Abstract
Objective
To determine race- and sex-specific rates of total knee arthroplasty (TKA) and document independent effects of demographic factors on TKA incidence in a population with radiographically confirmed osteoarthritis (OA).
Methods
We used data from the Osteoarthritis Initiative (OAI), a US-based, multicenter, longitudinal study of knee OA. We selected subjects with radiographic, symptomatic OA at baseline and determined TKA incidence rates (ratio of TKAs to time at risk for TKA) over eighty-four months of follow-up. We used multivariable Poisson regression to identify independent associations between demographics factors and TKA utilization.
Results
During study period there were 223 TKAs among 1,915 subjects for an incidence of 1.9% (95% CI: 1.7%–2.2%). The overall rate was 1.9% (95% CI: 1.5%–2.3%) in men vs. 2.0% (95% CI: 1.7%–2.3%) in women, and 2.2% (95% CI: 1.9%–2.6%) in Whites vs. 1.0% (95% CI: 0.7%–1.5%) in non-Whites. We observed a statistically significant interaction between sex and age (stratified at <65 and ≥65 years at end of follow-up), wherein male sex was associated with decreased risk of TKA for younger participants (RR 0.32) but not for older participants. Non-White race was associated with a decreased risk of TKA for both younger (RR 0.32) and older (RR 0.43) participants.
Conclusion
Our finding that non-Whites were less likely to undergo TKA than Whites in adjusted analyses confirm racial differences observed in population-based studies and underscore the need for interventions to address lower use of TKA among non-Whites with OA.
Keywords: Knee osteoarthritis, total knee arthroplasty, total knee replacement, Osteoarthritis Initiative, race, sex, health disparities
Knee osteoarthritis (OA) is one of the most prevalent chronic medical conditions in the United States.1 Patients with symptomatic, advanced knee OA often turn to total knee arthroplasty (TKA), an elective surgical procedure, to restore functional ability and reduce pain.2–4 Over 600,000 TKAs are performed annually in the US to treat OA,5 and about 80% of TKA recipients experience substantial improvement in symptoms and function.6,7
TKA utilization rates have increased dramatically over the past two decades in the United States,8,9 with much of the increase not fully explained by the growing obesity epidemic and overall aging of the population.10 Many studies have pointed to lower TKA utilization in Hispanics and African Americans, while the role of sex is less clear, with some studies suggesting a differentially greater uptake of TKA in women and others finding no sex effect.11–14 However, many of these studies did not restrict analyses to subjects with OA, and therefore were unable to distinguish between the effects of demographic factors on the prevalence of knee OA versus the uptake of TKA among those with knee OA.13–16 Studies that did focus on patients with OA often used self-report or administrative data to identify OA status. These studies did not have a measure of disease severity and were unable to adjust for potential differences in disease severity among demographic groups.12,17–21
The Osteoarthritis Initiative (OAI) has previously been used to determine a variety of clinical features associated with knee OA, including progression to arthroplasty.11,22,23 However, previous studies have not examined in detail age-, sex- and race-stratified incidence and predictors of arthroplasty. In this analysis, we seek to estimate sex- and race-stratified TKA incidence rates over eighty-four months of follow-up and document the independent effect of demographic and clinical factors on TKA incidence in a population with radiographically confirmed knee OA. The comprehensive OAI database will allow us to adjust for baseline OA severity and to incorporate changes in disease severity over time.
Patients and Methods
Sample
We selected data from the OAI, a US multicenter, longitudinal, prospective observational study of knee OA that enrolled men and women ages 45–79 between 2004 and 2006. Subjects were recruited at four clinical centers in the United States: (1) Ohio State University, (2) University of Maryland/Johns Hopkins University joint center, (3) University of Pittsburgh, and (4) Memorial Hospital of Rhode Island. The OAI enrolled subjects with, or at high risk for, knee OA. Exclusion criteria included inflammatory arthritis, bilateral total joint replacement or end-stage OA in both knees, unlikely contraindication or inability to undergo MRI, and use of ambulatory aids other than a single cane for more than 50% of the time. The study protocol was approved by Institutional Review Boards at all participating institutions.24 Subjects were assessed annually; as of January 2015, clinical data were available for the entire cohort through the 84 month visit and image assessment data, including central reader assessment of standardized fixed-flexion knee x-rays, were available through the 48 month visit. De-identified data and additional study details are publicly available online at https://oai.epi-ucsf.org, and the study is registered on ClinicalTrials.gov under identifier NCT00080171.
We selected subjects from the OAI with radiographic, symptomatic knee OA at baseline, defined by a Kellgren-Lawrence (KL) grade of 2–4 based on the central reading of a standardized fixed-flexion radiograph and a Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain subscale score pertaining to that knee of greater than zero.25–27 For subjects with two knees with radiographic, symptomatic OA, we selected the knee with the highest KL grade at baseline. If both knees were of the same KL grade, we selected the knee with the highest baseline WOMAC Pain, and if those were identical, we selected one at random. We excluded all subjects in the healthy control subcohort.
Primary outcome
Our primary outcome was total knee arthroplasty (TKA) adjudicated by the OAI team. Time at risk was defined from time of enrollment to time of TKA or to the last available visit date for those without TKA. We determined the TKA incidence rate as the ratio of the number of TKAs in a specific subgroup over the associated time at risk for TKA.
Factors associated with TKA
We examined the impact of age, sex, race, and education on the incidence of TKA. Age was stratified into <65 and >65 years at the 84 month clinic visit date in order to group together subjects becoming eligible at age 65 for Medicare over the course of follow-up. Race was classified as White vs. non-White, and education as high school or less vs. some college or more.
Statistical methods
Primary Analysis
We computed the overall incidence rate (IR) of TKA per person-year with 95% confidence intervals using Poisson regression. In addition to the overall IR, we present unadjusted stratified rates by baseline age, sex, race, and education. In order to evaluate the independent contribution of each factor to TKA incidence, we used multivariable Poisson regression. In multivariable models we adjusted evaluated the effect of our covariates of interest: sex, race, and education, adjusting for baseline KL grade, baseline WOMAC Pain, baseline body mass index (BMI), and the number of baseline comorbidities (measured by the Charlson index and grouped into scores of 0, 1, and 2+). We used interaction terms in our multivariable models to identify subgroups with differential rates of TKA: we hypothesized that the association between TKA and sex may depend on age and race, and that the association between TKA and race may depend on age. Significance was set at p<0.05 for main effects.
Secondary Analysis
As a secondary analysis, we conducted a time to event analysis. In initial analyses we used Kaplan-Meier survival curves to visualize time to TKA by race, using the log-rank test to evaluate differences among curves. We used a multivariable Cox proportional hazards regression model to evaluate the effect of demographic and clinical factors on time to TKA, adjusting for baseline KL grade, baseline WOMAC Pain, baseline BMI, and the number of baseline comorbidities. We assessed the proportional hazards assumption graphically and with time by covariate interaction effects. We first included KL grade at baseline as an independent variable and then, in additional analysis, included KL grade as a time-varying covariate. Since knees can progress in KL grade over time, this allowed us to distinguish periods of time with different KL grades where the hazard of TKA may be different.
At the time of analysis, KL grade data were only available through the 48 month time point. In order to include time-varying KL grade we restricted our analysis to the baseline through 48 month data. Subjects undergoing TKA prior to 48 months were counted as TKAs (with time up until TKA counted as time at risk) while subjects not undergoing TKA or undergoing TKA after 48 months were censored at the last study visit if prior to 48 months or at 48 months.
Sensitivity Analyses
We conducted a number of sensitivity analyses to investigate the robustness of our conclusions. First, to address the concern that most TKAs are performed in persons with more advanced OA, we re-ran the analysis including only knees with advanced radiographic, symptomatic OA, defined as KL grade 3 or 4 at baseline with WOMAC Pain greater than zero.28,29 In our primary analysis we required that TKAs be adjudicated by the OAI team; that is confirmed by OAI study staff using medical records or X-ray. In a second sensitivity analysis we also considered knees as having TKA if the subject self-reported TKA, if TKA was awaiting adjudication, or if the knee received unicompartamental knee arthroplasty (UKA).To address the concern that all non-Whites were grouped together, and that this group may be heterogeneous, we ran a third sensitivity analysis including only White and African American participants. As a fourth sensitivity analysis, in order to use all available data we included all knees meeting inclusion criteria of radiographic, symptomatic knee OA at baseline. Subjects could contribute 0, 1, or 2 knees to this analytic sample. In this analysis we used Poisson regression with repeated measures to account for multiple knees per person.
We conducted a final sensitivity analysis to examine the impact of subject dropout on TKA incidence rates. We used multiple imputation (MI) to impute TKA for those subjects dropping out of the study.30,31 First, we used logistic regression to compute each subject’s predicted probability p of TKA using the covariates deemed important in the primary analysis and then adjusted p based on time dropout: e.g., a subject completing 4 out of 7 years of follow-up TKA-free would have 3/7 * p probability of TKA in years 4–7. We imputed TKAs in two ways: (1) for each subject dropping out, we used the subject’s adjusted predicted probability p to assign TKA status and (2) we increased p assuming that subjects dropping out had a 15% higher probability of TKA than assigned by the logistic regression model. To more accurately reflect the uncertainty in missing values we created 25 imputed datasets and then used the MIANALYZE procedure in SAS to combine the results across the 25 imputations.
Software
Data analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC).
Results
Sample
Among the 4,796 participants in the OAI, 1,915 participants had at least one knee meeting inclusion criteria. Of these, 1,200 participants had one eligible knee and 715 participants had two eligible knees. For participants with two eligible knees, we selected one as described above for a final analytic sample of 1,915. Thirty-five percent of subjects were under 65 years of age at 84 months follow-up, 41% were male and 26% were non-Whites. 970 (51%) knees were KL 2, 676 (35%) knees were KL 3, and 269 knees (14%) were KL 4. Eighty-one percent of subjects had at least some college education (Table 1).
Table 1.
Description of Sample
| Characteristic | Level | Total Persons |
Persons with one knee |
Persons with two knees |
Total knees |
|---|---|---|---|---|---|
| Age, end of follow- up period |
<65 | 664 (35%) | 417 (35%) | 247 (35%) | 911 (35%) |
| 65+ | 1251 (65%) | 783 (65%) | 468 (65%) | 1719 (65%) | |
| Sex | Male | 786 (41%) | 546 (46%) | 240 (34%) | 1026 (39%) |
| Female | 1129 (59%) | 654 (55%) | 475 (66%) | 1604 (61%) | |
| Race | White | 1412 (74%) | 951 (79%) | 461 (64%) | 1873 (71%) |
| Non-White | 502 (26%) | 248 (21%) | 254 (36%) | 756 (29%) | |
| Education | High school or less |
364 (19%) | 197 (17%) | 167 (23%) | 531 (20%) |
| Some college or more |
1538 (81%) | 994 (83%) | 544 (77%) | 2082 (80%) | |
| Baseline KL grade | 2 | 970 (51%) | -- | -- | 1488 (57%) |
| 3 | 676 (35%) | -- | -- | 871 (33%) | |
| 4 | 269 (14%) | -- | -- | 271 (10%) | |
Note: one participant is missing information on sex. 13 participants are missing information on education.
Primary Analysis
Overall incidence rate of TKA
There were 223 TKAs over 11,645 person years, for an overall annual incidence rate of 1.9% (95% confidence interval [CI]: 1.7%–2.2%). Among those who had TKA, 8% had surgery prior to the 12 month visit, 12% between 12 and 24 months, 19% between 24 and 36 months, 16% between 36 and 48 months, 17% between 48 and 60 months, 16% between 60 and 72 months, and 13% between 72 and 84 months. Of those not undergoing TKA, 342 (20%) discontinued the study prior to the 84 month visit.
Race- and sex-specific incidence rates of TKA
The annual incidence rate of TKA among Whites was estimated at 2.2% (95% CI: 1.9%–2.6%) compared to 1.0% (95% CI: 0.7%–1.5%) in non-Whites. The annual incidence rate of TKA among those who were younger than 65 at follow-up was estimated at 1.3% (95% CI: 1.0%–1.8%) compared to 2.2% (95% CI: 1.9%–2.6%) among older persons. In race–sex subgroup analysis, White females had the highest incidence rate of TKA at 2.3% (95% CI: 1.9%–2.8%) while non-White males had the lowest observed rate at 0.9% (95% CI: 0.4%–1.7%). Race–age subgroup analysis identified older whites as having an annual incidence rate of 2.6% (95% CI: 2.2%–3.0%), higher than any of the three other groups (Table 2). Finally, in age–sex subgroup analysis, younger males had the lowest incidence rate at 1.1% (95% CI: 0.7%–1.7%).
Table 2.
Unadjusted Incidence Rates of TKA
| Characteristic | Level | n (%) | Number of TKAs |
Years at Risk |
Incidence Rate (IR) |
IR 95% CI |
|---|---|---|---|---|---|---|
| Age, end of follow-up period |
<65 | 664 (35%) |
56 | 4148.9 | 1.3% | 1.0%, 1.8% |
| 65+ | 1251 (65%) |
167 | 7496.1 | 2.2% | 1.9%, 2.6% | |
| Sex | Male | 786 (41%) |
88 | 4729.0 | 1.9% | 1.5%, 2.3% |
| Female | 1129 (59%) |
135 | 6916.0 | 2.0% | 1.7%, 2.3% | |
| Race | White | 1412 (74%) |
191 | 8551.7 | 2.2% | 1.9%, 2.6% |
| Non-White | 502 (26%) |
32 | 3086.8 | 1.0% | 0.7%, 1.5% | |
| Sex–Age | Males <65 | 295 (15%) |
21 | 1848.6 | 1.1% | 0.7%, 1.7% |
| Males 65+ | 491 (26%) |
67 | 2880.4 | 2.3% | 1.8%, 3.0% | |
| Females <65 | 369 (19%) |
35 | 2300.2 | 1.5% | 1.1%, 2.1% | |
| Females 65+ | 760 (40%) |
100 | 4615.7 | 2.2% | 1.8%, 2.6% | |
| Race–Age | Whites <65 | 447 (23%) |
44 | 2803.3 | 1.6% | 1.2%, 2.1% |
| Whites 65+ | 965 (50%) |
147 | 5748.4 | 2.6% | 2.2%, 3.0% | |
| Non-Whites <65 | 217 (11%) |
12 | 1345.6 | 0.9% | 0.5%, 1.6% | |
| Non-Whites 65+ | 285 (15%) |
20 | 1741.2 | 1.1% | 0.7%, 1.8% | |
| Race–Sex | White Males | 633 (33%) |
80 | 3797.7 | 2.1% | 1.7%, 2.6% |
| White Females | 779 (41%) |
111 | 4754.0 | 2.3% | 1.9%, 2.8% | |
| Non-White Males | 152 (8%) |
8 | 924.9 | 0.9% | 0.4%, 1.7% | |
| Non-White Females | 350 (18%) |
24 | 2161.9 | 1.1% | 0.7%, 1.7% | |
| Race–Sex– Age |
White Males <65 | 228 (12%) |
17 | 1441.7 | 1.2% | 0.7%, 1.9% |
| White Males 65+ | 405 (21%) |
63 | 2356.0 | 2.7% | 2.1%, 3.4% | |
| White Females <65 | 219 (11%) |
27 | 1361.6 | 2.0% | 1.4%, 2.9% | |
| White Females 65+ | 560 (29%) |
84 | 3392.4 | 2.5% | 2.0%, 3.1% | |
| Non-White Males <65 | 67 (4%) |
4 | 407.0 | 1.0% | 0.4%, 2.6% | |
| Non-White Males 65+ | 85 (4%) |
4 | 517.9 | 0.8% | 0.3%, 2.1% | |
| Non-White Females <65 | 150 (8%) |
8 | 938.6 | 0.9% | 0.4%, 1.7% | |
| Non-White Females 65+ | 200 (10%) |
16 | 1223.3 | 1.3% | 0.8%, 2.1% | |
| Baseline KL grade |
2 | 970 (51%) |
38 | 6205.7 | 0.6% | 5.3%, 8.0% |
| 3 | 676 (35%) |
95 | 4057.4 | 2.3% | 1.9%, 2.9% | |
| 4 | 269 (14%) |
90 | 1381.9 | 6.5% | 0.4%, 0.8% | |
| Education | High school or less | 364 (19%) |
46 | 2097.7 | 2.2% | 1.6%, 2.9% |
| Some college or more | 1538 (81%) |
175 | 9472.8 | 1.8% | 1.6%, 2.1% | |
Multivariable models
In adjusted analysis we found a statistically significant interaction between age, sex, and TKA incidence (p=0.025). For this reason, we present results stratified by age. The other subgroup comparisons (race–age, race–sex, and race–age–sex) were not statistically significant, meaning that the association between TKA and race did not depend on age or sex. For those younger than 65 at follow-up, lower incidence of TKA was significantly associated with non-White race and male sex: non-Whites had 0.32 times the rate of TKA compared to Whites, and males had 0.32 times the rate of TKA compared to females (Table 3A). For those older than 65 at follow-up, lower incidence of TKA was significantly associated with non-White race, but not with sex: non-Whites had 0.43 times the rate of TKA compared to Whites, while males and females were similarly likely to undergo TKA (Table 3A).
Table 3.
Independent predictors* of incident TKA Stratified by Age at End of Follow-up. Part A: all sample; Part B: Restricted to knees at baseline KL 3 or 4
| ALL SAMPLE | <65 | 65+ | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | p-value | RR | 95% CI | p-value | |
| Race: non-White vs. White | 0.32 | 0.15 , 0.70 | 0.004 | 0.43 | 0.26 , 0.71 | <.001 |
| Sex: Male vs. Female | 0.32 | 0.17 , 0.60 | <.001 | 0.79 | 0.57 , 1.1 | 0.155 |
| Education: Some college or more vs. high school or less |
0.52 | 0.27 , 1.0 | 0.052 | 1.04 | 0.68 , 1.6 | 0.866 |
| KL 3–4 only | <65 | 65+ | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | p-value | RR | 95% CI | p-value | |
| Race: non-White vs. White | 0.33 | 0.13 , 0.79 | 0.014 | 0.46 | 0.26 , 0.79 | 0.005 |
| Sex: Male vs. Female | 0.28 | 0.14 , 0.55 | <.001 | 0.75 | 0.53 , 1.1 | 0.108 |
| Education: Some college or more vs. high school or less |
0.48 | 0.24 , 0.96 | 0.038 | 1.07 | 0.66 , 1.7 | 0.792 |
Results from multivariate Poisson regression, adjusted for baseline KL grade, baseline WOMAC Pain, baseline BMI, and baseline number of comorbidities
Secondary Analysis
Time to TKA
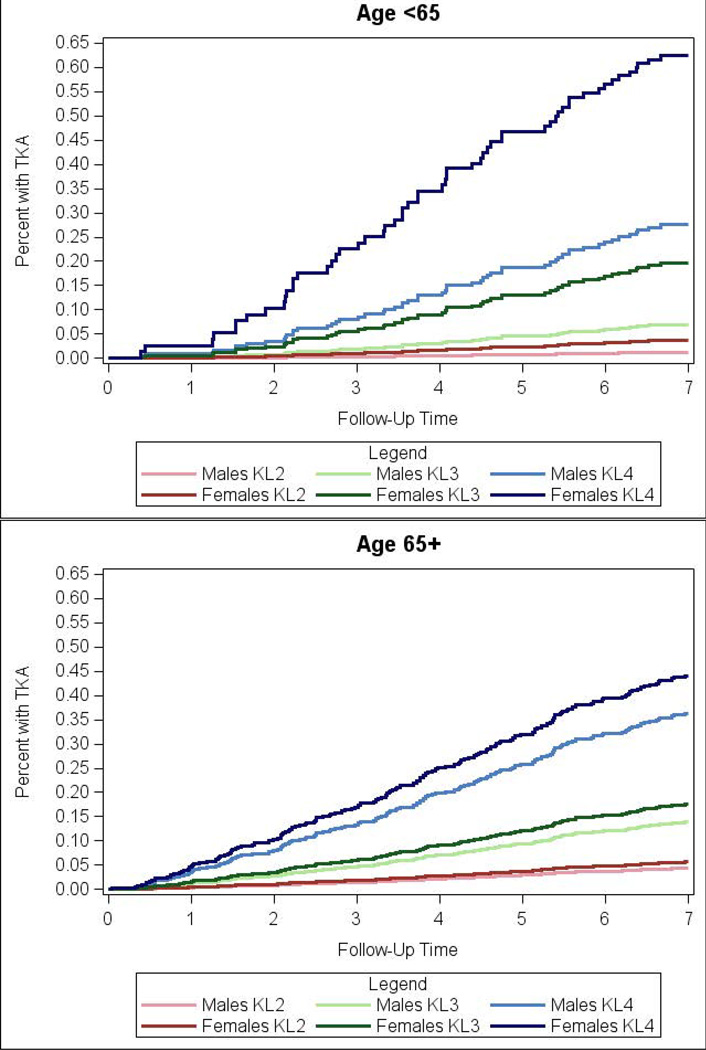
The unadjusted comparison of time to TKA by race using Kaplan-Meier survival curves demonstrated a statistically significant difference, with non-Whites less likely to undergo TKA (p<0.001, Figure 1). In Cox regression, we again observed the interaction between TKA, age and sex (p=0.079) and therefore present age-stratified results. This interaction can be visualized in the Kaplan-Meier survival curves for the unadjusted comparison of time to TKA by KL and sex, stratified by age (Figure 2). For participants younger than 65 at follow-up, within each KL grade the figure demonstrates a marked difference in the survival curves for men and women, with women more likely to undergo TKA. For participants older than 65 at follow-up, within each KL grade the survival curves for men and women are very close together, indicating that men and women are equally likely to undergo TKA.
Figure 1. Kaplan-Meier Survival Estimates with 95% Confidence Bands.
Follow-up time is along the x-axis and percent with TKA is along the y-axis. Each line represents the probability of undergoing TKA over time, stratified by race (blue line for Whites, red line for non-Whites). The shaded area around each line is the 95% confidence band. The log-rank p-value for the difference in the survival curves is <0.001.
Figure 2. Kaplan-Meier Survival Estimates for Age-Sex Subgroups by Baseline KL. (A) Those less 65 years at 7-years follow-up; (B) Those greater than 65 years at 7-years follow-up.
Follow-up time is along the x-axis and percent with TKA is along the y-axis. Each line represents the probability of undergoing TKA over time, stratified by baseline KL (red lines are baseline KL 2, green lines are baseline KL 3, and blue lines are baseline KL 4) and sex (lighter lines are males and darker lines are females). Figure A includes participants in the younger age group (<65 at follow-up) and Figure B includes participants in the older age group (>65 at follow-up). In Figure A, within each baseline KL grade (within each color), the dark line is substantially above the light line, indicating that women are more likely to undergo TKA as compared to men. In Figure B, within each baseline KL grade (within each color), the light and dark lines are much closer together, indicating that there is not a substantial difference in TKA utilization over time between men and women.
For the younger age group, multivariable Cox regression adjusting for time-varying KL grade demonstrated that male sex was significantly associated with decreased hazard of TKA in the adjusted model (HR=0.41). The hazard ratio comparing rates of TKA for non-Whites vs. Whites was 0.27, but did not reach statistical significance (p=0.093). For the older age group, race (non-White vs. White HR=0.17) was significantly associated with hazard of TKA, while sex (p=0.626) and education (p=0.989) were not significant (Table 4).
Table 4.
Hazard Ratios* Stratified by Age at End of Follow-up
| <65 | 65+ | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Race: non-White vs. White | 0.27 | 0.06, 1.2 | 0.093 | 0.17 | 0.06, 0.48 | <0.001 |
| Sex: Male vs. Female | 0.41 | 0.17, 0.99 | 0.047 | 0.89 | 0.57, 1.4 | 0.626 |
| Education: Some college or more vs. high school or less |
0.54 | 0.19, 1.5 | 0.237 | 1.0 | 0.56, 1.8 | 0.989 |
Hazard Ratios (HR) from multivariable Cox regression, adjusted for time-varying KL grade, baseline WOMAC Pain, baseline BMI, and baseline number of comorbidities.
Sensitivity Analyses
In sensitivity analysis restricted to knees with KL 3–4 at baseline, there were 185 TKAs over 84 months of follow-up, for an overall annual incidence rate of 3.4% (95% CI: 2.9%–3.9%). The associations between TKA and covariates were similar to primary analysis. Adjusted analysis demonstrated a statistically significant interaction between age and sex (p=0.009). (Table 3B).
In addition to the 223 adjudicated TKAs in our cohort, there were 5 self-reported knee replacements, 6 TKAs awaiting adjudication, and 17 UKAs. Including these raised the TKA incidence rate from 1.9% to 2.2% among the entire cohort and from 3.4% to 3.8% in the KL 3–4 subgroup. Including these additional surgeries did not change the observed relationships among variables of interest.
Of the non-Whites in our analytic cohort, 89% were African American. Our results did not change appreciably in sensitivity analysis that restricted the sample to Whites and African Americans only.
Among all 2,630 eligible knees there were 281 TKAs over 16,068 person-years, for an overall annual incidence rate of 1.7% (95% CI: 1.5%–2.0%). In sensitivity analysis restricted to knees with KL 3–4 at baseline, there were 211 TKAs over 84 months of follow-up, for an overall annual incidence rate of 3.2% (95% CI: 2.8%–3.7%). The associations between TKA and covariates were similar to primary analysis (Supplemental Table 1).
Twenty percent (342 subjects) of the cohort not receiving TKA dropped out of the study prior to the 84 month visit. The average follow-up time for these patients was 4 years (SD 1.6). Subjects dropping out of the study had higher mean baseline WOMAC pain than completers (28 (SD 19) vs. 24 (SD 19)) and lower mean baseline WOMAC pain than subjects undergoing TKA (30 (SD 17)). Ten percent of completers were KL grade 4 at baseline, compared to 13% of dropouts and 40% of TKAs. Associations between covariates and TKA were similar to the primary analysis. The relative risk of TKA for non-Whites vs. Whites for those aged less than 65 was 0.33 (95% CI: 0.15, 0.74) using the first imputation method and 0.35 (95% CI: 0.15, 0.78) using the second method.
Discussion
We used a large prospective, longitudinal cohort of persons with diagnosed knee OA to determine the incidence of TKA in specific demographic subgroups. We estimated the unadjusted annual incidence rate of TKA to be 1.9% among subjects with radiographic (KL 2–4), symptomatic OA and 3.4% among subjects with advanced radiographic (KL 3–4), symptomatic OA. Non-Whites had a lower rate of TKA as compared to Whites in analyses adjusted for baseline knee OA radiographic severity, pain, BMI, number of comorbidities, age, sex and education. We also noted a statistically significant interaction between age, sex, and TKA rates, with female sex associated with greater TKA uptake in younger (<65 at end of follow-up) persons but not in older persons. Finally, among younger persons more education (at least some college) was associated with a decreased risk for TKA. To our knowledge this study is the first to evaluate predictors of incident TKA adjusting for radiographic and symptomatic severity and the first to incorporate time-varying KL grade.
A number of population-based studies have suggested differential utilization of TKA by race and by sex, but these studies were not done in persons with confirmed knee OA and therefore could not distinguish between the effects of demographic factors on the prevalence of knee OA versus the uptake of TKA among those with OA.12–16,18–21 Our study is one a few that have evaluated persons at risk for TKA due to OA. In a large prospective longitudinal study in Ontario, Canada, Hawker and colleagues did not observe a difference by sex or race for total joint arthroplasty.20 However, 96% of their cohort was White, limiting our ability to compare it to the US-based OAI, which specifically targeted racial and ethnic minorities for enrollment. The Multicenter Osteoarthritis Study (MOST) is another long-term US-based multicenter, longitudinal, prospective observational study of knee OA.32 In an analysis of MOST subjects with radiographic, symptomatic knee OA, Niu et al. found that 26% of subjects underwent TKA over 60 months of follow-up. We found a cumulative 9.6% (95% CI: 8.2%–11.1%) at 60 months in our OAI cohort. Subjects in MOST were heavier than those in the OAI, more frequently had other musculoskeletal conditions and comorbidities, and had more severe knee symptoms at baseline.24 Riddle et al. used a subset of the OAI progression subcohort and found a 2-year incidence of TKA of 3.7% (95% CI: 2.6%–5.3%).11 Due to the small sample size and large number of predictors examined, the authors used the nonparametric random forest method and found that females and subjects with a high school education or less were more likely to undergo TKA, while African Americans were less likely to undergo TKA. Riddle and colleagues conducted their study at an earlier time in the evolution of the OAI, and therefore less data were available. Specifically, at the time of the analysis a subset of the progression subcohort (778 out of 1389 persons) had two year follow-up data available for public use and was included in the analysis. As of January 2015, follow-up data are available through 84 months, and our sample was comprised of all knees with pain and radiographic OA at baseline according to the central reading of a fixed-flexion radiograph. We found a cumulative incidence of 2.4% (95% CI: 1.7%–3.1%) at 24 months. Differences in cumulative incidences may be due to temporal trends, or due to the fact that we used slightly different inclusion criteria.
Across all analyses, we found that non-Whites were significantly less likely to undergo TKA as compared to Whites, controlling for important confounders such as disease severity, education, and pain. This difference has previously been suggested by population-based cohort studies that could not restrict the analysis to persons truly at risk by virtue of having OA, and was also noted in Riddle and colleagues’ OAI-based investigation of predictors of TKA over a two year period.11 Our work adds to these prior studies by using a sample of persons affected by OA and also by extending follow up to seven years, permitting a more extensive picture of TKA use. An additional goal of this analysis was to compute incidence rates in the population truly at risk (those with OA), which are presented here for the first time. We found that female sex was associated with an increased risk for TKA, but only for the younger (<65 at follow-up) age group. A possible explanation for this finding is that surgeons may be more reticent to perform surgery on younger men, who may be at greater risk of eventually requiring revision surgery.33 Finally less educational attainment was associated with an increased risk of TKA, again only for the younger age group. Less education may be a proxy for having a manual labor job. Heavy physical work or manual labor has been shown to be associated with increased risk of developing knee OA.34–37 Younger persons with lower levels of education may therefore both be at greater risk of knee OA and more inclined to opt for TKA in order to return to work. This proposition warrants further investigation, since details regarding occupation are not well captured by OAI demographic information.
Numerous previous studies have attempted to understand this racial disparity in TKA utilization.38,39 African American patients appear to have lower expectations of the benefit of TKA and higher perception of risks, which is reflected in a reduced willingness to consider surgery.40–44 Ibrahim et al. found that African Americans were less familiar with joint replacement compared to whites, and in particular were less likely to have friends or family who had undergone joint replacement.43,44 African American patients in the Johnston County Osteoarthritis Project, both with and without symptomatic OA, were less likely than Whites to consider joint arthroplasty even if recommended by their physician.45 A randomized controlled trial testing the efficacy of an educational intervention found that the intervention was successful in increasing the willingness of African Americans with knee OA to consider surgery, suggesting that this lack of willingness, or reduced expectations, is modifiable.46
Our analysis has several limitations. Over seven years of observation, we observed approximately 300 knee arthroplasties. Because we stratified the analyses by age group, some of our subgroups had very few outcomes (e.g., there were 12 TKAs among 217 non-White participants younger than 65 at end of follow-up). This limited our ability to demonstrate statistical significance with moderate effect sizes. We were also unable to stratify by location, though location was not significant when added to multivariable models. Approximately one-fifth of the cohort not receiving TKA dropped out of the study prior to the 84 month visit; however, Poisson regression takes into account person-time when calculating incidence rates, and participants contributed person-time up until the time of dropout. Further, sensitivity analysis using multiple imputation to gauge the impact of dropouts on incidence of TKA demonstrated this impact to be relatively minor. As of the time of analysis, data for the radiographic progression of OA among the OAI cohort was only available through 48 months; therefore, models with time-varying KL were truncated at the 48 month time point. We did not examine effects of health insurance coverage on TKA use as only a small proportion of the cohort was uninsured. The OAI excluded persons who were unlikely to demonstrate measurable loss of joint space, including persons that had plans to undergo bilateral TKA within three years, end-stage knee OA in both knees, or TKA in one knee and severe joint space narrowing in the contralateral knee. This could bias any estimates of TKA rates downwards as persons with more advanced disease were excluded.22 However, this should not affect associations found between covariates and TKA, since we adjusted for degree of radiographic severity. Finally, as these are publically available data we could not assess the rate of TKA at these centers among persons not enrolling in the OAI and were unable to assess selection bias.
In this study we examined differences in TKA incidence by age, sex, race, and education. Further, the associations between TKA and sex as well as TKA and education depended on age. Whereas females were more likely to have TKA than males among those under 65, among older patients females and males have similar rates. This finding remains largely unexplained and is an area for future research. Our data will help physicians and their patients discuss and plan for the likely need for TKA. These data also will assist health planners (e.g., in managed care organizations) to anticipate TKA utilization among members with knee OA. Our data confirm racial differences in TKA utilization suggested by population-based estimates in a sample of subjects with confirmed OA and underscore the need for interventions to address the lower use of TKA among non-Whites with OA.
Supplementary Material
Significance and Innovation.
We determined the incidence rates of total knee arthroplasty (TKA) over seven years of follow-up in a population with radiographically confirmed, symptomatic knee OA. Unlike many population-based studies, we were able to compute a true incidence rate using time at risk for TKA.
This is the first long-term analysis of TKA utilization that takes radiographic disease severity into consideration
We found that non-Whites were significantly less likely to undergo TKA as compared to Whites. Female sex and less education were associated with an increased risk of TKA for younger subjects but not for older subjects. The interaction between age and TKA is largely unexplained.
Acknowledgements
The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Role of the funding source
Supported by: NIH/NIAMS R01 AR 064320, K24 AR 057827, and P60 AR 047782.
Footnotes
Competing interest statement
The authors do not have any conflict of interest with respect to the content of this paper.
Contributions
Conception and design: Collins, Losina
Collection and assembly of data: Collins, OAI
Analysis and interpretation of the data: all authors
Statistical expertise: Collins, Losina
Drafting of the article: Collins, Deshpande
Critical revision of the article for important intellectual content: all authors
Final approval of the article: all authors
Provision of study materials or patients: OAI
Obtaining of funding: Losina
References
- 1.Losina E, Weinstein AM, Reichmann WM, Burbine SA, Solomon DH, Daigle ME, et al. Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res (Hoboken) 2013;65:703–711. doi: 10.1002/acr.21898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: A systematic review of published literature. Best Pract Res Clin Rheumatol. 2012;26:649–658. doi: 10.1016/j.berh.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paxton EW, Namba RS, Maletis GB, Khatod M, Yue EJ, Davies M, et al. A prospective study of 80,000 total joint and 5000 anterior cruciate ligament reconstruction procedures in a community-based registry in the United States. J Bone Joint Surg Am. 2010;92(Suppl 2):117–132. doi: 10.2106/JBJS.J.00807. [DOI] [PubMed] [Google Scholar]
- 4.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, et al. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am. 2013;95:385–392. doi: 10.2106/JBJS.L.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2:e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katz JN, Mahomed NN, Baron JA, Barrett JA, Fossel AH, Creel AH, et al. Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56:568–574. doi: 10.1002/art.22333. [DOI] [PubMed] [Google Scholar]
- 8.Odum SM, Springer BD, Dennos AC, Fehring TK. National obesity trends in total knee arthroplasty. J Arthroplasty. 2013;28:148–151. doi: 10.1016/j.arth.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 9.Bang H, Chiu YL, Memtsoudis SG, Mandl LA, Della Valle AG, Mushlin AI, et al. Total hip and total knee arthroplasties: trends and disparities revisited. Am J Orthop (Belle Mead NJ) 2010;39:E95–E102. [PubMed] [Google Scholar]
- 10.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–207. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riddle DL, Kong X, Jiranek WA. Two-year incidence and predictors of future knee arthroplasty in persons with symptomatic knee osteoarthritis: preliminary analysis of longitudinal data from the Osteoarthritis Initiative. Knee. 2009;16:494–500. doi: 10.1016/j.knee.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunlop DD, Manheim LM, Song J, Sohn MW, Feinglass JM, Chang HJ, et al. Age and racial/ethnic disparities in arthritis-related hip and knee surgeries. Med Care. 2008;46:200–208. doi: 10.1097/MLR.0b013e31815cecd8. [DOI] [PubMed] [Google Scholar]
- 13.Skinner J, Zhou W, Weinstein J. The influence of income and race on total knee arthroplasty in the United States. J Bone Joint Surg Am. 2006;88:2159–2166. doi: 10.2106/JBJS.E.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 15.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 16.Escarce JJ, McGuire TG. Changes in racial differences in use of medical procedures and diagnostic tests among elderly persons: 1986–1997. Am J Public Health. 2004;94:1795–1799. doi: 10.2105/ajph.94.10.1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeni JA, Jr, Axe MJ, Snyder-Mackler L. Clinical predictors of elective total joint replacement in persons with end-stage knee osteoarthritis. BMC Musculoskelet Disord. 2010;11:86. doi: 10.1186/1471-2474-11-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steel N, Clark A, Lang IA, Wallace RB, Melzer D. Racial disparities in receipt of hip and knee joint replacements are not explained by need: the Health and Retirement Study 1998–2004. J Gerontol A Biol Sci Med Sci. 2008;63:629–634. doi: 10.1093/gerona/63.6.629. [DOI] [PubMed] [Google Scholar]
- 19.Borrero S, Kwoh CK, Sartorius J, Ibrahim SA. Brief report: Gender and total knee/hip arthroplasty utilization rate in the VA system. J Gen Intern Med. 2006;21(Suppl 3):S54–S57. doi: 10.1111/j.1525-1497.2006.00375.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawker GA, Guan J, Croxford R, Coyte PC, Glazier RH, Harvey BJ, et al. A prospective population-based study of the predictors of undergoing total joint arthroplasty. Arthritis Rheum. 2006;54:3212–3220. doi: 10.1002/art.22146. [DOI] [PubMed] [Google Scholar]
- 21.Hawker GA, Wright JG, Coyte PC, Williams JI, Harvey B, Glazier R, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342:1016–1022. doi: 10.1056/NEJM200004063421405. [DOI] [PubMed] [Google Scholar]
- 22.Riddle DL, Perera RA, Stratford PW, Jiranek WA, Dumenci L. Progressing toward, and recovering from, knee replacement surgery: a five-year cohort study. Arthritis Rheum. 2013;65:3304–3313. doi: 10.1002/art.38139. [DOI] [PubMed] [Google Scholar]
- 23.Riddle DL, Kong X, Jiranek WA. Factors associated with rapid progression to knee arthroplasty: complete analysis of three-year data from the Osteoarthritis Initiative. Joint Bone Spine. 2012;79:298–303. doi: 10.1016/j.jbspin.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 24.Niu J, Nevitt M, McCulloch C, Torner J, Lewis CE, Katz JN, et al. Comparing the functional impact of knee replacements in two cohorts. BMC Musculoskelet Disord. 2014;15:145. doi: 10.1186/1471-2474-15-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Collins JE, Katz JN, Dervan EE, Losina E. Trajectories and risk profiles of pain in persons with radiographic, symptomatic knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2014;22:622–630. doi: 10.1016/j.joca.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Woolacott NF, Corbett MS, Rice SJ. The use and reporting of WOMAC in the assessment of the benefit of physical therapies for the pain of osteoarthritis of the knee: findings from a systematic review of clinical trials. Rheumatology (Oxford) 2012;51:1440–1446. doi: 10.1093/rheumatology/kes043. [DOI] [PubMed] [Google Scholar]
- 27.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riddle DL, Jiranek WA, Hayes CW. Use of a validated algorithm to judge the appropriateness of total knee arthroplasty in the United States: a multicenter longitudinal cohort study. Arthritis Rheumatol. 2014;66:2134–2143. doi: 10.1002/art.38685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Escobar A, Quintana JM, Arostegui I, Azkarate J, Guenaga JI, Arenaza JC, et al. Development of explicit criteria for total knee replacement. Int J Technol Assess Health Care. 2003;19:57–70. doi: 10.1017/s0266462303000060. [DOI] [PubMed] [Google Scholar]
- 30.Bell ML, Fairclough DL. Practical and statistical issues in missing data for longitudinal patient-reported outcomes. Stat Methods Med Res. 2014;23:440–459. doi: 10.1177/0962280213476378. [DOI] [PubMed] [Google Scholar]
- 31.Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons; 1987. [Google Scholar]
- 32.Segal NA, Nevitt MC, Gross KD, Hietpas J, Glass NA, Lewis CE, et al. The Multicenter Osteoarthritis Study: opportunities for rehabilitation research. PM&R. 2013;5:647–654. doi: 10.1016/j.pmrj.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O’Connor MI. Implant survival, knee function, and pain relief after TKA: are there differences between men and women? Clin Orthop Relat Res. 2011;469:1846–1851. doi: 10.1007/s11999-011-1782-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:507–515. doi: 10.1016/j.joca.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 35.Martin KR, Kuh D, Harris TB, Guralnik JM, Coggon D, Wills AK. Body mass index, occupational activity, and leisure-time physical activity: an exploration of risk factors and modifiers for knee osteoarthritis in the 1946 British birth cohort. BMC Musculoskelet Disord. 2013;14:219. doi: 10.1186/1471-2474-14-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jensen LK, Eenberg W. Occupation as a risk factor for knee disorders. Scand J Work Environ Health. 1996;22:165–175. doi: 10.5271/sjweh.127. [DOI] [PubMed] [Google Scholar]
- 37.Felson DT, Hannan MT, Naimark A, Berkeley J, Gordon G, Wilson PW, et al. Occupational physical demands, knee bending, and knee osteoarthritis: results from the Framingham Study. J Rheumatol. 1991;18:1587–1592. [PubMed] [Google Scholar]
- 38.Ibrahim SA, Franklin PD. Race and elective joint replacement: where a disparity meets patient preference. Am J Public Health. 2013;103:583–584. doi: 10.2105/AJPH.2012.301077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mota RE, Tarricone R, Ciani O, Bridges JF, Drummond M. Determinants of demand for total hip and knee arthroplasty: a systematic literature review. BMC Health Serv Res. 2012;12:225. doi: 10.1186/1472-6963-12-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Groeneveld PW, Kwoh CK, Mor MK, Appelt CJ, Geng M, Gutierrez JC, et al. Racial differences in expectations of joint replacement surgery outcomes. Arthritis Care Res (Hoboken) 2008;59:730–737. doi: 10.1002/art.23565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ang DC, Monahan PO, Cronan TA. Understanding ethnic disparities in the use of total joint arthroplasty: application of the health belief model. Arthritis Rheum. 2008;59:102–108. doi: 10.1002/art.23243. [DOI] [PubMed] [Google Scholar]
- 42.Figaro MK, Williams-Russo P, Allegrante JP. Expectation and outlook: the impact of patient preference on arthritis care among African Americans. J Ambul Care Manage. 2005;28:41–48. doi: 10.1097/00004479-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/white patient differences in “willingness” to consider joint replacement. Arthritis Rheum. 2002;46:2429–2435. doi: 10.1002/art.10494. [DOI] [PubMed] [Google Scholar]
- 44.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Understanding ethnic differences in the utilization of joint replacement for osteoarthritis: the role of patient-level factors. Med Care. 2002;40:I44–I51. doi: 10.1097/00005650-200201001-00006. [DOI] [PubMed] [Google Scholar]
- 45.Allen KD, Golightly YM, Callahan LF, Helmick CG, Ibrahim SA, Kwoh CK, et al. Race and sex differences in willingness to undergo total joint replacement: the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken) 2014;66:1193–1202. doi: 10.1002/acr.22295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ibrahim SA, Hanusa BH, Hannon MJ, Kresevic D, Long J, Kent Kwoh C. Willingness and access to joint replacement among African American patients with knee osteoarthritis: a randomized, controlled intervention. Arthritis Rheum. 2013;65:1253–1261. doi: 10.1002/art.37899. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.