Abstract
Background/Aims
This was a Phase 2 study (NCT02015793) to evaluate the pharmacokinetics, safety, and efficacy of adalimumab in Chinese patients with Crohn's disease (CD).
Methods
Thirty, adult Chinese patients with CD (CD Activity Index [CDAI] 220–450; high-sensitivity [hs]-C-reactive protein [CRP] ≥3 mg/L) received double-blind adalimumab 160/80 mg or 80/40 mg at weeks 0/2, followed by 40 mg at weeks 4 and 6. An open-label extension period occurred from weeks 8–26; patients received 40 mg adalimumab every other week. Serum adalimumab concentration and change from baseline in fecal calprotectin (FC) were measured during the double-blind period. Clinical remission (CDAI <150), response (decrease in CDAI ≥70 points from baseline), and change from baseline in hs-CRP were assessed through week 26. Nonresponder imputation was used for missing categorical data and last observation carried forward for missing hs-CRP/FC values. No formal hypothesis was tested. Adverse events were monitored.
Results
Mean adalimumab serum concentrations during the induction phase were 13.9–18.1 µg/mL (160/80 mg group) and 7.5−9.5 µg/mL (80/40 mg group). During the double-blind period, higher remission/response rates and greater reductions from baseline in hs-CRP and FC were observed with adalimumab 160/80 mg compared to that with 80/40 mg. Adverse event rates were similar among all treatment groups.
Conclusions
Adalimumab serum concentrations in Chinese patients with CD were comparable to those observed previously in Western and Japanese patients. Clinically meaningful remission rates and improvement in inflammatory markers were achieved with both dosing regimens; changes occurred rapidly with adalimumab 160/80 mg induction therapy. No new safety signals were reported.
Keywords: Crohn disease, Anti-tumor necrosis factor, Adalimumab
INTRODUCTION
Crohn's disease (CD) encompasses a spectrum of clinical and pathological processes manifested by focal asymmetric, trans mural, and occasionally granulomatous inflammation that can affect any segment of the gastrointestinal tract.1
The incidence of CD in Asia is lower than that in the West, ranging from 0.14 to 1.22 cases per 100,000 people.2,3,4 However, in mainland China, the incidence rates and prevalence of CD have been increasing; therefore, the disease is no longer uncommon in China. Rapid evolution in environmental and lifestyle factors such as socioeconomic changes, industrialization, and westernization are potential causes of the rise in IBD cases in Asia.4,5,6 The site of CD in Asian patients has been reported to be broadly similar to that reported in Western studies, although complex disease behavior (defined as stricturing, penetrating, or perianal disease) is present in a high proportion of patients.2,7
Current guidelines for the management of moderate-to-severe CD in Chinese patients include the use of corticosteroids (budesonide, prednisone), immunomodulators (azathioprine [AZA], 6-mercaptopurine, methotrexate [MTX]), or 5-aminosalicylic acid, antibiotics, or nutritional therapy.8 For patients with severe disease who are refractory to or intolerant of conventional therapies, surgery or infliximab is considered. A study conducted in Chinese patients (n=14) with active CD who failed to respond to conventional therapies showed that open-label infliximab induced remission at week 14 (5.6 point decrease in Harvey-Bradshaw index),9 while another study reported a 58% (14/24) clinical remission rate after 30 weeks of infliximab therapy.10 Recently, a single center, retrospective study conducted in Chinese patients with CD (n=70) showed that 77% of patients treated with infliximab achieved remission (CDAI <150) at week 30; however, 9% of patients relapsed.11 Adalimumab (Humira™, AbbVie Inc, North Chicago, Illinois, USA) is a fully human, anti-TNF monoclonal antibody that has been shown to be effective for induction and maintenance of remission in Western and Japanese patients with moderately to severely active CD who have failed conventional therapies.12,13,14
The current study was conducted to characterize the pharmacokinetics (PK) of adalimumab following subcutaneous injection in Chinese patients with moderately to severely active CD and elevated high-sensitivity-CRP protein (hs-CRP). Efficacy and safety assessments were also performed.
METHODS
1. Patients
Male and female Chinese adults 18–70 years-old with a diagnosis of CD (confirmed by endoscopy, radiologic evaluation, and/or histology) for at least 3 months prior to baseline, elevated hs-CRP (≥3 mg/L), and moderate to severely active CD (CDAI 220 to 450) despite concurrent or prior treatment with corticosteroids and/or immunomodulators, were enrolled. Stable doses of oral corticosteroids for at least 10 days prior to baseline (≤20 mg/day prednisone or equivalent; ≤9 mg/day budesonide) and/or immunomodulators for at least 28 days prior to baseline (defined as AZA [≥0.75−3 mg/kg/day], 6-mercaptopurine [≥0.5−1 mg/kg/day], or subcutaneous/intramuscular MTX [≥15−25 mg/week]) were allowed. Concomitant steroid or immunomodulator use was not required for patients who had a history of non-response (within 1 year) or intolerance (within 5 years) to one of these therapies. Fifteen patients per study arm were considered adequate to characterize the PK of adalimumab in this patient population, and thus a sample size of 30 patients was selected.
Exclusion criteria included UC or indeterminate colitis; prior exposure to any anti-tumor necrosis factor (TNF) agent or biologics (i.e., natalizumab, efalizumab, or rituximab) that have been associated with progressive multifocal leukoencephalopathy, use of cyclosporine, tacrolimus, or mycophenolate mofetil within 60 days prior to baseline; total parenteral nutrition during screening and/or at baseline, use of any traditional Chinese medicine <14 days prior to baseline, surgical bowel resection within the past 6 months, or likely need for surgical resection in the future, positive Clostridium difficile stool assay, history of invasive infection (e.g., Listeria monocytogenes, or histoplasmosis), HIV, chronic recurring infections, active tuberculosis (TB), or history of TB infection.
2. Study Design
Study M14-232 (ClinicalTrials.gov identifier NCT02015793) was a 26-week, randomized, double-blind, multi-center trial of two adalimumab dosing regimens in Chinese patients with moderately to severely active CD. The primary objective was to evaluate the PK of adalimumab in Chinese patients with CD over time. Secondary objectives included measurement of clinical remission (CDAI <150), clinical response (CDAI decrease of at least 70 points from baseline [CR-70]), CR-100 (CDAI decrease of at least 100 points from baseline), and changes in laboratory values (hs-CRP and FC) over time. Treatment-emergent adverse events (AEs) were assessed in all patients who received at least one dose of adalimumab during the study.
The study was initiated in December 2013 and completed on February 2015 at 6 sites in China.
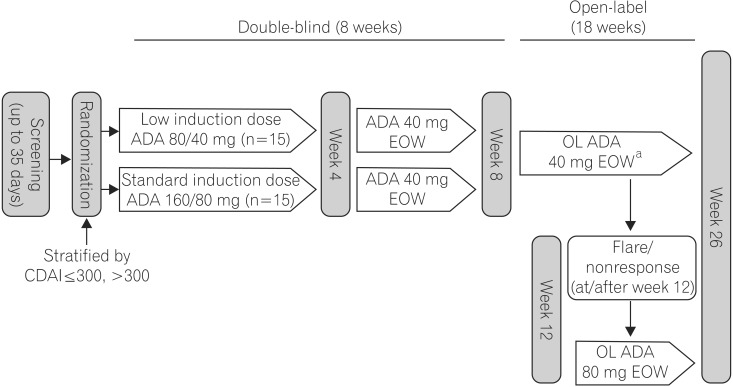
The study included an 8-week blinded phase followed by an optional 18-week open-label extension phase (Fig. 1) and a 70-day follow-up period. In the blinded phase, eligible patients were randomized 1:1 to either the standard induction or low induction adalimumab dosing regimen, with randomization stratified by CDAI (≤300 or >300). Patients randomized to the standard induction dose were treated with adalimumab 160 mg at week 0, 80 mg at week 2, and 40 mg at weeks 4 and 6, and patients randomized to the lower induction dose were treated with blinded adalimumab 80 mg at week 0, and 40 mg at weeks 2, 4, and 6. At week 8, all patients could enroll in the optional 18-week open-label extension phase to continue receiving adalimumab 40 mg every other week (EOW) up to week 24. At or after week 12, patients who experienced a disease flare (CDAI increase of ≥70 points compared to week 4 and absolute CDAI >220) or nonresponse (not achieving CR-70 on 2 consecutive visits, at least 1 week apart) could escalate their dose to adalimumab 80 mg EOW. Patients who continued to experience flares or those nonresponsive after dose escalation were to be withdrawn from the study.
Fig. 1. Study design. a, Dose escalation to 80 mg adalimumab (ADA) every other week (EOW) at/after week 12 for disease flares/non-response. OL, Open-label.
Enrolled patients were screened for TB using a QuantiFERON-TB Gold In-Tube test and chest x-ray (or chest CT scan at the investigator's discretion). Patients with positive or indeterminate TB screening results were assumed to have latent TB and were required to initiate TB prophylaxis at least 21 days prior to baseline and continue the prophylaxis regimen for the duration of the study. TB assessments were repeated at weeks 8, 16, and 26, or at the time of discontinuation from the study.
Beginning at week 4, all patients taking concomitant corticosteroids initiated a dose taper. Patients nonresponsive after initiation of the steroid taper between weeks 4 to 12 (before adalimumab dose escalation was permitted) were to be excluded from the study.
Study visits occurred at baseline (week 0), week 1, week 2, and at 2-week intervals up to week 26. Physical examinations, CDAI calculation, vital signs collection, and clinical laboratory tests were performed at study visits. Stool samples were collected for FC measurement at baseline, week 4, and week 8. FC was measured using an ELISA-based assay (DRG International Inc, Springfield, NJ, USA).
This study was performed in accordance with the International Conference on Harmonization (ICH) and Good Clinical Practice (GCP) guidelines, applicable regulations and guidelines for clinical trial conduct, and the ethical principles originating from the Declaration of Helsinki. The protocol and informed consent forms were approved by an Institutional Review Board (IRB) or Independent Ethics Committee (IEC) at each study site and patients were required to provide informed consent forms before any study-related procedures were performed.
3. PK and Immunogenicity
Blood samples were collected for measurement of serum adalimumab concentration immediately prior to dosing at baseline (week 0), weeks 1, 2, 4, 6, and 8/premature discontinuation, by using a validated ELISA method. The same methods of testing (e.g., ELISA kit) were used to measure serum levels of adalimumab and anti-adalimumab antibodies as those used for the Chinese, Japanese, and Western as the expression refers to other studies performed in China as well as in other countries. The lower limit of quantitation for adalimumab was 31.3 ng/mL in undiluted human serum and 3.13 ng/mL in diluted serum.
Anti-adalimumab antibody (AAA) was measured in serum samples immediately before dosing at baseline (week 0), weeks 4, and 8/premature discontinuation. Patients were considered to be AAA+ if they had at least one AAA concentration >20 ng/mL (confirmatory assay was performed) and if the sample was collected within 30 days after adalimumab dosing. The assay was only performed if the serum sample had adalimumab concentrations <2 µg/mL.
4. Efficacy Endpoints
Efficacy was assessed in the intent-to-treat population, which included all patients who were randomized and received at least 1 injection of adalimumab during the blinded period. The final efficacy assessment for the 8-week double-blind period was the last non-missing data obtained within 70 days after the last adalimumab dose for patients who did not enter the open-label period and prior to the first adalimumab dose in the open-label period for patients who entered the open-label period. The last non-missing data obtained within 70 days after the last adalimumab dose was used as the final efficacy assessment for the open-label phase. Clinical remission (CDAI <150) and response (CR-70 and CR-100) were assessed at week 2 and every 2 weeks up to week 26. Week 4 remission rates were calculated by use of subgroups based on corticosteroid use, immunomodulator use, hs-CRP (≤median [31.25 mg/L] or >median [31.25 mg/L]), CDAI (≤median [305] or >median [305]) and body weight (≤median [49.25 kg] or >median [49.25 kg]). Discontinuation of corticosteroids and corticosteroid-free remission rates were determined in patients who received corticosteroids at study entry. Median changes from baseline in hs-CRP were evaluated through week 26. Median changes from baseline in FC were assessed at weeks 4 and 8. Mean changes in albumin, hemoglobin, and weight were assessed through week 26.
Post hoc analyses on the proportion of patients with clinical remission (CDAI <150) and normalization of hs-CRP (hs-CRP <3 mg/L), clinical remission and 50% reduction in hs-CRP, and clinical remission and FC ≤250, ≤200, or ≤150 µg/g during the double-blind period were assessed in the intent-to-treat population.
5. Statistics
As the intent of the study was primarily to characterize the PK of adalimumab in Chinese patients, no statistical hypothesis was tested. Adalimumab trough serum concentrations were summarized by treatment group over time by descriptive statistics (n, mean, and SD). Apparent clearance values were calculated using a population PK modeling approach. Adalimumab serum concentrations in Chinese patients in this study were compared to those from past studies in Western15 and Japanese14,16 patients with CD.
All efficacy endpoints were summarized descriptively. Continuous efficacy variables were summarized as n (%), mean (SD) and median (min, max). Categorical efficacy variables were summarized as n (% [95% CI]). Nonresponder imputation was used for missing categorical assessments and for patients whose dose was escalated (from the point of dose escalation onwards). Last observation carried forward was used for missing hs-CRP and FC data and for patients whose dose was escalated (from the point of dose escalation onwards).
6. Safety
Treatment-emergent AEs were defined as events that started or worsened on or after the first dose of adalimumab up to 70 days after the last adalimumab dose for any patient who was treated with adalimumab during the blinded or open-label periods. AEs were assessed during the blinded phase (weeks 0−8) and open-label phase (weeks 8−26), and were summarized using Medical Dictionary for Regulatory Activities (MedDRA) (version 17.1).
RESULTS
1. Patient Disposition, Demographics and Baseline Characteristics
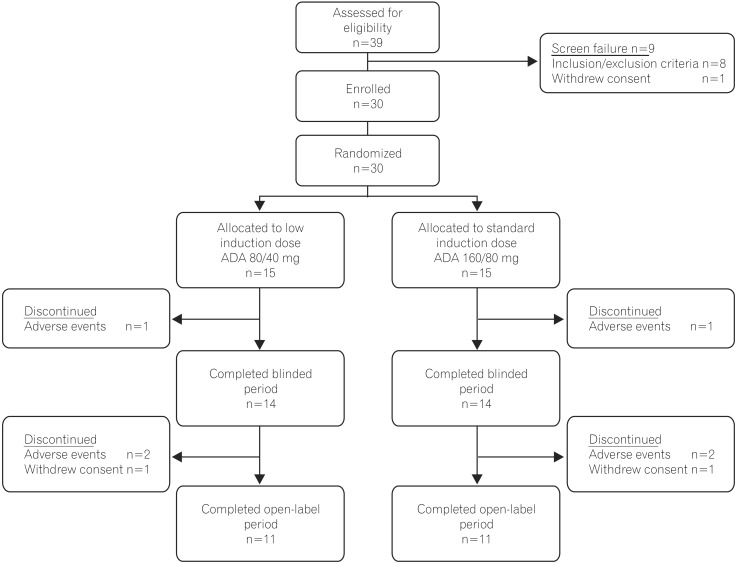
Thirty patients were enrolled in the study (n=15 each for the 80/40 mg and 160/80 mg induction dose groups) and 11/15 patients (73%) in each treatment group completed the study (Fig. 2). One patient (7%) from each of the treatment groups discontinued during the blinded period due to AEs. A total of 4/15 patients (27%) from each treatment group discontinued during the entire study, with the most common reasons for discontinuation being AEs (n=6, 20%) and withdrawal of consent (n=2, 7%).
Fig. 2. Flow diagram of patient disposition. ADA, Adalimumab. Patient disposition: number of patients enrolled, randomized, and completed the study.
Enrolled patients were mostly men (80%) and most had ileocolonic CD (60%). In the overall population, the reported duration of CD was 2.6 years, and there was a high rate (70%) of concomitant immunomodulator use (Table 1).
Table 1. Demographics and Baseline Characteristics of Patients.
| Characteristic | ADA 80/40 mg (n=15) | ADA 160/80 mg (n=15) | All patients (n=30) |
|---|---|---|---|
| Male gender | 13 (87) | 11 (73) | 24 (80) |
| Age, yrs, mean (SD) | 34 (15) | 36 (13) | 35 (14) |
| Weight, kg, mean (SD) | 52 (10) | 54 (13) | 53 (11) |
| Current smoker | 1 (7) | 0 | 1 (3) |
| Current alcohol use | 1 (7) | 1 (7) | 2 (7) |
| CD duration, yrs, mean (SD) | 1.7 (1.8) | 3.6 (4.1) | 2.6 (3.3) |
| CD location | |||
| Colonic | 2 (13) | 2 (13) | 4 (13) |
| Ileal | 3 (20) | 4 (27) | 7 (23) |
| Ileocolonica | 10 (67) | 8 (53) | 18 (60) |
| Upper diseaseb | 1 (7) | 1 (7) | 2 (7) |
| Fissures and draining fistulas | |||
| ≥1 anal/internal fissures | 0 | 2 (13) | 2 (6) |
| ≥1 draining perianal/anal fistula | 1 (7) | 1 (7) | 2 (7) |
| CDAI, mean (SD) | 320 (56) | 311 (56) | 315 (55) |
| CDAI, >300 | 8 (53) | 9 (60) | 17 (57) |
| hs-CRP, mg/L, median (min-max) | 31 (1, 119) | 32 (5, 195) | 31 (1, 195) |
| hs-CRP, ≥10 mg/L | 12 (80) | 13 (87) | 25 (83) |
| FC, µg/g, median (min, max) | 802 (128, 2756) | 945 (214, 2754) | 911 (128, 2756) |
| Albumin, g/L, mean (SD) | 37 (4) | 34 (6) | 36 (5) |
| Hematocrit, fraction, mean (SD) | 0.36 (0.06) | 0.36 (0.06) | 0.36 (0.06) |
| Concomitant medication | |||
| Immunomodulators | 10 (67) | 11 (73) | 21 (70) |
| Corticosteroids | 3 (20) | 5 (33) | 8 (27) |
| Aminosalicyclates | 3 (20) | 6 (40) | 9 (30) |
Values are presented as n (%).
aPatients with both colonic and ileal CD were categorized as ileocolonic. The locations of colonic, ileal, and ileocolonic disease do not overlap.
bA patient could have upper disease alone or in addition to disease in another category.
ADA, adalimumab; hs-CRP, high-sensitivity-CRP protein; FC, fecal calprotectin.
2. PK and Immunogenicity
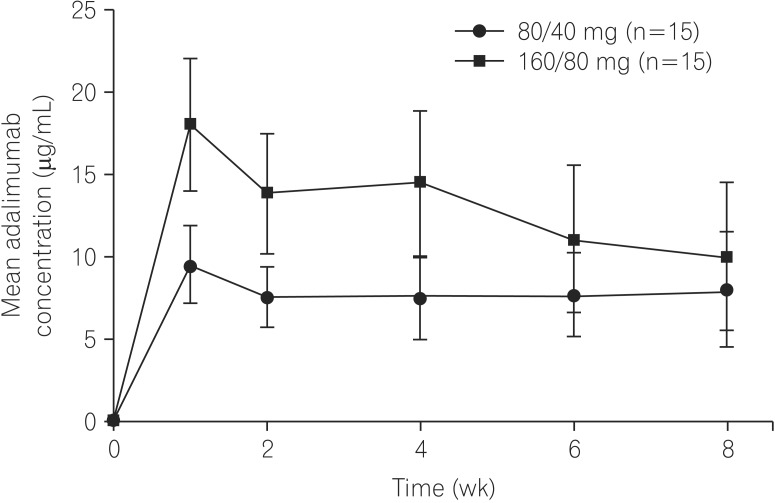
From weeks 1 to 4, mean adalimumab serum concentration was two-fold higher in patients who received the 160/80 mg induction dose (13.9−18.1 µg/mL) compared to those who received the 80/40 mg induction dose (7.5−9.5 µg/mL) (Fig. 3). At week 8, mean serum adalimumab concentrations were 8.0±3.5 µg/mL (n=14) and 10.0±4.6 µg/mL (n=12) for the 80/40 and 160/80 groups, respectively. At week 4, mean serum adalimumab levels were 14.5±4.4 µg/mL for Chinese patients (n=15) receiving 160/80 mg induction treatment. Week 8 maintenance phase mean serum adalimumab concentrations in Chinese patients (n=26) were 8.9±4.1 µg/mL. However, a significant overlap in adalimumab concentrations was observed in Chinese, Western, and Japanese patients with CD at all measurement time points. Using population PK modeling, median adalimumab clearance values in Chinese patients (0.33 [0.17−0.58] L/day) were found to be comparable to that of Western (0.39 [0.11−1.22] L/day) and Japanese (0.47 [0.13−1.25] L/day) patients.
Fig. 3. Mean adalimumab serum concentrations over time. Mean adalimumab concentrations during the double-blind period in adalimumab-treated Chinese patients with CD. Error bars represent SD.
No patient sample was found to be positive for AAA.
3. Efficacy
1) Clinical Remission and Response Rates
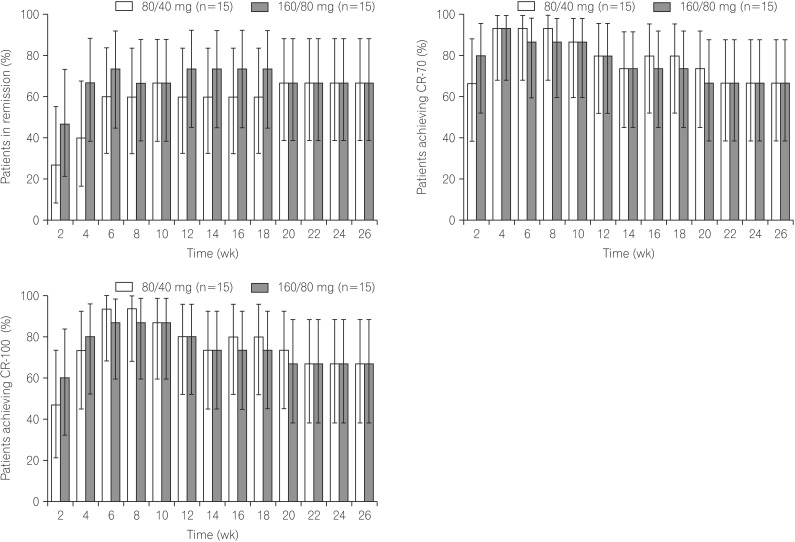
Clinically relevant remission and response were observed as early as week 2 and were sustained to week 26 (Fig. 4A–C). Numerically higher remission rates were observed in the 160/80 mg group as early as week 2 (47%) compared to that in the 80/40 mg group (27%), and this trend was sustained at all time points through week 8 (Fig. 4A). At week 2, CR-70 and CR-100 rates were higher in the 160/80 mg group than in the 80/40 mg group, and similar rates were observed through week 26 (Fig. 4B, C). Week 4 remission rates in subgroups based on baseline variables are shown in Supplementary Table 1. Due to small numbers of patients in some strata, conclusions are difficult to draw.
Fig. 4. Clinical remission, clinical response, and CDAI over time. Percentages of patients in remission (CDAI <150) over time (A). Percentages of patients achieving CR-70 (decrease from baseline CDAI of ≥70 points) over time (B). Percentages of patients achieving CR-100 (decrease from baseline CDAI of ≥100 points) over time (C). Error bars represent 95% CI. Non-responder imputation was used for data analysis.
2) Steroid-Sparing Effects
Of the patients receiving corticosteroid therapy at baseline, 7/8 (88%) discontinued corticosteroid use at week 26. Moreover, half (4/8) of baseline corticosteroid users that discontinued corticosteroid use during the study achieved remission at the end of the 8-week blinded phase, which was sustained during the open-label phase to week 26 (3/8, 38%).
3) Laboratory and Weight Assessments
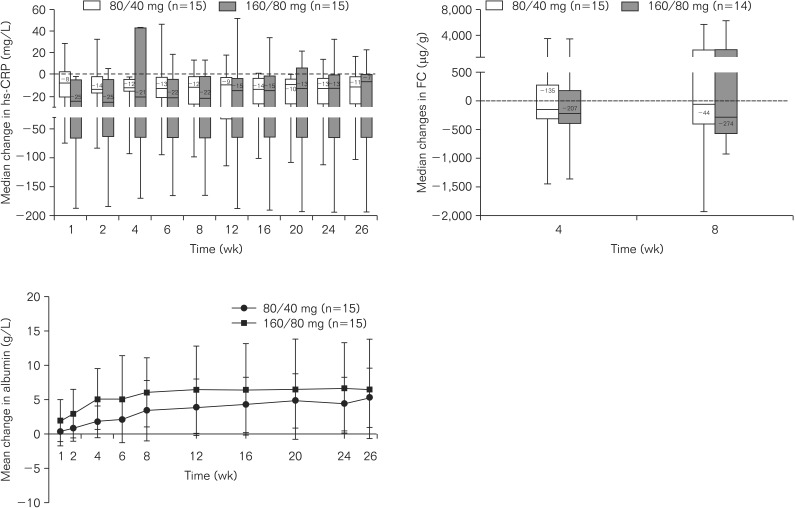
Numerically greater median decreases from baseline in hs-CRP were observed in the 160/80 mg group as early as week 1 (-25 mg/L) compared to that of the 80/40 mg group (-8 mg/L), and this trend was sustained through week 8 (Fig. 5A). Median hs-CRP remained decreased throughout the study in both induction dose groups (Fig. 5A).
Fig. 5. Changes in laboratory parameters over time. Median changes from baseline in high-sensitivity-CRP protein (hs-CRP) (A), fecal calprotectin (FC) (B), and mean changes from baseline in albumin (C) concentrations over time. Error bars represent SD. Data were analyzed using last observation carried forward.
Numerically larger median decreases from baseline in FC were observed at weeks 4 and 8 in the 160/80 mg group than in the 80/40 mg group (Fig. 5B).
Greater mean improvements from baseline in albumin were observed in the 160/80 mg group as early as week 1 (2.0 g/L) compared to those of the 80/40 mg group (0.3 g/L), and were sustained through week 26 (Fig. 5C). Mean increases from baseline in body weight were similar in both groups at week 8 (160/80 group, 1.9 kg vs. 80/40 group, 2.3 kg), and were sustained through week 26 (3.2 kg vs. 3.5 kg). Mean hemoglobin levels also improved from baseline in both groups at week 8 (160/80 mg group, 5.3 g/L vs. 80/40 mg group, 4.0 g/L), and were sustained through week 26 (160/80 mg group, 8.3 g/L vs. 80/40 mg group, 11.8 g/L).
4) Clinical Remission and Decreased Inflammation
During the double-blind treatment period, numerically more patients in the 160/80 mg group achieved clinical remission and normalized hs-CRP values (hs-CRP <3 mg/L) from weeks 4−8 than in the 80/40 mg group. In a separate post hoc analysis, 46.7% of patients (7/15) receiving 160/80 mg induction achieved clinical remission and a 50% reduction in hs-CRP at week 2. The proportion of patients achieving clinical remission and a 50% reduction in hs-CRP was numerically greater in the 160/80 mg group than the 80/40 mg group from weeks 2−6. At week 8, the proportion of patients with clinical remission and 50% reduction in hs-CRP was 40% (6/15) in both treatment groups (Supplemental Table 2). More patients in the 160/80 mg group achieved remission than in the 80/40 mg group (26.7 vs. 6.7%, respectively) and had FC values ≤250, ≤200, or ≤150 µg/g at week 4. Similar results were observed at week 8 (Supplemental Table 3).
5) Dose Escalation
Three patients dose escalated to adalimumab 80 mg EOW during the study. One patient (7%) from the 80/40 mg group dose escalated at week 22, and 2 patients (13%) dose escalated from the 160/80 mg group at weeks 12 and 20. One of the 2 patients from the 160/80 mg group with dose escalation achieved clinical remission at week 26.
4. Safety
The mean duration of exposure to adalimumab during the entire study was similar for the 80/40 mg (154±53 days) and 160/80 mg groups (155±52 days), and the mean total dose of adalimumab administered was 483±154 mg and 621±149 mg, respectively. During the double-blind and open-label phases, the percentage of patients who experienced AEs was comparable between the 80/40 mg group and 160/80 mg group (Table 2). During the study, 5/30 patients (17%) experienced serious AEs including worsening of CD and gastrointestinal TB. During the open-label period, serious AEs were experienced by 1 patient (8%) in the 80/40 mg group and 2 patients (14%) in the 160/80 mg group, and infections occurred in 2 patients (15%) in the 80/40 mg group and in 1 patient (8%) in the 160/80 mg group. Leukopenia (6/30, 20%), worsening CD (4/30, 13%), and pyrexia (4/30, 13%) were the most frequently reported AEs in both dose groups during the entire study. Of the 6 patients who developed leukopenia during the study, 5 patients received concomitant AZA, mesalazine, or both medications, and 1 patient had a medical history of leukopenia/neutropenia of unknown cause. One patient (7%) in the 160/80 mg group developed a severe AE of active gastrointestinal TB during the blinded phase, which led to discontinuation from the study. This patient also developed multiple AEs including infection, serious infection, and serious AEs, and had received prior and concomitant medications for CD including prednisone, MTX, and thalidomide. During the open-label period, 1 patient (8%) in the 80/40 mg group and 2 patients (14%) in the 160/80 mg group developed latent TB, defined as a patient with a positive Mycobacterium TB test but with negative results from a CT scan and/or gamma-interferon release assay. Overall, no deaths, malignancy, or demyelinating disorder was reported during the entire study.
Table 2. Treatment-Emergent Adverse Events (AE).
| Variable | Double-blind (Wk 0−8) | Open-label (Wk 8−26) | ||
|---|---|---|---|---|
| ADA 80/40 mg (n=15) | ADA 160/80 mg (n=15) | ADA 80/40 mg (n=13) | ADA 160/80 mg (n=14) | |
| AE | 6 (40) | 7 (47) | 7 (54) | 7 (50) |
| Serious AE | 1 (7) | 1 (7) | 1 (8) | 2 (14) |
| AE leading to discontinuation | 2 (13) | 1 (7) | 1 (8) | 2 (14) |
| Severe AE | 0 | 1 (7) | 0 | 1 (8) |
| AE with reasonable possibility of being related to study drug | 3 (20) | 6 (40) | 5 (39) | 6 (43) |
| Infection | 0 | 1 (7) | 2 (15) | 1 (8) |
| Serious infection | 0 | 1 (7) | 0 | 0 |
| Opportunistic infection (excluding oral candidiasis and TB) | 0 | 0 | 0 | 0 |
| TB (active) | 0 | 1 (7) | 0 | 0 |
| TB (latent) | 0 | 0 | 1 (7) | 2 (14) |
| Lymphoma | 0 | 0 | 0 | 0 |
| NMSC | 0 | 0 | 0 | 0 |
| Malignancy other than lymphoma, NMSC, HSTCL, melanoma, or leukemia | 0 | 0 | 0 | 0 |
| Demyelinating disorder | 0 | 0 | 0 | 0 |
| Death | 0 | 0 | 0 | 0 |
Values are presented as n (%).
ADA, adalimumab; TB, tuberculosis; NMSC, Non-melanoma skin cancer; HSTCL, hepatosplenic T-cell lymphoma.
DISCUSSION
Anti-TNF therapies are being studied for multiple inflammatory disorders17,18,19,20 in the Chinese population, including patients with CD.9,11 However, this is the first randomized trial designed to examine the PK, efficacy, and safety of adalimumab in Chinese patients with CD. In the current study, we examined the PK, efficacy, and safety of adalimumab in Chinese patients with moderately to severely active CD and elevated hs-CRP treated with two different induction dosing regimens of adalimumab and maintenance therapy through week 26. Elevated hs-CRP, a non-specific inflammatory marker, is associated with disease activity in CD,21,22 and was used to identify symptoms due to inflammation in the absence of performing endoscopy in this trial. Patients enrolled in this trial weighed similar to patients enrolled in the Japanese adalimumab trial14 but were approximately 20 kg lighter than patients enrolled in the trials conducted in Western countries.12,13,23 Compared to the patients enrolled in the Western and Japanese adalimumab CD trials, the Chinese patients enrolled in this study had a markedly higher baseline CRP value (which is not unexpected given the inclusion criterion requiring elevated CRP in this trial), shorter reported duration of disease, and a higher rate of concomitant immunomodulator use. These factors may have contributed to the higher remission and response rates observed in this trial compared to that in previous Western and Japanese CD trials.12,13,14
In this relatively small sample set, the PK of adalimumab was assessed during the first 8 weeks of the study. Although serum adalimumab concentrations reported in Western and Japanese patients at induction (12.6±5.3 µg/mL, n=71 and 12.4±4.5 µg/mL, n=33, respectively)14,15,16 and maintenance (6.9±3.6 µg/mL Western patients; 6.5±2.5 µg/mL for Japanese patients)14,15,16 were slightly lower than those in the Chinese patients in this study, the serum adalimumab concentrations observed in Chinese patients with CD during the induction and maintenance phases in this study overlapped with those observed in Western and Japanese patients with CD who received similar doses, in spite of the differences in baseline characteristics observed in these different populations. In addition, Chinese patients had similar adalimumab clearance values to the Western and Japanese populations, supporting the use of the same doses of adalimumab that have been tested and approved in other patient populations with CD in Chinese patients. Currently, for adults with moderately to severely active CD, the approved adalimumab induction dosing regimen is 160 mg at week 0 and 80 mg at week 2 in the United States, Canada, and Japan, followed by maintenance dosing of 40 mg EOW. No patient samples were positive for AAA in this trial. Low rates of immunogenicity have been reported in previous adalimumab trials in Western and Japanese patients with CD.14,24
Clinically relevant remission and response were observed as early as week 2 and were maintained throughout the trial. More patients in the higher 160/80 mg dose group achieved remission at early time points (weeks 2−6) than in the 80/40 mg group. These findings are consistent with observations from Western (CLASSIC-I trial) and Japanese trials demonstrating that treatment with the 160/80 mg adalimumab induction dosing regimen results in greater rates of remission than the 80/40 mg dose.14,23 In addition, the current findings show that maintenance therapy with 40 mg EOW adalimumab provides clinical benefit for Chinese patients with CD, consistent with results from previous trials in Western (CLASSIC-II, CHARM, EXTEND) and Japanese patients.12,13,14,24 The mean clinical remission rates observed in this trial were higher than those observed in trials of Western (CLASSIC-I and CHARM trials) and Japanese patients with CD.14,23,24 Possible reasons for the higher remission rates include the shorter disease duration and higher baseline hs-CRP values in Chinese patients in this study, both of which were found to be predictors of response in post hoc analyses of CHARM.25 Furthermore, the average weight of Chinese patients with CD in this study was lower than that of both the Western and Japanese patients in prior clinical trials. This may have contributed to both the higher serum concentrations and higher clinical remission rates observed. However, it is important to mention that since this trial did not have patients randomized to placebo, a treatment effect size could not be determined. Therefore, any differences observed in this trial should be interpreted with caution.
hs-CRP and FC are inflammatory biomarkers that are used to assess disease activity in IBD. Chronic inflammation in CD is marked owing to increased hs-CRP, and has been shown to be a prognostic marker for poor outcome.21,22,26,27 FC is elevated in patients with CD, and is correlated with endoscopic disease activity.28 In this study, induction and maintenance adalimumab therapy improved inflammatory responses, as demonstrated by reductions in hs-CRP as early as week 1 and decreased FC at week 4. The higher 160/80 mg dose had a numerically greater effect on hs-CRP reduction between weeks 1−12 compared to the 80/40 mg dose, and reductions in FC were numerically greater with the 160/80 mg dose compared to that with the 80/40 mg dose during the blinded phase. Ongoing maintenance therapy with adalimumab 40 mg EOW was associated with a sustained reduction in hs-CRP through week 26. Post hoc analyses also demonstrated that 1/3 of patients achieved clinical remission and normalized hs-CRP values after 4 weeks of treatment with the standard induction dose and approximately 1/4 of patients achieved clinical remission and decreased FC levels by week 4 of treatment, confirming that adalimumab induction treatment in patients with CD produced symptomatic relief as measured by CDAI as well as objective reductions in inflammatory burden.
Overall, our findings are consistent with those of other trials conducted in Chinese patients that showed the effectiveness and safety of adalimumab for treatment of rheumatoid arthritis and ankylosing spondylitis.17,18 Multiple global trials conducted in different patient populations with CD and other indications have shown a consistent safety profile of adalimumab.29,30 No new safety signals were identified in Chinese patients with CD treated with adalimumab, nor were any cases of malignancy, demyelinating disease or death reported. One case of active TB and 3 cases of latent TB infection were diagnosed during the trial. These findings, along with the fact that TB is endemic in China, underscore the need to closely monitor for TB in Chinese CD patients receiving immunosuppressive treatment.31 Close monitoring for the development of TB infection is recommended for patients prior to initiating therapy, and periodically while receiving adalimumab therapy.32
This study has several limitations. This was a Phase 2 study with relatively few patients enrolled, thus, a larger Phase 3 study is ongoing to evaluate the efficacy and safety of adalimumab in the Chinese population (ClinicalTrials.gov identifier NCT02499783). Endoscopic assessment of disease activity by ileocolonoscopy was not performed in this study; as a result, mucosal healing was not assessed.
Data from this Phase 2 study confirm that the PK profile, including clearance, of adalimumab in Chinese patients with moderately to severely active CD is similar to that observed in trials from other regions, both East and West. In addition, similar to the data observed in Western and Japanese trials, adalimumab treatment resulted in rapid clinical and biological responses, particularly with the 160/80 mg induction dose, and ongoing treatment with adalimumab 40 mg EOW resulted in maintenance of clinical remission and response, and improvement in inflammatory biomarkers to week 26.
ACKNOWLEDGEMENTS
AbbVie funded the study. AbbVie participated in the study design, data collection, data management, data analysis, review and approval of the publication. All authors were involved in the design of the analyses reported in the manuscript, interpretation of the data, and critical review and revision of each draft of the manuscript. All authors had access to relevant data and approved the content of the manuscript for submission. Medical writing support was provided by Adebusola A. Ajibade, PhD, of AbbVie Inc.
Footnotes
Financial support: AbbVie funded the study.
Conflict of interest: Kamm MA has been a consultant to AbbVie and has received speaker fees and research support from AbbVie. Travis S conducted no industry consulting during his time as ECCO President, but since that time has acted as advisor to, lecturer for, or been in receipt of research support from AbbVie, Boerhinger, Cosmo, Ferring, Genentech, GSK, Novo Nordisk, NPS, Pfizer, Takeda, Topivert and VHSquared. Robinson AM, Mostafa NM, Wallace K, Shapiro M, Li Y, Thakkar RB, AbbVie employees, may own AbbVie stock and/or options.
Supplementary Materials
Week 4 Remission Rates by Subgroups (Nonresponder Imputation Analysis)
Proportion of Patients With Clinical Remission (CDAI <150) and Normalization of High-sensitivity-CRP (hs-CRP <3 mg/L), or Clinical Remission and 50% Reduction of hs-CRP During the Double-blind Phase (Nonresponder Imputation Analysis)
Proportion of Patients With Clinical Remission (CDAI <150) and Fecal Calprotectin ≤250, ≤200, and ≤150 µg/g at weeks 4 and 8 (Nonresponder Imputation Analysis)
References
- 1.Hanauer SB, Sandborn W Practice Parameters Committee of the American College of Gastroenterology. Management of Crohn's disease in adults. Am J Gastroenterol. 2001;96:635–643. doi: 10.1111/j.1572-0241.2001.3671_c.x. [DOI] [PubMed] [Google Scholar]
- 2.Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn's and colitis epidemiology study. Gastroenterology. 2013;145:158–165. doi: 10.1053/j.gastro.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Zeng Z, Zhu Z, Yang Y, et al. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong Province, China: a prospective population-based study. J Gastroenterol Hepatol. 2013;28:1148–1153. doi: 10.1111/jgh.12164. [DOI] [PubMed] [Google Scholar]
- 4.Zhao J, Ng SC, Lei Y, et al. First prospective, population-based inflammatory bowel disease incidence study in mainland of China: the emergence of "western" disease. Inflamm Bowel Dis. 2013;19:1839–1845. doi: 10.1097/MIB.0b013e31828a6551. [DOI] [PubMed] [Google Scholar]
- 5.Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012;27:1266–1280. doi: 10.1111/j.1440-1746.2012.07150.x. [DOI] [PubMed] [Google Scholar]
- 6.Ooi CJ, Makharia GK, Hilmi I, et al. Asia Pacific Consensus Statements on Crohns disease. Part 1: Definition, diagnosis, and epidemiology: (Asia Pacific Crohn's Disease Consensus-Part 1) J Gastroenterol Hepatol. 2016;31:45–55. doi: 10.1111/jgh.12956. [DOI] [PubMed] [Google Scholar]
- 7.Ng SC, Zeng Z, Niewiadomski O, et al. Early course of inflammatory bowel disease in a population-based inception Cohort study from 8 countries in Asia and Australia. Gastroenterology. 2016;150:86–95. doi: 10.1053/j.gastro.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Ooi CJ, Makharia GK, Hilmi I, et al. Asia-Pacific consensus statements on Crohn's disease. Part 2: Management. J Gastroenterol Hepatol. 2016;31:56–68. doi: 10.1111/jgh.12958. [DOI] [PubMed] [Google Scholar]
- 9.Zheng JJ, Zhi P, Wang YM, et al. Short-term study of infliximab treatment for Crohn's disease in China. J Dig Dis. 2011;12:105–109. doi: 10.1111/j.1751-2980.2011.00485.x. [DOI] [PubMed] [Google Scholar]
- 10.Xiao YL, Chen BL, He Y, et al. The clinical and endoscopic efficacy of step-up and top-down infliximab therapy in Crohn's disease. Zhonghua Nei Ke Za Zhi. 2012;51:100–103. [PubMed] [Google Scholar]
- 11.Zhou Y, He H, Wang P, et al. Infliximab for the treatment of Crohn's disease: efficacy and safety in a Chinese single-center retrospective study. Eur J Gastroenterol Hepatol. 2015;27:1270–1275. doi: 10.1097/MEG.0000000000000447. [DOI] [PubMed] [Google Scholar]
- 12.Colombel JF, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn's disease: the CHARM trial. Gastroenterology. 2007;132:52–65. doi: 10.1053/j.gastro.2006.11.041. [DOI] [PubMed] [Google Scholar]
- 13.Rutgeerts P, Van Assche G, Sandborn WJ, et al. Adalimumab induces and maintains mucosal healing in patients with Crohn's disease: data from the EXTEND trial. Gastroenterology. 2012;142:1102–1111. doi: 10.1053/j.gastro.2012.01.035. [DOI] [PubMed] [Google Scholar]
- 14.Watanabe M, Hibi T, Lomax KG, et al. Adalimumab for the induction and maintenance of clinical remission in Japanese patients with Crohn's disease. J Crohns Colitis. 2012;6:160–173. doi: 10.1016/j.crohns.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 15.Chiu YL, Rubin DT, Vermeire S, et al. Serum adalimumab concentration and clinical remission in patients with Crohn's disease. Inflamm Bowel Dis. 2013;19:1112–1122. doi: 10.1097/MIB.0b013e3182813242. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe M, Hibi T, Mostafa NM, et al. Long-term safety and efficacy of adalimumab in Japanese patients with moderate to severe Crohn's disease. J Crohns Colitis. 2014;8:1407–1416. doi: 10.1016/j.crohns.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 17.Huang F, Zhang FC, Bao CD, et al. Adalimumab plus methotrexate for the treatment of rheumatoid arthritis: a multi-center randomized, double-blind, placebo-controlled clinical study. Zhonghua Nei Ke Za Zhi. 2009;48:916–921. [PubMed] [Google Scholar]
- 18.Huang F, Gu J, Zhu P, et al. Efficacy and safety of adalimumab in Chinese adults with active ankylosing spondylitis: results of a randomised, controlled trial. Ann Rheum Dis. 2014;73:587–594. doi: 10.1136/annrheumdis-2012-202533. [DOI] [PubMed] [Google Scholar]
- 19.Huang F, Zhang J, Zheng Y, et al. A multicenter, double-blind, randomized, placebo-controlled clinical trial of etanercept treatment of Chinese patients with active ankylosing spondylitis. Zhonghua Nei Ke Za Zhi. 2011;50:1043–1047. [PubMed] [Google Scholar]
- 20.Huang F, Zhang J, Huang JL, et al. A multicenter, double-blind, placebo-controlled, randomized, phase III clinical study of etanercept in treatment of ankylosing spondylitis. Zhonghua Nei Ke Za Zhi. 2010;49:741–745. [PubMed] [Google Scholar]
- 21.Vermeire S, Van Assche G, Rutgeerts P. C-reactive protein as a marker for inflammatory bowel disease. Inflamm Bowel Dis. 2004;10:661–665. doi: 10.1097/00054725-200409000-00026. [DOI] [PubMed] [Google Scholar]
- 22.Zilberman L, Maharshak N, Arbel Y, et al. Correlated expression of high-sensitivity C-reactive protein in relation to disease activity in inflammatory bowel disease: lack of differences between Crohn's disease and ulcerative colitis. Digestion. 2006;73:205–209. doi: 10.1159/000094531. [DOI] [PubMed] [Google Scholar]
- 23.Hanauer SB, Sandborn WJ, Rutgeerts P, et al. Human anti-tumor necrosis factor monoclonal antibody (adalimumab) in Crohn's disease: the CLASSIC-I trial. Gastroenterology. 2006;130:323–333. doi: 10.1053/j.gastro.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 24.Sandborn WJ, Hanauer SB, Rutgeerts P, et al. Adalimumab for maintenance treatment of Crohn's disease: results of the CLASSIC II trial. Gut. 2007;56:1232–1239. doi: 10.1136/gut.2006.106781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schreiber S, Reinisch W, Colombel JF, et al. Subgroup analysis of the placebo-controlled CHARM trial: increased remission rates through 3 years for adalimumab-treated patients with early Crohn's disease. J Crohns Colitis. 2013;7:213–221. doi: 10.1016/j.crohns.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 26.Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut. 2006;55:426–431. doi: 10.1136/gut.2005.069476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henriksen M, Jahnsen J, Lygren I, et al. C-reactive protein: a predictive factor and marker of inflammation in inflammatory bowel disease. Results from a prospective population-based study. Gut. 2008;57:1518–1523. doi: 10.1136/gut.2007.146357. [DOI] [PubMed] [Google Scholar]
- 28.Mosli MH, Zou G, Garg SK, et al. C-reactive protein, fecal calprotectin, and stool lactoferrin for detection of endoscopic activity in symptomatic inflammatory bowel disease patients: a systematic review and meta-analysis. Am J Gastroenterol. 2015;110:802–819. doi: 10.1038/ajg.2015.120. [DOI] [PubMed] [Google Scholar]
- 29.Colombel JF, Sandborn WJ, Panaccione R, et al. Adalimumab safety in global clinical trials of patients with Crohn's disease. Inflamm Bowel Dis. 2009;15:1308–1319. doi: 10.1002/ibd.20956. [DOI] [PubMed] [Google Scholar]
- 30.Burmester GR, Panaccione R, Gordon KB, McIlraith MJ, Lacerda AP. Adalimumab: long-term safety in 23 458 patients from global clinical trials in rheumatoid arthritis, juvenile idiopathic arthritis, ankylosing spondylitis, psoriatic arthritis, psoriasis and Crohn's disease. Ann Rheum Dis. 2013;72:517–524. doi: 10.1136/annrheumdis-2011-201244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang L, Zhang H, Ruan Y, et al. Tuberculosis prevalence in China, 1990-2010; a longitudinal analysis of national survey data. Lancet. 2014;383:2057–2064. doi: 10.1016/S0140-6736(13)62639-2. [DOI] [PubMed] [Google Scholar]
- 32.HUMIRA [package insert] North Chicago, IL: AbbVie Inc.; 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Week 4 Remission Rates by Subgroups (Nonresponder Imputation Analysis)
Proportion of Patients With Clinical Remission (CDAI <150) and Normalization of High-sensitivity-CRP (hs-CRP <3 mg/L), or Clinical Remission and 50% Reduction of hs-CRP During the Double-blind Phase (Nonresponder Imputation Analysis)
Proportion of Patients With Clinical Remission (CDAI <150) and Fecal Calprotectin ≤250, ≤200, and ≤150 µg/g at weeks 4 and 8 (Nonresponder Imputation Analysis)