Abstract
Study Objectives:
Disrupted sleep is one of the prominent but often overlooked presenting symptoms in the clinical course of psychotic disorders. The aims of this study were to examine the prevalence of sleep disturbances, particularly insomnia and nightmares, and their prospective associations with the risk of suicide attempts in patients with schizophrenia-spectrum disorders.
Methods:
A naturalistic longitudinal study was conducted in outpatients diagnosed with schizophrenia-spectrum disorders recruited from the psychiatric outpatient clinic of a regional university-affiliated public hospital in Hong Kong. A detailed sleep questionnaire was completed by 388 patients at baseline in May–June 2006. Relevant clinical information was extracted from clinical case notes from June 2007–October 2014.
Results:
Prevalence of frequent insomnia and frequent nightmares was 19% and 9%, respectively. Baseline frequent insomnia was significantly associated with an increased incidence of suicide attempts during the follow-up period (adjusted hazard ratio = 4.63, 95% confidence interval 1.40–15.36, P < 0.05). Nightmare complaint alone did not predict the occurrence of suicide attempts, but the comorbidity of nightmares and insomnia was associated with the risk of suicide attempt over follow-up (adjusted HR = 11.10, 95% confidence interval: 1.68–73.43, P < 0.05).
Conclusions:
Sleep disturbances are common in patients with schizophrenia-spectrum disorders. The association between sleep disturbances and suicidal risk underscores the need for enhanced clinical attention and intervention on sleep disturbances in patients with schizophrenia.
Citation:
Li SX, Lam SP, Zhang J, Yu MW, Chan JW, Chan CS, Espie CA, Freeman D, Mason O, Wing YK. Sleep disturbances and suicide risk in an 8-year longitudinal study of schizophrenia-spectrum disorders. SLEEP 2016;39(6):1275–1282.
Keywords: insomnia, nightmares, psychosis, schizophrenia, sleep, suicide
Significance.
Suicide is the leading cause of premature death among patients with schizophrenia. Timely identification of the individuals at risk of suicide remains a major challenge for clinicians. This is the first study to illustrate the risk over time of suicidal behaviors in relation to sleep complaints in individuals with schizophrenia spectrum disorders. Sleep disturbances, including insomnia and nightmares, were found to predict an increased risk of suicide attempts in outpatients with schizophrenia spectrum disorders. This prognostic implication underscores the need to timely assess and address sleep disturbances in this clinical population. Future research is needed to examine the efficacy of sleep-focused treatments in managing sleep disturbances in the context of psychotic disorders.
INTRODUCTION
Sleep disturbances, one of the most common presenting complaints in psychiatric patients, are often associated with substantial personal distress, pronounced impairment of daytime functioning, reduced quality of life, and aggravation of the comorbid clinical conditions.1 Growing evidence also reveals a significant association between sleep disturbances and an increased risk of suicidal behaviors in both general and clinical populations.2–4 However, there have been limited longitudinal data examining this association specifically in patients with schizophrenia. Given that suicide is a leading cause of premature death, accounting for 12% of the excessive mortality among schizophrenia patients,5 there is a need to investigate the link between sleep disturbances and suicidal risk in this clinical population.
Sleep disturbances are often implicated in the clinical course of psychosis. For example, insomnia is one of the most common prodromal symptoms preceding a psychotic episode6; it may exacerbate during the acute phase of the illness or may present as a residual symptom in the clinically stabilized patients.7 Recent evidence also suggests a link between the presence of insomnia and a particular dimensional psychotic experience, notably paranoia, in both clinical and general populations.8,9 Nonetheless, there is a relative paucity of data on the prevalence of sleep disturbances, including insomnia and nightmares, in patients with schizophrenia, as most previous studies were focused on polysomnographic and actigraphic sleep features of patients with schizophrenia in selected small samples using case-control design.10–13 To address the limitations of the existing literature, the objectives of the current study were to examine the prevalence of sleep disturbances, particularly frequent insomnia and nightmares, and their prospective associations with the risk of suicide attempts in patients in whom schizophrenia spectrum disorders were diagnosed.
METHODS
Participants
The current study was an 8-y observational study on a consecutively recruited cohort of psychiatric outpatients in whom schizophrenia-spectrum disorders were diagnosed. All the participants provided their written informed consent. The study protocol was approved by the Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee.
The baseline assessment was a part of a clinical epidemiologic study on the sleep problems among psychiatric patients conducted in the psychiatric outpatient clinic of a regional university-affiliated public hospital, which served 8.9% (0.6 million) of the total population of Hong Kong. A detailed description of the study design and recruitment at baseline has been reported elsewhere.4,14 In brief, all eligible patients aged 18–65 y attending the clinic consecutively during the 4-w recruitment period in May–June 2006 were invited to take part in the baseline study, which involved a sleep questionnaire assessment. Patients were excluded if they: (1) were unable to provide a valid informed consent; (2) had an intellectual difficulty or organic brain syndrome; (3) had a hearing or speech deficit; or (4) were attending the university-affiliated sleep clinic, which is a part of the psychiatric department. A total of 1,235 psychiatric outpatients (female: 68.1%; mean age: 42.4 y, standard deviation [SD] 11.3 y) were recruited at baseline, and 388 patients (31.4%) in whom schizophrenia spectrum disorders had been diagnosed in this cohort were the target study population of the current study.
Measurements
Instrument
The sleep questionnaire used in the current study has been validated locally as a measure of different sleep problems among psychiatric patients.14 It included items to assess demography, lifestyle practice, sleep habit, and specific sleep problems, including insomnia and nightmares, and was designed to measure sleep problems on the basis of lifetime occurrence and frequency over the past year. Frequency of sleep disturbances over the previous year was rated on a five-point scale (0 = none, 1 = rarely, 2 = at least once a month, 3 = once or twice a week, 4 = at least three times a week). The sleep questionnaire has been shown to have satisfactory psychometric properties.14 The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the overall questionnaire were 0.92, 0.83, 0.88, and 0.88, respectively. In line with the previous research,4,15–17 frequent insomnia was defined as having one or more of the following sleep problems with the frequency of at least three times a week in the past year: difficulty initiating sleep, difficulty maintaining sleep, and early morning awakening. Frequent nightmares were defined as having nightmares of at least once a week in the past year. Frequency of alcohol consumption and drug compliance was assessed on a three-point scale (0 = never, 1 = sometimes, 2 = always).
Case Note Information
Each study participant was diagnosed by the attending psychiatrist based on the criteria of the International Classification of Diseases, Tenth Revision (ICD-10). Relevant clinical information on the study participants was reviewed in the Clinical Management System (CMS), an integrated computerized clinical workstation that is implemented in all public hospitals in Hong Kong. The CMS provides comprehensive and detailed documentation of the clinical history of a patient who is followed up in any public health care sector of Hong Kong. Clinical information retrieved from the CMS for the current study included the medical history, duration of mental illness, and prescription of psychotropic medications. Period of observation was from June 2006 (the date that the participants completed the baseline questionnaire assessment) to October 2014. Documentation of any suicide attempt in the case notes during the study period was used to analyze the prospective association between sleep disturbances, as reported in the baseline assessment in 2006, and suicide attempts over the 8-y follow-up period. To reduce the potential for bias, the investigator was blind to the baseline sleep status of the study participants when conducting the case note review. A suicide attempt was defined as a deliberate act of self-harm with the intention to end one's life.4,18 All the clinical records and documentation in the CMS were reviewed. These included the progress notes from the outpatient clinics of all specialties where the patients had any medical or psychiatric follow-up appointments, inpatient psychiatric admission notes and discharge summary, as well as the medical notes following the attendance to the emergency department. Psychotherapy notes were not included as these were not routinely entered into the computerized system. The clinical notes where self-injury was documented were specifically reviewed, and the written description of the index incident was examined thoroughly for evidence of suicide attempt, i.e., an intention to end one's life. Examples of suicide attempts included: self-inflicted poisoning (ICD-10 code X60-69), self-inflicted injury by cutting and piercing instruments (ICD-10 code X78, X79), self-inflicted injury by hanging, strangulation, and suffocation (ICD-10 code X70), and self-inflicted injury by jumping from places (ICD-10 code X80).
Statistical Analysis
Chi-square analyses or t-tests, where appropriate, were used to determine the significant differences in the demographic and clinical characteristics between the participants with and without sleep disturbances at baseline. The index date was the date of the participants completing the baseline questionnaire assessment. The primary end point was an incident of suicide attempt as documented in the case notes of the CMS. Observations were censored in the survival analysis for the cases that were lost to follow-up (e.g., no longer had any updated medical records shown in the CMS or no longer had any type of follow-up appointment in the public health care sector of Hong Kong) or had died (cause of death unrelated to a suicide attempt). The date of the last primary or speciality care follow-up of the study participants in the public health care sector was used as the censoring date. Kaplan-Meier curves were used to depict the cumulative probability of suicide attempt during the follow-up period between the participants with and without sleep disturbances reported at baseline. Survival curves were compared using the log-rank test. Cox proportional hazards regression models were used to examine the association between the sleep disturbances and incidents of suicide attempt while controlling for the potential confounders and effect modifiers. These variables were selected based on the initial univariate and bivariate statistical results, as well as the potential relationships, as reported in the previous studies.19 Selected covariates included the baseline demographics (age, sex) and relevant clinical factors (i.e., duration of mental illness, subtype of psychotic disorders, prescription of benzodiazepines and anti-depressants, past history of suicide attempt(s) and hospitalizations prior to the baseline questionnaire assessment, and use of more than one psychotropic medication). Relative risks were expressed as hazard ratios (HRs) with 95% confidence intervals (CIs). All statistical analyses were undertaken using the software Statistical Package for the Social Sciences, Version 16.0 for Windows (SPSS Inc., Chicago, IL). Statistical significance was set at 0.05 (two-tailed).
RESULTS
The study sample comprised 388 patients in whom schizophrenia spectrum disorders were diagnosed (Table 1 and Table 2). At the time that the case notes were reviewed, 369 patients (95.1%) continued to attend regular medical or psychiatric follow-up appointments, 6 patients (1.5%) did not have any accessible medical record as they were no longer followed up in the public health care sector, and 13 patients (3.4%) were deceased during the follow-up period due to a medical condition (e.g., cancer) or an accident (e.g., hiking accident) that was not considered as a suicide attempt. Seventeen patients (4.4%) have attempted suicide but there was no completed suicide during the follow-up period.
Table 1.
Prevalence of nocturnal sleep disturbances in relation to ICD-10 diagnosis in the study participants.

Table 2.
Demographic and clinical characteristics of the study participants.

The 1-y prevalence of frequent insomnia and frequent nightmares at baseline was 19.3% and 9.0%, respectively. Comorbid insomnia and nightmare were reported in 3.4% of the overall participants. Participants who had frequent nightmares were more likely to report frequent insomnia (37.1% versus 17.6%, χ2 = 7.8, d.f. = 1, P < 0.01). Likewise, participants with frequent insomnia were more likely to have co-morbid nightmare disturbances (17.3% versus 7.0%, χ2 = 7.8, d.f. = 1, P < 0.01). One-year prevalence of sleep disturbances among the participants with different psychotic diagnoses is presented in Table 1.
Participants with frequent insomnia were more likely to be married (χ2 = 8.0, d.f. = 1, P < 0.01), and were less likely to be single (χ2 = 7.8, d.f. = 1, P < 0.01) and have completed a higher education (χ2 = 6.6, d.f. = 1, P < 0.05) (Table 2). They were also more likely to be prescribed more than one psychotropic medication (χ2 = 9.6, d.f. = 1, P < 0.01), especially antidepressants (χ2 = 4.3, d.f. = 1, P < 0.05) and benzodiazepines (χ2 = 11.2, d.f. = 1, P < 0.01), and to report a better drug compliance (χ2 = 6.4, d.f. = 1, P < 0.05). Frequent nightmares were found to be associated with the comorbid physical illness (χ2 = 5.9, d.f. = 1, P < 0.05) (Table 2).
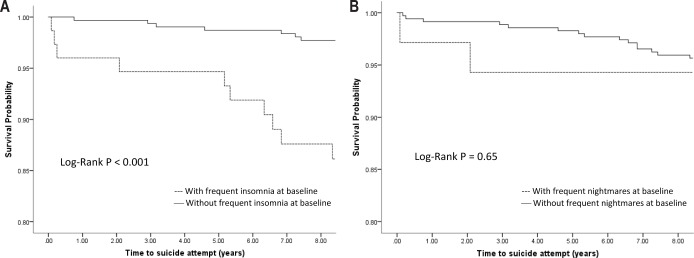
The Kaplan-Meier survival analysis revealed significantly higher cumulative incidence of suicide attempt in the group of the participants with frequent insomnia at baseline as compared to their counterparts (P < 0.001, log-rank test, Figure 1A). Cox regression models further confirmed this observation. Frequent insomnia reported at baseline was significantly associated with the new incidence of suicide attempt during the follow-up period after controlling for potential confounding factors (adjusted HR = 4.63, 95% CI 1.40–15.36, P < 0.05) (Table 3).
Figure 1.
Survival curves of time to suicide attempt between the participants with and without frequent sleep disturbances reported at baseline. (A) Frequent insomnia reported at baseline in relation to the incident of suicide attempt over the follow-up period. (B) Frequent nightmares reported at baseline in relation to the incidents of suicide attempt over the follow-up period.
Table 3.
Unadjusted and adjusted Cox regression models for insomnia predicting the incidents of suicide attempt over the 8-y follow-up period.

Although the complaint of frequent nightmares was associated with a lifetime history of suicide attempts (42.9% versus 19.3%, χ2 = 10.5, d.f. = 1, P < 0.01), it did not predict an increased risk of suicide attempt over the follow-up period (P = 0.65, log-rank test, Figure 1B). Further scrutiny of the data revealed a distinct pattern that the comorbidity of insomnia and nightmare disturbances was significantly associated with an increased risk of suicide attempts not only in lifetime (P < 0.001, linear-by-linear association) but also during the 8-y follow-up period (P < 0.01, linear-by-linear association) (Figure 2). Cox regression analysis suggested that the participants who reported comorbid insomnia and nightmares at baseline had a greater risk of suicide attempts in the following 8 y (crude HR = 7.43, 95% CI: 1.54–35.81, P < 0.05) as compared to those without any sleep disturbances at baseline. This significance persisted after adjusting for demographic and clinical confounding factors (adjusted HR = 11.10, 95% CI: 1.68–73.43, P < 0.05). However, because of the limited number of cases, the interaction between frequent insomnia and frequent nightmares could not be tested in the regression model.
Figure 2.
Presence of sleep disturbances at baseline in relation to the incidents of suicide attempt in lifetime and during the 8-y follow-up period. *Linear-by-linear association.
DISCUSSION
The current study provides the prevalence and correlates of sleep disturbances in a cohort of patients in whom schizophrenia spectrum disorders were diagnosed. To the best of our knowledge, this is the first study to illustrate the risk over time of suicidal behaviors in relation to sleep complaints in patients with schizophrenia spectrum disorders.
Sleep Disturbances in Schizophrenia-Spectrum Disorders
The prevalence of frequent nightmares was 9.0% in this study sample, which was higher than that of the local general adult population (5.1%).16 In a small survey conducted in an outpatient clinic, 16.7% of 54 schizophrenia patients reported having experienced nightmares in the past year, which is higher than that of the healthy controls (4.9%).20 There have been only two studies that reported the prevalence of insomnia (36% to 44%) in the clinically stable schizophrenia outpatients,7,21 which appears to be relatively higher as compared to the percentage (19%) found in this study. The discrepancy in the prevalence rates might be partly explained by the use of more stringent criteria to define the symptomatic timeframe (e.g., past 1 y versus past 2 w) and the heterogeneity of the clinical samples in different studies (e.g., schizophrenia versus schizophrenia spectrum disorders). Previous studies based on the polysomnographic or actigraphic data have consistently showed a marked sleep disruption, characterized by difficulty initiating and maintaining sleep, in patients with schizophrenia using a case-control design.10,11,13 Similarly, the prevalence rates of frequent insomnia in this clinical cohort across different psychotic diagnoses (14% to 46%) were found to be variably higher than that of the local general adult population (9% to 13%).15,22 Subjective sleep disturbances, such as insomnia, may be related to the circadian dysregulation often observed in patients with schizophrenia.23 Further investigation incorporating the measures of circadian rhythm would be needed to unravel the potential mechanism underlying the sleep disturbances in this clinical population.
Sleep Disturbances in Relation to the Suicidal Risk
Our study confirmed that sleep disturbances confer a greater risk for suicide attempts in patients with schizophrenia spectrum disorders. In particular, frequent insomnia reported at baseline was independently associated with fourfold higher incidence of suicide attempt over the longitudinal follow-up. Similarly, insomnia was identified as one of the risk factors for completed suicide in a retrospective case-control study of suicide victims with a diagnosis of schizophrenia.24 Although the complaint of frequent nightmares alone did not appear to be a significant predictor of suicide attempt in the initial analysis, the comorbidity of frequent nightmares and insomnia was shown to confer an increased risk of future suicide attempt (11-fold higher). The observation that sleep disturbances may predict the suicidal risk in not only near but also distant future may suggest that sleep disturbances might be persistent in some patients and represent a proximal risk factor for suicidal behaviors in this clinical population. Community-based longitudinal studies suggest that sleep disturbances, such as insomnia, once developed, may follow a persistent course in 40% to 80% of the community-based subjects over 3 to 5 y of follow-up.15,25 Nonetheless, there have been limited data that documented the longitudinal course of sleep symptoms in patients with schizophrenia spectrum disorders. Further longitudinal studies are warranted to examine the persistence of sleep disturbances in this clinical population.
Our findings are in line with the growing literature suggesting a significant association of the sleep disturbances, including insomnia and nightmares, with suicidal behaviors in the general and other clinical populations, such as major depression and anxiety disorders.2–4 The mechanistic relationship between sleep disruption and suicidal behaviors in the patients with schizophrenia and other psychotic disorders remains untested, albeit there are several possible pathways. There is evidence to suggest an association between sleep disturbances and certain psychotic experiences, such as paranoia and command hallucination,8,26 which may potentially increase the risk for suicide. In addition, individuals with sleep disturbances are often at an increased risk for the development of depression,15,16 which is also an independent risk factor for suicide.19 Thus, it is possible that sleep disturbances may exacerbate mood symptoms and psychotic experiences,8,27 rendering the individuals more susceptible to engage in suicidal behaviors. However, sleep disturbances may contribute to the suicidal risk independently by impairing cognitive and executive functions, and compromising emotional processing,28,29 thereby leading to deficits in problem solving and vulnerability to impulsive behaviors.29 Although the clinical severity of the mood symptoms and psychotic experiences was not directly assessed in this study, several clinical variables were taken into account and included in the multivariate models, such as the duration of mental illness, prescription of antidepressants, and history of admission to a psychiatric ward and suicide attempt(s). Frequent insomnia and comorbid insomnia and nightmares remained significantly associated with new incidence of suicide attempt during the follow-up period, even after adjusting for these potentially confounding factors. The findings might therefore lend support to the independent role of sleep disturbances in increasing the suicidal risk in the patients with schizophrenia-spectrum disorders. Nonetheless, further research is needed to delineate the mechanism underlying the relationship between sleep disturbances and risk of suicidal behaviors in this clinical population.
Clinical Implications
Schizophrenia is associated with an elevated risk of suicide, with a lifetime rate of completed suicide estimated to be 4.9%.30 Timely identification of the individuals at risk of suicide remains a major challenge for clinicians. Although a number of risk factors for suicide in patients with schizophrenia have been identified, some of these factors (e.g., age, sex, family history of suicide) may not be amenable to intervention. In this regard, the prospective association between sleep disturbances and suicidal risk found in this study has important clinical implications, because sleep disturbances are potentially modifiable factors that could be ameliorated through proper interventions. Clinical efficacy of sleep-focused psychological treatments, such as cognitive behavioral therapy for insomnia (CBT-I) or imagery rehearsal therapy (IRT) for nightmares, has been well established in a variety of clinical populations and settings.31,32 A recent study has shown that effective treatment of CBT-I reduced suicidal ideation even after accounting for the effect of concurrent improvement in the severity of depressive symptoms.33 Although the data on the treatment outcome of CBT-I in the context of psychotic disorders remain limited, there have been some promising results.9,34 Meanwhile, sleep disturbances could be a side effect of medication or a residual symptom despite the optimized medication treatment for patients with schizophrenia. Different pharmacological approaches have been suggested to manage residual sleep disturbances in schizophrenia,35 including the use of antipsychotics with sedating properties or adding short-term adjunctive medications, such as benzodiazepines or hypnotic agents, to a nonsedating antipsychotic agent. However, the evidence base of these treatment approaches is limited, and there remains a concern with regard to potentially increasing suicide risk by prescribing sedatives and hypnotic agents in vulnerable individuals. Of note, 60% of the study participants with frequent insomnia were prescribed antipsychotic agents with moderate to marked sedative properties, and were more often prescribed benzodiazepines and on poly-pharmacy treatment, as compared to those without insomnia. However, the adjunct pharmacologic treatment did not seem to alleviate their sleep problems. Collectively, the findings of this study and the existing literature suggest a need for further interventional studies to examine the efficacy of sleep-focused treatments in managing sleep disturbances in the context of psychotic disorders.
Strengths and Limitations of the Study
The major strength of this study is the follow-up of a large consecutive cohort of outpatients in whom schizophrenia spectrum disorders were diagnosed in a naturalistic clinical setting. These data provided a more realistic picture showing the strength of the associations between sleep disturbance and suicidal risk in the general clinical practice. Nonetheless, the findings of this study should be interpreted with caution in light of several methodological caveats. Although a series of the variables associated with suicidal risk were included in the analysis, some of the risk factors, such as social support network, could not be adequately evaluated in this study. Moreover, the measurement of sleep disturbances in this study was based on only self-report without further objective assessment. The data on the suicide attempts were based on the review of case records, which might have potentially underestimated the prevalence and incidence. Incidents might be less likely to be documented if the suicide attempts were not severe enough to warrant medical treatment or if the patients chose not to disclose their act to the attending medical practitioners. However, the lifetime prevalence of suicide attempt in this study cohort (21.4%) was comparable to that of a previous study based on the clinical interview (30.2%).18 Furthermore, the limited number of cases precluded further subgroup analyses to examine whether some of the clinically relevant factors, e.g., prescription of more than one medication and drug compliance, would affect the time to first suicide attempt in the follow-up period among patients with sleep disturbances at baseline.
CONCLUSION
Sleep disturbances are significantly associated with an increased risk of suicide attempts in schizophrenia spectrum disorders. This prognostic implication underscores the need for enhanced clinical attention towards sleep problems in patients with schizophrenia spectrum disorders. Future research is needed to examine the efficacy of sleep-focused treatments in managing sleep disturbances in this clinical population.
DISCLOSURE STATEMENT
This was not an industry-supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders: a meta-analysis. Arch Gen Psychiatry. 1992;49:651–68. doi: 10.1001/archpsyc.1992.01820080059010. [DOI] [PubMed] [Google Scholar]
- 2.Malik S, Kanwar A, Sim LA, et al. The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: a systematic review and meta-analysis. Syst Rev. 2014;3:18. doi: 10.1186/2046-4053-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73:e1160–7. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- 4.Li SX, Lam SP, Yu MWM, Zhang J, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71:1440–6. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- 5.Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry. 1997;171:502–8. doi: 10.1192/bjp.171.6.502. [DOI] [PubMed] [Google Scholar]
- 6.Yung A, McGorry P. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–70. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- 7.Xiang Y, Weng Y, Leung C, Tang W. Prevalence and correlates of insomnia and its impact on quality of life in Chinese schizophrenia patients. Sleep. 2009;32:105–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Freeman D, Pugh K, Vorontsova N, Southgate L. Insomnia and paranoia. Schizophr Res. 2009;108:280–4. doi: 10.1016/j.schres.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Myers E, Startup H, Freeman D. Cognitive behavioural treatment of insomnia in individuals with persistent persecutory delusions: a pilot trial. J Behav Ther Exp Psychiatry. 2011;42:330–6. doi: 10.1016/j.jbtep.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chouinard S, Poulin J, Stip E, Godbout R. Sleep in untreated patients with schizophrenia: a meta-analysis. Schizophr Bull. 2004;30:957–67. doi: 10.1093/oxfordjournals.schbul.a007145. [DOI] [PubMed] [Google Scholar]
- 11.Monti J, Monti D. Sleep in schizophrenia patients and the effects of antipsychotic drugs. Sleep Med Rev. 2004;8:133–48. doi: 10.1016/S1087-0792(02)00158-2. [DOI] [PubMed] [Google Scholar]
- 12.Martin J, Jeste DV, Caliguiri MP, Patterson T, Heaton R, Ancoli-Israel S. Actigraphic estimates of circadian rhythms and sleep/wake in older schizophrenia patients. Schizophr Res. 2001;47:77–86. doi: 10.1016/s0920-9964(00)00029-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afonso P, Figueira ML, Paiva T. Sleep-wake patterns in schizophrenia patients compared to healthy controls. World J Biol Psychiatry. 2014;15:517–24. doi: 10.3109/15622975.2012.756987. [DOI] [PubMed] [Google Scholar]
- 14.Lam SP, Fong SYY, Ho CKW, Yu MWM, Wing YK. Parasomnia among psychiatric outpatients: a clinical, epidemiologic, cross-sectional study. J Clin Psychiatry. 2008;69:1374–82. doi: 10.4088/jcp.v69n0904. [DOI] [PubMed] [Google Scholar]
- 15.Zhang J, Lam SP, Li SX, et al. Long-term outcomes and predictors of chronic insomnia: a prospective study in Hong Kong Chinese adults. Sleep Med. 2012;13:455–62. doi: 10.1016/j.sleep.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Li SX, Zhang B, Li AM, Wing YK. Prevalence and correlates of frequent nightmares: a community-based 2-phase study. Sleep. 2010;33:774–80. doi: 10.1093/sleep/33.6.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li SX, Lam SP, Chan JWY, Yu MWM, Wing YK. Residual sleep disturbances in patients remitted from major depressive disorder: a 4-year naturalistic follow-up study. Sleep. 2012;35:1153–61. doi: 10.5665/sleep.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radomsky ED, Haas GL, Mann JJ, Sweeney JA. Suicidal behavior in patients with schizophrenia and other psychotic disorders. Am J Psychiatry. 1999;156:1590–5. doi: 10.1176/ajp.156.10.1590. [DOI] [PubMed] [Google Scholar]
- 19.Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9–20. doi: 10.1192/bjp.187.1.9. [DOI] [PubMed] [Google Scholar]
- 20.Mume CO. Nightmare in schizophrenic and depressed patients. Eur J Psychiatry. 2009;23:177–83. [Google Scholar]
- 21.Palmese LB, DeGeorge PC, Ratliff JC, et al. Insomnia is frequent in schizophrenia and associated with night eating and obesity. Schizophr Res. 2011;133:238–43. doi: 10.1016/j.schres.2011.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang J, Li AM, Kong APS, Lai KYC, Tang NLS, Wing YK. A community-based study of insomnia in Hong Kong Chinese children: prevalence, risk factors and familial aggregation. Sleep Med. 2009;10:1040–6. doi: 10.1016/j.sleep.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Wulff K, Dijk DJ, Middleton B, Foster RG, Joyce EM. Sleep and circadian rhythm disruption in schizophrenia. Br J Psychiatry. 2012;200:308–16. doi: 10.1192/bjp.bp.111.096321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pompili M, Lester D, Grispini A, et al. Completed suicide in schizophrenia: evidence from a case-control study. Psychiatry Res. 2009;167:251–7. doi: 10.1016/j.psychres.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 25.Morin CM, Belanger L, LeBlanc M, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169:447–53. doi: 10.1001/archinternmed.2008.610. [DOI] [PubMed] [Google Scholar]
- 26.Taylor MJ, Gregory AM, Freeman D, Ronald A. Do sleep disturbances and psychotic-like experiences in adolescence share genetic and environmental influences ? J Abnorm Psychol. 2015;124:674–84. doi: 10.1037/abn0000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freeman D, Stahl D, McManus S, et al. Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1195–203. doi: 10.1007/s00127-011-0433-1. [DOI] [PubMed] [Google Scholar]
- 28.Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep-a prefrontal amygdala disconnect. Curr Biol. 2007;17:R877–8. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 29.Anderson C, Platten CR. Sleep deprivation lowers inhibition and enhances impulsivity to negative stimuli. Behav Brain Res. 2011;217:463–6. doi: 10.1016/j.bbr.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 30.Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia. Arch Gen Psychiatry. 2005;62:247–53. doi: 10.1001/archpsyc.62.3.247. [DOI] [PubMed] [Google Scholar]
- 31.Hansen K, Höfling V, Kröner-Borowik T, Stangier U, Steil R. Efficacy of psychological interventions aiming to reduce chronic nightmares: a meta-analysis. Clin Psychol Rev. 2013;33:146–55. doi: 10.1016/j.cpr.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 32.Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia:update of the recent evidence (1998-2004) Sleep. 2006;29:1398–414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- 33.Trockel M, Karlin BE, Taylor CB, Brown GK, Manber R. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. Sleep. 2015;38:259–65. doi: 10.5665/sleep.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freeman D, Waite F, Startup H, et al. Efficacy of cognitive behavioural therapy for sleep improvement in patients with persistent delusions and hallucinations (BEST): a prospective, assessor-blind, randomised controlled pilot trial. Lancet Psychiatry. 2015;2:975–83. doi: 10.1016/S2215-0366(15)00314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Andrade C, Suresh Kumar PN. Treating residual insomnia in schizophrenia: examining the options. Acta Psychiatr Scand. 2013;127:11. doi: 10.1111/acps.12019. [DOI] [PubMed] [Google Scholar]