Abstract
BACKGROUND
Among people who inject drugs (PWID) in the U.S., those who initiated drug injection in Puerto Rico (immigrant Puerto Rican PWID) engage in more injection and sexual risk behaviors, and have higher HIV incidence than non-Hispanic whites.
OBJECTIVE
Understand the persistence of HIV risk behaviors.
METHODS
In a cross-sectional study conducted in New York City (NYC) in 2012 (National HIV Behavioral Surveillance), PWID aged ≥ 18 years were recruited using Respondent-Driven Sampling, interviewed, and tested for HIV. Participants were categorized into 5 different groups: (1) US-born non-Hispanic PWID, (2) US-born Puerto Rican PWID, (3) recent immigrant Puerto Rican PWID (≤ 3 years in NYC), (4) medium-term immigrant Puerto Rican PWID (> 3 and ≤ 10 years in NYC), and (5) long-term immigrant Puerto Rican PWID (> 10 years in NYC). We examined the relationship between time since migrating on sexual and injection risk behaviors among immigrant Puerto Rican PWID, compared with U.S.-born Puerto Rican PWID and US-born non-Hispanic PWID. Adjusted odds ratios (aOR) and 95% confidence intervals (95% CI) were estimated using logistic regression.
RESULTS
A total of 481 PWID were recruited. In adjusted analyses using US-born non-Hispanic PWID as the comparison group, syringe sharing was significantly more likely among medium-term immigrants; and unprotected sex with casual partners was more likely among recent and long-term immigrants.
CONCLUSIONS
The risk-acculturation process for immigrant Puerto Rican PWID may be non-linear and may not necessarily lead to risk reduction over time. Research is needed to better understand this process.
Keywords: Puerto Rican, immigrants, HIV, syringe sharing, acculturation, enculturation
1.1 Introduction
Researchers consistently use the acculturation hypothesis to study immigrant health in the United States (US). This hypothesis contends that as immigrants spend more time in the US, they embrace mainstream behaviors (i.e., English language proficiency, diets, alcohol and illicit drug use, etc.) that ultimately render negative health outcomes such as diabetes, obesity, and HIV (Afable-Munsuz et al., 2014; Alegria et al., 2007; Borges et al., 2007; Borges et al., 2011; Broesch and Hadley, 2012; Garcia and Gonzalez, 2009; Lee et al., 2013; Robertson et al., 2012; Robertson et al., 2012a; Strathdee et al., 2008; Strathdee and Magis-Rodriguez, 2008a).
Studies show that an immigrant’s generational “bracket” and “length of time” since immigration are markers of negative health outcomes. For first generation immigrants, negative health outcomes can become apparent after only one year after immigration (Lee et al., 2013). These negative health outcomes are known as “the paradox of acculturation” (Abraido-Lanza et al. 2005; Dow, 2011; Rumbaut, 1997), where some behaviors retained post-migration among new immigrants are health-protective (i.e., no illicit drug use, healthier diets) but are lost over time (Breslau et al., 2007). While acculturation may help immigrants improve access better employment opportunities and higher educational attainment, it also generates disease vulnerability (Robertson et al., 2012; Robertson et al., 2012a; Strathdee et al., 2008; Strathdee and Magis-Rodriguez, 2008a).
Increasingly, acculturation is portrayed as complex process in which immigrants may or may not adopt American norms and lifestyles (Acevedo-Garcia et al., 2012; Alegria, 2009; Broesch and Hadley, 2012; Cortés et al., 2003; Lopez-Class et al., 2011; Thomson and Hoffman-Goetz, 2009). These scholars note that immigrants are not passive recipients of culture, and that “enculturation,” defined as the process where immigrants perpetuate elements of their native culture amidst the host’s culture (Alegria, 2009), escape analyses based on variables like language and length of time in the US. However, because of the large-scale nature of many immigrant health studies, including the present study, acculturation measures often revolve around these proxy variables.
Puerto Rican people who inject drugs (PWID) in Puerto Rico (P.R.) and their immigrant counterparts in the Northeast have also been a population of concern (Deren et al., 2007; Deren et al. 2007a; Deren et al., 2005; Kang et al., 2009; López et al., 2008; Zerden et al., 2010). Researchers consistently point to the scarcity of syringe exchange, HIV counseling and testing, and drug treatment in P.R. as important contextual variables behind the very high HIV and Hepatitis C (HCV) risk behaviors among Puerto Rican PWID natives (Deren et al., 2007; Deren et al., 2007a; Deren et al., 2005; Finlinson et al., 2002; Kang et al., 2009), and a recent study noted the disparity in HIV/HCV prevention service availability between P.R. and the Northeastern U.S. persists (Deren et al., 2014; Deren et al., 2014a, in press; López et al., 2014, in press). In Puerto Rico, injection drug use is responsible for nearly half of accumulated AIDS cases and almost 26% of HIV cases diagnosed between 2005–2011. Whereas in 2010 PWID accounted for 8.6% of new HIV infections across the U.S. the proportion in Puerto Rico was over two times greater (20.4%) (Department of Health of Puerto Rico 2012). Furthermore, HCV prevalence is estimated to be as high as 90% (Reyes et al., 2006; Perez et al., 2015). It has been argued that the context of a dearth of HIV/HCV prevention services in P.R. translates into the cultural normalization of risk among native PWID, and these culturally-informed risk behaviors persist among those who immigrate to other geographies (e.g. the Northeastern U.S.) with ampler service availability (Deren et al., 2007; López et al., 2008; Zerden et al., 2010).
These risk norms, along with pronounced language barriers and a cultural perception of people from “the island” as different, distance these immigrants both from their non-immigrant Puerto Rican counterparts, and from non-Hispanic white and black PWID in NYC (Cortés et al., 2003; Gelpí-Acosta et al., 2011; Kang et al., 2009). These differing patterns of risk behaviors and language/culture call for using the lens of acculturation theory, especially when studies suggest that adopting NYC-specific norms may be “HIV-protective” (Kang et al., 2009) for immigrant Puerto Rican PWID. Still, contrary to other immigrant groups’ health outcomes, immigrant Puerto Rican PWID’s health may benefit from “risk-acculturation,” defined as adopting the less risky NYC-specific sexual and injection norms while abandoning imported (risky) norms. While there is evidence of the presence of risk-acculturation (Kang et al., 2009), we do not understand how rapidly this occurs, because comparison groups in previous studies included immigrants with a wide range of time since immigration.
As new waves of immigrant Puerto Rican PWID arrive to the Northeast, the relationship between length of time in the mainland U.S. and risk norms/behaviors remains unclear. This knowledge void is particularly troubling because in NYC in 2012, Hispanics represented 45% of PWID who were newly HIV-infected, and 39% of these were immigrant Puerto Rican PWID. (Deren et al. 2014a) Because immigrant Puerto Rican PWID consistently differ from U.S.-born PWID in risk behaviors and because of their disease vulnerability (CDC, 2014), placing this immigrant group within the broader immigrant health and acculturation discussion may help delineate improved strategies to address their HIV vulnerabilities.
Using “language” and “length of time” as proxy variables, we examine the relationship between time since immigration and HIV risk behaviors using an “immigration recency scale,” and categorizing Puerto Rican PWID by place of birth and years since immigration. We seek to elucidate more precise knowledge on the duration of risk behaviors to understand HIV transmission risks in this population. We hypothesize that length of time and English proficiency are positively associated with risk-acculturation. However, adding to the analysis of these two proxy variables, we further interpret and contextualize our findings using secondary data that provide an in-depth look into the cultural variables behind risk endurance after migration in this population.
1.2 Methods
1.2.1 Sampling
Data were collected in New York City as a part of the third round of the U.S. Centers for Disease Control and Prevention (CDC)-sponsored National HIV Behavioral Surveillance (NHBS) study of PWID in 2012. NHBS is a cross-sectional study that investigates sexual and drug use-related risk behaviors, and HIV and HCV prevalence, among populations at elevated risk for HIV in 20 major cities of the United States (Lansky et al., 2007). The CDC conducts the NHBS in collaboration with local health departments, universities, and other institutions.
1.2.2 Procedures
We used Respondent-Driven Sampling (RDS) to recruit people who inject drugs (PWID) in NYC (Heckathorn, 2007). RDS requires recruitment by members of the target population who are socially linked. Ethnographers recruited a small group of initial participants (“seeds”) who, after completing the study, each referred up to three other PWID to take part in the study. Seeds were recruited directly from syringe exchange programs (SEPs) in Jamaica, Queens; Bushwick and East New York, Brooklyn; Mott Haven, the Bronx; and the Lower East Side, Manhattan. They were selected to represent the diverse PWID populations in NYC, with factors such as age, race/ethnicity, drug preference, and geography considered. Seed referrals completed the study and were each provided with three coupons to give to PWID peers, who could then be referred to the study. Successive recruitment waves took place until the target sample size was reached. Eligibility criteria included age 18 or older, proficiency in English or Spanish, having injected illicit drugs at least once in the past 12 months, and residing in the NYC metropolitan area.
In the study’s research offices (Bronx, Brooklyn, and Manhattan), trained bilingual interviewers privately administered a structured questionnaire with each recruit. Survey topics included sociodemographics, drug use and sexual behaviors, HIV, and HCV and hepatitis B (HBV) testing experiences. In addition, phlebotomists collected blood specimens using venipuncture. Specimens were tested for HIV antibody on HIV1/2 enzyme-linked immunosorbent assay (ELISA) and confirmed using HIV1 western blot platforms (Bio-Rad Laboratories, Hercules, CA). HCV infection was determined using chemiluminescence immunoassay (CIA) (VITROS Anti-HCV assay, Ortho-Clinical Diagnostics, Raritan, NJ, USA). Hepatitis B infection was determined based on the results of anti-HBs, anti-HBc, and HbsAg tests (VITROS Eci, Ortho-Clinical Diagnostics, Raritan, NJ, USA).
Individuals were paid incentives for completing the questionnaire ($20), HIV ($10), and HCV/HBV ($10) testing, and peer recruitment (up to 3 eligible recruits, $10 each). All study procedures were approved by the Institutional Review Boards of the participating organizations. After the interview, recruitment methods were explained to them, all participants provided written informed consent to participate.
1.2.3 Variables and analyses
Participants were categorized into 5 different groups: (1) U.S.-born non-Hispanic PWID, (2) U.S.-born Puerto Rican PWID, (3) recent immigrant Puerto Rican PWID (3 or fewer years in NYC), (4) medium-term immigrant Puerto Rican PWID (more than 3 years, up to 10 years in NYC), and (5) long-term immigrant Puerto Rican PWID (more than 10 years in NYC). These time periods were selected to maximize power. Using more time periods would have made the groups too small for multivariable analysis, and we wanted to use more than two to test whether the relationships between time in NYC and risk behaviors were monotonic. U.S.-born non-Hispanic PWID were used as a comparison group whose risk behaviors should reflect behavioral norms in NYC, without the influence of immigration or risk-acculturation. Their inclusion makes little difference for the regression results, but including them provides greater context for interpretation. While U.S.-born Puerto Rican PWID may also reflect the behavioral norms in NYC, separating them from U.S.-born non-Hispanic PWID helps identify differences in service needs between these two otherwise culturally distinct populations and to target resources in NYC. Non-Puerto Rican immigrants were excluded from the analysis (N=14) as well as other U.S.-born non-Puerto Rican Hispanics (N=18) because their numbers were too small for analysis. Puerto Rican immigrants who initiated injection drug use in NYC (N=12) were also excluded. Because their injection risk behaviors are post-migration, their risk behaviors are not imported behaviors subject to acculturation.
The first layer of data analysis examined differences in language (whether English or Spanish was used during survey administration), sociodemographics, sexual and injection-related risks, and disease outcomes between these groups. We also investigated two main outcome measures: 1) unprotected sex with a casual partner or partners, and 2) receptive syringe sharing, in each case during the 12 months prior to survey administration. The first is defined as having engaged in anal or vaginal sex without a condom with one or more casual partners, defined as someone to whom the participant did not feel committed to or did not know well, including both heterosexual and men-with-men unprotected sex. The second is defined as having injected drugs with a syringe already used by another injector to inject drugs. These variables were selected because of their relevance to HIV transmission, and to be consistent with previous research in this population. Also, four main sociodemographic covariates were: 1) poverty (past 12-month income below $10,000), 2) past 12-month homelessness; 3) current homelessness; and 4) past 12-month incarceration. Bivariate statistical comparisons were made using chi-square tests.
We then developed multivariable logistic regression models to evaluate the association between the immigration recency and the two behavioral risk outcomes. To represent the main comparisons of interest, we created a 5-group categorical variable with recent, medium-term, and long-term immigrant, U.S.-born Puerto Rican PWID, and U.S.-born non-Hispanic PWID as the reference group. Based on previous research, young age (defined as anyone below 30 years of age), non-injection crack use and past 12-month incarceration were identified as potential confounding factors. We tested the relationships between the two risk outcomes and the migration categories, accounting for these factors, and other factors in Table 1 that were significantly associated (P < 0.10) in bivariate comparisons. To maintain parsimony, only variables that remained statistically significant (P < 0.05) or exhibited confounding effects were retained in the final models.
Table 1.
Sociodemographic Characteristics, HIV Risk Behaviors and Disease Outcomes Among PWID in NYC by Place of Birth, Puerto Rican Ancestry and PR Migration Scale, 2012. N = 481.
| By Place of birth, Puerto Rican ancestry and migration recency2
|
||||||
|---|---|---|---|---|---|---|
| Total | U.S.-born Non-Hispanic | U.S.-born Puerto Rican | Long-term PR Immigrant | Medium-term PR Immigrant | Recent PR Immigrant | |
|
|
||||||
| 481 % |
191 % |
128 % |
82 % |
41 % |
39 % |
|
|
|
||||||
| Language (interview administration)** | ||||||
|
|
||||||
| English | 91 | 100 | 96 | 87 | 63 | 69 |
| Spanish | 9 | 0 | 4 | 13 | 37 | 31 |
|
|
||||||
| Gender** | ||||||
|
|
||||||
| Male | 77 | 70 | 72 | 88 | 93 | 95 |
| Female | 23 | 30 | 28 | 12 | 7 | 5 |
|
|
||||||
| Race/Ethnicity** | ||||||
|
|
||||||
| Hispanic | 60 | 0 | 100 | 100 | 100 | 100 |
| White | 16 | 40 | 0 | 0 | 0 | 0 |
| Black | 23 | 57 | 0 | 0 | 0 | 0 |
| Other | 1 | 3 | 0 | 0 | 0 | 0 |
|
|
||||||
| Age** | ||||||
|
|
||||||
| 18–29 | 8 | 11 | 6 | 0 | 5 | 16 |
| 30–39 | 24 | 16 | 23 | 20 | 46 | 51 |
| 40–49 | 38 | 31 | 52 | 38 | 42 | 23 |
| 50+ | 30 | 42 | 19 | 42 | 7 | 10 |
|
|
||||||
| Sociodemographics1 | ||||||
|
|
||||||
| Homeless past 12 months* | 50 | 45 | 52 | 45 | 51 | 72 |
| Currently Homeless** | 35 | 28 | 40 | 31 | 39 | 54 |
| Household Income <$10K | 73 | 67 | 74 | 75 | 81 | 84 |
| Incarcerated** | 34 | 40 | 37 | 23 | 37 | 13 |
|
|
||||||
| Sexual Risk Behaviors1 | ||||||
|
|
||||||
| Unprotected VA† intercourse (UI) | 69 | 63 | 74 | 73 | 66 | 74 |
| UI VA w/Casual partner* | 32 | 27 | 30 | 42 | 24 | 49 |
| ≥ 3 total Partners (UI VA)** | 25 | 18 | 23 | 31 | 27 | 51 |
|
|
||||||
| Alcohol Use1 | ||||||
|
|
||||||
| Binge Alcohol use** | 42 | 47 | 50 | 31 | 29 | 23 |
| Binge Alcohol use ≥ x1/week | 22 | 24 | 27 | 17 | 20 | 8 |
|
|
||||||
| Non-Injection Drug Use1 | ||||||
|
|
||||||
| NI drug use ≥ x1/week* | 44 | 49 | 50 | 33 | 32 | 31 |
| NI Crack Use** | 25 | 34 | 27 | 12 | 15 | 15 |
|
|
||||||
| Injection Drug Use1 | ||||||
|
|
||||||
| Drug Injection ≥ x1/day* | 62 | 63 | 55 | 56 | 78 | 80 |
| Drugs Most Injected** | ||||||
| Heroin alone | 66 | 79 | 67 | 59 | 49 | 33 |
| Speedball | 26 | 13 | 25 | 38 | 46 | 51 |
| Cocaine alone | 7 | 7 | 8 | 4 | 5 | 15 |
|
|
||||||
| Injection Risk Behaviors1 | ||||||
|
|
||||||
| Receptive Syringe Sharing** | 26 | 20 | 24 | 24 | 49 | 41 |
| Distributive Syringe Sharing* | 26 | 22 | 22 | 29 | 34 | 41 |
| Receptive/Distributive Syringe Sharing** | 34 | 29 | 29 | 33 | 56 | 49 |
| Cooker, cotton, water sharing | 46 | 41 | 45 | 43 | 63 | 56 |
|
|
||||||
| Disease Outcomes | ||||||
|
|
||||||
| HIV Seroinfection (n= 462) | 12 | 17 | 12 | 12 | 5 | 3 |
| HCV Seroinfection (n=447)** | 68 | 58 | 62 | 76 | 98 | 92 |
|
|
||||||
Past 12 months;
Recent = immigrated within the past 3 years, medium-term = immigrated more than 3 years but less than 10 years in the past, and long-term = immigrated more than 10 years ago.
p < 0.05;
p < 0.01.
Vaginal/Anal.
RDS weighted estimates may not be generalizable to the target population if RDS assumptions are not met and large sample sizes may be needed to obtain precise weighted estimates (Heckathorn 2007, White et al. 2015). There were no significant differences between unweighted and weighted percentages for the outcome variables (migration category, unprotected sex with a casual partner, and receptive syringe sharing), so we used unweighted data in the analyses.
1.3 Results
In Table 1 we summarize sociodemographic results for a sample of 481 PWID in NYC (after excluding non-Puerto Rican immigrants, U.S.-born non-Puerto Rican Hispanics and Puerto Rican immigrants who initiated injection drug use in NYC (N=44). With 91% of the interviews conducted in English, the remaining 9% were conducted in Spanish. Overall, 77% were males. Most (60%) were of Puerto Rican ancestry (U.S.-born and PR-born), 23% were non-Hispanic Black, and 16% were non-Hispanic White. Most (68%) were 40 or older, 24% were in their 30’s and 8% were between 18–29 years old. Also, 35% were homeless at the time of the interview, and 50% experienced homelessness in the past 12 months. Almost 75% had legal incomes below $10,000, and 34% had been incarcerated in the past 12 months.
Almost 70% reported unprotected anal/vaginal sex in the past 12 months; 32% overall did so with casual partners. During that same period of time, 25% had 3 or more sexual partners. A total of 42% reported binge alcohol use (consumed 5 – or 4 for women – or more alcoholic beverages in one sitting at least once in the past 12 months), while 25% reported using non-injection crack in the past 12 months.
Overall, 62% reported injecting drugs at least once a day, and most (66%) only injected heroin. As to syringe sharing, 26% reported receptive and distributive syringe sharing respectively, while 34% reported receptive and/or distributive syringe sharing in the past 12 months. An even higher percentage (46%) reported sharing other injection equipment such as cookers, cottons, and rinse water. HIV seroprevalence was 12%, and HCV seroprevalence was 68%.
Table 1 also shows results of bivariate analyses by place of birth/immigration recency category. Interview language was more likely to be Spanish for immigrant Puerto Rican PWID. Immigrants were also more likely to be male. Homelessness (past 12 month and current) differed significantly by group, with the highest proportion reported by recent immigrants. Recent incarceration differed by group, with the lowest frequency reported by recent immigrants.
The proportions reporting unprotected sex with a casual partner, and having 3 or more total sex partners differed significantly, with recent immigrant reporting the highest values. Binge alcohol use and crack cocaine use also differed significantly among groups, with U.S.-born Puerto Rican PWID (alcohol) and U.S.-born non-Hispanic PWID (crack cocaine) reporting the highest values.
Injection frequency differed by place of birth/immigrant recency, with recent immigrants reporting the highest frequency. The most frequently injected drugs also differed among groups, with U.S.-born non-Hispanic PWID reporting heroin alone, and recent immigrants reporting speedballs and cocaine alone most frequently. Receptive and distributive syringe sharing also differed significantly by group, with recent and medium-term immigrants more likely to report both types of syringe sharing. Although HIV seroprevalence did not differ significantly across groups, HCV seroprevalence varied widely, from a low of 58% among U.S.-born non-Hispanic PWID to a high of 98% among medium-term immigrants.
Tables 2a and 2b show the prevalence of sexual and injection risk behaviors and their bivariate associations with participant characteristics. Table 2a shows recent and long-term immigrants were more likely to have unprotected sex with casual partners compared to U.S.-born non-Hispanic PWID. Unprotected sex with casual partners was also significantly associated with current homelessness, crack cocaine use, and binge alcohol use. In contrast, Table 2b shows recent and medium-term immigrants were more likely to receptively share syringes compared to U.S.-born non-Hispanic PWID. Receptive syringe sharing was also significantly associated with age 30–39 compared to those over 50, current homelessness, and injection frequency.
Table 2a.
Factors associated with unprotected sex with casual sexual partners in the past 12 months. N = 481.
| Unprotected Sex with a Casual Partner
|
|||
|---|---|---|---|
| % | Odds Ratio (95% CI1) | Adjusted Odds Ratio (95% CI) | |
|
|
|||
| Overall | 33.1 | - | - |
| Gender | |||
| Male | 35.4 | 1 | |
| Female | 25.9 | 0.64 (0.40, 1.03) | |
| Age | |||
| 18–29 | 47.2 | 2.00 (0.96, 4.22) | |
| 30–39 | 41.4 | 1.58 (0.95, 2.64) | |
| 40–49 | 26.8 | 0.82 (0.51, 1.33) | |
| 50+ | 30.8 | 1 | |
| Migration category | |||
| U.S.-Born Non-Hispanic | 27.8 | 1 | 1 |
| U.S.-Born Puerto Rican | 31.3 | 1.18 (0.73, 1.93) | 1.23 (0.75, 2.03) |
| Recent Immigrant | 51.3 | 2.74 (1.36, 5.54) | 3.61 (1.74, 7.49) |
| Medium-term Immigrant | 29.3 | 1.08 (0.51, 2.27) | 1.35 (0.63, 2.89) |
| Long-term Immigrant | 41.5 | 1.84 (1.07, 3.17) | 2.36 (1.34, 4.17) |
| Sociodemographics | |||
| Currently homeless | 39.8 | 1.58 (1.06, 2.34) | |
| Household Income < $10,000 | 33.6 | 1.05 (0.68, 1.61) | |
| Incarcerated in past 12 months | 38 | 1.40 (0.94, 2.08) | |
| Substance Use | |||
| Non-injection crack use | 41.3 | 1.62 (1.06, 2.48) | 1.82 (1.16, 2.86) |
| Binge Alcohol Use | 38.5 | 1.52 (1.04, 2.23) | 1.67 (1.12, 2.51) |
| Injection frequency once per day or more | 35.7 | 1.38 (0.92, 2.05) | |
|
|
|||
CI = Confidence interval.
Table 2b.
Factors associated with receptive syringe sharing in the past 12 months. N = 481.
| Receptive Syringe Sharing
|
|||
|---|---|---|---|
| % | Odds Ratio (95% CI1) | Adjusted Odds Ratio (95% CI) | |
|
|
|||
| Overall | 25 | - | - |
| Gender | |||
| Male | 35.4 | 1 | |
| Female | 25.9 | 1.00 (0.61, 1.65) | |
| Age | |||
| 18–29 | 22.2 | 1.38 (0.56, 3.39) | |
| 30–39 | 35.3 | 2.65 (1.49, 4.70) | |
| 40–49 | 25.1 | 1.63 (0.94, 2.80) | |
| 50+ | 17.1 | 1 | |
| Migration category | |||
| U.S.-Born Non-Hispanic | 19.4 | 1 | 1 |
| U.S.-Born Puerto Rican | 23.4 | 1.27 (0.74, 2.20) | 1.25 (0.71, 2.19) |
| Recent Immigrant | 35.9 | 2.33 (1.11, 4.92) | 2.07 (0.94, 4.53) |
| Medium-term Immigrant | 46.3 | 3.60 (1.77, 7.32) | 3.48 (1.66, 7.30) |
| Long-term Immigrant | 24.4 | 1.34 (0.72, 2.49) | 1.47 (0.77, 2.80) |
| Sociodemographics | |||
| Currently homeless | 34.3 | 2.09 (1.37, 3.19) | 1.77 (1.14, 2.76) |
| Household Income < $10,000 | 26.7 | 1.45 (0.88, 2.36) | |
| Incarcerated in past 12 months | 23.9 | 0.92 (0.59, 1.43) | |
| Substance Use | |||
| Non-injection crack use | 28.1 | 1.25 (0.78, 1.98) | |
| Binge Alcohol Use | 29 | 1.44 (0.95, 2.19) | 1.60 (1.02, 2.50) |
| Injection frequency once per day or more | 30.1 | 2.42 (1.51, 3.87) | 2.15 (1.32, 3.51) |
|
|
|||
CI = Confidence interval.
Results from our multivariable logistic regression analyses are also shown in Tables 2a and 2b. In adjusted analyses (Table 2a), recent immigrants were more than three times as likely (AOR 3.61, CI: 1.74–7.49), and long-term immigrants were more than twice as likely to have unprotected sex with casual partners (AOR 2.36, CI: 1.34, 4.17) compared to U.S.-born non-Hispanic PWID. Having unprotected sex with casual partners was also significantly associated with crack cocaine use (AOR 1.82, CI: 1.16, 2.86), and binge alcohol use (AOR 1.67, CI: 1.12, 2.51). Also in adjusted analyses (Table 2b), medium-term immigrants were more than three times as likely to receptively share syringes (AOR 3.48, CI: 1.66, 7.30) compared to U.S.-born non-Hispanic PWID. In addition, receptive syringe sharing was also significantly associated with current homelessness (AOR 1.77, CI: 1.14, 2.76), binge alcohol use (AOR 1.60, CI: 1.02, 2.50) and injecting once per day or more frequently (AOR 2.15, CI: 1.32, 3.51).
1.4 Discussion
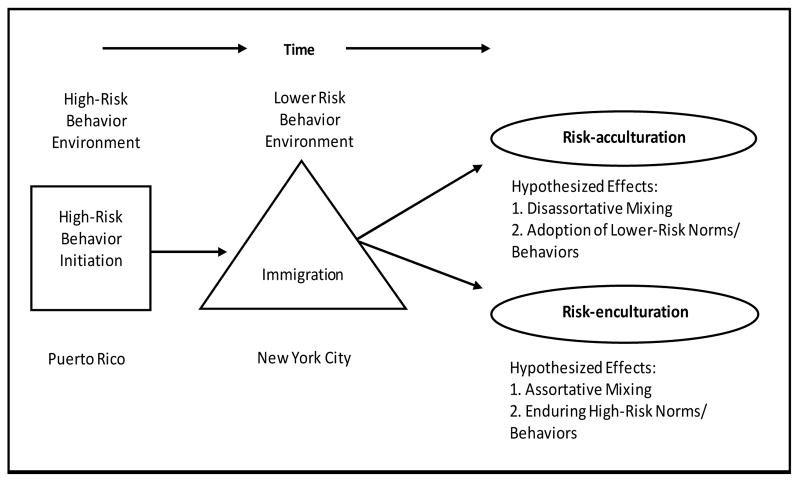
Our results confirm previous findings of elevated HIV risk behaviors among immigrant Puerto Rican PWID in NYC (Deren et al., 2007; Kang et al., 2009). Unlike previous studies, however, we tested the relationship between time since migration and English-language proficiency with HIV behavioral risks using a linear risk-acculturation model. Our results support the risk-acculturation hypothesis only partially, and suggest that acculturation proceeds differently with different types of risk behaviors (e.g., sexual behavior vs. drug use), and raise important questions about how risks persist over time. The risk-acculturation process may be accompanied by other factors behind risk behaviors (Figure 1).
Figure 1.
Puerto Rican People Who Inject Drugs Immigration Risk-Acculturation/Risk-Enculturation Model
1.4.1 Risk-acculturation
In this analysis, receptive syringe sharing and frequency of injection among long-term immigrants are not significantly different than those of U.S.-born non-Hispanic PWID, and are similar to U.S.-born Puerto Rican PWID. This suggests the effects of risk-acculturation. The fact that homelessness, which is significantly associated with receptive syringe sharing (Table 2b), is not more prevalent among medium-term immigrants supports this risk-acculturation thesis. Similarly, binge alcohol use, also associated with increased receptive syringe sharing, is less frequent among immigrants, further supporting our risk-acculturation hypothesis.
Still, if immigrant Puerto Rican PWID were simply risk-acculturating, we would expect recent immigrants to report the highest rate of syringe sharing, followed by medium-term immigrants, and then long-term immigrants. However, in multivariable analyses, medium-term immigrants were most likely to share syringes. The non-monotonicity of the relationship between immigration recency and syringe sharing suggests that other factors may have contributed to the results. There may be cohort differences in risk behaviors, potentially leading to medium-term immigrants having had the highest syringe sharing at the time of immigration.
Intriguingly, medium-term immigrants were not more likely to engage in unprotected sex with casual partners than U.S.-born non-Hispanic PWID, while recent and long-term immigrants were more than twice as likely. This increased sexual risk for long-term immigrants suggests that sexual risk-acculturation does not occur and the need to better incorporate sexual risk reduction efforts into injection-related risk reduction services for immigrants. This heightened sexual risk and reduced injection risks among long-term immigrants was also found in a previous study (Gelpí-Acosta et al., 2011). However, our more precise categorization of immigration recency show more complex, non-linear relationships between immigration recency and risks. More research is needed to understand the complex ways that risk behaviors are reduced over time due to risk-acculturation, or persist.
1.4.2 Risk-enculturation and structural instability
Acculturation is not merely the replacing of native cultural traits with new ones in the host country. The influence of context (Page and Fraile, 2001; Tempalski and McQui, 2009) and enculturation (Alegria, 2009; Cortés et al., 2003) over immigrant health have been noted. To unfold, enculturation requires a cultural enclave. There is a sizeable Puerto Rican PWID population in the Northeast (CDC, 2010; Pouget et al., 2012), and in NYC, the presence of Spanish-monolingual immigrant Puerto Rican PWID is documented (Gelpí-Acosta et al., 2011; Neaigus et al., 2013). A qualitative study found a risk-prone “Puerto Rican-way of injecting drugs” that endorses syringe sharing among “brothers,” (immigrant-only) perpetuating their injection risks in NYC (Gelpí-Acosta et al., 2011). Another qualitative study found heroin misuse dispositions may require comprehensive structural and psychodynamic changes to recede (Gelpí-Acosta, 2014; Gelpí-Acosta, 2015). We contend that risk-enculturation (Figure 1), defined as the maintenance of culturally-informed risk behaviors, may be at play behind sustained injection risks (Table 2b) among recent and medium-term immigrants. Comparable risk-enculturation phenomena occur among immigrant Russian PWID in Brooklyn (Guarino et al., 2012). Also, structural instability (e.g., current homelessness, poverty) may influence these injection risks.
Because the association between time and sexual risks was not linear, risk-enculturation may also explain sexual risks. Lack of condom availability and sexual education in Puerto Rico translates into PR-specific sexual norms that facilitate greater sexual risk behaviors (Kang et al., 2009; Oliver-Vélez et al., 2003). These immigrants often hold negative attitudes towards condom use campaigns in NYC perceived as “too open,” whilst condom use counters “emotional connections” sought in the sexual act (Oliver-Vélez et al., 2003). In an immigrant Puerto Rican PWID enclave (NYC), these attitudes and beliefs may be perpetuated over time and explain sustained sexual risk, especially if language and other cultural factors lead to partner-seeking within the immigrant group. As shown in Table 1, the lower frequency of binge alcohol use and crack use (both associated with increased sexual risk - Table 2a) among immigrants compared to U.S.-born PWID is consistent with our risk-enculturation interpretation.
1.4.3 Health outcomes
Overall, unlike other immigrant health research findings where acculturation increases illicit drug use and HIV risk, evidence indicates that Puerto Rican PWID migrate to the U.S. with already established cultural norms for elevated risk behaviors. This way, acculturation to NYC-specific norms would reduce HIV risk behaviors, leading to positive health outcomes. However, because risk-acculturation may be long-term (10 years for injection and longer for sexual risks), and modulated by risk-enculturation, HIV may be acquired during that period. While HIV prevalence for recent immigrants was 3%, prevalence of long-term immigrants was 12%, implying ongoing exposure to HIV in their networks. A previous analysis found significantly higher HIV prevalence among long-term immigrant Puerto Rican PWID (Gelpí-Acosta et al., 2011).
Although our data do not allow for reaching definitive conclusions, there may be two conflicting processes informing these health outcomes: network disassortative mixing (or the interaction between migrant Puerto Rican PWID and U.S.-born HIV-infected PWID), and risk-acculturation (Figure 1). Immigrants who participate in risk reduction programs may reduce their risk behaviors as a result, but may increase their exposure to HIV if program participation also leads them to enter new HIV risk networks. The precise extent and timeframes of these processes regarding HIV risk remain unclear. If future research confirms the relationship between changing norms and reduced risk behavior, more effective norms-based interventions could be developed to accelerate risk-acculturation among these immigrants. Finally, while HCV prevalence is high across the sample, it is substantially higher among immigrants. This may indicate the saturation of HCV (but not HIV) among immigrants’ injection networks, heightening their elevated vulnerability to future HIV acquisition if those networks interact with networks that have higher HIV prevalence.
1.5 Limitations
Since NHBS is a cross-sectional study, caution must be exercised when attributing differences in risk to the migration phenomenon. While cross-sectional data are hardly adequate for analyzing behavioral changes over time, our results are consistent with previous analyses. Another limitation is that we measure risk-acculturation and risk-enculturation using proxy variables (e.g., language and length of time) that might be limited in capturing the complexities of cultural phenomena. Still, the systematic inclusion of secondary data in the analysis of our findings helps overcome this limitation. It is also conceivable that participants may have migrated to other geographies prior to migration to NYC, and the inability to control for this could have biased our findings. Also, while RDS can potentially reduce bias with long recruitment chains, oversampling of well-connected networks that differ from the general target population, or homophily in recruitment (where respondents recruit others like themselves), may have occurred. Moreover, the possibility of social desirability bias in respondent’s’ responses (including those of respondents who knew they were HIV-infected) is also a limitation. In addition, limiting seed selection to participants enrolled in syringe exchange programs might have helped exclude migrants not enrolled in these programs, and with different (arguably greater) sexual and injection risk behaviors. There was also limited statistical power to test more specific comparisons of potential effects of time since migration, and to test interactions with gender or racial subgroups. Finally, the sample size was insufficient to assess the potential effects of the interaction between age and recency of migration on risk behaviors.
1.6 Conclusions
It is crucial for HIV-negative immigrants to reduce their risk behaviors to avoid HIV infection; acculturation to local behavioral norms can be a risk-reduction mechanism. Some Puerto Rican immigrants in NYC do not seem to acculturate to less risky norms and behaviors over time. In order to identify risk reduction barriers and develop more effective interventions for them, qualitative and longitudinal research are needed on the mechanisms by which risk reduction and/or harm reduction practices are integrated into risk-acculturation processes, and how they can better overcome the countervailing process of risk-enculturation.
Glossary (key terms)
- Acculturation
a process by which immigrants adopt mainstream cultural aspects of the host country
- Risk-acculturation
a process by which immigrant PWID adopt the risk behaviors of local (native to the host country) PWID
- Enculturation
a process by which immigrants actively retain aspects of their native culture amidst the host culture
- Risk-enculturation
a process by which immigrant PWID retain the risk behaviors practiced in their native country amidst the host country
Biographies
Camila Gelpí-Acosta received her Ph.D. in Sociology from the New School University in 2013. Her dissertation explores the experiences of street heroin users with different narratives that define addiction as a “disease.” These data led to her “Junkie habitus” theory, which has appeared in a number of manuscript publications and academic conference presentations. She also consults in an RO1 (R01DA037117) studying infectious diseases among rural injectors in Puerto Rico. In 2014, she was appointed as Assistant Professor at LaGuardia/CUNY, Criminal Justice Program. She also collaborates with El Punto en la Montaña, a syringe exchange program in Puerto Rico.
Dr. Pouget is an epidemiologist whose work is focused on social determinants of health and health disparities, mental disorders, substance use, HIV, other sexually transmitted infections and hepatitis C. He is an experienced methodologist and quantitative analyst, with expertise in scale development, clinical trials, process and systems modeling, and mixed effects modeling. He is Contact Principal Investigator of “Developing measures to study how structural interventions may affect HIV risk (R01 DA031597),” which is developing measures of pathways by which structural interventions can change the size of the population of susceptibles, and affect HIV outbreaks and epidemics.
Katie Reilly is the Project Director of the NYC National HIV Behavioral Surveillance System at the NYC Department of Health and Mental Hygiene. Dr. Reilly’s research has focused on behavioral epidemiology of HIV both in the United States and internationally.
Dr. Holly Hagan is a Professor at NYU College of Nursing and Co-Director of the NIH Center for Drug Use and HIV Research. She holds a PHD in Epidemiology from the University of Washington School of Public Health and Community Medicine. Her research has focused on the infectious disease consequences of substance use, and reducing hepatitis C in people who inject drugs. Her NIH RO1 uses methods of implementation to optimize HCV control strategies in the United States. She is a member of the WHO Global Burden of Disease Study Diseases and Injuries Group, and served on the Institute of Medicine Committee on the Prevention and Control of Viral Hepatitis.
Alan Neaigus, PhD (Sociology) was, until recently, the Director of Research in the HIV Epidemiology Program at the New York City Department of Health and Mental Hygiene. He is an Adjunct Associate Professor in the Department of Epidemiology at the Mailman School of Public Health, Columbia University, and is also an independent research consultant. For over 25 years he has conducted research on HIV/AIDS among injecting and non-injecting drug users and in other at-risk populations in New York City, Newark (NJ), and elsewhere in the USA and internationally. He has also conducted research on the factors associated with the initiation and resumption of injecting among non-injecting drug users. He has authored or co-authored numerous publications in peer-reviewed journals.
Travis Wendel, JD, PhD, is an ethnographer working with marginalized populations in NYC since 1996, is Research Director of St. Ann’s Corner of Harm Reduction in the Bronx, and Principal Investigator of a CDC-funded ethnographic study of prescription opioid and heroin markets in Vermont. From 2004-13, he was Project Director, Co-Investigator, and Principal Investigator on the CDC’s NYC National HIV Behavioral Surveillance study. He has also been funded by NIJ, NIDA, and NSF. Dr. Wendel’s research interests center on the roles of social networks in illicit drug markets, and the harms caused by drug criminalization. His favorite color is green.
David M Marshall IV graduated Summa Cum Laude and as class Salutatorian from John Jay College of Criminal Justice, with a major in Deviance and Culture Studies and minors in Gender Studies and Forensic Psychology. David authored a paper titled “Methamphetamine Use and Mental Health,” which led to his work with the National Institute of Justice, the Social Justice Sexuality Initiative, the NYC National HIV Behavioral Surveillance (Centers for Disease Control and Prevention), and the Center for HIV Educational Studies and Training. David’s publications focus on HIV prevention and transmission in relation to sexual orientation, drug misuse, and other factors.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Contributor Information
C Gelpí-Acosta, Email: camilagelpi@gmail.com.
ER Pouget, Email: pouget@ndri.org.
KH Reilly, Email: kreilly3@health.nyc.gov.
H Hagan, Email: hh50@nyu.edu.
A Neaigus, Email: an2118@cumc.columbia.edu.
T Wendel, Email: traviswendel@gmail.com.
D Marshall, Email: dmarshalliv@gmail.com.
References
- Abraído-Lanza AF, Chao MT, Flórez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61(6):1243–55. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: A cross-national framework. Soc Sci Med. 2012;75: 2060–2068. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- Afable-Munsuz A, Mayeda ER, Perez-Stable EJ, Haan MN. Immigrant generation and diabetes risk among Mexican Americans: The Sacramento Area Latino Study on Aging. Am J Public Health. 2014;104(Suppl 2):S234–50. doi: 10.2105/AJPH.2012.300969r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Woo M, Cao Z, Torres M, Meng X-L, Striegel-Moore R. Prevalence and correlates of eating disorders in Latinos in the United States. Int J Eat Disord. 2007;40: S15–S21. doi: 10.1002/eat.20406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M. The challenge of acculturation measures: what are we missing? A commentary on Thomson and Hoffman-Goetz. Soc Sci Med. 2009;69: 996–998. doi: 10.1016/j.socscimed.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Medina-Mora ME, Breslau J, Aguilar-Gaxiola S. The effect of migration to the Unites States on sustance use disorders among returned Mexican migrants and families of migrants. Am J Public Health. 2007;97(10): 1847–1851. doi: 10.2105/AJPH.2006.097915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Breslau J, Orozco R, Tancredi DJ, Anderson H, Aguilar-Gaxiola S, Medina-Mora ME. A cross-national study on Mexico-US migration, substance use and substance use disorders. Drug Alcohol Depend. 2011;117(1):16–23. doi: 10.1016/j.drugalcdep.2010.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Borges G, Kendler KS, Su M, Kessler RC. Risk for psychiatric disorder among immigrants and their US-born descendants: Evidence from the National Comorbidity Survey-Replication. J Nerv Ment Dis. 2007;195(3):189–195. doi: 10.1097/01.nmd.0000243779.35541.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broesch J, Hadley C. Putting culture back into acculturation: Identifying and overcoming gaps in the definition and measurement of acculturation. Soc Sci Med. 2012;48:375–385. doi: 10.1016/j.soscij.2012.02.004. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. Geographic Differences in HIV Infection Among Hispanics or Latinos- 46 States and Puerto Rico 2010. MMWR. 2012;(61):805–810. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Hispanics or Latinos living with diagnosed HIV: progress along the continuum of HIV care – United States 2010. MMWR. 2014;(63):886–890. No. 40. [PMC free article] [PubMed] [Google Scholar]
- Cortés DE, Deren S, Andía J, Colón HM, Robles RR, Kang S-Y. The use of the Puerto Rican biculturality scale with Puerto Rican drug users in New York and Puerto Rico. J Psychoactive Drugs. 2003;35(2):197–207. doi: 10.1080/02791072.2003.10400001. [DOI] [PubMed] [Google Scholar]
- Department of Health of Puerto Rico. Perfil Epidemiológico Integrado para la Prevención del VIH en Puerto Rico, 2005 – 2011. San Juan, Puerto Rico: Department of Health of Puerto Rico; 2012. [Google Scholar]
- Deren S, Shedlin M, Decena CU, Mino M. Research challenges to the study of HIV/AIDS among migrant and immigrant Hispanic populations in the United States. J Urban Health. 2005;82(2, Supplement 3):iii13–iii25. doi: 10.1093/jurban/jti060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deren S, Kang SY, Colón HM, Robles RR. The Puerto Rico-New York Airbridge for drug users: description and relationship to HIV risk behaviors. J Urban Health. 2007;84(2):243–54. doi: 10.1007/s11524-006-9151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deren S, Kang SY, Colón HM, Robles RR. Predictors of injection drug use cessation among Puerto Rican drug injectors in New York and Puerto Rico. Am J Drug Alcohol Abuse. 2007a;33(2):291–9. doi: 10.1080/00952990601175037. [DOI] [PubMed] [Google Scholar]
- Deren S, Gelpí-Acosta C, Albizu C, González A, Des Jarlais D. Addressing the HIV/AIDS epidemic among Puerto Rican people who inject drugs: the Need for a Multi-Region Approach. Am J Public Health. 2014a;104(11):2030–6. doi: 10.2105/AJPH.2014.302114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deren S, Gelpí-Acosta C, Albizu C, González A, Des Jarlais D. Deren et al. Respond. Am J Public Health. 2014:e1. doi: 10.2105/AJPH.2014.302409. Published online ahead of print November 13, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dow HD. The acculturation process: The strategies and factors affecting the degree of acculturation. Home Health Care Management and Practice. 2011;23(3):221–227. doi: 10.1177/1084822310390877. [DOI] [Google Scholar]
- Finlinson HA, Oliver-Vélez D, Colón HM, Deren S, Robles RR, Beardsley M, Cant JG, Andía J, Soto-López M. Syringe Acquisition and use of syringe exchange programs by Puerto Rican drug injectors in New York and Puerto Rico: comparisons based on quantitative and qualitative methods. AIDS Behav. 2002;4(4): 341–351. doi: 10.1023/A:1026498321919. [DOI] [Google Scholar]
- Garcia V, Gonzalez L. Labor migration, drug trafficking organizations, and drug use: major challenges for transnational communities in Mexico. Urban Anthropol Stud Cult Syst World Econ Dev. 2009;38(2–4):203–344. [PMC free article] [PubMed] [Google Scholar]
- Gelpí-Acosta C, Hagan H, Jenness SM, Wendel T, Neaigus A. Sexual and injection-related risks in Puerto Rican-born injection drug users living in New York City: a mixed methods analysis. Harm Reduct J. 2011;8:28. doi: 10.1186/1477-7517-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelpí-Acosta C. Challenging biopower: “Liquid cuffs” and the “Junkie” habitus. Drugs: education, prevention and policy. 2014;(0):1–7. doi: 10.3109/09687637.2014.987219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelpí-Acosta C. Junkie habitus: Beyond disease and moral defect. Drug & Alcohol Dependence. 2015;146:e122. http://dx.doi.org/10.1016/j.drugalcdep.2014.09.250. [Google Scholar]
- Guarino H, Moore SK, Marsch LA, Florio S. The social production of substance abuse and HIV/HCV risk: an exploratory study of opioid-using immigrants from the former Soviet Union living in New York City. Subst Abuse Treat Prev Policy. 2012;7:2. doi: 10.1186/1747-597X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn D. Extensions of respondent-driven sampling: analyzing continuous variables and controlling for differential recruitment. Sociological Methodology. 2007;37(1):151–207. doi: 10.1111/j.1467-9531.2007.00188.x. [DOI] [Google Scholar]
- Kang S-Y, Deren S, Mino M, Cortés DE. Biculturality and HIV-risk behaviors among Puerto Rican drug users in New York City. Subst Use Misuse. 2009;44:578–592. doi: 10.1080/10826080802487341. [DOI] [PubMed] [Google Scholar]
- Lansky A, Sullivan PS, Gallagher KM, Fleming PL. HIV behavioral surveillance in the U.S.: a conceptual framework. Public Health Rep. 2007;122(Suppl 1):16–23. doi: 10.1177/00333549071220S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, O’Neill AH, Ihara ES, Chae DH. Change in self-reported health status among immigrants in the United States: Associations wirth measures of acculturation. PLOS One. 2013;8(10):e76494. doi: 10.1371/journal.pone.0076494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López LM, Zerden L, Fitzgerald TC, Lundgren LM. Puerto Rican injection drug users: implications in Massachusetts and Puerto Rico. Eval Program Plann. 2008;31:64–73. doi: 10.1016/j.evalprogplan.2007.05.013. [DOI] [PubMed] [Google Scholar]
- López LM, Zerden LS, Bourgois P, Hansen H, Abadie R, Dombrowski K, Curtis R. HIV/AIDS in Puerto Rican People Who Inject Drugs: Policy Considerations. Am J Public Health. 2014 doi: 10.2105/AJPH.2014.302387. e-View Ahead of Print. American Journal of Public Health 0 0, 0, e1–e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Class M, Gonzalez-Castro F, Ramirez AG. Conceptions of acculturation: A review and statement of critical issues. Soc Sci Med. 2011;72: 1555–1562. doi: 10.1016/j.socscimed.2011.03.011. [DOI] [PubMed] [Google Scholar]
- Neaigus A, Reilly KH, Jenness SM, Hagan H, Wendel T, Gelpí-Acosta C. Dual HIV risk: receptive syringe sharing and unprotected sex among HIV-negative injection drug users in New York City. AIDS Behav. 2013;17(7): 2501–9. doi: 10.1007/s10461-013-0496-y. [DOI] [PubMed] [Google Scholar]
- Oliver-Vélez D, Deren S, Finlinson A, Shedlin M, Robles RR, Andía J, Colón HM, Kang S-Y. Sexual risk behaviors of Puerto Rican drug users in East Harlem, New York and Bayamon, Puerto Rico. Cult Health Sex. 2003;5: 19–35. doi: 10.1080/713804636. [DOI] [Google Scholar]
- Page B, Fraile JS. Where you live and where you shoot: Suggestive data from Valencia, Spain. Subst Use Misuse. 2001;36(1–2):113–129. doi: 10.1081/ja-100000231. [DOI] [PubMed] [Google Scholar]
- Pérez CM, Albizu-García CE, Torres EA. Tackling the health challenge posed by hepatitis C in Puerto Rico: a call for immediate public health actions. Puerto Rico Health Sciences Journal. 2015;34(2) [PubMed] [Google Scholar]
- Pouget ER, Friedman SR, Cleland CM, Tempalski B, Cooper HL. Estimates of the population prevalence of injection drug users in among Hispanic residents of large US metropolitan areas. J Urban Health. 2012;89(3): 527–564. doi: 10.1007/s11524-012-9670-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes JC, Colon HM, Robles RR, et al. Prevalence and correlates of hepatitis C virus infection among street-recruited injection drug users in San Juan, Puerto Rico. J Urban Health. 2006;83(6):1105–13. doi: 10.1007/s11524-006-9109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson AM, Rangel G, Lozada R, Vera A, Ojeda VD. Male injection drug users try new drugs following U.S. deportation to Tijuana, Mexico. Drug Alcohol Depend. 2012;120:142–148. doi: 10.1016/j.drugalcdep.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson AM, Lozada R, Pollini RA, Rangel G, Ojeda VD. Correlates and contexts of U.S. injection drug initiation among undocumented Mexican migrant men who were deported from the United States. AIDS Behav. 2012a;16(6):1670–1680. doi: 10.1007/s10461-011-0111-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumbaut R. Paradoxes of assimilation. Sociological Perspectives. 1997;40:483–511. [Google Scholar]
- Strathdee SA, Lozada R, Ojeda VD, Pollini RA, Brouwer KC, Vera A, Cornelius W, Nguyen L, Magis-Rodriguez C, Patterson TL. Differential effects of migration and deportation on HIV infection among male and female injection drug users in Tijuana, Mexico. PLoS ONE. 2008;3:e2690. doi: 10.1371/journal.pone.0002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Magis-Rodriguez C. Mexico’s evolving HIV epidemic. JAMA. 2008a;300:571–573. doi: 10.1001/jama.300.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, McQuie H. Drugscapes and the role of place and space in injection drug use-related HIV risk environments. Int J Drug Policy. 2009;20(1):4–13. doi: 10.1016/j.drugpo.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009 Oct;69(7):983–91. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- White RG, Lansky A, Goel S, Wilson D, Hladik W, Hakim A, Frost SD. Respondent driven sampling—where we are and where should we be going? Sexually transmitted infections. 2012;88(6):397–399. doi: 10.1136/sextrans-2012-050703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerden L, López LM, Lundgren LM. Needle Sharing Among Puerto Rican Injection Drug Users in Puerto Rico and Massachusetts: Place of Birth and Residence Matter. Subst Use Misuse. 2010;45(10):1605–22. doi: 10.3109/10826081003682842. [DOI] [PubMed] [Google Scholar]