Abstract
Objective:
To study the prevalence of anterior dental trauma and its associated factors among 800 preschool children aged 3 to 5 years in Jaipur City, Rajasthan, India.
Materials and Methods:
A cross-sectional survey was conducted among children aged 3-5 years, who were enrolled in various private and public schools in Jaipur. Parents were asked to fill a form addressing socio-demographic data and clinical examinations were performed by a single dentist. Traumatic dental injuries (TDI) were assessed and recorded based on Andreasen's classification. Associated factors such as sex, socioeconomic status (SES), and the type of injury were also analyzed. The data were analyzed statistically using Statistical Package for the Social Sciences software (version 20).
Results:
An overall 10.2% prevalence of TDI was observed among the study population. TDI were reported to be more among male children (11.87%) compared to female children (8.14%). Enamel fractures (69%) were the most prevalent type of anterior dental trauma. Upper central incisors were the most frequently affected. The SES of the parents had little influence on the prevalence of TDI.
Conclusions:
The prevalence rate of dental trauma among children aged 3-5 years was 10.2%. Associated factors, such as SES, were observed to be not significantly correlated to dental trauma among the studied preschoolers.
Keywords: Preschool children, socio-economic status, traumatic dental injury
INTRODUCTION
Traumatic dental injuries (TDI) are the most overlooked oral conditions regardless of their high prevalence rate and associated impact on children.[1] Dental trauma in addition to causing pain and loss of function has the potential for periapical sequelae, which can adversely affect the development of the permanent teeth as well as the developing occlusion.[2,3] Epidemiological data showed a wide variation in the prevalence of dental injuries in children.[4,5,6,7] Dental injuries to the deciduous teeth can result in problems to the underlying permanent teeth, such as hypoplasia, discoloration, and delay in eruption time, and tooth malformation.[8] Along with pain and possible infection, the consequence of dental trauma includes alteration in physical appearance, speech defects, and emotional impacts; thus, affecting the child's quality of life.[9,10,11]
Risks and severity to dental trauma vary according to the age, sex, and location of the tooth in the oral cavity.[12,13] A review of literature has shown that a higher degree of prevalence among anterior dental trauma exists compared to posterior teeth.[12] Preschool children are more prone to TDI due to their poor stability, passive reflexes and indefinite movements.[11,14,15]
A correlation between low socio-economic status and high prevalence of dental trauma have been emphasized.[11,16] Reports also highlighted that children of parents with low educational level tend to have increased rate of dental trauma.[17] However, the clarification on impact of socio-economic status of the parents or their educational level are still under investigation.[11,18]
Parents and home environment have a significant impact on the perception and attitude towards oral health among young children.[19] Delaying the treatment of the dental injuries in children are common in many countries.[20,21,22,23] This can be attributed to various factors such as short-lived primary dentition, memory bias, and lack of required attention because the child might not show any associated sign or symptom. Other determinants such as high cost, low standard of living and lack of knowledge also play a vital role.[11]
Only a few studies have been conducted in India on the prevalence of TDI among preschool children.[6,24,25] Shekhar and Mohan[25] reported a prevalence of 6.2% of injuries among deciduous anterior teeth in a sample of 1,126 preschool children in Chennai. A study from Gulbarga city reported a prevalence of 76.13% deciduous teeth injury among 4-6-year-old children.[6] Another study involving preschool as well as school children between the age of 3-16 years reported a prevalence of 5.29% of incisors and canine fractures.[24]
Jaipur city, the capital of the state of Rajasthan, is located in the north-western side of India, and is home to diverse culture and population belonging to different socio-economic status.[26] There is scarcity of epidemiological data on the prevalence of dental trauma among preschoolers in this region and the factors associated with it. Thus, due to limitations of the prevailing data, the present study was conducted to assess the prevalence of anterior dental trauma in primary dentition among 3-5-year-old children in Jaipur city, India, and its associated factors such as the socioeconomic status (SES) of their parents.
MATERIALS AND METHODS
The study was conducted in 800 preschool children aged 3 to 5 years residing in Jaipur city, India during June 2014 to September 2014. The study was approved by the institutional review board. The sample size was calculated using the Epi-Info 6.0 software program (CDC, 1600 Clifton Rd, Atlanta, GA 30333). It was estimated that a minimum sample size of 625 children was required to achieve a level of precision with a standard error of 4% or less. The 95% confidence interval level and a prevalence of dental trauma of 50% were used for the calculation. To compensate for the possible losses during the survey of data, the sample size was increased, resulting in a final sample of 800 children.
Parents were asked to fill out a form addressing socio-demographic data that included their education level and SES. Children with debilitating systemic disease, missing incisors due to caries or physiological exfoliation, and who failed to return the consent forms and completed questionnaires were excluded from the study.
Clinical examination was performed by a single dentist with a specialization in Pediatric Dentistry. Children were examined on a dental chair using mouth mirror under normal sunlight. Dental examination comprised only the primary maxillary and mandibular teeth. The anterior dental trauma was assessed by the method used by Andreasen et al.[27] consisting of the visual assessment of tooth discoloration and dislocation of teeth [Table 1]. Root fracture was not recorded and no radiographs were obtained. The SES of the family was calculated using Modified Kuppuswamy Scale for SES of an Indian population, which includes occupation, education level, and income of the parents to arrive at an SES score.[28] The data were then subjected to simple descriptive analysis and the statistical analysis was performed with Statistical Package for the Social Sciences version 20 (SPSS, IBM SPSS Inc, Chicago, IL). Chi-square test was employed to compare qualitative data and determine the statistical significance. The level of statistical significance was set at P < 0.05.
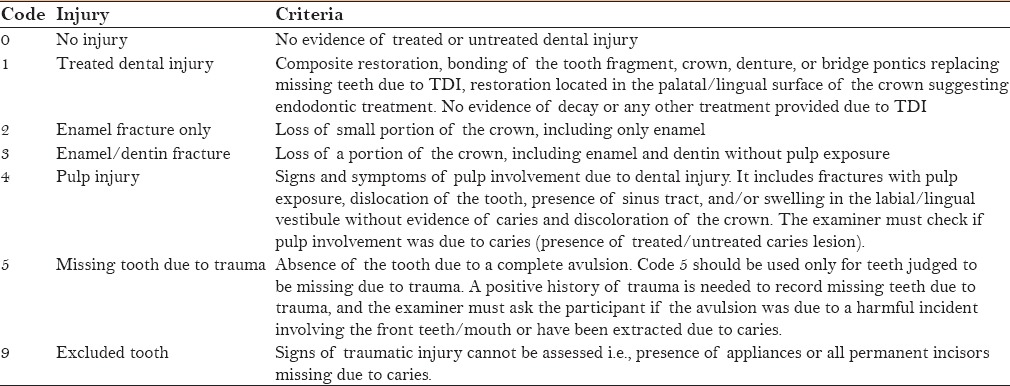
Table 1.
Visual assessment of tooth discoloration and dislocation of teeth by Andreasen et al. (2012)
RESULTS
Out of the 800 children enrolled in the study, only 686 were included based on the inclusion criteria. Out of the 686 children, 379 (55.2%) were males and 308 (44.8%) were females. The prevalence of children sustaining anterior dental trauma was recorded to be 10.2%. Out of the 70 children who suffered TDI, 64.3% were males and 35.7% were females. However, the association of gender characteristics with children exposed to anterior dental trauma was not significantly correlated (P = 0.109) [Table 2]. Maxillary anterior teeth were affected more compared to the mandibular teeth, and central incisors were the most affected teeth. The teeth least involved were the maxillary and mandibular canines [Table 3].
Table 2.
Gender wise distribution of dental injuries in the study population
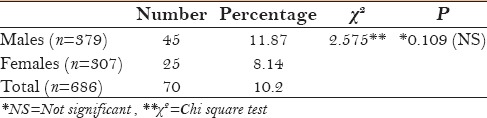
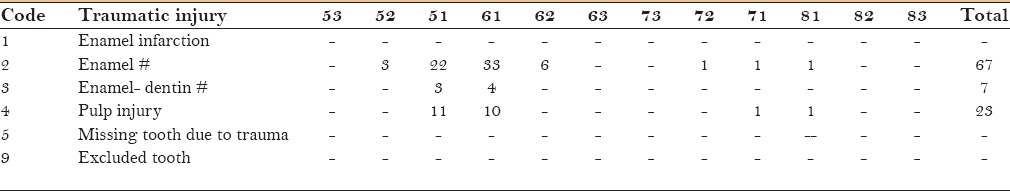
Table 3.
The type and distribution of TDI vs. tooth type
Enamel fracture was 69% followed by 24% of pulpal injury or crown discoloration and 7% of enamel and dentin fracture [Table 3 and Figure 1]. Majority of anterior dental trauma was observed at an older age of 5 years followed by 4 and 3 years [Figure 2]. Males were more prone to dental injury than females [Figure 3]. Although anterior dental trauma was not significantly correlated to the SES of their parents, it was relatively more among high SES (57.2%) compared to low SES (42.9%) [Table 4].
Figure 1.
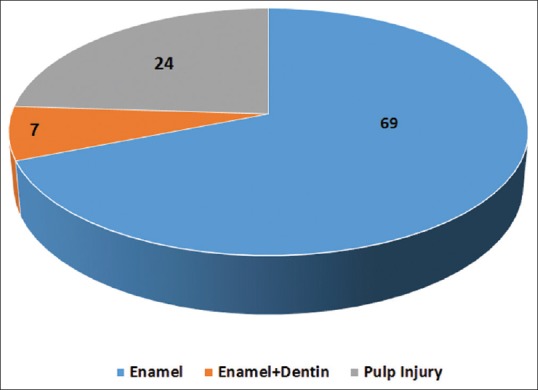
Distribution of the type of traumatic injury
Figure 2.
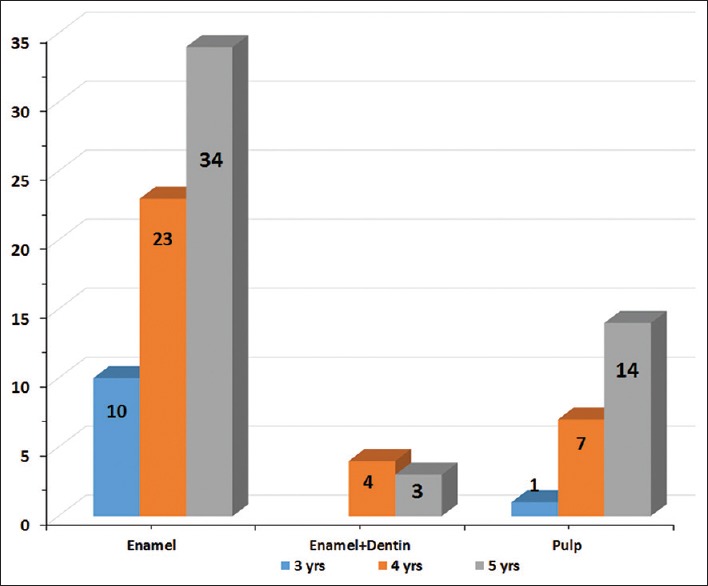
Distribution of the type of injury vs. age of the study population
Figure 3.
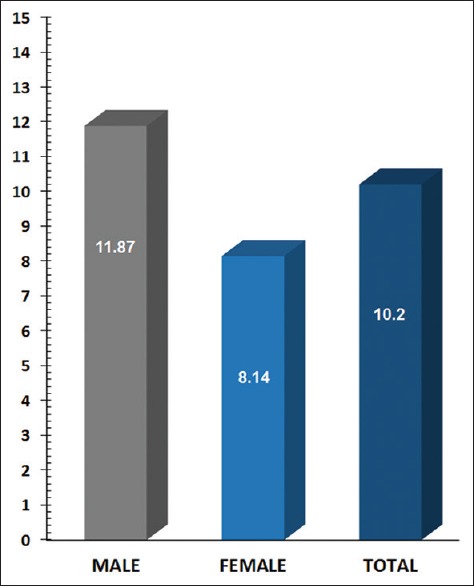
Percentage distribution of TDI vs. Gender
Table 4.
Distribution of TDI vs. socioeconomic status of parents

DISCUSSION
TDI range from minor fractures of the enamel to major damage involving the displacement or avulsion of teeth. The prevalence of TDI in primary teeth ranges from 9.4% to 71.4%.[10,29,30,31,32] Of all the dental injuries that occur before 30 years of age, 50% occur before the age of 10 with the peak being between 2-4 years.[33] However comparisons between studies should be performed with caution due to the lack of uniformity in the samples, clinical diagnostic criteria, location of the study, and age groups.[33] The prevalence of anterior dental trauma in the present study population was 10.2%, which was in concordance with the studies reported earlier.[24,25,33]
Males experienced more dental trauma than females, and accidents at home and school are the major sources of TDI.[34] In the present study, males experienced significantly higher incidence of dental trauma compared to females. Gender is a well-known risk variable in which males experience dental injuries twice as often as females. However, other studies depict conflicting reports with no sex predilection in primary dentition trauma.[33] Most common dental trauma is the crown fracture that account for approximately 80-90% of the cases. In the present study we observed a similar trend of fracture of the crown with complete involvement of enamel. This finding is in agreement with earlier reports.[33] A considerable amount of studies have depicted that traumatic injury to the primary teeth often involves a single tooth and infrequently more than two teeth.[33]
In the present study, we could not find any correlation between SES and dental trauma. Earlier studies have reported inconsistencies in the association between SES and dental trauma in children.[7,33] A study conducted among various school children in Jordon, Jamani, and Fayyad[35] reported high prevalence of dental injuries among children from high SES in Jordon, which is in agreement with a later study from Brazil.[36] Hamilton et al.[37] reported that children in the lower socioeconomic groups had significantly more dental injuries. Several other studies failed to establish any conclusion regarding the SES of the parents and TDI.[33,38,39,40] In the Indian population, the measurement of SES is generally done using BG Prasad's scale and Uday Pareek scale for urban and rural areas and rural areas, respectively.[41] On the other hand, for the urban population, the scale developed by Kuppuswamy in 1976 attempts to accurately measure the SES of the family based on three variables; education, occupation of the head of the family, and per capita income per month.[28] In this study, we used the Kuppuswamy scale to assess the SES.
Dental injuries occurs more often in the maxilla than in the mandible, and the upper central incisors are the teeth most commonly injured.[42,43] The explanation for this could be the natural protection of the mandibular incisors combined with the relative prominence of the maxillary central incisors.[44] In the present study, we found that the maxillary central incisors are the worst affected. Thus, they tend to be the first ones to procure a direct blow resulting in a fracture. In addition, the upper jaw is attached to the skull which makes it rigid, whereas mandible, being a flexible part, aids in reduced impact forces toward lower anterior teeth by movement.[38]
The study was conducted in a selected area in a city. Future studies should aim at randomizing the sample with a larger group of children. This preliminary data can be used by health policy makers to conduct a national community-level survey at a later stage to implement specific policies.[45]
CONCLUSION
The prevalence rate of dental trauma among children aged 3-5 years was 10.2%. This observation is in accordance with similar studies conducted elsewhere. However, limitations such as different systems used to record the injuries has crippled the comparison of the observations. However, this observation will be helpful in organizing national-level surveys as well as to assess the treatment requirements. It will also help in educating parents and primary school caregivers on the consequence of injuries to children and educating them regarding the preventive strategies. Associated factors such as SES was observed to be not significantly correlated to dental trauma among the studies preschoolers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.de Paiva HN, Paiva PC, de Paula Silva CJ, Lamounier JA, Ferreira EFE, Ferreira RC, et al. Is there an association between traumatic dental injury and social capital, binge drinking and socioeconomic indicators among schoolchildren? PLoS One. 2015;10:e0118484. doi: 10.1371/journal.pone.0118484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cortes MI, Marcenes W, Sheiham A. Impact of traumatic injuries to the permanent teeth on the oral health-related quality of life in 12-14-year-old children. Community Dent Oral Epidemiol. 2002;30:193–8. doi: 10.1034/j.1600-0528.2002.300305.x. [DOI] [PubMed] [Google Scholar]
- 3.Feliciano KM, de Franca Caldas A., Jr A systematic review of the diagnostic classifications of traumatic dental injuries. Dent Traumatol. 2006;22:71–6. doi: 10.1111/j.1600-9657.2006.00342.x. [DOI] [PubMed] [Google Scholar]
- 4.Berti GO, Hesse D, Bonifacio CC, Raggio DP, Bonecker MJ. Epidemiological study of traumatic dental injuries in 5- to 6-year-old Brazilian children. Braz Oral Res. 2015;29:1–6. doi: 10.1590/1807-3107BOR-2015.vol29.0103. [DOI] [PubMed] [Google Scholar]
- 5.ElKarmi RF, Hamdan MA, Rajab LD, Abu-Ghazaleh SB, Sonbol HN. Prevalence of traumatic dental injuries and associated factors among preschool children in Amman, Jordan. Dent Traumatol. 2015;31:487–92. doi: 10.1111/edt.12183. [DOI] [PubMed] [Google Scholar]
- 6.Bhayya DP, Shyagali TR. Traumatic injuries in the primary teeth of 4- to 6-year-old school children in gulbarga city, India. A prevalence study. Oral Health Dent Manag. 2013;12:17–23. [PubMed] [Google Scholar]
- 7.Lam R. Epidemiology and outcomes of traumatic dental injuries: A review of the literature. Aust Dent J. 2016;61((Suppl) 1):4–20. doi: 10.1111/adj.12395. [DOI] [PubMed] [Google Scholar]
- 8.Bijella MF, Yared FN, Bijella VT, Lopes ES. Occurrence of primary incisor traumatism in Brazilian children: A house-by-house survey. ASDC J Dent Child. 1990;57:424–7. [PubMed] [Google Scholar]
- 9.Aldrigui JM, Jabbar NS, Bonecker M, Braga MM, Wanderley MT. Trends and associated factors in prevalence of dental trauma in Latin America and Caribbean: A systematic review and meta-analysis. Community Dent Oral Epidemiol. 2014;42:30–42. doi: 10.1111/cdoe.12053. [DOI] [PubMed] [Google Scholar]
- 10.Cardoso M, de Carvalho Rocha MJ. Traumatized primary teeth in children assisted at the Federal University of Santa Catarina, Brazil. Dent Traumatol. 2002;18:129–33. doi: 10.1034/j.1600-9657.2002.00030.x. [DOI] [PubMed] [Google Scholar]
- 11.Siqueira MB, Gomes MC, Oliveira AC, Martins CC, Granville-Garcia AF, Paiva SM. Predisposing factors for traumatic dental injury in primary teeth and seeking of post-trauma care. Braz Dent J. 2013;24:647–54. doi: 10.1590/0103-6440201302352. [DOI] [PubMed] [Google Scholar]
- 12.Oliveira LB, Marcenes W, Ardenghi TM, Sheiham A, Bonecker M. Traumatic dental injuries and associated factors among Brazilian preschool children. Dent Traumatol. 2007;23:76–81. doi: 10.1111/j.1600-9657.2005.00413.x. [DOI] [PubMed] [Google Scholar]
- 13.American Academy on Pediatric Dentistry Clinical Affairs Committee-Developing Dentition S, American Academy on Pediatric Dentistry Council on Clinical A: Guideline on management of the developing dentition and occlusion in pediatric dentistry. Pediatr Dent. 2008;30(7)(Suppl):184–95. [PubMed] [Google Scholar]
- 14.Bharath KP. The reverberations of traumatized primary dentition: A practitioner's perspective. J Contemp Dent Pract. 2011;12:511–5. [PubMed] [Google Scholar]
- 15.Norton E, O’Connell AC. Traumatic dental injuries and their association with malocclusion in the primary dentition of Irish children. Dent Traumatol. 2012;28:81–6. doi: 10.1111/j.1600-9657.2011.01032.x. [DOI] [PubMed] [Google Scholar]
- 16.Malikaew P, Watt RG, Sheiham A. Prevalence and factors associated with traumatic dental injuries (TDI) to anterior teeth of 11-13 year old Thai children. Community Dent Health. 2006;23:222–7. [PubMed] [Google Scholar]
- 17.Freire-Maia FB, Auad SM, Abreu MH, Sardenberg F, Martins MT, Paiva SM, et al. Oral Health-Related Quality of Life and Traumatic Dental Injuries in Young Permanent Incisors in Brazilian Schoolchildren: A Multilevel Approach. PLoS One. 2015;10(8):e0135369. doi: 10.1371/journal.pone.0135369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Bajjali TT, Rajab LD. Traumatic dental injuries among 12-year-old Jordanian schoolchildren: An investigation on obesity and other risk factors. BMC Oral Health. 2014;14:101. doi: 10.1186/1472-6831-14-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mattila ML, Rautava P, Ojanlatva A, Paunio P, Hyssala L, Helenius H, Sillanpaa M. Will the role of family influence dental caries among seven-year-old children? Acta Odontol Scand. 2005;63:73–84. doi: 10.1080/00016350510019720. [DOI] [PubMed] [Google Scholar]
- 20.Altay N, Gungor HC. A retrospective study of dento-alveolar injuries of children in Ankara, Turkey. Dent Traumatol. 2001;17:201–4. doi: 10.1034/j.1600-9657.2001.170502.x. [DOI] [PubMed] [Google Scholar]
- 21.Blinkhorn FA. The aetiology of dento-alveolar injuries and factors influencing attendance for emergency care of adolescents in the north west of England. Endod Dent Traumatol. 2000;16:162–5. doi: 10.1034/j.1600-9657.2000.016004162.x. [DOI] [PubMed] [Google Scholar]
- 22.Rocha MJ, Cardoso M. Traumatized permanent teeth in Brazilian children assisted at the Federal University of Santa Catarina, Brazil. Dent Traumatol. 2001;17:245–9. doi: 10.1034/j.1600-9657.2001.170601.x. [DOI] [PubMed] [Google Scholar]
- 23.Awooda EM, Ali YA. Social judgments made by children (10-15 year old) in relation to visible incisors trauma: School-based cross-sectional study in Khartoum state, Sudan. J Int Soc Prev Community Dent. 2015;5:425–31. doi: 10.4103/2231-0762.165931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rai SB, Munshi AK. Traumatic injuries to the anterior teeth among South Kanara school children - A prevalence study. J Indian Soc Pedod Prev Dent. 1998;16:44–51. [PubMed] [Google Scholar]
- 25.Shekhar MG, Mohan R. Traumatic dental injuries to primary incisors and the terminal or occlusal plane relationship in Indian preschool children. Community Dent Health. 2011;28:104–6. [PubMed] [Google Scholar]
- 26.Singhal S, Gupta P, Mathur B, Banda S, Dandia R, Gupta R. Educational status and dietary fat and anti-oxidant intake in urban subjects. J Assoc Physicians India. 1998;46:684–8. [PubMed] [Google Scholar]
- 27.Andreasen JO, Lauridsen E, Gerds TA, Ahrensburg SS. Dental Trauma Guide: A source of evidence-based treatment guidelines for dental trauma. Dent Traumatol. 2012;28:345–50. doi: 10.1111/j.1600-9657.2011.01059_1.x. [DOI] [PubMed] [Google Scholar]
- 28.Kuppuswamy B. Manual of Socioeconomic Status (urban families) Manasayan Delhi: 1981. [Google Scholar]
- 29.Al-Majed I, Murray JJ, Maguire A. Prevalence of dental trauma in 5-6- and 12-14-year-old boys in Riyadh, Saudi Arabia. Dent Traumatol. 2001;17:153–8. doi: 10.1034/j.1600-9657.2001.170403.x. [DOI] [PubMed] [Google Scholar]
- 30.Saroglu I, Sonmez H. The prevalence of traumatic injuries treated in the pedodontic clinic of Ankara University, Turkey, during 18 months. Dent Traumatol. 2002;18:299–303. doi: 10.1034/j.1600-9657.2002.00093.x. [DOI] [PubMed] [Google Scholar]
- 31.Granville-Garcia AF, Vieira IT, Siqueira MJ, de Menezes VA, Cavalcanti AL. Traumatic dental injuries and associated factors among Brazilian preschool children aged 1-5 years. Acta Odontol Latinoam. 2010;23:47–52. [PubMed] [Google Scholar]
- 32.Francisco SS, Filho FJ, Pinheiro ET, Murrer RD, de Jesus Soares A. Prevalence of traumatic dental injuries and associated factors among Brazilian schoolchildren. Oral Health Prev Dent. 2013;11:31–8. doi: 10.3290/j.ohpd.a29373. [DOI] [PubMed] [Google Scholar]
- 33.Correa-Faria P, Martins CC, Bonecker M, Paiva SM, Ramos-Jorge ML, Pordeus IA. Clinical factors and socio-demographic characteristics associated with dental trauma in children: A systematic review and meta-analysis. Dent Traumatol. 2016 doi: 10.1111/edt.12268. doi: 10.1111/edt. 12268. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 34.Bastone EB, Freer TJ, McNamara JR. Epidemiology of dental trauma: A review of the literature. Aust Dent J. 2000;45:2–9. doi: 10.1111/j.1834-7819.2000.tb00234.x. [DOI] [PubMed] [Google Scholar]
- 35.Jamani KD, Fayyad MA. Prevalence of traumatized permanent incisors in Jordanian children, according to age, sex and socio-economic class. Odontostomatol Trop. 1991;14:17–20. [PubMed] [Google Scholar]
- 36.Cortes MI, Marcenes W, Sheiham A. Prevalence and correlates of traumatic injuries to the permanent teeth of schoolchildren aged 9-14 years in Belo Horizonte, Brazil. Dent Traumatol. 2001;17:22–6. doi: 10.1034/j.1600-9657.2001.170105.x. [DOI] [PubMed] [Google Scholar]
- 37.Hamilton FA, Hill FJ, Holloway PJ. An investigation of dento-alveolar trauma and its treatment in an adolescent population. Part 1: The prevalence and incidence of injuries and the extent and adequacy of treatment received. Br Dent J. 1997;182:91–5. doi: 10.1038/sj.bdj.4809313. [DOI] [PubMed] [Google Scholar]
- 38.Marcenes W, Alessi ON, Traebert J. Causes and prevalence of traumatic injuries to the permanent incisors of school children aged 12 years in Jaragua do Sul, Brazil. Int Dent J. 2000;50:87–92. doi: 10.1002/j.1875-595x.2000.tb00804.x. [DOI] [PubMed] [Google Scholar]
- 39.Nicolau B, Marcenes W, Sheiham A. Prevalence, causes and correlates of traumatic dental injuries among 13-year-olds in Brazil. Dent Traumatol. 2001;17:213–7. doi: 10.1034/j.1600-9657.2001.170505.x. [DOI] [PubMed] [Google Scholar]
- 40.Singh M, Ingle NA, Kaur N, Yadav P. Evaluation of knowledge and attitude of school teachers about emergency management of traumatic dental injury. J Int Soc Prev Community Dent. 2015;5:108–13. doi: 10.4103/2231-0762.155735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holyachi S, Santosh A. Socioeconomic status scales-An update. Annals of Community Health. 2013;1:24–7. [Google Scholar]
- 42.Koroluk LD, Tulloch JF, Phillips C. Incisor trauma and early treatment for Class II Division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2003;123:117–25. doi: 10.1067/mod.2003.86. [DOI] [PubMed] [Google Scholar]
- 43.Bauss O, Rohling J, Schwestka-Polly R. Prevalence of traumatic injuries to the permanent incisors in candidates for orthodontic treatment. Dent Traumatol. 2004;20:61–6. doi: 10.1111/j.1600-4469.2004.00230.x. [DOI] [PubMed] [Google Scholar]
- 44.Artun J, Behbehani F, Al-Jame B, Kerosuo H. Incisor trauma in an adolescent Arab population: Prevalence, severity, and occlusal risk factors. Am J Orthod Dentofacial Orthop. 2005;128:347–52. doi: 10.1016/j.ajodo.2004.06.032. [DOI] [PubMed] [Google Scholar]
- 45.Kothia NR, Bommireddy VS, Devaki T, Vinnakota NR, Ravoori S, Sanikommu S, et al. Assessment of the Status of National Oral Health Policy in India. Int J Health Policy Manag. 2015;4:575–81. doi: 10.15171/ijhpm.2015.137. [DOI] [PMC free article] [PubMed] [Google Scholar]


