Abstract
Background
Childhood obesity is a major public health problem in the United States, particularly among American Indian communities.
Objective
The objective was to evaluate the effectiveness of a school-based, multicomponent intervention for reducing percentage body fat in American Indian schoolchildren.
Design
This study was a randomized, controlled, school-based trial involving 1704 children in 41 schools and was conducted over 3 consecutive years, from 3rd to 5th grades, in schools serving American Indian communities in Arizona, New Mexico, and South Dakota. The intervention had 4 components: 1) change in dietary intake, 2) increase in physical activity, 3) a classroom curriculum focused on healthy eating and lifestyle, and 4) a family-involvement program. The main outcome was percentage body fat; other outcomes included dietary intake, physical activity, and knowledge, attitudes, and behaviors.
Results
The intervention resulted in no significant reduction in percentage body fat. However, a significant reduction in the percentage of energy from fat was observed in the intervention schools. Total energy intake (by 24-h dietary recall) was significantly reduced in the intervention schools but energy intake (by direct observation) was not. Motion sensor data showed similar activity levels in both the intervention and control schools. Several components of knowledge, attitudes, and behaviors were also positively and significantly changed by the intervention.
Conclusions
These results document the feasibility of implementing a multicomponent program for obesity prevention in elementary schools serving American Indian communities. The program produced significant positive changes in fat intake and in food- and health-related knowledge and behaviors. More intense or longer interventions may be needed to significantly reduce adiposity in this population.
Keywords: Obesity, American Indians, schoolchildren, prevention programs, randomized trials
INTRODUCTION
Childhood obesity is well recognized as an increasing public health problem in the United States (1, 2). The number of 6–11-y-old children with a body mass index (BMI) above the 85th percentile (of the 1963 National Health Examination Survey) increased from 15% in 1963 to 22% in 1994. Although nationwide data on obesity rates in American Indian communities are still limited, the available surveys indicate that 34% of men and 40% of women have a BMI > 30, which is markedly higher than the all-race national averages of 24% and 25% (3, 4). A 1990 national survey of 9464 American Indian children aged 5–18 y reported that 39% had a BMI above the 85th percentile of the second National Health and Nutrition Examination Survey (5). Other tribe-specific or regional surveys reported prevalences ranging from 25% to 46% in that age group (6–8). The Pathways Study was designed to evaluate the effectiveness of a school-based, multicomponent intervention to prevent or reduce excess weight gain in elementary schoolchildren. This article reports the final results of the 3-y intervention.
SUBJECTS AND METHODS
Study design
The Pathways Study was organized in 2 phases. During the first 3-y phase, all components of the intervention were developed and tested, and measurement instruments were validated. The approach for measuring the main outcome variable, percentage body fat (%BF), was also defined and validated. The results of this feasibility phase were previously reported in detail (9, 10). In the second phase, an intervention was implemented for 3 consecutive years.
Study population
School selection was based on the following eligibility criteria: 1) a projected 3rd grade enrollment of ≥ 15 children, 2) ≥ 90% of 3rd grade children of American Indian ethnicity, 3) retention from 3rd to 5th grade over the past 3 y of ≥ 70%, 4) school meals prepared and administered on site, 5) availability of minimum facilities to deliver a physical activity program at the school, and 6) approval of the study by school, community, and tribal authorities. In addition, schools that were considering closing or merging in the next 3 y were excluded.
A total of 41 schools in 7 American Indian communities were enrolled. All schools worked in partnership with a participating academic institution: White Mountain Apache and San Carlos Apache (Johns Hopkins University, Baltimore), Navajo (University of New Mexico, Albuquerque), Sicangu Lakota and Oglala Lakota (University of Minnesota, Minneapolis), and the Tohono O’odham Nation and Gila River Indian Community (University of Arizona, Tucson). The University of North Carolina at Chapel Hill served as the coordinating center.
Children were enrolled in the study, and baseline measurements were made at the end of the 2nd grade. To ensure that the average %BF was similar in both groups, schools were assigned to intervention and control groups by a process of stratified randomization. After the baseline measurements were made, upper and lower %BF strata were defined for schools at each site, and random allocation was determined for each stratum.
The study protocols were approved by tribal, school, and university authorities. Written informed consent was obtained from the parents, and verbal consent was obtained from the children for all measurement procedures and for intervention activities as required by school boards and tribal health authorities.
Intervention components
The Pathways Study intervention consisted of 4 components (Table 1): classroom curriculum, food service, physical activity, and family involvement. Each component was developed and pilot-tested during the feasibility phase of the study and was based on formative research performed at each site (11). The intervention approach combined constructs from social learning theory and principles of American Indian culture and practices. Several indigenous learning modes (eg, story telling) were also incorporated into the intervention (12).
TABLE 1.
Components of the Pathways intervention
| Component | Objective | Content |
|---|---|---|
| Classroom curriculum | Targeted at 3rd, 4th, and 5th grades | 12 wk/y (8 wk in the 5th grade), twice weekly for 45-min as a classroom lesson |
| Promote healthful eating behaviors and increased physical activity | Lessons linked by adventures of imaginary American Indian characters on their journey to healthy living | |
| Integrate social learning constructs with American Indian traditions | ||
| Food service | Reduce percentage of energy from fat to ≤ 30% | Pathways guidelines for food-service personnel |
| Introduce dietary practices aimed at increasing the use of lower-fat foods and fruit and vegetables | Regular visit by Pathways nutritionist to support and monitor school-lunch preparation | |
| Physical education | Increase energy expenditure | Three 30-min physical-education sessions per week during school time |
| Encourage moderate-to-high amounts of physical activity in all children | Exercise break during classroom time | |
| Promote practice of health-related physical activity during and after school | Guided play during recess | |
| Family | Keep families informed and involved in the program | Family fun nights, workshops, and events at school |
| Extend positive health behaviors learned at school to family members by promoting involvement of family and child in school-based program activities | Family packs linked to classroom curriculum | |
| Create a supportive environment for children to adopt positive health practices |
Classroom curriculum
The classroom curricula for 3rd, 4th, and 5th grades were designed to promote healthful eating behaviors and to increase physical activity. Two 45-min lessons were delivered by teachers each week for 12 wk during the 3rd and 4th grades. This component was decreased to 8 wk during 5th grade to allow for the follow-up measurements during the final 2 mo of the school year.
Food service
The food service intervention provided nutrient guidelines and practical tools for reducing the fat content of school meals while complying with nutrient requirements as defined by the US Department of Agriculture School Lunch and Breakfast programs. The Pathways Behavioral Guidelines for food service staff provided skill-building techniques for use in planning, purchasing, and preparing lower-fat school meals.
Physical education
The physical education (PE) program aimed at increasing energy expenditure in the school environment by implementing a minimum of three 30-minute sessions per week of moderate-to-vigorous physical activity. The PE program was based on the SPARK (Sports, Play and Active Recreation for Kids) program (13), with the addition of an American Indian Games module. In addition, the program included exercise breaks of 2–10 min duration, which were designed to increase energy expenditure and promote physical activity in the classroom. Typically, these exercise breaks consisted of simple exercises that could be performed in the classroom or outside, during recess.
Family involvement
The goal of the family-involvement component was to introduce families to the Pathways intervention and to assist them in creating a supportive environment for healthy behaviors. The activities also offered families an interactive forum to discuss practical aspects of the Pathways program and to extend their knowledge on healthy lifestyle and eating behaviors. The family component consisted of 1) family action packs, which were take-home materials related to the Pathways intervention, including snack packs with samples of low-fat foods and tips for preparing healthful snacks at home; and 2) family events at schools, which included cooking demonstrations and activities for healthier lifestyle, with the direct involvement of children.
Training
Each intervention component included a specific training plan. Teachers and food service staff were trained annually in local or regional meetings. Concepts and procedures were reinforced at regular visits to school classrooms and kitchens. PE teachers, aides, or regular teachers in charge of PE at each intervention school were trained annually by licensed SPARK instructors or by Pathways instructors who had experience in delivering that program. These Pathways staff also acted as mentors for PE teachers, offering regular support and filling in for PE teachers when needed to ensure a minimum of PE every week.
Measurements
To avoid operator bias, measurement teams were not involved in delivering the intervention. Training, certification, and cross-validation of measurement staff were done centrally or regionally, supervised by the Measurement Committee.
Anthropometry
A full set of anthropometric and body-composition data were collected at baseline (end of 2nd grade) and at follow-up (end of 5th grade). Interim measurements of weight and height were also obtained annually, at the end of the school year, for use by the Data Safety and Monitoring Board for safety monitoring. Measurements were performed in a dedicated room at each school while the children were wearing light clothing and no shoes. All measurements were made early in the morning, on arrival at school. Weight was measured with the use of self-calibrating precision digital scales (Seca 770; Vogel & Halke GmbH, Hamburg, Germany) and height with a fixed Shorr measuring board (Shorr Productions, Olney, MD). Two measurements were obtained and the average was recorded. Triceps and subscapular skinfold thicknesses were measured in triplicate with Lange calipers. Bioelectrical impedance was measured in duplicate with a single-frequency tetrapolar plethysmograph (Valhalla Scientific, Valhalla, NY). Calibration of scales, calipers, and bioimpedance instruments were checked before each use. Maximum acceptable ranges were defined for all measurements.
Percentage body fat
%BF was estimated from bioelectrical impedance and anthropometry with the use of an equation developed and validated specifically for this study (14). This equation has been shown to be highly predictive of %BF in American Indian children (R2 = 0.84). In instances where ≤ 2 of the variables used in the prediction equation were missing, a reduced equation (without the missing variables) was used to predict %BF if the reduced equation produced an R2 of ≥ 0.7 for the prediction of %BF in the same data set used for development of the full prediction equation. For all measurements, deviation from a set range of the 2 measurements would trigger a repeat measurement by the quality control supervisor. In addition, every 10th child was measured a third time by the QC supervisor. Operators deviating from the supervisor’s measurements beyond a set range were excluded from further measurement and sent to retraining.
Physical activity
Physical activity was measured with the use of both a motion sensor and a self-reported activity questionnaire. Minute-by-minute recordings of vector magnitudes, measured with a 3-dimensional accelerometer (TriTrac R3D; Hemokinetics, Iowa City) were collected for 24 h on a random sample of 15 children in each school at the end of the 2nd grade. At the end of the 5th grade, measurements were taken on those same children who were still enrolled; additional children were randomly selected at each school to replace those lost to follow-up.
The physical activity questionnaire was designed to assess activity during the preceding 24 h with the use of a standardized checklist of activities that were selected during the feasibility phase of the study. An activity index was derived from estimates of the energy cost of each activity weighted by its duration (none, a little, a lot).
Knowledge, attitudes, and behavior
A questionnaire about knowledge, attitudes, and behavior was developed and pilot-tested during the feasibility phase of the Pathways Study to measure knowledge, attitudes, and behaviors related to diet and physical activity among American Indian schoolchildren (15). Three scales assessed knowledge of concepts taught in the Pathways curriculum in each grade (3rd, 4th, and 5th). The α coefficients of these scales, measured during the feasibility phase in 5th grade children, were 0.54, 0.50, and 0.51, respectively. Additional scales assessed self-efficacy related to physical activity (α = 0.69), self-efficacy to eating a healthy diet (α = 0.75), and healthy food intentions (α = 0.74).
Questionnaires were distributed to children in their classrooms. Trained Pathways staff read aloud each question and the corresponding answer choices. Children followed along and marked their answers on the questionnaire.
Dietary intake
Food intake during school lunch was measured by direct observation, as previously described (16). Groups of 2–3 children were observed during lunch, in a nonintrusive manner, by 2 trained Pathways staff. Food intake was calculated after all food left on the tray was measured. Twenty-four-hour dietary recall was performed only at the end of the study (5th grade), because a pilot study performed during the feasibility phase showed that 2nd graders could not provide reliable answers about their food intake.
Menu data were collected from 38 schools for breakfast and from 41 schools for lunch, representing menus offered during a 5-d period. All meal-composition data were analyzed with the use of the Nutrition Data System at the University of Minnesota.
Process evaluation
Process evaluation was conducted annually by Pathways investigators and staff not involved in the intervention. Eighteen survey instruments were used to cover all 4 components of the intervention in the 21 intervention schools. Types of data collected included attendance logs for training sessions (teachers, food service personnel, and PE instructors) and for family event (parents or guardians), PE calendars, kitchen-visit contact forms, and student and parent evaluation forms (17). Interim results were used by the Steering Committee to track the implementation of the intervention at each study site, and aggregate results were used to evaluate the overall implementation of the program.
Study organization, data management, and safety
The study was coordinated by a Steering Committee that included the principal investigators, the project officer (from the National Heart, Lung, and Blood Institute), and 2 American Indian representatives elected by all American Indian study personnel. Scientific and ethical issues were monitored throughout the duration of the study by an external Data Safety and Monitoring Board.
Weight and height were measured annually to detect any potential adverse effects of the intervention on growth. Children with BMIs below the 5th percentile of the Centers for Disease Control and Prevention 2000 growth charts or with growth velocity below the 3rd percentile of Tanner’s reference values (18) were identified. Parents were notified when their children met one of these criteria and were referred to the local primary care facility. Children with both low BMI and low growth velocity were followed up by letter, visit, or telephone call, and the principal of the school was notified. To monitor possible adverse effects of the PE intervention, all schools were asked to keep a log of physical activity-related injuries.
Statistical analysis
Mixed linear models were used to test for intervention effects, with %BF at the end of 5th grade as the primary outcome variable. Fixed effects were baseline %BF and treatment group. Field sites and schools within sites were treated as random effects. Preliminary tests were done to identify possible site-by-treatment or sex-by-treatment interaction effects for the main outcome variable, but none were statistically significant. Therefore, mixed models with only main effects terms are presented. Similar mixed models were constructed for the secondary outcome variables. Some outcome variables were not controlled for baseline values, either because no baseline data were available (24-h dietary recall and knowledge of 4th and 5th grade curricula) or because the repeated measurements were not done in the same group of children (school lunch observation and physical activity by motion sensor). The SAS procedure PROC MIXED (SAS Institute, Cary, NC) was used to estimate all the models.
The primary statistical analysis applied the intention-to-treat principle, which calls for all subjects to be analyzed according to their treatment assignment at the time of randomization, regardless of whether they complete the study or not. Therefore, imputed values were used for missing data at follow-up (5th grade). For this, a prediction equation was developed with the use of data from control schools (19) and a procedure based on Rubin’s multiple imputation method (20). A secondary analysis was performed that included only students with both 2nd and 5th grade %BF measurements.
RESULTS
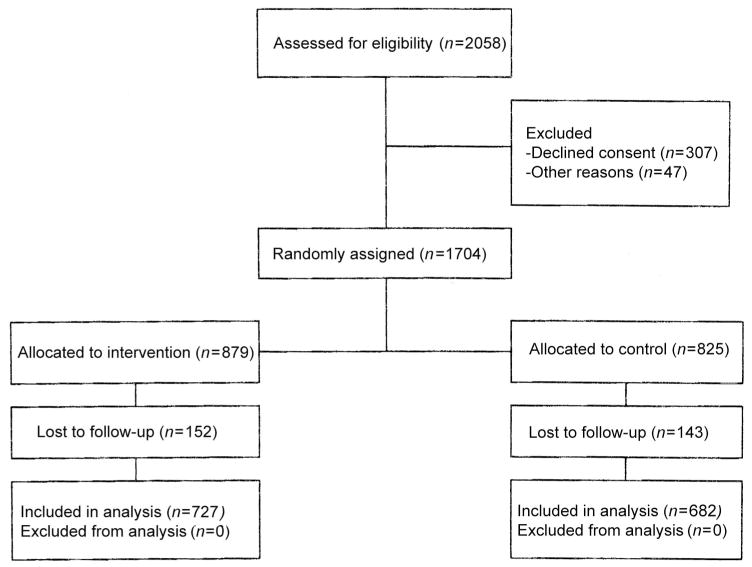
A flow chart for enrollment and follow-up is presented in Figure 1. Of the 2059 2nd-grade students in the 41 participating schools, 1760 received parental permission to be measured and 1704 were measured, which represented the number of children who were actually present at the schools on measurements days. The mean age of children at baseline was 7.6 ± 0.6 y. Detailed results from baseline measurements are reported elsewhere (21). All 41 schools completed the 3-y study. Of the 1704 children screened at baseline, 1409 (83%) were measured at the end of the intervention period.
FIGURE 1.
Flow chart for enrollment and follow-up in the Pathways Study.
Weight, %BF, height, BMI, and triceps and subscapular-skinfold thicknesses are presented in Table 2. There were no significant interactions by sex; therefore, data are shown with values from boys and girls combined. There were no statistically significant differences between the intervention and control groups in any of the anthropometric variables at baseline or follow-up, and estimates of the magnitude of the differences in changes from baseline to follow-up between the control and intervention groups were small. %BF increased by ≈7% in both groups. Imputation of %BF for children who were lost to follow-up did not change these results. With the use of data from children who completed the study, the mean difference in change in %BF between the intervention and control schools was 0.2 (95% CI: −0.84, 1.31). After imputation this difference was 0.0 (95% CI: −0.85, 0.82).
TABLE 2.
Anthropometric measurements of American Indian children in the Pathways Study1
| Baseline
|
Follow-up
|
Mean difference at follow-up2 | 95% CI | P | |||
|---|---|---|---|---|---|---|---|
| Intervention (n = 879) | Control (n = 825) | Intervention (n = 727) | Control (n = 682) | ||||
| Percentage body fat | 32.8 | 33.3 | 40.3 | 40.0 | 0.2 | −0.84, 1.31 | 0.664 |
| Percentage body fat with imputation | — | — | 39.8 | 39.8 | 0.0 | −0.85, 0.82 | 0.974 |
| Height (cm) | 129.9 | 130.4 | 148.1 | 147.6 | 0.5 | 0.03, 0.97 | 0.038 |
| Weight (kg) | 32.5 | 32.9 | 49.0 | 49.0 | −0.0 | −0.86, 0.86 | 0.996 |
| BMI | 19.0 | 19.1 | 22.0 | 22.2 | −0.2 | −0.50, 0.15 | 0.298 |
| Triceps skinfold thickness (mm) | 13.3 | 13.3 | 17.2 | 17.2 | 0.1 | −0.67, 0.83 | 0.837 |
| Subscapular | 10.6 | 10.6 | 15.0 | 15.0 | −0.1 | −0.85, 0.70 | 0.848 |
Results from mixed models. See Subjects and Methods for specific models and details of imputation procedure for percentage body fat. Sample sizes correspond to body fat measurements and may vary slightly from other variables because of missing values.
Calculated from mean values at follow-up (intervention – control).
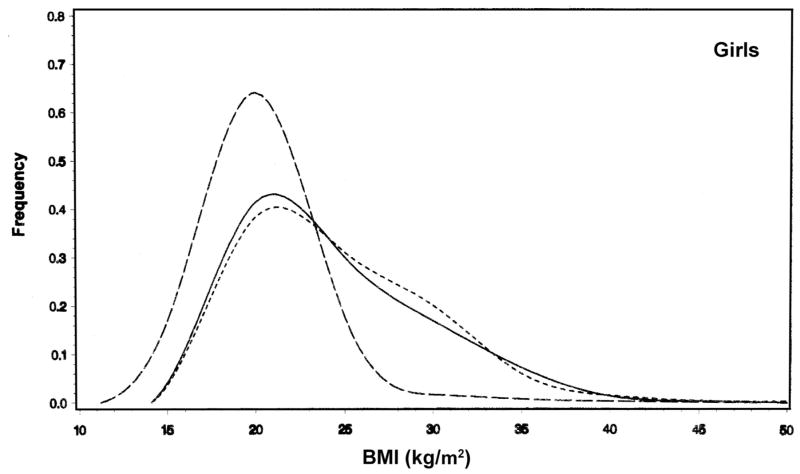
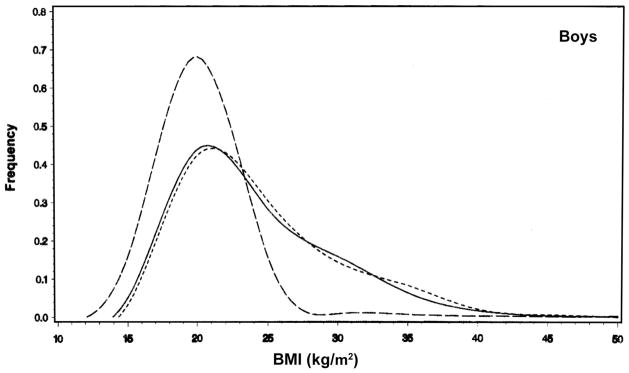
The distributions of BMI in boys and girls in the intervention and control schools are shown in Figures 2 and 3, compared with reference values from the Centers for Disease Control and Prevention’s Growth Charts 2000 (Internet: www.cdc.gov/growthcharts). The distribution of BMI among children in the Pathways Study was clearly shifted toward higher values compared with the reference. At baseline, 47% of the children in the intervention school had BMIs greater than the 85th percentile of the Centers for Disease Control and Prevention’s reference values, whereas 48% of children in the control schools had a BMI that exceeded this cutoff. At the 5th grade follow-up the percentage of children with a BMI greater than the 85th percentile was 53% in the intervention schools and 56% in the control schools.
FIGURE 2.
Frequency distribution of BMI at follow-up for girls in the intervention (——) and control (- - - -) groups from the Pathways Study. The distribution from the Centers for Disease Control and Prevention’s 2000 growth charts reference population is also depicted (– – –).
FIGURE 3.
Frequency distribution of BMI at follow-up for boys in the intervention (——) and control (- - - -) groups from the Pathways Study. The distribution from the Centers for Disease Control and Prevention’s 2000 growth charts reference population is also depicted (– – –).
At baseline there were 3 children with a BMI below the 5th percentile in the intervention schools (0.3%) and 7 in control schools (0.8%). At follow-up, the number was the same in both groups: 6 (0.8%).
Dietary intake
The total energy intake and the percentage of energy from fat as measured by 24-h dietary recall and direct observation of children eating lunch at school are shown in Table 3. The 24-h recall showed a significantly lower total daily energy intake (1892 compared with 2157 kcal/d) and percentage of energy from total fat (31.1% compared with 33.6%) in the intervention group than in the control group. The data from school-lunch observation confirmed a lower fat intake in the intervention group but no difference in energy intake between the 2 groups.
TABLE 3.
Diet, physical activity, and knowledge, attitudes, and behaviors in American Indian children in the Pathways Study1
| Mean at baseline
|
Mean at follow-up
|
Mean difference at follow-up2 | 95% CI | P | |||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||||
| Dietary | |||||||
| 24-h Dietary recall (n = 621) | |||||||
| Energy (kcal) | — | — | 1892 | 2157 | −265 | −437, −94 | 0.003 |
| Fat (% of energy) | — | — | 31.1 | 33.6 | −2.5 | −3.9, −1.1 | 0.001 |
| School-lunch observation (n = 683) | |||||||
| Energy (kcal) | 522.9 | 573.6 | 500.2 | 494.4 | 5.8 | −40.0, 51.5 | 0.804 |
| Fat (% of energy) | 33.1 | 34.1 | 28.2 | 32.4 | −4.2 | −7.1, −1.3 | 0.005 |
| Physical activity | |||||||
| Motion sensor (n = 278) (average vector magnitude/min) | 282.04 | 303.13 | 267.22 | 246.79 | 20.43 | −19.05, 59.92 | 0.310 |
| Questionnaire (n = 1503) | 0.35 | 0.35 | 0.27 | 0.24 | 0.04 | 0.01, 0.06 | 0.001 |
| Knowledge | |||||||
| 3rd Grade curriculum (n = 1150) | 0.46 | 0.46 | 0.77 | 0.65 | 0.11 | 0.08, 0.15 | 0.001 |
| 4th Grade curriculum (n = 1150) | — | — | 0.70 | 0.67 | 0.04 | 0.01, 0.06 | 0.013 |
| 5th Grade curriculum (n = 1150) | — | — | 0.55 | 0.48 | 0.07 | 0.03, 0.11 | 0.001 |
| Attitudes | |||||||
| Physical activity self-efficacy (n = 1146) | 0.66 | 0.66 | 0.78 | 0.75 | 0.03 | 0.00, 0.06 | 0.060 |
| Food self-efficacy (n = 1149) | 0.69 | 0.72 | 0.75 | 0.76 | −0.02 | −0.05, 0.02 | 0.332 |
| Reported behaviors | |||||||
| Food choice intentions (n = 1150) | 0.46 | 0.46 | 0.66 | 0.53 | 0.12 | 0.07, 0.18 | 0.001 |
Results are from mixed-models analyses. See Subjects and Methods for models used.
Calculated from mean values at follow-up (intervention – control).
Analyses of the menus and recipes showed the same trends as seen in the data from the lunch observation (data not shown). The energy content of the lunches served was 683 kcal in the intervention schools and 688 kcal in the control schools. The percentage of energy as fat was 28.2% in the intervention school and 32.0% in the control school.
Physical activity
Results of the physical activity measures at baseline and follow-up are presented in Table 3. The motion sensor measurements indicated no significant difference over a 24-h period between the children measured in the intervention and control schools. Self-reported physical activity levels (by Physical Activity Questionnaire) were higher among intervention-than control-school students at the end of the trial (Table 3). No increase in PE-related injuries was detected in the intervention schools on the basis of injury logs maintained by the schools (data not shown).
Knowledge, attitudes, and behavior
Knowledge targeted in the 3rd, 4th, and 5th grade Pathways curricula increased significantly in the children in the intervention schools compared with the control schools (Table 3). The difference tended to be largest for the information targeted in the 3rd grade curriculum (intervention group: 0.77; control group: 0.65). Self-efficacy to be physically active was higher in the intervention group than in the control group; however, there was no significant difference between the 2 groups in self-efficacy to choose healthy foods. Nevertheless, children who received the intervention reported more healthy food choice intentions than did control children.
Family participation
Intervention schools held 9 different family events throughout the 3 y. The events took place at each school and attracted, on average, 59% of the children enrolled in the study, or 0.9 adults per child. Relative to anecdotal reports of parental attendance at other school events, this attendance level appeared to be very good.
Process evaluation data indicated a strong degree of implementation for the classroom curriculum, with 94% of lessons completed. Seventy-eight percent of the food service guidelines were implemented, with a progression of 51%, 80%, and 87% for years 1, 2, and 3, respectively. The minimum of 3 PE sessions/wk was achieved by 81% of schools in the first year and by essentially 100% in years 2 and 3. However, only 56% of the schools reached the recommended goal of 5 sessions/wk. Average student attendance at family events over 3 y was 58%. The process evaluation data also indicated that a large majority of those attending family events enjoyed the activities and reported learning something new about diet, physical activity, and health.
DISCUSSION
A general aim of the Pathways Study was to implement a multicomponent school-based intervention for the primary prevention of obesity in public schools serving American Indian communities. Our study received strong support from tribal, educational, and community authorities, particularly the daily support of teachers, parents, and principals, who had to be actively involved in delivering and supporting the program. Almost the entire intervention was delivered by school personnel, teachers, and food service staff; the Pathways staff focused on research measurements and training and support of school staff.
The primary aim of the study was to reduce the rate of body fat gain in intervention schools, documented by a significant difference in the rate for the control schools after 3 y. This goal was not reached, and %BF in both groups was essentially identical at the end of the intervention period.
Over the past 30 y, several school-based studies have implemented and evaluated programs aimed at reducing cardiovascular disease risk or obesity prevalence (22–34). Several of these programs were targeted at only obese children and thus did not attempt to modify risk behaviors in nonobese children. The results from true primary prevention interventions that included at least a dietary and a physical activity component show that most interventions were able, to a variable degree, to reduce dietary fat intake, increase physical activity during school time, increase consumption of fresh fruit and vegetables, and reduce television viewing (23, 31–34). However, these studies also indicate the resiliency of body weight and adiposity in this age group: virtually none of these interventions, which ranged in duration from 1 to 4 y, significantly reduced average body weight or adiposity in interventions. One of these studies, the Planet Health intervention (31), showed a significant reduction in obesity prevalence, defined by a combination of BMI and triceps-skinfold thickness, but only in girls.
A reduction in the rate of body fat accumulation in children requires a net decrease in positive energy balance, leaving less unspent energy available for storage as adipose tissue. This can be achieved by reducing energy intak, increasing energy output through physical activity, or both. Because our intervention was aimed at all children at the school and not only at those with excess body weight, restriction of energy intake was not an option. Furthermore, the federal school lunch and breakfast programs have minimum mandatory amounts of calories to be served at school cafeterias. Thus, instead of targeting calories, our food service intervention aimed at reducing the energy density of foods by reducing their fat content and at increasing the availability of less energy-dense foods, such as fresh fruit and vegetables. These changes resulted in a significantly lower percentage of energy as fat at lunch in the intervention schools than in the control schools: 28.2% compared with 32.4% (Table 3).
The 24-h dietary recall at the end of the study showed a significantly lower total daily energy intake in the intervention group, ≈150 kcal/d less than in the control group. Because there were no significant differences in weight, adiposity, or physical activity between the groups, this difference in energy intake may be the result of reporting bias. Alternatively, the reduction in energy intake in the intervention schools may have occurred too late in the study to cause a significant difference in body weight or adiposity by the time of the follow-up measurement. Excess weight gain during the 3-mo summer recess, which was not assessed, is another possible mechanism.
The second approach to reduce excess positive energy balance was to increase energy expenditure by increasing the time children spent in moderate-to-vigorous physical activity. By including physical activity breaks throughout the day, our physical activity intervention sought to increase the daily active time and reduce sedentary time, an approach positively associated with weight maintenance in reduced-obese children (35). Although the motion sensor data indicated a positive trend toward more active time in the intervention schools, this measurement did not confirm the significant increase in PE found by self-report on the questionnaire. Note that whereas the motion sensor data are a direct measurement of physical activity, the questionnaire provides the self-reported frequency of a limited number of activities.
The significant effect of the intervention on the fat content of the school menus and the dietary fat intake of children show that a reduction in caloric density and in the consumption of saturated fat are feasible while maintaining adequate total energy and micronutrient intakes. Food preparation techniques to reduce fat content and the introduction of low-fat products were ultimately widely accepted by children and by food service personnel. However, these changes were only progressively implemented, and only 51% of scheduled guidelines were implemented during the first year of the intervention.
In summary, the Pathways Study showed that significant reductions in the fat content of school menus and in the dietary fat intake of children can be achieved by training and supporting food service staff. The study also showed that properly trained teachers can achieve significant changes in the health-related knowledge and behaviors of 7–10-y-old children with the use of a culturally appropriate classroom curriculum. The intervention showed positive but no statistically significant trend in the level of physical activity during school time. The lack of effect of the intervention on %BF suggests that more intense or longer interventions may be needed to modify the continuing trend toward higher adiposity in this population.
Acknowledgments
We express our deepest appreciation to all of the Pathways Study staff who assisted in the development and implementation of the study and to the students, parents, leaders, school staff, school administrators, and American Indian communities at the study locations: Gila River Indian Community of Arizona (Akimel O’odham), Tohono O’odham Nation, Navajo Nation (Dine), Oglala Sioux Tribe (Oglala Lakota), Rosebud Sioux Tribe (Sicangu Lakota), San Carlos Apache Tribe (Dee’), and the White Mountain Apache Tribe (Ndee’).
Supported by National Heart, Lung, and Blood Institute grants U01-HL-50869, -50867, -50905, -50885, and -50907.
Footnotes
All authors were members of the study’s Steering Committee and had direct responsibility, as principal investigators or field center coordinators, for the oversight of the study, including its design and the collection and interpretation of data. JS and the staff at the study’s coordinating center were responsible for data processing and analysis. BC drafted this manuscript, which was reviewed and approved by all authors. None of the authors had financial interests related to this study.
Personnel at each of the participating field centers are as follows. Gila River Indian Community and University of Arizona (Tohono O’odham): Larry Stephenson and Timothy Lohman (Principal Investigators), K Booth, C Cornell, J Ekland, Scott Going, H Flint-Wagner, J Martin, L Metcalfe, L Nielson, Juanita Pablo, and J Weber; Johns Hopkins University (White Mountain Apache Tribe and San Carlos Apache Tribe): Benjamin Caballero (Principal Investigator and Chair, Steering Committee), Jean Anliker, Ronald Alsenay, Jackie Altaha, Joelian Armstrong, Lucie Billie, Becky Ethelbah, Joel Gittelsohn, Stacy Gyenizse, Corleone Hastings, Delta Hinton, Sheri Kessay, Lydia Kinney, David Nelson, and Ray Reid. University of Minnesota (Oglala Sioux Tribe and Rosebud Sioux Tribe): Mary Story (Principal Investigator), John Himes, Lisa Harnack, Bonnie Holy Rock, Mary Smyth, Pat Snyder, Wilbur Ferguson, Pam Livermont, Mary Jane Steele, Dawn Rassmusson, Patty Iron Cloud, Cordelia White Elk, Travis Goings, Liz Kingi, and Mona Massingale. University of New Mexico (Navajo Nation): Sally M Davis (Principal Investigator), Vivian Arviso, Catherine Axtell, Elverna Bennett, Brenda Broussard, Theresa Clay, Dustin Cole, Leslie Cunningham-Sabo, Michelle Curtis, Anne Doering, David Fenn, Willow Foster, Blanche Harrison, Karen Heller, Francesca Lanier, Raylene McCalman, Will McCoy, Cindy McKay Chavez, Rachel Middleman, Lydia Montoya, Marla Pardilla, Shirley Pareo, Harrison Platero, Stephanie Rider Pier, Nancy Risenhoover, Jennifer Schoenberg, Betty Skipper, Janice Thompson, Leslie Trickey, and Venita Wolfe. University of North Carolina at Chapel Hill (Coordinating Center): June Stevens (Principal Investigator), Ed Davis, Allan Steckler, Chirayath Suchindran, Richard Brice, Brad Black, Nancy Cohn, Kim Ring, Dawn Stewart, and Mal Foley. National Heart, Lung, and Blood Institute: Marguerite Evans, Richard Fabsitz, Sally Hunsberger, Jared B Jobe, James Norman, and Elaine Stone.
Members of the Data Safety and Monitoring Board are as follows: Philip Nader (Chair; University of California, San Diego), Tom Baranowski (Baylor College of Medicine, Linda Burhansstipanov, Pine, CO), Allan Donner (University of Western Ontario), Sue YS Kimm (University of Pittsburgh), Barbara Shannon (Pennsylvania State University).
References
- 1.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents. Arch Pediatr Adolesc Med. 1995;149:1085–91. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 2.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. [PubMed] [Google Scholar]
- 3.Broussard BA, Johnson A, Himes JH, et al. Prevalence of obesity in American Indians and Alaskan Natives. Am J Clin Nutr. 1991;53(suppl):1535S–42S. doi: 10.1093/ajcn/53.6.1535S. [DOI] [PubMed] [Google Scholar]
- 4.Byers T. The epidemic of obesity in American Indians. Am J Dis Child. 1992;146:285–6. doi: 10.1001/archpedi.1992.02160150023013. [DOI] [PubMed] [Google Scholar]
- 5.Jackson MY. Height, weight, and body mass index of American Indian schoolchildren, 1990–91. J Am Diet Assoc. 1993;93:1136–40. doi: 10.1016/0002-8223(93)91645-7. [DOI] [PubMed] [Google Scholar]
- 6.Sugarman JR, White LL, Gilbert TJ. Evidence for a secular change in obesity, height, and weight among Navajo Indian schoolchildren. Am J Clin Nutr. 1990;52:960–6. doi: 10.1093/ajcn/52.6.960. [DOI] [PubMed] [Google Scholar]
- 7.Nelson DM. Height and weight changes among White Mountain Apache children. The IHS Provider. 1994:50–5. [Google Scholar]
- 8.Zephier E, Himes JH, Story M. Prevalence of overweight and obesity in American Indian school children and adolescents in the Aberdeen area: a population study. Int J Obes. 1999;23:S28–30. doi: 10.1038/sj.ijo.0800856. [DOI] [PubMed] [Google Scholar]
- 9.Caballero B. Obesity prevention in American Indian schoolchildren: Pathways. Am J Clin Nutr. 1999;69(suppl):745S–824S. doi: 10.1093/ajcn/69.4.745S. [DOI] [PubMed] [Google Scholar]
- 10.Caballero B, Davis CE, Evans MD, et al. Pathways: a school-based program for the primary prevention of obesity in American Indian children. J Nutr Biochem. 1998;9:535–43. doi: 10.1016/S0955-2863(98)00049-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gittelsohn J, Evans M, Story M, et al. Multisite formative assessment for the Pathways study to prevent obesity in American Indian schoolchildren. Am J Clin Nutr. 1999;69(suppl):767S–72S. doi: 10.1093/ajcn/69.4.767S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis SM. General guidelines for an effective and culturally sensitive approach to health education. In: Matiella AC, editor. Comprehensive health education in a multicultural world. Santa Cruz, CA: ETR Associates; 1994. [Google Scholar]
- 13.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Hovell MF, Nader PR. Project SPARK. Effects of physical education on adiposity in children. Ann N Y Acad Sci. 1993;699:127–36. doi: 10.1111/j.1749-6632.1993.tb18844.x. [DOI] [PubMed] [Google Scholar]
- 14.Lohman TG, Caballero B, Himes JH, et al. Estimation of body fat from anthropometry and bioelectrical impedance in Native American children. Int J Obes. 2000;24:1–7. doi: 10.1038/sj.ijo.0801318. [DOI] [PubMed] [Google Scholar]
- 15.Stevens J, Cornell CE, Story M, et al. Development of a questionnaire to assess knowledge, attitudes, and behaviors in American Indian children. Am J Clin Nutr. 1999;69(suppl):773S–81S. doi: 10.1093/ajcn/69.4.773S. [DOI] [PubMed] [Google Scholar]
- 16.Gittelsohn J, Harris S, Burris K, et al. Use of ethnographic methods for applied research on diabetes among Ojibwa-Cree Indians in Northern Ontario. Health Ed Q. 1996;23:365–82. doi: 10.1177/109019819602300307. [DOI] [PubMed] [Google Scholar]
- 17.Helitzer D, Davis S, Gittelsohn J, et al. Process evaluation in a multisite obesity primary prevention trial for Native American school children. Am J Clin Nutr. 1998;69(suppl):816S–24S. doi: 10.1093/ajcn/69.4.816S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tanner JM, Whitehouse RH. Clin longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51:170–9. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hunsberger S, Murray D, Davis CE, Fabsitz RR. Imputation strategies for missing data in a school-based multi-centre study: the Pathways study. Stat Med. 2001;20:305–16. doi: 10.1002/1097-0258(20010130)20:2<305::aid-sim645>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 20.Rubin D. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- 21.Caballero B, Himes JH, Lohman TG, et al. Body composition and overweight prevalence in 1,704 schoolchildren from seven American Indian communities. Am J Clin Nutr. 2003 doi: 10.1093/ajcn/78.2.308. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harrell JS, Gansky SA, McMurray RG, Bangdiwala SI, Frauman AC, Bradley CB. School-based interventions improve heart health in children with multiple cardiovascular disease risk factors. Pediatrics. 1998;102:371–80. doi: 10.1542/peds.102.2.371. [DOI] [PubMed] [Google Scholar]
- 23.Luepker RV, Perry CL, McKinlay SM, et al. Outcomes of a field trial to improve children’s dietary patterns and physical activity. JAMA. 1996;275:768–76. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 24.Ewart CK, Young DR, Hagberg JM. Effects of school-based aerobic exercise on blood pressure in adolescent girls at risk for hypertension. Am J Public Health. 1998;88:949–51. doi: 10.2105/ajph.88.6.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The DISC Collaborative Research Group. The efficacy and safety of lowering dietary intake of total fat, saturated fat, and cholesterol in children with elevated LDL-choleserol: the dietary intervention study in shildren (DISC) JAMA. 1995;273:1429–35. doi: 10.1001/jama.1995.03520420045036. [DOI] [PubMed] [Google Scholar]
- 26.Seltzer CC, Mayer J. An effective weight control program in a public school system. Am J Public Health. 1970;60:679–89. doi: 10.2105/ajph.60.4.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Angelico F, DelBen M, Fabiani L, et al. Management of childhood obesity through a school-based programme of general health and nutrition education. Public Health. 1991;105:393–8. doi: 10.1016/s0033-3506(05)80599-2. [DOI] [PubMed] [Google Scholar]
- 28.Donnelly JE, Jacobsen DJ, Whatley JE, et al. Nutrition and physical activity program to attenuate obesity and promote physical and metabolic fitness in elementary school children. Obes Res. 1996;4:229–43. doi: 10.1002/j.1550-8528.1996.tb00541.x. [DOI] [PubMed] [Google Scholar]
- 29.Brownell KD, Kaye FS. A school-based behavior modification, nutrition education, and physical activity program for obese children. Am J Clin Nutr. 1982;35:277–83. doi: 10.1093/ajcn/35.2.277. [DOI] [PubMed] [Google Scholar]
- 30.Simonetti D’Arca A, Tarsitani G, Cairella M, et al. Prevention of obesity in elementary and nursery school children. Public Health. 1986;100:166–73. doi: 10.1016/s0033-3506(86)80030-0. [DOI] [PubMed] [Google Scholar]
- 31.Gortmaker SL, Peterson KE, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth (Planet Health) Arch Pediatr Adolesc Med. 1999;153:409–18. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 32.Gortmaker SL, Cheung LWY, Peterson KE, et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children. Arch Pediatr Adolesc Med. 1999;153:975–83. doi: 10.1001/archpedi.153.9.975. [DOI] [PubMed] [Google Scholar]
- 33.Perry CL, Stone EJ, Parcel G, et al. School-based cardiovascular health promotion: the child and adolescent trial for cardiovascular health (CATCH) J School Health. 1990;60:406–13. doi: 10.1111/j.1746-1561.1990.tb05960.x. [DOI] [PubMed] [Google Scholar]
- 34.Simons-Morton B, Parcel G, Baranowski T, Forthofer R, O’Hara NM. Promoting physical activity and a healthful diet among children: results of a school-based intervention study. Am J Public Health. 1991;81:986–91. doi: 10.2105/ajph.81.8.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epstein LH, Valoski A, Vara LS, et al. Effects of decreasing sedentary behavior and increasing physical activity on weight change in obese children. Health Psychol. 1991;14:109–15. doi: 10.1037//0278-6133.14.2.109. [DOI] [PubMed] [Google Scholar]