Abstract
Study Objectives:
Obstructive sleep apnea (OSA) is the single most important preventable medical cause of excessive daytime sleepiness (EDS) and driving accidents. OSA may also adversely affect work performance through a decrease in productivity, and an increase in the injury rate. Nevertheless, no systematic review and meta-analysis of the relationship between OSA and work accidents has been performed thus far.
Methods:
PubMed, PsycInfo, Scopus, Web of Science, and Cochrane Library were searched. Out of an initial list of 1,099 papers, 10 studies (12,553 participants) were eligible for our review, and 7 of them were included in the meta-analysis. The overall effects were measured by odds ratios (OR) and 95% confidence intervals (CI). An assessment was made of the methodological quality of the studies. Moderator analysis and funnel plot analysis were used to explore the sources of between-study heterogeneity.
Results:
Compared to controls, the odds of work accident was found to be nearly double in workers with OSA (OR = 2.18; 95% CI = 1.53–3.10). Occupational driving was associated with a higher effect size.
Conclusions:
OSA is an underdiagnosed nonoccupational disease that has a strong adverse effect on work accidents. The nearly twofold increased odds of work accidents in subjects with OSA calls for workplace screening in selected safety-sensitive occupations.
Commentary:
A commentary on this article appears in this issue on page 1171.
Citation:
Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N. Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-analysis. SLEEP 2016;39(6):1211–1218.
Keywords: excessive daytime sleepiness, injury, mean effect size, meta-analysis, obstructive sleep apnea, safety, systematic review, work accident, workplace
Significance.
This is the first systematic review and meta-analysis of studies about the relationship between obstructive sleep apnea (OSA) and work accidents. Workers with OSA have a nearly doubled risk of having an accident at work. Until now there was a large consensus about this concept, but our study shows how urgent the need for high-quality studies on this issue is. Screening for OSA in the workplace may help to prevent work accidents.
INTRODUCTION
Obstructive sleep apnea (OSA) is an underdiagnosed1 chronic disease characterized by recurrent episodes of apneas and hypopneas during sleep, associated with repetitive episodes of intermittent hypoxemia, intrathoracic pressure changes, arousals, and excessive daytime sleepiness (EDS).2
A recent study estimates the prevalence of moderate to severe OSA (≥ 15 events/h) at 23.4% in women and 49.7% in men age 40 years or older.3 Patients with untreated OSA are at significantly increased risk of cardiovascular, metabolic, neurocognitive disease4–6 and motor vehicle accidents (MVAs).7 It has been recently estimated that 7% of road traffic injuries for a population of male drivers involved in MVAs are attributable to OSA.8
OSA may also adversely affect work performance, work processes, and business in general. Studies show that it is associated with an increase in the injury rate,9,10 a decrease in productivity,11 and has a substantial adverse effect on economic systems.12,13
Given its associated morbidity, and the effectiveness of treatment, identification of patients with OSA is an important public health issue.14,15 In the United States, to prevent accidents and related injuries in driving workers, a protocol for the screening and monitoring of commercial vehicle drivers with a clinical suspicion or diagnosis of OSA has been validated.16 With a wider target, extended to all drivers, the European Commission recently recommended mandatory testing for OSA and EDS, in all European countries, before a driver's license is granted or renewed.17
Nevertheless, so far there are no systematic analyses of the literature on OSA and accidents at work. Previous review analyses were narrative18,19 or included studies adopting heterogeneous case definitions (e.g., snoring,20–22 EDS,22–24 low quantity24–26 or low quality of sleep25) and/or a number of different diagnostic criteria (self-reporting of symptoms or instrumental monitoring). Although there is a lack of decisive evidence that OSA increases the risk of accidents at work, some companies have already started health promotion programs regarding OSA.27 The elevated prevalence of OSA and the high incidence of work accidents make it vital to pinpoint the relationship between the two phenomena.
The aim of our research was to quantify the risk of occupational accidents associated with OSA, through a systematic review and a meta-analysis of the literature.
METHODS
We followed the guidelines developed by the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) group.28
Search Strategy
We systematically searched PubMed, PsycInfo, Scopus, Web of Science, and the Cochrane Library. All pre-September 2015 literature in English, Italian, French, Spanish, and Portuguese was included. The overall search strategy combined keywords from population (professional drivers OR occupational OR truck OR lorry OR commercial OR taxi OR bus), workplace (occupational OR worker OR working OR job OR employment OR occupational diseases), (risk OR relative risk), diagnosis (sleep apnea syndrome OR apnea OR obstructive sleep apnea) and endpoint (accidents OR safety OR injuries). In addition, we manually searched for additional published articles.
Selection of Published Studies
Two independent investigators (SG and OG) first reviewed all titles/abstracts to identify potentially relevant articles. They then performed the study selection, based on a full-text review, according to inclusion/exclusion rules. Disagreements were resolved by discussion. When full manuscript texts were not retrievable, the corresponding authors were contacted directly. All the empirical studies (cross-sectional, prospective, case-control, and quasi-experimental) were included. Studies on the frequency of accidents in the workplace (including traffic accidents involving professional drivers) were selected if they involved adult workers (age 18 y or older) with OSA in whom the condition had been diagnosed using polygraphy, i.e., portable, limited channel devices; polysomnography (PSG), i.e., full, multiparametric test; or standardized questionnaires, and compared with a control group of subjects not affected by OSA. In the selected studies, subjects with others sleep disorders, medical or other conditions, or who consumed drugs, alcohol, or other substances that provoke EDS were excluded. We excluded studies concerning accidents occurring outside of work, or not specifically regarding workers; studies based on driving simulators; studies regarding all breathing disorders during sleep not specifically diagnosed as OSA, studies that failed to distinguish different sleep disorders or that failed to diagnose OSA using one of the aforementioned methods; and studies analyzing the prevalence of sleep disorders without reference to accidents at work. Finally, we excluded all secondhand studies, such as systematic reviews or meta-analyses.
Selected studies were included in the systematic review. Two meta-analyses were made: the first including cases of suspected OSA (diagnosis performed by a validated questionnaire), the second limited to studies in which diagnosis was confirmed using instrumental techniques (polygraphy or PSG).
Assessment of the Methodological Quality of the Selected Studies
Two authors (OG and SG) assessed each study independently by applying the Newcastle-Ottawa scale (NOS).29 This inventory, which is used to check the quality of nonrandomized studies, is based on three broad perspectives: the study and control group selection criteria, the comparability of the groups, and ascertainment of the exposure/outcome of interest. Disagreement on quality assessment was resolved by discussion and consensus finding.
Data Extraction
The following data were extracted for each study: general data (study design, year of publication), type of job and characteristics, country, mean age of workers; number of subjects, diagnostic criteria for OSA. Other risk factors and outcomes (accidents) were obtained independently by two reviewers (OG and NM), who also calculated the odds ratios (OR) and the corresponding confidence intervals (95% CIs) when they were not reported, for every study included. Disagreement was resolved by discussion and consensus finding, and the opinion of a third reviewer (SG).
Quantitative Data Synthesis
Data concerning effect sizes were extracted from each article. Most of the studies reported the OR as the effect size. The other effect size estimates were standardized to the OR. We reported results according to a random-effect model, based on the assumption that the effects being estimated in the different studies were not identical, but followed some distribution.
Heterogeneity among studies was assessed by visual inspection of the forest plot and by using a standard chi-square test with a significance level of alpha = 0.01.30 The percentage of heterogeneity among effect size in the various studies was quantified by I2, with an I2 of 25%, 50%, and 75% corresponding to a small, medium, and large degree of heterogeneity, respectively.31
Moderator analysis was performed to analyze the source of heterogeneity in the different study results. Moderator analysis with categorical models analogous to analysis of variance was carried out to ascertain whether coded study characteristics systematically predict variation in effect sizes across studies. Categories included in the a priori model were: type of occupational accident (traffic accident/other work injuries); type of work (commercial vehicle drivers/bus drivers/others); method of diagnosis (questionnaire/PSG). Publication bias was evaluated using the funnel plot32 and was quantified by the Egger test.33
Analyses were performed with Comprehensive Meta-Analysis, version 2.2.064 (Biostat, Inc. Englewood, NJ 07631 USA) software. Moderator analysis and publication bias analysis were conducted using the statistical R program.
RESULTS
Our search strategy yielded a total of 1,099 studies (Figure 1). There were 794 papers that were discarded because they were not related to the research, 33 records were duplicate papers, and 241 studies were not empirical. From the remaining 31 papers we had to discard 5 studies because they did not distinguish OSA from other sleep disorders, 7 because diagnosis was based on non-standardized questionnaires, 6 because they did not report work-related accidents, and 3 because OR was not reported nor calculable. The final sample for systematic review comprised 10 studies, with a total of 12,553 participants. Seven studies were cross-sectional, 3 were case-control. Sample sizes ranged from 87 to 6,933 workers. Quality of studies, assessed with NOS method, was often low (Table 1).
Figure 1.
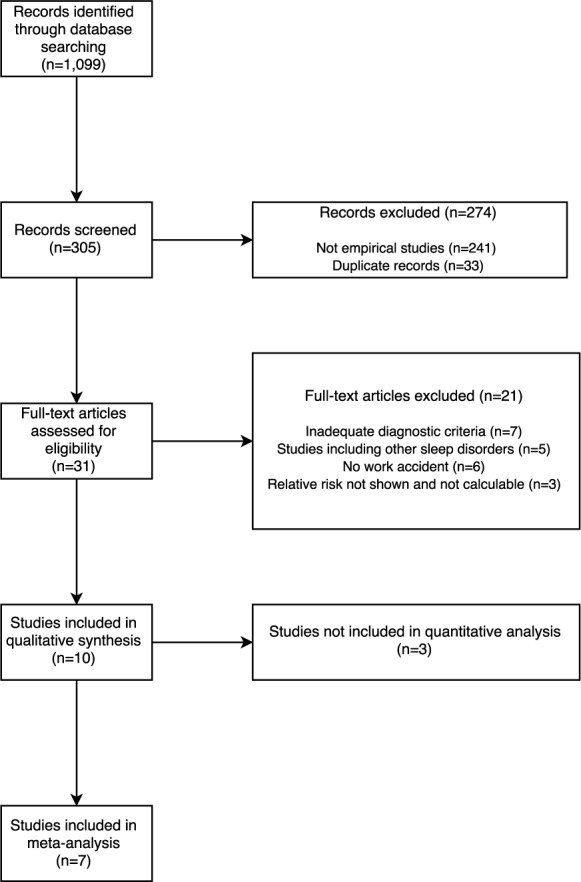
Article selection algorithm.
Table 1.
Systematic analysis and study characteristics.
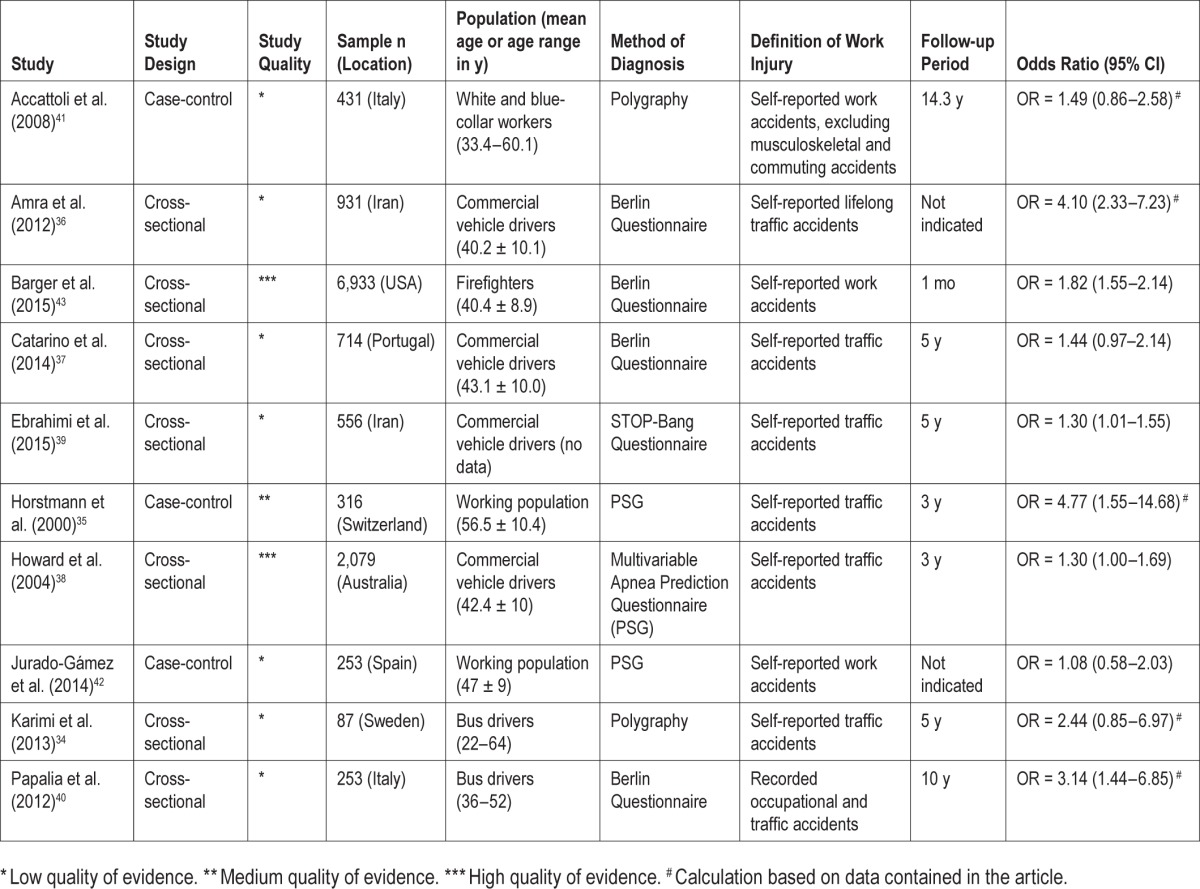
Most studies calculated the OR and 95% CI; some studies did not report the OR and 95% CI that were calculated from the number or the frequency of accidents in workers affected by OSA and in controls. One study evaluated the relative risk34 and another study reported the chi square value of a comparison of workers with OSA and those without OSA.35 In one study,36 an incorrect OR value was recalculated. The different effect sizes were then standardized to the unadjusted OR in the meta-analysis.
Most of the included studies34–40 regarded work-related traffic accidents; the others41–43 comprised all occupational injuries. In most cases, the workers were professional drivers, and in one study they were firefighters.43 The three case-control studies38,44,45 recruited observations in outpatient clinics; occupations were then mixed and included both high- and low-risk jobs. The study of Horstmann et al.35 investigating traffic accidents occurring during the previous 3 y, observed up to a 15-fold increase of the accident rate per 1 million driven km in the group with severe OSA compared to normal, and dropping of the motor vehicle accident rate after appropriate treatment of OSA. In two other case-control studies, the increase of accident rate in the OSA group was not significant.
The recall period varied greatly, ranging from 1 mo in the study of Barger et al.43 to more than 14 y41 or the whole working life in others.36,42 In addition, the accident rate greatly varied, from a low 1.74 per 100 workers per year in Italian white and blue collar workers,41 to approximately 10% per month in US firefighters.43
The occurrence of accidents was generally self-reported with reference to the previous 3 or 5 y, more rarely drawn from accident recording,40 or compared to them.43 All studies showed high prevalence of OSA and EDS, associated with higher odds of falling asleep at the wheel or having accidents and near-miss accidents (Table 1).
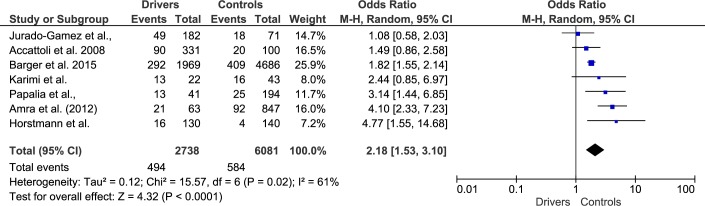
One cross-sectional study38 defined cases as responsible for driving accidents; for this reason it could not be included in the meta-analysis with all the other studies that defined cases as affected by OSA. Two other studies37,39 did not report the number of cases and controls, but only the resulting ORs, so they could not be included in the meta-analysis. The first meta-analysis was performed on 7 studies (Figure 2).
Figure 2.
Meta-analysis of the association of self-reported obstructive sleep apnea and workplace accidents (seven studies).
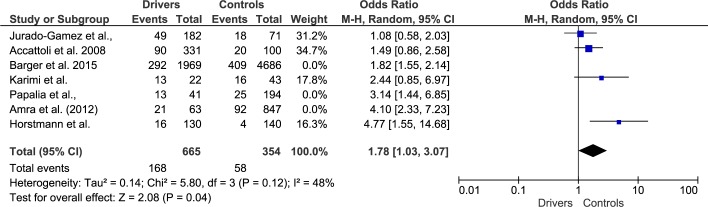
Diagnosis of suspect OSA was mainly obtained with the Berlin Questionnaire. In two studies, OSA was diagnosed by polygraphy,34,41 and in two further studies OSA diagnosis was performed by PSG.35,42 In these studies, according to the American Academy of Sleep Medicine diagnostic criteria,44,45 OSA was diagnosed if apnea-hypopnea index was ≥ 534,41,42 or ≥ 10.35 The second meta-analysis was therefore performed in four studies where diagnosis was confirmed with polygraphy/ PSG (Figure 3).
Figure 3.
Meta-analysis of the association of instrumentally diagnosed obstructive sleep apnea and workplace accidents. Studies without polygraphy/ PSG were excluded from calculation. CI, confidence interval.
Workers with suspected OSA had a near twofold increased odds of being involved in occupational accidents compared to workers without OSA: OR = 2.18; 95% CI: 1.53–3.10 in studies including also suspected OSA; OR = 1.78; 95% CI: 1.03–3.07 in studies with confirmed diagnosis. No data on the effect of severity of OSA on the risk of occupational accidents were found.
Heterogeneity and Publication Bias
Homogeneity analysis performed using the χ2 statistic yielded a χ2 = 15.57, P = 0.02. Because this result may be a sensitive statistic in a meta-analysis based on a limited number of studies, the analysis was supplemented with the I2 statistic, with a resulting total of 61% of real heterogeneity, indicating a medium to high degree of heterogeneity between studies.
Moderator analysis showed that the effect size was influenced by the type of occupational accident. In studies that analyzed work-related traffic accidents, the effect size was significantly higher than in research focused on other types of work accidents (traffic accident: Cohen d = 0.717, P < 0.001; work accident: Cohen d = 0.304, P < 0.001). The type of work was also found to exert an influence as the result was significantly higher in the case of commercial vehicle drivers (Cohen d = 0.780, P < 0.001) compared to bus drivers (Cohen d = 0.576, P < 0.001) and unspecified jobs (Cohen d = 0.313, P < 0.001). Finally, the method of diagnosis was another significant source of heterogeneity; studies that used questionnaires had a higher effect size (Cohen d = 0.380, P < 0.001), whereas no significant differences in effect size were observed in studies using PSG (Cohen d = 0.229, P = 0.131).
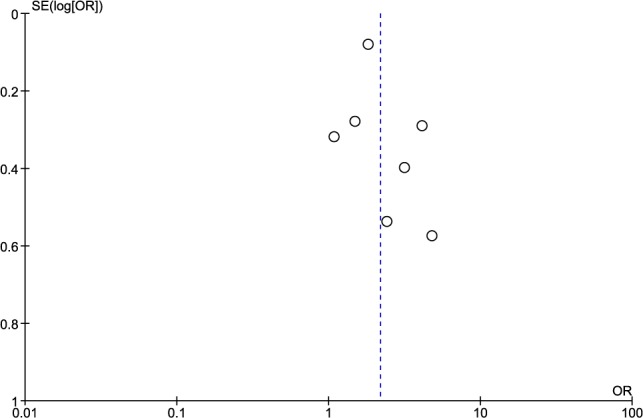
A funnel plot (Figure 4) was used to evaluate the possible imbalance between positive and negative results reported in the studies selected in this meta-analysis. The Egger test was used to evaluate asymmetry in the negative and positive effect size. Because no asymmetry was detected in the funnel plot and the Egger test was not significant (P = 0.610), we found no evidence of publication bias, even if we cannot definitively rule out this possibility, given the low number of observations.
Figure 4.
Funnel plot. OR, odds ratio; SE, standard error.
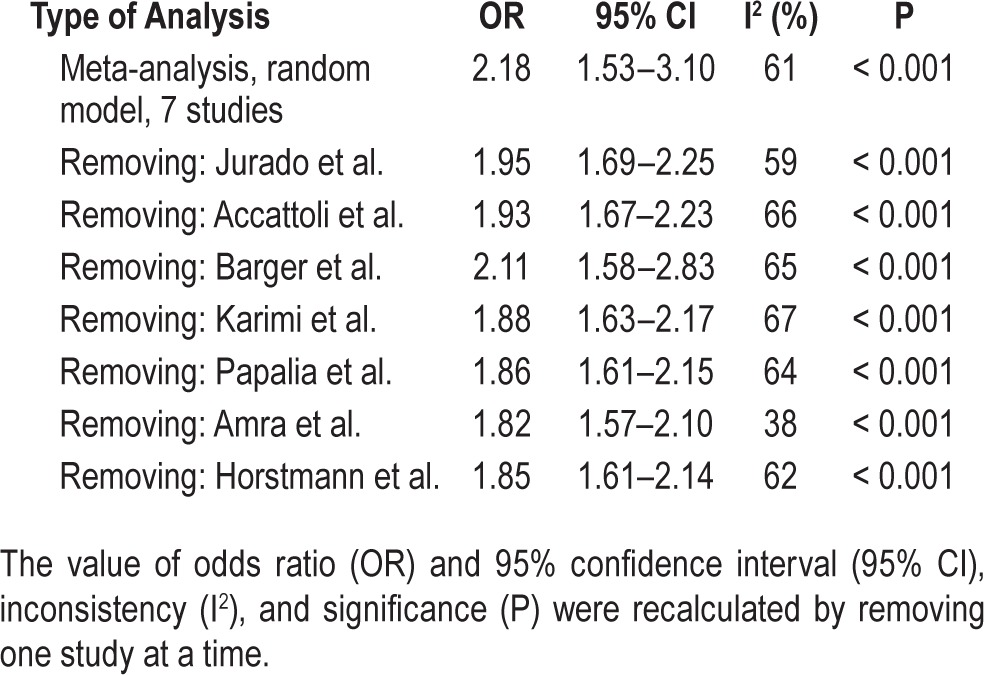
Given the variation in sample sizes, we have recalculated several times the meta-analysis by removing one study at a time. The results of each analysis were not significantly different from the previous calculation (Table 2).
Table 2.
Meta-analysis of the studies on obstructive sleep apnea and work accidents.
DISCUSSION
Our review, which is the first to be entirely based on studies in which OSA was diagnosed with standardized criteria, shows that workers with OSA have a near twofold increased odds of being involved in an accident at work compared to workers not affected by OSA.
Our results are in line with those of previous studies. In a recent systematic review and meta-analysis of studies on sleep disorders and work-related injuries,46 OSA had the strongest association with workplace accidents compared to all other sleep disorders, with a relative odds of 2.88. Studies included in the aforementioned meta-analysis adopted a number of different case definitions (snoring,47–49 EDS,47 breathing pauses during sleep,48 low quantity or low quality of sleep47,50). Moreover, the review included studies in which OSA was diagnosed with different methods. Our methodological approach, based on a systematic review of all available data, an assessment of the methodological quality of the studies, and a meta-analysis of studies in which OSA was diagnosed instrumentally, enabled us to quantify more accurately the risk of occupational accidents attributable to OSA.
In a previous review on motor vehicle crashes,7 on observing that only two studies38,51 had considered the relationship between work-related traffic accidents and OSA, the authors concluded that there was only limited evidence for the reported association. Because the literature now includes a number of additional studies that deal specifically with OSA, we were able to conduct two meta-analyses on work-related accidents. The analysis based only on studies in which OSA was diagnosed instrumentally (OR = 2.18; 95% CI: 1.53–3.10) yielded results similar to the other, which also included self-reported OSA (OR = 1.78; 95% CI: 1.03–3.07). Given the limited number of retrieved studies, this should be considered a preliminary finding. The analysis of subsequent, high-quality studies will give a better estimate of the association.
Based on the results, OSA screening may decrease or prevent some accidents in safety-sensitive occupations. Positive screens should then receive formal diagnostic tests to confirm or rule out OSA. Previous studies demonstrated that screening followed by PSG for high-risk subjects can have a high yield among workers.52 Body mass index cutoffs are a very useful and simple approach for workplace screening that can be augmented by clinical means.16 Even workers of normal weight may be affected by OSA.53 It is well known that in the work-place setting, when job security is potentially at stake, questionnaire techniques might be subject to underreporting from the workers who want and learn to avoid the diagnosis. Thus, the most effective approach will likely be a clinical evaluation, with the help of validated questionnaires, aimed at seeking the signs and symptoms most frequently associated with OSA. Such assessments, aimed at addressing instrumental diagnosis and OSA treatment in workers, should be made by a physician skilled in the management of patients with OSA.
Our research has shown that a number of variables may affect the magnitude of the results obtained. First, diagnostic criteria influence the variance observed. In studies in which OSA was diagnosed with a questionnaire, the risk of occupational injury was found to be greater than in those in which diagnosis was confirmed with instrumental examination. This could be because of smaller sample size, or by the confounding effect of sleepiness. Second, effect size was influenced by the type of outcome observed. Studies that analyzed accidents occurring while driving at work obtained a higher OR than those that included all types of work accidents. Third, the type of job was relevant. Studies that included only professional drivers obtained higher ORs than studies in which cases were drawn from all types of jobs. It is apparent that OSA represents a hazard, especially while driving. This result is in agreement with the findings of studies showing that drivers with OSA have a twofold to eightfold increased risk of motor vehicle crash.54–57 In addition, our results suggest that, like other sleep disorders and EDS,58 OSA is a major risk factor for occupational accidents during workplace activities that do not involve driving.
Our study has some limitations. Given the high level of heterogeneity of studies, some challenges in data interpretation should be kept in mind: variability in how OSA is defined, inconsistency with ascertainment of occupational accidents as well as type of accidents, varying populations which have been studied (bus drivers, firefighters, white collar workers, etc.), with very different accident rates, and differences in epidemiological designs. The fact that the injuries were mainly retrospectively self-reported and that the observation period was often very long can lead to recall bias. A possible source of bias that occurs in this meta-analysis is represented by the work organization that in some categories of workers implies night shift: the consequent sleep-wake cycle disruption and the sleep loss accumulation could be a variable that affects the relationship between OSA and work-related accidents. Furthermore, patients with OSA frequently present with co-morbidities (hypertension, obesity, diabetes, respiratory failure) that could influence the results. The use of sedative medications should be considered as a potential confounder.
According to Cochrane guidelines59 we incorporated heterogeneity into random-effect models, and tried to address heterogeneity through moderator analysis, and publication bias through Egger test; however, the statistical power of these measures is limited, given the low number of selected studies. Moderator analysis could not include all the specific variables that may influence the association between OSA and work accidents. In addition, Egger test results should be viewed with caution. Indeed, few workplace data are available regarding OSA. The results of a limited number of high-quality studies conducted in the workplace need to be confirmed in larger studies involving subjects undergoing PSG. Moreover, the elevated prevalence and suspected negative effect of OSA on working processes in general indicate the need for high-quality studies, especially interventional trials, to be conducted in workplaces.
The lack of well-conducted studies is impressive, if we consider the number of workers using vehicles, heavy machinery, and other safety-sensitive devices, and the fact that so many people have to drive to the workplace or while working. The main reason for this seems to be that OSA is not an occupational disease. The traditional, labor approach to occupational health and safety, and the legislation that derives from this model (still the most common in developed countries), indicated that the surveillance would apply only to aspects related to the work environment. Consequently, despite the high prevalence of OSA among the general population and therefore in adults at work, OSA is still not considered a risk factor pertaining to work. Fortunately, a new holistic approach to occupational health is raising awareness that a number of stakeholders (employers, physicians, sickness insurance, health and environment authorities, and the workers themselves) must work together to control all risk factors, both occupational and non-occupational. The aforementioned European directive stems from this awareness.
Weaknesses and heterogeneities of published studies undoubtedly reduce the power of statistical association that we have actually quantified. Our study confirms that the risk of occupational accidents is associated with OSA. Because the EDS has a significant and clinically relevant association with OSA, neurologists and neurophysiologists could be playing an active role in prevention.
As part of medical assessment in the workplace, there is an urgent need to develop and implement better strategies for screening workers for OSA, especially (but not only) if their job involves the use of vehicles or machinery.
Screening for OSA can be done at a low cost. An instrumental diagnosis can be reserved for workers with suspected OSA. A sleep specialist evaluation is mandatory in the case of workers with OSA who have an associated sleep disorder other than OSA or residual EDS, although in optimal treatment for OSA. The early identification and successful treatment of OSA would probably reduce the number of occupational accidents and improve work performance, with benefits for work processes and business in general.60
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Ms. Elisabeth Ann Wright for assistance with the English version of this manuscript, and Dr. Enrico Di Stasio, MD, Università Cattolica del Sacro Cuore, Roma, for checking statistical analyses. Authors' contributions: Dr. Garbarino conceived, designed, and coordinated the study, and collaborated in paper selection and drafting of the manuscript. Dr. Guglielmi performed the study and participated in statistical analysis and drafting of the manuscript. Dr. Sanna collaborated in study design and critically revised the manuscript. Dr. Mancardi collaborated in conceptualization of the study and paper selection. Dr. Magnavita performed the statistical analysis, drafted the manuscript, and critically revised it. Dr. Garbarino is the Principal Investigator or Guarantor, he has access to all the data and takes responsibility for the data, accuracy of the data analysis, and the conduct of the research. Dr. Magnavita is the Corresponding Author, responsible for all communications with the Journal throughout the review process, including ensuring that all Authors have approved the final submitted version, revised versions before they are submitted, and the final accepted version of the manuscript. All authors gave final approval of the version to be published and take responsibility for the conduct of the research.
REFERENCES
- 1.Costa LE, Uchôa CH, Harmon RR, Bortolotto LA, Lorenzi-Filho G, Drager LF. Potential underdiagnosis of obstructive sleep apnoea in the cardiology outpatient setting. Heart. 2015;101:1288–92. doi: 10.1136/heartjnl-2014-307276. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Sleep Medicine. The international classification of sleep disorders. 3rd. ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 3.Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–8. doi: 10.1016/S2213-2600(15)00043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoeahypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 5.Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apneahypopnea and incident stroke: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2010;182:269–77. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kendzerska T, Gershon AS, Hawker G, Tomlinson G, Leung RS. Obstructive sleep apnea and incident diabetes: a historical cohort study. Am J Respir Crit Care Med. 2014;190:218–25. doi: 10.1164/rccm.201312-2209OC. [DOI] [PubMed] [Google Scholar]
- 7.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5:573–81. [PMC free article] [PubMed] [Google Scholar]
- 8.Garbarino S, Pitidis A, Giustini M, Taggi F, Sanna A. Motor vehicle accidents and obstructive sleep apnea syndrome: a methodology to calculate the related burden of injuries. Chron Respir Dis. 2015;12:320–8. doi: 10.1177/1479972315594624. [DOI] [PubMed] [Google Scholar]
- 9.Sanna A. Obstructive sleep apnoea, motor vehicle accidents, and work performance. Chron Respir Dis. 2013;10:29–33. doi: 10.1177/1479972312473134. [DOI] [PubMed] [Google Scholar]
- 10.Heaton K, Azuero A, Reed D. Obstructive sleep apnea indicators and injury in older farmers. J Agromedicine. 2010;15:148–56. doi: 10.1080/10599241003636020. [DOI] [PubMed] [Google Scholar]
- 11.Mulgrew AT, Ryan CF, Fleetham JA, et al. The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med. 2007;9:42–53. doi: 10.1016/j.sleep.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Hillman DR, Murphy AS, Pezzullo L. The economic cost of sleep disorders. Sleep. 2006;29:299–305. doi: 10.1093/sleep/29.3.299. [DOI] [PubMed] [Google Scholar]
- 13.AlGhanim N, Comondore VR, Fleetham J, Marra CA, Ayas NT. The economic impact of obstructive sleep apnea. Lung. 2008;186:7–12. doi: 10.1007/s00408-007-9055-5. [DOI] [PubMed] [Google Scholar]
- 14.Baumel MJ, Maislin G, Pack AI. Population and occupational screening for obstructive sleep apnea: are we there yet? Am J Respir Crit Care Med. 1997;155:9–14. doi: 10.1164/ajrccm.155.1.9001281. [DOI] [PubMed] [Google Scholar]
- 15.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 16.Talmage JB, Hudson TB, Hegmann KT, Thiese MS. Consensus criteria for screening commercial drivers for obstructive sleep apnea: evidence of efficacy. J Occup Environ Med. 2008;50:324–9. doi: 10.1097/JOM.0b013e3181617ab8. [DOI] [PubMed] [Google Scholar]
- 17.European Commission. Commission directive 2014/85/EU of 1 July 2014 amending Directive 2006/126/EC of the European Parliament and of the Council on driving licenses. [Accessed August 24, 2015]. Retrieved at: http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=uriserv:OJ.L_.2014.194.01.0010.01.ENG.
- 18.Hirsch Allen AJ, Bansback N, Ayas NT. The effect of OSA on work disability and work-related injuries. Chest. 2015;147:1422–8. doi: 10.1378/chest.14-1949. [DOI] [PubMed] [Google Scholar]
- 19.Garbarino S, Gelsomino G, Magnavita N. Sleepiness, safety and transport. J Ergonomics. 2014;S3 003. doi: 10.4172/2165-7556.S3-003. [Google Scholar]
- 20.Dosman J, Hagel L, Skomro R, Sun X, Day A, Pickett W Saskatchewan Farm Injury Study Team. Loud snoring is a risk factor for occupational injury in farmers. Can Respir J. 2013;20:42–6. doi: 10.1155/2013/469391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Torzsa P, Keszei A, Kalabay L, et al. Socio-demographic characteristics, health behavior, co-morbidity and accidents in snorers: a population survey. Sleep Breath. 2011;15:809–18. doi: 10.1007/s11325-010-0442-4. [DOI] [PubMed] [Google Scholar]
- 22.Lindberg E, Carter N, Gislason T, Janson C. Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med. 2001;164:2031–5. doi: 10.1164/ajrccm.164.11.2102028. [DOI] [PubMed] [Google Scholar]
- 23.Vennelle M, Engleman HM, Douglas NJ. Sleepiness and sleep-related accidents in commercial bus drivers. Sleep Breath. 2010;14:39–42. doi: 10.1007/s11325-009-0277-z. [DOI] [PubMed] [Google Scholar]
- 24.de Pinho RS, da Silva-Junior FP, Bastos JPC, et al. Hypersomnolence and accidents in truck drivers: a cross-sectional study. Chronobiol Int. 2006;23:963–71. doi: 10.1080/07420520600920759. [DOI] [PubMed] [Google Scholar]
- 25.Spengler S, Browning SR, Reed D. Sleep deprivation and injuries in part-time Kentucky farmers. AAOHN J. 2004;52:373–82. [PubMed] [Google Scholar]
- 26.Choi SW, Peek-Asa C, Prince NL, et al. Sleep quantity and quality as a predictor of injuries in a rural population. Am J Emerg Med. 2006;24:189–96. doi: 10.1016/j.ajem.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Garbarino S, Magnavita N. Obstructive sleep apnea syndrome (OSAS), metabolic syndrome and mental health in small enterprise workers. Feasibility of an action for health. PLoS ONE. 2014;9:e97188. doi: 10.1371/journal.pone.0097188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic reviews and meta-analyses protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wells G, Shea B, O'Connel D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomised studies in metaanalyses. [Accessed September 5, 2015]. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 30.Greenland S. Variance estimators for attributable fraction estimates consistent in both large strata and sparse data. Stat Med. 1987;6:701–8. doi: 10.1002/sim.4780060607. [DOI] [PubMed] [Google Scholar]
- 31.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Chichester, UK: Wiley; 2009. [Accessed January 15, 2015]. Introduction to meta-analysis. Available at: http://www.meta-analysis.com/downloads/Meta%20Analysis%20Fixed%20vs%20Random%20effects.pdf. [Google Scholar]
- 32.Thornton A, Lee P. Publication bias in meta-analysis: its causes and consequences. J Clin Epidemiol. 2000;53:207–16. doi: 10.1016/s0895-4356(99)00161-4. [DOI] [PubMed] [Google Scholar]
- 33.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karimi M, Eder DN, Eskandari D, Zou D, Hedner JA, Grote L. Impaired vigilance and increased accident rate in public transport operators is associated with sleep disorders. Accid Anal Prev. 2013;51:208–14. doi: 10.1016/j.aap.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 35.Horstmann S, Hess CH, Bassetti C, Gugger M, Mathis J. Sleepiness-related accidents in sleep apnea patients. Sleep. 2000;23:383–9. [PubMed] [Google Scholar]
- 36.Amra B, Dorali R, Mortazavi S, et al. Sleep apnea symptoms and accident risk factors in Persian commercial vehicle drivers. Sleep Breath. 2012;16:187–91. doi: 10.1007/s11325-010-0473-x. [DOI] [PubMed] [Google Scholar]
- 37.Catarino R, Spratley J, Catarino I, Lunet N, Pais-Clemente M. Sleepiness and sleep-disordered breathing in truck drivers: risk analysis of road accidents. Sleep Breath. 2014;18:59–68. doi: 10.1007/s11325-013-0848-x. [DOI] [PubMed] [Google Scholar]
- 38.Howard ME, Desai AV, Grunstein RR, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 39.Ebrahimi MH, Sadeghi M, Dehghani M, Sadegh NK, Niiat KS. Sleep habits and road traffic accident risk for Iranian occupational drivers. Int J Occup Med Environ Health. 2015;28:305–12. doi: 10.13075/ijomeh.1896.00360. [DOI] [PubMed] [Google Scholar]
- 40.Papalia L, Goldoni M, Spaggiari MC, et al. Sleep disorders, risk of accidents and traffic accidents in a group of drivers of public. G Ital Med Lav Ergon. 2012;34:353–6. [PubMed] [Google Scholar]
- 41.Accattoli MP, Muzi G, dell'Omo M, et al. Occupational accidents, work performance and obstructive sleep apnea syndrome (OSAS) G Ital Med Lav Ergon. 2008;30:297–303. [PubMed] [Google Scholar]
- 42.Jurado-Gámez B, Guglielmi O, Gude F, Buela-Casal G. Workplace accidents, absenteeism and productivity in patients with sleep apnea. Arch Broncopneumol. 2015;51:213–8. doi: 10.1016/j.arbres.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 43.Barger LK, Rajaratnam SM, Wang W, et al. Common sleep disorders increase risk of motor vehicle crashes and adverse health outcomes in firefighters. J Clin Sleep Med. 2015;11:233–40. doi: 10.5664/jcsm.4534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iber C, Ancoli-Israel S, Chesson AL, Quan SF for the American Academy of Sleep Medicine. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specification, 1st ed. [Google Scholar]
- 45.American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 46.Uehli K, Mehta AJ, Miedinger D, et al. Sleep problems and work injuries: a systematic review and meta-analysis. Sleep Med Rev. 2014;18:61–73. doi: 10.1016/j.smrv.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 47.Fransen M, Wilsmore B, Winstanley J, et al. Shift work and work injury in the New Zealand blood donors' health study. Occup Environ Med. 2006;63:352–8. doi: 10.1136/oem.2005.024398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ulfberg J, Carter N, Edling C. Sleep-disordered breathing and occupational accidents. Scand J Work Environ Health. 2000;26:237–42. doi: 10.5271/sjweh.537. [DOI] [PubMed] [Google Scholar]
- 49.Kamil MA, Teng CL, Hassan SA. Snoring and breathing pauses during sleep in the Malaysian population. Respirology. 2007;12:375–80. doi: 10.1111/j.1440-1843.2007.01030.x. [DOI] [PubMed] [Google Scholar]
- 50.Nakata A, Ikeda T, Takahashi M, et al. Sleep-related risk of occupational injuries in Japanese small and medium-scale enterprises. Ind Health. 2005;43:89–97. doi: 10.2486/indhealth.43.89. [DOI] [PubMed] [Google Scholar]
- 51.Stoohs RA, Guilleminault C, Itoi A, Dement WC. Traffic accidents in commercial long-haul truck drivers: the influence of sleep-disordered breathing and obesity. Sleep. 1994;17:619–23. [PubMed] [Google Scholar]
- 52.Berger M, Varvarigou V, Rielly A, Czeisler CA, Malhotra A, Kales SN. Employer-mandated sleep apnea screening and diagnosis in commercial drivers. J Occup Environ Med. 2012;54:1017–25. doi: 10.1097/JOM.0b013e3182572e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol. 2005;99:1592–9. doi: 10.1152/japplphysiol.00587.2005. [DOI] [PubMed] [Google Scholar]
- 54.Meuleners L, Fraser ML, Govorko MH, Stevenson MR. Obstructive sleep apnea, health-related factors, and long distance heavy vehicle crashes in Western Australia: a case control study. J Clin Sleep Med. 2015;11:413–8. doi: 10.5664/jcsm.4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lloberes P, Levy G, Descals C, et al. Self-reported sleepiness while driving as a risk factor for traffic accidents in patients with obstructive sleep apnoea syndrome and non-apnoeic snorers. Respir Med. 2000;94:971–6. doi: 10.1053/rmed.2000.0869. [DOI] [PubMed] [Google Scholar]
- 56.Barbé F, Sunyer J, de la Peña A, et al. Effect of continuous positive airway pressure on the risk of road accidents in sleep apnea patients. Respiration. 2007;74:44–9. doi: 10.1159/000094237. [DOI] [PubMed] [Google Scholar]
- 57.Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 58.Philip P, Akerstedt T. Transport and industrial safety, how are they affected by sleepiness and sleep restriction? Sleep Med Rev. 2006;10:347–56. doi: 10.1016/j.smrv.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 59.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Updated March 2011. The Cochrane Collaboration. 2011. Available from www.cochrane-handbook.org.
- 60.Garbarino S, Nobili L, Costa G, editors. Sleepiness and human impact assessment. Berlin: Springer Link; 2014. [Google Scholar]