Abstract
To overcome challenges associated with optimizing function and physical activity among hospitalized older adults we developed Function Focused Care for Acute Care (FFC-AC). The purpose of this study was to test the feasibility and preliminary effectiveness of this intervention. We hypothesized that hospitalized trauma patients exposed to FFC-AC would: (1) maintain or improve function, spend more time in physical activity and have fewer adverse events between admission and discharge; and (2) maintain or improve function, have less fear of falling, fewer depressive symptoms, less pain, be more physically resilient and be less likely to experience adverse events at one month post discharge compared to those exposed to FFC-Education Only (EO). FFC-AC was implemented by a Research Function Focused Care Nurse who worked on the participating units for 20 hours a week for 16 months to implement the three components of FFC-AC. The sample included 89 older orthopedic trauma patients the majority of whom were female (N=59, 66%), white (N= 82, 92%) and not married (N=53, 59%). At discharge and/or 30 days post discharge participants in the treatment site showed greater improvement in function, less fear of falling and better physical resilience when compared to those in the FFC-EO site. Future research is needed to continue to work on engaging staff in function focused care approaches and optimizing the hospital environment and policies to support nurses in this type of care approach.
Keywords: Trauma, Older Adults, Function
It has repeatedly been recognized that early mobility and engagement in other functional activities has a positive impact on physical and psychosocial outcomes among older adults post hospitalization. In a recent review article it was concluded that there were significant physical benefits associated with inpatient mobilization and no evidence for associated risk of adverse events (Kalish, Lee, & Dabney, 2013). Benefits included less pain (Augustin, de Quadros, & Sarmento-Leite, 2010), less risk of delirium (Schweickert et al., 2009) or adverse events such as deep vein thrombosis (Chandrasekaran, Ariaretnam, Tsung, & Dickison, 2009; Nakao et al., 2010), urinary tract infections (Kurabe, Ozawa, Watanabe, & Aiba, 2010; Langhorne et al., 2010) or pneumonia (Clark, Lowman, Griffin, Matthews, & Reiff, 2013; Kurabe et al., 2010), and no increase in falls (Clark et al., 2013; Fisher, Galloway, et al., 2011). Moreover, ambulation and other types of physical activity helped to prevent the all too common functional decline noted in older hospitalized patients (Cumming et al., 2011; Langhorne et al., 2010).
Despite known benefits, physical activity is not routinely encouraged and older hospitalized adults continue to engage in very low levels of activity once hospitalized (Brown, Redden, Flood, & Allman, 2009; Resnick, Galik, Wells, Boltz, & Holtzman, in press). Generally older hospitalized medical patients spend at least 83% of their acute care stay in bed (Brown et al., 2009) and engage in only 2.4 minutes (SD=2.5) of moderate level of activity ( Resnick et al., in press).
Physiologically, lying in a bed results in a decrease in hydrostatic pressure within the cardiovascular system, an unloading of the forces of the skeletal muscles and a decrease in total energy expended. This adversely affects multiple systems particularly the musculoskeletal, cardiovascular and pulmonary systems and has psychological consequences. Among adults there is a reduction in anabolic processes and an increase in catabolic processes of the muscle proteins with an approximately 5% rate of loss of muscle and strength over the first few days of bedrest (Stein & Wade, 2005). It is anticipated that the rate of loss is even more among older adults who are more likely to be sarcopenic and have less muscle mass, increased intramuscular fat and decreased muscle thickness. The first three days of bedrest also result in hypovolemia initiated by the cephalad fluid shift and a lack of arterial baroreceptor input (Platts et al., 2009) and an overall fluid loss ranging from 4–17%. This loss of fluid can result in orthostatic hypotension. In addition, bedrest commonly results in generalized myalgias and arthralgias (particularly head and back) and insomnia (Meck, Dreyer, & Warren, 2009).
The side effects and symptoms associated with bedrest result in a vicious cycle of continued bedrest and progressive functional loss and deconditioning. Orthostatic hypotension is often considered a risk factor for getting patients up when hospitalized (Nordon-Craft, Moss, Quan, & Schenkman, 2012) and pain and weakness make patients unwilling and unable to transfer out of bed. Increasingly, mechanical lifts are used which likewise propagate further weakening as this limits the activity that patients would otherwise participate in during transfers.
Patient factors, acute care environments, and medical and nursing interventions all influence functional decline ( Brown et al., 2009; Zisberg et al., 2015). Patient factors include age, sociodemographic characteristics, preexisting disability and disease states, delirium, cognitive status, anemia, pain, fear of falling, depression, motivation, nutritional status, sedation and polypharmacy. Acute care environments generally provide limited opportunity for any physical activity. The bed is often the only furniture in the hospital room, and the height of the bed or chairs may limit the patient's ability to transfer. Even when patients are encouraged to get out of bed, there generally are no pleasant walking areas or destinations and patients are restricted from walking to tests and procedures (Resnick et al., 2011).
Medical factors and interventions limiting physical activity and contributing to functional decline include the tethering effects of such things as indwelling urinary catheters, sequential compression devices, continuous pulse oximetry and intravenous infusions; prescribed bedrest; sedating medications; insufficient or excessive management of pain; and limited food/fluid (Leditschke, Green, Irvine, Bissett, & Mitchell, 2012; Zisberg et al., 2015). Nurses working in acute care tend to focus on completing physical assessments of patients, medication administration and indirect care activities (Resnick et al., in press) with little time spent encouraging physical activity (Boltz, Resnick, Capezuti, & Shabbat, 2011; Resnick et al., in press). In addition, nurses tend to perform functional tasks for patients (e.g., bathing the patient) which further eliminates opportunities for physical activity ( Leditschke et al., 2012).
To overcome the challenges associated with optimizing function and physical activity among hospitalized older adults we developed the Function Focused Care for Acute Care (FFC-AC) intervention (Table 1). When implemented in long term care settings, Function Focused Care maintained and improved function, increased physical activity and decreased risk for adverse events (Galik, Resnick, Hammersla, & Brightwater, 2014; Resnick & Galik, 2014). The purpose of this study was to test the feasibility and effectiveness of FFC-AC. Specifically, it was hypothesized that hospitalized patients exposed to FFC-AC would: (1) maintain or improve function, spend more time in physical activity and have fewer adverse events between admission and discharge; and (2) maintain or improve function, have less fear of falling, better mood, less pain, be more physically resilient and be less likely to experience adverse events at one month post discharge compared to those exposed to Function Focused Care-Education Only. Changing how patients are cared for in acute care settings is a critical next step to improving the persistent deconditioning older adults commonly experience during acute care hospitalizations.
Table 1.
Description of the Components of the Function Focused Care for Acute Care Intervention
| Component | Description of the Component |
|---|---|
| Component I : Education and Training |
Section 1: Overview of Function Focused Care; Section 2. Patient Goal Development; Section 3. Optimizing Physical Activity Safely; and Section 4. Patient Motivation. Classes were provided by an advanced practice nurse (APN) and physical therapist with function focused care experience. In the FFC-AC setting, nurses who missed attending a class were provided with the information during one-on-one sessions with the Research Function Focused Care Nurse (Research FFC Nurse). At the end of class, nurses completed the Knowledge of Function Focused Care Activities Test (Burkett et al., 2013; Resnick, Cayo, Galik, & Pretzer-Baboff, 2009). |
| Component II: Environmental and Policy Assessment |
Environment and policy assessments were done by the Research FFC Nurse with unit champions and recommendations for change discussed with administration and initiated as approved. |
| Component III: Ongoing Training and Motivation of Nurses |
The Research FFC Nurse engaged the involvement of the therapists working on the study units and mentored champions and staff nurses to integrate function focused care into routine patient care. This included: (a) oversight during patient admissions to assure that nurses evaluated patients for underlying physical capability and performance; (b) established physical activity goals for the patient; (c) used motivation strategies to encourage patients to engage in functional tasks and physical activity; and (d) eliminated known barriers to physical activity such as unnecessary tethers, pain, fear and sedation. |
Theoretic Basis of Function Focused Care-Acute Care
FFC-AC is theoretically based on the Social Ecological Model and Social Cognitive Theory and addresses many barriers that prevent physical activity (e.g., environmental barriers). FFC-AC uses established motivational interventions to change beliefs and is practical in that it incorporates physical activity into routine care. The Social Ecological Model addresses intra-personal, interpersonal, environment, and policy all of which influence behavior ( Gregson et al., 2003). Social Cognitive Theory (SCT) (Bandura A, 2004) is used at the interpersonal level to facilitate behavior change. Function focused care interactions include such things as nurses engaging patients in bed mobility during care so that the patient performs the activity with cueing versus the nurse performing the activity (e.g., the nurse pulling the patient up in bed); facilitating performance of activities of daily living; or ambulating patients to the bathroom or in the hallway and engaging families to do likewise.
Methods
Design
This study was a randomized trial including trauma units from two regionally designated trauma facilities. The settings were similar in that they were both Level I or II trauma centers, had designated trauma units, followed Maryland Institute for Emergency Medical Services Systems criteria and the American College of Surgeons Committee "Gold Book" to allocate resources, were teaching facilities and maintained similar staffing ratios and retention rates (1 nurse to 3–4 patients; <10% turnover of nursing staff annually). The hospitals were randomly allocated to treatment or attention control to avoid the risk of treatment carryover within hospitals.
Sample
Patients were eligible to participate in this study if they were 65 years of age or older, spoke English, and were admitted to a trauma unit in participating hospitals for a first trauma admission for any of the following ICD-9 codes: 805–809 Fracture Of Spine, Trunk; 810–819 Fracture Of Upper Limb; 820–829 Fracture Of Lower Limb; 830–839 Dislocation; 840–848 Sprains and Strains of Joints/Muscles. Patients were excluded from the study if they scored less than one out of three recall on the Mini-Cog (i.e., if they could not recall at least 1/3 words) (Borson, Scanlan, Chen, & et al, 2003), were in intensive care units, on a ventilator or had experienced a head trauma. As per the Institutional Review Board (IRB) and the Health Insurance Portability and Accountability Act (HIPAA), patients consented to participate in the study prior to determining eligibility. If the patient did not pass the Evaluation to Sign Consent he/she was asked to sign an assent to participate and the legally authorized representative (LAR) was asked to provide consent.
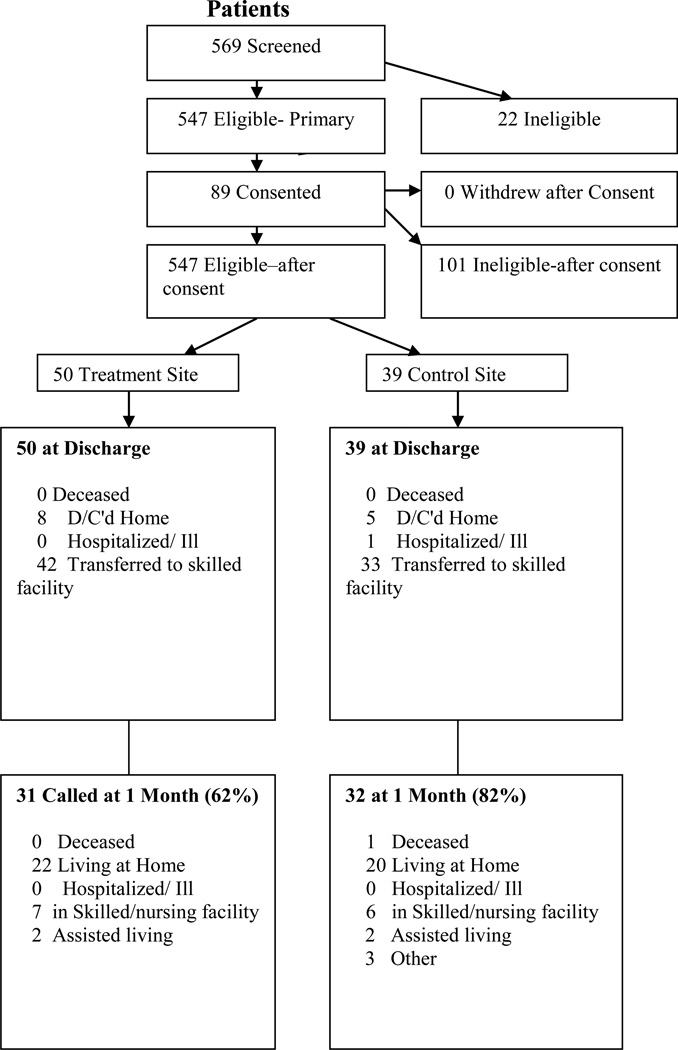
As shown in Figure 1, there were 569 older orthopedic trauma patients admitted to study hospitals and 547 of these individuals were eligible to participate. Of those eligible, 89 (16%) consented to participate and 210 (39%) refused. The remaining potentially eligible individuals were too sedated or confused to complete the assent (N=132, 24%), were discharged prior to being approached or had acute medical/surgical issues making approach impossible (N=116, 21%). Our consent rate of those approached was 30%. At follow up we were able to contact 63 participants (71%). There was no difference between those contacted versus not contacted with regard to number of fractures, age, comorbidities, cognition, transfer from another setting or length of stay. There was a difference, however, with regard to setting (more lost to follow up were from the treatment site), gender (more loss to follow up were males), and education level (more loss to follow up were less educated).
Figure 1.
Flow of Participants Through FFC-AC Trial
The majority of participants were female (N=59, 66%), white (N= 82, 92%), just over half were widowed, never married or divorced (N=53, 59%) with the others married (N=37, 41%). Approximately a quarter of the participants had at least some high school education or were high school graduates (N=22, 25%), approximately half had trade school, some college or a completed undergraduate degree (N=46, 51%) and the remaining had graduate degrees (N=20, 23%). The participants were 80 (SD=9) years of age and had on average 3 medical comorbidities (SD=3). The majority of the traumatic events were falls (N=68, 76%), 19 (21%) were motor vehicle accidents, 1 was related to a gunshot incidence (1%) and 1 involved a pedestrian trauma (1%).
Of the 89 participants, 24 (27%) were transferred from other non-trauma designated acute care settings to the trauma settings, 25(28%) did not require any surgical intervention and 10 (12%) were in the intensive care unit prior to being admitted to the medical units. Hip/femur fractures were the most common admitting diagnosis (N=36, 40%), with upper extremity fractures including shoulder, humerus and forearm being the next most frequent orthopedic event (N=16, 18%), then fractures of the spine (N=11, 13%), pelvis and acetabular fractures (N=10, 12%), sternal and rib fractures (N=9, 11%) and finally patella, tibia and/or fibula fractures (N=7, 8%). The majority of participants were admitted with a single fracture (N=60, 67%), although 19 (22%) of the participants had a second fracture, 7 (8%) had two additional fractures, 2 (8%) participants had 3 additional fracture and 1 (N=1%) had 4 additional fractures. There were no differences between patients in the control versus treatment group on any of the descriptive factors with the exception of a greater percentage of individuals in the treatment site having been transferred from another site prior to admission (treatment setting was 49% versus 0% in the control site, χ2 = 26.27, p=.001) and requiring intensive care unit admissions prior to being transferred to the medical trauma unit [9 in the treatment site (18%) versus 1 (3%) in the control site, χ2 = 26.27, p=.001].
Intervention
FFC-AC was coordinated and implemented by a Research Function Focused Care Nurse (Research FFC Nurse) who worked on the participating units for 20 hours a week over a 16 month period to implement the three components of FFC-AC (Table 1): Component I Education of Nurses; Component II Environmental and Policy Assessments; and Component III Ongoing Training and Motivation of Nurses. In addition, each unit was asked to identify at least two champions to work with the Research FFC Nurse over the course of the implementation period. Prior to recruitment of patients, the first two components of the FFC-AC intervention were implemented over a four month period to initiate behavior change among the nurses. The Research FFC Nurse continued to work with the designated champions and staff to role model function focused care interactions and guide and motivate staff to provide function focused care among all older trauma patients. Environmental and policy changes were initiated and education was reinforced and reiterated. The control intervention, FFC-ED included only Component I of FFC-AC, exposing the nurses in the control site to the same education as those in the FFC-AC site. Treatment fidelity was evaluated based on design, delivery, receipt and enactment as shown in Table 2.
Table 2.
Treatment Fidelity Measures and Outcomes
| Component of Treatment Fidelity Evaluated |
Measure Used | Outcomes |
|---|---|---|
| Design | Adherence to randomization | Only those in the treatment group/treatment setting were exposed to Components II and III of FFC-AC. |
| Delivery | Education provided to both control and treatment sites; Function Focused Care Nurse in treatment site for 14 months and all components of FFC-AC done. |
All of the nurses in the FFC-AC site were exposed to education during the group classes (61%) or during one-on- one review (39%) with the Research FFC nurse. In the FFC-EO only site, 40% of the nurses were exposed to education during the group classes and the remaining 60% received the educational materials via a PowerPoint handout. |
| Receipt | Knowledge Test post educational component of the intervention for both treatment and control settings |
Mean scores on the knowledge test were similar across the sites [10.54 (SD=1.57) in the FFC-AC group and 10.09 (SD=.83) in the FFC-EO]. Both groups had a mean percentage score of 70% correct. |
| Enactment | Observed care interactions using the Function Focused Care Behavioral Checklist for Nurses; Tethering of patients by the nurses. |
Increased performance of function focused care activities by nurses in treatment site from a mean of 3.40 (SD=2.43) at 2 months post implementation of the intervention to a mean of 4.00 (2.82) at 8 months and a mean of 5.58 (SD=3.20) at 12 months; and decreased tethering by nurses in treatment sites versus control site (Overall Wald χ2 = 214.23, p=.001; p at discharge = .01). |
Measures
Descriptive information included age, gender, race, marital status, education, traumatic event and admission orthopedic diagnosis, course between the traumatic event and admission to the medical unit (e.g., transfer from a different hospital, surgical interventions, and days in intensive care), comorbidities based on the Charlson Comorbidity Index (Charlson, Pompei, Ales, & MacKenzie, 1987), cognitive status based on the Mini-Cog (Borson et al., 2003) and discharge location and living location at 1 month post discharge. Adverse events during hospitalization included infections, pressure ulcers, and acute events requiring transfers off the trauma unit (e.g., need for acute surgical interventions or medical monitoring). Data was obtained based on chart review. Outcome measures are described Table 3 along with evidence of reliability and validity. Survey responses were obtained directly from patients and confirmed with nursing staff with regard to function and physical activity outcomes.
Table 3.
Outcome Measures
| Concept | Measure | Description of Measure and Reliability and Validity |
|---|---|---|
| Cognition | Mini-Cog | Includes a three-item recall test for memory and a scored clock-drawing test (CDT) (Borson et al., 2003). The Mini-Cog has established validity, inter-rater and test-retest reliability. |
| Comorbidities | Charlson Comorbidity Index (CCI) |
Includes 19 diseases that were weighted and summed (Charlson et al., 1987). Prior use demonstrated predictive validity, test-retest reliability and inter-rater reliability. |
| Pain | Verbal Descriptor Scale |
Provides patients with the opportunity to describe pain [none (1) to excruciating (6)] and has evidence of concurrent validity and test-retest reliability (Herr, 2011; Herr, Spratt, Mobily, & Richardson, 2004) |
| Fear of Falling | Fear of Falling | Patients are asked to rate their fear of falling on a scale of 0 to 4 (Scheffer, Schuurmans, Van Dijk, Van der Hooft, & De Rooij, 2008), There is evidence of test retest reliability and validity (Scheffer et al., 2008). |
| Depression | The 5-Item Geriatric Depression Scale |
Evaluates 5 symptoms of depression and use has demonstrated specificity, validity and interrater and test retest reliability (Rinaldi et al., 2003). |
| Delirium | Delirium-O- Meter |
Is an observation measure assessing 12 symptoms of delirium. Prior use supported internal consistency and validity (de Jonghe et al., 2005) |
| Physical Resilience |
The Physical Resilience Measure |
Includes 17 items reflecting resilience with prior use providing evidence of reliability and validity based on Rasch analysis (Resnick, et al., 2011). |
| Function | Barthel Index | Evaluates basic activities of daily living with varying degrees of assistance. Prior use provided evidence of internal consistency and validity (Mahoney, 1965; Sainsbury, Seebass, Bansal, & Young, 2005). |
| Performance | Physical Performance Mobility Exam (PPME) |
Includes 6 tasks which are observed (low to high functioning). Prior testing established test retest and inter-rater reliability (r=.86) and inter-rater reliability (96.6%) and convergent and divergent validity (Sherrington, 2005; Winograd et al., 1994). |
| Actigraphy | ActiGraph (24 hours) |
Objectively measured oactivitybased onactivity counts Prior use has demonstrated evidence of reliability and validity (ActiGraph, 2004). |
| Physical Activity Survey |
Physical Activity Survey in Long Term Care |
A subjective measure of physical activity performed over a 24 hour period. Prior use provided evidence of criterion-referenced validity and inter-rater reliability (Resnick & Galik, 2007). |
| Function Focused Care Knowledge Test |
Knowledge of Function Focused Care |
A 15-item paper and pencil test There is evidence of test-retest reliability and validity based on contrasted groups (Burkett et al., 2013). |
| Objective function focused care behaviors of patients |
Function Focused Care Behavior Checklist for Patients |
A 19 item checklist reflecting patients' enactment of function focused care activities. There is evidence of inter-rater reliability and (Boltz, Capezuti, Shuluk, Secic, 2012). |
| Objective function focused care behaviors by nurses |
Function Focused Care Behavior Checklist for Nurses |
A 19 item checklist reflecting nurses’ performance of function focused care. Prior testing provided evidence of inter-rater reliability , validity was based on contrasted groups and Rasch analysis (Resnick et al., 2007) |
Measures
Function, performance and physical activity were evaluated based on the Barthel Index (Mahoney, 1965), the Physical Performance and Mobility Examination (Winograd et al., 1994), the Physical Activity Survey (Resnick & Galik, 2007), the Function Focused Care Behavior Checklist for Patients (Boltz et al., 2011) and Actigraphy (ActiGraph, 2004). Evidence of depressive symptoms were evaluated using the 5-Item Geriatric Depression Scale (GDS-5)(Rinaldi et al., 2003). Pain was based on verbal report of pain (yes or no) and the patient’s description of the intensity of the pain using the Pain Verbal Descriptor Scale (VDS)(Herr, 2011). Delirium was evaluated using the Delirium-O-Meter (DOM) (de Jonghe, Kalisvaart, Timmers, Kat, & Jackson, 2005). Fear of falling was based on a single item question rating fear on a scale of 0 (no fear) to 4 (a lot of fear) and physical resilience was measured using the Physical Resilience Scale (Resnick, Galik, Dorsey, Scheve, Gutkin, 2011).
Treatment Fidelity Data
To establish receipt, the 15-item Knowledge of Function Focused Care test (Burkett, Hippensteel, Penrod, & Resnick, 2013) (Table 4) was given to all nurses in both treatment and control sites after exposure to the education session. Enactment of function focused care was evaluated based on evidence of decreased tethering of patients by the nurses and evidence of function focused care being provided during observed care interactions using the Function Focused Care Behavioral Checklist for Nurses (Resnick, Rogers, Galik, & Gruber-Baldini, 2007)(Table 4). Tethering was based on a sum of the total number of tethers patients were exposed to (indwelling urinary catheters, sequential compression devices, continuous intravenous, fall alarms, cardiac monitoring, restraints, orders for bedrest or negative pressure wound therapy devices).
Table 4.
Patient Outcomes by Treatment Site, N=89
| FFC-ED |
FFC-AC |
|||
|---|---|---|---|---|
| N=39 |
N=50 |
|||
| Outcome | Mean (S.E.) | Mean (S.E.) | Mean (S.E.) | p-value* |
| Function | ||||
| Barthel Index, 0–100 | 0.001 | |||
| Admission | 34.45(3.22) | 41.84(3.44) | 27.36(2.57) | 0.001 |
| Discharge | 44.57(2.74) | 48.50(5.07) | 39.94(2.79) | 0.140 |
| One Month Post Discharge | 84.14(2.95) | 90.04(3.76) | 78.21(4.37) | 0.040 |
| Performance | ||||
| Physical Performance and Mobility Exam, 0–16 | 0.130 | |||
| Admission | 1.11(.26) | 1.58(0.5) | 0.65(0.15) | 0.070 |
| Discharge | 1.64(.57) | 1.00(0.33) | 2.38(1.03) | 0.200 |
| Actigraph | ||||
| Discharge counts | NA | 37329(32171) | 62092(40029) | 0.090 |
| Discharge moderate activity (minutes) | NA | 2.68(3.78) | 3.44(3.36) | 0.570 |
| Physical Activity Survey (mobility) | 0.039 | |||
| Admission | .69(.26) | 1.58(0.49) | 0.20(0.19) | 0.070 |
| Discharge | .76(.38) | 0.78(0.54) | 0.74(0.49) | 0.950 |
| Physical Activity Survey (personal care) | 0.270 | |||
| Admission | 30.26(1.92) | 33.39(2.74) | 27.14(2.66) | 0.100 |
| Discharge | 33.78(3.38) | 35.35(3.77) | 32.21(2.99) | 0.510 |
| Physical Activity Survey (exercise ) | 0.030 | |||
| Admission | 12.68(2.35) | 18.76(4.24) | 6.60(2.05) | 0.010 |
| Discharge | 14.01(2.01) | 9.04(3.04) | 5.00(1.87) | 0.260 |
| Depression, 0–1 | 0.020 | |||
| Admission | .38(.05) | 0.26(0.07) | 0.50(0.07) | 0.010 |
| Discharge | .40(.06) | 0.25(0.09) | 0.54(0.08) | 0.020 |
| One Month Post Discharge | .33(.06) | 0.18(0.08) | 0.48(0.09) | 0.010 |
| Fear of Falling, 0–4 | 0.001 | |||
| Admission | 1.78(.18) | 1.64(0.29) | 1.88(0.22) | 0.510 |
| Discharge | 1.55(.22) | 2.29(0.35) | 1.35(0.27) | 0.030 |
| One Month Post Discharge | 1.12(.22) | 1.18(0.36) | 0.73(0.20) | 0.260 |
| Pain, 0–1 | 0.450 | |||
| Admission | .61(.05) | 0.62(0.08) | 0.60(0.07) | 0.880 |
| Discharge | .50(.07) | 0.50(0.1) | 0.50(0.09) | 1.000 |
| One Month Post Discharge | .47(.07) | 0.41(0.1) | 0.52(0.09) | 0.440 |
| Pain Intensity, 1(none)-6(excruciating) | 0.040 | |||
| Admission | 2.37(.16) | 2.41(0.25) | 2.34(0.19) | 0.820 |
| Discharge | 2.21(.20) | 2.38(0.33) | 2.09(0.23) | 0.470 |
| One Month Post Discharge | 1.75(.16) | 1.64(0.24) | 1.83(0.21) | 0.550 |
| Tethering, 0–10 | 0.001 | |||
| Admission | 2.74(.12) | 1.28(0.18) | 4.20(0.16) | 0.010 |
| Discharge | 2.06(.14) | 0.95(0.16) | 3.17(0.24) | 0.010 |
| Skills performed, 0–4 | 0.001 | |||
| Admission | 1.06(.23) | 1.55(0.29) | 0.56(0.16) | 0.001 |
| Discharge | .49(.19) | 0.75(0.21) | 0.23(0.15) | 0.040 |
| Delirium, 0–36 | 0.910 | |||
| Admission | .80(.21) | 0.90(0.35) | 0.69(0.23) | 0.620 |
| Discharge | .95(.50) | 0.91(0.32) | 1.00(0.47) | 0.890 |
| Resilience, 0–17 | 0.001 | |||
| Baseline | 12.97(.25) | 12.71(0.38) | 13.25(0.33) | 0.270 |
| Discharge | 13.20(.30) | 13.04(0.43) | 13.42(0.4) | 0.510 |
| One Month Post Discharge | 13.79(.51) | 12.9(1.07) | 14.55(0.28) | 0.040 |
p-values for overall intervention tests and for group comparison at each time point are provided
Data Analysis
Descriptive analysis of the data by experimental group was done at baseline to evaluate for differences in these factors. Generalized estimating equations (GEE) were used to test the intervention effects. For each outcome, exploratory analyses (scatterplots, frequencies, and boxplots) were performed to assess model assumptions. There were no baseline treatment group differences with regard to cognitive status, age, race, education, marital status or gender. Chi-square or Fisher’s Exact test was done to determine if there were treatment differences with regard to re-hospitalizations and adverse events (i.e., whether or not there was an adverse event that occurred). An analysis of variance was done to evaluate differences in Actigraphy findings at discharge (single one time testing time point). All tests were two-sided with a 5% significance level, adjusted for clustering within hospital settings and baseline differences were controlled for as appropriate.
Results
As shown Table 4, on admission the participants were functionally dependent and engaged in less than a minute per day in mobility/ambulation, approximately 30 minutes per day in personal care activities and less than 15 minutes per day in exercise. Just a little over half of the participants reported pain, 62% reported some fear of falling, they were generally physically resilient, over a third screened positively for depression and there was limited evidence of delirium. The overall length of stay on the trauma units was 4.92 days (SD=3.30) and participants were exposed to 2 to 3 tethers during the hospital stay, 2 to 3 physical therapy sessions and 2 occupational therapy sessions.
There were differences between the groups at baseline with regard to function, reported time in exercise, depressive symptoms, the amount of tethering and the number of function focused care behaviors the patients engaged in. There were no baseline differences between the groups with regard to the other outcome variables or number of therapy sessions they received. Overall 6 participants had infections, 4 needed to be transferred to the intensive care unit, 3 needed additional surgery and 1 individual obtained a pressure ulcer during the hospital stay. There was no difference between the groups with regard to percentage of individuals experiencing any one of the four adverse events during hospitalization (χ2 = 2.20, p=.14).
There was no significant difference at discharge between groups with regard to function (p at discharge =.14) or verbal reports of time spent in mobility (p=.13). Objective recording of physical activity at discharge showed a trend toward the treatment group spending more time in overall counts of activity based on 24 hour recording of Actigraphy. At discharge, the majority of participants were discharged to a skilled nursing facility (N=75, 84%) for rehabilitation, 13 (15%) were discharged home and one individual was discharged to another acute care hospital (1%). There was no difference between the two groups with regard to discharge location.
During the 30 days post discharge there were a total of 11 rehospitalizations (χ2 = .28, p=.59), 5 emergency room visits (χ2 = .01, p=.97), 3 falls (χ2 = .07, p=.79) and 7 infections (χ2 = 2.33, p=.13) and no differences between groups in these outcomes. Among those contacted, there was no difference between the groups with regard to living location. As shown in Figure 1, a total of 42 (47% of all participants) individuals lived at home and 20 (22% of all participants) were in nursing homes or assisted living or other type of supervised living setting, and 1 individual was deceased (1% of all participants) (χ2 = 1.81, p=.40). Consistent across treatment groups, approximately a third of the participants lived alone at 30 days post discharge (χ2 = .06, p=.81). There was no difference in the groups with regard to the percentage of individuals remaining in the nursing home at the 30 day follow up.
At 30 days post discharge, there was greater improvement in function (p=.04) and physical resilience (p=.04) among those in the treatment versus control group. There was a greater decrease in symptoms indicative of depression in the control group participants versus among those in the treatment group (p = .01). There was not a difference in the groups with regard to having pain or in pain intensity.
Treatment Fidelity
Overall we were able to implement all components of the intervention as intended and supported the delivery, receipt and enactment of the intervention activities. Environment and policies were evaluated and appropriate environmental changes made including replacing the unit toilets, which were not practical for trauma patients, with commode chairs. In addition, the routine policy for pulse oximetry on all patients was questioned and the FFC Nurse Facilitator worked with the nurses to decrease tethers when clinically appropriate. This was demonstrated by a significant decrease in the number of tethers patients experienced in the treatment versus control sites (p = .01). The educational component of the intervention was delivered as intended. In the FFC-AC hospital 61% of the nurses were exposed to education during group classes and the remaining during one-on-one interactions with the FFC Nurse Facilitator. In the FFC-EO site, 40% of nurses were exposed to the function focused care educational materials via the group classes and the remaining via a PowerPoint handout. Mean scores on the knowledge of function focused care test were similar across the groups with a mean of 10.09 (SD=.83) in the FFC-ED only group and a score of 10.54 (SD=1.57) in the FFC-AC group. Evidence of enactment of function focused care by nurses was based on an increase in the number of function focused care activities provided by the staff in the treatment site. This increased from a mean of 3.40 (SD=2.43) activities at 2 months post implementation of the intervention to a mean of 4.00 (2.82) at 8 months and a mean of 5.58 (SD=3.20) at 12 months.
Discussion
The findings from this study provided some evidence to support the feasibility and effectiveness of FFC-AC. Specifically, we were able to engage champions to work with us and to recruit study participants. Our recruitment rate was low at 30% of those approached but consistent with findings from prior studies in acute care (Boltz, Resnick, Chippendale, & Galvin, 2014; NeSmith et al., 2013). The biggest challenges with regard to recruitment were related to medical problems and sedation as patients who were nonresponsive due to drug side effects could neither consent nor assent. In future work, it would be helpful to obtain a waiver of written assent given the acute status of these individuals. Likewise, a waiver to allow for verbal consent from licensed authorized representatives that could not meet face-to-face would further facilitate the recruitment process.
Although we were able to implement the intervention as intended, there were some challenges identified. Unit champions in the intervention site were identified and willing to work with us for the 12 month intervention period. Due to clinical responsibilities, however, they were often not accessible and acute patient needs took precedence over meeting with the Function Focused Care Nurse Facilitator. Similarly, there was administrative support for the study, although these individuals (e.g., unit managers) did not provide any direct supervision, acknowledgement or positive reinforcement for the work done by the champions. In future research, we would strongly recommend the use of a more participatory approach based on the Evidence Integration Triangle (EIT) (Glasgow, Green, Taylor, & Stange, 2012). An EIT approach brings together evidence (e.g., the effectiveness of a function focused care approach) and key stakeholders from the hospital setting to influence care practices. EIT includes: participatory implementation processes, provision of practical evidence-based interventions, and pragmatic measures of progress toward goals. Further, the EIT approach allows for differences between settings and encourages tailoring of the implementation process.
As might be expected from patients following an orthopedic trauma, the participants in this study had very low levels of physical function and activity at both baseline and discharge. The majority of the study participants sustained lower extremity fractures which certainly could impact independent ambulation. Lower extremity fractures do not explain the limited performance of bathing, dressing and grooming. The treatment site participants demonstrated particularly low levels of function. We anticipate this was because these individuals experienced non-fracture associated complications, spent days in the intensive care unit prior to transfer to the medical trauma units and were more likely to have been transferred from another acute care site based on the Maryland Interhospital Transport Guidelines (Maryland Institute of Emergency Medicine Services System, 2014). Based on these guidelines, individuals over 55 years of age who sustained a trauma were automatically transferred to a trauma center, if not initially transported to such a center. The site randomized to treatment was designated in this guidance as the Primary Adult Resource Center and so patients from other acute care settings were generally transported to the treatment site over other state trauma centers. While we controlled for baseline differences between the settings in terms of function and activity, there may have been medical conditions and interventions that were difficult to quantify or control for such as internal trauma or contusions.
As was noted in our study, prior research with patients admitted for medical reasons (Zisberg et al., 2011) has shown that not all older hospitalized patients demonstrate a decline in function. As with medical patients, for trauma patients there may have been some natural course of improvement once the traumatic event and/or any underlying medical problem was stabilized.
Consistent with prior research (Edmonds & Smith, 2014; Pedersen et al., 2013) our study found that there was limited amounts of time spent in physical activity among trauma patients. Although not statistically significant, based on survey and objective actigraphy data the participants in the treatment group engaged in more time in physical activity at discharge compared to those in the control group. This small improvement was also noted in the study by Boltz et al. (Boltz et al., 2014) in which nurses and families were taught to optimize function and physical activity among older hospitalized patients. The findings of both of these studies suggest that working with nursing staff to engage patients in physical activity during the acute care stay may help patients’ maintain function and engage in physical activity. Unfortunately, there continues to be a limited focus on function and activity among patients and a greater emphasis on use of advanced medical interventions (e.g., ongoing tethering with pulse oximetry and monitoring) , narcotics and psychotropic medications (Leditschke et al., 2012). In less developed countries such as China, nursing care focuses on prevention, health care, life cultivation and rehabilitation rather than administration of medications and invasive procedures and interventions (Hao, Liu, Yue, & Liu, 2011). In China nurses spend the greatest percentage of their time focused on elimination issues for patients (22% of time), nutrition (21% of time) and nursing procedures (17% of time) (Jiang, Li, Ma, & Gu, 2015). Medication administration includes just 8% of nursing time and rehabilitation exercise involves 3% of nursing time. This is in contrast to the four most commonly reported nursing activities performed by nurses in the United States: surveillance, intravenous therapy, fluid management and diet staging (Shever, Titler, Dochterman, Fei, & Picone, 2007).
Based on observations of patient care interactions there was limited evidence that nurses encouraged patients or facilitated their ability to engage in any type of physical activity. Although our treatment fidelity data demonstrated that the nurses in the treatment site provided more function focused care interventions over the course of the study period (e.g., encouraged patients to participate in personal care, transfer, ambulate) this was still limited to only 5 to 6 activities versus a total of 19 possible activities. Prior observation studies of nursing care have likewise noted that nurses are generally not focused on patients performance of physical activity and when they do it is limited to having the patient stand and transfer (Doherty-King, Yoon, Pecanac, Brown, & Mahoney, 2014). In addition to the many noted barriers around provider and caregiver beliefs and institutional policies, older hospitalized patients themselves do not expect to be physically active during their hospital stay (So & Pierluissi, 2012).
We had some success in overcoming environmental barriers to physical activity in the treatment setting. A persistent challenge throughout the course of the study, however, was the fear among nurses and other members of the health care team that older hospitalized patients would fall during their acute care stay. There were no falls in either setting during this study. Based on prior research there is no evidence to suggest that physical activity contributes to falls or any other adverse events in older adults (Bailey et al., 2007; Gruber-Baldini, Resnick, Galik, & Zimmerman, 2011). Rather, optimizing strength and function can facilitate fall prevention (Lahmann et al., 2015). In addition to fear, hospital based protocols and care cultures required involvement of physical therapy prior to having nurses transfer or ambulate a patient. In the treatment setting, our Research FFC Nurse was able to work with the unit champions and physical therapists on an initiative to have nursing evaluate patients at the bedside and determine if they were able to safely transfer and/or ambulate. This was an important first step in having nurses focus more on physical activity for hospitalized older patients post trauma and in bringing the disciplines together to optimize the care of patients.
The impact of the intervention on psychosocial outcomes also showed some positive trends with the exclusion of depression. At 30 days post discharge those in the treatment group showed a greater decline in fear of falling and greater increase in physical resilience when compared to the control group. These differences were small and may not be clinically significant. Consistent with other studies (Boltz et al., 2014; Jerofke, Weiss & Yakusheva 2014), these findings support the possibility, however, that encouragement by nurses to engage patients in physical activity post traumatic event can have a positive impact on psychosocial recovery.
Study Limitations
This study was limited by small sample size and the inclusion of only two trauma centers. While we controlled for clustering and differences in such things as function and physical activity at baseline, there may have been unknown factors that were not controlled. Findings were also limited by virtue of our recruitment of individuals who were able to self-consent and did not include those who were moderate to severely cognitively impaired, sedated or delirious. Future research needs to incorporate these individuals in such studies as they may be even more likely to benefit from function focused care interactions. In addition, we did not obtain information about function prior to admission (i.e., at least verbal report of that function). Future research should consider those findings. Lastly, although we obtained follow up on the majority of patients, we did miss follow up on approximately 25% of the sample. We believe these individuals were missing at random but it is possible that there may have been some bias (e.g., they may have been rehospitalized or placed in a long term care facility).
Conclusion
Despite these limitations the findings provide some evidence to suggest that implementing FFC-AC is feasible and is beneficial to patients. Future research is needed to continue to work on engaging staff in function focused care approaches and optimizing the hospital environment and policies to support nurses in this type of care approach.
Key points.
Engaging trauma patients in function and physical activity has the potential to improve clinical outcomes.
Currently older trauma patients are generally functionally impaired and spend little time in physical activity.
Nurses need to work closely with therapy to effectively engage trauma patients in physical activity.
Contributor Information
Barbara Resnick, University of Maryland School of Nursing, 655 West Lombard Street, Baltimore, MD 21201, Resnick@son.umaryland.edu, Phone: 410 706 5176; Fax: 410 706 0344.
Chris Wells, University of Maryland School of Medicine, 100 Penn St., Baltimore MD 21201.
Elizabeth Galik, University of Maryland School of Nursing, 655 West Lombard Street, Baltimore, MD 21201.
Lauren Holtzman, University of Maryland School of Nursing, 655 West Lombard Street, Baltimore, MD 21201.
Shijun Zhu, University of Maryland School of Nursing, 655 West Lombard Street, Baltimore, MD 21201.
Elise Gamertsfelder, University of Maryland Medical Center, Baltimore, MD 21201.
Terry Laidlow, University of Maryland.
Marie Boltz, Associate Professor, Boston College.
References
- ActiGraph. [Last accessed October, 2015];Actigraph Analysis Software. 2004 Available at http://www.theactigraph.com/ (3.2 User's Manual)
- Augustin A, de Quadros A, Sarmento-Leite R. Early sheath removal and ambulation in patients submitted to percutaneous coronary intervention: A randomized clinical trial. International Journal of Nursing Studies. 2010;47:939–945. doi: 10.1016/j.ijnurstu.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Bailey P, Thomsen GE, Spuhler VJ, Blair R, Jewkes J, Bezdjian L, Hopkins RO. Early activity is feasible and safe in respiratory failure patients. Critical Care Medicine. 2007;35(1):139–145. doi: 10.1097/01.CCM.0000251130.69568.87. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education Behavior. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Boltz M, Resnick B, Capezuti E, Shabbat N. Function-focused activity and changes in physical function in Chinese and non-Chinese hospitalized older adults. Rehabilitation Nursing. 2011;36(6):233–240. doi: 10.1002/j.2048-7940.2011.tb00088.x. [DOI] [PubMed] [Google Scholar]
- Boltz, Resnick B, Capezuti E, Shuluk J, Secic M. Functional decline in hospitalized older adults: Can nursing make a difference? Geriatric Nursing. 2012;33(4):272–279. doi: 10.1016/j.gerinurse.2012.01.008. [DOI] [PubMed] [Google Scholar]
- Boltz M, Resnick B, Chippendale T, Galvin J. Testing a family-centered intervention to promote functional and cognitive recovery in hospitalized older adults. Journal of the American Geriatrics Society. 2014;62(12):2398–2407. doi: 10.1111/jgs.13139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borson S, Scanlan J, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: Validation in a population-based sample. Journal of the American Geriatrics Society. 2003;51:1451–1454. doi: 10.1046/j.1532-5415.2003.51465.x. [DOI] [PubMed] [Google Scholar]
- Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. Journal of the American Geriatrics Society. 2009;57(9):1660–1667. doi: 10.1111/j.1532-5415.2009.02393.x. [DOI] [PubMed] [Google Scholar]
- Burkett T, Hippensteel N, Penrod J, Resnick B. Pilot testing of the Function Focused Care Intervention on an acute care trauma unit. Geriatric Nursing. 2013;34(3):241–246. doi: 10.1016/j.gerinurse.2013.02.001. [DOI] [PubMed] [Google Scholar]
- Chandrasekaran S, Ariaretnam S, Tsung J, Dickison D. Early mobilization after total knee replacement reduces the incidence of deep venous thrombosis. ANZ Journal of Surgery. 2009;79:526–529. doi: 10.1111/j.1445-2197.2009.04982.x. [DOI] [PubMed] [Google Scholar]
- Charlson M, Pompei P, Ales K, MacKenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: Prognostic development and validation. Journal of Chronic Disease. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Clark D, Lowman J, Griffin R, Matthews H, Reiff D. Effectiveness of an early mobilization protocol in a trauma and burns intesive care unit: A retrospective cohort study. Physical Therapy. 2013;93(2):186–196. doi: 10.2522/ptj.20110417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming T, Thrift A, Collier J, Churilov L, Dewey H, Donnan G, Bernhardt J. Very early mobilization after stroke fast-tracks return to walking: Further results from the phase II AVERT randomized controlled trial. Stroke. 2011;42:153–158. doi: 10.1161/STROKEAHA.110.594598. [DOI] [PubMed] [Google Scholar]
- de Jonghe J, Kalisvaart K, Timmers J, Kat M, Jackson J. Delirium-O-Meter: A nurses’ rating scale for monitoring delirium severity in geriatric patients. International Journal of Geriatric Psychiatry. 2005;20:1158–1166. doi: 10.1002/gps.1410. [DOI] [PubMed] [Google Scholar]
- Doherty-King B, Yoon J, Pecanac K, Brown R, Mahoney J. Frequency and duration of nursing care related to older aptient mobility. Journal of Nursing Scholarship. 2014;46(1):20–27. doi: 10.1111/jnu.12047. [DOI] [PubMed] [Google Scholar]
- Fisher S, Galloway R, Kuo Y, Graham J, Ottenbacher K, Ostir G, Goodwin J. Pilot study examining the association between ambulatory activity and falls amonghospitalized older adults. Archives of Internal Medicine. 2011;92:2090–2092. doi: 10.1016/j.apmr.2011.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galik E, Resnick B, Hammersla M, Brightwater J. Optimizing function and physical activity among nursing home residents with dementia: Testing the impact of function focused care. The Gerontologist. 2014;54(6):930–943. doi: 10.1093/geront/gnt108. [DOI] [PubMed] [Google Scholar]
- Glasgow R, Green L, Taylor M, Stange K. An evidence integration traingle for aligning science with poliy and practice. American Journal of Preventive Medicine. 2012;42:646–654. doi: 10.1016/j.amepre.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregson J, Foerster S, Orr R, Jones L, Benedict J, Clarek B, Zotz K. System, environment and policy changes: Using the Social Ecological Model as a framework for evaluating nutrition eductaion and social marketing programs with low income audiences. Journal of Nutrition Education. 2003;33:S4–S15. doi: 10.1016/s1499-4046(06)60065-1. [DOI] [PubMed] [Google Scholar]
- Gruber-Baldini A, Resnick B, Galik E, Zimmerman S. Adverse events associated with safety of the Res-Care Intervention. Journal of the American Medical Directors Association. 2011;12(8):584–589. doi: 10.1016/j.jamda.2010.05.011. [DOI] [PubMed] [Google Scholar]
- Hao Y, Liu H, Yue S, Liu X. Introducing traditional Chinese nursing: A review of concepts, theories and practices. International Nursing Review. 2011;58:319–327. doi: 10.1111/j.1466-7657.2011.00918.x. [DOI] [PubMed] [Google Scholar]
- Herr K. Pain assessment strategies in older patients. Journal of Pain. 2011;12(3 Suppl 1):S3–S13. doi: 10.1016/j.jpain.2010.11.011. [DOI] [PubMed] [Google Scholar]
- Herr K, Spratt K, Mobily P, Richardson G. Pain intensity assessment in older adults: use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clinical Journal of Pain. 2004;20(4):207–219. doi: 10.1097/00002508-200407000-00002. [DOI] [PubMed] [Google Scholar]
- Jerofke T, Weiss M, Yakusheva O. Patient perceptions of patient-empowering nurse behaviors, patient activation, and functional health status in postsurgical patients with life-threatening long-term illnesses. Journal of Advanced Nursing. 2014;70(6):1310–1322. doi: 10.1111/jan.12286. [DOI] [PubMed] [Google Scholar]
- Jiang H, Li H, Ma L, Gu Y. Nurses' roles in direct nursing care delivery in China. Applied Nursing Research. 2015;28:132–136. doi: 10.1016/j.apnr.2014.09.003. [DOI] [PubMed] [Google Scholar]
- Kalish B, Lee S, Dabney B. Outcomes of inpatient mobiliation: A literature review. Journal of Clinical Nursing. 2013;23:1486–1501. doi: 10.1111/jocn.12315. [DOI] [PubMed] [Google Scholar]
- Kurabe S, Ozawa T, Watanabe T, Aiba T. Efficacy and safety of postoperative early mobilization for chronic subdural hematoma in elderly patients. Acta Neurochirurgica. 2010;52:1171–1174. doi: 10.1007/s00701-010-0627-4. [DOI] [PubMed] [Google Scholar]
- Lahmann N, Tannen A, Kuntz S, Raeder K, Schmitz G, Dassen T, Kottner J. Mobility is the key! Trends and associations of common care problems in German long-term care facilities from 2008 to 2012. International Journal of Nursing Studies. 2015;52(1):167–174. doi: 10.1016/j.ijnurstu.2014.07.014. [DOI] [PubMed] [Google Scholar]
- Langhorne P, Stott D, Knight A, Bernhardt J, Barer D, Watkins C. Very early rehabilitation or intensive telemetry after stroke: a pilot randomised trial. Cerebrovascular Disease. 2010;29:352–360. doi: 10.1159/000278931. [DOI] [PubMed] [Google Scholar]
- Leditschke A, Green M, Irvine J, Bissett B, Mitchell IA. What are the barriers to mobilizing intensive care patients? Cardiopulmonary Physical Therapy Journal. 2012;23(1):26–29. [PMC free article] [PubMed] [Google Scholar]
- Mahoney F, Barthel D. Functional evaluation: The Barthel Index. Maryland State Medical Journal. 1965;14(2):61–66. [PubMed] [Google Scholar]
- Maryland Institute of Emergency Medicine Services System. [Last accessed October, 2015];Interhospital Transfer Resource. 2014 Available at: http://www.miemss.org/home/Portals/0/Docs/Guidelines_Protocols/Interhospital_Transfer.pdf?ver=2015-07-27-114139-390.
- Meck J, Dreyer S, Warren L. Long duration head down bed rest: Project overview, vital signs and fluid balance. Aviation, Space and Environmental Medicine. 2009;80(5):A1–A8. doi: 10.3357/asem.br01.2009. [DOI] [PubMed] [Google Scholar]
- Nakao S, Takata S, Uemura H, Nakano S, Egawa H, Kawasaki Y, Yasui N. Early ambulation after total knee arthroplasty prevents patients with osteoarthritis and rheumatoid arthritis from developing postoperative higher levels of D-dimer. The Journal of Medical Investigation. 2010;57:146–151. doi: 10.2152/jmi.57.146. [DOI] [PubMed] [Google Scholar]
- NeSmith E, Medeiros R, Ferdinand C, Hawkins M, Holsten S, Zhu H, Dong Y. "It takes a village" to raise research productivity: Impact of a Trauma Interdisciplinary Group for Research at an urban Level 1 trauma center. Journal of Trauma and Acute Care Surgery. 2013;75(1):173–178. [PubMed] [Google Scholar]
- Nordon-Craft A, Moss M, Quan D, Schenkman M. Intensive care unit-acquired weakness: Implications for physical therapist management. Physical therapy. 2012;92(12):1494–1506. doi: 10.2522/ptj.20110117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen M, Bodilsen A, Petersen J, Beyer N, Andersen O, Lawson-Smith L, Bandholm T. Twenty-four hour mobility during acute hospitalization in older medical patients. Journals of Geronotlogy A Biological Sciences Medicine and Science. 2013;68(3):331–337. doi: 10.1093/gerona/gls165. [DOI] [PubMed] [Google Scholar]
- Platts S, Martin D, Stenger M, Perez S, Ribeiro L, Summers R, Meck J. Cardiovascular adaptations to long duration head down bed rest. Aviation, Space and Environmental Medicine. 2009;80(5, Section II):A29–A36. doi: 10.3357/asem.br03.2009. [DOI] [PubMed] [Google Scholar]
- Resnick B, Cayo J, Galik E, Pretzer-Baboff I. Implementation of the six-week educational component in the Res-Care Intervention: Process and outcomes. Journal of Continuing Education. 2009;40(8):353–360. doi: 10.3928/00220124-20090723-04. [DOI] [PubMed] [Google Scholar]
- Resnick B, Gruber-Baldini A, Galik E, Pretzer-Aboff I, Russ K, Hebel J, Zimmerman SI. Changing the philosophy of care in long-term care: Testing of the Restorative Care Intervention. The Gerontologist. 2009;49(2):175–184. doi: 10.1093/geront/gnp026. [DOI] [PubMed] [Google Scholar]
- Resnick B, Rogers V, Galik B, Gruber-Baldini A. Measuring restorative care provided by nursing assistants: Reliability and validity of the Restorative Care Behavior Checklist. Nursing Research. 2007;56(6):387–398. doi: 10.1097/01.NNR.0000299854.52429.ac. [DOI] [PubMed] [Google Scholar]
- Resnick B, Galik E. Reliability and validity testing of the Physical Activity Survey in Long Term Care (PAS-LTC) Journal of Aging and Physical Activity. 2007;15:439–458. doi: 10.1123/japa.15.4.439. [DOI] [PubMed] [Google Scholar]
- Resnick B, Galik E, Enders H, Sobol K, Hammersla M, Boltz M, Trotman S. Functional and physical activity of older adults in acute care settings: Where we are and where we need to go. Journal of Nursing Care Quality. 2011;26(2):169–177. doi: 10.1097/NCQ.0b013e3181eefd94. [DOI] [PubMed] [Google Scholar]
- Resnick B, Galik E, Vigne E. Translation of Function Focused Care to assisted living facilities. Family and Community Health. 2014;37(2):101–165. doi: 10.1097/FCH.0000000000000021. [DOI] [PubMed] [Google Scholar]
- Resnick B, Galik E, Wells C, Boltz M, Holtzman L. Optimizing physical activity among older adults post trauma: Overcoming system and patient challenges. International Journal of Orthopaedic and Trauma Nursing. In press doi: 10.1016/j.ijotn.2015.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B, Galik E, Dorsey S, Scheve A, Gutkin S. Reliability and validity testing of the Physical Resilience Measure. The Gerontologist. 2011;51(5):643–652. doi: 10.1093/geront/gnr016. [DOI] [PubMed] [Google Scholar]
- Rinaldi P, Mecocci P, Benedetti C, Ercolani S, Bregnocchi M, Menculini G, Cherubini A. Validation of the five-item geriatric depression scale in elderly subjects in three different settings. Journal of the American Geriatrics Society. 2003;51(5):694–698. doi: 10.1034/j.1600-0579.2003.00216.x. [DOI] [PubMed] [Google Scholar]
- Sainsbury A, Seebass G, Bansal A, Young JB. Reliability of the Barthel Index when used with Older People. Age and Aging. 2005;34:228–232. doi: 10.1093/ageing/afi063. [DOI] [PubMed] [Google Scholar]
- Scheffer A, Schuurmans M, Van Dijk N, Van der Hooft T, De Rooij S. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- Schweickert W, Pohlman M, Pohlman A, Nigos C, Pawlik A, Esbrook C, Kress J. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seiman I, Rozzini R, Barbisoni P, Morandi A, Ricci A, Giordano A, Trabucchi M. Functional trajectories during hospitalization: A prognostic sign for elderly patients. Journals of Gerontology Series A Biological Sciences Medicine and Science. 2009;64A:659–663. doi: 10.1093/gerona/glp015. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Lord S, Finch CF. Reliability of simple portable tests of physical performance in older people after hip fracture. Clinical Rehabilitation. 2005;19(5):496–504. doi: 10.1191/0269215505cr833oa. [DOI] [PubMed] [Google Scholar]
- Shever LL, Titler M, Dochterman J, Fei Q, Picone DM. Patterns of nursing intervention use across 6 days of acute care hospitalization for three older patient populations. International Journal of Nursing Terminologies & Classifications. 2007;18(1):18–29. doi: 10.1111/j.1744-618X.2007.00044.x. [DOI] [PubMed] [Google Scholar]
- So C, Pierluissi E. Attitudes and expectations regarding exercise n the hospital of hospitalized older adults: A qualitative study. Journal of the American Geriatrics Society. 2012;60:713–718. doi: 10.1111/j.1532-5415.2012.03900.x. [DOI] [PubMed] [Google Scholar]
- Stein T, Wade C. Metabolic consequences of muscle disuse atrophy. Journal of Nutrition. 2005;135(7):1824–1828. doi: 10.1093/jn/135.7.1824S. [DOI] [PubMed] [Google Scholar]
- Zisberg A, Sahadmi E, Gur-Yaish N, Tonkikh O, Sinoff G. Hosptial association functional decline: The role of hospitalization processes beyond individual risk factors. Journal of the American Geriatrics Society. 2015;63(1):55–62. doi: 10.1111/jgs.13193. [DOI] [PubMed] [Google Scholar]