Abstract
Objective
In this review, we offer a conceptual framework that identifies risk factors of postpartum depression (PPD) in immigrant and U.S.-born Latinas in the U.S. by focusing on psychosocial and neuroendocrine factors. While the evidence of the impact psychosocial stressors have on the development of PPD have been well documented, less is known about the biological etiology of PPD or how these complex stressors jointly increase the risk of PPD in immigrant and U.S.-born Latinas in the U.S.
Methods
Using PubMed, CINAHL and Embase, we reviewed the literature regarding psychosocial and physiological risk factors associated with PPD to develop a conceptual model for Latinas from 1990 to 2015.
Results
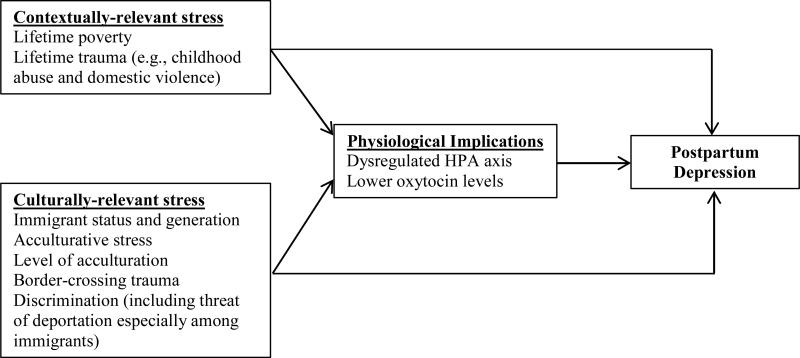
Our search yielded 16 relevant studies. Based on our review of the literature, we developed a biopsychosocial conceptual model of PPD for Latinas in the U.S. We make arguments for an integrated model designed to assess psychosocial and physiological risk factors and PPD in a high-risk population. Our framework describes the hypothesized associations between culturally- and contextually-relevant psychosocial stressors, neurobiological factors (e.g., Hypothalamic-pituitary-adrenal (HPA) axis response system and oxytocin signaling) and PPD in Latinas in the U.S.
Conclusions
Future studies should prospectively evaluate the impact psychosocial stressors identified here have on the development of PPD in both immigrant and U.S-born Latinas while examining neuroendocrine function, such as the HPA axis and oxytocin signaling. Our conceptual framework will allow for the reporting of main and indirect effects of psychosocial risk factors and biomarkers (e.g., HPA axis and oxytocin function) on PPD in foreign- and U.S.-born postpartum Latinas.
Keywords: Latina, stress, postpartum depression, risk, HPA axis, oxytocin
Introduction
Latinas are part of the fastest growing minority group in the U.S. In 2010, Latinas accounted for 24% of all births and immigrant Latinas accounted for 56 percent of births that year (Livingston & Cohn, 2012). Despite the rapid growth of this population and high fertility rates among U.S.- and foreign-born Latinas, there is limited information about the mental health of these women following delivery.
Postpartum depression (PPD), a major depressive episode that occurs following delivery or within the first four weeks after delivery (American Psychiatric Association, 2013), is the leading medical complication among new mothers, and affects an estimated 12-19% of the general population of new mothers (Gavin et al., 2005). The prevalence of PPD in Latinas in the U.S. has been estimated at three to four times greater (30-43%) than the general population of new mothers (Lucero, Beckstrand, Callister, & Sanchez Birkhead, 2012). A growing body of research suggests that psychosocial stressors are important risk factors for PPD (Liu & Tronick, 2013). There is evidence in the literature that prolonged exposure to stress is associated with hyperactivity of stress response systems, such as the hypothalamic-adrenal-pituitary (HPA) axis, which can become dysregulated over time, making it difficult for the individual to adapt to later stressors (Juruena, 2014; Juster, McEwen, & Lupien, 2010; Tomfohr, 2013). Dysregulation of the HPA axis has been implicated in the development of PPD (Jolley, Elmore, Barnard, & Carr, 2007). However, the biological mechanisms by which psychosocial stressors are associated with an increased risk of PPD are poorly understood, particularly among immigrant and U.S-born Latinas who experience high rates of complex and long-lasting psychosocial stressors, because they are not well-represented in biomedical research (Lara-Cinisomo, Wisner, & Meltzer-Brody, 2015) and the multifaceted stressors they encounter throughout their life have not been, to our knowledge, simultaneously examined.
To help address this gap, we reviewed the literature to identify the most robust psychosocial and physiological risk factors associated with PPD and developed a biopsychosocial conceptual framework of PPD risk in foreign and native-born Latinas in the U.S as the first step toward developing an integrated model of stress and PPD. We identified psychosocial stressors that are contextual and culturally-relevant as well as neurobiological contributors. This model is meant to serve a heuristic purpose guiding the design and implementation of future research on the causes of PPD in Latinas. We acknowledge that Latinas are a highly heterogeneous group where country of origin, immigrant history in the U.S. and beliefs about mental health disorders must be carefully considered. For example, while Mexicans make up the largest proportion (64.6%) of the Latino population in the U.S., 13 other subgroups are represented among Latinas in the U.S. (Lopez, Gonzalez-Barrera, & Cuddington, 2013). We further recognize that immigrant Latinas are likely to experience unique stressors associated with the migration experience. However, given that U.S.-born Latinas are usually the children of immigrants and are likely exposed to and experience a number of relevant cultural and contextual stressors, we concluded that our conceptual framework should include both immigrant and U.S.-born Latinas. Future work will allow those testing our model to further explore associations between immigrant-specific stressors, such as legal status, and biological factors identified here. Thus, this article reviews the research on psychosocial and biological factors shown to be associated with PPD. Figure 1 provides an illustration of how these complex factors directly and indirectly impact the development of PPD in immigrant and U.S.-born Latinas in the U.S.
Figure 1.
Conceptual Framework of Latinas Postpartum Depression
Methods
Search Strategy
A systematic review of the literature was conducted using PubMed, CINAHL, and Embase. Only English language articles were selected. The following key words and search terms were used: prenatal, postpartum, postpartum depression, risk, predictors, stress, biomarkers, acculturation, HPA axis, cortisol, oxytocin, and neurobiological and Latina/Hispanic. A start date was not selected to ensure comprehensive results of the published literature. However, the earliest study that met our criteria was published in 2000. The search was conducted in July 2015.
Study Selection
Titles and abstracts were screened for the following inclusion criteria: a) study based on human models; b) empirical studies of PPD; c) assessment of risk factors and stressors; and d) inclusion of postpartum Latina and non-Latina women; e) relevance to Latinas in the U.S.; and f) published in English. Here, Latina refers to women with origins from Mexico, Central and South America.
Results
The following is a review of the most robust and relevant psychosocial and physiological risk factors associated with or contributors to PPD in Latina and non-Latinas in the U.S. We found 16 studies that met our criteria and contributed to our model (see Table 1). Here, we propose a biopsychosocial conceptual framework based on the 16 studies reviewed. Our conceptual framework was developed based on a systematic search of the literature and proposes a direct association between contextually- and culturally-relevant stressors or risk factors and PPD as well as an indirect association mediated primarily through their deleterious effects on the hypothalamic-pituitary-adrenal (HPA) stress response system and oxytocin signaling. There are many biological changes associated with the transition from pregnancy to the early postpartum that are thought to contribute to increased susceptibility to PPD in non-Latinas women. These biological changes include immune, sympathetic nervous system, stress axes and other physiological changes over this time period. However, we have chosen to focus on these two biological contributors because of their robustness and role in stress responses. Furthermore, oxytocin has been demonstrated to inhibit HPA axis during stress (Donaldson-Myles, 2012) and breastfeeding (Cox et al., 2015), suggesting that these two biomarkers might be potential simultaneous points of intervention, particularly given high rates of stress and low breastfeeding rates among Latinas (Center for Disease Control, 2012). We recognize there is a growing body of research showing an association between inflammatory biomarkers (e.g., interleukin-g (IL-6) stress, and depressive symptoms during pregnancy (Christian, 2014). We also acknowledge that there are numerous psychosocial risk factors (e.g., weight and body mass index) that contribute to risk. Our primary focus was to develop a conceptual model based on cultural, contextual and neurobiological risk factors that have been well-established or are considerable stressors for both native-born and immigrant Latinas in the U.S.
Table 1.
Summary Characteristics of Studies Represented in the Proposed Conceptual Framework
| Author | Purpose | Study Design | Sample | Depression-related Measures | Results |
|---|---|---|---|---|---|
| Beck, C.T., Froman, Robin D., & Bernal, H. (2005) | To explore associations between acculturation levels and postpartum depressive symptomatology and PPD in Hispanic subgroups. | Secondary data analysis | Two Hispanic women samples were analyzed in two phases: First phase 1 included 377 women who were on average 10 weeks postpartum and the second phase sample consisted of 150 who were one month postpartum | PDSS-Spanish Version; Short Acculturation Scale | Acculturation was not significantly associated with postpartum depression. |
| Bloch, M., Rubinow, D. R., Schmidt, P. J., Lotsikas, A., Chrousos, G. P., & Cizza, G. (2005) | Examine the effects of high concentration gonadal steroids on stress response in women with and without a history of postpartum depression. | Experimental | Twelve women with a history of postpartum depression (n = 5) and seven matched control without (n = 7) a past postpartum depression. Women were between 22–45 years old. | Edinburgh Postnatal Depression Scale (EPDS) and the Structured Clinical Interview for DSM-IV (SCID) | Women with a history of postpartum depression exhibited higher HPA axis reactivity to the high levels of gonadal steroids. |
| Cox, E. Q., Stuebe, A., Pearson, B., Grewen, K., Rubinow, D., & Meltzer-Brody, S. (2015) | Determine if there is an association between dysregulated oxytocin levels and HPA reactivity in women with postpartum depression in during breastfeeding and stress testing. | Experimental | Prospective cohort of 47 women whom were assessed at 8 weeks postpartum. | Edinburgh Postnatal Depression Scale (EPDS) | Women with postpartum depression had lower oxytocin concentration levels and higher HPA axis reactivity during breastfeeding and stress testing compared to women without depression. |
| Davila, M., McFall, S. L., & Cheng, D. (2009) | Determine prevalence of postpartum depression and its association with acculturation among U.S.-and Mexico-born Latinas. | Cross-sectional | 439 prenatal and postpartum women | Center for Epidemiologic Studies Depression (CES-D) Scale | More than a third reported depression symptoms (21% moderate and 15% high). Results showed a positive association between acculturation and depressive symptoms. Also, single and pregnant women reported more depressive symptoms. |
| D'Anna-Hernandez, K. L., Aleman, B., & Flores, A. M. (2015) | Determine the unique contributions acculturation, acculturative stress and perceived discrimination have on prenatal Mexican-American mothers’ mental health while controlling for general and perceived stress. | Cross-sectional | 98 prenatal Mexican and Mexican-American women between 18 and 45 years of age | Center for Epidemiologic Studies Depression (CES-D) Scale | An estimated 40% reported depressive symptoms. Results showed that acculturative stress and perceived stress predicted increased depressive symptoms. Women who experienced more acculturative stress identified with a blend of Mexican and American cultural values. Also, the Mexican cultural value of respect was found to be protective. |
| Garabedian, M.J., Lain, K.Y., Hansen, W.F., Garcia, L.S., Williams, C.M., & Crofford, L.J. (2011) | Explore the relationship between childhood and adult violent victimization and a history of postpartum depression. | Secondary data analysis | 5380 women from the Kentucky Women's Health Registry, 18 years and older | Yes/No to question regarding history of postpartum depression | A history of violent victimization was associated with reporting a postpartum depression. A higher number of violent traumas had a stronger association with a reported history of postpartum depression. |
| Heim, C., Newport, D. J., Heit, S., Graham, Y. P., Wilcox, M., Bonsall, R., . . . Nemeroff, C. B. (2000) | Determine whether early life abuse is associated with stress reactivity to a laboratory stressor in women with or without depression. | Experimental | 49 women between the 18 and 45 years of age. | Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) | Women with a history of childhood abuse exhibited increased HPA axis response to a laboratory stress, particularly among women with depression. |
| Jackson, C. L., Ciciolla, L., Crnic, K. A., Luecken, L. J., Gonzales, N. A., & Coonrod, D. V. (2015) | Establish the prevalence of victims of intimate partner violence (IPV), investigate the relationship between IPV, demographic characteristics, sociocultural factors (e.g., acculturation) and postpartum depression. | Cross-sectional | 320 perinatal low-income U.S. - and foreign-born Mexican and Mexican-American women | Edinburgh Postnatal Depression Scale (EPDS) | Women with a history of IPV reported elevated levels of depressive symptoms. After controlling for key demographic characteristics, increased number of violent traumatic events increased likelihood of reporting a history of postpartum depression. |
| Jolley, S. N., Elmore, S., Barnard, K. E., & Carr, D. B. (2007) | Determine if women with postpartum depression demonstrated dysregulated HPA axis response to a physiological stressor (treadmill exercise) compared to nondepressed postpartum women. | Prospective, Experimental | 22 prenatal women followed prospectively for approximately 16 weeks | Postpartum Depression Screening Scale (PDSS) | At six and 12 weeks postpartum, women with depression had higher adrenocorticotropic hormone (ACTH) and lower cortisol response to the physiological stressor compared to nondepressed mothers. |
| Magiakou, M. A., Mastorakos, G., Rabin, D., Dubbert, B., Gold, P. W., & Chrousos, G. P. (1996) | Evaluate HPA axis function (i.e., ACTH concentration levels) and psychological well-being in late pregnancy through the 20 weeks postpartum in a sample of health pregnant women. | Prospective, Experimental | Prospective sample of 17 nondepressed pregnant women. | Hamilton Rating Scale for Depression (HRS-D) | Women who developed mild depressive symptoms (i.e., baby blues) or major depression during the postpartum period had suppressed ACTH response to exogenous administration of corticotropic-releasing hormone (CRH). |
| Rodriguez, M. A., Heilemann, M. V., Fielder, E., Ang, A., Nevarez, F., & Mangione, C. M. (2008). | Examine intimate partner violence, strength factors, and adverse social behavioral circumstances in relation to the incidence of depression or PTSD among pregnant Latinas. | Cross-sectional | 210 prenatal Latina women in the second and third trimester between the ages of 18 and 42 years old with and without histories of intimate partner violence | Beck Depression Inventory Fast Screen (BDI-FS) | Approximately 44% of participants had histories of intimate partner violence. Results showed that pregnant Latinas who had experienced intimate partner violence had more than twice the odds of reporting elevated levels of depressive or PTSD symptoms. However, intimate partner violence was only significantly associated with depression after controlling for covariates. |
| Segre, L. S., O'Hara, M. W., Arndt, S., & Stuart, S. (2007) | Examine the relationship between income, education and occupational prestige and the prevalence of postpartum depression in a heterogeneous sample of postpartum women. | Cross-sectional | 4,332 postpartum women (M = 4.6 months), 18 years of age and older | Inventory to Diagnose Depression (IDD) | Income was the most significant predictor of postpartum depression. Low-income women were overrepresented among those with depression. |
| Stuebe, A. M., Grewen, K., & Meltzer-Brody, S. (2013) | Assess neuroendocrine function among lactating postpartum women with and without depression or anxiety. | Prospective, Experimental | 47 prenatal women followed for approximately 12 weeks | Edinburgh Postnatal Depression Scale (EPDS) | Depression and anxiety were negatively correlated with oxytocin levels. At 8 weeks postpartum, breastfeeding women with higher depressive and anxious symptoms had lower levels of oxytocin. |
| Surkan, P. J., Peterson, K. E., Hughes, M. D., & Gottlieb, B. R. (2006) | Explore the relationship between social support and social networks in a racially/ethnically diverse sample of postpartum women. | 415 postpartum women (White, African American, and Latina), mean age = 29.0 (SD = ±6.2) | Center for Epidemiologic Studies Depression (CES-D) Scale | A history of discrimination was associated with depression. Less acculturated women reported elevated depressive symptoms. Higher social support was associated with fewer depressive symptoms. | |
| Valentine, J. M., Rodriguez, M. A., Lapeyrouse, L. M., & Zhang, M. (2011) | Evaluate recent intimate partner violence as a potential prenatal risk factor for postpartum depression among pregnant Latina women. | Prospective, Observational | 210 prenatal Latina women between 18 and 42 years of age who were and were not exposed to intimate partner violence | Beck Depression Inventory Fast Screen (BDI-FS) | In the postpartum period, almost 44% of women experienced elevated depressive symptoms, compared to 33% in the prenatal period. Prenatally, nearly 44% experienced recent or remote intimate partner violence (IPV). Results indicated prenatal depression, recent IPV, low social support, and non-IPV trauma as predictors of postpartum depression. However, only recent IPV and prenatal depression showed highly significant associations in multivariate analyses. |
| Zeiders, K. H., Umaña-Taylor, A. J., Updegraff, K.A., & Jahromi, L. B. (2015) | Examine changes in Mexican adolescent mothers’ depressive symptoms and evaluate potential contributing and protective factors. | Longitudinal | 204 unmarried adolescent mothers of Mexican descent between the ages of 15 and 18 from the third trimester to3 years postpartum | Center for Epidemiologic Studies Depression (CES-D) Scale | Results indicated that depressive symptoms declined in adolescents mothers of Mexican origin after they transitioned into motherhood. Both higher acculturative and enculturative stress were associated with elevated depressive symptoms. However, the association between depressive mod and acculturative stress only held for U.S.-born mothers. |
Contextually- and culturally-relevant psychosocial contributors
Poverty, an important contextual factor, is a significant risk factor for PPD during the vulnerable perinatal period (Segre, O'Hara, Arndt, & Stuart, 2007); Latinas are at high risk of poverty. One in four Latina women in the U.S. lives in poverty (National Poverty Center, 2009). The demands of pregnancy and caring for an infant along with the daily stress of being poor can make Latinas especially vulnerable to PPD, particularly because this population tends to have limited or no access to health care (Rodríguez & Vega, 2009) and often experiences food scarcity (Hromi - Fiedler, Bermúdez - Millán, Segura - Pérez, & Pérez - Escamilla, 2011). A recent study of a low-income, racially and ethnically diverse mothers which included Spanish-speaking women from a Northeastern city in the U.S., revealed that Latinas had higher rates of depression compared to Black and White low-income mothers (Surkan, Peterson, Hughes, & Gottlieb, 2006).
Traumatic experiences in childhood and adulthood are another important contextual stressor in our model. Traumatic events relevant to PPD include, but are not limited to, childhood sexual and physical abuse (Heim et al., 2000) and intimate partner violence (physical and sexual), particularly during pregnancy (Garabedian et al., 2011; Jackson et al., 2015; Rodriguez, 2008; Sumner et al., 2011; Valentine, Rodriguez, Lapeyrouse, & Zhang, 2011). Given the risk of witnessing or experiencing a trauma while illegally crossing the U.S. border, and the number of women who cross the border (Androff & Tavassoli, 2012), our model includes “border-crossing trauma” as a unique risk factor for PPD among Latinas. In addition, Latinas also experience high rates of trauma that begin early in life. The National Child Abuse and Neglect Data System (NCTSN, 2005) reported that Latino children in the U.S. are more likely to experience childhood trauma compared to white children. Therefore, given the importance of capturing the timing of the trauma (Jackson et al., 2015), our model captures trauma history and its proximity to the postpartum period.
Acculturation and Acculturative Stress
Acculturative stress (i.e., stress experienced by social and psychological difficulties when attempting to adapt to a new culture) has been implicated in the development of depression in immigrant populations, including Latinas (Revollo, Qureshi, Collazos, Valero, & Casas, 2011). Numerous studies have shown an association between acculturative stress and poor mental health in Latinos (Araújo Dawson & Panchanadeswaran, 2010; Torres, 2010; Torres, Driscoll, & Voell, 2012). Studies examining the role of acculturative stress in the development of PPD have shown a correlation, with mothers who experience higher levels of acculturative stress during the perinatal period reporting higher depressive symptoms (D'Anna-Hernandez, Aleman, & Flores, 2015; Zeiders, Umaña-Taylor, Updegraff, & Jahromi, 2015). Related is the concept of acculturation (i.e. the degree to which one adapts to host country values, practices and beliefs), which has been explored as a risk factor for PPD in Latinas but findings to date are mixed. Early studies suggested that there was no association of acculturation and PPD (Beck, Froman, & Bernal, 2005). Later studies revealed that less acculturated Latina mothers were more likely to report more depressive symptoms than more acculturated women (Surkan et al., 2006). More recent studies suggest that more acculturated (e.g., those who prefer to speak English) and U.S.-born Latinas were more likely to experience PPD compared to immigrant or less acculturated perinatal Latinas (Davila, McFall, & Cheng, 2009).
The discrepancies in the literature may stem from limited ability of acculturative stress measures, per se, to explain differences in PPD rates among Latinas. Also, those measures do not typically assess immigrant generation or timing of migration that might be captured with more robust measures of acculturative stress. We suggest that stressors unique to the immigrant status experience may explain the disparity. For instance, newer immigrant Latinas (first generation) must contend with a number of factors likely not experienced by more established immigrant and U.S.-born Latinas (second generation), such as language barriers and upward mobility. Undocumented Latinas might also experience fear of deportation, limited prospects of postsecondary education, and in some U.S. states, no prospect of securing a driver's license. Therefore, our conceptual framework accounts for stressors associated with immigrant status and generation as well as level of acculturation to identify immigrant-specific factors that contribute to PPD Latinas.
Racial Discrimination is common among Latinas who often experience and witness racial discrimination from a young age (Lee & Ahn, 2012). Moreover, current political climates and discriminatory laws and policies increase the risk of racial profiling and discrimination across multiple contexts (e.g., roads, place of employment, business, etc.). While there has been limited investigation of the effects that discrimination-related stressors have on PPD in Latinas, one study of postpartum, racially diverse mothers revealed elevated depressive symptoms among those who reported discrimination (Surkan et al., 2006).
Biological Contributors
The cultural and contextual stressors and contributors in our conceptual framework may exert their predictive power via the physiological processes that are involved in both responding to stress and maintaining good mental health. While we acknowledge that there are several important physiologic systems involved in the stress response, here, we focus on the hypothalamic-pituitary-adrenal (HPA) axis because of the existing literature suggesting HPA axis involvement in PPD. Briefly, in response to a perceived stressor, the hypothalamic paraventricular nucleus of the hypothalamus releases corticotropic-releasing hormone (CRH), which triggers the anterior pituitary to release adrenocorticotropic hormone (ACTH) into the blood stream (Tsigos & Chrousos, 2002). ACTH then stimulates the adrenal cortex to promote the synthesis and release of cortisol. Activation of the HPA axis is tempered by a negative feedback loop, which involves cortisol suppressing the release of CRH and ACTH by binding to glucocorticoid receptors in the hypothalamus and pituitary gland (Blume, Douglas, & Evans, 2011). This negative feedback mechanism is intended to reestablish homeostasis and ultimately regulate cortisol release in response to stress.
The HPA axis and stress on postpartum depression
Dysregulation of the HPA axis is a marker of depression in men and women. Women in the perinatal period may be especially vulnerable to depression because of the physiological and psychological stress often associated with pregnancy and motherhood. Dysregulation of the HPA axis has been demonstrated in an experimental model of PPD in non-Latinas (Bloch et al., 2005), which found increased stimulated cortisol levels in women with a history of PPD compared to those without prior PPD. Jolley and colleagues (2007) reported that at 6 and 12 weeks postpartum, depressed women exhibited increased ACTH, the pituitary hormone that mediates the full HPA axis in response to stress, secretion during physiological stress testing, and decreased cortisol response as compared with nondepressed postpartum women. This suggests dysregulation of the HPA axis in women with PPD (Jolley et al., 2007). However, previously, others found a blunted ACTH response in a sample of postpartum women with depression (Magiakou et al., 1996) highlighting the need for additional investigation into the role dysregulated HPA axis function has on the development of PPD.
Stress and trauma have been shown to have a negative effect on HPA axis function in women, particularly on ACTH and cortisol responses (Heim et al., 2000). Heim and colleagues (2000) found that women with histories of trauma exhibited increased ACTH response to experimentally-induced laboratory stress regardless of depression status. Women with histories of abuse and current depression had a 6-fold increase in ACTH release as well as increased cortisol levels compared to controls. Adverse life events, particularly those that occur early in life, such as sexual or physical trauma and poverty, have also been associated with dysregulation of the HPA axis in women with postpartum depression (Heim et al., 2000).
Understanding how stress impacts perinatal Latinas is important due to the high number of stressors they experience over their lifetime that may contribute to this population's ability to adapt to the psychosocial and physiological stress of motherhood. Yet, despite growing interests in PPD and neuroendocrine function in depressed and non-depressed non-Latinas, we do not know how U.S.-born and immigrant Latinas in the U.S. fare because this population is often not engaged in laboratory-based studies (Lara-Cinisomo et al., 2015). Recent studies have begun to examine associations between maternal stress and cortisol levels in Latinas (D'Anna-Hernandez, Ross, Natvig, & Laudenslager, 2011) and in particular their association with levels of acculturation (D'Anna-Hernandez et al., 2015). However, less is known about how culturally-specific factors, such as acculturation, are associated with HPA axis function and PPD. Therefore, understanding how stress impacts this population is important because of the cultural and contextual stressors they encounter prior to and in proximity to the postpartum period, especially given that Latinas experience various psychosocial stressors over many years, if not decades. As such, they would be expected to have a differential impact on stress-responsive systems. Our conceptual framework addresses this gap by proposing a direct association between culturally- and contextually-relevant stress and physiological stress response as well as an indirect association of these stressors through their impact on HPA axis function.
Oxytocin response, stress and PPD
In addition to dysregulated HPA axis, decreased levels of the oxytocin (OT), a hormone originating in the hypothalamus best known for its role in labor, lactation, maternal bonding, and its anxiolytic effects during stress, has also recently been associated with PPD (Stuebe, Grewen, & Meltzer-Brody, 2013). Briefly, oxytocin (OT) is a produced in the hypothalamus, specifically the paraventicular and supraoptic nuclei. In addition to its well known role in facilitating child birth and lactation, it has also been shown to have a positive effect on maternal behavior and bonding, and has been shown to temper HPA axis response in postpartum women (Cox et al., 2015). Furthermore, that there is an inverse association between peripherally measured OT and HPA response during late pregnancy and lactation. Specifically, OT has been shown to increase while HPA axis activity decreases during laboratory stress (Cox et al., 2015) . OT release during breastfeeding has also been related to reduced anxiety behaviors in lactating women (Kim et al., 2013). Additionally, the literature demonstrates that lower levels of OT during pregnancy and shortly after delivery are associated with depressive symptoms (Stuebe et al., 2013).
Given the positive effects OT, particularly higher levels of this hormone, has on perinatal mood and stress, it is important that we examine its function in immigrant and U.S.-born Latinas given the complex stressors and high prevalence of PPD in this population. Oxytocin in Latinas is also important to examine because of observed disparities in breastfeeding rates in immigrant and U.S.-born women, as well as by levels of acculturation. Studies have shown that more acculturated Latinas (i.e., those who have adopted host country values and practices to a greater degree) are less likely to breastfeed compared to less acculturated Latinas (Ahluwalia, D'Angelo, Morrow, & McDonald, 2012). Understanding the potential neuroendocrine contributors and consequences associated with differential levels of breastfeeding and mood is important given Latinas’ vulnerability (e.g., high rates of stress and PPD). Consequently, our framework includes the contribution of OT in the etiology of PPD in immigrant and U.S.-born Latinas in the U.S. On the basis of the prior literature, our conceptual framework proposes that reduced levels of OT are associated with increased psychosocial stress and PPD in this population. We also suggest that decreased levels of OT mediate the association between culturally- and contextually-relevant stress and PPD among Latinas.
Discussion and Conclusion
Here, we propose the first, to our knowledge, conceptual framework based on cultural and contextual stressors and contributors in immigrant and U.S.-born Latinas in the U.S. that have been shown to be the most robust in the literature and that are believed to be chronic. Our model also captures the temporal aspects of these stressors to explore their chronic or cumulative effects on the woman's psychological status, particularly PPD. Our conceptual framework further proposes that future research capture the impact of lifetime stress and trauma as well as the proximity of these stressors to pregnancy and childbirth in order to determine how chronic cultural and contextual stressors are associated with dysregulation of neuroendocrine function and the subsequent development of PPD in Latina women in the U.S. For instance, as cited here, studies of prenatal and postpartum women have shown an association between culturally- and contextually-relevant stressors and PPD, as well as hormone levels (e.g., D'Anna-Hernandez et al., 2011; Stuebe et al., 2013). On the basis of the cited literature, we propose a framework for future research that integrates psychosocial and physiological factors that will improve our understanding of the role biopsychosocial determinants have on the development of PPD in immigrant and U.S.-born Latinas in the U.S. Specifically, we suggest that culturally- and contextually-relevant stressors are directly associated with neuroendocrine function (e.g., HPA axis and OT) and PPD. Furthermore, we theorize that stress response as measured by ACTH and CORT levels is directly associated with stressors discussed here and development of PPD. We also propose that stress-related hormone and OT levels will mediate the relationship between stressors and PPD in immigrant and U.S.-born Latinas by accounting for the association between stressors and PPD. Our conceptual framework allows investigators to not only test these proposed associations, but to explore differences by immigrant status, which might advance our understanding of how contextual, cultural and biological factors contribute to the development of PPD in Latinas. This model is the first step toward unraveling the complex indicators shown to be associated with PPD. For example, border crossing and that threat of deportation can have deleterious effects on the woman and her family. Therefore, in future work, it will be important to determine the extent to which each of these stressors is associated with PPD in immigrant and US-born Latinas.
Results from such investigations can provide findings from individual and joint effects of stressors and neuroendocrine factors discussed here. Our conceptual framework of Latina PPD provides the first step toward a more comprehensive assessment of risk factors among immigrant and U.S.-born Latinas in the U.S. However, while not explored here, protective factors at the individual, family and contextual level (e.g., neighborhood) should also be considered in future studies. For instance, social support has been shown to be an important treatment option for Latinas (Lara-Cinisomo & Wisner, 2013). Moreover, level of social support has been shown to be an important predictor of PPD, with lower levels associated with higher levels of depressive symptomatology (Diaz, Le, Cooper, & Muñoz, 2007; Nylen, O'Hara, & Engeldinger, 2013). In contrast, higher levels of social support from meaningful individuals, such as a romantic partner, have been shown to be protective throughout the perinatal period, particularly among Latinas versus European women (Stapleton et al., 2012). Finally, given the cultural importance placed on social support among Latinas (Campos et al., 2008), this will be an important factor to consider in future PPD models of U.S.- and foreign-born Latinas.
Implications for Practice
The results from this review suggest that Latinas experience cultural and contextual contributors for PPD that should be assessed simultaneously along with biological factors, such as the HPA axis, that are affected by high levels of stress. This study has implications for clinical practice. Health care providers should routinely assess the presence, proximity and degree of the contributors discussed here when evaluating immigrant and U.S.-born postpartum Latinas for mood disorders. Similarly, health professionals should consider the potential effects of how a dysregulated HPA stress response might impact a woman's mood. In sum, it is vital that health providers take into account the broad range of cultural, contextual and biological contributors to PPD identified here.
Acknowledgements
The authors would like to acknowledge the National Institute of Health (MH093315 – “Postdoctoral Training in Reproductive Mood Disorders”; Drs. Girdler & Rubinow, PIs), the Foundation of Hope, and the North Carolina Translational and Clinical Sciences (NC TraCS) Institute for their support of Sandraluz Lara-Cinisomo's research.
Biography
Sandraluz Lara-Cinisomo, EdM, PhD was a T32 NIH Fellow in reproductive mood disorders at the UNC Chapel Hill when this work was completed. She has recently joined the University of Illinois Urbana-Champaign faculty. Her research interests include perinatal mood disorders in Latina and military populations.
Susan Girdler, PhD is Professor in the Department of Psychiatry, Director for the UNC Chapel Hill Psychiatry Stress and Health Research Program and Co-Director of the first NIH-funded T32 in Reproductive Mood Disorders. Dr. Girdler's research interests include the adrenergic and neuroendocrine basis of reproductive mood disorders.
Karen Grewen, PhD is an Associate Professor of Psychiatry, Neurobiology and Psychology at UNC Chapel Hill. Dr. Grewen examines the effects of social affiliation and stress on endocrine, neural, and cardiovascular activity, with a focus on potential biologic mediators.
Samantha Meltzer-Brody, MD, MPH is a clinician and NIH-funded investigator at UNC Chapel Hill where she is an Associate Professor, Associate Chair of Faculty Development in the Department of Psychiatry, and Director of the UNC Perinatal Psychiatry Program of the UNC Center for Women's Mood Disorders.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosures Statement
Samantha Meltzer-Brody received a Research grant from Astra Zeneca. No other competing financial interests exist.
References
- Ahluwalia IB, D'Angelo D, Morrow B, McDonald JA. Association between acculturation and breastfeeding among Hispanic women: data from the Pregnancy Risk Assessment and Monitoring System. Journal of Human Lactation : Official Journal of International Lactation Consultant Association. 2012;28(2):167. doi: 10.1177/0890334412438403. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5) American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Androff DK, Tavassoli KY. Deaths in the Desert: The Human Rights Crisis on the U.S.-Mexico Border. Social Work. 2012;57(2):165–173. doi: 10.1093/sw/sws034. doi: 10.1093/sw/sws034. [DOI] [PubMed] [Google Scholar]
- Dawson Araújo, Beverly, Panchanadeswaran, Subadra Discrimination and Acculturative Stress Among First-Generation Dominicans. Hispanic Journal of Behavioral Sciences. 2010;32(2):216–231. doi: 10.1177/0739986310364750. [Google Scholar]
- Beck CT, Froman Robin D., Bernal Henrietta. Acculturation level and postpartum depression in Hispanic mothers. MCN, The American Journal of Maternal/Child Nursing. 2005;30(5):299–304. doi: 10.1097/00005721-200509000-00006. [DOI] [PubMed] [Google Scholar]
- Bloch M, Rubinow DR, Schmidt PJ, Lotsikas A, Chrousos GP, Cizza G. Cortisol response to ovine corticotropin-releasing hormone in a model of pregnancy and parturition in euthymic women with and without a history of postpartum depression. The Journal of Clinical Endocrinology and Metabolism. 2005;90(2):695–699. doi: 10.1210/jc.2004-1388. doi: 10.1210/jc.2004-1388. [DOI] [PubMed] [Google Scholar]
- Blume J, Douglas SD, Evans DL. Immune suppression and immune activation in depression. Brain, Behavior, and Immunity. 2011;25(2):221–229. doi: 10.1016/j.bbi.2010.10.008. doi: 10.1016/j.bbi.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos Belinda, Schetter Christine Dunkel, Abdou Cleopatra M., Hobel Calvin J., Glynn Laura M., Sandman Curt A. Familialism, Social Support, and Stress: Positive Implications for Pregnant Latinas. Cultural Diversity and Ethnic Minority Psychology. 2008;14(2):155–162. doi: 10.1037/1099-9809.14.2.155. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian Lisa M. Effects of stress and depression on inflammatory immune parameters in pregnancy. American Journal of Obstetrics and Gynecology. 2014;211(3):275–275. doi: 10.1016/j.ajog.2014.06.042. doi: 10.1016/j.ajog.2014.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox EQ, Stuebe A, Pearson B, Grewen K, Rubinow D, Meltzer-Brody S. Oxytocin and HPA stress axis reactivity in postpartum women. Psychoneuroendocrinology. 2015;55:164–172. doi: 10.1016/j.psyneuen.2015.02.009. doi: 10.1016/j.psyneuen.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Anna-Hernandez KL, Aleman B, Flores AM. Acculturative stress negatively impacts maternal depressive symptoms in Mexican-American women during pregnancy. Journal of Affective Disorders. 2015;176:35–42. doi: 10.1016/j.jad.2015.01.036. doi: 10.1016/j.jad.2015.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Anna-Hernandez KL, Ross RG, Natvig CL, Laudenslager ML. Hair cortisol levels as a retrospective marker of hypothalamic–pituitary axis activity throughout pregnancy: Comparison to salivary cortisol. Physiology & Behavior. 2011;104(2):348–353. doi: 10.1016/j.physbeh.2011.02.041. doi: 10.1016/j.physbeh.2011.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davila M, McFall SL, Cheng D. Acculturation and depressive symptoms among pregnant and postpartum Latinas. Maternal and Child Health Journal. 2009;13(3):318–325. doi: 10.1007/s10995-008-0385-6. doi: 10.1007/s10995-008-0385-6. [DOI] [PubMed] [Google Scholar]
- Diaz Manuela A., Le Huynh-Nhu, Cooper Bruce A., Muñoz Ricardo F. Interpersonal Factors and Perinatal Depressive Symptomatology in a Low-Income Latina Sample. Cultural Diversity and Ethnic Minority Psychology. 2007;13(4):328–336. doi: 10.1037/1099-9809.13.4.328. doi: 10.1037/1099-9809.13.4.328. [DOI] [PubMed] [Google Scholar]
- Donaldson-Myles Fiona. Can hormones in breastfeeding protect against postnatal depression? British Journal of Midwifery. 2012;20(2):88–93. [Google Scholar]
- Garabedian Matthew J., Lain Kristine Y., Hansen Wendy F., Garcia Lisandra S., Williams Corrine M., Crofford Leslie J. Violence against women and postpartum depression. Journal of women's health (2002) 2011;20(3):447–453. doi: 10.1089/jwh.2010.1960. doi: 10.1089/jwh.2010.1960. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstetrics and Gynecology. 2005;106(5 Pt 1):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Nemeroff CB. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA : the journal of the American Medical Association. 2000;284(5):592–597. doi: 10.1001/jama.284.5.592. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- Hromi-Fiedler Amber, Bermúdez-Millán Angela, Segura-Pérez Sofia, Pérez-Escamilla Rafael. Household food insecurity is associated with depressive symptoms among low-income pregnant Latinas. Maternal & Child Nutrition. 2011;7(4):421–430. doi: 10.1111/j.1740-8709.2010.00266.x. doi: 10.1111/j.1740-8709.2010.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson CL, Ciciolla L, Crnic KA, Luecken LJ, Gonzales NA, Coonrod DV. Intimate Partner Violence Before and During Pregnancy: Related Demographic and Psychosocial Factors and Postpartum Depressive Symptoms Among Mexican American Women. Journal of Interpersonal Violence. 2015;30(4):659–679. doi: 10.1177/0886260514535262. doi: 10.1177/0886260514535262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolley SN, Elmore S, Barnard KE, Carr DB. Dysregulation of the hypothalamic-pituitary-adrenal axis in postpartum depression. Biological Research for Nursing. 2007;8(3):210–222. doi: 10.1177/1099800406294598. doi: 10.1177/1099800406294598. [DOI] [PubMed] [Google Scholar]
- Juruena MF. Early-life stress and HPA axis trigger recurrent adulthood depression. EPILEPSY & BEHAVIOR. 2014;38:148–159. doi: 10.1016/j.yebeh.2013.10.020. doi: 10.1016/j.yebeh.2013.10.020. [DOI] [PubMed] [Google Scholar]
- Juster Robert-Paul, McEwen Bruce S., Lupien Sonia J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience and Biobehavioral Reviews. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Kim S, Soeken TA, Cromer SJ, Martinez SR, Hardy LR, Strathearn L. Oxytocin and postpartum depression: Delivering on what's known and what's not. Brain Research. 2013 doi: 10.1016/j.brainres.2013.11.009. doi: 10.1016/j.brainres.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara-Cinisomo S, Wisner KL, editors. Perinatal Depression among Spanish- Speaking and Latin American Women : A Global Perspective on Detection and Treatment. Springer; New Yor, NY: 2013. [Google Scholar]
- Lara-Cinisomo S, Wisner Katherine L., Meltzer-Brody S. Advances in science and biomedical research on postpartum depression do not include meaningful numbers of Latinas. Journal of Immigrant and Minority Health. 2015 doi: 10.1007/s10903-015-0205-1. [DOI] [PubMed] [Google Scholar]
- Lee DL, Ahn S. Discrimination Against Latina/os: A Meta-Analysis of Individual-Level Resources and Outcomes. COUNSELING PSYCHOLOGIST. 2012;40(1):28–65. doi: 10.1177/0011000011403326. [Google Scholar]
- Liu CH, Tronick E. Rates and Predictors of Postpartum Depression by Race and Ethnicity: Results from the 2004 to 2007 New York City PRAMS Survey (Pregnancy Risk Assessment Monitoring System). Maternal and Child Health Journal. 2013;17(9):1599–1610. doi: 10.1007/s10995-012-1171-z. doi: 10.1007/s10995-012-1171-z. [DOI] [PubMed] [Google Scholar]
- Livingston G, Cohn D. U.S. Birth Rate Falls to a Record Low; Decline Is Greatest Among Immigrants Social and Demographic Trends. Pew Research Center; 2012. [Google Scholar]
- Lopez MH, Gonzalez-Barrera A, Cuddington D. Center PR, editor. Diverse Origins: The Nation's 14 Largest Hispanic-Origin Groups. 2013 Retrieved from http://www.pewhispanic.org/files/2013/06/summary_report_final.pdf.
- Lucero NB, Beckstrand RL, Callister LC, Sanchez Birkhead AC. Prevalence of postpartum depression among Hispanic immigrant women. Journal of the American Academy of Nurse Practitioners. 2012;24(12):726–734. doi: 10.1111/j.1745-7599.2012.00744.x. doi: 10.1111/j.1745-7599.2012.00744.x. [DOI] [PubMed] [Google Scholar]
- Magiakou MA, Mastorakos G, Rabin D, Dubbert B, Gold PW, Chrousos GP. Hypothalamic corticotropin-releasing hormone suppression during the postpartum period: Implications for the increase in psychiatric manifestations at this time. Journal of Clinical Endocrinology & Metabolism. 1996;81(5):1912–1917. doi: 10.1210/jcem.81.5.8626857. [DOI] [PubMed] [Google Scholar]
- National Poverty Center, NPC The Colors of Poverty: Why Racial & Ethnic Disparities Persist. 2009 [Google Scholar]
- NCTSN, National Child Traumatic Stress Network Promoting Culturally Competent Trauma-Informed Practices. Culture and Trauma Brief. 2005;1 http://www.nctsn.org/sites/default/files/assets/pdfs/culture_and_trauma_brief.pdf. [Google Scholar]
- Nylen Kimberly J., O'Hara Michael W., Engeldinger Jane. Perceived social support interacts with prenatal depression to predict birth outcomes. Journal of Behavioral Medicine. 2013;36(4):427–440. doi: 10.1007/s10865-012-9436-y. doi: 10.1007/s10865-012-9436-y. [DOI] [PubMed] [Google Scholar]
- Revollo H, Qureshi A, Collazos F, Valero S, Casas M. Acculturative stress as a risk factor of depression and anxiety in the Latin American immigrant population. International Review of Psychiatry. 2011;23(1):84–92. doi: 10.3109/09540261.2010.545988. doi: 10.3109/09540261.2010.545988. [DOI] [PubMed] [Google Scholar]
- Rodriguez MA. Intimate partner violence, depression, and PTSD among pregnant Latina women. Ann Fam Med. 2008;6(1):44–52. doi: 10.1370/afm.743. doi: 10.1370/afm.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez Michael A., Vega William A. Confronting inequities in Latino health care. Journal of General Internal Medicine. 2009;24(3):S505–S507. doi: 10.1007/s11606-009-1128-0. doi: 10.1007/s11606-009-1128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segre LS, O'Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression: The relative significance of three social status indices. Social Psychiatry and Psychiatric Epidemiology. 2007;42(4):316–321. doi: 10.1007/s00127-007-0168-1. doi: 10.1007/s00127-007-0168-1. [DOI] [PubMed] [Google Scholar]
- Stapleton Lynlee R. Tanner, Schetter Christine Dunkel, Westling Erika, Rini Christine, Glynn Laura M., Hobel Calvin J., Sandman Curt A. Perceived Partner Support in Pregnancy Predicts Lower Maternal and Infant Distress. Journal of Family Psychology. 2012;26(3):453–463. doi: 10.1037/a0028332. doi: 10.1037/a0028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuebe AM, Grewen K, Meltzer-Brody S. Association Between Maternal Mood and Oxytocin Response to Breastfeeding. Journal of Women's Health (2002) 2013;22(4):352–361. doi: 10.1089/jwh.2012.3768. doi: 10.1089/jwh.2012.3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner Lekeisha A., Valentine Jeanette, Eisenman David, Ahmed Sawsann, Myers Hector, Wyatt Gail, Rodriguez Michael A. The Influence of Prenatal Trauma, Stress, Social Support, and Years of Residency in the US on Postpartum Maternal Health Status Among Low-Income Latinas. Maternal and Child Health Journal. 2011;15(7):1046–1054. doi: 10.1007/s10995-010-0649-9. doi: 10.1007/s10995-010-0649-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan PJ, Peterson KE, Hughes MD, Gottlieb BR. The Role of Social Networks and Support in Postpartum Women's Depression: A Multiethnic Urban Sample. Maternal and Child Health Journal. 2006;10(4):375–383. doi: 10.1007/s10995-005-0056-9. doi: 10.1007/s10995-005-0056-9. [DOI] [PubMed] [Google Scholar]
- Tomfohr, Marie Lianne. Psychosocial Mediators of Ethnic Disparities in Allostatic Load. (Dissertation/Thesis) ProQuest Dissertations Publishing; 2013. Retrieved from http://unc.summon.serialssolutions.com/2.0.0/link/0/eLvHCXMwnV1bS8MwGA3i01DwrtMJ-QPVXLqmeRpONwTn2_C15FYclla3-eC_N1_a1eLlxccQWkpKTnK-yzkIcXZFom-Y4IzTuVAxM1wPBYmtZc5jZ-rPO8osgV7lpzGfPYjJOJ43Tf0QKaj_9gYkA3LbykDQ_JoGsSp_fJLR61sENlKQbm08NTwmU5akdfL2F_YOyM2ETJNGhKcdix-YHPBzutctCKkrTIKUU2k6ldcdCcd_f_k-2rnrZOIP0JYrD1GvhcOPIzSqB3VQHT8GS49qucJVjifr53JhsH8DeBiCJCtelPimKCroT_Izs0rZYzSfTua391FjtxC9CM8hY5kKY2UiqZImAR21XCeg_66kJ9xMCwfSZUMWC6lyzws1XCYNjZ0TOlVc8hO0q6Aqv1yH7j17hjBRBvK2-TAHHkp46iHFJsZwQzWxlvfR6WaFMlsUGdAh0IvntI8G7Uyzq1bZ18Kd__ngBeqx4FgBUZIB2l4v392lvzeU5hNuCsEz. [Google Scholar]
- Torres Lucas. Predicting Levels of Latino Depression: Acculturation, Acculturative Stress, and Coping. Cultural Diversity and Ethnic Minority Psychology. 2010;16(2):256–263. doi: 10.1037/a0017357. doi: 10.1037/a0017357. [DOI] [PubMed] [Google Scholar]
- Torres Lucas, Driscoll Mark W., Voell Maria. Discrimination, Acculturation, Acculturative Stress, and Latino Psychological Distress: A Moderated Mediational Model. Cultural Diversity and Ethnic Minority Psychology. 2012;18(1):17–25. doi: 10.1037/a0026710. doi: 10.1037/a0026710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsigos C, Chrousos GP. Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress. Journal of Psychosomatic Research. 2002;53(4):865–871. doi: 10.1016/s0022-3999(02)00429-4. doi: 10.1016/S0022-3999(02)00429-4. [DOI] [PubMed] [Google Scholar]
- Valentine Jeanette M., Rodriguez Michael A., Lapeyrouse Lisa M., Zhang Muyu. Recent intimate partner violence as a prenatal predictor of maternal depression in the first year postpartum among Latinas. Archives of Women's Mental Health. 2011;14(2):135–143. doi: 10.1007/s00737-010-0191-1. doi: 10.1007/s00737-010-0191-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiders Katharine H., Umaña-Taylor Adriana J., Updegraff Kimberly A., Jahromi Laudan B. Acculturative and enculturative stress, depressive symptoms, and maternal warmth: examining within-person relations among Mexican-origin adolescent mothers. Development and psychopathology. 2015;27(1):293–308. doi: 10.1017/S0954579414000637. doi: 10.1017/S0954579414000637. [DOI] [PMC free article] [PubMed] [Google Scholar]