Abstract
Objectives
To test the association of age (adolescents vs. older women) and place of delivery with receipt of immediate postpartum contraception in Mexico.
Study design
Retrospective cohort study, Mexico, nationally representative sample of women 12–39 years old at last delivery. We used multivariable logistic regression to test the association of self-reported receipt of postpartum contraception prior to discharge with age and place of delivery (public, employment based, private, or out of facility). We included individual and household-level confounders and calculated relative and absolute multivariable estimates of association.
Results
Our analytic sample included 7022 women (population, N = 9,881,470). Twenty percent of the population was 12–19 years old at last birth, 55% aged 20–29 and 25% 30–39 years old. Overall, 43% of women reported no postpartum contraceptive method. Age was not significantly associated with receipt of a method, controlling for covariates. Women delivering in public facilities had lower odds of receipt of a method (Odds Ratio = 0.52; 95% Confidence Interval (CI) = 0.40–0.68) compared with employment-based insurance facilities. We estimated 76% (95% CI = 74–78%) of adolescents (12–19 years) who deliver in employment-based insurance facilities leave with a method compared with 59% (95% CI = 56–62%) who deliver in public facilities.
Conclusion
Both adolescents and women ages 20–39 receive postpartum contraception, but nearly half of all women receive no method. Place of delivery is correlated with receipt of postpartum contraception, with lower rates in the public sector. Lessons learned from Mexico are relevant to other countries seeking to improve adolescent health through reducing unintended pregnancy.
Implications
Adolescents receive postpartum contraception as often as older women in Mexico, but half of all women receive no method.
Keywords: Mexico, Postpartum contraception, Adolescents, IUD
1. Introduction
Short interpregnancy interval is a known risk factor for poor maternal and infant health outcomes worldwide [1], [2], [3], [4]. Adolescent women (< 20 years old) are at increased risk of poor obstetric outcomes [5] and are at high risk of rapid repeat pregnancy (defined as a pregnancy within 2 years of a previous pregnancy) [6]. Postpartum contraception is a key strategy to prevent rapid repeat pregnancy [7], [8], [9].
To be most effective, postpartum contraception should be provided prior to leaving place of delivery [6]. For many women, especially in low- and middle-income countries, the next health care encounter may only happen with the next pregnancy [10], [11]. The traditional approach of waiting to discuss and provide contraception until the 4–8-week postpartum visit may be too late, and adolescents may be at even higher risk of loss to follow-up and subsequent unintended pregnancy than older women [6].
Reducing adolescent births [12], [13] and disparities in access to and use of contraceptive methods are health policy priorities in Mexico [14]. National population policy supports access to contraception for all women, including promoting postpartum contraception provision [15]. There were over 2.2 million births in Mexico in 2014 [16], 19% of which were to adolescents [17]. Postpartum sterilization is common in Mexico [18] and is a very effective contraceptive method for women who have achieved desired family size. Adolescents and young women, however, may desire more children in the future and need additional contraceptive options.
Insertion of an intrauterine device (IUD) immediately postpartum is safe and has been studied in diverse cultural and health care settings [19], [20]. Provider and cultural biases, however, persist and may limit the use of IUDs by adolescents [21] and/or immediate insertion following delivery [6]. Previous descriptive reports in Mexico suggest that adolescents are at higher risk of leaving place of delivery without contraception [18].
We examined whether age at last birth (women aged 12–19 vs. 20–29 and 30–39) or place of delivery is associated with receipt of any postpartum contraception and, in particular, whether these factors are associated with IUD use. We hypothesized that older women would have higher odds than adolescents of receiving any contraceptive method overall, and the IUD in particular, but that odds would not be significantly different by type of facility.
2. Methods
2.1. Data and sample
We used the 2012 National Health and Nutrition Survey (Encuesta Nacional de Salud y Nutricion, ENSANUT), a nationally representative survey (at the state level and by rural/urban stratum; n = 194,758 individuals, population N = 115,170,278; 87% of households responded) [22], [23]. The ENSANUT is a face-to-face household survey undertaken approximately every 5 years to assess population-level health in Mexico. Population pyramid estimates derived from the ENSANUT are identical to those based on census data, supporting the representativeness of the ENSANUT. Women residing in the household who report a live birth during the 6 years prior (2006–2012) are asked a series of questions about their prenatal and delivery care experiences. The 2012 ENSANUT is the first year to include data on immediate postpartum contraception. We used the household, adult (20 years and over) and adolescent (12–19 years) modules. We included women who reported a live birth in the previous 5 years and were aged 12–39 at the time of delivery. All participants provide informed consent at the time of survey data collection. This study was approved by the Comité de Ética en Investigación (Research Ethics Committee) at the National Institute of Public Health, Cuernavaca, Mexico (October 2, 2014, CI:1258, No. 1576).
2.2. Outcome variables
We focused on two primary binary outcomes: self-reported receipt of any modern postpartum contraceptive method prior to leaving place of delivery and receipt of an IUD. We collapsed contraceptive methods into sterilization, IUD/implant, hormonal method, barrier method, or none. We focused solely on IUD as our second outcome due to the extremely low prevalence of implants in this population (1% of the survey sample).
2.3. Independent variables
Our key independent variables are age and place of delivery. We grouped women into three groups based on age at last birth (12–19, 20–29, 30–39 years old). Place of delivery was classified as employment-based, public, private or out of facility (see Fig. A1).
We included several household-level variables in our analysis. We created an indicator of household wealth with an asset index collapsed into deciles. We developed the asset index using factor analysis and based upon household characteristics and possessions [24]. We classified households as rural (< 2500 inhabitants) or not and created an indicator of enrolment in the Oportunidades conditional cash transfer program [24], an indicator of poverty. We included indigenous status, measured by whether anyone in the household speaks an indigenous language [25]. The 32 Mexican states were collapsed into six regions by socioeconomic level [26].
We included the woman's level of education by calculating educational gap — the difference between the number of years of schooling expected based on age (up to 12 years of schooling total) and the number reported. This measure of years of school missed allows us to compare adolescents, who may still be in school, with adults who have finished schooling. We created a categorical variable (0 years missed, 1–3, 4–6, 7–9, 10 +). We included health insurance (public, employment based or none); in Mexico, health facility types are highly correlated with type of insurance, but the overlap is not complete (see Fig. A1).
We included health care utilization and obstetric history and outcomes variables, which may be correlated both with age and uptake of postpartum contraception. We examined gravidity as a continuous and categorical (1–2, 3–5, 6 +) variable, whether the woman received her first prenatal visit during the first trimester and whether 75% of a list of 11 prenatal processes of care (such as weight and height measurement and glucose tolerance and syphilis testing) were completed. We included mode of delivery (vaginal, planned cesarean, urgent cesarean) and whether the woman reported any type of complication with delivery. We tested models including marital status, but results were unchanged, and we excluded this variable from our final analysis. Our sample includes only women who have given birth; they have thus all been sexually active, and marriage as a proxy for sexual activity is not relevant.
2.4. Analyses
We incorporated survey weights to account for the complex sampling scheme. We report insample and population-level descriptive statistics. We developed multivariable regression models for our two outcomes (any postpartum contraception and postpartum IUD) including the variables described above. We report population-level estimates of odds ratios and 95% confidence intervals. Finally, we calculated absolute estimates of association (as opposed to relative estimates provided by odds ratios) using insample multivariable predicted probabilities controlling for model covariates [27].
We performed several sensitivity analyses: we excluded Region 1, the richest region which only includes Mexico City, from analyses; we examined interactions to test whether the relationship of age and postpartum contraception was modified by insurance, place of delivery or rural residence; and we restricted the sample to women who were not sterilized following delivery. We compared results from models using educational gap variable to models using level of schooling completed, which contained fewer missing observations. Our results were robust to all sensitivity analyses, and we present only our main models below.
3. Results
Our analytic sample included 7022 women aged 12–39 who reported a live birth between 2006 and 2012 (population, N = 9,881,470). Twenty percent of the population was 12–19 years old at last birth, 55% aged 20–29 and 25% 30–39 years old (Table 1). The vast majority of women delivered in facility; only 3% delivered out of facility (Table 2). Close to half of all deliveries were via cesarean (45%; Table 2). Compared with women 20–29 and 30–39, a greater proportion of adolescents reported having no insurance or having public insurance, delivering at a public facility, and delivering vaginally; a lower proportion of adolescents reported initiating prenatal care in the first trimester (Table 2).
Table 1.
Sample characteristics of women 12–39 at last birth, Mexico, 2012
| Overall |
12–19 |
20–29 |
30–39 |
|||||
|---|---|---|---|---|---|---|---|---|
| Sample, n | Population estimate | Sample, n | Population estimate | Sample, n | Population estimate | Sample, n | Population estimate | |
| 7022 | 9,881,470 | 1529 | 1,958,925 | 3495 | 5,445,605 | 1998 | 2,476,939 | |
| 100% | 100% | 21.8% | 19.8% | 49.8% | 55.1% | 28.5% | 25.1% | |
| % (n) | % | % (n) | % | % (n) | % | % (n) | % | |
| Indigenous household | 12.8 (899) | 9.9 | 11.8 (181) | 8.6 | 12.4 (432) | 9.4 | 14.3 (286)⁎ | 12⁎⁎ |
| Oportunidades household | 26.4 (1853) | 21.0 | 21.0 (321) | 19.8 | 25.2 (881) | 19.5 | 32.6 (651)⁎⁎⁎ | 25.2⁎⁎ |
| Rural household | 34.4 (2418) | 23.3 | 35.1 (536) | 25.3 | 34.3 (1198) | 23.1 | 34.2 (684) | 22.2 |
| Educational gap (years of school missed based on age) | ||||||||
| 0 | 17.7 (1243) | 21.3 | 14.3 (219) | 18.0 | 19.7 (687) | 23.4 | 16.9 (337)⁎⁎⁎ | 19.2⁎⁎⁎ |
| 1–3 | 39.5 (2776) | 39.1 | 53.2 (814) | 52.8 | 38.7 (1351) | 37.9 | 30.6 (611) | 31.0 |
| 4–6 | 23.1 (1625) | 20.1 | 23.7 (362) | 21.0 | 22.9 (800) | 19.5 | 23.2 (463) | 20.5 |
| 7–9 | 6.8 (475) | 5.6 | 4.3 (66) | 4.2 | 6.3 (220) | 5.1 | 9.5 (189) | 7.8 |
| 10 + | 5.3 (375) | 4.1 | 2.4 (36) | 1.3 | 4.3 (151) | 3.6 | 9.4 (188) | 7.6 |
| Household wealth decile (1–2 = poorest) | ||||||||
| 1–2 | 25.6 (1792) | 19.0 | 29.6 (450) | 21.6 | 25.3 (884) | 18.8 | 23.0 (458)⁎⁎⁎ | 17.3⁎⁎ |
| 3–4 | 22.1 (1548) | 19.9 | 24.0 (366) | 21.2 | 23.2 (809) | 20.9 | 18.7 (373) | 16.7 |
| 5 + | 52.3 (3665) | 60.8 | 46.4 (707) | 57.0 | 51.5 (1796) | 60.2 | 58.3 (1162) | 65.4 |
| States grouped by socioeconomic region (1 = richest) | ||||||||
| 1 | 2.4 (170) | 6.7 | 2.9 (44) | 6.9 | 1.8 (61) | 5.2 | 3.3 (65)⁎⁎ | 10.0⁎ |
| 2 | 32.5 (2285) | 39.6 | 35.6 (545) | 41.1 | 31.7 (1107) | 40.4 | 31.7 (633) | 36.8 |
| 3 | 17.7 (1246) | 9.5 | 18.0 (275) | 10.1 | 18.2 (636) | 9.8 | 16.8 (335) | 8.2 |
| 4 | 29.7 (2084) | 23.8 | 28.0 (428) | 22.2 | 29.7 (1039) | 23.7 | 30.9 (617) | 25.2 |
| 5 | 6.1 (426) | 9.1 | 5.8 (88)) | 9.3 | 6.5 (227) | 9.4 | 5.6 (111) | 8.3 |
| 6 | 11.5 (811) | 11.3 | 9.7 (149) | 10.4 | 12.2 (425) | 11.6 | 11.8 (237) | 11.6 |
Note: All data are population estimates accounting for complex survey design. n = 5 women were missing data on age, and n = 47 women were missing data on postpartum contraception and excluded from analysis. Women 12–19 were not more likely to be missing data than older women (data not shown); n = 528 women missing data on educational gap, with a higher percentage of older women missing data (data not shown).
= p <.05.
= p <.001.
= p < .0001 for difference by age group between insample or population proportions; chi-square tests.
Table 2.
Health system and delivery characteristics of women 12–39 at last birth, Mexico, 2012
| Overall |
12–19 |
20–29 |
30–39 |
|||||
|---|---|---|---|---|---|---|---|---|
| Sample, n | Population estimate | Sample, n | Population estimate | Sample, n | Population estimate | Sample, n | Population estimate | |
| 7022 | 9,881,470 | 1529 | 1,958,925 | 3495 | 5,445,605 | 1998 | 2,476,939 | |
| 100% | 100% | 21.8% | 19.8% | 49.8% | 55.1% | 28.5% | 25.1% | |
| % (n) | % | % (n) | % | % (n) | % | % (n) | % | |
| Health system utilization variables | ||||||||
| Insurance | ||||||||
| Public | 55.1 (3871) | 48.2 | 59.5 (909) | 50.1 | 54.4 (1902) | 48.1 | 53.1 (1060)⁎⁎⁎ | 46.9⁎⁎⁎ |
| Employment based | 28.1 (1974) | 29.8 | 19.0 (290) | 20.4 | 29.0 (1012) | 30.0 | 33.6 (672) | 36.8 |
| None | 16.8 (1177) | 22.1 | 21.6 (330) | 29.5 | 16.6 (581) | 22.0 | 13.3 (266) | 16.4 |
| Prenatal care initiated in the 1st trimester | 80.9 (5677) | 82.0 | 75.5 (1155) | 75.5 | 82.1 (2870) | 83.0 | 82.7 (1652)⁎⁎⁎ | 85.1⁎⁎⁎ |
| 75% of prenatal processes of care completed | 80.7 (5663) | 79.2 | 79.5 (1216) | 77.5 | 80.1 (2801) | 78.8 | 82.4 (1646) | 81.6 |
| Place of delivery | ||||||||
| Employment based | 26.9 (1890) | 27.9 | 18.4 (282) | 20.7 | 29.3 (1025) | 29.7 | 29.2 (583)⁎⁎⁎ | 29.4⁎⁎⁎ |
| Public | 53.5 (3755) | 48.2 | 67.2 (1028) | 59.8 | 50.9 (1778) | 46.5 | 47.5 (949) | 42.7 |
| Private | 15.1 (1060) | 20.8 | 11.4 (174) | 17.4 | 14.8 (518) | 20.5 | 18.4 (368) | 24.3 |
| Out of facility | 4.5 (317) | 3.1 | 3.0 (45) | 2.1 | 5.0 (174) | 3.3 | 4.9 (98) | 3.5 |
| Obstetric variables | ||||||||
| Gravidity (mean;standard deviation or CI) | 2.70; 1.6 | 2.5 (2.5–2.6) | 1.49; 0.7 | 1.5 (1.5–1.6) | 2.61; 1.3 | 2.4 (2.4–2.5) | 3.8; 1.8 | 3.5 (3.4–3.6) |
| Mode of delivery | ||||||||
| Vaginal | 58.2 (4008) | 54.5 | 62.4 (954) | 61.3 | 59.5 (2081) | 55.4 | 52.7 (1053)⁎⁎⁎ | 47.1⁎⁎⁎ |
| Urgent cesarean | 24.1 (1693) | 25.4 | 26.8 (410) | 27.5 | 23.8 (833) | 26.0 | 22.5 (450) | 22.7 |
| Planned cesarean | 17.7 (1240) | 20.0 | 10.8 (165) | 11.2 | 16.6 (580) | 18.5 | 24.8 (495) | 30.2 |
| Any complication with delivery | 18.3 (1282) | 19.6 | 17.9 (274) | 18.3 | 18.2 (636) | 20.5 | 19.8 (372)⁎ | 18.7 |
Note: All data are population estimates accounting for complex survey design. n = 5 women were missing data on age and n = 47 women were missing data on postpartum contraception and excluded from analysis. Women 12–19 were not more likely to be missing data than older women (data not shown).
= p <.05.
= p < .0001 for difference by age group between insample or population proportions; chi-square tests.
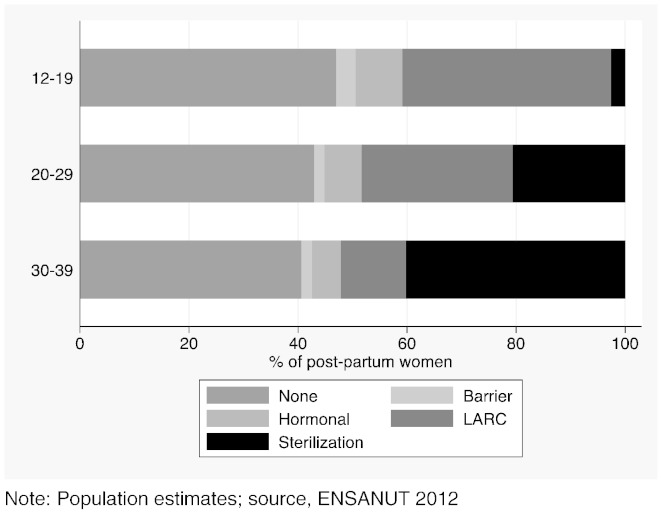
Overall, 43% of women left place of delivery without a contraceptive method. A greater but nonsignificant proportion of women aged 12–19 left place of delivery without a method of contraception (47% vs. 43% women 20–29 and 41% women 30–39; p = .07; Fig. 1). However, 38% of women aged 12–19 left place of delivery with a long-acting reversible contraceptive (LARC) method, which were overwhelmingly IUDs (sample prevalence of implants was 1%; n = 75). Both barrier and hormonal methods were rare in this postpartum sample (Fig. 1). A greater proportion of women delivering in public facilities left without a method (40%) compared with women delivering in employment-based facilities (27%; Fig. A2).
Fig. 1.
Proportion of women receiving postpartum contraception by age at last delivery, Mexico, 2012.
Note: Population estimates; source, ENSANUT 2012.
Age was not significantly associated with receipt of any postpartum method, nor with receipt of an IUD (among the subsample of women receiving reversible contraception), controlling for individual, household, health system and obstetric covariates (Table 3 left column). Place of delivery was significantly and strongly associated with receipt of a method. Compared with employment-based facilities, public (Odds Ratio (OR) = 0.52; 95% Confidence Interval (CI) = 0.40–0.68), private (OR = 0.13; 95% CI = 0.10–0.18) and out-of-facility (OR = 0.06; 95% CI = 0.03–0.12) deliveries all had lower odds of receipt of any method (Table 3 left column). Gravidity, delivery by cesarean and receipt of 75% of processes of prenatal care were positively associated with receipt of any method, but initiation of care in the first trimester was not.
Table 3.
Association of receipt of any postpartum contraception or IUD prior to discharge and age and place of delivery
| Any contraception | IUD among those receiving reversible contraception | |||
|---|---|---|---|---|
| Model, n | 6276 | 2218 | ||
| Population, N | 8,677,287 | 3,090,498 | ||
| OR | 95% CI | OR | 95% CI | |
| Age at last birth (12–19 is referent) | ||||
| 20–29 | 0.99 | 0.79–1.26 | 1.14 | 0.78–1.66 |
| 30–39 | 0.95 | 0.69–1.31 | 0.81 | 0.47–1.41 |
| Rural household | 0.73 | 0.61–0.89 | 0.82 | 0.61–1.10 |
| Educational gap (0 years missed for age is referent) | ||||
| 1–3 years missed for age | 1.15 | 0.90–1.47 | 1.29 | 0.91–1.83 |
| 4–6 | 1.09 | 0.84–1.43 | 1.05 | 0.69–1.60 |
| 7–9 | 0.68 | 0.46-1.00 | 0.96 | 0.37–2.50 |
| 10 + | 0.71 | 0.47–1.07 | 1.40 | 0.62–3.17 |
| Household wealth decile (1–2, poorest, is referent) | ||||
| 3–4 | 0.99 | 0.77–1.27 | 0.90 | 0.60–1.36 |
| 5 + | 0.90 | 0.69–1.17 | 0.96 | 0.64–1.44 |
| Antenatal care content (75% of processes of care) | 1.29 | 1.04–1.60 | 1.12 | 0.75–1.68 |
| Antenatal care timeliness entry into care in first trimester) | 1.23 | 0.99–1.53 | 0.58 | 0.38–0.90 |
| Gravidity (continuous) | 1.24 | 1.14–1.32 | 0.91 | 0.80–1.03 |
| Mode of delivery (vaginal is referent) | ||||
| Urgent cesarean | 1.56 | 1.26–1.94 | 0.73 | 0.50–1.05 |
| Planned cesarean | 2.06 | 1.59–2.68 | 0.94 | 0.60–1.47 |
| Place of delivery (employment based is referent) | ||||
| Public | 0.52 | 0.40–0.68 | 0.49 | 0.32–0.73 |
| Private | 0.13 | 0.10–0.18 | 0.11 | 0.05–0.21 |
| Lay midwife/home | 0.06 | 0.03–0.12 | 0.08 | 0.02–0.28 |
Note. Model incorporates survey weights and controls for additional variables not shown: rural residence, indigenous or Oportunidades household, region, insurance and complication with delivery. Women 12–39 at last birth, Population estimates, Mexico, ENSANUT 2012
Among women receiving reversible contraception prior to discharge, Age was not associated with receipt of an IUD; place of delivery was strongly associated with receipt of an IUD, with similar patterns to receipt of any method.
In absolute terms, insample multivariable predicted probabilities (Table A1) indicate that an estimated 60% (95% CI = 57%–62%) of adolescents leave place of delivery with a method, controlling for all covariates in Table 3. An estimated 74% (95% CI = 72–75%) of women who delivered at employment-based facilities leave with a method, compared with 56% (95% CI = 55–57%) in public facilities. Sixty-eight percent of women who deliver by planned cesarean leave with contraception, compared with 52% of women who deliver vaginally. Within the subsample of women ages 12–19, those who deliver in public facilities are significantly less likely to leave with contraception than those who deliver in employment-based facilities (59%; 95% CI = 56%–62% public vs. 76%; 95% CI = 74%–78% employment-based).
4. Discussion
Contrary to our hypothesis, our data suggest that adolescents are not at higher risk of leaving place of delivery without a contraceptive method compared with older women. Postpartum IUD uptake is 38% among adolescents. A previous study using population-based data estimated that 20% of all Mexican women ages 15–24 used IUDs and that IUDs were more commonly used than hormonal (e.g., pill) methods in this age group [26], but this study did not focus on postpartum provision prior to leaving place of delivery. Misperceptions about the use of IUDs in adolescents may not be as widespread in Mexico, or government efforts to improve access to IUDs by including them on the public insurance formulary may play a role in the high rates of postpartum IUD use by Mexican adolescents.
Forty-three percent of the population of women who delivered reported leaving place of delivery without a contraceptive method. We would not anticipate the proportion to be zero; some women do not desire a contraceptive method or may want to become pregnant again soon, and some women may desire methods not commonly available in the postpartum hospital setting (e.g., hormonal methods). In addition, some women may obtain a method at a later postpartum visit. However, many women will either not return for a postpartum visit or not receive a method at that visit [11]. Postpartum contraception at the place of delivery is important, especially for women with higher risk for loss to follow-up for postpartum care, such as adolescents.
Our data suggest that place and mode of delivery are important correlates of immediate postpartum contraception in Mexico. Previous work has been descriptive [18] or has focused on specific populations [28]. A study at a single facility in Mexico reported a 50% uptake of postpartum contraception in hospital (68% of which were IUDs and 29% sterilization) and identified parity and history of cesarean as significantly and positively associated with acceptance of a method [28]. Cesarean delivery, known to be very common in Mexico [29], was associated with increased odds of receiving contraception in our study as well. As we seek to reduce cesarean delivery rates, especially preventing first cesareans [30], we must maintain focus on postpartum contraception as an essential strategy to promote maternal and newborn health. Providers need knowledge and skills to provide long-acting reversible contraception (i.e., IUDs and implants) after both vaginal and cesarean births.
Antenatal counseling or intensity of antenatal care has been shown to be associated with contraceptive use in Mexico [31] and in other populations [32], [33] but has also been shown to have no effect [34]. We found that intensity of antenatal care, as measured by 75% of recommended processes of care delivered, was significantly associated with any postpartum contraception but that timeliness of prenatal care (accessing care in the first trimester) was not.
The public sector provides the majority of obstetric care in Mexico. Contrary to our hypothesis, we found lower probabilities of postpartum contraception in public compared with employment-based facilities; this is of concern. In theory, all women have access to IUDs in Mexico, and hospitals that want to be certified to receive public insurance reimbursements must be able to provide them. We do not know from our data why there are lower rates of postpartum contraception in the public facilities; this deserves further scrutiny.
Our study must be interpreted with the following limitations in mind. First, our study shares the limitations of any study based on self-reported data; however, we only include births in the past 5 years to reduce the probability of recall bias. Second, we do not know about IUD expulsion or continuation. Previous data from Mexico reported between 77 and 83% continuation rate at 12 months in a randomized controlled trial population [35]. Even in a context of high rates of discontinuation, LARC can reduce rapid repeat pregnancy because it offers protection from pregnancy during the period it is used [6]. Third, our findings about the private sector must be interpreted with caution; our variable includes expensive private hospitals, nonprofit or Non-Governmental Organization facilities, and independent facilities of unknown quality. Fourth, we do not know about the content or quality of counseling that occurs at facilities included in our study. We have weak evidence about postpartum contraceptive educational interventions [36]. Poor or minority women in the US have reported poor communication with providers or feeling coerced [37]; it is unknown whether this also occurs in Mexico. Finally, this is a cross-sectional study. It will be important to track changes in postpartum contraception over time in specific at-risk populations identified in our study (e.g., rural and poor women). The 2012 survey is the first survey wave to include data on immediate postpartum contraception and we were therefore unable to compare our results with prior years. A strength of our analysis is that we report on immediate postpartum contraception as a proportion of all women reporting deliveries; most prior work on postpartum contraception has excluded the many women who do not return for 6-week postpartum visits and therefore likely include biased samples.
In Mexico, adolescents receive postpartum contraception as often as older women, but nearly half of women receive no method. Place of delivery is a key correlate of receipt of postpartum contraception, with lower rates in the public sector than the employment-based facilities, and vaginal delivery is negatively correlated with receipt of a method. Provision of contraception after both vaginal and cesarean births is a key strategy to prevent rapid repeat pregnancy worldwide, especially for adolescents. Lessons learned from Mexico are relevant to other developing countries seeking to improve adolescent health through reducing unintended pregnancy.
The following are the supplementary data related to this article.
Facility and health insurance definitions, Mexico.
Proportion of women receiving postpartum contraception by place of delivery, Mexico, 2012 Note: Population estimates; source, ENSANUT 2012.
Probabilities of receipt of any contraception prior to discharge, women 12–39 at birth, Mexico, 2012, selected variables. N = 6276
Disclosure of interests
The authors have no relevant disclosures.
Details of ethics approval
This study was approved by the Comité de Ética en Investigación (Research Ethics Committee) at the National Institute of Public Health, Cuernavaca, Mexico (October 2, 2014, CI:1258, No. 1576).
Funding
This study was funded by the World Health Organization Department of Reproductive Health and Research. The views expressed here are those of the authors themselves, and they do not necessarily represent the views of the World Health Organization. Dr. Darney was partially supported by an Agency for Healthcare Research and Quality postdoctoral award (HS017582) and by a Junior Investigator Award from the Society of Family Planning (SFPRF9-JI2).
Acknowledgements
The authors wish to thank Zafiro Del Carmen-Andrade and Laura Chavira-Razo for their assistance with the literature review and Biani Saavedra-Avendano for her assistance with analysis.
Portions of this study were presented at the 2014 North American Forum on Family Planning, Miami, FL.
References
- 1.Zhu B.P., Rolfs R.T., Nangle B.E., Horan J.M. Effect of the interval between pregnancies on perinatal outcomes. N Engl J Med. 1999;340:589–594. doi: 10.1056/NEJM199902253400801. [DOI] [PubMed] [Google Scholar]
- 2.Conde-Agudelo A., Rosas-Bermudez A., Kafury-Goeta A.C. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295:1809–1823. doi: 10.1001/jama.295.15.1809. [DOI] [PubMed] [Google Scholar]
- 3.Conde-Agudelo A., Rosas-Bermúdez A., Kafury-Goeta A.C. Effects of birth spacing on maternal health: a systematic review. Am J Obstet Gynecol. 2007;196:297–308. doi: 10.1016/j.ajog.2006.05.055. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva, Switzerland: 2005. Report of a WHO technical consultation on birth spacing. [Google Scholar]
- 5.Ganchimeg T., Ota E., Morisaki N., Laopaiboon M., Lumbiganon P., Zhang J. Pregnancy and childbirth outcomes among adolescent mothers: a world health organization multicountry study. BJOG. 2014;121:40–48. doi: 10.1111/1471-0528.12630. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin M.K., Edelman A.B. The effect of long-acting reversible contraception on rapid repeat pregnancy in adolescents: a review. J Adolesc Health. 2013;52:S47–S53. doi: 10.1016/j.jadohealth.2012.10.278. [DOI] [PubMed] [Google Scholar]
- 7.Chandra-Mouli V., Camacho A.V., Michaud P.A. WHO guidelines on preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. J Adolesc Health. 2013;52:517–522. doi: 10.1016/j.jadohealth.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Damle L.F., Gohari A.C., McEvoy A.K., Desale S.Y., Gomez-Lobo V. Early initiation of postpartum contraception: does is decrease rapid repeat pregnancy in adolescents? J Pediatr Adolesc Gynecol. 2015;28:57–62. doi: 10.1016/j.jpag.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 9.de Bocanegra H Thiel, Chang R., Howell M., Darney P. Interpregnancy intervals: impact of postpartum contraceptive effectiveness and coverage. Am J Obstet Gynecol. 2014;210(311):e1–e8. doi: 10.1016/j.ajog.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 10.Moran C., Fuentes G., Amado F., Higareda H., Bailon R., Zarate A. Postpartum contraceptive practice in hospitals of the federal district. Salud Publica Mex. 1992;34:18–24. [PubMed] [Google Scholar]
- 11.Speroff L., Mishell D.R., Jr. The postpartum visit: it's time for a change in order to optimally initiate contraception. Contraception. 2008;78:90–98. doi: 10.1016/j.contraception.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 12.INMUJERES (Instituto Nacional de las Mujeres) 2012. Elevado riesgo de embarazado no planificado en adolescentes. [Google Scholar]
- 13.Consejo Nacional de Poblacion . CONAPO; Mexico, DF: 2014. Estrategia nacional para la prevencion del embarazo en adolescentes. [Google Scholar]
- 14.Frenk J., Gomez-Dantes O., Langer A. A comprehensive approach to women's health: lessons from the Mexican health reform. BMC Womens Health. 2012;12:42. doi: 10.1186/1472-6874-12-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Consejo Nacional de Poblacion . CONAPO; Mexico, DF: 2008. Programa nacional de poblacion 2008–2012. Por un cambio demografico a favor del desarrollo. [Google Scholar]
- 16.Consejo Nacional de Poblacion . CONAPO; Mexico, DF: 2014. Indicadores sociodemograficos. [Google Scholar]
- 17.Instituto Nacional de Estatistica y Geografia . INEGI; Mexico, DF: 2014. Porcentaje de naciminetos registrados de amdres adolescentes. [Google Scholar]
- 18.Allen-Leigh B., Villalobos-Hernandez A., Hernandez-Serrato M.I., Suarez L., de la Vara E., de Castro F. Use of contraception and family planning in adolescent and adult women in Mexico. Salud Publica Mex. 2013;55(Suppl. 2):S235–S240. [PubMed] [Google Scholar]
- 19.Grimes D.A., Lopez L.M., Schulz K.F., Van Vliet H.A., Stanwood N.L. 2010. Immediate post-partum insertion of intrauterine devices. The Cochrane database of systematic reviews. [CD003036] [Google Scholar]
- 20.Levi E.E., Stuart G.S., Zerden M.L., Garrett J.M., Bryant A.G. Intrauterine device placement during cesarean delivery and continued use 6 months postpartum: a randomized controlled trial. Obstet Gynecol. 2015;126:5–11. doi: 10.1097/AOG.0000000000000882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Callegari L.S., Darney B.G., Godfrey E.M., Sementi O., Dunsmoor-Su R., Prager S.W. Evidence-based selection of candidates for the levonorgestrel intrauterine device (IUD) J Am Board Fam Med. 2014;27:26–33. doi: 10.3122/jabfm.2014.01.130142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gutierrez J.P., Rivera-Dommarco J., Shamah-Levy T., Villalpando-Hernandez S., Franco A., Cuevas-Nasu L. Instituto Nacional de Salud Publica; Cuernavaca, MX: 2012. Encuesta nacional de salud y nutrición 2012. Resultados nacionales. [Google Scholar]
- 23.Romero-Martínez M., Shamah-Levy T., Franco-Núñez A., Villalpando S., Cuevas-Nasu L., Gutiérrez J. Encuesta nacional de salud y nutrición 2012: diseño y cobertura. Salud Publica Mex. 2013;55:S332-S40. [PubMed] [Google Scholar]
- 24.Darney B.G., Weaver M., Sosa-Rubi S.G., Walker D., Mori E., Prager S. The oportunidades conditional cash transfer program: effects on pregnancy and contraceptive use among young rural women in Mexico. Int Perspect Sex Reprod Health. 2013;39:205–217. doi: 10.1363/3920513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Comision Nacional para el Desarrollo de los Pueblos Indigenas . In: Indicadores y estadisticas. Indigenas Comision Nacional para el Desarrollo de los Pueblos Indigena, editor. 2012. [Mexico, DF] [Google Scholar]
- 26.Juarez F., Luis Palma J., Singh S., Bankole A. In: Las necesidades de salud sexual y reproductiva de las adolescentes en Mexico: retos y oportunidades. Institute G., editor. Guttmacher Institute; New York: 2010. [Google Scholar]
- 27.Tomz M., Wittenberg J., King G. CLARIFY: software for interpreting and presenting statistical results. J Stat Softw. 2003;8:1–30. [Google Scholar]
- 28.Romero-Gutierrez G., Garcia-Vazquez M.G., Huerta-Vargas L.F. Ponce-ponce de Leon AL. Postpartum contraceptive acceptance in Leon, Mexico: a multivariate analysis. Eur J Contracept Reprod Health Care. 2009;8:210–216. [PubMed] [Google Scholar]
- 29.Heredia-Pi I., Servan-Mori E.E., Wirtz V.J., Avila-Burgos L., Lozano R. Obstetric care and method of delivery in Mexico: results from the 2012 national health and nutrition survey. PLoS One. 2014;9 doi: 10.1371/journal.pone.0104166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spong C.Y., Berghella V., Wenstrom K.D., Mercer B.M., Saade G.R. Preventing the first cesarean delivery. Summary of a joint eunice kennedy shriver national institute of child health and human development, society for maternal-fetal medicine, and American college of obstretricians and gynecologists workshop. Obstet Gynecol. 2012;120:1181–1193. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barber S.L. Family planning advice and postpartum contraceptive use among low-income women in Mexico. Int Fam Plan Perspect. 2007;33:6–12. doi: 10.1363/3300607. [DOI] [PubMed] [Google Scholar]
- 32.Do M., Hotchkiss D. Relationships between antenatal and postnatal care and post-partum modern contraceptive use: evidence from population surveys in Kenya and Zambia. BMC Health Serv Res. 2013;13:6. doi: 10.1186/1472-6963-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zapata L.B., Murtaza S., Whiteman M.K., Jamieson D.J., Robbins C.L., Marchbanks P.A. Contraceptive counseling and postpartum contraceptive use. Am J Obstet Gynecol. 2015;212(2):171.e1–171.e8. doi: 10.1016/j.ajog.2014.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Akman M., Tuzun S., Uzuner A., Basgul A., Kavak Z. The influence of prenatal counselling on postpartum contraceptive choice. J Int Med Res. 2010;38:1243–1249. doi: 10.1177/147323001003800405. [DOI] [PubMed] [Google Scholar]
- 35.Lara Ricalde R., Menocal Tobias G., Ramos Perez C., Velazquez Ramirez N. Random comparative study between intrauterine device multiload Cu375 and TCu 380a inserted in the postpartum period. Ginecol Obstet Mex. 2006;74:306–311. [PubMed] [Google Scholar]
- 36.Lopez L.M., Hiller J.E., Grimes D.A., Chen M. Education for contraceptive use by women after childbirth. Cochrane Database Syst Rev. 2012;8 doi: 10.1002/14651858.CD001863.pub3. [CD001863] [DOI] [PubMed] [Google Scholar]
- 37.Yee L.M., Simon M.A. Perceptions of coercion, discrimination and other negative experiences in postpartum contraceptive counseling for low-income minority women. J Health Care Poor Underserved. 2011;22:1387–1400. doi: 10.1353/hpu.2011.0144. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Facility and health insurance definitions, Mexico.
Proportion of women receiving postpartum contraception by place of delivery, Mexico, 2012 Note: Population estimates; source, ENSANUT 2012.
Probabilities of receipt of any contraception prior to discharge, women 12–39 at birth, Mexico, 2012, selected variables. N = 6276