Synopsis
US children with emotional, mental, or behavioral conditions (EMB) have disproportionate exposure to potentially traumatizing adverse childhood experiences (ACEs) (70.7% EMB vs. 46.9% non-EMB). Neuroscience, epigenetic, developmental, social, epidemiologic, and other sciences provide theoretical and empirical explanations for observed early and lifelong physical, mental, emotional, educational, and social impacts of the trauma and chronic stress that can result from ACEs. Together, these sciences point to possibilities to strengthen families and promote child resilience and school and life success using mindfulness-based, mind-body approaches (MBMB) that neuroscience and other studies show promote healthy regulation of stress, resilience, and healing from emotional trauma. This paper examines US population-based associations between prevalence of EMB, ACEs, and risk regulating protective factors that are potentially malleable using MBMB, such as child resilience, parental coping and stress, and parent-child engagement. US rates of MBMB use among children with EMB are estimated. Findings encourage family-centered and mindfulness-based approaches to address social and emotional trauma and potentially interrupt intergenerational cycles of ACEs and prevalence of EMB among children and youth.
Keywords: child and adolescent mental health, adverse childhood experiences, resilience, protective factors, parent stress, mindfulness
Introduction
An estimated 19.8% of all US children have a chronic condition requiring more than routine health and related services. This prevalence increases to 31.6% for the nearly one fourth of US children exposed to two or more adverse childhood experiences (ACEs),1 such as those experiences studied in the widely recognized Centers for Disease Control (CDC) and Kaiser Permanente study of adults exposed to ACEs.2 Adapted for children and parental report, the National Survey of Children's Health (NSCH) now assesses nine types of ACEs, including serious economic hardship, witnessing or experiencing violence in the neighborhood, alcohol, substance abuse, domestic violence, mental health problems in the home, parental divorce, loss of parents to death or incarceration, and social rejection through racial and ethnic discrimination. Measured in this way, NSCH findings confirm those from the CDC/Kaiser and other studies revealing a linear, dose-response effect of ACEs across a wide range of health and social impacts. This effect is stable even in the absence of more detailed information about the occurrence, frequency, and severity of any specific event or set of experiences. Exposure to ACEs is 71% for all US children in fair or poor health. Additionally, US children exposed to ACEs are substantially and significantly more likely to repeat a grade in school and lack resilience, such as usually or always being able to stay calm and in control when faced with a challenge.1
Reports on the NSCH show that 70% of the 7.9% of US children ages 2-17 with attention deficit hyperactivity disorder (ADHD) have been exposed to ACEs. Less is known about ACEs prevalence and impact for US children with any type of emotional, mental, or behavioral condition(s) (EMB). Because common symptoms are shared by children exposed to ACEs and those diagnosed with EMB,3,4 it is important to understand the prevalence of ACEs exposure among children with EMB, how these phenomena are related to each other, and to assess whether adaptations are needed in approaches to the prevention, diagnosis, or treatment of EMB in children who may also carry the social and emotional trauma and chronic stress that can result from ACEs.
Growing neuroscience, epigenetic, social, developmental, epidemiologic, resilience and other sciences are coming together to explain observed early and lifelong impacts of childhood social and emotional trauma and chronic stress that can arise from ACEs and perhaps, in turn, evolve into or contribute to EMB.5-12 Catalyzed by this evolution of scientific understanding, and anchored in recognition of safe, stable, and nurturing relationships as a pillar for child and adult health,13ACEs, trauma-informed practices (a popular terminology for responding to ACEs), and intergenerational approaches are a growing focus in clinical, early care, educational, and community contexts, especially for children with EMB, for promoting trauma healing and resilience for the entire family. 14-16
Integral to many of these approaches to addressing the emotional trauma and chronic stress that can arise with ACEs are mindfulness-based, mind-body methods (MBMB), which now enjoy growing evidence of effectiveness to promote trauma healing, resilience, and self-regulation of stress, emotions, and behavior.17-22 This evidence has accumulated sufficiently for the American Academy of Pediatrics to have begun to develop what is expected to be a forthcoming policy statement on the use of mind–body methods in clinical practice. Systematic reviews of research on MBMB suggest that these methods can attenuate cognitive, behavioral and emotional symptoms of conditions like anxiety, ADHD, and depression, can decrease physical pain, promote positive health behaviors and social functioning and increase school engagement and attendance. Purposeful moment-by-moment presence and self-awareness of one’s breathing, body sensations, emotions, and/ or thoughts in a nonjudgmental manner (eg, mindfulness) is a common, cross- cutting component of most mind–body methods, like biofeedback, guided imagery, yoga, hypnosis, and meditation.
Showing relevance of MBMB to parents, Whitaker and colleagues assessed ACEs exposure, health outcomes, and mindfulness among adults, showing that among persons reporting three or more ACEs, those in the highest quartile of mindfulness had a prevalence of multiple health conditions two-thirds that of those in the lowest quartile.17 Other studies conclude that regardless of the presence of trauma, youth-based mindfulness-based stress reduction (MBSR) training in primary care and other settings is effective in improving self-regulation of stress, improving mental health symptoms, lowering blood pressure, and improving overall coping.18-22
Although research has demonstrated that MBMBs, such as mindfulness, yoga, Tai chi, and other forms of meditative movement can be effective for general well-being and to address a wide variety of symptoms and conditions, 23-25 this paper focuses on the promising application of MBMB to children and youth with EMB, most of whom are also exposed to ACEs and may carry trauma and chronic stress owing to these experiences. Specifically, this paper aims to provide further insights into why children with ACEs may (or may not) also experience EMB with the goal to inform burgeoning efforts to both reduce EMB prevalence as well as interrupt intergenerational cycles of ACEs.13-14 To begin, we examined associations among prevalence of EMB among US children with varying levels of ACEs and by differences in risk regulating factors hypothesized to ameliorate negative effects of ACEs, which research shows are also potentially malleable using MBMB. These factors include child resilience and factors indicative of the presence of safe, stable and nurturing family relationships, such as parental coping and stress and parent-child engagement. Rates of use of MBMB among children with EMB is estimated along with their total expenditures for conventional medical care, which may point to delayed use of MBMB that could attenuate severity and costs of care for children with EMB.
Methods
Population and Data
This study used data from the 2011–12 NSCH, the 2007 National Health Interview Survey (NHIS), the NHIS Child Complementary and Alternative Medicine (CAM) Supplement and the 2008 Medical Expenditure Panel Survey (MEPS).26 The NSCH surveyed a representative sample of children ages 0–17 (95,677 children, with approximately 1,800 per state). Child-level household surveys were conducted with parents or guardians under the leadership of the Maternal and Child Health Bureau and implemented through the National Center for Health Statistics (NCHS). Analyses here are limited to children ages 2-17 owing to age parameters for questions related to whether a child had an emotional, mental, or behavioral condition. Further stratification occurred where variables were only available for school-age children (ages 6-17). Data were weighted to represent the population of non-institutionalized children nationally and in each state.
Data from the 2007 NHIS and 2008 MEPS were used as the most recent available that allow linking data from the NHIS-CAM Supplement to the MEPS health care expenditures data sets to develop estimates of mind-body methods among children with EMB problems in the US. To estimate prevalence of EMB conditions and use of mind-body methods, we linked five 2007 NHIS data files (Family, Imputed Income, Person, Sample Child, and Child CAM Supplement), resulting in an integrated NHIS data file that included 9,417 sampled children. To obtain health care expenditure data for children with EMB and who used mind-body methods, we further linked this integrated NHIS file with the 2008 MEPS Full-Year Consolidated Household File, which included the NHIS sampling frame (Panel 13). The NHIS/MEPS linked file contains 2,411 sample children and were weighted to represent the US population of children ages 0-17. Weights for the NHIS/MEPS linked file were constructed adjusting the MEPS Panel 13 weights to reflect the NHIS probabilities of selection for sub-sampling of children and then, as recommended, weights were further adjusted through ranking by age, sex, race/ethnicity, and US geographic region.
Key Measures
As noted, the 2011–12 NSCH ACEs questions are based on those used in the adult CDC/Kaiser study, with modifications overseen by a federal Maternal and Child Health Bureau technical expert panel and evaluated through standard survey item testing by the National Center for Health Statistics. The NSCH included nine ACEs deemed valid for reporting by parents and guardians as outlined.1 To evaluate associations between EMB and ACEs, an EMB variable was constructed to include whether a child have been told by a doctor or other provider that they currently have ADHD, depression, anxiety, behavior or conduct problems, autism spectrum disorder, developmental delay, or Tourette syndrome. Variables assessing protective factors were also constructed using the NSCH data and included child resilience (defined simply here as usually or always “staying calm and in control when faced with a challenge,” for children ages 6–17), engagement in school (multi-item measure), and missed school days. Variables constructed to assess hypothesized risk regulating associations between EMB, ACEs, and protective family relationship factors included parental coping, parental aggravation and stress owing to parenting, whether a child and parent do well sharing ideas and talking about things that matter, whether a child's parent knows her or his child's friends and participates in child's events and activities, and the mental health status of the child's mother.
For analyses of the NHIS and MEPS data, six health conditions or problems asked about in the 2007 NHIS were grouped together to identify children with EMB conditions or problems: (a) parent has ever been told by a health professional that child has ADHD or ADD; (b) parent has been told by a health professional that child experienced depression or phobia/fears in the past 12 months and/or (c) parent report that child experienced anxiety/stress, incontinence/bed wetting, or insomnia/trouble sleeping in the past 12 months. MBMBs included biofeedback, hypnosis, yoga, Tai chi, Qi gong, meditation, guided imagery, progressive relaxation, deep breathing exercises, support group meeting, and stress management class (like Mindfulness-Based Stress Reduction). Total conventional medical care expenditures estimates were constructed based on standard two-part models and were adjusted for child's age, sex, race/ethnicity, income, and US region. All variables used in this study have been documented previously, and their properties and coding are presented in publicly available NSCH and NHIS variable codebooks developed by the Child and Adolescent Health Measurement Initiative.26
Analytic Methods
Bivariate, rate ratio analyses, chi square tests, and t tests were used in addition to multivariate logistic regression models to evaluate variations in prevalence of EMB by a child's ACEs status and to further evaluate these associations by a child's age, household income, resilience, and protective family relationship factors. Similar analyses were conducted to determine the impact of ACEs on school engagement and missed school among children with EMB, and potential mitigating impact when a child had learned and demonstrated resilience. All regression analyses controlled for child age, sex, race/ethnicity, health insurance status/type, and household income (for models not stratified by income). We used SPSS, version 22 (SPSS Inc, Chicago, IL). Unless otherwise noted, all adjusted odds ratios that we report were significant based on their 95% confidence intervals.
Results
Characteristics of US Children with Emotional, Mental, or Behavioral Conditions by Adverse Childhood Experiences Status
Children with EMB are disproportionately older, compared to children generally. This is especially true if they also experience multiple ACEs. Children with EMB are also more likely to be male, regardless of their ACEs status. Independent of their EMB status, children with multiple ACEs are more likely to live in lower income homes and have public insurance; however, those with both ACEs and EMB are especially likely to have public insurance (63.9%). Children without EMB but with multiple ACEs are 1.4 time more likely to be uninsured. (Table 1)
Table 1.
Demographic and health insurance characteristics among US children age 2-17 with ACEs by emotional, mental, or behavioral health status. Data from 2011-2012 National Survey of Children's Health
| Demographic and Health Insurance Characteristics | All US children, 2-17 Years (%) | ACEs 2-17 Years (%) | Children with Emotional, Mental, or Behavioral Problemsa, 2-17 years (%) | Children With Emotional, Mental, or Behavioral Problemsa, 2-17 years (%) | Children Without Emotional, Mental, or Behavioral Problemsa, 2-17 years (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥4 ACEs | 2-3 ACEs | 1 ACE | None | Yes | No | No ACEs | 1 ACE | ≥2 ACEs | No ACEs | 1 ACE | ≥2 ACEs | ||
| All children, 2-17 years | 100 | 7.1 | 17.6 | 25.6 | 49.7 | 14.0 | 86.0 | 29.3 | 25.0 | 45.7 | 53.1 | 25.7 | 21.2 |
| Age (years) | |||||||||||||
| 2-5 | 24.4 | 11.8 | 17.1 | 23.5 | 29.1 | 11.2 | 26.5 | 13.1 | 12.5 | 8.9 | 30.6 | 25.3 | 17.9 |
| 6-11 | 37.3 | 35.4 | 37.5 | 37.4 | 37.3 | 39.6 | 37.0 | 42.5 | 37.3 | 38.9 | 36.8 | 37.5 | 36.2 |
| 12-17 | 38.3 | 52.8 | 45.4 | 39.0 | 33.6 | 49.2 | 36.5 | 44.5 | 50.1 | 52.1 | 32.6 | 37.3 | 45.9 |
| Sex | |||||||||||||
| Male | 51.2 | 52.4 | 50.3 | 51.6 | 51.3 | 63.7 | 49.2 | 68.3 | 62.0 | 61.7 | 49.8 | 50.0 | 47.1 |
| Female | 48.8 | 47.6 | 49.7 | 48.4 | 48.7 | 36.3 | 50.8 | 31.7 | 38.0 | 38.3 | 50.2 | 50.0 | 52.9 |
| Race | |||||||||||||
| Hispanic | 23.2 | 21.8 | 22.8 | 26.2 | 21.8 | 17.3 | 24.1 | 15.8 | 19.4 | 17.0 | 22.4 | 27.3 | 24.5 |
| White, Non-Hispanic | 53.0 | 50.3 | 48.1 | 49.3 | 57.1 | 59.2 | 52.0 | 66.5 | 57.1 | 55.5 | 56.2 | 48.1 | 46.3 |
| Black, Non-Hispanic | 13.8 | 16.4 | 19.5 | 15.7 | 10.3 | 14.8 | 13.6 | 10.4 | 16.4 | 16.8 | 10.3 | 15.5 | 19.3 |
| Other, Non-Hispanic | 10.1 | 11.5 | 9.6 | 8.8 | 10.7 | 8.8 | 10.3 | 7.4 | 7.1 | 10.7 | 11.0 | 9.0 | 9.9 |
| Household Income (FPL%) | |||||||||||||
| 0-99 | 21.9 | 39.1 | 31.8 | 26.5 | 13.6 | 27.5 | 21.0 | 13.8 | 24.8 | 38.1 | 13.6 | 26.8 | 32.5 |
| 100-199 | 21.6 | 28.5 | 27.1 | 25.9 | 16.5 | 22.9 | 21.4 | 13.1 | 24.7 | 28.3 | 16.8 | 26.1 | 27.2 |
| 200-399 | 28.5 | 24.0 | 27.6 | 27.5 | 30.1 | 26.6 | 28.8 | 30.1 | 28.5 | 23.4 | 30.1 | 27.4 | 27.7 |
| ≥400 | 28.0 | 8.4 | 13.5 | 20.0 | 39.8 | 22.9 | 28.8 | 43.0 | 22.0 | 10.2 | 39.5 | 19.7 | 12.7 |
| Insurance type | |||||||||||||
| Public | 36.3 | 63.2 | 51.7 | 41.2 | 24.3 | 48.4 | 34.3 | 27.7 | 44.7 | 63.9 | 24.0 | 40.7 | 51.8 |
| Private | 57.9 | 28.4 | 41.5 | 52.0 | 71.2 | 47.7 | 59.5 | 70.1 | 51.5 | 31.2 | 71.3 | 52.1 | 40.1 |
| Uninsured | 5.8 | 8.4 | 6.8 | 6.8 | 4.6 | 3.9 | 6.1 | 2.2 | 3.8 | 4.9 | 4.8 | 7.2 | 8.1 |
| Insurance adequacyb | |||||||||||||
| Adequate | 75.8 | 74.3 | 75.0 | 73.7 | 77.4 | 68.8 | 77.0 | 68.3 | 65.6 | 71.0 | 78.2 | 75.0 | 76.2 |
| Inadequate | 24.2 | 25.7 | 25.0 | 26.3 | 22.6 | 31.2 | 23.0 | 31.7 | 34.4 | 29.0 | 21.8 | 25.0 | 23.8 |
Abbreviations: ACEs: adverse childhood experiences; FPL: federal poverty level.
Defined as children who qualify on the Children with Special Health Care Needs Screener criteria for having emotional, developmental, or behavioral conditions that have lasted or are expected to last for ≥12 months and require treatment or counseling and/or who have had a doctor indicate current presence of ≥1 of 7 emotional, mental, or behavioral conditions asked in the National Survey of Children's Health.
Among currently insured children.
Prevalence of Emotional, Mental, or Behavioral Conditions by Adverse Childhood Experiences Status, Household Income, and Age of Child
Across levels of ACEs (1, 2-3, 4+), prevalence of EMB among US children ages 2-17 is 1.65 to 4.46 times higher compared to those with no ACEs. (Table 2) Consistent effects exist across child household income and age groups. Strongest effects are found for younger children (ages 2-5) and those living in households with incomes below 200% of the federal poverty level. Across four income categories, prevalence of EMB is 3.77 to 5.40 higher for children and youth exposed to four or more ACEs. Differences in the prevalence of EMB for these children are not statistically significant across income categories (p =.33). (Table 2). This finding remains for each of the individual conditions included in the EMB measures, with the exception of conduct or behavioral problems, which are systematically higher for lower income children with multiple ACEs compared to similar higher income children. (data not shown)
Table 2.
Prevalence of EMBa among US children ages 2-17 by ACEs exposure status and household income and age. Data from 2011-2012 National Survey of Children's Health.
| EMB Prevalence: All US Children Age 2-17 (%) | EMB Prevalence: Children Age 2-17 with No ACEs | EMB Prevalence: Children Age 2-17 with 1 ACE | EMB Prevalence: Children Age 2-17 with 2-3 ACEs | EMB Prevalence: Children Age 2-17 with ≥4 ACEs of 9 ACEs | Ratio of EMB Prevalence | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | AORb | % | AORb | % | AORb | % | AORb | No ACES vs ≥1 ACEs | No ACEs vs 1, 2-3 or ≥4 ACEs | ||
| All children 2-17 | 14.0 | 8.3 | Ref | 13.7 | 1.64 | 21.7 | 2.62 | 37.0 | 5.02 | 2.39 | 1.65- 4.46 |
| Household income (FPL%) | |||||||||||
| 0-99 | 17.6 | 8.5 | Ref | 12.8 | 1.44 | 24.0 | 2.66 | 40.0 | 5.21 | 2.58 | 1.50-4.70 |
| 100-199 | 14.9 | 6.6 | Ref | 13.1 | 1.89 | 23.1 | 3.34 | 35.7 | 5.59 | 3.04 | 1.98-5.40 |
| 200-399 | 13.1 | 8.3 | Ref | 14.2 | 1.69 | 18.9 | 2.27 | 34.8 | 4.86 | 2.23 | 1.71-4.19 |
| ≥400 | 11.5 | 9.0 | Ref | 15.1 | 1.57 | 19.2 | 2.02 | 33.9 | 3.67 | 1.97 | 1.68-3.77 |
| p value (chi-square test) | <.001 | .05 | Ref | .41 | - | .03 | - | .33 | - | - | - |
| Child age (years) | |||||||||||
| 2-5 | 6.4 | 3.7 | Ref | 7.3 | 1.85 | 12.6 | 3.13 | 23.5 | 6.59 | 2.78 | 1.97-6.35 |
| 6-11 | 14.9 | 9.5 | Ref | 13.7 | 1.44 | 23.6 | 2.69 | 38.0 | 5.08 | 2.16 | 1.44-4.00 |
| 12-17 | 18.1 | 11.0 | Ref | 17.6 | 1.75 | 23.6 | 2.44 | 39.4 | 4.71 | 2.14 | 1.60-3.58 |
| p value (chi-square test) | <.001 | <.001 | Ref | <.001 | - | <.001 | - | .001 | - | - | - |
Abbreviations: ACEs: adverse childhood experiences; AOR: adjusted odds ratio; EMB: emotional, mental, or behavioral health conditions; FPL: federal poverty level.
Defined as children who qualify on the Children with Special Health Care Needs Screener criteria for having emotional, developmental, or behavioral conditions that have lasted or are expected to last for ≥12 months and require treatment or counseling and/or who have had a doctor indicate current presence of ≥1 of 7 emotional, mental, or behavioral conditions asked in the National Survey of Children's Health.
Adjusted for age, sex, race/ethnicity, insurance status/type.
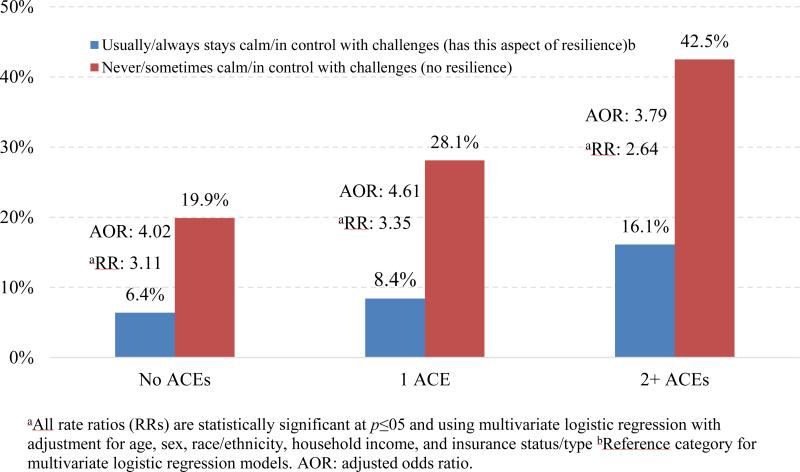
Prevalence of Emotional, Mental, or Behavioral Conditions by Adverse Childhood Experiences and Resilience Status
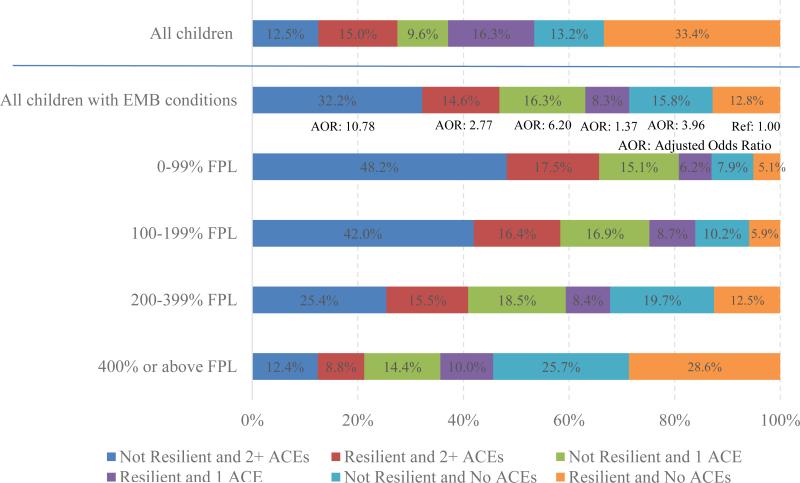
In this study, a single construct of resilience is measured as parental observation of whether their child is usually or always able to stay calm and in control when faced with a challenge. The presence of resilience measured in this minimal way is significantly associated with a lower prevalence of EMB, even for children with no ACEs. On average, the prevalence of EMB is 3.3 times greater when children lack this single aspect of resilience. (Table 3) Across ACEs status categories (0, 1, 2+), the prevalence of EMB is 2.64 to 3.35 times greater when children lack this aspect of resilience. (Figure 1) Only one third of US children (33.4%) and 12.8% with EMB are resilient and ACEs free. Although substantial variations exist across income categories, only 28.6% of children with EMB in the highest income category are both resilient and free from ACEs. (Figure 2) Compared to the 12.8% of children with EMB who both demonstrate resilience and lack ACEs, those without resilience and multiple ACEs are 6.6 times more likely to have an EMB (6.4% vs. 42.5%; data not shown). On the contrary, when children with two or more ACEs nonetheless demonstrate resilience, they are 2.64 times less likely to have EMB than their peers with two or more ACEs who lack resilience. (Table 3)
Table 3.
Prevalence of EMBa among children (2–17 or 6–17 depending on variable) by child resilience and protective factors status: by EMB and among EMB with 2 or more adverse childhood experiences (ACEs: 70.7% EMB have ≥1 ACEs). Data from 2011-2012 National Survey of Children's Health.
| Protective Factors | EMB Prevalence and Rate Ratios (Children with Negative vs Positive Result on Protective Factor) | Distribution of Children with Protective Factors: by EMB and ACEs Status (Age 2-17 or 6-17 Depending Upon Protective Factor Variable) | ||||||
|---|---|---|---|---|---|---|---|---|
| EMB Prevalence: All Children (%)b | EMB RRc | EMB Prevalence: Children with ≥2 ACEs (%)b | EMB RRc | Distribution of Protective Factor: Children with EMB (%) | Distribution of Protective Factor: Children without EMB (%) | Distribution of Protective Factor: Children with EMB and ≥2 ACEs (%) | Distribution of Protective Factor: All Children (%) | |
| Child demonstrates resilience (usually or always stays calm and in control when faced with a challenge) (age 6-17) | ||||||||
| Yes | 9.1 | 3.30 | 16.1 | 2.64 | 35.8 | 70.4 | 31.3 | 64.7 |
| No | 30.0 | 42.5 | 64.2 | 29.6 | 68.7 | 35.3 | ||
| Parent and child share ideas and talk about things that matter (very well) (age 6-17) | ||||||||
| Yes | 13.0 | 1.92 | 23.4 | 1.56 | 55.3 | 73.3 | 52.7 | 70.4 |
| No | 24.9 | 36.6 | 44.7 | 26.7 | 47.3 | 29.6 | ||
| Parent has met most/all child's friends and attends most/all of child's events (age 6-17) | ||||||||
| Yes | 13.7 | 1.45 | 23.1 | 1.55 | 48.4 | 59.7 | 41.3 | 57.9 |
| No | 19.8 | 35.9 | 51.6 | 40.3 | 58.7 | 42.1 | ||
| Parent is usually or always stressed with parenting or aggravated with child (age 2-17) | ||||||||
| Yes | 38.7 | 3.62 | 53.3 | 2.64 | 32.9 | 8.5 | 36.4 | 11.9 |
| No | 10.7 | 20.2 | 67.1 | 91.5 | 63.6 | 88.1 | ||
| Parent reports coping very well w/parenting (age 2-17) | ||||||||
| Yes | 10.2 | 1.92 | 20.6 | 1.52 | 42.6 | 61.6 | 37.7 | 59.0 |
| No | 19.6 | 31.3 | 57.4 | 38.4 | 62.3 | 41.0 | ||
| Mothers mental health excellent/very good (age 2-17) | ||||||||
| Yes | 10.9 | 1.82 | 21.3 | 1.42 | 57.3 | 72.9 | 43.7 | 70.8 |
| No | 19.8 | 30.2 | 42.7 | 27.1 | 56.3 | 29.2 | ||
| Child is usually/always engaged in school (age 6-17) | ||||||||
| Yes | 11.3 | 3.35 | 19.5 | 2.39 | 55.0 | 85.4 | 46.8 | 80.4 |
| No | 37.9 | 46.5 | 45.0 | 14.6 | 53.2 | 19.6 | ||
| Child missed 2 or more weeks of school/year (age 6-17) | ||||||||
| Yes | 38.6 | 2.59 | 48.5 | 1.91 | 14.5 | 4.5 | 18.8 | 6.2 |
| No | 14.9 | 25.4 | 85.5 | 95.5 | 81.2 | 93.8 | ||
Abbreviations: ACEs: adverse childhood experiences; EMB: emotional, mental, or behavioral health conditions; FPL: federal poverty level; RR: rate ratio.
Defined as children who qualify on the Children with Special Health Care Needs Screener criteria for having emotional, developmental, or behavioral conditions that have lasted or are expected to last for ≥12 months and require treatment or counseling and/or who have had a doctor indicate current presence of ≥1 of 7 emotional, mental, or behavioral conditions asked in the National Survey of Children's Health.
All EMB prevalence rate differences for each factor are statistically significant at p≤05.
RR between those with or without the positive valence of the protective factor.
Figure 1.
Prevalence of emotional, mental, or behavioral conditions (EMB) by adverse childhood experiences (ACEs) exposure and resilience status (all US children ages 6–17). Data from 2011-2012 National Survey of Children's Health
Figure 2.
Distribution of all school age children (6–17) and children with emotional, mental, or behavioral conditions (EMBs): by resilience, adverse childhood experiences (ACEs) status and income (federal poverty level [FPL]). Data from 2011-2012 National Survey of Children's Health
Prevalence of Emotional, Mental, or Behavioral Conditions by School Success Factors, Adverse Childhood Experiences, and Resilience
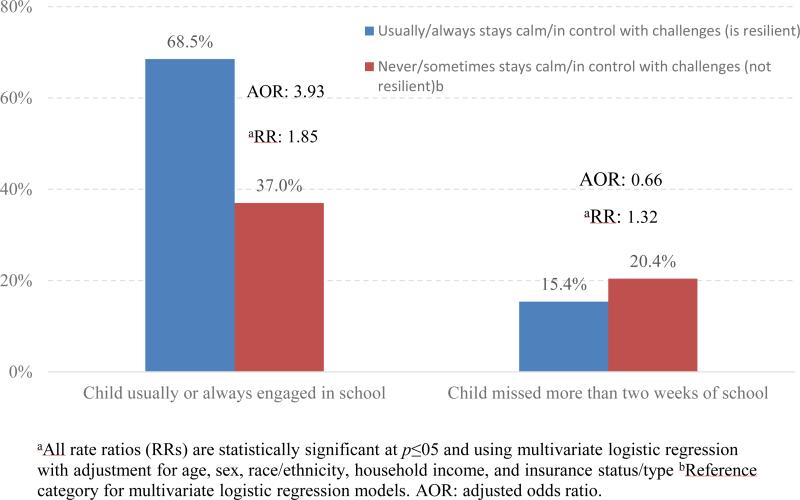
Children with two or more ACEs are 2.39 and 1.91 times more likely to not be engaged in school or missed more than 2 weeks of school, respectively. (Table 3) Children with EMB and multiple ACEs have 1.85 times higher rates of school engagement and are 1.32 times less likely to miss 2 or more weeks of school if they demonstrate the aspect of resilience assessed here. (Figure 3)
Figure 3.
Prevalence of school success factors among US children age 6 to 17 with emotional, mental or behavioral conditions (EMB) and 2 or more adverse childhood experiences exposures (ACEs) by resilience status. Data from 2011-2012 National Survey of Children's Health
Prevalence of Emotional, Mental, or Behavioral Conditions by Family Protective Factors and Associations with Adverse Childhood Experiences and Resilience
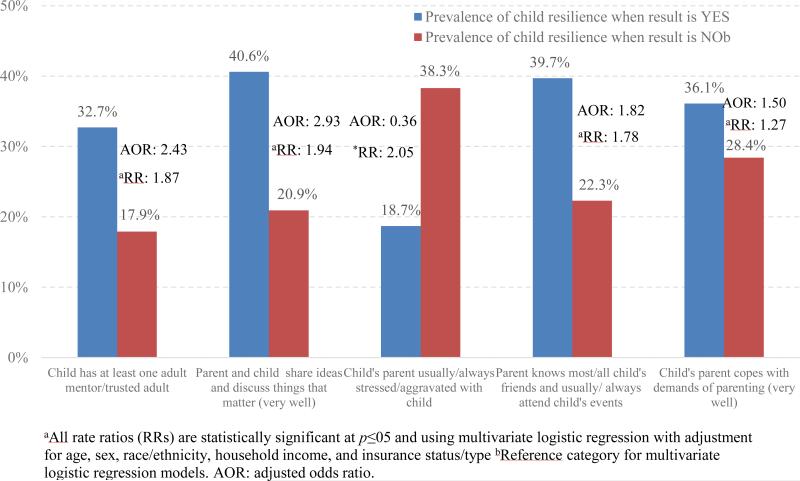
Prevalence of EMB is 1.45 to 3.62 times higher when the following five family-focused protective factors assessed are missing (Table 3): (1) parent-child share ideas and discuss things that matter (rate ratio: 1.92); (2) parent has met most or all of child's friends and usually or always participates in child's events (rate ratio: 1.45); (3) parent manages stress and aggravation with parenting (rate ratio: 3.62); (4) parent copes well with parenting (rate ratio: 1.92); and/or (5) mother's mental health is excellent or very good (rate ratio: 1.82). These variations are somewhat attenuated when children have also been exposed to two or more ACEs (1.42-2.64 across the five factors), such that those with multiple ACEs are more likely to have EMB, regardless of these factors. Among family protective factors assessed, parental stress and aggravation has the biggest effect on prevalence of EMB for all children, as well as for those with multiple ACEs. For children with multiple ACEs, the effect of having parents who have met all or most of the child's friends and usually or always attend their events is somewhat stronger.
Across all five family-focused protective factors, children with EMB are 1.23 to 1.44 times less likely to live in homes where the five family-focused protective factors exist compared to children without EMB. Similarly, children with EMB and multiple ACEs are also 1.44 to 2.08 less likely to live in such homes. (Table 3) Conversely, when children with EMB and multiple ACEs live in homes with at least one family-focused protective factor, they are 1.27 to 2.05 times more likely to demonstrate resilience. These effects are greatest for children in homes where the parent and child share ideas and discuss things that really matter. (Figure 4)
Figure 4.
Prevalence of resilience among US children age 2 to 17 with emotional, mental or behavioral conditions (EMB) and 2 or more adverse childhood experiences (ACEs) exposures by key protective factors. Data from 2011-2012 National Survey of Children's Health
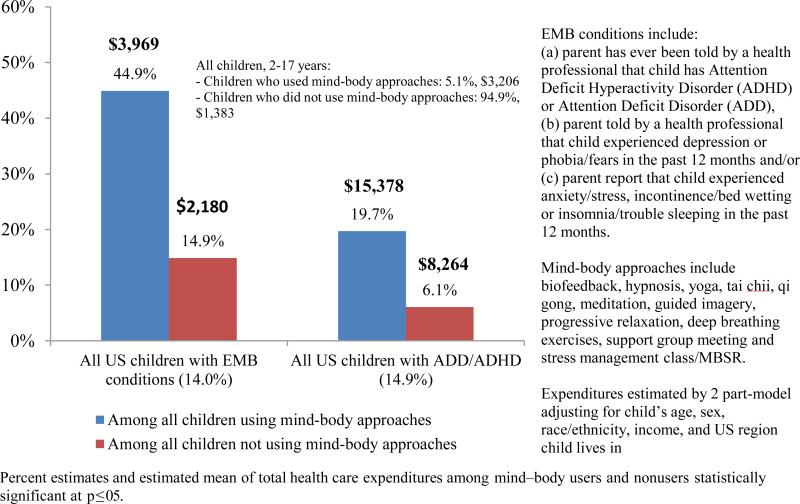
Use of Risk Regulating Mindfulness-Based, Mind–Body Approaches, and Medical Expenditures
About 5% of US children age 2-17 have parents who reported their child has used the MBMB assessed in the NHIS-CAM Supplement. This increases to 14% for children with EMB and to 14.9% for children with ADD/ADHD. (Figure 5) Those with any type of EMB who use MBMB used more conventional medical care for their conditions and have 1.82 times higher adjusted total conventional medical expenditures compared to those who did not use MBMB. This effect is similar for children with ADD/ADHD (1.86 times greater adjusted expenditures) and for all children generally (2.32 times greater adjusted expenditures). These differences are statistically significant. (Figure 5)
Figure 5.
Use of mind—body approaches and mean of total conventional medical care expenditures for US children age 2 to 17: all children, those with emotional, mental or behavioral conditions (EMB) and those with attention deficit disorder (ADD)/attention deficit hyperactivity disorder (ADHD). Data from 2007 NHIS and NHIS-Child CAM Supplement and 2008 MEPS
Discussion
Findings presented herein are the first showing hypothesized associations among EMB, ACEs, resilience, and family protective factors in a population-based sample of US children and youth. In this way, results are critical to confirm more narrowly focused studies27, 28, 29 and are useful to guide rapidly evolving efforts underway nationally to prevent and decrease the impact of EMB and ACEs and promote positive health. This includes the many efforts taking place to integrate primary care and mental and behavioral health services and in educational and other community based settings.14, 16
The co-occurring nature of EMB, ACEs, and school success factors, and the mediating effects of resilience, parental stress, parent-child engagement, and other family-focused protective factors are likely not surprising to many clinicians and child health leaders. The population-based findings presented here may simply confirm current understanding. Findings also raise questions about the directionality of observed effects. Specifically, because ACEs are largely a function of failures in the safety, stability, and nurturing properties of the child's relationships and environment, by their nature, ACEs challenge a child's capacity to manage stress and build resilience. In this way, lower rates of resilience and protective factors among children with ACEs are not surprising.
What is more revealing here is the relative effect of building a child's resilience and family protective factors to both attenuate the impact of ACEs that have already occurred and associations between these factors and prevalence of EMB, regardless of ACEs status. The cross-cutting attenuating effects of child resilience, parental stress management, and engagement found here suggest the importance of population-based promotion of these protective factors overall and especially for children already exposed to ACEs. MBMB methods hold promise for doing so, yet are used infrequently. When children with EMB do use MBMB, findings suggest do so after extensive use of conventional medical care approaches. This is indicated by the higher use and costs of medical care expenditures for these children. This suggests that parents turn to MBMB only after their child's condition becomes more severe and they have sought help across a range of health care providers and pharmaceutical treatments.
Although more research is required, findings hold promise for potentially decreasing health care costs for children and their families, especially those with EMB and exposure to ACEs. Given growing evidence on the effectiveness of MBMB to attenuate symptoms associated with many types of EMB (ADHD, depression, anxiety, conduct disorders), findings from this study suggest a delayed and underuse of MBMB approaches for children.
Findings from this study emphasize the importance of resilience and the quality of the very family relationships implicated in a child's ACEs status. In this way, findings support attention to the ACEs status of parents and their own capacities to manage stress and heal from the trauma and chronic stress that can accumulate when exposed to ACEs. Findings may also lead to rethinking the sufficiency and appropriateness of predominant EMB treatment norms, such as the widespread use of pharmaceutical-based treatment plans (e.g. 68% of children with ADHD currently take medications)27 and consider use of mindfulness and other mind-body based methods in conjunction with more comprehensive clinical approaches that address trauma.
Common, so-called, “trauma-informed” efforts specifically target the prevention and reduction of impacts from ACEs and the chronic stress and trauma that can result and impact health early and across the lifespan. Such approaches are defined, recommended, and supported by the federal Substance Abuse and Mental Health Administration (SAHMSA)30, the federal Centers for Medicare and Medicaid Services (CMS)31, the Administration for Children and Families11 (ACF) and, more recently, by the American Academy of Pediatrics. In particular, although not as yet addressed by many pediatric providers,32 ACEs are a growing consideration among pediatric clinicians who increasingly share goals to advance resilience and social and emotional well-being of children and youth. We suggest three reasons for this: (1) similarities in symptoms of many EMB diagnoses and those associated with exposure to ACEs; (2) the many undiagnosed children with untreated symptoms related to ACEs exposure; and, (3) new possibilities for prevention, healing, and treatment introduced by growing neuroscience, epigenetic, resilience, positive health, and mindfulness and mind-body related research.
A primary limitation of this study is the cross-sectional nature of the NSCH. Unfortunately, the United States does not have a longitudinal population-based study that includes information on EMB, ACEs and other variables evaluated here. Such data, including integration with medical and other services and costs of care and biologic and other environmental measurements are needed to document causal effects and better understand variations in outcomes between and within risk subgroups. In the absence of a national longitudinal study that includes such data, follow-back surveys among cohorts of children included in the 2011–12 NSCH hold promise as does the integration of ACEs and protective factors data in existing longitudinal cohort studies. Additional limitations exist to the extent that NSCH items/measures used here lack sensitivity, specificity or comprehensiveness for the concepts assessed. Generally, surveys such as the NSCH are biased in the direction of positive reporting, suggesting that with improvement the effects observed here likely show even more marked effects of ACEs and lack of resilience and family protective factors.
Conclusions
Based on a recent United Nations report, the US ranks 26th out of 29 countries in child well-being.33 We also lag in educational and health care system promotion of resilience and social and emotional skills especially impacted by ACEs and highlighted as critical to health of society and the world in the International Organization for Economic Co-Operation and Development.34 Many would attribute these embarrassing results to failures to strengthen families and communities and the proactive promotion of social and emotional skills of children and all people; skills especially impacted by ACEs and effecting generations of children if not addressed.35
As the call for the transformation of the US health care system grows, clinicians, policymakers, educators, and system leaders are challenged to catalyze and foster a model of health care focused on the proactive pursuit of whole person, whole family, and whole population health and well-being. This paper further confirms the importance of addressing the growing prevalence of EMB, ACEs, and risk regulating protective factors that are potentially malleable using MBMB, such as child resilience, parental coping and stress, and parent-child engagement. Rates of use of MBMB among children with EMB in the United States suggest delayed and underuse of these promising methods.36-38 Findings support integrated, family-centered, and mindfulness-based trauma-informed approaches to address social and emotional trauma and interrupt intergenerational cycles of ACEs and their contribution to EMB among children and youth.
Diagnosing resilience begins with an assessment of exposure to adversity and the impact risk factors have on children's experience of wellbeing. (Michael Unger, Professor, Dalhousie University, Author: We Generation)
“Without mindfulness, there is no therapy...All growth occurs because you are in a state of mindfulness. Without mindfulness, there is no growth.” Bessel van der Kolk, Professor of Psychiatry, Boston University. Author: The Body Keeps the Score and Treating Traumatic Stress in Children and Adolescents
Key Points.
Compared with children with no adverse childhood experiences (ACEs), prevalence of emotional, mental, or behavioral conditions (EMB) is 1.65 to 4.46 times higher across ACEs levels.
Those without resilience and multiple ACEs have nearly 11 times greater adjusted odds of having an EMB compared with children with EMB with resilience and no ACEs.
With resilience, children with EMB and multiple ACEs have 1.85 times higher rates of school engagement and are 1.32 times less likely to miss 2 or more school weeks.
Resilience is nearly 2 times greater among children with EMB and multiple ACEs when their parents report less parenting stress and more engagement in their child’s lives.
Attenuating effects of child resilience, parental stress management, and engagement suggest promotion of these protective factors. Mindfulness-based, mind–body methods hold promise for doing so.
Acknowledgments
Funding Source: This study was supported by the Child and Adolescent Health Measurement Initiative (CAHMI) and by a grant from the National Center for Complementary and Alternative Medicine 1 R21 AT004960 01A2. Funded by the National Institutes of Health (NIH).
Abbreviations
- EMB
Emotional, mental, or behavioral conditions
- ACEs
Adverse childhood experiences
- ADHD
Attention deficit hyperactivity disorder
- NSCH
National Survey of Children's Health
- MEPS
Medical Expenditure Panel Survey
- NHIS
National Health Interview Survey
- MBMB
Mindfulness-Based and Mind-Body Methods
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Bethell CD, Newacheck P, Hawes E, et al. Adverse childhood experiences: assessing the impact on health and school. Engagement and the mitigating role of resilience. Health Aff. 2014;33(12):2106–15. doi: 10.1377/hlthaff.2014.0914. [DOI] [PubMed] [Google Scholar]
- 2.Injury Prevention & Control: Division of Violence Prevention . Adverse childhood experiences. Centers for Disease Control and Prevention; [October 10, 2015]. Available at: http://www.cdc.gov/violenceprevention/acestudy/. [Google Scholar]
- 3.Rahim M. Developmental trauma disorder: An attachment-based perspective. Clin Child Psychol Psychiatry. 2014 Oct;19(4):548–560. doi: 10.1177/1359104514534947. [DOI] [PubMed] [Google Scholar]
- 4.Schmid M, Petermann F, Fegert JM. Developmental trauma disorder: pros and cons of including formal criteria in the psychiatric diagnostic systems. BMC Psychiatry. 2013 Jan;13(3) doi: 10.1186/1471-244X-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garner AS, Forkey H, Szilagyi M. Translating developmental science to address childhood adversity. Acad Pediatr. 2015;15(5):493–502. doi: 10.1016/j.acap.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 6.McEwen BS, Gianaros PJ. Ann N Y Acad Sci. 1. Vol. 1186. Blackwell Publishing Inc.; 2010. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. pp. 190–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine and National Research Council . Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- 8.Shonkoff JP, Boyce W, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–9. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 9.Van der Kolk B. The body keeps the score: brain, mind, and body in the healing of trauma. Penguin Books; New York: 2014. [Google Scholar]
- 10.Zannas AS, West AE. Epigenetics and the regulation of stress vulnerability and resilience. Neuroscience. 2014;0:157–170. doi: 10.1016/j.neuroscience.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamoudi A, Murray DW, Sorensen L, et al. OPRE Report # 2015-30. Office of Planning, Research and Evaluation, Administration for Children and Families, US Department of Health and Human Services; Washington, DC: 2015. Self-regulation and toxic stress: a review of ecological, biological, and developmental studies of self-regulation and stress. [Google Scholar]
- 12.Ungar M, Ghazinour M, Richter J. Annual research review: what is resilience within the social ecology of human development? J Child Psychol Psychiatry. 2013;54:348–66. doi: 10.1111/jcpp.12025. [DOI] [PubMed] [Google Scholar]
- 13.Sege R, Linkenbach J. Essentials for childhood: promoting healthy outcomes from positive experiences. Pediatrics. 2014;133(6):e1489–91. doi: 10.1542/peds.2013-3425. [DOI] [PubMed] [Google Scholar]
- 14.Flynn AB, Fothergill KE, Wilcox HC, et al. Primary care interventions to prevent or treat traumatic stress in childhood: a systematic review. Acad Pediatr. 2015;15(5):480–92. doi: 10.1016/j.acap.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fraser JG, Lloyd SW, Murphy RA, et al. Child exposure to trauma: comparative effectiveness of interventions addressing maltreatment. Comparative Effectiveness Review No. 89. Agency for Healthcare Research and Quality; Rockville (MD): 2013. (Prepared by the RTIUNC Evidence-based Practice Center under Contract No. 290-2007-10056-I.) AHRQ Publication No. 13-EHC002-EF.
- 16.Wissow LS, Brown J, Fothergill KE, et al. Universal mental health screening in pediatric primary care: a systematic review. J Am Acad Child Psychiatry. 2013;52(11):1134–47. e23. doi: 10.1016/j.jaac.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitaker RC, Dearth-Wesley T, Gooze RA, et al. Adverse childhood experiences, dispositional mindfulness, and adult health. Prev Med. 2014;67:147–53. doi: 10.1016/j.ypmed.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 18.Black DS. In: Mindfulness training for children and adolescents: a state-of-the-science review. Handbook of mindfulness: theory, research, and practice. Brown KW, Creswell JD, Ryan RM, editors. Guilford Press; New York: 2015. pp. 283–310. [Google Scholar]
- 19.Felver JC, Celis-de Hoyos CE, Tezanos K, Singh NN. A Systematic Review of Mindfulness-Based Interventions for Youth in School Settings. Mindfulness. 2015 [Google Scholar]
- 20.Kallapiran K, Koo S, Kirubakaran R, et al. Effectiveness of mindfulness in improving mental health symptoms of children and adolescents: a meta-analysis. Child and Adol Mental Health. 2015 Aug 6;20(4):182–194. doi: 10.1111/camh.12113. [DOI] [PubMed] [Google Scholar]
- 21.Takimoto-Ohnishi E, Ohnishi J, Murakami K. Mind–body medicine: effect of the mind on gene expression. Personalized Medicine Universe. 2012;1(1):2–6. [Google Scholar]
- 22.Harnett PS, Dawe S. Review: The contribution of mindfulness-based therapies for children and families and proposed conceptual integration. Child and Adolescent Mental Health. 2012;17(4):195–208. doi: 10.1111/j.1475-3588.2011.00643.x. [DOI] [PubMed] [Google Scholar]
- 23.Hempel S, Taylor SL, Marshall NJ, et al. Evidence map of mindfulness. Department of Veterans Affairs (US); Washington, DC: 2014. Project #05–226. [PubMed] [Google Scholar]
- 24.Coeytaux RR, McDuffie J, Goode A, et al. Evidence map of yoga for high-impact conditions affecting veterans. Department of Veterans Affairs (US); Washington, DC: 2014. Project #09–010. [PubMed] [Google Scholar]
- 25.Hempel S, Taylor SL, Solloway M, et al. Evidence map of Tai Chi. Department of Veterans Affairs (US); Washington, DC: 2014. Project #05–226. [PubMed] [Google Scholar]
- 26.Child and Adolescent Health Measurement Initiative. Data Resource Center for Child and Adolescent Health; [September 17, 2015]. Learn about the surveys. Available at: www.child-healthdata.org. [Google Scholar]
- 27.Howie LD, Pastor PN, Lukacs SL. NCHS data brief, no 148. National Center for Health Statistics; Hyattsville (MD): 2014. Use of medication prescribed for emotional or behavioral difficulties among children aged 6–17 years in the United States, 2011–2012. [PubMed] [Google Scholar]
- 28.Kerker BD, Zhang J, Nadeem E, et al. Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Acad Pediatr. 2015;15(5):510–7. doi: 10.1016/j.acap.2015.05.005. http://dx.doi.org/10.1016/j.acap.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fuller-Thomson E, Lewis DA. The relationship between early adversities and attention-deficit/hyperactivity disorder. Child Abuse Negl. 2015 Apr;47:94–101. doi: 10.1016/j.chiabu.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Substance Abuse and Mental Health Services Administration . Adverse childhood experiences. [Internet] SAMHSA; Rockville (MD): [October 31, 2014]. Available at: http://captus.samhsa.gov/prevention-practice/targeted-prevention/adverse-childhood-expe-riences/1. [Google Scholar]
- 31.Sheldon GH, Tavenner M, Hyde PS. Letter to state directors [Internet] Department of Health and Services; Washing-ton, DC: 2013. [October 31, 2014]. Available at: http://medicaid.gov/Federal-Policy-Guidance/Downloads/SMD-13-07-11.pdf. [Google Scholar]
- 32.Kerker BD, Storfer-Isser A, Szilagyi M, et al. Do pediatricians ask about adverse childhood experiences in pediatric primary care? Acad Pediatr. 2015 doi: 10.1016/j.acap.2015.08.002. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 33.UNICEF Office of Research . Child well-being in rich countries: a comparative overview, innocenti report card 11. UNICEF Office of Research; Florence (Italy): 2013. [October 10, 2015]. Available at: www.unicef-irc.org/publications/pdf/rc11_eng.pdf. [Google Scholar]
- 34.Office of Economic Cooperation and Development (OECD) Skills for social progress: the power of social and emotional skills, OECD skills studies. OECD Publishing; Paris (France): 2015. [Google Scholar]
- 35.Schor EL, Menaghan EG. Family pathways to child health. In: Amick BC III, Levine S, Tarlov AR, et al., editors. Society and health. Oxford University Press; New York: 1995. pp. 18–45. [Google Scholar]
- 36.McClafferty H. Integrative pediatrics: looking forward. Children. 2015;2(1):63–5. doi: 10.3390/children2010063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bethell CD, Hassink S, Abatemarco D, et al. Leveraging mind-body neuroscience and mindfulness to improve pediatrics. [October 10];Child and adolescent health measurement initiative mindfulness in pediatrics white paper initiative. 2012 Available at http://beta.cahmi.org/wp-content/uploads/2013/12/Mindfulness-In-Pediatrics-and-MCH-Overview-Poster-Content-4_29_13-CB-1.pdf.
- 38.Gloria CT, Steinhardt MA. Relationships among positive emotions, coping, resilience and mental health. Stress Health. 2014 doi: 10.1002/smi.2589. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]