Abstract
Objectives:
Musculoskeletal problems (MSPs) are a major complication for practitioners in the field of dentistry. The present study is designed to define the prevalence of MSPs among Iranian dentists.
Materials and Methods:
This was a cross-sectional survey conducted on 600 dentists. The questions were about demographic characteristics, headache, and physical problems of different parts of the body. Data were analyzed using logistic regression analysis.
Results:
Of all dentists studied, 67.5% had physical problems. These MSPs were observed in neck (51.87%), wrist (92.96%), waist (11.11%), and shoulder (7.40%) of the practitioners. Some practitioners took leave of absence (18.52%), while others (7.40%) underwent medical care. There was a direct correlation between age (P = 0.0001), high body mass index (BMI; P = 0.021), total number of daily under-care patients (P = 0.002), and little physical activity (P = 0.0001) with MSPs.
Conclusion:
The prevalence of MSPs is very high among dentists. Awareness about preventive care is necessary for dentists. The dental curriculum also should address ergonomic issues for dental educators.
Keywords: Dental profession, dentist, ergonomics, musculoskeletal problems, dental education
INTRODUCTION
Dental profession is categorized as a high-risk job due to increased physical involvement in performance.[1] No other health professionals are so much prone to occupational diseases. The constant malposition of the practitioner when performing a dental procedure is a predisposing factor for many future physical limitations in a long-term professional life. Uncomfortable positions assumed by dentists during work, without doubt, cannot remain without affecting the health.[2,3] These problems are evidenced in neck, back, hand, shoulder, and some other parts of the body.[2,4,5,6,7,8] Other healthcare providers have also not been secure from musculoskeletal problems (MSPs).[9]
A limited number of well-defined workshops or booklets have been developed for promoting the awareness of healthcare workers of the hazards and consequences of the nonstandard working position when delivering health services.[10] Nor is there a mandatory course in the dental curriculum to teach students on the basis and the principles of ergonomics for healthy practice. However, some countries have individually developed their own guidelines and introduced preventive measures in this regard.[6,11]
The MSPs may disrupt the regular professional activity of the practitioners. If not treated, some of these problems may progress to permanent skeletal deformity.[6] Early retirement is a consequence of progression of MSPs.[3,12] Obviously, all of these problems cannot be without a financial burden for the fellow practitioner.[13,14]
Occurrence of such MSPs in dental professionals is unfortunately under-reported.[15] The science of “ergonomics” has proposed very helpful guidelines for dental professionals.[3,16] Educating the dental professionals based upon such guidelines is a crucial issue for “healthy maintaining” of this important group of the health professionals.
MSPs may also appear in others due to their own individual factors (smoking, overweight, nonstandardized physical activity, etc.).[17] In Iran, MSPs has been reported among the workers of rubber factory.[18] There are other studies that detected the MSPs among dentists practicing in some large cities.[19,20,21] This study was accordingly designed to find the prevalence of such physical complications among Iranian dentists.
MATERIALS AND METHODS
The study design is of descriptive and cross-sectional type. The participants were randomly selected from the entire list of 25,000 licensed dentists at the Medical Council of Islamic Republic of Iran (MCIRI) office. They were the general dentists running a private dental office in different cities of the country. Of the 760 forms sent, 600 questionnaires were returned and were acceptable, fully filled-out with no ambiguity.
The questionnaire contained queries about the following: Age, gender, height, weight, the time lapse after graduation, number of days in office, average number of patients being treated in a day, and physical posture when performing a dental procedure for patients (seated or standing). It also contained a question on whether the practitioner was suffering from any type of musculoskeletal disturbance and its location (back, neck, wrist or hand, and/or shoulder). They were also asked to express the characteristics of pain, concerning the time duration, the extent of involvement, whether the problem forced him/her to take leave of absence from the job, and/or whether taking medications was additionally required for resolution of the problem.
The questionnaires were anonymous. Participation in the study was obviously fully voluntary. The duration of the process of mailing the questionnaires and returning the forms by the participants was around 8 months, from early September 2013 till late April 2014. Obviously, this study was not exempted from the limitations of a survey research method, such as problems related to postal services, displacing and/or losing the mail by the participants, and receiving incomplete questionnaires.
The data were analyzed by SPSS software (version 17.0). The frequency, standard deviation, and percent of demographic characteristics of participants related to the variables of the study were calculated. A significance level of 5% was used for the analysis. The prevalence of musculoskeletal disturbances among dentists was calculated according to the location, frequency, and continuity of pain. To evaluate the correlation of all nine variables that may contribute to MSPs, logistic regression analysis was used. The mean value of those with or without MSPs was compared if a variable had statistically significant effect on the prevalence of the physical symptoms. The α-error was considered 0.05 and a value lower than that was reflected as the level of significance.
RESULTS
The prevalence of musculoskeletal pain among 600 Iranian dentists was analyzed in this study. The participating dentists comprised 195 (32.5%) female and 405 (67.5%) male practitioners. The age range of dentists was 26-74 years and the mean age was 42.18 ± 9.59 years. The range of body mass index (BMI) of the dentists was 8.35-33.30 Kgr/M2 and its mean was 24.24 ± 3.15 Kgr/M2 .
The average length of post-graduation years was 15.29 ± 9.18 and the range was 1-35 years. The mean weekdays of practice of dentists were 4.96 ± 0.96 with a range of 3-6 days. The average daily work hours of dentists were 5.89 ± 1.3 with a range of 3-9 h/day. The mean number of patients treated daily was 7.94 ± 2.72, with a minimum of 1 and a maximum of 20 cases treated per day.
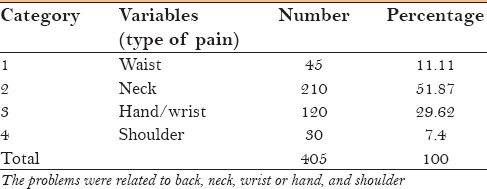
According to the results of this study, 463 (77.25%) dentists used to work “seated” while 137 (22.75%) habitually worked “standing.” Overall, 405 (67.5%) of the participants had been suffering from some kind of physical symptoms in the past 12 months. These physical symptoms were mostly located in the following: Waist [45 (11.11%)], neck [210 (51.87%)], hand/wrist [120 (29.62%)], and shoulder [30 (7.4%)] [Table 1].
Table 1.
Frequency of numbers of dentists with different “musculoskeletal problems”
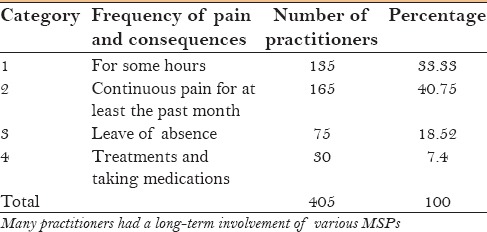
Concerning the duration and characteristics of pain among 405 participants of this study who had complaints of some physical problems, 135 (33.33%) had the pain persisting for some hours. Also, 165 (40.75%) reported having background pain for the past 30 days. Moreover, in 75 (18.52%) fellow practitioners, the symptom was serious enough for them to take leave of absence from the job for recovery. The rest of the participants [20 (7.4%)] suffered from MSPs that forced them to go through some treatment and/or taking medications in the past 12 months [Table 2].
Table 2.
Frequency of “MSPs” based upon length of time and characteristics of the discomfort
Another detectable MSP was headache. However, 450 (75%) dentists had no symptom of such pain, but the remaining [150 (25%)] participants have had an experience of headache during the past 30 days. The pain was categorized into four groups based upon the intensity of the problem. The pain intensity was mild for 45 (30%) persons, with no need to take any analgesic. The other group with moderate headache consisted of 71 (47%) practitioners who had to take medication for relief. The third group consisting of 30 (20%) participants was formed of those who had to take leave of absence due to severity of the symptom. The fourth group [4 (3%)] of participants had to refer to a physician to receive professional medical care. The frequency of pain for the past month was only once for 13 (9%), twice for 59 (39%), three times for 36 (24%), four times for 21 (14%), five times for 15 (10%), but 6 (4%) dentists experienced headache six times or more. Interestingly enough, all practitioners had been involved in some sort of physical activity, but only 150 (25%) did this on a regular basis. The rest [450 (75%)] of the participants had no weekly scheduled plan for that.
To evaluate the effect of different variables on the occurrence of various MSPs, logistic regression analysis was performed on the related data. There was a statistically significant correlation between age of the dentist (P = 0.0001), BMI (P = 0.021), the number of patients treated per day (P = 0.002), and regular physical activity (P = 0.0001) of the dentist and the occurrence of MSPs [Table 3].
Table 3.
Evaluation of the significance level of different variables of this study on the occurrence of musculoskeletal problems among Iranian dentists (a logistic regression analysis)
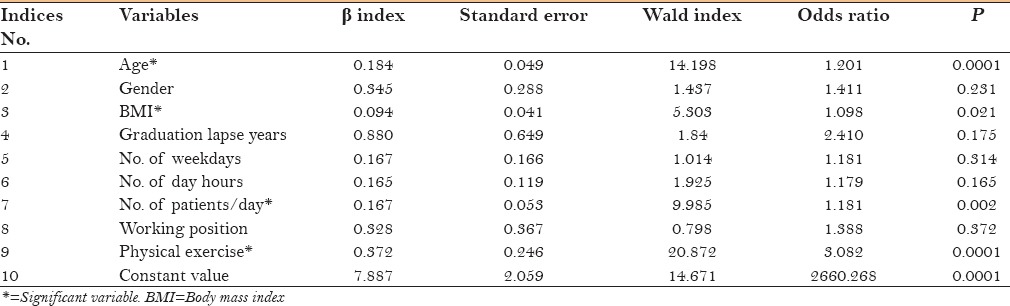
The above result is supported by the fact that the mean age of the practitioners affected with MSPs was 44.35 years and that of practitioners who were not affected was 36.02 years. Moreover, the BMI of those with symptom was 24.65 and that of those without symptom was 23.09. The MSPs were prevalent among those who treated 8.2 patients per day compared to those who treated, on an average, not more than 7.16 patients per day, who were without any problem. Regular physical activity also played the role of a positive intervention for prevention from musculoskeletal symptoms. This could keep 60 practitioners (out of 150 with regular physical activity) (40%) away from the physical problems. On the other hand, among the 450 persons who had no physical activity, only 63 (14%) persons were symptomless.
Based upon logistic regression analysis, it should be noted that gender (P = 0.231), the years elapsed since graduation (P = 0.119), the number of weekdays in office (P = 0.314), the number of day hours treating patients (P = 0.165), and the body posture during work (P = 0.372) had no statistically significant effect on the prevalence of MSPs [Table 3].
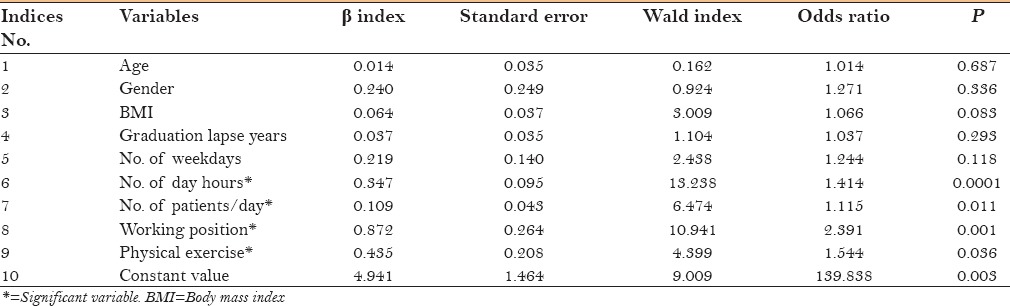
Logistic regression analysis also showed that only the number of day hours treating patients (P = 0.0001), the number of patients treated per day (P = 0.011), the body posture during work (P = 0.001), and regular physical activity (P = 0.036) (totally four variables out of nine) had a significant role on practitioners’ involvement with headache. The rest of the variables had no correlation with the prevalence of headache [Table 4].
Table 4.
Evaluation of the significance level of different variables of this study on the occurrence of headache among Iranian dentists (a logistic regression analysis)
DISCUSSION
Collectively, the results of this study clearly emphasize on the fact that dental professionals are very prone to many MSPs. The posture during work exposes dentists to physical discomfort, disorders of the musculoskeletal system, and irritation of the peripheral nervous system. To prevent these symptoms, the Occupational Safety and Health Association (OSHA) has provided some guidelines in this regard for healthcare professionals.[11]
Among these physical disturbances, “neck” may be the most affected (51.87%), followed by hand/wrist (29.62%), waist (11.11%), and finally shoulder (7.4%) being the least affected location of pain among Iranian dentists. Some other studies also found similar order of prevalence.[6,17,19,20,21,22,23]
Concerning the continuity of pain, two-fifths of participants (40.75%) suffered from persistent pain for the past month at the time of this study. One-third of dentists (33.33%) had the complaint of some hours of pain, occasionally. Nearly, one fifth (18.52%) had to take leave of absence due to physical restriction from provocative pain in some parts of their body. In comparison, this was nearly one-half of the number of Saudi Arabian (37%)[22] and Australian dentists (37.5%)[23] who had to go through the same procedure. Finally, one-fourteenth (7.4%) of the dentists had to desperately seek some professional medical care and/or take medication for relief.
A Polish study in 2002 found that 81.71% of dentists were bound to physical exercise while 66.79% of them only believed that this could be an effective method for prevention.[2] Nevertheless, the regression analysis of this study proved the tremendous effect of physical activity in prevention of musculoskeletal symptoms (P = 0.0001). According to Ghoussoub et al.,[24] new generation of Lebanese dentists are more aware of maintaining a healthy body. In fact, a recent study in New Zealand on 3003 workers emphasized on the role of other risk factors that may also be causative to musculoskeletal symptoms.[25] It seems that medical care policies in different countries can have an effect on the number of these referrals for treatment. Encouraging options in health insurance policies, facilitated reimbursement policies, and healthcare provider incentives are other influential factors for seeking preventive care or treatment.
This study indicated that five out of nine variables had no influence on the physical problems, but the remaining variables (4) were definitely risk factors for MSPs. Gender, years in practice, number of workdays, and daily work hours had no significant correlation with the practitioners’ symptoms. Also, the sitting or standing posture can equally expose the dentist to musculoskeletal symptoms. Nevertheless, age, BMI of the dentist, the number of patients treated per day, and physical exercise were the factors correlated to being unaffected with the above-mentioned symptoms.
It should be mentioned that although the questionnaire of this study was very user-friendly, its limitation was the accuracy of the answers, as there was no face-to-face contact. In addition, the survey research has the advantage of collecting a large number of samples, while the disadvantage is the lower response rate in comparison to other types of similar study design.
CONCLUSION
By nature, dentistry would not lend itself to a healthy posture; nonetheless, with provision of clear instructions and practice, the unwanted and harmful postural consequences of the dental profession can be eliminated. MSPs may decrease the active years of dentists in practice, if not addressed properly and timely. The curriculum of dentistry should accommodate a course that educates students with the principles of ergonomics in the oral health profession. Continuing Dental Education courses, like other dental courses, may equally “remind” and “update” the knowledge of graduates with regard to maintaining a healthy body for providing a higher quality of oral health services.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This research is registered as a doctoral thesis in orthodontics at Shahid Beheshti University of Medical Sciences School of Dentistry at the Office of Academic Affairs under the No. 3067. The authors would like to thank Dr. Ali Rajaee for his sincere assistance in data collection for this study.
REFERENCES
- 1.Murphy DC. Ergonomics in dentistry. NY State Dent J. 1997;63:30–4. [PubMed] [Google Scholar]
- 2.Szymañska J. Disorders of the muskuloskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann Agric Environ Med. 2002;9:169–73. [PubMed] [Google Scholar]
- 3.Gupta A, Bhat M, Mohammed T, Bansal N, Gupta G. Ergonomics in dentistry. Int J Clin Pediatr Dent. 2014;7:30–4. doi: 10.5005/jp-journals-10005-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Visser JL, Straker LM. An investigation of discomfort experienced by dental therapists and assistants at work. Aust Dent J. 1994;39:39–44. doi: 10.1111/j.1834-7819.1994.tb05545.x. [DOI] [PubMed] [Google Scholar]
- 5.Akesson I, Lundborg G, Horstmann V, Skerfving S. Neuropathy in female dental personnel exposed to high frequency vibrations. Occup Environ Med. 1995;52:116–23. doi: 10.1136/oem.52.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29:119–25. doi: 10.1016/s0003-6870(97)00017-3. [DOI] [PubMed] [Google Scholar]
- 7.Ratzon NZ, Yaros T, Mizlik A, Kanner T. Musculoskeletal symptoms among dentists in relation to work posture. Work. 2000;15:153–68. [PubMed] [Google Scholar]
- 8.Marshall ED, Duncombe LM, Robinson RQ, Kilbreath SL. Musculoskeletal symptoms in New South Wales dentists. Aust Dent J. 1997;42:240–6. doi: 10.1111/j.1834-7819.1997.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 9.Jacobsen N, Hensten-Pettersen A. Occupational health problems among dental hygienists. Community Dent Oral Epidemiol. 1995;23:177–81. doi: 10.1111/j.1600-0528.1995.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 10.Dougherty M. Feel-based design: A reason to endorse ergonomics standards. J Colo Dent Assoc. 1999;78:22–5. [PubMed] [Google Scholar]
- 11.Safety and Health Topics: Occupational Safety and Health Association. 2014. [Last accessed on 2015 Jun 23]. Available from: https://www.osha.gov/SLTC/ergonomics/
- 12.Burke FJ, Main JR, Freemand R. The practice of dentistry: An assessment of reasons for premature retirement. Br Dent J. 1997;182:250–4. doi: 10.1038/sj.bdj.4809361. [DOI] [PubMed] [Google Scholar]
- 13.Andersson GB. Epidemiologic features of chronic low-back pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 14.Rundcrantz BL. Pain and discomfort in the musculoskeletal system among dentists. Swed Dent J Suppl. 1991;76:1–102. [PubMed] [Google Scholar]
- 15.Fish DR, Morris-Allen DM. Musculoskeletal disorders in dentists. N Y State Dent J. 1998;64:44–8. [PubMed] [Google Scholar]
- 16.Akesson I, Johnsson B, Rylander L, Moritz U, Skerfving S. Musculoskeletal disorders among female dental personnel--clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health. 1999;72:395–403. doi: 10.1007/s004200050391. [DOI] [PubMed] [Google Scholar]
- 17.Akesson I, Schütz A, Horstmann V, Skerfving S, Moritz U. Musculoskeletal symptoms among dental personnel;-lack of association with mercury and selenium status, overweight and smoking. Swed Dent J. 2000;24:23–38. [PubMed] [Google Scholar]
- 18.Choobineh AR, Tabatabaei SH, Mokhtarzadeh A, Salehi M. Musculuskeletal problems among workers of an Iranian rubber factory. J Occup Health. 2007;49:418–23. doi: 10.1539/joh.49.418. [DOI] [PubMed] [Google Scholar]
- 19.Pargali N, Jowkar N. Prevalence of musculoskeletal pain among dentists in Shiraz, Southern Iran. Int J Occup Environ Med. 2010;1:69–74. [PubMed] [Google Scholar]
- 20.Rabiei M, Shakiba M, Dehgan Shahreza H, Talebzadeh M. Musculoskeletal disorders in dentists. Int J Occup Hyg. 2012;4:36–40. [Google Scholar]
- 21.Shadmehr A, Haddad O, Azarnia S, Sanamloo S. Disorders of the Musculoskeletal System among Tehran, Iranian dentists. J Musculoskelet Pain. 2014;22:256–9. [Google Scholar]
- 22.Al Wazzan KA, Almas K, Al-Shethri SE, Al-Qahtani MQ. Back and neck problems among dentists and dental auxiliaries. J Contemp Dent Parct. 2001;2:17–30. [PubMed] [Google Scholar]
- 23.Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust Dent J. 2006;51:324–7. doi: 10.1111/j.1834-7819.2006.tb00451.x. [DOI] [PubMed] [Google Scholar]
- 24.Sayegh Ghoussoub M, Ghoussoub K, Moucharrafieh L, Khoury A, Sleilaty G, Rifaï K. Musculo-skeletal problems among Lebanese dental surgeons: Occurrence and risk factors. J Med Liban. 2005;53:21–7. [PubMed] [Google Scholar]
- 25.Widanarko B, Legg S, Devereux J, Stevenson M. The combined effect of physical, psychosocial/organisational and/or environmental risk factors on the presence of work-related musculoskeletal symptoms and its consequences. Appl Ergon. 2014;45:1620–1. doi: 10.1016/j.apergo.2014.05.018. [DOI] [PubMed] [Google Scholar]


