugular, subclavian, femoral | Jugular |
| Günther Tulip (Cook) | Cobalt–chromium alloy | Four longer primary legs with anchors, eight secondary limbs that bridge the primary legs | 7F | 30 mm | Jugular, femoral | Jugular |
| Option Elite (Argon Medical Devices, Plano, TX) | Nickel–titanium alloy | Six legs with anchors | 5F | 30 mm | Jugular, antecubital, femoral, popliteal | Jugular |
| Nonconical designs | ||||||
| Crux (Volcano, San Diego, CA) | Nickel–titanium alloy and ePTFE | Symmetrical nitinol wire spiral design with ePTFE filter web in the caudal portion, five tissue anchors | 9F | 28 mm | Jugular, femoral | Jugular, femoral |
| OptEase (Cordis, Fremont, CA) | Nickel–titanium alloy | Double basket with side struts and six superior barbs, caudal hook | 6F | 30 mm | Jugular, antecubital, femoral | Femoral |
Abbreviations: ePTFE, expanded polytetrafluoroethylene; IVC, inferior vena cava.
Fig. 1.
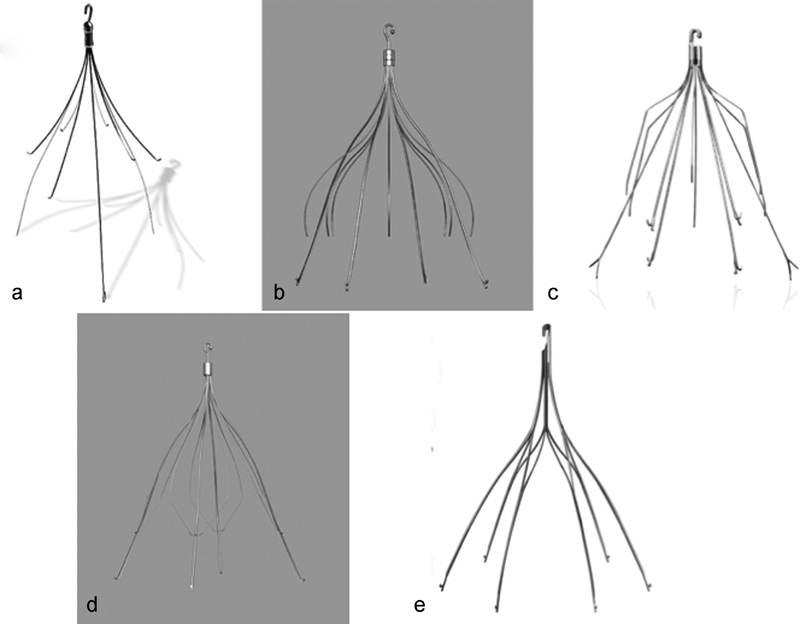
Retrievable inferior vena cava filters with a conical design. (a) ALN (ALN Implants Chirurgicaux, Ghisonaccia, France); (b) Celect Platinum (Cook, Bloomington, IN); (c) Denali (Bard; Tempe, AZ); (d) Günther Tulip (Cook); (e) Option Elite (Argon Medical Devices, Plano, TX).
The ALN filter can be placed from a brachial approach, the Denali from a subclavian approach, and the small introducer size of the Option Elite permits an antecubital or popliteal approach. All conical filters are retrieved from a jugular approach. These filters are manufactured from stainless steel (ALN), nickel–titanium alloy (Denali and Option Elite), or cobalt–chromium alloy (Celect Platinum and Günther Tulip). All are rated magnetic resonance imaging (MRI) conditional. The ALN filter can be placed in an IVC with a maximal diameter of 32 mm. The Denali filter is rated for an IVC with a maximal diameter of 28 mm, and the remaining conical filters can be placed in an IVC with a maximal diameter of 30 mm.
The two retrievable filters currently marketed in the United States that do not have a conical design are the OptEase (Cordis) and the Crux (Volcano, San Diego, CA) (Table 1, Fig. 2). Both of these filters are made from nickel–titanium alloy and are rated MRI conditional. The OptEase has a double-basket design with side struts and six superior anchoring barbs. Although the filter looks symmetrical, suggesting the same filter can be placed from a jugular or femoral approach, the anchoring barbs preventing cephalad migration are directed differently based on whether the filter is indicated as a femoral or jugular device. It features a caudal hook and is retrieved from a femoral approach. The OptEase uses a 6F introducer sheath and can be delivered via a jugular, antecubital, or femoral approach; it can be placed in an IVC with a maximal diameter of 30 mm. The Crux filter is an entirely different design with two symmetric spiral wire forms connected at the ends with a web of expanded polytetrafluoroethylene (ePTFE) in the caudal portion, five tissue anchors, and a sinusoidal retrieval tail at each end. It can be deployed in an IVC measuring 17 to 28 mm via a jugular or femoral approach. The delivery sheath measures 9F. Because of the tails at each end, this filter can be retrieved from either a jugular or femoral approach.
Fig. 2.
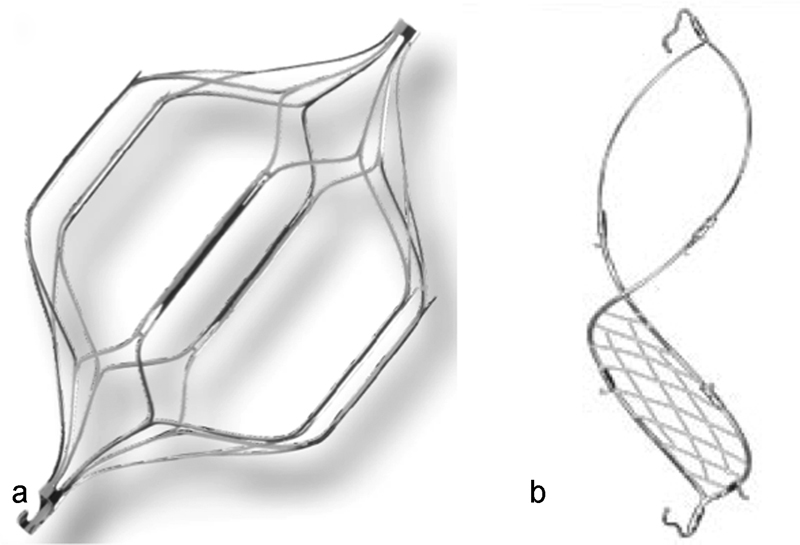
Retrievable inferior vena cava filters with a nonconical design. (a) OptEase (Cordis, Fremont, CA); (b) Crux (Volcano, San Diego, CA).
An alternative to the traditional retrievable filter is the VenaTech Convertible filter (B. Braun, Melsungen, Germany) (Fig. 3). The design of this filter, made from chromium–cobalt alloy, is based on the permanent VenaTech filter and features eight arms and lateral stabilizers. The key difference is that, instead of retrieval, the filter head can be removed via a jugular approach, “unlocking” the filter and converting the configuration into a nonfiltration design that appears similar to a stent when fully converted. The filter can be placed into an IVC measuring up to 32 mm by a jugular or femoral approach.
Fig. 3.

VenaTech Convertible filter (B. Braun, Melsungen, Germany). The cranial hook can be detached converting the filter into a nonfiltering configuration.
Filter Data
The evidence on the efficacy and potential complications of the available retrievable filters is limited. While a few prospective studies exist, most of the published literature is composed of retrospective cohorts or case reports. When describing complications, most publications conform to the SIR Standards of Practice Committee definitions as will this article unless otherwise stated.10 Filter penetration describes a strut or anchoring device extending more than 3 mm outside of the vena cava. Filter embolization is movement of the filter or filter component completely out of the target zone. Filter movement or migration is a change in position of more than 2 cm compared with its deployed position. Filter fracture is any loss of structural integrity. Finally, filter tilt is considered significant when it is more than 15 degrees from the IVC axis.
ALN
Mismetti et al published a prospective study of the ALN filter with a cohort of 220 patients, 148 of who completed 18 months of follow-up (median follow-up 338.5 days).11 Placement was technically successful in 98.6%. The three unsuccessful placements were due to one case of IVC stenosis and two cases of extrinsic IVC compression. Immediate complications were reported in 11.8% of patients, consisting most commonly of filter tilt (5.7%), access site hematoma (4.2%), and filter migration (1.4%). The median dwell time of the filters was 166 days. Of the 217 patients with filters implanted, a recurrent venous thromboembolic event occurred at least once in 17%, with an 18 months cumulative rate of 24.1%. The majority of these patients were either not receiving anticoagulation or were on prophylactic doses of anticoagulation. Fatal PE occurred in 2.3% of patients, and DVT occurred in 15.2%. Filter retrieval was attempted in 25.3% of patients and was 92.7% successful at the first attempt and 100% successful after two attempts. A retrospective study examining early and late retrieval of 123 successfully placed ALN filters described no evidence of penetration or migration of these filters,12 although there was a 5% incidence of significant filter tilt. In this cohort of patients, there were no symptomatic PE that occurred while the filter was in place. Retrieval was successful in 99% of patients, with a mean dwell time of 93 days (46% of filters were retrieved at >2 months). Two of the filters with significant tilt required jugular and femoral access for retrieval; the one unsuccessful retrieval had severe tilt and no option for femoral access. A more recent article demonstrated successful late retrievals of ALN filters.13 This study examined 29 patients in whom the filter had been in place for more than 1 year (mean dwell: 25.6 months, range: 14.8–40.8 months). There was significant tilt present in 6.8% and filter penetration in 3.4%, but there were no cases of migration, fracture, or IVC thrombosis. Retrieval success was 100%, with a combined jugular and femoral approach needed in two cases. While the aforementioned studies all report a similar rate of filter tilt, other complications of fracture and embolization are rare. Filter fracture with leg embolization has been described in a case report of an ALN filter in place for 10 years.14 Another case of filter fracture was also reported in a patient undergoing complex retrieval due to severe pain from multileg penetration.15 This filter had been in place over 2 years and also had an embedded tip. When penetration of ALN filter legs is reported, it is often associated with prolonged dwell times.13 15 16
Denali
A prospective study evaluating the Denali filter was recently published.17 This publication represents an interim report including 200 patients, 160 of who had at least 6 months of follow-up or retrieval of the filter. Filter placement was technically successful in 99.5% of cases. The single technical failure was a filter that was introduced but could not be deployed. Immediate complications included three patients with access site pain without clinical sequelae. Six patients (3%) experienced recurrent PE (one of who also had caval occlusion). New or worsening DVT was reported in 12.8%, and filter penetration occurred in 2.5% of cases. There was no reported filter migration, fracture, embolization, or tilt. Retrieval was attempted in 111 patients with a mean dwell time of 165 days and was technically successful in 97.3%. Of note, 39.8% of retrievals occurred after the filter had been in place more than 6 months. Of the three filters that could not be retrieved, the hook could not be engaged in two, while in the third the hook was engaged but the filter could not be collapsed due to IVC thrombus. There was one case of intimal injury with caval narrowing following retrieval that required no intervention. This study is designed with a 2-year patient follow-up, and these interim results are promising.
Prior Bard retrievable filters, the Recovery and G2, were plagued with reports of filter fracture and embolization.18 19 20 21 22 While there was no incidence of these complications in the aforementioned interim analysis of the Denali filter, there is a published case report of a Denali filter fracture with embolization that resulted in cardiac tamponade.23 Analysis by electron microscopy of this incident demonstrated high-cycle metal fatigue. Longer-term results with the Denali filter are still needed.
Celect
To date, there are no published reports specifically on the Celect Platinum filter. As this has minimal modifications from the Celect filter, data on this filter will be considered. A prospective study on the Celect filter was published in 2009, including 95 patients.24 The study endpoints were 1 year of follow-up, 3 months of follow-up after retrieval, or the decision to leave the filter permanently in place. Placement complications included two cases of deployment difficulties, one with an introducer malfunction and one sheath movement with suboptimal position. Tilt of greater than or equal to 16 degrees at placement occurred in 6.3%. Retrieval was attempted in 58 patients with a mean dwell time of 179 days and 96.6% retrieval success rate. The two unsuccessful cases occurred at 360 and 385 days postinsertion, and were due to tilt in one case and an embedded hook in the other. Kaplan–Meier analysis predicted the probability of retrieval at 100% at 50 weeks and 74% at 55 weeks. Tilt was also reevaluated at filter retrieval compared with placement. There was a lesser degree of tilt reported in 31% of filters and a greater degree of tilt in 17.2%. Filter strut penetration as defined by transmural incorporation was reported in 21 patients. There were no reports of filter perforation, contrast extravasation, or hemorrhage. There was one fatal PE reported but no cases of IVC occlusion, filter fracture, embolization, or migration.
Another report on the Celect filter that same year was a retrospective analysis of 73 patients.25 Successful placement was 100%, with tilt occurring in 6.5%. Mean follow-up for 71 patients was 68 days (range: 1–370 days). There were two cases of confirmed recurrent PE (2.8%) and two patients with symptoms of recurrent DVT. For 17 patients with imaging of the lower extremity veins, 6 had new DVT (35%). For the 47 patients with imaging follow-up, there was no filter migration. Of the 18 patients with computed tomographic (CT) follow-up, filter strut penetration was reported in 7 (39%) and filter fracture in 1 (5.6%). In published studies, the Celect filter has very few reports of filter fracture. Dinglasan et al reported two cases of Celect filter fractures of 148 IVC filters retrieved, while Wang et al reported no cases of filter fracture out of 539 Celect filters with direct follow-up imaging.22 26 Wang et al also reported a filter migration rate of 3.9% for 534 patients with pre- and postprocedural imaging. While fracture and migration are extremely rare, filter strut penetration is commonly reported for the Celect filter. In a retrospective analysis of 265 patients with the Celect filter and follow-up CT imaging, penetration was seen in 39% within 30 days and 80% within 90 days.27 Penetration into an adjacent structure was seen in 13.2% of cases. Another recent study also reported a high rate of Celect strut penetration that increased with filter dwell time.28 This study retrospectively evaluated 91 patients who had at least three follow-up CTs after Celect filter placement. Strut penetration was noted on the initial follow-up CT (mean dwell time: 75 days) in 36% of patients, and on the final CT (mean: 554 days) in 79% of patients. Of the patients with strut penetration noted initially, 66% demonstrated progressive penetration with additional struts. Patients with strut penetration also showed a progressive decrease in IVC cross-section, and a computer model confirmed that decreasing diameter leads to increased force, likely contributing to the progressive penetration.
Another recent retrospective study of 193 Celect filter placements with follow-up CT imaging had a lower incidence of strut penetration (28.5%) that was associated with longer dwell times (>100 days).29 Filter tilt was present in 10.4% of cases, filter thrombus in 1.4%, and there were no reported filter migrations. They reported a recurrent PE rate of 12.7%; however, this was limited to patients who had CT-pulmonary angiography. In this study, retrieval was attempted in 150 cases with 96.7% success. Strut penetration was not associated with recurrent PE or retrieval failure. There was one complication during retrieval with an intraprocedural leg fracture and embolization to the left pulmonary artery requiring snare retrieval.
Günther Tulip
A prospective study of the Günther Tulip filter enrolled and placed filters in 554 patients.30 At placement, filter tilt of greater than or equal to 16 degrees was reported in 4.5% of patients, and there was one case of IVC injury without sequelae. Retrieval was attempted in 275 patients with a success rate of 90.2%. There were three cases of recurrent PE. Following retrieval, there was one case of suspected PE with caval injury and thrombus, and one case of self-resolving caval stenosis. The mean dwell time of those presenting for retrieval was 58.9 days, while the mean dwell time for failed retrievals was 114 days. Failed attempts were attributed to unsatisfactory hook orientation (10), embedded legs (16), and small filter clot burden (1). At retrieval, tilt was reevaluated and nine filters were assessed to have lesser degree of tilt, while only three filters had a greater degree of tilt compared with placement. Kaplan–Meier analysis predicted the probability of retrieval to be 99% at 4 weeks, 94% at 12 weeks, 67% at 26 weeks, and 37% at 52 weeks.
A more recent retrospective study of the Günther Tulip filter examined the outcomes of 369 patients with a mean follow-up of 780 days (range: 1–2,843 days).31 Technical success of placement was 99.5%, with two cases of malposition considered technical failures. Other immediate complications included one patient who experienced an arrhythmia during placement and two access site hematomas. The rate of new or recurrent PE was 3.3% (with two cases of fatal PE), and the rate of new or recurrent DVT was 14.4%. Kaplan–Meier analysis calculated the incidence of new or recurrent PE to be 3% at 1 year, 4.6% at 2 years, and 5.2% for years 3 to 5. Kaplan–Meier analysis for new or recurrent DVT incidence was 11.6% at 1 year, 15.7% at 2 years, and 21.2% at 4 years. IVC thrombus was seen in 4.1%. Filter migration occurred in 12.5% and filter fracture occurred in 0.4%, although all were asymptomatic. There were no reports of filter embolization. Of 122 patients with follow-up CTs, caval penetration was noted in 43.3%. Retrieval was attempted only in 10 patients with a mean dwell time of 66 days; retrieval was successful in 90%.
Option
A prospective study on the Option filter included 100 patients who were followed up for 180 days after placement or 30 days after retrieval.32 Initial placement was 100% technically successful, but only 88% clinically successful. The clinical failures were a combination of 13 events in 12 patients, including an 8% rate of recurrent PE, 3% rate of symptomatic caval thrombosis, and 2% rate of filter migration. Of the eight cases of recurrent PE, only six were confirmed by imaging and four deemed to be filter related. Recurrent DVT occurred in 18% of patients. Retrieval was attempted in 39% of patients and successful in 92.3% of those with a mean dwell time of 67.1 days (range: 1–175 days). Caval irregularity was noted following 16.7% of retrievals, but none required intervention. At the time of retrieval, filter tilt was seen in 7.7%. The Option Elite has minimal modifications from the Option and outcomes presumably would be similar to the earlier published data.
OptEase
A prospective study of the OptEase filter evaluated outcomes in 126 patients at 1 month and 95 patients at 6 months in whom the filter was placed as a permanent device.33 OptEase filter placement occurred in 150 patients, with the only immediate complication being a single case of filter tilt (17 degrees). At 1-month follow-up, symptomatic filter-related DVT was reported in one patient and caudal migration in another. Additionally, there were four new cases of filter tilt and two new cases of filter fracture. At 6-month follow-up, no additional cases of filter-related symptomatic thrombosis or filter migration were reported; however, there were three new cases of filter tilt and one new case of filter fracture. There were no cases of recurrent or new PE in this study. The long-term outcomes of the OptEase filter were evaluated in a retrospective study of 71 patients with a mean follow-up of 20 months (range: 1–78 months).34 Technical success of placement was 98.6% with one malpositioned filter placed upside down. PE was clinically suspected in 11 patients (15.5%); however, 8 of these patients underwent CT-pulmonary angiography and there were no new visible PEs. While clinical symptoms of DVT occurred in 10% of patients, only one patient (1.4%) demonstrated a new DVT on imaging. Symptomatic caval occlusion occurred in one patient. No filter fracture, migration, penetration, or tilt was reported. Retrieval was planned in 24% of patients and successful in 70.6% of those cases (12 of 17 patients). In the cases of failed retrieval, three patients had filter thrombus; one filter was adherent to the caval wall at 12 days and one filter could not be retrieved into the sheath. This final was damaged and dislodged, ultimately requiring surgical removal.
There is a recently published study examining the delayed retrieval outcomes of the OptEase and TrapEase filters.35 This retrospective study examined the retrieval of five OptEase and five TrapEase filters that had greater than 60 days of dwell time. The average dwell for the OptEase patients was 977 days (range: 123–2,584 days), and the average dwell for the TrapEase patients was 1,273 days (range: 129–3,582 days). Retrieval was technically successful in 100%. All patients had caval stenosis following retrieval, with two patients undergoing angioplasty and one with stent placement. There was a single case of an IVC pseudoaneurysm that resolved, one case of a fractured filter strut left embedded in the caval wall, and two patients with multiple barbs left embedded. Another study evaluated retrieval of just the OptEase filter.36 Of 811 OptEase filters placed, 164 patients were referred for retrieval. Retrieval was deferred in 25 patients due to large (>1 cm) thrombus present in the filter. The remaining 139 patients were evaluated as two groups: retrieval attempted before 2007 (60 patients, Group A) and retrieval attempted from January 2007 onward (79 patients, Group B). Overall retrieval success was 92% (95% for Group A, 90% for Group B). The mean dwell time was statistically longer for group B (31.0 ± 29.8 days vs. 17.7 ± 9.2 days). Of the 11 retrieval failures, four were due to an inability to engage the hook (three for Group A, one for Group B) and seven were due to an inability to sheath the filter (all Group B). Retrieval failures had a mean dwell time of 16 days for Group A and 54 days for Group B. The OptEase filter's “Instructions for Use” recommends retrieval within 12 days. While this study indicates that retrieval is possible at longer dwell times, retrieval of the OptEase filter is likely more difficult with longer dwell times compared with conical filters due to the six vertical struts contacting the caval wall and potentially being incorporated by the intima.
Crux
A prospective study of the Crux filter followed up 125 patients for 180 days after placement or 30 days after retrieval.37 Placement was technically successful in 98.4%. There was a single case in which the cranial loop was placed too high, and a single case in which the device moved caudally when the delivery sheath was retracted. Both of these filters were successfully retrieved. Clinical success occurred in 96% of all patients. This was decreased to 95.1% when patients who did not complete the study were excluded, and further decreased to 94.4% of patients when suspected but unproven PE were included. The recurrent PE rate was 2.4% for patients with proven PE, and 4% for patients with suspected or proven PE. Nonocclusive thrombus was seen in or near the filter in 7.2% of patients. There was a recurrent DVT rate of 10.4%; however, there were no reported filter migrations, embolizations, fractures, or tilt. Retrieval was attempted in 54 of 123 patients (43.9%) at a mean of 84.6 days (range: 6–190 days, and was successful in 98.1% of cases. The single failed retrieval occurred at a dwell time of 167 days. There was a single self-limited IVC pseudoaneurysm reported.
VenaTech Convertible Filter
The VenaTech Convertible filter was investigated in a multicenter clinical trial in the United States (ClinicalTrials.gov NCT01112917).38 The primary endpoint of the study assessed the technical success of filter conversion without the loss of filter head components or incomplete opening of the filter legs. Patients were followed up for 6 months to evaluate them for any adverse events. The filter has been approved for clinical use by the FDA, and publication of the clinical trial results is anticipated.
There is a published preclinical trial of the VenaTech Convertible filter evaluating filter conversion in 49 Pre-Alp sheep.39 Conversion of the filter was attempted immediately following placement (19 filters), or after 1, 3, or 6 months (20 filters). Immediate conversion was 100% successful. Of the delayed conversions, the filter head was unlocked easily in 19 of 20. In 12 cases, the filter opening required the use of a 9-mm balloon to completely juxtapose the filter against the IVC. On gross anatomic examination, the filter stabilizers were completely incorporated into the caval wall within 4 weeks. There were no cases of filter thrombosis, migration, or tilting.
Comparative Studies
There are few studies directly comparing filters to one another. A recent retrospective study examined 225 Celect, 160 Günther Tulip, and 50 Greenfield filters in patients with follow-up CT imaging.40 The mean dwell time for the Celect and Tulip filters were 277 and 437 days, respectively. Penetration of one or more legs was seen with 49% of Celect filters and 43% of Tulip filters, with strut penetration more likely in filters with more than 90 days of dwell time. Progression of leg penetration was seen in 38.8% of Celect filters and 20.5% of Tulip filters. There were two cases of Celect filter fracture seen at 324 and 566 days and one case of Tulip fracture at 781 days. A separate retrospective study comparing the rates of strut penetration with the Günther Tulip filter and the Option filter examined CT follow-up of 37 Tulip filters and 21 Option filters.41 There was strut penetration in 22% of Tulip filters and 10% of Option filters, although this difference was not statistically significant. Günther Tulip filters, however, demonstrated an increased likelihood of leg penetration with increased dwell time, while Option filter penetration did not appear time dependent. Another retrospective study examined 99 Celect and 86 Option filters.42 Tilting that abutted caval wall was reported in 8.9% of Celect filters and 16.7% of Option filters, although the difference was not statistically significant. Perforation was significantly increased in Celect filters (43%) when compared with Option filters (0%). Retrieval of the Celect filters was attempted in 59% of patients with a mean dwell time of 2.1 months, demonstrated a 3.4% failure rate, and required advanced techniques in 5.4%. Retrieval of the Option filters was attempted in 76% of patients with a mean dwell time of 1.94 months, had a 7.7% failure rate, and required advanced techniques in 18.3% of cases. Despite increased strut penetration with the Celect filter, retrieval of the Option filter required increased use of adjunct retrieval techniques and increased fluoroscopy time.
Future Directions
As vena cava filters continue to be placed in large numbers, research into alternative filter designs continues to advance. The Angel Catheter (BiO2 Medical, San Antonio, TX) is a new temporary filter and central venous catheter combination available in Europe (Fig. 4). This is a triple lumen central venous catheter with a tethered, temporary IVC filter made of nickel–titanium alloy. The filter has a self-centering design without barbs or hooks. It is placed by a femoral approach, and is designed for placement at bedside without fluoroscopic guidance. This device can be placed in an IVC measuring 15 to 30 mm in diameter, but should be removed within 30 days. For removal, the filter is collapsed into the 9F catheter and the catheter and filter are removed as a unit. Outcomes of the Angel Catheter were initially reported from a pilot study of eight patients.43 The combined filter and central venous catheters were all placed at the bedside without the use of fluoroscopy. There was a mean dwell time of 4 days and patients were followed up for 30 days following placement. There was no reported DVT or PE, catheter-related thrombosis, major bleeding, or catheter-related bloodstream infection. A pre-retrieval cavogram was performed in six of the eight patients (one device was removed inadvertently at the bedside and one patient had a contrast allergy). Of the six cavograms performed prior to device removal, one demonstrated a 5-cm trapped thrombus; this patient underwent placement of a conventional retrievable filter as thrombolytics were contraindicated. A more recent publication assessed the outcomes of 60 patients at eight centers who underwent placement of the Angel Catheter.44 Average follow-up was 17 days and average dwell time was 6 days. Bedside placement occurred in 90% of patients, with correct placement confirmed by radiograph. The device could not be visualized in one patient and was subsequently removed. In these patients, there was one PE diagnosed 1 day after filter-catheter placement that was not clinically relevant and may have been present prior to device placement. There were no catheter-related bloodstream infections or access site infections. Migration of the filter occurred in two patients; however, the filter remained attached in all instances. Pre-retrieval imaging was performed in 73% of cases . The device was inadvertently removed in 7%, and 10% of patients died with the device in place. Of those with imaging, 5% had clots greater than 2 cm in size. One patient in this cohort underwent thrombolysis, while the other had a conventional retrievable filter placed. There were no reported complications with removal of the device.
Fig. 4.
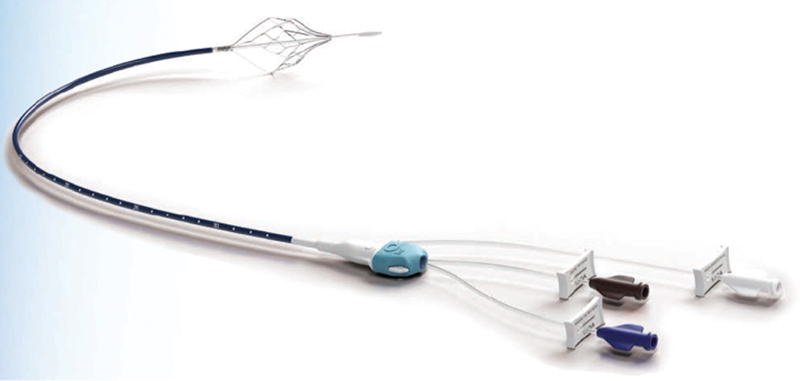
Angel Catheter (BiO2 Medical, San Antonio, TX). A temporary filter and central venous catheter combination available in Europe.
In a similar concept to the VenaTech Convertible vena cava filter, Novate Medical (Galway, Ireland) has developed a convertible vena cava filter, the Sentry (Fig. 5). However, in great distinction to the VenaTech Convertible filter, the Sentry vena cava filter is bioconvertible. The Sentry does not require an additional procedure to convert into a nonfiltering configuration, but converts spontaneously at a minimum of 60 days. A prospective, multicenter clinical trial is currently underway (ClinicalTrials.gov NCT01975090). This trial will evaluate the technical success in deployment, freedom from symptomatic PE, and freedom from IVC filter-related complications as a composite primary endpoint. Patients will be followed up for 12 months.
Fig. 5.
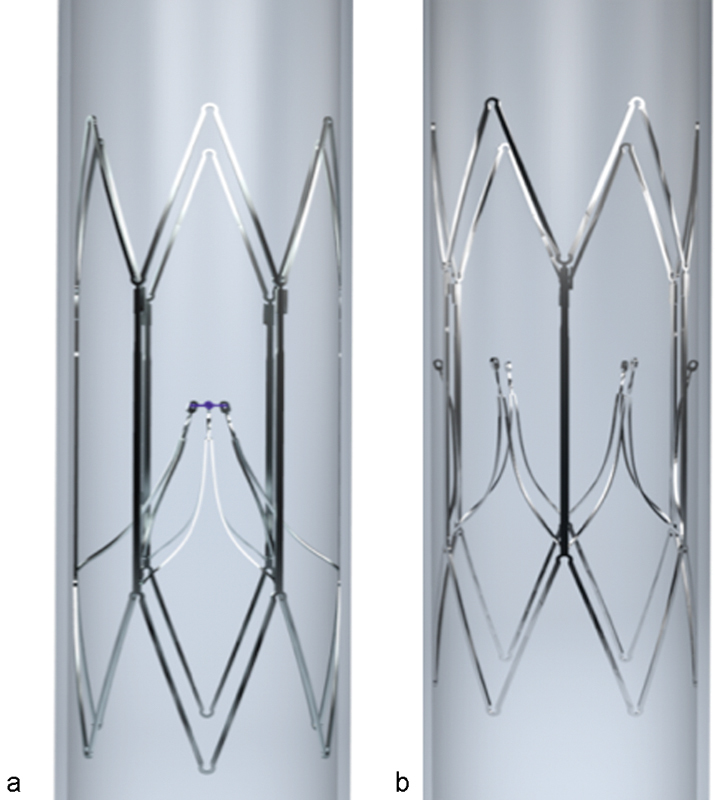
Sentry filter (Novate Medical, Galway, Ireland). A bioconvertible filter that converts to a nonfiltering configuration at a minimum of 60 days. (a) Filtration configuration; (b) Nonfiltration configuration.
A step further than the Sentry bioconvertible filter is research into creating a completely absorbable vena cava filter.45 46 While research is still in the early stages, a recent study examined the effectiveness of infusing an absorbable IVC filter with iodine-based contrast agents to produce a more radiopaque device.47 This increased the radiopacity of an absorbable IVC filter, so it was visible on micro-CT imaging. Increased visualization permits potentially improved deployment and monitoring of this developing technology.
There are also attempts to design a drug-eluting vena cava filter.48 In this study, the Aegisy filter (Lifetech Scientific Corporation, Shenzhen, China) was coated with rapamycin and heparin in an attempt to inhibit intimal hyperplasia and thrombus formation. Filters with and without drug coating were placed in 12 adult sheep. More than half of the heparin was released at day 1, while the rapamycin elution occurred little in the first few days and then increased at 20 to 30 days. Filter thrombus was the same in experimental and control groups and the effect of the heparin was not satisfactory. Filters were retrieved at 10, 20, or 30 days, either by laparotomy or endovascular means. Filters without drug coating were successfully retrieved endovascularly only at the day 10 endpoint, while the drug-eluting filters were retrieved at the day 10 and 20 endpoints. No filters were successfully retrieved at day 30 by endovascular techniques. On gross examination, intimal hyperplasia was decreased in the drug-eluting group at day 20 but was similar to the control group at day 30. On gross examination, the experimental filters also demonstrated increased adhesion between the IVC and adjacent tissues compared with control filters.
Conclusion
The ideal filter design remains elusive. The understanding of near and long-term filter performance continues to evolve, and the clinical milieu remains in flux. Each of the current designs has strengths and weaknesses, and as a result individual operator preference remains a powerful factor in device selection. Regardless of which device one chooses to place, what is known is that careful patient selection and follow-up are essential in the management of patients with vena cava filters.
References
- 1.Kaufman J A, Kinney T B, Streiff M B. et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol. 2006;17(3):449–459. doi: 10.1097/01.rvi.0000203418-39769.0d. [DOI] [PubMed] [Google Scholar]
- 2.Decousus H, Leizorovicz A, Parent F. et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338(7):409–415. doi: 10.1056/NEJM199802123380701. [DOI] [PubMed] [Google Scholar]
- 3.Group P S; PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study Circulation 20051123416–422. [DOI] [PubMed] [Google Scholar]
- 4.Duszak R Jr, Parker L, Levin D C, Rao V M. Placement and removal of inferior vena cava filters: national trends in the Medicare population. J Am Coll Radiol. 2011;8(7):483–489. doi: 10.1016/j.jacr.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 5.Stein P D, Kayali F, Olson R E. Twenty-one-year trends in the use of inferior vena cava filters. Arch Intern Med. 2004;164(14):1541–1545. doi: 10.1001/archinte.164.14.1541. [DOI] [PubMed] [Google Scholar]
- 6.Angel L F, Tapson V, Galgon R E, Restrepo M I, Kaufman J. Systematic review of the use of retrievable inferior vena cava filters. J Vasc Interv Radiol. 2011;22(11):1522–1.53E6. doi: 10.1016/j.jvir.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 7.Wang S L, Lloyd A J. Clinical review: inferior vena cava filters in the age of patient-centered outcomes. Ann Med. 2013;45(7):474–481. doi: 10.3109/07853890.2013.832951. [DOI] [PubMed] [Google Scholar]
- 8.Hammond C J, Bakshi D R, Currie R J. et al. Audit of the use of IVC filters in the UK: experience from three centres over 12 years. Clin Radiol. 2009;64(5):502–510. doi: 10.1016/j.crad.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Kaufman J A. Retrievable vena cava filters. Tech Vasc Interv Radiol. 2004;7(2):96–104. doi: 10.1053/j.tvir.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Caplin D M Nikolic B Kalva S P Ganguli S Saad W E Zuckerman D A; Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism J Vasc Interv Radiol 201122111499–1506. [DOI] [PubMed] [Google Scholar]
- 11.Mismetti P, Rivron-Guillot K, Quenet S. et al. A prospective long-term study of 220 patients with a retrievable vena cava filter for secondary prevention of venous thromboembolism. Chest. 2007;131(1):223–229. doi: 10.1378/chest.06-0631. [DOI] [PubMed] [Google Scholar]
- 12.Pellerin O, Barral F G, Lions C, Novelli L, Beregi J P, Sapoval M. Early and late retrieval of the ALN removable vena cava filter: results from a multicenter study. Cardiovasc Intervent Radiol. 2008;31(5):889–896. doi: 10.1007/s00270-008-9357-x. [DOI] [PubMed] [Google Scholar]
- 13.Pellerin O, di Primio M, Sanchez O, Meyer G, Sapoval M. Successful retrieval of 29 ALN inferior vena cava filters at a mean of 25.6 months after placement. J Vasc Interv Radiol. 2013;24(2):284–288. doi: 10.1016/j.jvir.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 14.Pontone G, Andreini D, Bertella E, Annoni A D, Pepi M, Montorsi P. Asymptomatic struts fracture and multiple embolization as a late complication of ALN removable vena cava filter implantation. Eur Heart J. 2013;34(30):2353. doi: 10.1093/eurheartj/ehs412. [DOI] [PubMed] [Google Scholar]
- 15.Kuo W T Robertson S W Odegaard J I Hofmann L V Complex retrieval of fractured, embedded, and penetrating inferior vena cava filters: a prospective study with histologic and electron microscopic analysis J Vasc Interv Radiol 2013245622–6300., quiz 631 [DOI] [PubMed] [Google Scholar]
- 16.Venturini M, Civilini E, Orsi M. et al. Successful endovascular retrieval of an ALN inferior vena cava filter causing asymptomatic aortic dissection, perforation of the cava wall and duodenum. J Vasc Interv Radiol. 2015;26(4):608–611. doi: 10.1016/j.jvir.2014.12.021. [DOI] [PubMed] [Google Scholar]
- 17.Stavropoulos S W Sing R F Elmasri F et al. The DENALI Trial: an interim analysis of a prospective, multicenter study of the Denali retrievable inferior vena cava filter J Vasc Interv Radiol 201425101497–1505., 1505.e1 [DOI] [PubMed] [Google Scholar]
- 18.Nicholson W, Nicholson W J, Tolerico P. et al. Prevalence of fracture and fragment embolization of Bard retrievable vena cava filters and clinical implications including cardiac perforation and tamponade. Arch Intern Med. 2010;170(20):1827–1831. doi: 10.1001/archinternmed.2010.316. [DOI] [PubMed] [Google Scholar]
- 19.Tam M D, Spain J, Lieber M, Geisinger M, Sands M J, Wang W. Fracture and distant migration of the Bard Recovery filter: a retrospective review of 363 implantations for potentially life-threatening complications. J Vasc Interv Radiol. 2012;23(2):199–2050. doi: 10.1016/j.jvir.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 20.Hull J E, Robertson S W. Bard Recovery filter: evaluation and management of vena cava limb perforation, fracture, and migration. J Vasc Interv Radiol. 2009;20(1):52–60. doi: 10.1016/j.jvir.2008.09.032. [DOI] [PubMed] [Google Scholar]
- 21.Vijay K, Hughes J A, Burdette A S. et al. Fractured Bard Recovery, G2, and G2 express inferior vena cava filters: incidence, clinical consequences, and outcomes of removal attempts. J Vasc Interv Radiol. 2012;23(2):188–194. doi: 10.1016/j.jvir.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Dinglasan L A, Trerotola S O, Shlansky-Goldberg R D, Mondschein J, Stavropoulos S W. Removal of fractured inferior vena cava filters: feasibility and outcomes. J Vasc Interv Radiol. 2012;23(2):181–187. doi: 10.1016/j.jvir.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 23.Kuo W T, Robertson S W. Bard Denali inferior vena cava filter fracture and embolization resulting in cardiac tamponade: a device failure analysis. J Vasc Interv Radiol. 2015;26(1):111–50. doi: 10.1016/j.jvir.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Lyon S M, Riojas G E, Uberoi R. et al. Short- and long-term retrievability of the Celect vena cava filter: results from a multi-institutional registry. J Vasc Interv Radiol. 2009;20(11):1441–1448. doi: 10.1016/j.jvir.2009.07.038. [DOI] [PubMed] [Google Scholar]
- 25.Sangwaiya M J, Marentis T C, Walker T G, Stecker M, Wicky S T, Kalva S P. Safety and effectiveness of the Celect inferior vena cava filter: preliminary results. J Vasc Interv Radiol. 2009;20(9):1188–1192. doi: 10.1016/j.jvir.2009.05.033. [DOI] [PubMed] [Google Scholar]
- 26.Wang W, Zhou D, Obuchowski N, Spain J, An T, Moon E. Fracture and migration of Celect inferior vena cava filters: a retrospective review of 741 consecutive implantations. J Vasc Interv Radiol. 2013;24(11):1719–1722. doi: 10.1016/j.jvir.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 27.Zhou D, Moon E, Bullen J, Sands M, Levitin A, Wang W. Penetration of Celect inferior vena cava filters: retrospective review of CT scans in 265 patients. AJR Am J Roentgenol. 2014;202(3):643–647. doi: 10.2214/AJR.13.11097. [DOI] [PubMed] [Google Scholar]
- 28.Dowell J D, Castle J C, Schickel M. et al. Celect inferior vena cava wall strut perforation begets additional strut perforation. J Vasc Interv Radiol. 2015;26(10):1510–1.518E6. doi: 10.1016/j.jvir.2015.06.020. [DOI] [PubMed] [Google Scholar]
- 29.Bos A, Van Ha T, van Beek D. et al. Strut penetration: local complications, breakthrough pulmonary embolism, and retrieval failure in patients with Celect vena cava filters. J Vasc Interv Radiol. 2015;26(1):101–106. doi: 10.1016/j.jvir.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 30.Smouse H B Rosenthal D Thuong V H et al. Long-term retrieval success rate profile for the Günther Tulip vena cava filter J Vasc Interv Radiol 2009207871–877., quiz 878 [DOI] [PubMed] [Google Scholar]
- 31.Hoffer E K, Mueller R J, Luciano M R, Lee N N, Michaels A T, Gemery J M. Safety and efficacy of the Gunther Tulip retrievable vena cava filter: midterm outcomes. Cardiovasc Intervent Radiol. 2013;36(4):998–1005. doi: 10.1007/s00270-012-0517-7. [DOI] [PubMed] [Google Scholar]
- 32.Johnson M S, Nemcek A A Jr, Benenati J F. et al. The safety and effectiveness of the retrievable option inferior vena cava filter: a United States prospective multicenter clinical study. J Vasc Interv Radiol. 2010;21(8):1173–1184. doi: 10.1016/j.jvir.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Ziegler J W, Dietrich G J, Cohen S A, Sterling K, Duncan J, Samotowka M. PROOF trial: protection from pulmonary embolism with the OptEase filter. J Vasc Interv Radiol. 2008;19(8):1165–1170. doi: 10.1016/j.jvir.2008.04.020. [DOI] [PubMed] [Google Scholar]
- 34.Kalva S P, Marentis T C, Yeddula K, Somarouthu B, Wicky S, Stecker M S. Long-term safety and effectiveness of the “OptEase” vena cava filter. Cardiovasc Intervent Radiol. 2011;34(2):331–337. doi: 10.1007/s00270-011-0216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scher D, Venbrux A, Okapal K. et al. Retrieval of TRAPEASE and OPTEASE inferior vena cava filters with extended dwell times. J Vasc Interv Radiol. 2015;26(10):1519–1525. doi: 10.1016/j.jvir.2015.06.021. [DOI] [PubMed] [Google Scholar]
- 36.Rimon U, Bensaid P, Golan G. et al. Optease vena cava filter optimal indwelling time and retrievability. Cardiovasc Intervent Radiol. 2011;34(3):532–535. doi: 10.1007/s00270-010-9920-0. [DOI] [PubMed] [Google Scholar]
- 37.Smouse H B Mendes R Bosiers M Van Ha T G Crabtree T; RETRIEVE Investigators. The RETRIEVE trial: safety and effectiveness of the retrievable crux vena cava filter J Vasc Interv Radiol 2013245609–621. [DOI] [PubMed] [Google Scholar]
- 38.Hohenwalter E J, Stone J, O'Moore P. et al. Multicenter trial of the VenaTech convertible filter: a novel approach to IVC filtration. J Vasc Interv Radiol. 2015;26:S5–S6. doi: 10.1016/j.jvir.2017.06.032. [DOI] [PubMed] [Google Scholar]
- 39.Le Blanche A F, Ricco J B, Bonneau M, Reynaud P. The optional VenaTech(™) Convertible (™) vena cava filter: experimental study in sheep. Cardiovasc Intervent Radiol. 2012;35(5):1181–1187. doi: 10.1007/s00270-011-0273-0. [DOI] [PubMed] [Google Scholar]
- 40.McLoney E D, Krishnasamy V P, Castle J C, Yang X, Guy G. Complications of Celect, Günther tulip, and Greenfield inferior vena cava filters on CT follow-up: a single-institution experience. J Vasc Interv Radiol. 2013;24(11):1723–1729. doi: 10.1016/j.jvir.2013.07.023. [DOI] [PubMed] [Google Scholar]
- 41.Olorunsola O G, Kohi M P, Fidelman N. et al. Caval penetration by retrievable inferior vena cava filters: a retrospective comparison of Option and Günther Tulip filters. J Vasc Interv Radiol. 2013;24(4):566–571. doi: 10.1016/j.jvir.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 42.Ryu R K, Desai K, Karp J. et al. A comparison of retrievability: Celect versus Option filter. J Vasc Interv Radiol. 2015;26(6):865–869. doi: 10.1016/j.jvir.2015.01.022. [DOI] [PubMed] [Google Scholar]
- 43.Cadavid C A, Gil B, Restrepo A. et al. Pilot study evaluating the safety of a combined central venous catheter and inferior vena cava filter in critically ill patients at high risk of pulmonary embolism. J Vasc Interv Radiol. 2013;24(4):581–585. doi: 10.1016/j.jvir.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 44.Taccone F S, Bunker N, Waldmann C. et al. A new device for the prevention of pulmonary embolism in critically ill patients: Results of the European Angel Catheter Registry. J Trauma Acute Care Surg. 2015;79(3):456–462. doi: 10.1097/TA.0000000000000756. [DOI] [PubMed] [Google Scholar]
- 45.Eggers M D, Reitman C A. In vitro analysis of polymer candidates for the development of absorbable vascular filters. J Vasc Interv Radiol. 2012;23(8):1023–1030. doi: 10.1016/j.jvir.2012.05.039. [DOI] [PubMed] [Google Scholar]
- 46.Thors A, Muck P. Resorbable inferior vena cava filters: trial in an in-vivo porcine model. J Vasc Interv Radiol. 2011;22(3):330–335. doi: 10.1016/j.jvir.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 47.Singhana B, Chen A, Slattery P. et al. Infusion of iodine-based contrast agents into poly(p-dioxanone) as a radiopaque resorbable IVC filter. J Mater Sci Mater Med. 2015;26(3):124. doi: 10.1007/s10856-015-5460-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhao H, Zhang F, Liang G. et al. Preparation and experimental research into retrievable rapamycin- and heparin-coated vena cava filters: a pilot study. J Thromb Thrombolysis. 2015 doi: 10.1007/s11239-015-1278-3. [DOI] [PubMed] [Google Scholar]


