Abstract
The SHIELD (Safety & Health Improvement: Enhancing Law Enforcement Departments) Study is a worksite wellness team-based intervention among police and sheriff departments assessing the program’s effectiveness to reduce occupational risks and unhealthy lifestyle behaviors. The SHIELD program focused on improving diet, physical activity, body weight and sleep and reducing the effects of unhealthy stress and behaviors such as tobacco and substance abuse. The SHIELD team-based health promotion program was found to be feasible and effective at 6 months in improving diet, sleep, stress, and overall quality of life of law enforcement department personnel. Both intervention and control groups were followed for 24 months, and we report those durability findings, along with qualitative group interview results that provide insight into the changes of the long term outcomes. Long term effects were observed for consumption of fruits and vegetables and there was some evidence for effects on tobacco and alcohol use. Assessment of dietary habits, physical activity behaviors, weight loss maintenance, and substance use is rare more than one year following an intervention, and in general, initial positive changes do not persist in prior research. The SHIELD program was feasible, effective, and durable for improving dietary changes.
Introduction
The National Institute of Occupational Safety and Health and the Affordable Care Act recognize that occupational wellness programs may be solutions to rising employee healthcare costs, while reducing absenteeism and improving productivity. (1, 2) Worksite wellness programs have the potential to reduce employee medical costs, however, a recent review found that few had documented effectiveness, and only a small number of the evidence-based programs were available for widespread use. (3) Even fewer programs have evidence for outcome durability. Assessment of dietary habits, physical activity behaviors, and weight loss maintenance is rare more than one year following an intervention, and in general, initial positive changes have not persisted in prior research. (4–12)
The SHIELD Study was funded by the Centers for Disease Control and Prevention and the National Institute for Occupational Safety and Health to evaluate the impact of a worksite wellness program to reduce the occupational health and safety risks associated with law enforcement work. The SHIELD program utilizes an evidence-based, peer-led, team-based format that has been effective with sports teams, fire fighters, and hospital and university employees (13–16) and we customized this approach for law enforcement officers and support personnel. It is well established that law enforcement work is associated with significant health and safety risks (17–19) with life expectancy between 6 and 15 years younger than the lifespan for an average American. (18, 20–21) The SHIELD program was tailored to address the occupational risk factors associated with law enforcement including high injury rates and early disability, high cardiovascular disease, increased mental stress and PTSD, sleep disorders, fatigue related motor vehicle accidents, poor dietary practices, and bad ergonomics with prolonged sitting among patrol officers and support staff. (22–26) We reported the trial’s 6-month findings, which demonstrated a positive impact from the SHIELD wellness program on nutrition, stress, sleep quality and quantity. (27) Both intervention and control groups were followed for an additional 18 months, and we report those findings, along with qualitative group interview results that provide insight into the changes that may underlie the long term outcomes.
Methods
Study population and recruitment
The study participants included law enforcement personnel from police and sheriff departments located in Oregon and Southwest Washington. One police department totalling 200 sworn and 35 civilian personnel, and two sheriff’s departments totalling 490 sworn officers and 203 civilian staff personnel were recruited. Of 928 eligible participants, 408 law enforcement officers and support staff consented for the study. The study was approved but the Oregon Health & Science University IRB in 2010.
Randomization
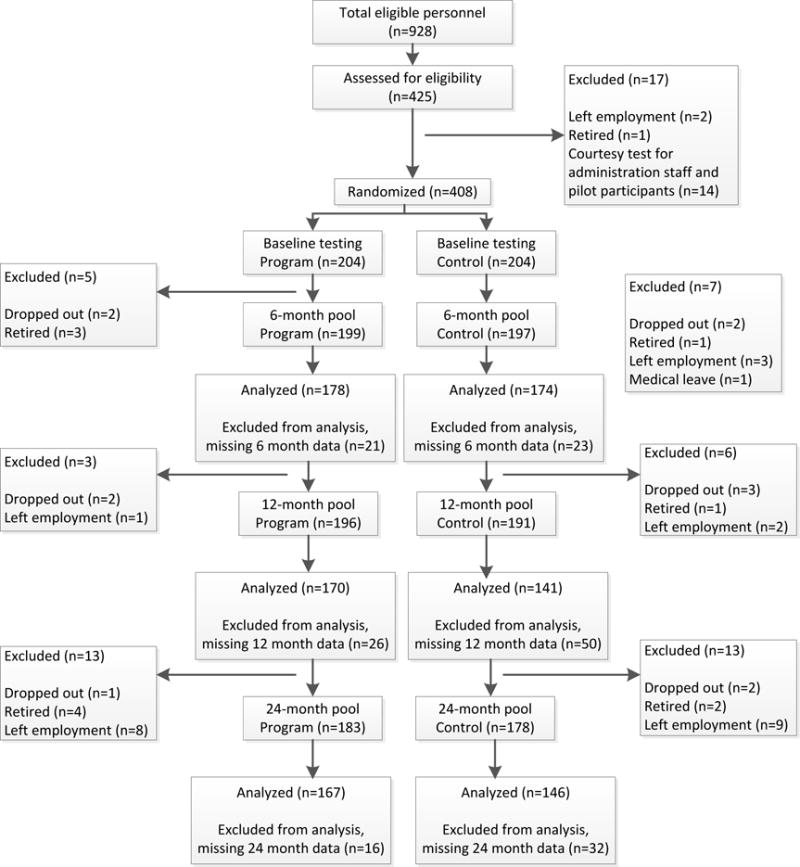
A complete detailed description of the study participants and randomization is included in the prior publication. (27) The intervention was delivered to individuals organized in naturally occurring teams of workers at each site organized based from the type of job duty and shift schedule (e.g., patrol officers on night shift, probation officers on days). These teams of 3–7 subjects were then organized into blocks which were then paired and used for matching in the randomization. There were a total of 86 teams with 21 matched pairs of blocks, which were then randomized by a computer automated system into treatment and control conditions. For all 408 participants from the three sites, the randomization scheme and waves of testing and follow up are presented in Figure 1 below.
Figure 1.
Measures
Study participants completed testing including written surveys at four points over the two year period: baseline, 6, 12 and 24 months. The validated survey was based on our previous studies (27, 28) and contained questions about demographics, gender, job type and shift schedule, number of years in law enforcement, diet, physical activity, sleep, fatigue, pain, stress, tobacco, alcohol and depression. More information on the scales can be obtained at the website, https://psychology.clas.asu.edu/research/labs/research-prevention-laboratory-mackinnon, and more detailed description of the study sites are included in the prior publication. (27)
As shown in Table 1, the intervention and control group did not have statistically significant differences on baseline variables with the exception of healthy eating. Intervention subjects rated themselves as healthier eaters than participants in the control group (p = 0.04).
Table 1.
Descriptive Demographic Variables (number or mean[sd])
| Baseline | 24-months | |||
|---|---|---|---|---|
| Variable | Control | Treatment | Control | Treatment |
| Age (years) | 41.7(9.4) | 44.6(9.5) | 43.1(8.6) | 45.9(9.3) |
| Gender | ||||
| Male | 141 | 118 | 127 | 104 |
| Female | 66 | 96 | 52 | 79 |
| Ethnicity | ||||
| White | 184 | 195 | 164 | 171 |
| Black/African Am. | 1 | 5 | 1 | 4 |
| Asian | 3 | 3 | 3 | 1 |
| Native Hawaiian/Other Pacific Islander | 4 | 1 | 4 | 1 |
| American Indian/Native Alaskan | 2 | 1 | 2 | 1 |
| Other | 8 | 7 | 4 | 5 |
| Marital Status | ||||
| Married | 137 | 161 | 102 | 120 |
| Divorced | 37 | 26 | 20 | 18 |
| Widowed | 1 | 8 | 1 | 6 |
| Separated | 1 | 3 | 2 | 4 |
| Never Married | 20 | 6 | 8 | 4 |
| Member of an Unmarried Couple | 8 | 8 | 1 | 5 |
| Time in Law Enforcement (years) | 13.56(7.66) | 15.23(9.00) | 14.83(7.36) | 16.39(8.76) |
Physical testing was conducted at baseline, 12 and 24 months. Physical measures included body weight and height, anthropometric measures, blood pressure, fasting lipid and lipoprotein and glucose levels (Cholestech PA Analyser from finger stick).
Qualitative data gathering
Group interviews were a convenience sample of intervention participants; each team was interviewed individually approximately 24-months after the intervention. Eleven 60-minute team interviews were held with a total of 38 law enforcement employees. Interviewers used a semi-structured guide, which outlined a series of open-ended questions in the domains of what they remembered most about the team session, along with potential promoters and hindrances to long-lasting health behaviour change relating to diet, exercise and sleep habits. Probative follow-up questions were included to expand on responses. The roadmap strategy allowed comparison of responses across groups. Because of the group setting, individual actions concerning alcohol use were not explored. These qualitative interviews were audiotaped, transcribed by a research assistant and then assembled for analysis.
Intervention Group
Participants randomized to the intervention participated in twelve, 30-minute, team-based, scripted, peer-led sessions during the first six study months. No additional intervention team meetings were held after that time. A detailed description of the intervention is published in the SHIELD 6 month study results publication. (27) The SHIELD program team meetings were scheduled once per week by the team leader and held during work hours. The team format fosters social support and accountability as one officer stated, “to help each other stay away from the donuts and take the stairs rather than the elevator”. Each member of the team would discuss weekly goals and there was a scripted set of questions to answer out loud regarding successful strategies identified by subjects to reach the weekly goal (e.g., achieving 10,000 steps per day on their pedometer, eating 5 servings of fruits and vegetables daily for the week, sleeping at least 7 hours each 24 hours for the week). There were a total of six hours of curriculum regarding these lifestyle goals in the SHIELD program and no other changes were made to the environment. It was up to the teams and participants to make the positive changes and achieve these lifestyle goals, or to change their unhealthy habits.
Control Group
Subjects that were randomized to the control condition still took the same battery of tests and surveys at the four intervals, baseline, 6, 12, and 24 months. At the baseline testing, participants in the control group received their test results and a physician discussed their confidential individual test results identifying abnormal values and discussing appropriate medical standards of care and follow up. There were a total of 24 individuals during the initial EKG exercise stress test that had a positive test and needed appropriate follow up with cardiology for treatment. They were not included in the study after that unless cleared by the cardiologist. There were no other health promotion programs or educational materials provided to control participants after the results discussion, however, the control group participants were expected to follow up on the recommendations of the physician.
Statistical Analysis
The statistical analyses reflect the nesting of individual persons within the 86 teams. The SAS Mixed program was used to estimate this multilevel regression model. Missing data at 6, 12, and 24 months were treated as missing at random including baseline data in the analyses. In this model for repeated measures, significant group by time interactions represented program effects, consistent with differential change over time in the program versus control conditions. The group by time interaction incorporated change between groups across all four time points. A primary contrast in this analysis was a test of whether the change between baseline and the average of the follow-ups differed between treatment and control groups. No adjustment for multiple comparisons were made. Additional contrasts compared group differences in change from baseline to each follow-up time.
Qualitative analysis
Thematic content analysis involved reiterative readings of interview transcripts to identify and code patterns and influences on the impact of the wellness program based on participants’ actual experiences. (29) The qualitative methodology as described by Mabry et al includes construction of themes and interpretations which avoids the substantive bias inherent in a priori categorization, and instead adapts the more inductive constant-comparative method typical of grounded theory. (30) As the data was reviewed several times by different research assistants to search for interpretations, emergent themes evolved. Preliminary findings were constructed to evaluate rival explanations, and organized thematically with participants actual phrasing. The “vicarious experiences” provided by the interview excerpts are intended to enhance understanding and the development of “tacit knowledge,” more influential than “propositional knowledge” for generalization to other occupational settings. (31, 32)
Results
Adherence to Format and Acceptability
There was good participation and adherence to the curriculum content and format with 97% of the scripted content delivered as written. Team members attended 87% of the “required sessions”.
Participants
Table 1 lists participant characteristics at baseline and at the end of the study.
Program Effects
Program effects were analysed in a series of multilevel models, including individuals nested within teams. Table 2 lists the estimates of program effects, adjusted means, effect sizes, and p-values for the test of baseline versus the average of the follow up outcome variables at 6, 12, and 24 months. The “All Follow-ups” column under effect size shows whether significant program effects were observed in the comparison of baseline to the average of the three follow-up measures thereby providing an overall test of the program effects across time points. The effect size was computed by taking the difference between baseline and the average of the follow-ups and then taking the difference of this difference between the intervention and control groups and standardizing using the pooled individual level standard deviation at baseline. (33) Statistically significant beneficial program effects were present for daily servings of fruit and vegetable intake, healthier eating, sleep quality and quantity (marginal), general health (marginal), stress, tobacco and heavy alcohol use (marginal). Table 2 also shows the adjusted means and program effects for 6, 12, and 24 months for the primary endpoints and distal physiological measures. The measure of effect was computed for each baseline versus follow-up comparison.
Table 2.
| Control Group | Intervention Group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Baseline | 6 month follow- up |
12 month follow- up |
24 month follow- up |
Baseline | 6 month follow- up |
12 month follow- up |
24 month follow- up |
|||||
|
| ||||||||||||
| Variables | Adjusted Mean |
Adjusted Mean |
Adjusted Mean |
Adjusted Mean |
Adjusted Mean |
Adjusted Mean |
Adjusted Mean |
Adjusted Mean |
6 Month Program Effect |
12 Month Program Effect |
24 Month Program Effect |
All Follow- ups |
| Fruit consumption | 2.175 | 2.095 | 2.142 | 2.079 | 2.050 | 3.055 | 2.760 | 2.755 | 0.49* | 0.34* | 0.36* | 0.40* |
|
| ||||||||||||
| Vegetable consumption | 3.674 | 3.550 | 3.241 | 3.740 | 3.554 | 4.413 | 4.147 | 3.923 | 0.29* | 0.31* | 0.09 | 0.23* |
|
| ||||||||||||
| Fruit/Vegetable consumption | 5.848 | 5.637 | 5.381 | 5.818 | 5.587 | 7.459 | 6.882 | 6.659 | 0.46* | 0.39* | 0.24* | 0.36* |
|
| ||||||||||||
| Healthy Eating Self | −0.082 | 0.117 | 0.089 | 0.074 | 0.085 | 0.4382 | 0.378 | 0.369 | 0.20* | 0.16* | 0.17* | 0.18* |
|
| ||||||||||||
| Physical Activity | −0.026 | 0.216 | 0.139 | 0.099 | 0.028 | 0.304 | 0.112 | 0.142 | 0.04 | −0.10 | −0.01 | −0.02 |
|
| ||||||||||||
| Sleep Quality | 0.004 | 0.015 | 0.074 | 0.057 | −0.011 | 0.287 | 0.143 | 0.201 | 0.32* | 0.09 | 0.18± | 0.20* |
|
| ||||||||||||
| Sleep Quantity | −0.030 | −0.005 | −0.015 | 0.038 | 0.032 | 0.250 | 0.140 | 0.137 | 0.23* | 0.11 | 0.04 | 0.13 |
|
| ||||||||||||
| SF36: General Health | 3.589 | 3.420 | 3.395 | 3.385 | 3.551 | 3.488 | 3.437 | 3.381 | 0.15* | 0.11 | 0.05 | 0.10 |
|
| ||||||||||||
| Stress Self | 4.052 | 4.050 | 4.066 | 4.033 | 4.119 | 4.331 | 4.336 | 4.187 | 0.16* | 0.16 | 0.07 | 0.13* |
|
| ||||||||||||
| Tobacco Use | 3.521 | 3.515 | 3.576 | 3.501 | 3.291 | 3.389 | 3.405 | 3.389 | 0.10* | 0.06 | 0.12* | 0.09* |
|
| ||||||||||||
| Alcohol Consumption | −0.016 | −0.024 | −0.032 | −0.021 | 0.025 | 0.080 | 0.117 | 0.105 | 0.09 | 0.16* | 0.12± | 0.12± |
|
| ||||||||||||
| Depression | 5.228 | 5.111 | 5.208 | 5.085 | 5.371 | 5.406 | 5.386 | 5.273 | 0.13 | 0.03 | 0.04 | 0.06 |
|
| ||||||||||||
| Systolic Blood Pressure±AG | 123.94 | N/A | 120.52 | 119.83 | 125.26 | N/A | 119.48 | 120.04 | N/A | −0.18* | −0.08 | −0.13± |
|
| ||||||||||||
| Diastolic Blood PressureAG | 77.52 | N/A | 75.72 | 75.58 | 78.36 | N/A | 76.07 | 75.82 | N/A | −0.05 | −0.06 | −0.05 |
|
| ||||||||||||
| BMI | 30.31 | NA | 30.30 | 30.50 | 29.21 | NA | 29.37 | 29.47 | NA | 0.03 | 0.01 | 0.02 |
Indicates statistically significant program effect of group by time. p < 0.05.
Indicates marginally significant program effect of group by time. p < 0.10.
Indicates statistically significant effect of covariate Age on physical outcome.
Indicates statistically significant effect of covariate Gender on physical outcome.
Note. Tobacco Use and Alcohol Consumption were not normally distributed variables so percentile bootstrap confidence intervals were also computed to test the significance of the effects at each wave. The significance of the effects at each wave based on the percentile bootstrap matched the results presented in this table.
Note. Effects of the Age and Gender covariates on the scale outcomes did not affect the significance of program effects and therefore were not included in this table.
Fruit and vegetable consumption were significantly improved for the intervention group at all follow-up time points (Figure 2). The effect size for fruit and or vegetable consumption ranges from 0.09 to 0.49, with fruit consumption consistently showing greater effect sizes. The construct measuring healthy eating also showed statistically significant program effects at each follow up point, with effect sizes ranging from 0.16 to 0.20.
Figure 2.
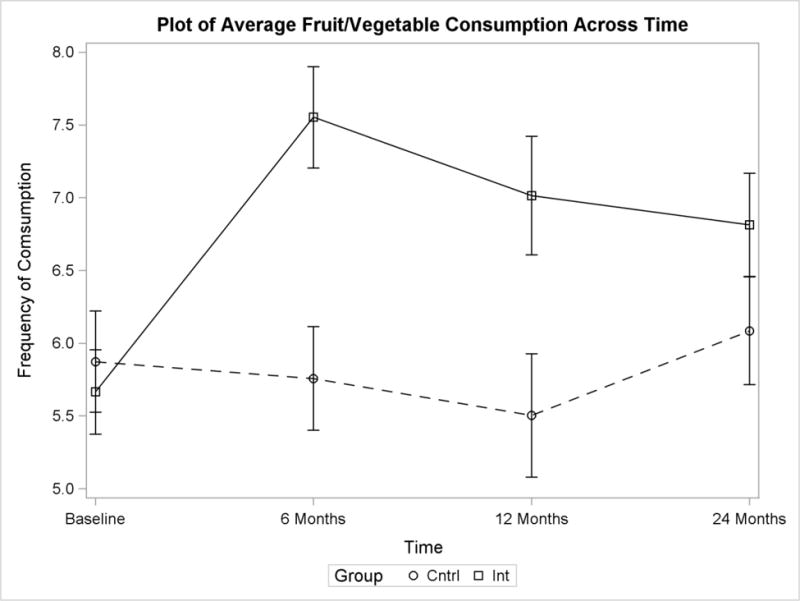
Average fruit/vegetable consumption for the intervention and control groups at each time of measurement +/− 1 standard error bars. Higher scores indicate higher consumption of fruits and vegetables.
Statistically significant program effects for sleep, stress and general health variables were observed at 6 month follow-up but not at the 12 and 24 month follow-ups. Similar patterns of change were observed for sleep quality, sleep quantity and amount of sleep, though not as pronounced as for fruit and vegetable intake (see a plot for the sleep variable found at the website https://psychology.clas.asu.edu/research/labs/research-prevention-laboratory-mackinnon).
Statistically significant program effects were observed for tobacco use at 6 months and 24 months and significant reduction of alcohol use at 12 months and a marginally significant reduction of alcohol use at 24 month follow up among the intervention group with effect sizes ranging from 0.09 to 0.16 for all effects on tobacco and alcohol.
Qualitative Findings
Fourteen males and 24 females participated in the group interviews, (mean age 44 years). Three major themes were observed and a matrix of evolving and refined themes and representative quotes were documented. The list of quotes can be found at the website, https://psychology.clas.asu.edu/research/labs/research-prevention-laboratory-mackinnon. In general, law enforcement personnel learned about the benefits of healthy nutrition, physical activity, adequate sleep quality and quantity, stress management, and reducing tobacco and heavy alcohol use. Although much could be recalled from the session and individuals made changes, the motivation for change appeared to remain external. Other than visible changes in eating habits, few personal or cultural changes assisted maintaining healthy action, and competing priorities and altered circumstances further constrained durability.
Discussion
Policing is a 24 hour occupation requiring shift work and multiple overtime schedules to keep our communities safe contributing to the high adverse health consequences observed among these workers. The SHIELD program was found to be feasible and in the short-term, effective in promoting the health of law enforcement officers and support personnel. Long term effects persisted and were observed for consumption of fruits and vegetables, healthier eating, and tobacco and heavy alcohol use reduction. The team program was well received with a high attendance and adherence to the scripted curriculum. After the 12 week intervention, significant positive changes occurred related to diet, sleep, stress, and tobacco and alcohol reduction use. (27) However, only increased fruit and vegetable consumption, healthy eating, and tobacco and heavy alcohol use reduction persisted 24 months after the intervention.
Fruits and Vegetables
Evidence suggests diets that a daily intake of 5 servings of fruits and vegetables per day are associated with a lower risk of disease including certain types of cancer, diabetes, and cardiovascular disease (CVD). (34, 35) A recent systematic review of worksite dietary interventions found increases in fruit and vegetable intake comparable to our findings (36) although comparisons are limited due to the variability in instruments and how change was reported. Similar to published results from our other team-based wellness programs (13–16) significant changes in diet were observed and durable at 24 months after intervention including increased daily servings of fruit and vegetables, and making healthier food choices. This may have substantial benefit to law enforcement personnel whose poor dietary habits increase risk of developing CVD, diabetes, high blood pressure, obesity, and metabolic syndrome. (23, 25, 26–27) The SHIELD occupational wellness program focuses on both nutrition education and behaviour change strategies on how to make better dietary decisions and choices. The curriculum targets specific dietary lifestyle habits with daily and weekly goals that encourage law enforcement officers and support staff on healthy nutrition alternatives both at work, when on patrol, or on break, when eating out, and at home. These activities included how to replace unhealthy fast food with healthy alternatives, how to shop and cook healthy on a budget, how to reduce calories in snacks, and addressed the industry of dietary supplements teaching them what is helpful or harmful. The durability of these healthy dietary changes persisting at 24 months suggest the 12 week, 30 minute once per week team-based SHIELD intervention program created a healthier culture at work.
Tobacco and Alcohol Use
Smoking causes 467,000 deaths per year from cardiovascular disease, cancer, and respiratory disease making it the number one preventable cause of death in the United States. (1) Tobacco use involving cigarette smoking is estimated at 19 percent in the U.S. and varies in law enforcement personnel from 6 to 32 percent (21, 23) with 16.7 percent of Buffalo police officers currently identified as smokers (26). Interestingly, the percentage of current smokers in the Buffalo Cardio-Metabolic Occupational Police Stress (BCOPS) study was twice as high for women at 26% than for men at 13% (18). The BCOPS study, however, involves a group of subjects that have been extensively sampled and understand that results may be biased from this over-studied population. In our current study, the SHIELD team curriculum focused on tobacco use cessation and results did show a statistically significant reduction for tobacco use at 6 months and 24 months post intervention. Likewise, heavy alcohol use among law enforcement personnel is a problem and has been linked to occupational stress and post-traumatic stress disorder (PTSD), certain cancers, and suicide. Violante and colleagues observed a ten-fold increased risk for suicide ideation among Buffalo police officers with PTSD and increased alcohol use. (22) Additionally, police officers have a high incidence of sleep disorders and alcohol is known to disrupt circadian rhythm and increase sleep disruption. (23) Our intervention focused on the harm of heavy alcohol use and alternatives to use and had an observed reduction of alcohol use at 12 months and a marginally significant reduction of alcohol use at 24 month follow up demonstrating the intervention was both feasible and able to affect a major risk factor for the epidemic of suicide and PTSD observed among law enforcement officers.
Mood, Stress, and Sleep
Law enforcement officers have a high prevalence of sleep and stress related disorders associated with adverse health outcomes including premature disability, high substance abuse, suicide, and high healthcare costs. (21–23, 25) An effective worksite wellness program needs to focus on the negative impact of sleep deprivation and mental and emotional stress and effective strategies to mitigate these occupational hazards of law enforcement work. Sleep disorders compounded with the mental and physical stress associated with law enforcement work can lead to fatigue, depression, and suicide ideation. (22,25,37,38). Depression alone is a major contributor of employee absenteeism and reduced productivity. A program that can reduce stress and depression will have a significant impact high employer healthcare costs.(39) Additionally, the negative impact of shift work among police officers, especially night shift work is associated with obesity, metabolic syndrome and diabetes (22, 25, 40–43) and increases employee benefit healthcare costs substantially. (44–46) There are few occupational wellness programs that have shown effectiveness to improve sleep (47,48), and the SHIELD program did improve sleep quality and quantity as well as reduce personal stress at 6 months. (27) These positive changes in sleep and stress in the short term, however, did not persist at 24 months. It may be that the sleep and stress improvements observed from the SHIELD wellness program in the short term are not as easily reinforced as the other behaviors like diet (since peer workers see what each other eat but not likely to know about sleep habits). A booster session on sleep and stress may be needed to continue the positive impact of the program.
Teams and social support
A major factor in the SHIELD program’s significant impact on behaviour change both in the short term and the longer term is the team-based aspect and social support of the program. It has been reported that social support from co-workers has positive influences on well-being and absenteeism. (49) Positive peer influence, which is the observance of seeing another person making positive changes, can impact others to pursue the same goal. This is the positive impact of a team when individuals on the team strive for a bigger goal, and help each other achieve the goal. In our previous PHLAME study, positive changes persisted for years after the intervention and appeared to diffuse, postulating a point where culture change occurred and became the norm. (15, 28, 30) There were beneficial individual changes that occurred, but when performed and incorporated in a team setting, it coalesced into group effects. We observed the same durability effect for long term healthy dietary change and tobacco and heavy alcohol use among our law enforcement personnel who participated in the 30 minute, once per week for 12 week SHIELD program.
Single Focus versus Multiple Intervention Targets
Another factor that may contribute to the longer term durability observed in this study is that our program targets multiple behaviors instead of just one behavior. The SHIELD program has seven main behavioral goals associated with the curriculum including daily healthy exercise and nutrition, achieving optimal body weight, reducing stress, improved sleep, reduced heavy alcohol use, and tobacco cessation. Interventions that focus on multiple behaviors may have a synergistic effect to make a bigger impact than if the intervention targets just one behavior. (50,51) The Synergy Hypothesis posits that goals are organized in associative cognitive networks (52) where an overarching goal, such as improved health, has sub goals, e.g., more physical activity and eating more fruits and vegetables, so that pursuing a sub goal can spread activation and reinforce the overriding goal. Additionally, focusing on multiple behaviors sequentially at various time points is associated with less cognitive effort, and the SHIELD program behavioral goals were delivered in sequence. Because behavior change is an effortful process, the sequential approach that was used in the SHIELD program enables these behaviors to become automatic habits that lack substantial drain on self-regulatory resources.
Qualitative findings
Qualitative interviews revealed explanatory factors relating to the observed differential durability of positive behavioral outcomes. Findings suggest the interventions’ specific and memorable information was comparable in its retention by participants. However, the ability for sustained reinforcement of the momentum achieved varied based on the behaviors modeling, encouragement and norms. For eating behaviors, that reinforcement appeared to sustain change. To sustain less visible and less social behaviors, such as sleep and stress coping strategies, which occur outside of work and not shared by teammates, specific means such as environmental cues, self-monitoring and booster content may be needed for maintenance.
Conclusions
It is well established that work in law enforcement is associated with significant occupational health and safety risks that impact premature morbidity and early mortality. There is not a cost effective, evidence-based worksite wellness program for law enforcement personnel despite these elevated risks of premature cardiovascular disease, certain cancers, high mental and emotional stress, metabolic syndrome, diabetes, and musculoskeletal injuries. This randomized prospective trial assessed the efficacy and durability of a team-based worksite wellness program among law enforcement officers and support staff. The SHIELD program is a peer-led, scripted, team-based health promotion program delivered once per week for 30 minutes for 12 weeks. Health and safety questionnaires administered before and after the intervention found significant improvements for increased fruit and vegetable consumption, overall healthy eating, increased sleep quantity and sleep quality, reduced personal stress, and reductions in tobacco and alcohol use at 6 months post intervention. Long term significant improvements persisted for increased fruit and vegetable consumption and reductions in tobacco and alcohol use at 24 months after the intervention. Although many studies have demonstrated the health and safety hazards associated with work in law enforcement, this study shows that a health promotion program tailored to these risks and conducted at police and sheriff departments during the work shift could counter the adverse health effects associated with this occupation.
Acknowledgments
Funding: This research was supported by a grant from the Centers for Disease Control and the National Institute on Occupational Safety and Health [5R01OH009676-02].
Footnotes
Conflict of Interest Disclosures: The PHLAME firefighter program is distributed through the Center for Health Promotion Research at Oregon Health & Science University (OHSU). OHSU and Drs. Kuehl, Elliot, and Goldberg have a financial interest from the commercial sale of technologies used in this research. This potential conflict of interest has been reviewed and managed by the OHSU Conflict of Interest in Research Committee.
References
- 1.Comprehensive Workplace Health Programs to Address Physical Activity, Nutrition, and Tobacco Use in the Workplace. 2013 Available from: http://www.cdc.gov/workplacehealthpromotion/nhwp/
- 2.Hymel PA, Loeppke RR, Baase CM, Burton WN, Hartenbaum NP, Hudson TW, et al. Workplace health protection and promotion: A new pathway for a healthier-and safer-workforce. J Occup Environ Med. 2011;53(6):695–702. doi: 10.1097/JOM.0b013e31822005d0. [DOI] [PubMed] [Google Scholar]
- 3.Kent Anger W, Elliot DL, Bodner T, Olson R, Rohlman DS, Truxillo DM, et al. Effectiveness of total worker health interventions. J Occup Health Psychol. 2015;20(2):226–47. doi: 10.1037/a0038340. [DOI] [PubMed] [Google Scholar]
- 4.Ory MG, Smith ML, Mier N, Wernicke MM. The science of sustaining health behavior change: The health maintenance consortium. Am J Health Behav. 2010;34(6):647–59. doi: 10.5993/ajhb.34.6.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 6.Madden SG, Loeb SJ, Smith CA. An integrative literature review of lifestyle interventions for the prevention of type II diabetes mellitus. J Clin Nurs. 2008;17(17):2243–56. doi: 10.1111/j.1365-2702.2008.02335.x. [DOI] [PubMed] [Google Scholar]
- 7.Müller-Riemenschneider F, Reinhold T, Nocon M, Willich SN. Long-term effectiveness of interventions promoting physical activity: A systematic review. Prev Med. 2008;47(4):354–68. doi: 10.1016/j.ypmed.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Brunner EJ, Rees K, Ward K, Burke M, Thorogood M. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev. 2007;(4) doi: 10.1002/14651858.CD002128.pub3. [DOI] [PubMed] [Google Scholar]
- 9.Hillsdon M, Foster C, Thorogood M. Interventions for promoting physical activity. Cochrane Database Syst Rev. 2005;(1) doi: 10.1002/14651858.CD003180.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toobert DJ, Strycker LA, Barrera M, Glasgow RE. Seven-year follow-up of a multiple-health-behavior diabetes intervention. Am J Health Behav. 2010;34(6):680–94. doi: 10.5993/ajhb.34.6.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Osilla KC, Van Busum K, Schnyer C, Larkin JW, Eibner C, Mattke S. Systematic review of the impact of worksite wellness programs. Am J Managed Care. 2012;18(2):e68–81. [PubMed] [Google Scholar]
- 12.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. New Engl J Med. 2006;355(15):1563–71. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg L, MacKinnon DP, Elliot DL, Moe EL, Clarke G, Cheong JW. The adolescents training and learning to avoid steroids program: Preventing drug use and promoting health behaviors. Arch Pediatr Adolesc Med. 2000;154(4):332–8. doi: 10.1001/archpedi.154.4.332. [DOI] [PubMed] [Google Scholar]
- 14.Elliot DL, Goldberg L, Moe EL, DeFrancesco CA, Durham MB, Hix-Small H. Preventing substance use and disordered eating: Initial outcomes of the ATHENA (Athletes Targeting Healthy Exercise and Nutrition Alternatives) program. Arch Pediatr Adolesc Med. 2004;158(11):1043–9. doi: 10.1001/archpedi.158.11.1043. [DOI] [PubMed] [Google Scholar]
- 15.Elliot DL, Goldberg L, Kuehl KS, Moe EL, Breger RKR, Pickering MA. The PHLAME (Promoting Healthy Lifestyles: Alternative Models’ Effects) firefighter study: Outcomes of two models of behavior change. J Occup Environ Med. 2007;49(2):204–13. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg L, Lockwood C, Garg B, Kuehl KS, Healthy Team Healthy U A Prospective Validation of an Evidence-Based Worksite health Promotion and Wellness Platform. Frontiers in Pub Health. 2015;(3):188. doi: 10.3389/fpubh.2015.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hessl SM. Introduction to the history, demographics, and health effects of law enforcement work. Clin Occup Environ Med. 2003;3(3):369–84. [Google Scholar]
- 18.Violanti JM, Fekedulegn D, Hartley TA, Andrew ME, Gu JK, Burchfiel CM. Life expectancy in police officers: a comparison with the U.S. general population. Int J Emerg Ment Health. 2013;15(4):217–28. [PMC free article] [PubMed] [Google Scholar]
- 19.Gyi DE, Porter JM. Musculoskeletal problems and driving in police officers. Occup Med (Oxf) 1998 Apr;48(3):153–60. doi: 10.1093/occmed/48.3.153. [DOI] [PubMed] [Google Scholar]
- 20.Richmond RL, Wodak A, Kehoe L, Heather N. How healthy are the police? A survey of life-style factors. Addiction. 1998 Nov;93(11):1729–37. doi: 10.1046/j.1360-0443.1998.9311172910.x. [DOI] [PubMed] [Google Scholar]
- 21.Franke WD, Ramey SL, Shelley MC., II Relationship between cardiovascular disease morbidity, risk factors, and stress in a law enforcement cohort. J Occup Environ Med. 2002;44(12):1182–9. doi: 10.1097/00043764-200212000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Violanti JM, Charles LE, Hartley TA, Mnatsakanova A, Andrew ME, Fekedulegn D, et al. Shift-work and suicide ideation among police officers. Am J Ind Med. 2008;51(10):758–6. doi: 10.1002/ajim.20629. [DOI] [PubMed] [Google Scholar]
- 23.Violanti JM, Burchfiel CM, Hartley TA, Mnatsakanova A, Fekedulegn D, Andrew ME, et al. Atypical work hours and metabolic syndrome among police officers. Archiv Environ Occup Health. 2009;64(3):194–201. doi: 10.1080/19338240903241259. [DOI] [PubMed] [Google Scholar]
- 24.Obst PL, Davey JD. Does the Police Academy change your life? A longitudinal study of changes in socialising behaviour of police recruits. International Journal of Police Science and Management. 2003;5(1):31–40. [Google Scholar]
- 25.Rajaratnam SMW, Barger LK, Lockley SW, Shea SA, Wang W, Landrigan CP, et al. Sleep disorders, health, and safety in police officers. J Am Med Assoc. 2011;306(23):2567–78. doi: 10.1001/jama.2011.1851. [DOI] [PubMed] [Google Scholar]
- 26.Violanti JM, Burchfiel CM, Miller DB, Andrew ME, Dorn J, Wactawski-Wende J, et al. The Buffalo Cardio-Metabolic Occupational Police Stress (BCOPS) pilot study: Methods and participant characteristics. Ann Epidemiol. 2006;16(2):148–56. doi: 10.1016/j.annepidem.2005.07.054. [DOI] [PubMed] [Google Scholar]
- 27.Kuehl K, Elliot D, G L, MacKinnon D, Vila B, Defrancesco C, et al. The safety and health improvement: enhancing law enforcement departments study: feasibility and findings. Frontiers Pub Health Educ Prom. 2014;2(38):1–5. doi: 10.3389/fpubh.2014.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elliot DL, Goldberg L, Kuehl KS, Moe EL, Breger RK, Pickering MA. The PHLAME (Promoting Healthy Lifestyles: Alternative Models’ Effects) firefighter study: outcomes of two models of behavior change. Journal of Occupational & Environmental Medicine. 2007 Feb;49(2):204–13. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]
- 29.Bamberger M, Rugh J, Mabry L. Conducting evaluation in the real world: Overcoming budget, time, and data constraints. 2nd. Newbury Park, CA: Sage; 2011. Qualitative Evaluation Methods; pp. 289–318. [Google Scholar]
- 30.Mabry L, Elliot DL, MacKinnon DP, Thoemmes F, Kuehl KS. Understanding the durability of a fire department wellness program. Am J Health Behav. 2013;37(5):693–702. doi: 10.5993/AJHB.37.5.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Strauss A, C J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 32.Carter K, Delamont S. Qualitative Research: The Emotional Dimension. Vermont: Avebury: Jun, 1996. [Google Scholar]
- 33.Morris SB. Estimating effect sizes from pre-test-posttest control group designs. Organizational Research Methods. 11(2):364–386. [Google Scholar]
- 34.Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ (Online) 2014:349. doi: 10.1136/bmj.g4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hung H, Joshipura KJ, Jiang R, Hu FB, Hunter D, Smith-Warner SA, et al. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004;96(21):1577–84. doi: 10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- 36.Ni Mhurchu C, Aston LM, Jebb SA. Effects of worksite health promotion interventions on employee diets: a systematic review. BMC Public Health. 2010;10:62. doi: 10.1186/1471-2458-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kalia M. Assessing the economic impact of stress – The modern day hidden epidemic. Metab Clin Exp. 2002;51(6 SUPPL. 1):49–53. doi: 10.1053/meta.2002.33193. [DOI] [PubMed] [Google Scholar]
- 38.Callen BL, Lindley LC, Niederhauser VP. Health risk factors associated with presenteeism in the workplace. J Occup Environ Med. 2013;55(11):1312–7. doi: 10.1097/JOM.0b013e3182a200f4. [DOI] [PubMed] [Google Scholar]
- 39.Goldberg RJ, Steury S. Depression in the workplace: Costs and barriers to treatment. Psychiatr Serv. 2001;52(12):1639–43. doi: 10.1176/appi.ps.52.12.1639. [DOI] [PubMed] [Google Scholar]
- 40.Chaput J, Després J, Bouchard C, Tremblay A. The association between short sleep duration and weight gain is dependent on disinhibited eating behavior in adults. Sleep. 2011;34(10):1291–7. doi: 10.5665/SLEEP.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep Med. 2014;15(12):1456–62. doi: 10.1016/j.sleep.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 42.Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30(12):1667–73. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolk R, Somers VK. Sleep and the metabolic syndrome. Exp Physiol. 2007;92(1):67–78. doi: 10.1113/expphysiol.2006.033787. [DOI] [PubMed] [Google Scholar]
- 44.Rosekind MR, Gregory KB, Mallis MM, Brandt SL, Seal B, Lerner D. The cost of poor sleep: Workplace productivity loss and associated costs. J Occup Environ Med. 2010;52(1):91–8. doi: 10.1097/JOM.0b013e3181c78c30. [DOI] [PubMed] [Google Scholar]
- 45.Swanson LM, Arnedt JT, Rosekind MR, Belenky G, Balkin TJ, Drake C. Sleep disorders and work performance: Findings from the 2008 National Sleep Foundation Sleep in America poll. J Sleep Res. 2011;20(3):487–94. doi: 10.1111/j.1365-2869.2010.00890.x. [DOI] [PubMed] [Google Scholar]
- 46.Thorndike FP, Ritterband LM, Gonder-Frederick LA, Lord HR, Ingersoll KS, Morin CM. A randomized controlled trial of an internet intervention for adults with insomnia: Effects on comorbid psychological and fatigue symptoms. J Clin Psychol. 2013;69(10):1078–93. doi: 10.1002/jclp.22032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Atlantis E, Chow C, Kirby A, Singh MAF. Worksite intervention effects on sleep quality: A randomized controlled trial. J Occup Health Psychol. 2006;11(4):291–304. doi: 10.1037/1076-8998.11.4.291. [DOI] [PubMed] [Google Scholar]
- 48.Steffen MW, Hazelton AC, Moore WR, Jenkins SM, Clark MM, Hagen PT. Improving sleep: Outcomes from a worksite healthy sleep program. J Occup Environ Med. 2015;57(1):1–5. doi: 10.1097/JOM.0000000000000370. [DOI] [PubMed] [Google Scholar]
- 49.Shirey MR. Social support in the workplace: nurse leader implications. Nurs Econ. 2004;22(6):313, 319, 291. [PubMed] [Google Scholar]
- 50.Atkins D, Clancy C. Multiple risk factor interventions – are we up to the challenge? American Journal of Preventive Medicine. 2004;27:102–3. doi: 10.1016/j.amepre.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 51.Kremers SPJ, De Brujn GL, Schaalma H, Brug J. Clustering of enrgy-balance related behaviors and their intrapersonal determinants. Psychology & Health. 2004;19(5):595–606. [Google Scholar]
- 52.Anderson JR, Bothell D, Byrne MD, Douglass S, Lebiere C, Qin Y. An integrated theory of the mind. Psychol Rev. 2004;111(4):1036–60. doi: 10.1037/0033-295X.111.4.1036. [DOI] [PubMed] [Google Scholar]


