Sporadic melioidosis cases have been reported in the African mainland and Indian Ocean islands, but until recently, these regions were not considered areas where B. pseudomallei is endemic. Given the high mortality rate of melioidosis, it is crucial that this disease be recognized and suspected in all regions of endemicity. Previous work has shown that B. pseudomallei originated in Australia, with subsequent introduction into Asia; however, the precise origin of B. pseudomallei in other tropical regions remains poorly understood. Using whole-genome sequencing, we characterized B. pseudomallei isolates from Madagascar and Burkina Faso. Next, we compared these strains to a global collection of B. pseudomallei isolates to identify their evolutionary origins. We found that African B. pseudomallei strains likely originated from Asia and were closely related to South American strains, reflecting a relatively recent shared evolutionary history. We also identified substantial genetic diversity among African strains, suggesting long-term B. pseudomallei endemicity in this region.
KEYWORDS: Burkholderia, epidemiology, infectious disease, melioidosis, phylogeography, population genetics
ABSTRACT
Burkholderia pseudomallei, an environmental bacterium that causes the deadly disease melioidosis, is endemic in northern Australia and Southeast Asia. An increasing number of melioidosis cases are being reported in other tropical regions, including Africa and the Indian Ocean islands. B. pseudomallei first emerged in Australia, with subsequent rare dissemination event(s) to Southeast Asia; however, its dispersal to other regions is not yet well understood. We used large-scale comparative genomics to investigate the origins of three B. pseudomallei isolates from Madagascar and two from Burkina Faso. Phylogenomic reconstruction demonstrates that these African B. pseudomallei isolates group into a single novel clade that resides within the more ancestral Asian clade. Intriguingly, South American strains reside within the African clade, suggesting more recent dissemination from West Africa to the Americas. Anthropogenic factors likely assisted in B. pseudomallei dissemination to Africa, possibly during migration of the Austronesian peoples from Indonesian Borneo to Madagascar ~2,000 years ago, with subsequent genetic diversity driven by mutation and recombination. Our study provides new insights into global patterns of B. pseudomallei dissemination and adds to the growing body of evidence of melioidosis endemicity in Africa. Our findings have important implications for melioidosis diagnosis and management in Africa.
IMPORTANCE Sporadic melioidosis cases have been reported in the African mainland and Indian Ocean islands, but until recently, these regions were not considered areas where B. pseudomallei is endemic. Given the high mortality rate of melioidosis, it is crucial that this disease be recognized and suspected in all regions of endemicity. Previous work has shown that B. pseudomallei originated in Australia, with subsequent introduction into Asia; however, the precise origin of B. pseudomallei in other tropical regions remains poorly understood. Using whole-genome sequencing, we characterized B. pseudomallei isolates from Madagascar and Burkina Faso. Next, we compared these strains to a global collection of B. pseudomallei isolates to identify their evolutionary origins. We found that African B. pseudomallei strains likely originated from Asia and were closely related to South American strains, reflecting a relatively recent shared evolutionary history. We also identified substantial genetic diversity among African strains, suggesting long-term B. pseudomallei endemicity in this region.
INTRODUCTION
The soil-dwelling bacterium Burkholderia pseudomallei is the etiological agent of melioidosis, a disease with high mortality rates in humans and many animals (1). Melioidosis has diverse clinical manifestations and can be difficult to diagnose microbiologically, even in technologically sophisticated laboratories (2, 3). Because of the high mortality rate of melioidosis, which ranges from 10 to 40% even with treatment, the intrinsic resistance of B. pseudomallei to many antibiotics, the potential for acquisition via the aerosol route, and the lack of an effective vaccine, this bacterium is among a small group of pathogens listed as Tier 1 Select Agents by the United States government (1, 4).
The true global distribution of B. pseudomallei remains unclear, although regions not previously thought to harbor this organism are now being identified (1, 5–7). Outside the known hyperendemicity foci of northern Australia and Southeast Asia, B. pseudomallei has been sporadically found in most other tropical regions, including Africa, the Indian Ocean islands, and the Americas (8). It remains unclear whether the spread of melioidosis beyond the known regions where B. pseudomallei is endemic has occurred in recent decades or if it is just being unmasked in Africa and the Americas by better recognition and increased surveillance (9). Several African mainland countries have reported suspected locally acquired melioidosis cases, including Gabon, Malawi, and Sierra Leone (10–12), and there are several instances of travelers acquiring melioidosis during visits to Africa (13–15). Cases have also been reported in Madagascar and the Indian Ocean islands of Mauritius, Seychelles, and La Réunion (16–19). Additionally, countries in Central and South America, including Brazil, Colombia, Ecuador, and Honduras, and several islands in the Caribbean, including Guadeloupe, Martinique, and Puerto Rico, have also reported melioidosis cases (20–31), suggesting that B. pseudomallei is endemic in almost all tropical regions across the globe, as recently predicted by an extensive global modeling study (32).
Although B. pseudomallei has one of the most highly recombinogenic genomes identified to date (33), phylogeographic reconstruction and subsequent geographic attribution of B. pseudomallei populations is possible. The strong geographic signal present in the B. pseudomallei genome reflects its primary mode of transmission; melioidosis is almost invariably caused by contact with contaminated surface water or soil, with human-to-human transmission being exceptionally rare. Thus, large geographic barriers (e.g., the Wallace Line, which separates most of Asia from Australasia) have substantially restricted gene flow between populations. These factors have led to distinct Asian and Australasian B. pseudomallei populations that have regionally evolved over hundreds or thousands of years (33, 34).
Multilocus sequence typing (MLST) is commonly used to study the population structure of many pathogens, including B. pseudomallei (http://pubmlst.org/bpseudomallei), and can be a useful tool for determining the geographic origin of B. pseudomallei strains (34, 35). More recently, an inexpensive capillary electrophoresis-based typing method that exploits size and allelic variations in the 16S-23S rDNA intergenic transcribed spacer (ITS) region has been used to detect geographic signal and diversity in B. pseudomallei (36, 37). However, we and others have noted that these typing methods are unable to determine fine-scale population structure because of low genotyping resolution and high rates of recombination among local B. pseudomallei populations (33, 35). In addition, we have shown that MLST can, albeit infrequently, lead to confounding results because of sequence type (ST) homoplasy (38). Thus, phylogenetic reconstruction of B. pseudomallei populations using genome-wide single-nucleotide polymorphisms (SNPs) derived from whole-genome data is needed to identify the true geographic origins of strains.
In 2009, using emerging next-generation whole-genome sequencing (WGS) technologies, Pearson and coworkers were the first to hypothesize that B. pseudomallei originated in Australia, followed by one or more rare transmission events to Southeast Asia. Using Bayesian inference and molecular clock estimates, Pearson et al. estimated that B. pseudomallei moved into Southeast Asia during the last glacial period (between 16 and 225 thousand years ago), when the Sahul and Sunda land masses were in closest proximity because of greatly lowered sea levels. Subsequently, B. pseudomallei has disseminated to other parts of the globe via similarly rare but significant transmission events (33). This seminal study by Pearson and coworkers was based on relatively few strains, but subsequent studies across larger and more diverse B. pseudomallei data sets have supported their initial hypothesis (35, 38, 39). Although the relationship between Asian and Australian strains has been reasonably well characterized, the origin of B. pseudomallei in other parts of the world is still poorly understood. Of particular interest are Africa and the Americas, where melioidosis was once considered sporadic but is now being unmasked as likely endemic (5). In this study, we aimed to further characterize the global phylogeography of B. pseudomallei by using large-scale comparative genomics to determine the origin of melioidosis in Africa, which has not yet been investigated on a whole-genome scale.
RESULTS AND DISCUSSION
Phylogenomic analysis identifies an African and South American B. pseudomallei clade.
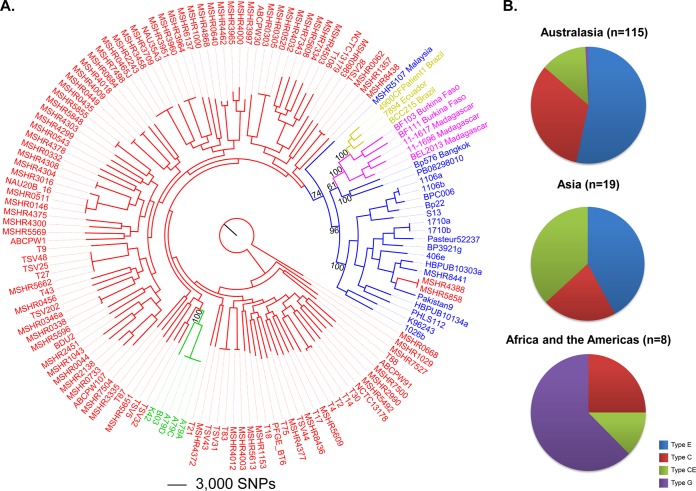
Comparative analysis of the 144 B. pseudomallei genomes, including the five new African genomes generated in this study, identified 202,245 bi-allelic SNPs among these strains. These SNPs were used to reconstruct a maximum-parsimony phylogenetic tree (Fig. 1A). As previously shown (33, 35, 38, 39), we observed a clear distinction between Australasian (red or green) and Asian (blue) B. pseudomallei strains, which was supported by a bootstrap value of 74%. The separation of the Australasian and Asian B. pseudomallei clades is due to the restricted dispersal of B. pseudomallei between these two geographic regions, with ST-562 being the only example where a recent overlap between these two regions has been confirmed (39, 40). The African (pink) and South American (gold) strains all reside on a separate, highly supported (bootstrap value = 100%) branch within the Asian clade.
FIG 1 .
Genetic and genomic comparisons of the African B. pseudomallei isolates with global B. pseudomallei reference strains. (A) Maximum-parsimony phylogeny of 144 B. pseudomallei genomes. This tree was drawn by using 202,245 core genome, orthologous, bi-allelic SNPs identified by the SPANDx pipeline (75) and rooted by using MSHR0668. Isolates are color coded by origin as follows: Australia, red; Papua New Guinea, green; Asia, blue; Africa (including Madagascar), pink; South America, gold. African and South American isolates form their own clade that falls within the more ancestral Asian clade, which is separate from Australasian B. pseudomallei. Bootstrap values were generated on the basis of 200 replicates. The consistency index is 0.19. (B) Distribution of ITS types by geographic region. Similarly to earlier studies, isolates from Africa and the Americas show an overrepresentation of ITS type G in comparison to strains from Australasia and Asia; however, African isolates also possess ITS types CE and C, alleles that are commonly identified in isolates from regions of Asia and Australasia where B. pseudomallei is hyperendemic.
Interestingly, the three South American strains (4900CFPatient1 [36, 41], 7894 [42], and BCC215 [24]) share a node with the two Burkina Faso strains, although the Burkina Faso strains are more closely related to each other than to the South American strains; in contrast, the three Madagascan isolates reside on a separate branch within the African-South American clade (bootstrap value = 100%). This observation demonstrates that African and South American B. pseudomallei likely originated from an Asian ancestor, with no evidence of B. pseudomallei transmission directly from Australia. The location of the African and South American strains within the Asian clade also confirms that transmission into Africa must have occurred after the first B. pseudomallei transmission from Australia to Asia, which has been estimated to have occurred between 16,000 and 225,000 years ago (33). Further, our analysis hints at African ancestry for South American strains, with these strains emerging from a relatively recent branch within the deeper African node (Fig. 1A). This finding suggests that B. pseudomallei was transmitted from West Africa to the Americas. Genomic data from additional American B. pseudomallei isolates will provide much-needed insight into this possibility.
We were next interested in investigating the region in Asia where African B. pseudomallei originated. The Asian isolates closest to the African and South American strains in our phylogeny are B. pseudomallei 576 and PB08298010. However, this branch has only moderate bootstrap support (61%), likely because of undersampling of this clade in the current data set, so we were unable to identify the precise origin of this ancestor. B. pseudomallei 576 was obtained from a 49-year-old female from Bangkok, Thailand, and B. pseudomallei PB08298010 was isolated from a melioidosis case that occurred in Arizona, United States, and was speculated to have originated from contaminated medical supplies imported from Malaysia (35). In support of an Asian origin for PB08298010, its MLST profile is ST-426, which matches the ST of MSHR0158, an isolate from an Australian traveler thought to have acquired melioidosis in Penang, Peninsular Malaysia (http://pubmlst.org/bpseudomallei). Our global phylogeny also supports an Asian origin for B. pseudomallei PB08298010, although this strain does not group with a second Malaysian isolate included in our analysis (MSHR5107). However, unlike MSHR0158, MSHR5107 was isolated from Sarawak, Malaysian Borneo. ST data show little overlap between the Peninsular Malaysia and Malaysian Borneo isolates; thus, it is not surprising that PB08298010 and MSHR5107 do not group together on a whole-genome level.
Our phylogeny demonstrates support for African strains being of Asian origin, although a greater number of Asian strains from more diverse locations will enable more accurate identification of the precise origin(s) of African B. pseudomallei. In particular, there are several suspected regions of endemicity in Asia that have no representative WGS data in our phylogeny, such as Indonesia, Philippines, and Myanmar. Additional isolates from these locations will increase the resolution of these poorly populated clades and may potentially identify a more precise origin of African B. pseudomallei. Of note, genetic analysis of the Malagasy, the indigenous people of Madagascar, shows that approximately half have shared ancestry with Indonesian Borneo people (43). Austronesian migration from Indonesian Borneo to Madagascar is thought to have occurred between 1,500 and 2,000 years ago (44, 45). This migration provides a possible date for an anthropogenically driven introduction of Asian B. pseudomallei into Madagascar and subsequent transfer from Madagascar to the African mainland, potentially through human migration, trade, or slavery routes. At the time of this Austronesian migration, pigs were also introduced to Madagascar (46). Pigs are known to become infected with B. pseudomallei, although they are generally less susceptible than sheep, goats, or horses (47, 48); it is plausible that pigs acted as a reservoir for this pathogen, facilitating the transfer of B. pseudomallei into Madagascar. Several studies have shown that certain bird species may be infected by or commensally carry B. pseudomallei (47, 49). Therefore, an additional possibility is that B. pseudomallei was disseminated from Asia to Madagascar by migratory birds flying along the Asia-East Africa flyway, similar to what has been observed in the introduction of West Nile virus to the Americas from West Africa (50). Future phylogenomic and molecular clock investigations using a larger number of strains from Southeast Asia, Africa, and the Americas will provide further important clues to the origin of B. pseudomallei in Africa and the Americas.
MLST hints at deeper phylogenetic relationships but is subject to homoplasy.
The three clinical isolates from Madagascar belong to STs 1043, 1053, and 1054 (Table 1; see Table S3 in the supplemental material). STs 1043 and 1053 are single-locus variants, whereas ST-1054 is a double-locus variant of ST-1053 and a triple-locus variant of ST-1043. All three of these STs share identical ace, lipA, narK, and ndh alleles but differ at the remaining three loci (gltB, gmhD, and lepA). The two isolates from Burkina Faso belong to STs 1122 and 1121 and are triple-locus variants of one another. STs 1122 and 1043 are double-locus variants, although one strain originated in Madagascar and the other originated in Burkina Faso, a relationship that is potentially misleading and not reflected on a whole-genome scale (Fig. 1A). All five STs are unique, with no other matches in the B. pseudomallei MLST database, including other characterized strains from Africa and South America (see Table S3 in the supplemental material). Although MLST shows some utility for determining strain origin, it can be unreliable in highly recombinogenic organisms like B. pseudomallei when trying to determine deeper phylogenetic relationships (51). Such homoplasy has been demonstrated previously, where B. pseudomallei isolates from Cambodia and Australia were identical by MLST but differed greatly on a whole-genome level (38), thereby making accurate geographic attribution in these cases impossible without WGS. One conclusion that can be made is that there is considerable underlying genetic diversity in these regions, a finding supported by our WGS phylogeny (Fig. 1A) and noted previously in multiple studies using less highly resolving typing methods (13, 16). This underlying diversity further supports the notion that the introduction of B. pseudomallei to these regions is not a recent event, as sufficient time has elapsed since their introduction for divergence to occur.
TABLE 1 .
African and American B. pseudomallei isolates used in this study and associated genotyping information
| Strain name | Other name(s) | STb (allelic profile) | ITS type | Geographic origin, reference (GenBank accession no.) |
|---|---|---|---|---|
| 11-1617 | MSHR7969 | 1054 (4, 12, 34, 1, 5, 2, 1) |
CE | Madagascar, 16 (SRR3145392) |
| 11-1696 | MSHR7968 | 1053 (4, 12, 3, 2, 5, 2, 1) |
C | Madagascar, 16 (SRR3145393) |
| BEL2013 | MSHR7966 | 1043 (4, 1, 3, 2, 5, 2, 1) |
G | Madagascar, 62 (SRR3145396) |
| BF103 | ITM BF103, MSHR7964 |
1121 (1, 18, 13, 2, 5, 6, 1) |
G | Burkina Faso (SRR3145394) |
| BF111 | ITM BF111, MSHR7965 |
1122 (1, 1, 19, 2, 5, 2, 1) |
C | Burkina Faso (SRR3145395) |
| 4900CFPatient1 | NAa | 92 (1, 1, 2, 1, 5, 1, 1) |
G | Brazil (ARZE00000000) |
| 7894 | 7894/300 | 11 (1, 1, 13, 1, 6, 1, 1) |
G | Ecuador (CP009535, CP009536) |
| BCC215 | NA | 1355 (1, 156, 2, 2, 5, 1, 1) |
G | Ceará, Brazil (ABBR00000000) |
NA, not applicable.
Per the B. pseudomallei MLST database (http://pubmlst.org/bpseudomallei).
ITS typing shows unexpected diversity in African, but not American, isolates.
Previously, ITS typing of 1,191 B. pseudomallei isolates revealed that strains from Africa and the Americas have restricted diversity at the 16S-23S rDNA ITS locus, with a dominance of the ITS type G allele among these isolates (36, 37). However, prior to this study, only four African strains had been examined by ITS typing (2002721628 from Madagascar [ITS type G], 2002721629 and 2002721639 from Kenya [ITS types G and C, respectively], and 2002721691 from Mauritius [ITS type GC]) (37). Using WGS data, we determined the ITS genotypes of all of the strains in our data set, including the five African strains. Australasian isolates (n = 115; MSHR6137 could not be typed because of a lack of sequence information covering the 16S-23S spacer region) were predominantly ITS type E (53%), followed by ITS type C (33%) and ITS type CE (13%), with a very small percentage of ITS type G isolates (<1%). Asian isolates (n = 19; excluding PB08298010 due to uncertain provenance) were mostly ITS type CE (42%), followed by ITS type E (37%) and ITS type C (21%). The distribution of Australasian ITS types was almost identical to that seen previously (37); however, the distribution of ITS types among Asian strains differed somewhat, most likely because of sampling bias incurred by our small data set. We did not identify an ITS type G isolate among our Asian strains, which was expected, given the rarity of type G in Asia (<1%) (37). Although the precise origin of PB08298010 is not known, it has previously been shown to be ITS type G (36). The three Madagascan isolates were ITS types C, CE, and G, and the two Burkina Faso isolates were ITS types C and G (Table 1; Fig. 1B). These results reveal further diversity among B. pseudomallei strains from Africa, with the CE allele not previously reported.
The finding of an additional ITS type in the African isolates indicates a complex evolutionary history of B. pseudomallei in this region that is not yet well understood. We pose three possible explanations for this diversity. First, the introduction of B. pseudomallei to Africa from Asia may have occurred as a single transmission event that involved a mixed population of strains, and thus ITS types, with this ITS diversity persisting to the present day. Second, multiple introduction events with different strains may have occurred following several independent dissemination events from Asia. Third, the ITS region in some strains may have undergone convergent evolution across distinct geographic regions, perhaps because of similar selective pressures on B. pseudomallei populations. The ostensible rarity of ITS type G in Asia suggests that the introduction of this ITS allele to Africa was a highly improbable event, although comprehensive analysis of ITS allele distribution across Asian isolates, particularly those from Indonesian Borneo, is currently lacking. To date, ITS type G has been identified in only three Thai strains (Songkhla 25 W-1, Songkhla 25 W-2, and Phattalung 52 W-1). This observation is consistent with the node shared by African strains and Bangkok B. pseudomallei 576 on the whole-genome phylogeny, and it is therefore possible that ITS type G B. pseudomallei in Africa originated from Thailand. All 24 Malaysian strains examined in the study of Liguori et al. (37) lacked the ITS type G allele, although these isolates were derived from a historic B. pseudomallei collection and it is therefore unclear what proportion of these strains, if any, are from Malaysian Borneo. In addition, the heavy sampling bias toward isolates from Thailand (443/480 [92%] Asian strains) may explain the low abundance of ITS type G reported to date. Further ITS typing and WGS data from Bornean and African strains are needed to explore these hypotheses, with such data likely to assist in the more precise determination of the Asian ancestor of ITS type G in Africa.
In contrast to the African strains, the 18 American strains characterized by the ITS typing method have, to date, been genotyped only as ITS type G (36), suggesting a genetic bottleneck during B. pseudomallei dissemination from Africa to the Americas. This finding is consistent with our genome phylogeny, which hints at recent transmission of B. pseudomallei from Africa to the Americas. Although the route of this transmission is highly speculative, one possibility is the movement of West Africans to South America during the transatlantic slave trade between the 16th and 19th centuries. Using pulsed-field gel electrophoresis and MLST, a study of B. pseudomallei isolates from a 2003 Brazilian melioidosis outbreak showed some genetic diversity among strains (24), supporting our hypothesis that the introduction of B. pseudomallei to the Americas did not occur very recently. In addition, our WGS phylogeny confirmed that the three South American strains are not homogeneous on a whole-genome level (Fig. 1A). Whether this diversity also extends to the 16S-23S ITS region in other South American isolates remains to be elucidated.
African B. pseudomallei strains vary in their virulence gene content.
B. pseudomallei has an impressive virulence arsenal, including capsular polysaccharide I, lipopolysaccharides (LPS), a diverse complement of autotransporters, multiple specialized secretion systems, a lethal toxin, and iron-scavenging siderophores (52). To assess the virulence potential of African B. pseudomallei strains, assembled genomes were screened against a large panel of known and putative B. pseudomallei virulence genes (Fig. 2; see Table S2 in the supplemental material). All African isolates and the two isolates from Brazil lacked boaB (BPSL1705), which encodes a trimeric autotransporter adhesin (TAA) that may have a role in macrophage invasion and survival (53); however, boaB was also absent from 81 other B. pseudomallei strains, including Australian clinical blood isolate MSHR0668 and Thai clinical liver abscess isolate 1106a (54), and is therefore unlikely to be a crucial virulence factor. Two additional TAAs were found to be variably present among the African strains; bpaD (BPSS0088) was absent from all five African strains, and BPSL2063 (55) was absent from Madagascan strain BEL2013. Although bpaD was also variably present across the larger data set (absent from ~25% of the strains), BPSL2063 was conserved across the other 142 genomes and variable in only one other isolate (B. pseudomallei Pakistan9; BLAST score ratio [BSR] = 0.72). The best characterized TAA, Burkholderia intracellular motility A (encoded by bimA [BPSS1492]), which is responsible for the actin-based motility of B. pseudomallei (56), was found in all of the African strains. These strains encoded for the more common bimABp variant, which is associated with primary pneumonia presentation of melioidosis (57). The less common variant of bimA, bimABm, is found in ~12% of Australian strains. Outside Australia, it has been reported in only a single isolate from India (58); the bimABm variant is strongly associated with neurological melioidosis (57).
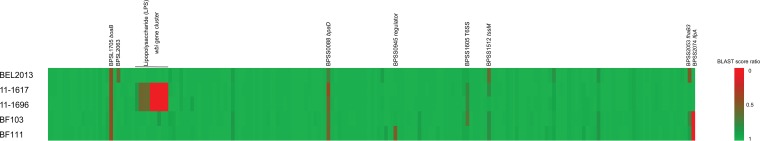
FIG 2 .
Blast score similarity ratios of all of the known virulence markers in B. pseudomallei K96243 compared to the African B. pseudomallei strains. African strains possess variable virulence gene contents, with trimeric autotransporter adhesions, LPS (wbi cluster), filamentous hemagglutinin (fhaB3), and lactonase family protein A (lfpA) all showing variability across strains.
In addition to their variable TAA content, the African B. pseudomallei strains were highly varied at multiple genomic islands (GIs), including at GI16, which encodes two virulence factors, filamentous hemagglutinin (fhaB3) and lactonase family protein A (lfpA) (Fig. 2 and 3). Three out of five African B. pseudomallei strains contained the full-length fhaB3 gene; however, BF103 (Burkina Faso) contained a truncated version (BSR = 0.77) and BEL2013 (Madagascar) lacked fhaB3 entirely. The fhaB3 gene is variably present in B. pseudomallei and was absent from or truncated in 24 additional strains across the larger data set. Absence of this gene has been previously associated with localized skin abscess formation without septicemia, a less severe form of melioidosis that is rarely fatal (57). An additional virulence factor located directly downstream of fhaB3, lfpA, is able to modify host macrophage expression to resemble osteoclastogenesis and is required for full virulence in the Syrian hamster model (59). The lfpA gene is absent from the two Burkina Faso strains but is present in all three strains from Madagascar. The presence of lfpA was highly variable across the remainder of the data set, being absent from ~50% of the strains.
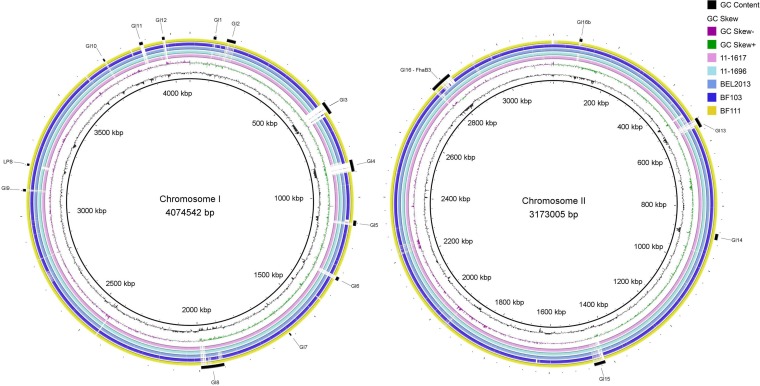
FIG 3 .
Whole-genome comparison of B. pseudomallei African strains aligned with B. pseudomallei K96243 by BLAST ring image generator. The outer ring shows the locations of the known genomic islands in the B. pseudomallei chromosomes. Also shown is the 13.5-kb deletion of the LPS locus in two of the Madagascan B. pseudomallei strains, 11-1617 and 11-1696, at positions ~3,198,200 to ~3,211,800 relative to strain K96243.
The type II O-antigenic polysaccharide (O-PS; wbi gene cluster) is absent from two of the isolates from Madagascar (11-1617 and 11-1696). There is an ~14-kb deletion (genomic coordinates 3,198,200 to 3,211,800 relative to B. pseudomallei K96243 chromosome I), encompassing rmlCD, wzm, wzt, and wbiABCDEFGHI (Fig. 3). Type II O-PS has previously been shown to be required for serum resistance and virulence in animal models (60). Interestingly, this locus also shows a propensity for loss-of-function mutations in a persistent-carriage infection of an Australian patient who has been colonized with B. pseudomallei for >14 years (61). The type II O-PS is also variably present across the larger isolate collection, being absent from an additional 18 strains, so is likely not an essential factor for infection, although it may be required for full virulence.
It remains uncertain why the reported incidence of melioidosis in both Africa and the Americas is far lower than that in other regions where it is endemic, such as Australasia and Thailand. Despite the potential for lower virulence, as shown by the virulence gene profiles, all three cases from Madagascar were blood culture positive and two were fatal (16, 62), suggesting that African B. pseudomallei strains possess full virulence. Decreased virulence should not be ruled out; however, other explanations may account for the low reported melioidosis rates in Africa and the Americas, including limited awareness of melioidosis in these regions, poor access to modern diagnostic and laboratory facilities for B. pseudomallei detection, a lower likelihood of exposure in the general population because of differences in agricultural practices, or a lower incidence of risk factors in the population (5). A final and noncontradictory factor is that B. pseudomallei may indeed be far less common in the environments of Africa and South America than in those of northern Australia and Southeast Asia, although recent modeling suggests that the African and South American environments are permissive for the presence and persistence of B. pseudomallei (32); environmental surveillance studies are under way to assess this possibility. Future studies concentrating on functional virulence assessment and genomic analyses of additional B. pseudomallei strains from these regions are needed to ascertain the true rate of melioidosis and determine if these strains have maintained their full virulence potential.
Conclusions.
Despite high levels of recombination in B. pseudomallei, sufficient signal exists across the genome to robustly determine the geographic origins of strains. In this study, we used WGS to uncover diverse MLST profiles, ITS types, and variation in the virulence gene content of African isolates. Such diversity strongly supports the premise of long-term endemicity of B. pseudomallei in Africa and rules out its recent introduction. Phylogenomic analysis revealed that African B. pseudomallei formed a separate clade that was closely related to South American strains, with this clade residing within the deeper Asian clade, suggesting an ancestral Asian origin for B. pseudomallei in Africa and the Americas. Phylogenomic analysis also showed that the South American strains emerged more recently within the African clade, an observation supported by the single ITS type (G) of all of the American isolates characterized to date. Anthropogenically driven factors provide a plausible explanation for B. pseudomallei transmission to these regions, where B. pseudomallei was previously not endemic.
MATERIALS AND METHODS
Strain selection.
Two B. pseudomallei isolates from Madagascar were obtained from clinical cases occurring in 2012 and 2013 (16), with a third isolate obtained from a French patient in Belgium following a visit to Mahajanga, a city on the northwestern coast of Madagascar (62). The two Burkina Faso isolates were both from children who had not traveled outside Burkina Faso and who presented with localized melioidosis without systemic sepsis. All of the strains used in this study are described in Table 1 (see also Table S1 in the supplemental material). For phylogenomic analysis, we used 144 B. pseudomallei isolates from diverse geographic locations encompassing Asia (n = 20), Australasia (n = 116), Brazil (n = 2), Burkina Faso (n = 2; this study), Madagascar (n = 3; this study), and Ecuador (n = 1).
Complete list of B. pseudomallei isolates used in this study. Download Table S1, XLSX file, 0.02 MB (20.1KB, xlsx) .
Copyright © 2016 Sarovich et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Virulence gene heat map of all of the B. pseudomallei isolates included in this study. Download Table S2, XLSX file, 0.1 MB (119.1KB, xlsx) .
Copyright © 2016 Sarovich et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
African and South American isolates in the B. pseudomallei MLST database and their corresponding allele profiles. Download Table S3, XLSX file, 0.01 MB (12.3KB, xlsx) .
Copyright © 2016 Sarovich et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
MLST.
MLST of all of the isolates was performed either in silico from WGS data by exporting the consensus sequence from the MLST loci with GATK (63) or by Sanger sequencing as previously described (64).
WGS, variant identification, and phylogenetic reconstruction.
Genomic DNA was extracted from the five African genomes as previously described (65). High-quality DNA was subjected to paired-end WGS with the Illumina HiSeq2000 instrument and NextEra XT library preparation to an average depth of 65× (range, 50× to 80×). Publicly available B. pseudomallei genomes were downloaded from NCBI and, where required, converted to simulated Illumina reads with ART (version VanillaIceCream, 85× coverage, paired-end and quality shifts of 10) (66). B. pseudomallei MSHR1655, a sequential isolate from a chronic-carriage infection that has undergone genome reduction (61), was excluded from this analysis to maximize core genome size; all of the other available genomes of acceptable quality were included. Core genome, orthologous, biallelic SNPs were identified by GATK v3.1 (63) within the comparative genomics pipeline SPANDx v2.7 (75) by using default parameters. The B. pseudomallei K96243 reference genome (67) was used for read mapping by BWA v0.6.2 (68) (GenBank accession numbers BX571965 and BX971966). Maximum-parsimony analyses were performed by a heuristic search with PAUP v4.0b10 (69). Trees were bootstrapped in PAUP using 200 replicates.
16S-23S rDNA ITS typing.
The ITS types of the five African isolates were determined from whole-genome sequences. Briefly, genomes were assembled with an in-house assembly pipeline (38) or retrieved from the NCBI genome database. BLAST (70) was used to align the B. pseudomallei ITS types (E, C, and G) against the assembled genomes. All of the alignments were manually inspected to determine the ITS types. Where BLAST results were ambiguous (because multiple ITS types were present in a single genome), short-read data were aligned against ITS types E, C, and G using SPANDx and alignments were visually inspected with Tablet v1.15.08.25 (71) to determine the ITS type(s) and their allelic abundance.
Virulence gene and accessory gene screening.
To assess the virulence potential of the five African strains, we developed an in silico virulence gene panel comprising all known B. pseudomallei virulence determinants (see reference 52 for a review). All of the genes in this panel are described in Table S2 in the supplemental material. The tBLASTn (72) algorithm was used to assess amino acid identity. BLAST matches were normalized by calculating the BSR (73) with B. pseudomallei K96243 as the control. A standard BSR cutoff of 0.70 was applied to call a virulence factor present; loci with scores below this cutoff were considered absent or highly variable. BRIG v0.95 (74) was used to visualize synteny and gene presence or absence across the genome.
Data availability.
The whole-genome short-read data generated in this study are available in the NCBI Sequence Read Archive under accession no. SRP067905. All of the ST profiles have been submitted to and are available in the B. pseudomallei MLST database (http://pubmlst.org/bpseudomallei).
ACKNOWLEDGMENTS
We sincerely thank Vanessa Theobald (Menzies School of Health Research) and Andriniana Rakotondrasoa (Bacteriology Unit, Institut Pasteur de Madagascar) for laboratory assistance. We are also grateful to Nana Ashmed Chèickh Bachirou, Traoré Ben Djibril Kiswendsida, and Traoré Mah Alima Esther (Clinical Research Unit of Nanoro) for laboratory data review and Jessica Maltha (Clinical Research Unit of Nanoro) for retrieval of clinical data.
D.S.S., B.J.C., and E.P.P. conceived and designed the experiments. D.S.S., B.G., B.D.S., P.L., M.C.T., and I.D. performed the experiments. D.S.S. and E.P.P. analyzed the data. D.S.S., B.G., B.D.S., M.K., M.M., P.V., J.J., P.L., M.C.T., H.T., I.D., B.C., B.J.C., and E.P.P. assisted with the collection of bacterial isolates and description and diagnoses of clinical cases and/or contributed materials/analysis tools. D.S.S. and E.P.P. wrote the paper. All of the authors read and approved the final manuscript.
REFERENCES
- 1.Wiersinga WJ, Currie BJ, Peacock SJ. 2012. Melioidosis. N Engl J Med 367:1035–1044. doi: 10.1056/NEJMra1204699. [DOI] [PubMed] [Google Scholar]
- 2.Wuthiekanun V, Dance DA, Wattanagoon Y, Supputtamongkol Y, Chaowagul W, White NJ. 1990. The use of selective media for the isolation of Pseudomonas pseudomallei in clinical practice. J Med Microbiol 33:121–126. doi: 10.1099/00222615-33-2-121. [DOI] [PubMed] [Google Scholar]
- 3.Hoffmaster AR, AuCoin D, Baccam P, Baggett HC, Baird R, Bhengsri S, Blaney DD, Brett PJ, Brooks TJ, Brown KA, Chantratita N, Cheng AC, Dance DA, Decuypere S, Defenbaugh D, Gee JE, Houghton R, Jorakate P, Lertmemongkolchai G, Limmathurotsakul D, Merlin TL, Mukhopadhyay C, Norton R, Peacock SJ, Rolim DB, Simpson AJ, Steinmetz I, Stoddard RA, Stokes MM, Sue D, Tuanyok A, Whistler T, Wuthiekanun V, Walke HT. 2015. Melioidosis diagnostic workshop, 2013. Emerg Infect Dis 21. doi: 10.3201/eid2102.141045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butler D. 2012. Viral research faces clampdown. Nature 490:456. doi: 10.1038/490456a. [DOI] [PubMed] [Google Scholar]
- 5.Dance DAB. 2015. Editorial commentary: melioidosis in Puerto Rico: the iceberg slowly emerges. Clin Infect Dis 60:251–253. doi: 10.1093/cid/ciu768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doker TJ, Sharp TM, Rivera-Garcia B, Perez-Padilla J, Benoit TJ, Ellis EM, Elrod MG, Gee JE, Shieh WJ, Beesley CA, Ryff KR, Traxler RM, Galloway RL, Haberling DL, Waller LA, Shadomy SV, Bower WA, Hoffmaster AR, Walke HT, Blaney DD. 2015. Contact investigation of melioidosis cases reveals regional endemicity in Puerto Rico. Clin Infect Dis 60:243–250. doi: 10.1093/cid/ciu764. [DOI] [PubMed] [Google Scholar]
- 7.Yip TW, Hewagama S, Mayo M, Price EP, Sarovich DS, Bastian I, Baird RW, Spratt BG, Currie BJ. 2015. Endemic melioidosis in residents of desert region after atypically intense rainfall in central Australia, 2011. Emerg Infect Dis 21:1038–1040. doi: 10.3201/eid2106.141908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Currie BJ, Dance DA, Cheng AC. 2008. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg 102(Suppl 1):S1–S4. doi: 10.1016/S0035-9203(08)70002-6. [DOI] [PubMed] [Google Scholar]
- 9.Currie BJ. 2015. Melioidosis: evolving concepts in epidemiology, pathogenesis, and treatment. Semin Respir Crit Care Med 36:111–125. doi: 10.1055/s-0034-1398389. [DOI] [PubMed] [Google Scholar]
- 10.Katangwe T, Purcell J, Bar-Zeev N, Denis B, Montgomery J, Alaerts M, Heyderman RS, Dance DA, Kennedy N, Feasey N, Moxon CA. 2013. Human melioidosis, Malawi, 2011. Emerg Infect Dis 19:981–984. doi: 10.3201/eid1906.120717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dodin A, Ferry R. 1974. Epidemiological studies of the bacillus of Whitmore in Africa. Bull Soc Pathol Exot Fil 67:121–126. [PubMed] [Google Scholar]
- 12.Wall RA, Mabey DCW, Corrah PT, Peters L. 1985. A case of melioidosis in West Africa. J Infect Dis 152:424–425. doi: 10.1093/infdis/152.2.424a. [DOI] [PubMed] [Google Scholar]
- 13.Morosini MI, Quereda C, Gil H, Anda P, Núñez-Murga M, Cantón R, López-Vélez R. 2013. Melioidosis in traveler from Africa to Spain. Emerg Infect Dis 19:1656–1659. doi: 10.3201/eid1910.121785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salam AP, Khan N, Malnick H, Kenna DT, Dance DA, Klein JL. 2011. Melioidosis acquired by traveler to Nigeria. Emerg Infect Dis 17:1296–1298. doi: 10.3201/eid1707.100502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuadros J, Gil H, Miguel JD, Marabé G, Gómez-Herruz TA, Lobo B, Marcos R, Anda P. 2011. Case report: melioidosis imported from West Africa to Europe. Am J Trop Med Hyg 85:282–284. doi: 10.4269/ajtmh.2011.11-0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garin B, Djaomazala I, Dubois-Cauwelaert N, Mahafaly, Raharimanga V, Ralison F, Herindrainy P, Andriamalala NC, Sarovich DS, Mayo M, Kaestli M, Currie BJ. 2014. Autochthonous melioidosis in humans, Madagascar, 2012 and 2013. Emerg Infect Dis 20:1739–1741. doi: 10.3201/eid2010.131524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borgherini G, Poubeau P, Paganin F, Picot S, Michault A, Thibault F, Berod CA. 2006. Melioidosis: an imported case from Madagascar. J Travel Med 13:318–320. doi: 10.1111/j.1708-8305.2006.00050.x. [DOI] [PubMed] [Google Scholar]
- 18.Borgherini G, Camuset G, Foucher A, Maiza JC, Thibault FM, Picot S, Poubeau P. 2015. The first autochthonous case of human melioidosis in Reunion Island. Med Mal Infect 45:47–49. doi: 10.1016/j.medmal.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Issack MI, Bundhun CD, Gokhool H. 2005. Melioidosis in Mauritius. Emerg Infect Dis 11:139–140. doi: 10.3201/eid1101.040605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corral DM, Coates AL, Yau YC, Tellier R, Glass M, Jones SM, Waters VJ. 2008. Burkholderia pseudomallei infection in a cystic fibrosis patient from the Caribbean: a case report. Can Respir J 15:237–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pérez J, Petiot A, Adjidé C, Gerry F, Goursaud R, Juminer B. 1997. First case report of melioidosis in Guadeloupe, a French West Indies archipelago. Clin Infect Dis 25:164–165. doi: 10.1086/516896. [DOI] [PubMed] [Google Scholar]
- 22.Biegeleisen JZ Jr., Mosquera R, Cherry WB. 1964. Case of human melioidosis; clinical, epidemiological and laboratory findings. Rev Ecuat Hig Med Trop 21:23–37. (In Spanish.) [PubMed] [Google Scholar]
- 23.Inglis TJ, Rolim DB, Sousa Ade Q. 2006. Melioidosis in the Americas. Am J Trop Med Hyg 75:947–954. [PubMed] [Google Scholar]
- 24.Rolim DB, Vilar DC, Sousa AQ, Miralles IS, de Oliveira DC, Harnett G, O’Reilly L, Howard K, Sampson I, Inglis TJ. 2005. Melioidosis, northeastern Brazil. Emerg Infect Dis 11:1458–1460. doi: 10.3201/eid1109.050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rolim DB, Rocha MF, Brilhante RS, Cordeiro RA, Leitão NP, Inglis TJ, Sidrim JJ. 2009. Environmental isolates of Burkholderia pseudomallei in Ceará State, northeastern Brazil. Appl Environ Microbiol 75:1215–1218. doi: 10.1128/AEM.01953-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dorman SE, Gill VJ, Gallin JI, Holland SM. 1998. Burkholderia pseudomallei infection in a Puerto Rican patient with chronic granulomatous disease: case report and review of occurrences in the Americas. Clin Infect Dis 26:889–894. doi: 10.1086/513928. [DOI] [PubMed] [Google Scholar]
- 27.Aardema H, Luijnenburg EM, Salm EF, Bijlmer HA, Visser CE, Van’t Wout JW. 2005. Changing epidemiology of melioidosis? A case of acute pulmonary melioidosis with fatal outcome imported from Brazil. Epidemiol Infect 133:871–875. doi: 10.1017/S0950268805004103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gétaz L, Abbas M, Loutan L, Schrenzel J, Iten A, Simon F, Decosterd A, Studer R, Sudre P, Michel Y, Merlani P, Emonet S. 2011. Fatal acute melioidosis in a tourist returning from Martinique island, November 2010. Euro Surveill 16 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19758. [PubMed] [Google Scholar]
- 29.Montúfar FE, Ochoa JE, Ortega H, Franco L, Montúfar MC, Monsalve A, Jaramillo C, Zapata M. 2015. Melioidosis in Antioquia, Colombia: an emerging or endemic disease? A cases series. Int J Infect Dis 37:50–57. doi: 10.1016/j.ijid.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention 2006. Imported melioidosis—South Florida, 2005. MMWR Morb Mortal Wkly Rep 55:873–876. [PubMed] [Google Scholar]
- 31.Benoit TJ, Blaney DD, Doker TJ, Gee JE, Elrod MG, Rolim DB, Inglis TJ, Hoffmaster AR, Bower WA, Walke HT. 2015. A review of melioidosis cases in the Americas. Am J Trop Med Hyg 93:1134–1139. doi: 10.4269/ajtmh.15-0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Limmathurotsakul D, Golding N, Dance DAB, Messina JP, Pigott DM, Moyes CL, Rolim DB, Bertherat E, Day NPJ, Peacock SJ, Hay SI. 2016. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol 1:15008. doi: 10.1038/nmicrobiol.2015.8. [DOI] [PubMed] [Google Scholar]
- 33.Pearson T, Giffard P, Beckstrom-Sternberg S, Auerbach R, Hornstra H, Tuanyok A, Price EP, Glass MB, Leadem B, Beckstrom-Sternberg JS, Allan GJ, Foster JT, Wagner DM, Okinaka RT, Sim SH, Pearson O, Wu Z, Chang J, Kaul R, Hoffmaster AR, Brettin TS, Robison RA, Mayo M, Gee JE, Tan P, Currie BJ, Keim P. 2009. Phylogeographic reconstruction of a bacterial species with high levels of lateral gene transfer. BMC Biol 7:78. doi: 10.1186/1741-7007-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dale J, Price EP, Hornstra H, Busch JD, Mayo M, Godoy D, Wuthiekanun V, Baker A, Foster JT, Wagner DM, Tuanyok A, Warner J, Spratt BG, Peacock SJ, Currie BJ, Keim P, Pearson T. 2011. Epidemiological tracking and population assignment of the non-clonal bacterium, Burkholderia pseudomallei. PLoS Negl Trop Dis 5:e1381. doi: 10.1371/journal.pntd.0001381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Engelthaler DM, Bowers J, Schupp JA, Pearson T, Ginther J, Hornstra HM, Dale J, Stewart T, Sunenshine R, Waddell V, Levy C, Gillece J, Price LB, Contente T, Beckstrom-Sternberg SM, Blaney DD, Wagner DM, Mayo M, Currie BJ, Keim P, Tuanyok A. 2011. Molecular investigations of a locally acquired case of melioidosis in southern AZ, USA. PLoS Negl Trop Dis 5:e1347. doi: 10.1371/journal.pntd.0001347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gee JE, Allender CJ, Tuanyok A, Elrod MG, Hoffmaster AR. 2014. Burkholderia pseudomallei type G in Western Hemisphere. Emerg Infect Dis 20:682–684. doi: 10.3201/eid2004.130960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liguori AP, Warrington SD, Ginther JL, Pearson T, Bowers J, Glass MB, Mayo M, Wuthiekanun V, Engelthaler D, Peacock SJ, Currie BJ, Wagner DM, Keim P, Tuanyok A. 2011. Diversity of 16S-23S rDNA internal transcribed spacer (ITS) reveals phylogenetic relationships in Burkholderia pseudomallei and its near-neighbors. PLoS One 6:e29323. doi: 10.1371/journal.pone.0029323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Smet B, Sarovich DS, Price EP, Mayo M, Theobald V, Kham C, Heng S, Thong P, Holden MT, Parkhill J, Peacock SJ, Spratt BG, Jacobs JA, Vandamme P, Currie BJ. 2015. Whole-genome sequencing confirms that Burkholderia pseudomallei multilocus sequence types common to both Cambodia and Australia are due to homoplasy. J Clin Microbiol 53:323–326. doi: 10.1128/JCM.02574-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Price EP, Sarovich DS, Smith EJ, MacHunter B, Harrington G, Theobald V, Hall CM, Hornstra HM, McRobb E, Podin Y, Mayo M, Sahl JW, Wagner DM, Keim P, Kaestli M, Currie BJ. 2016. Unprecedented melioidosis cases in northern Australia caused by an Asian Burkholderia pseudomallei strain identified by using large-scale comparative genomics. Appl Environ Microbiol 82:954–963. doi: 10.1128/AEM.03013-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen H, Xia L, Zhu X, Li W, Du X, Wu D, Hai R, Shen X, Liang Y, Cai H, Zheng X. 2015. Burkholderia pseudomallei sequence type 562 in China and Australia. Emerg Infect Dis 21:166–168. doi: 10.3201/eid2101.140156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barth AL, de Abreu E Silva FA, Hoffmann A, Vieira MI, Zavascki AP, Ferreira AG, da Cunha LG Jr., Albano RM, de Andrade Marques E. 2007. Cystic fibrosis patient with Burkholderia pseudomallei infection acquired in Brazil. J Clin Microbiol 45:4077–4080. doi: 10.1128/JCM.01386-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johnson SL, Bishop-Lilly KA, Ladner JT, Daligault HE, Davenport KW, Jaissle J, Frey KG, Koroleva GI, Bruce DC, Coyne SR, Broomall SM, Li PE, Teshima H, Gibbons HS, Palacios GF, Rosenzweig CN, Redden CL, Xu Y, Minogue TD, Chain PS. 2015. Complete genome sequences for 59 Burkholderia isolates, both pathogenic and near neighbor. Genome Announc 3:e00159-15. doi: 10.1128/genomeA.00159-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hurles ME, Sykes BC, Jobling MA, Forster P. 2005. The dual origin of the Malagasy in island Southeast Asia and East Africa: evidence from maternal and paternal lineages. Am J Hum Genet 76:894–901. doi: 10.1086/430051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dewar RE, Wright HT. 1993. The culture history of Madagascar. J World Prehist 7:417–466. doi: 10.1007/BF00997802. [DOI] [Google Scholar]
- 45.Burney DA, Burney LP, Godfrey LR, Jungers WL, Goodman SM, Wright HT, Jull AJ. 2004. A chronology for late prehistoric Madagascar. J Hum Evol 47:25–63. doi: 10.1016/j.jhevol.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 46.Yanagida T, Carod JF, Sako Y, Nakao M, Hoberg EP, Ito A. 2014. Genetics of the pig tapeworm in Madagascar reveal a history of human dispersal and colonization. PLoS One 9:e109002. doi: 10.1371/journal.pone.0109002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choy JL, Mayo M, Janmaat A, Currie BJ. 2000. Animal melioidosis in Australia. Acta Trop 74:153–158. doi: 10.1016/S0001-706X(99)00065-0. [DOI] [PubMed] [Google Scholar]
- 48.Ferry R, Poutrel B, Bruneau F. 1973. Isolation of Whitmore’s bacillus from lesions found in pigs from the Niamey slaughterhouse in Niger. Bull Soc Pathol Exot Filiales 66:42–45. (In French.) [PubMed] [Google Scholar]
- 49.Hampton V, Kaestli M, Mayo M, Choy JL, Harrington G, Richardson L, Benedict S, Noske R, Garnett ST, Godoy D, Spratt BG, Currie BJ. 2011. Melioidosis in birds and Burkholderia pseudomallei dispersal, Australia. Emerg Infect Dis 17:1310–1312. doi: 10.3201/eid1707.100707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reed KD, Meece JK, Henkel JS, Shukla SK. 2003. Birds, migration and emerging zoonoses: West Nile virus, Lyme disease, influenza A and enteropathogens. Clin Med Res 1:5–12. doi: 10.3121/cmr.1.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turner KM, Hanage WP, Fraser C, Connor TR, Spratt BG. 2007. Assessing the reliability of eBURST using simulated populations with known ancestry. BMC Microbiol 7:30. doi: 10.1186/1471-2180-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stone JK, DeShazer D, Brett PJ, Burtnick MN. 2014. Melioidosis: molecular aspects of pathogenesis. Expert Rev Anti Infect Ther 12:1487–1499. doi: 10.1586/14787210.2014.970634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dowling AJ, Wilkinson PA, Holden MT, Quail MA, Bentley SD, Reger J, Waterfield NR, Titball RW, Ffrench-Constant RH. 2010. Genome-wide analysis reveals loci encoding anti-macrophage factors in the human pathogen Burkholderia pseudomallei K96243. PLoS One 5:e15693. doi: 10.1371/journal.pone.0015693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lazar Adler NR, Stevens JM, Stevens MP, Galyov EE. 2011. Autotransporters and their role in the virulence of Burkholderia pseudomallei and Burkholderia mallei. Front Microbiol 2:151. doi: 10.3389/fmicb.2011.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schell MA, Lipscomb L, DeShazer D. 2008. Comparative genomics and an insect model rapidly identify novel virulence genes of Burkholderia mallei. J Bacteriol 190:2306–2313. doi: 10.1128/JB.01735-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sitthidet C, Stevens JM, Chantratita N, Currie BJ, Peacock SJ, Korbsrisate S, Stevens MP. 2008. Prevalence and sequence diversity of a factor required for action-based motility in natural populations of Burkholderia species. J Clin Microbiol 46:2418–2422. doi: 10.1128/JCM.00368-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sarovich DS, Price EP, Webb JR, Ward LM, Voutsinos MY, Tuanyok A, Mayo M, Kaestli M, Currie BJ. 2014. Variable virulence factors in Burkholderia pseudomallei (melioidosis) associated with human disease. PLoS One 9:e91682. doi: 10.1371/journal.pone.0091682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mukhopadhyay C, Kaestli M, Vandana KE, Sushma K, Mayo M, Richardson L, Tuanyok A, Keim P, Godoy D, Spratt BG, Currie BJ. 2011. Molecular characterization of clinical Burkholderia pseudomallei isolates from India. Am J Trop Med Hyg 85:121–123. doi: 10.4269/ajtmh.2011.11-0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boddey JA, Day CJ, Flegg CP, Ulrich RL, Stephens SR, Beacham IR, Morrison NA, Peak IR. 2007. The bacterial gene lfpA influences the potent induction of calcitonin receptor and osteoclast-related genes in Burkholderia pseudomallei-induced TRAP-positive multinucleated giant cells. Cell Microbiol 9:514–531. doi: 10.1111/j.1462-5822.2006.00807.x. [DOI] [PubMed] [Google Scholar]
- 60.DeShazer D, Brett PJ, Woods DE. 1998. The type II O-antigenic polysaccharide moiety of Burkholderia pseudomallei lipopolysaccharide is required for serum resistance and virulence. Mol Microbiol 30:1081–1100. doi: 10.1046/j.1365-2958.1998.01139.x. [DOI] [PubMed] [Google Scholar]
- 61.Price EP, Sarovich DS, Mayo M, Tuanyok A, Drees KP, Kaestli M, Beckstrom-Sternberg SM, Babic-Sternberg JS, Kidd TJ, Bell SC, Keim P, Pearson T, Currie BJ. 2013. Within-host evolution of Burkholderia pseudomallei over a twelve-year chronic carriage infection. mBio 4:e00388-00313. doi: 10.1128/mBio.00388-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rossi C. 3 May 2013. Melioidosis—Belgium ex Madagascar. ProMED-mail. http://www.promedmail.org. Accessed 29 December 2015.
- 63.McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, Garimella K, Altshuler D, Gabriel S, Daly M, DePristo MA. 2010. The genome analysis toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res 20:1297–1303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Godoy D, Randle G, Simpson AJ, Aanensen DM, Pitt TL, Kinoshita R, Spratt BG. 2003. Multilocus sequence typing and evolutionary relationships among the causative agents of melioidosis and glanders, Burkholderia pseudomallei and Burkholderia mallei. J Clin Microbiol 41:2068–2079. doi: 10.1128/JCM.41.5.2068-2079.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Currie BJ, Gal D, Mayo M, Ward L, Godoy D, Spratt BG, LiPuma JJ. 2007. Using BOX-PCR to exclude a clonal outbreak of melioidosis. BMC Infect Dis 7:68. doi: 10.1186/1471-2334-7-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huang W, Li L, Myers JR, Marth GT. 2012. ART: a next-generation sequencing read simulator. Bioinformatics 28:593–594. doi: 10.1093/bioinformatics/btr708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Holden MT, Titball RW, Peacock SJ, Cerdeño-Tárraga AM, Atkins T, Crossman LC, Pitt T, Churcher C, Mungall K, Bentley SD, Sebaihia M, Thomson NR, Bason N, Beacham IR, Brooks K, Brown KA, Brown NF, Challis GL, Cherevach I, Chillingworth T, Cronin A, Crossett B, Davis P, DeShazer D, Feltwell T, Fraser A, Hance Z, Hauser H, Holroyd S, Jagels K, Keith KE, Maddison M, Moule S, Price C, Quail MA, Rabbinowitsch E, Rutherford K, Sanders M, Simmonds M, Songsivilai S, Stevens K, Tumapa S, Vesaratchavest M, Whitehead S, Yeats C, Barrell BG, Oyston PC, Parkhill J. 2004. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc Natl Acad Sci U S A 101:14240–14245. doi: 10.1073/pnas.0403302101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li H, Durbin R. 2009. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Swofford DL. 2003. PAUP*. Phylogenetic analysis using parsimony (*and other methods), V 4.0b10. Sinauer Associates, Sunderland, MA. [Google Scholar]
- 70.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. 1990. Basic local alignment search tool. J Mol Biol 215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 71.Milne I, Bayer M, Cardle L, Shaw P, Stephen G, Wright F, Marshall D. 2010. Tablet—next generation sequence assembly visualization. Bioinformatics 26:401–402. doi: 10.1093/bioinformatics/btp666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Altschul SF, Madden TL, Schäffer AA, Zhang J, Zhang Z, Miller W, Lipman DJ. 1997. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res 25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rasko DA, Myers GS, Ravel J. 2005. Visualization of comparative genomic analyses by BLAST score ratio. BMC Bioinformatics 6:2. doi: 10.1186/1471-2105-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alikhan N-F, Petty NK, Ben Zakour NL, Beatson SA. 2011. BLAST Ring Image Generator (BRIG): simple prokaryote genome comparisons. BMC Genomics 12:402. doi: 10.1186/1471-2164-12-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sarovich DS, Price EP. 2014. SPANDx: a genomics pipeline for comparative analysis of large haploid whole genome re-sequencing datasets. BMC Res Notes 7:618. doi: 10.1186/1756-0500-7-618. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Complete list of B. pseudomallei isolates used in this study. Download Table S1, XLSX file, 0.02 MB (20.1KB, xlsx) .
Copyright © 2016 Sarovich et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Virulence gene heat map of all of the B. pseudomallei isolates included in this study. Download Table S2, XLSX file, 0.1 MB (119.1KB, xlsx) .
Copyright © 2016 Sarovich et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
African and South American isolates in the B. pseudomallei MLST database and their corresponding allele profiles. Download Table S3, XLSX file, 0.01 MB (12.3KB, xlsx) .
Copyright © 2016 Sarovich et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Data Availability Statement
The whole-genome short-read data generated in this study are available in the NCBI Sequence Read Archive under accession no. SRP067905. All of the ST profiles have been submitted to and are available in the B. pseudomallei MLST database (http://pubmlst.org/bpseudomallei).