Abstract
Background
Primary care providers often fail to identify patients who are overweight or obese or discuss weight management with them. Electronic health record (EHR)-based tools may help providers with the assessment and management of overweight and obesity.
Purpose
We describe the design of a trial to examine the effectiveness of EHR-based tools for the assessment and management of overweight and obesity among adult primary care patients, as well as the challenges we encountered.
Methods
We developed several new features within the EHR used by primary care practices affiliated with Brigham and Women’s Hospital in Boston, MA. These features included: 1) reminders to measure height and weight; 2) an alert asking providers to add overweight or obesity to the problem list; 3) reminders with tailored management recommendations; and 4) a Weight Management screen. We then conducted a pragmatic, cluster-randomized controlled trial in 12 primary care practices.
Results
We randomized 23 clinical teams (“clinics”) within the practices to the intervention group (n = 11) or the control group (n = 12). The new features were activated only for clinics in the intervention group. The intervention was implemented in 2 phases; the height and weight reminders went live on December 15, 2011 (Phase 1), and all of the other features went live on June 11, 2012 (Phase 2). Study enrollment went from December 2011 through December 2012, and follow-up ended in December 2013. The primary outcomes were 6-month and 12-month weight change among adult patients with BMI ≥ 25 who had a visit at one of the primary care clinics during Phase 2. Secondary outcome measures included the proportion of patients with a recorded BMI in the EHR; the proportion of patients with BMI ≥ 25 who had a diagnosis of overweight or obesity on the EHR problem list; and the proportion of patients with BMI ≥ 25 who had a follow-up appointment about their weight or were prescribed weight loss medication.
Lessons Learned
We encountered challenges in our development of an intervention within the existing structure of an EHR. For example, although we decided to randomize clinics within primary care practices, this decision may have introduced contamination and led to some imbalance of patient characteristics between the intervention and control practices. Using the EHR as the primary data source reduced the cost of the study, but not all desired data were recorded for every participant.
Conclusions
Despite the challenges, this study should provide valuable information about the effectiveness of EHR-based tools for addressing overweight and obesity in primary care.
Keywords: Overweight, obesity, primary care, electronic health records
INTRODUCTION
Overweight and obesity are problems of great clinical and public health importance. Over 35% of U.S. adults are obese (body mass index [BMI] ≥ 30 kg/m2) and another 33% are overweight (BMI 25–29.9 kg/m2).1 Overweight and obesity are associated with many serious health conditions, including type 2 diabetes, cardiovascular disease, and some cancers.2–5
Even small amounts of weight loss (3–5%) can lead to significant health benefits,6–11 and a variety of weight loss strategies have been shown to be effective.6, 10 Clinical practice guidelines urge providers to screen for overweight and obesity using BMI and to recommend appropriate treatment options.6, 10, 12–14 Despite these guidelines, however, primary care providers often fail to identify patients who are overweight or obese or to discuss weight management with them.15–24
Many providers use electronic health records (EHRs); adoption of EHRs has been increasing since the Health Information Technology for Economic and Clinical Health Act was introduced in 2009.25 Reminders and clinical decision support within EHRs have been shown to improve compliance with medical practice guidelines for conditions such as hypertension, diabetes, and coronary artery disease.26–28 Electronic health records also may be used to help providers with assessment and management of overweight and obesity, but few studies have examined this possibility.29
Therefore, the aims of this study were: 1) to develop EHR-based tools to help primary care providers identify, evaluate, and treat patients who are overweight or obese; and 2) to conduct a cluster-randomized trial to examine the effectiveness of the new EHR-based tools. In this paper, we describe the development of the EHR-based tools, some of the issues we encountered, and the design of the trial. Statistical analyses of outcome data are underway; those results will be reported separately.
METHODS
Development of EHR-based tools
We developed several new features within the Longitudinal Medical Record, an internally-developed, certified EHR used by all primary care and outpatient specialty practices at Brigham and Women’s Hospital.30 We first reviewed clinical practice guidelines on the identification, evaluation, and management of overweight and obesity that had been published by organizations such as the National Institutes of Health (NIH),6, 12 the U.S. Preventive Services Task Force,13 and the American College of Physicians.31, 32 The 2013 guidelines from the American Heart Association, American College of Cardiology, and The Obesity Society had not been published at the time this study was initiated.10 We next convened an expert panel that included primary care providers, registered dietitians, and information technology specialists who formulated recommendations for the proposed new features in the EHR. The expert panel’s recommendations were reviewed by two committees that oversee the design and content of the local EHR, in order to decide on the final set of features.
A major challenge was that the EHR-based tools had to fit within the existing structure of our EHR and into the clinical workflow of primary care providers. As a result, only a few of the features that were recommended by the expert panel could be incorporated. For example, one such feature was a graphical display of patients’ weight measurements over time. However, there is no graphical interface within our EHR system, and adding one was not feasible within the time and budgetary constraints of this project. Also, many clinical practice guidelines suggest that waist circumference be measured at annual visits or more frequently in overweight and obese adults, as waist circumference is an independent risk factor for cardiovascular morbidity and mortality.6 Although the expert panel considered incorporating waist circumference into the new features, there is no coded field for waist circumference in the EHR, and most primary care providers do not measure or document waist circumference. Thus, waist circumference was not included in the EHR modifications.
At the completion of this process, four new features were developed in the EHR.
Reminders to measure height and weight. Whenever a patient has no measurement of height in the EHR or no measurement of weight entered in the EHR within the past year, a reminder appears on the summary screen, asking the provider to enter a height and/or weight for the patient. The EHR automatically calculates BMI from patients’ most recent height and weight entries; therefore, any patient with both height and weight entered should have a BMI value in the EHR.
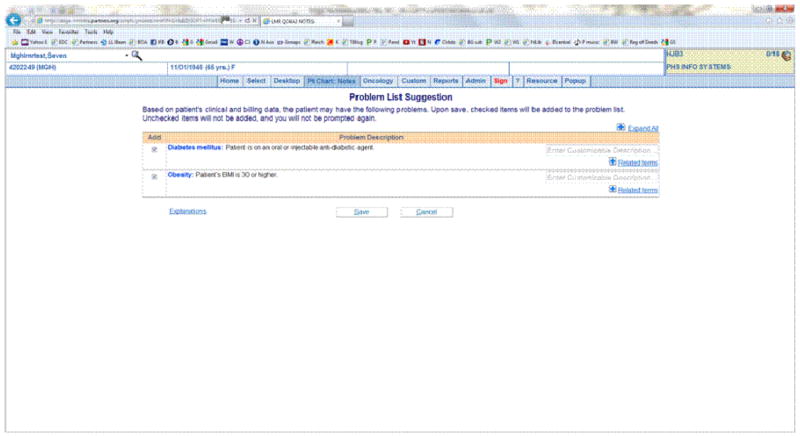
An alert asking providers whether they want to add overweight or obesity to the problem list, for patients with BMI 25–29.9 or ≥ 30 kg/m2, respectively. The alert appears as a “pop-up” screen, and the provider has the option to add overweight or obesity or to dismiss the alert (Figure 1). This alert was added to an existing clinical alerting system, introduced in May 2010, which was designed to improve the completeness of electronic problem list documentation for 17 other conditions.33, 34
Reminders with tailored management recommendations, based on patients’ BMI and other risk factors (e.g., hypertension, hyperlipidemia, type 2 diabetes) included on the problem list or identified from medications or laboratory results.34 For each patient with BMI ≥ 25, one reminder appears on the summary screen with a recommendation that was based on the NIH guidelines (Table 1).12
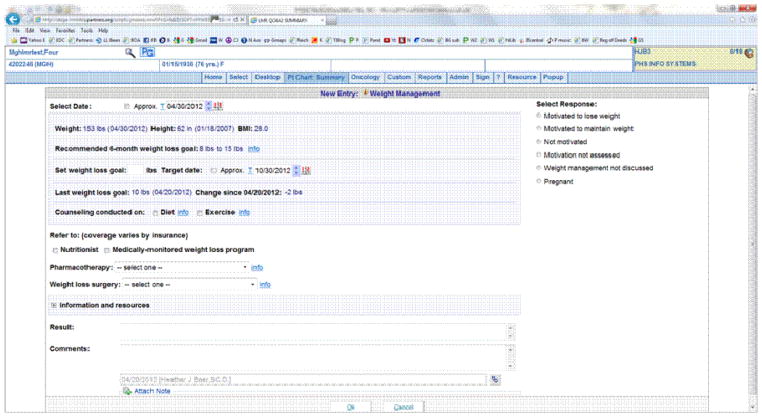
A Weight Management screen with several features, including tools to help providers assess patients’ motivation to lose weight, calculate and set a 6-month weight loss goal, refer patients to other resources (e.g., nutritionist or medically-monitored weight loss program), and access more information (Figure 2).
Figure 1.
Alert to add overweight or obesity to the problem list
Table 1.
Reminders with management recommendations for primary care providers
| BMI and other risk factors | Reminder text in EHR |
|---|---|
| BMI 25–26.9, or BMI 27–29.9 with no other risk factors | BMI ≥ 25: recommend weight loss or weight maintenance with diet, physical activity, and behavior therapy. |
| BMI 27–29.9 with ≥ 1 risk factor (e.g., cardiovascular disease, type 2 diabetes, sleep apnea, hypertension, dyslipidemia) | BMI ≥ 27 and comorbid condition(s): recommend weight loss with diet, physical activity, and behavior therapy. May be eligible for pharmacotherapy. |
| BMI 30–34.9, or BMI 35–39.9 with no other risk factors | BMI ≥ 30: recommend weight loss with diet, physical activity, and behavior therapy. May be eligible for pharmacotherapy. |
| BMI 35–39.9 with ≥ 1 risk factor (e.g., cardiovascular disease, type 2 diabetes, sleep apnea, hypertension, dyslipidemia) | BMI ≥ 35 and comorbid condition(s): recommend weight loss with diet, physical activity, and behavior therapy. May be eligible for pharmacotherapy and/or weight loss surgery. |
| BMI ≥ 40 | BMI ≥ 40: recommend weight loss with diet, physical activity, and behavior therapy. May be eligible for pharmacotherapy and/or weight loss surgery. |
BMI: body mass index; EHR: electronic health record
Figure 2.
Weight management screen
Study design and setting
After developing and testing the new features in the EHR, we conducted a pragmatic clinical trial within all primary care practices (n = 12) affiliated with Brigham and Women’s Hospital, an academic medical center in Boston.35 These practices are located in both urban and suburban areas across the greater-Boston area; they serve a racially and socioeconomically diverse population of patients. The 12 practices were divided into 23 clinical areas or teams (hereafter called “clinics”) based on pre-existing administrative divisions within some of the practices. For example, one of the larger practices is divided into three suites; each suite has its own team of individual providers (including physicians, nurse practitioners, and physician assistants), who work together as a cohesive unit. Each of these three suites was considered to be a separate clinic (cluster) for trial purposes and was randomized individually. Providers within a clinic see patients in that clinic only. There are trainees (clinical fellows and residents) in all of the clinics and medical students in some of them.
Randomization and intervention
Prior to randomization, the 23 clinics were grouped into 3 strata: hospital-based clinics (n = 10), community-based clinics (n = 11), and federally-qualified community health centers (n = 2). The clinics within each of these strata were randomly allocated to the control or intervention group using a computer algorithm, with 12 clinics randomized to the control group and 11 to the intervention group (Table 2).
Table 2.
Final allocation of clinics after randomization
| Strata | Practice | Clinic | Study arm |
|---|---|---|---|
| Hospital-based clinics (n = 10) | 1 | A | Control |
| 2 | B | Intervention | |
| 2 | C | Intervention | |
| 2 | D | Control | |
| 3 | E | Control | |
| 3 | F | Intervention | |
| 3 | G | Intervention | |
| 3 | H | Control | |
| 3 | I | Control | |
| 3 | J | Intervention | |
| Community-based clinics (n = 11) | 4 | K | Intervention |
| 5 | L | Control | |
| 6 | M | Intervention | |
| 6 | N | Control | |
| 6 | O | Control | |
| 7 | P | Control | |
| 8 | Q | Control | |
| 9 | R | Intervention | |
| 10 | S | Intervention | |
| 10 | T | Intervention | |
| 10 | U | Control | |
| Community health centers (n = 2) | 11 | V | Control |
| 12 | W | Intervention |
There were several reasons for choosing the clinic as the unit of randomization. First, all decision support within the EHR has to be activated either at the practice level or the clinic level; therefore, it was not possible to randomize individual patients or providers. Our rationale for randomizing clinics, rather than practices, was to achieve a better balance of patient characteristics in the intervention and control groups. For example, at the largest hospital-based practice, approximately 25% of patients are black and 15% are Hispanic; the other hospital-based practices have fewer black and Hispanic patients. If we had randomized practices, the entire large practice would have been assigned to either the intervention or the control group. Instead, the six clinics within this practice were randomized individually; three of them were assigned to the intervention group and three to the control group.
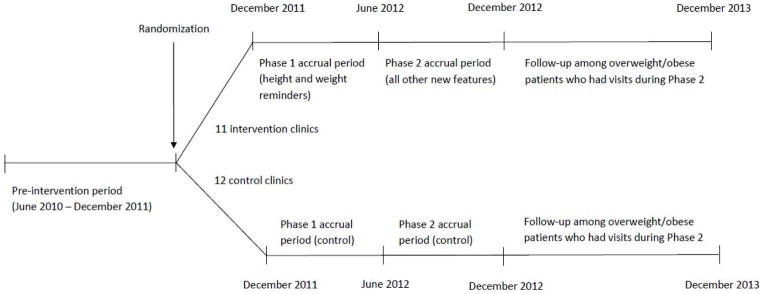
The new EHR features were activated for clinics in the intervention arm and were not activated for clinics in the control arm. The original intent was to activate all of the new features at the same time. However, due to other projects that the EHR development team was working on simultaneously, and the fact that modifications to the EHR are released for use at 6-month intervals, the intervention was implemented in 2 phases; the height and weight reminders went live on December 15, 2011 (Phase 1), and all of the other features went live on June 11, 2012 (Phase 2). Blinding of providers was not possible, given the nature of the intervention.
Before the new features were activated, the Principal Investigator (HJB) conducted a brief presentation for providers at each intervention clinic and circulated a quick reference guide with information about the new features. Although no written information about the new features was distributed to providers in control clinics, the presentations were conducted in regularly-scheduled practice meetings because that was the only time when most providers were available; providers in both intervention and control clinics within a given practice could attend these meetings.
The study was approved by the Partners Human Research Committee and was registered with ClinicalTrials.gov (NCT01480466). Patients in the participating clinics were not made aware of the intervention and were not required or requested to give consent.
Study population, data collection, and outcomes
There were different eligibility criteria and outcomes for Phase 1 and Phase 2 of the study. Both phases consisted of a 6-month accrual period, followed by 12 months of follow-up for the relevant outcomes (Figure 3).
Figure 3.
Study schema
For Phase 1, the study population included all adult patients (age 20 or older) who had a visit at one of the intervention or control clinics between December 15, 2011 and June 10, 2012. The main outcome was the proportion of patients with a documented BMI in the EHR within 12 months after the initial visit in the study “enrollment” period.
For Phase 2, the study population included all adult patients who had a visit at one of the intervention or control clinics between June 11, 2012 and December 10, 2012 and had a BMI ≥ 25 kg/m2. The primary outcomes for this phase were 6-month and 12-month weight change. Weight change over these 2 time periods was calculated as the difference between the patient’s weight at the first primary care visit during Phase 2 with BMI ≥ 25 (index visit) and his or her weight at the visit closest to 6 months later (4- to 8-month window) and closest to 12 months later (9- to 15-month window). Secondary outcome measures for Phase 2 included the proportion of patients with BMI ≥ 25 who had a diagnosis of overweight or obesity on the problem list; the proportion of patients with BMI ≥ 25 who had a subsequent appointment with a provider in the medical center’s Nutrition Consultation Service, the Program for Weight Management (the medically-monitored weight loss program), or the Center for Metabolic and Bariatric Surgery; and the proportion of patients with BMI ≥ 25 who were prescribed weight loss medications. Data for these outcomes, as well as other patient characteristics, were collected during routine clinical care and then extracted from coded fields in the EHR or from the medical center’s scheduling system. Similar data also were extracted for an 18-month pre-intervention period (6-month accrual period plus 12 months of follow-up), i.e., altogether from June 15, 2010 to December 14, 2011.
Provider data collection and outcomes
We assessed providers’ attitudes about management of overweight and obesity using web-based surveys.36 Links to the surveys were sent by email to all primary care providers at the intervention and control clinics immediately before Phase 1 of the intervention period and again at the end of Phase 2. The survey at the end of the intervention period included additional questions for providers in the intervention clinics, which were designed to assess the usability of the new features in the EHR.37 At the end of the second survey, providers in the intervention group also were asked whether they would be interested in participating in a 15-minute telephone interview to discuss the new features in more detail.
Power and sample size
Based on previous studies in the primary care setting, we estimated that the difference in weight change between patients in the intervention and control clinics would be between 2.2 and 7.1 pounds.9, 38 To be conservative, we calculated the necessary sample size for detecting a difference of 2 pounds in the amount of weight change among patients in the intervention and control clinics, using a standard deviation of 9 pounds (unpublished data.)
We initially assumed that weight change in each individual patient would be an independent event, not influenced by clustering effects at the level of the provider. With these assumptions, using a two-sided Student’s t test with 90% power and α (probability of type I error) of 0.05, we estimated that we would need 427 patients per group. We then used the following formula to account for the intra-provider correlation between patients:
where N1 is the sample size under the assumption of independence, m is the average number of patients per provider, and ρ is the intraclass correlation coefficient (ICC). Assuming an average of 100 patients per provider and using an ICC of 0.05, based on ICCs that have been observed for weight and similar measures in other cluster randomized trials in primary care,39 the required sample size would be 2541 patients per group. We expected that there would be approximately 60,000 patients with visits at the intervention and control clinics during Phase 2 of the study, that 70% of these patients (n = 42,000) would have a recorded BMI in the EHR, and that at least 60% of patients with a recorded BMI (n = 25,200) would have a BMI ≥ 25 kg/m2. Thus, the available number of patients (approximately 12,600 per group) should be sufficient under a wide range of assumptions. In fact, even if we limited our power estimates to the 320 providers with 20 or more patients and conservatively assumed only 20 patients per provider in our calculations, we still expected to have 3200 patients per arm (greater than the 2541 proposed above), and to have an effective sample size of 1648 per arm, much greater than the 427 required for 90% power.
We also calculated the necessary sample size for the secondary outcome of diagnosis of overweight and obesity among patients with BMI ≥ 25 kg/m2, assuming a percentage of 16% at the beginning of the study based on our preliminary data.40 We judged that a 10% absolute increase in diagnosis would be clinically meaningful. Prior to accounting for clustering, using a two-sided Chi-square test with 90% power and α of 0.05, 347 patients would be needed per group. Using the same formula as shown above to account for clustering, the required sample size to detect this change would be 2065 patients per group. Again, the large number of available patients in the primary care practices was expected to provide sufficient power under a range of assumptions.
Nested substudy
We conducted a smaller substudy in a sample of overweight and obese patients within the main trial to obtain more detailed information about their experiences with weight management and about discussion of weight management with their primary care providers, as these outcomes are difficult to assess using data from the EHR. In addition, we wanted to collect more systematic data on weight change at 6 months after the primary care visit for patients in the substudy, since many patients in the main trial would not have another visit at their primary care practice within the 4- to 8-month timeframe. To be eligible for the substudy, patients had to have a new patient visit or an annual examination during Phase 2, be between ages 20 and 70 at the time of the visit, and speak English. They also had to have a recorded BMI in the past year of 30–50 kg/m2, or a recorded BMI in the past year of 27–29.9 kg/m2 as well as a diagnosis of type 2 diabetes, hypertension, or hyperlipidemia on their problem list.
Eligible patients were mailed a written survey about their past experiences with weight management, their diet and physical activity, and their motivation and self-efficacy around weight loss. The survey also included questions about their most recent primary care visit, such as whether the provider recommended that they lose weight, helped them to set a specific weight loss goal, or gave them any information or referred them to any resources related to weight management.
At the end of the survey, patients were asked whether they would be interested in participating in a 30-minute study visit. A research assistant called interested patients and screened them over the telephone to confirm their eligibility. The research assistant scheduled eligible patients for a study visit 6 months (± 2 weeks) after the patient’s routine primary care visit. At the study visit, a research coordinator measured the patient’s height, weight, and blood pressure, and the patient completed another survey. Patients had to provide written consent for the substudy.
Due to financial and logistical constraints, we could enroll a maximum of 200 patients in the nested substudy. Given this sample size and assuming an ICC of 0.05 between patients treated by the same provider, with an average of 2 patients per provider, we estimated that we would have 86% power to detect a 4-pound difference in weight change between patients in the intervention and control groups.
Planned analyses
There were 88,150 patients who had a visit during either Phase 1 or Phase 2 of the study (49,066 in the control group and 39,084 in the intervention group). There were some minor differences in demographic characteristics between patients in the intervention and control clinics (Table 3). For example, there was a higher percentage of women in the intervention group (67.3%) than the control group (60.6%) because there is one women’s health clinic, which was randomly allocated to the intervention group. There also was a higher percentage of Hispanic patients in the intervention (18.7%) than the control group (11.3%) because there is one Spanish clinic, which was randomly allocated to the intervention group.
Table 3.
Demographic characteristics of patients with visits in Phase 1 or Phase 2
| Patient characteristics | Control Clinics | Intervention Clinics |
|---|---|---|
| No. in group | 49,066 | 39,084 |
| Mean age, years (SD) | 50.1 (16.6) | 51.0 (16.1) |
| Gender (%) | ||
| Women | 60.6 | 67.3 |
| Men | 39.4 | 32.7 |
| Race/ethnicity (%) | ||
| White, not Hispanic | 69.3 | 59.4 |
| Black, not Hispanic | 10.3 | 13.8 |
| Hispanic | 11.3 | 18.7 |
| Other or missing | 9.2 | 8.1 |
| Primary language (%) | ||
| English | 91.4 | 86.6 |
| Spanish | 5.6 | 10.8 |
| Other or missing | 3.0 | 2.6 |
SD: standard deviation
All statistical analyses are being conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC). We are comparing changes in BMI documentation from the pre-intervention period to Phase 1 for patients in the intervention and control clinics, using mixed effects logistic regression models (SAS PROC GLIMMIX) to account for the within-clinic and within-provider correlation and to adjust for other covariates. We are using a similar approach to compare changes in management outcomes from the pre-intervention period to Phase 2 for patients with BMI ≥ 25 kg/m2 in the intervention and control clinics.
In addition, we are comparing weight change over 6 months and 12 months for patients with BMI ≥ 25 kg/m2 in the intervention and control clinics during Phase 2, using mixed effects linear regression models (SAS PROC MIXED) to account for the within-clinic and within-provider correlation and to adjust for baseline weight as well as other covariates. Because the trial was conducted within routine clinical care, not all patients with a recorded weight during Phase 2 have a follow-up measurement of weight during the required visit windows. Patients who are missing follow-up data on weight may be systematically different from those who are not. Also, the amount of missing weight data may differ between the intervention and control groups; thus, including only patients with non-missing follow-up weight data could cause bias. To reduce this bias, we will use Markov chain Monte Carlo multiple imputation (SAS PROC MI) to predict missing weights at 6 months and 12 months, using patients’ available weight measurements and data on other covariates, such as age, gender, race/ethnicity, risk factors, and comorbidities.
For patients in the nested substudy, we are conducting similar analyses to compare differences in weight change and other outcomes for patients in the intervention and control clinics. We also are comparing changes in attitudes about management of overweight and obesity among providers in the intervention and control clinics.
DISCUSSION
Because many studies have shown that providers under-identify overweight and obese patients and fail to counsel them about weight management,15–24 we added reminders, alerts, and clinical decision support within our EHR to help primary care providers address overweight and obesity with their patients. We conducted a cluster-randomized clinical trial to evaluate the effectiveness of these tools in 23 clinics (11 intervention, 12 control) with a total of 88,150 eligible patients. As of December 2014, we have completed data collection and currently are analyzing trial outcome data.
Few studies have examined the effects of EHR-based tools on the identification, evaluation, and treatment of overweight and obesity in adults.29 Among the studies that have been conducted, most have focused only on increasing identification of overweight and obesity and have not included additional features to assist providers with management, such as patient-specific recommendations or tools for referring patients to other resources. Moreover, almost all of the studies have focused only on provider performance outcomes and have not examined effects on patient outcomes, such as changes in weight, diet, and physical activity. Our study addressed these gaps by adding several features to assist providers with management and by assessing a number of patient outcomes, such as weight change over 6 and 12 months.
Lessons Learned
One of the most important lessons from this study is that it can be challenging to develop and implement an intervention within an existing EHR without making major changes to the EHR architecture or clinical workflow. We obtained buy-in and approval from several different groups, including the primary care practice leaders and our local EHR oversight committee, a process that took a substantial amount of time. Furthermore, researchers had to be realistic about what could be accomplished in the context of routine clinical practice. Our expert panel originally requested many changes to the EHR that could not be incorporated; the new features were less comprehensive than originally anticipated. As a result, the effect of the intervention may be smaller than expected initially.
There also are some unique methodological issues with this kind of pragmatic trial. It was not possible to randomize at the level of the individual patient or provider. We decided to randomize clinics instead of multi-clinic practices to try to make the intervention and control groups more comparable and, thus, to minimize confounding. However, some clinic and patient characteristics were not balanced as a result of assignment of clinics with unique populations to one trial arm or the other. Furthermore, the main disadvantage of randomizing clinics rather than practices is that there is the potential for contamination, since individual providers in intervention and control clinics may be within the same practices and could discuss management of overweight and obesity, thus leading to attenuation of the estimated effect of the intervention.
Finally, using the EHR as the primary source of data is advantageous from the standpoint of cost and logistics, but imposes limitations. In clinical practice, many patients do not come in for visits at regular intervals. Thus, no index or return visit may occur during a specified interval, resulting in missing data and the potential for selection bias. In addition, some of the outcomes of interest may not be well-documented in the EHR. Therefore, trial investigators must give careful thought as to a design that minimizes missing data and to analyses to account for missing outcomes for some trial participants.
Conclusions
In summary, overweight and obesity often are not adequately addressed in primary care. Use of electronic health records has been increasing in recent years, and clinical decision support within EHRs has been shown to improve compliance with medical practice guidelines for other chronic conditions. The current study sought to examine the effectiveness of EHR-based tools for addressing overweight and obesity in primary care. The results should provide valuable information to providers and healthcare organizations about the use of EHRs for addressing overweight and obesity in the primary care setting.
Acknowledgments
Grant support: AHRQ K01-HS-019789
Funding
This work was supported by a mentored research scientist career development award from the Agency for Healthcare Research and Quality [grant number K01-HS-019789] and a pilot and feasibility grant from the Boston Nutrition Obesity Research Center. Dr. Wee is supported by a midcareer mentorship award from the National Institutes of Health [grant number K24-DK-087932].
The authors acknowledge Ms. Li Chen, Dr. Florencia Halperin, Dr. Andrew Karson, Ms. Lynn Klokman, Ms. Irina Kofman, Ms. Katherine McManus, Dr. Harley Ramelson, Dr. Caren Solomon, and Dr. Jane Sillman for their contributions to this study.
Footnotes
ClinicalTrials.gov identifier: NCT01480466
Conflict of interest
None declared.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Overweight obesity, and health risk. National Task Force on the Prevention and Treatment of Obesity. Archives of internal medicine. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, McDowell MA, Flegal KM. NCHS data brief no 1. Hyattsville, MD: National Center for Health Statistics; 2007. Obesity among adults in the United States - no change since 2003–2004. [PubMed] [Google Scholar]
- 5.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132:2087–102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 6.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 7.The prevention or delay of type 2 diabetes. Diabetes Care. 2002;25:742–9. doi: 10.2337/diacare.25.4.742. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JW, Konz EC. Obesity and disease management: effects of weight loss on comorbid conditions. Obes Res. 2001;9(Suppl 4):326S–34S. doi: 10.1038/oby.2001.138. [DOI] [PubMed] [Google Scholar]
- 9.Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–67. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2013 [Google Scholar]
- 11.Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2004;110:2952–67. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 12.The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. National Heart, Lung, and Blood Institute (NHLBI); 1998. [Google Scholar]
- 13.Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139:930–2. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 14.McTigue KM, Harris R, Hemphill B, et al. Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;139:933–49. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 15.Abid A, Galuska D, Khan LK, Gillespie C, Ford ES, Serdula MK. Are healthcare professionals advising obese patients to lose weight? A trend analysis. Med Gen Med. 2005;7:10. [PubMed] [Google Scholar]
- 16.Bardia A, Holtan SG, Slezak JM, Thompson WG. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clin Proc. 2007;82:927–32. doi: 10.4065/82.8.927. [DOI] [PubMed] [Google Scholar]
- 17.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? Jama. 1999;282:1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 18.Ko JY, Brown DR, Galuska DA, Zhang J, Blanck HM, Ainsworth BE. Weight loss advice U.S. obese adults receive from health care professionals. Prev Med. 2008;47:587–92. doi: 10.1016/j.ypmed.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loureiro ML, Nayga RM., Jr Obesity, weight loss, and physician’s advice. Soc Sci Med. 2006;62:2458–68. doi: 10.1016/j.socscimed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 20.Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Archives of internal medicine. 2009;169:313–4. doi: 10.1001/archinternmed.2008.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma J, Xiao L, Stafford RS. Adult obesity and office-based quality of care in the United States. Obesity (Silver Spring) 2009;17:1077–85. doi: 10.1038/oby.2008.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McAlpine DD, Wilson AR. Trends in obesity-related counseling in primary care: 1995–2004. Med Care. 2007;45:322–9. doi: 10.1097/01.mlr.0000254575.19543.01. [DOI] [PubMed] [Google Scholar]
- 23.Rodondi N, Humair JP, Ghali WA, et al. Counselling overweight and obese patients in primary care: a prospective cohort study. Eur J Cardiovasc Prev Rehabil. 2006;13:222–8. doi: 10.1097/01.hjr.0000209819.13196.a4. [DOI] [PubMed] [Google Scholar]
- 24.Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? Results from a multistate survey. Archives of internal medicine. 2000;160:2334–9. doi: 10.1001/archinte.160.15.2334. [DOI] [PubMed] [Google Scholar]
- 25.The American Recovery and Reinvestment Act: HR1 2009.
- 26.Hicks LS, Sequist TD, Ayanian JZ, et al. Impact of computerized decision support on blood pressure management and control: a randomized controlled trial. J Gen Intern Med. 2008;23:429–41. doi: 10.1007/s11606-007-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murff HJ, Gandhi TK, Karson AK, et al. Primary care physician attitudes concerning follow-up of abnormal test results and ambulatory decision support systems. Int J Med Inform. 2003;71:137–49. doi: 10.1016/s1386-5056(03)00133-3. [DOI] [PubMed] [Google Scholar]
- 28.Sequist TD, Gandhi TK, Karson AS, et al. A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. Journal of the American Medical Informatics Association: JAMIA. 2005;12:431–7. doi: 10.1197/jamia.M1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baer HJ, Cho I, Walmer RA, Bain PA, Bates DW. Using electronic health records to address overweight and obesity: a systematic review. American Journal of Preventive Medicine. 2013;45:494–500. doi: 10.1016/j.amepre.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 30.Poon EG, Wald J, Bates DW, Middleton B, Kuperman GJ, Gandhi TK. Supporting patient care beyond the clinical encounter: three informatics innovations from partners health care. AMIA Annu Symp Proc. 2003:1072. [PMC free article] [PubMed] [Google Scholar]
- 31.Bray GA, Wilson JF. In the clinic Obesity. Ann Intern Med. 2008;149:ITC4-1-15. doi: 10.7326/0003-4819-149-7-200810070-01004. quiz ITC4-6. [DOI] [PubMed] [Google Scholar]
- 32.Snow V, Barry P, Fitterman N, Qaseem A, Weiss K. Pharmacologic and surgical management of obesity in primary care: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2005;142:525–31. doi: 10.7326/0003-4819-142-7-200504050-00011. [DOI] [PubMed] [Google Scholar]
- 33.Wright A, Pang J, Feblowitz JC, et al. Improving completeness of electronic problem lists through clinical decision support: a randomized, controlled trial. Journal of the American Medical Informatics Association: JAMIA. 2012;19:555–61. doi: 10.1136/amiajnl-2011-000521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright A, Pang J, Feblowitz JC, et al. A method and knowledge base for automated inference of patient problems from structured data in an electronic medical record. Journal of the American Medical Informatics Association: JAMIA. 2011;18:859–67. doi: 10.1136/amiajnl-2011-000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–32. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- 36.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brooke J. SUS: a “quick and dirty” usability scale. In: Jordan PW, Thomas B, Weerdmeester BA, McClelland IL, editors. Usability evaluation in industry. London: Taylor & Francis; 1996. pp. 189–94. [Google Scholar]
- 38.Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med. 2009;24:1073–9. doi: 10.1007/s11606-009-1042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parker DR, Evangelou E, Eaton CB. Intraclass correlation coefficients for cluster randomized trials in primary care: the cholesterol education and research trial (CEART) Contemp Clin Trials. 2005;26:260–7. doi: 10.1016/j.cct.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 40.Baer HJ, Karson AS, Soukup JR, Williams DH, Bates DW. Documentation and diagnosis of overweight and obesity in electronic health records of adult primary care patients. JAMA Intern Med. 2013;173:1648–52. doi: 10.1001/jamainternmed.2013.7815. [DOI] [PubMed] [Google Scholar]