Abstract
We examined effects of prices of fast foods (FF) and fruits and vegetables (FV) on dietary intake, body mass index (BMI) and obesity risks and whether the associations varied across groups according to their family income. Data from the US Department of Agriculture Continuing Survey of Food Intakes by Individuals (CSFII, 1994–96) for 7,331 individuals aged 20–65 years with complete data on two 24-hr recalls were used. We computed two food price indices (FFPI and FVPI) which were linked to individuals through geocoded identifiers. Main outcomes included dietary intakes of energy, selected nutrients and food groups, fast food consumption, and diet quality measured using two indices (HEI and aMED), BMI and obesity. Interaction terms between key variables were tested in regression analyses and in further stratified analysis by family income. Higher fast food prices (FFPI) were associated with higher, fiber intake, low saturated fat, and better overall diet quality as measured by aMED. FVPI was positively associated with improved dietary quality as well in terms of lower cholesterol and sodium intakes, improved HEI and lower BMI. Most of these associations showed homogeneous strengths across income groups as evidenced by a non-significant FFPI*PIR or FVPI*PIR interaction term (p<0.10). While increasing FFPI by one standard deviation was only borderline protective against FF consumption (OR=0.89; 95% CI: 0.78, 1.02), its association with other binary outcomes that were considered was non-significant. In contrast, FVPI was protective against obesity, particularly among the near poor. It was also associated with improved aMED score (OR: 2.22; 95% CI: 1.22, 4.03). Analyses of these national data suggest that changing fast food and fruit and vegetable prices may affect people’s dietary quality and to some extent their adiposity, although the present study is limited by the available food price data.
Keywords: food prices, dietary intake, dietary quality, fast food consumption, family income
INTRODUCTION
Obesogenic environments promoting excessive food consumption coupled with sedentary lifestyles are primary suspects for the current obesity epidemic in the United States and many other industrialized countries (French, Story, & Jeffery, 2001b). Consumption of energy dense foods, frequent meal consumption, high intake of fat and low intake of fiber was found to be associated with increased risk of overweight and obesity (Howarth, Huang, Roberts, Lin, & McCrory, 2006; Howarth, Huang, Roberts, & McCrory, 2005; Howarth, Murphy, Wilkens, Hankin, & Kolonel, 2006). Moreover, food choice is thought to be influenced by a number of environmental and individual factors. Environmental factors may include the changing nature of food supply, food advertising, marketing and promotion as well as food prices (Popkin, Duffey, & Gordon-Larsen, 2005). Controlling for individual factors that may determine food preferences, such as age, sex, ethnicity, education, and income, food prices can also act on food choice by changing the relative prices of certain types of foods with marked consequences on diet quality, a pattern hypothesized to be more salient among the poor segment of the population. In addition, studies have shown that lower income was associated with poorer dietary quality (Darmon, Ferguson, & Briend, 2003; Darmon, Ferguson, & Briend, 2002).
Whereas many of the studies conducted addressed quality of the diet consumed and its associated costs (Andrieu, Darmon, & Drewnowski, 2006; Cade, Upmeier, Calvert, & Greenwood, 1999; Darmon, Briend, & Drewnowski, 2004; Darmon, Ferguson, & Briend, 2006; Drewnowski, 2003, 2004; Drewnowski & Darmon, 2005a, b; Jetter & Cassady, 2006; Schroder, Marrugat, & Covas, 2006), few have looked at the effect of food prices as an environmental factor operating at the institutional (e.g. schools) or neighborhood level on food purchasing behavior and dietary intake (French, 2005; French, Jeffery, Story, Breitlow, Baxter, Hannan et al., 2001a; French, Story, Jeffery, Snyder, Eisenberg, Sidebottom et al., 1997; Jeffery, French, Raether, & Baxter, 1994; Lakdawalla, Philipson, & Bhattacharya, 2005; Powell, Auld, Chaloupka, O'Malley, & Johnston, 2007a). For example, one intervention study (The CHIPS study) found that price reductions in vending machines at schools and work settings (of 10%, 25% and 50%) increased low-fat snack sales by 9%, 39% and 93%, respectively (French et al., 2001a). Another study showed that when fresh fruits and baby carrots were reduced in price by 50%, their sales increased by four-fold and two-fold, respectively. Sales returned to baseline with the reinstatement of usual prices (French et al., 1997). A recent cross-sectional study suggested local area prices of fast foods and fruits and vegetables may influence healthy eating behaviors among adolescents (Powell et al., 2007a).. Based on the Third National Health and Nutrition Examination Survey (NHANES III 1988–94) data, a recent study found that local area relative prices of certain foods were significantly associated with several nutrient deficits: higher prices for peaches and orange juice were associated with vitamin-C deficiency, higher orange juice prices were associated with folate deficiency and higher ground beef prices were associated with anemia (Lakdawalla et al., 2005).
No published studies to our knowledge, however, have examined local area fast food pricing effects on American adults’ dietary intake. In addition, several recent studies suggest that food prices are significantly associated with BMI and/or obesity status among children (Sturm & Datar, 2005), adolescents (Powell et al., 2007a) and adults (Chou, Grossman, & Saffer, 2004), suggesting that increasing prices of fast foods and/or reducing those of fruits and vegetables may lower BMI and/or the rates of obesity in various age groups. However, none of these studies examined whether family income affects these associations, and none assessed food price impacts on overall diet quality or fast food consumption.
Our current study aimed to examine the effects of prices of “fast foods (FF)” and “fruits and vegetables (FV)” on dietary intakes (including energy, nutrients, food groups, and overall diet quality and fast food consumption). In addition, we examined the association between these food prices and BMI and risk of obesity, though these were only secondary objectives due to the limitations of available anthropometric measures. Further we studied the differences in these associations across family income categories.
MATERIALS AND METHODS
Study Design and Subjects
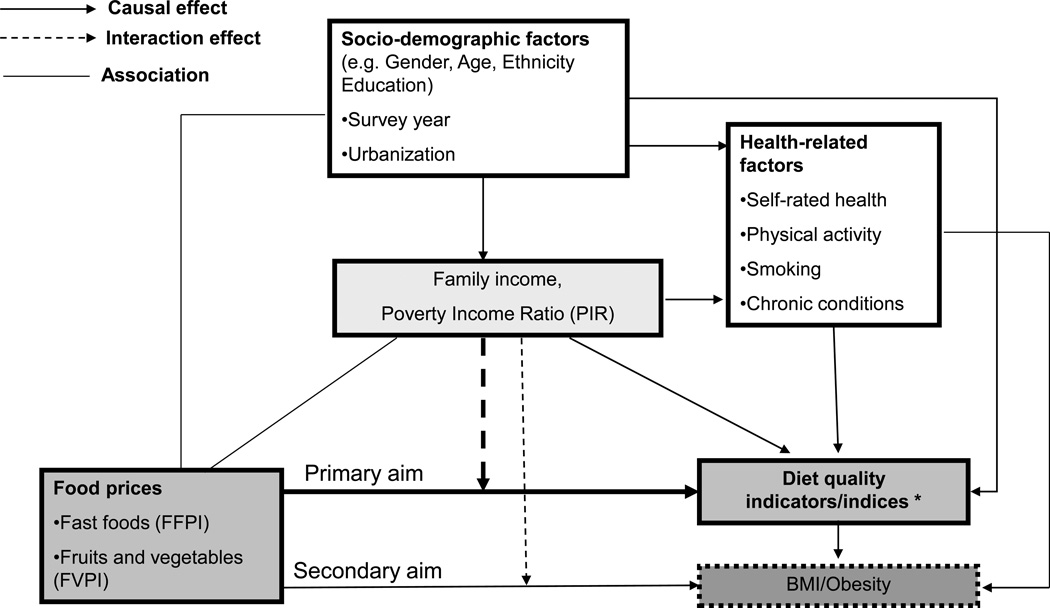
Figure 1 presents the conceptual model used in our analyses. This study undertook empirical analyses to examine the effects of FF and FV prices on overall dietary quality, nutrient intakes, FV and FF consumption, and BMI and obesity prevalence. We hypothesized that increased prices of FF have a positive (i.e., desirable) effect on dietary intakes and are reversely associated with risk of obesity, while these same effects are anticipated for reduced prices of FV. We suspect that these associations were more pronounced among the lower incomes group, who may be more price-sensitive.
Figure 1.
Analyses were undertaken using nationally representative data from the US Department of Agriculture (USDA) Continuing Survey of Food Intakes by Individuals (CSFII) 1994–96 (US Department of Agriculture, 1994–96). A multi-stage stratified sample of 16,103 non-institutionalized persons aged 0 to 90 years residing in the United States contained information about dietary intake (by one or two nonconsecutive, multiple-pass 24-hour recalls that were 3 to 10 days apart), socioeconomic, demographic and health parameters. Demographic, socio-economic and lifestyle variables were available for all individuals who participated in the CSFII survey.
Among the 16,103 respondents of all ages who completed the CSFII 1994–96, 9,872 were 20 years or older and had complete data on day 1 of recall. We further excluded those over the age of 65 years (n=2,127), to ensure relatively healthy individuals with no special dietary needs being selected. We also excluded those who completed only one 24-hour dietary recall (n=414). This resulted in a final sample of 7,331 individuals (3,721 men and 3,610 women).
Measures
1) Outcome variables
Dietary intakes and dietary quality indicators
Dietary intake was elicited from subjects participating in the CSFII 1994–96 survey using two 24-hour dietary recalls. Based on responses which uncovered types of foods consumed during these two days along with their portion sizes, nutrient intake was estimated using food composition tables that were designed specifically to be used for this survey. Moreover, the foods consumed were grouped into broader categories. Average dietary intakes of foods and nutrients from the two-day 24-hour recalls were considered. Indicators considered included energy, total fat and saturated fat intake (as percent of total calories), sodium, cholesterol and sugar, the excess of which are believed to reduce diet quality. We also considered intake of FV (grams), fiber (grams), dairy products (grams) and calcium (grams), adequate intake of which are believed to improve diet quality.
Diet quality indices (DQI)
To assess the overall quality of diet, we applied two widely known diet quality indices, namely the USDA’s Health Eating Index (HEI) (McCullough, Feskanich, Rimm, Giovannucci, Ascherio, Variyam et al., 2000) and the Alternate Mediterranean Diet Score (aMED) (Trichopoulou, Costacou, Bamia, & Trichopoulos, 2003; Trichopoulou, Kouris-Blazos, Wahlqvist, Gnardellis, Lagiou, Polychronopoulos et al., 1995). Whereas HEI is measured on a scale of 0 to 100, aMED may range from 0 to 10. Appendix A shows the criteria for scoring points on each of these two indices. For many of the food group criteria, serving estimates rather than grams were used as made available by the USDA. A HEI and aMED score was calculated for each subject, respectively. Our analysis shows a moderate agreement between the HEI and aMED scores, with a spearman correlation r=0.50 (P<0.05), a kappa=0.15 (P<0.05) and percent agreement of 32.2% (>expected agreement by chance of 20%) for age- and gender-specific quintiles. HEI and aMED were used as continuous outcomes, but in another part of our analysis, the upper quintile (80th percentile) was used to indicate “good” diet quality.
Fast food consumption indices (FFCI)
Two FF consumption indices were computed based on the average intake of foods: a) a FFCI count index consisting of the sum of all food items that were reported to be consumed at a FF restaurant, including beverages; and b) a FFCI binary index of consuming (=1) vs. not consuming (=0) the items included in the count index over the two 24-hr recall periods.
Body Mass Index (BMI) and weight status
Information on self-reported weight and height was collected in the CSFII. BMI was calculated as weight (kg)/height(m)2. Obesity was defined as BMI≥30kg/m2. Note that although some research suggests that such self-reported measures are valid and widely used in epidemiologic studies (Ajani, Lotufo, Gaziano, Lee, Spelsberg, Buring et al., 2004; Freedman, Ron, Ballard-Barbash, Doody, & Linet, 2006), others show that they are prone to measurement error, usually underreporting in weight (Kuczmarski, Kuczmarski, & Najjar, 2001; Wang, Patterson, & Hills, 2002).
2) Primary exposure variables: Price of foods
Food price data were obtained from the American Chamber of Commerce Researchers Association (ACCRA) Cost of Living Index reports that contained quarterly information on prices across more than 300 US cities annually. The ACCRA collected 62 different prices across a range of products. Price data, which were based on establishment samples, reflected a mid-management standard of living. For consistency, national brands were stipulated where possible. Otherwise, “lowest price” was specified and was the average of the lowest prices found in all stores surveyed. In the CSFII 1994–96, there was an initial sampling of 62 PSUs out of the 1,404 PSUs that were created for all of the United States. Price data were matched to the CSFII sample based on the closest city match available in the ACCRA data using MSA/county geocode data provided for the CSFII data corresponding to the sampled PSUs and was also dependent on the survey year in which each subject was selected (n=62 PSUs*3years=186 possible values per food price in the dataset).
We generated three match indicators for the quality of the food price geocode match (nearest ACCRA city was within the CSFII household’s MSA/county vs. next contiguous county or other county). In all regression models, we accounted for the quality of the price match by including dummy variable match indicators and interactions of the match indicators with the two food prices in order to isolate price effects for the exact within MSA/county geocode match. For each year, the price data were averaged across quarters 1 through 4. Hence, food prices were matched with CSFII based on geocode and survey year. From the items provided in the ACCRA data, we created two price indices: a fruit and vegetable price index (FVPI) and a fast food price index (FFPI).
Fruit and vegetable price index (FVPI)
The FVPI was based on prices collected in the following food categories: potatoes, bananas, lettuce, sweet peas, tomatoes, peaches and frozen corn. ACCRA reported weights for each item based on expenditure shares derived from the Bureau of Labor Statistics (BLS) Consumer Expenditure Survey. We used these weights to compute a weighted FVPI based on the seven food items noted above. The price was also deflated by the BLS Consumer Price Index (CPI) (1982–1984=1).
Fast food price index (FFPI)
The FFPI was based on the following three items included in the ACCRA data: a) a McDonald’s Quarter Pounder with cheese, b) a thin crust regular cheese pizza at Pizza Hut and/or Pizza Inn, and c) fried chicken (thigh and drumstick) at Kentucky Fried Chicken and/or Church’s Fried Chicken. The FFPI was computed as an average of these three food prices since they have equal weights. The FFPI was also deflated by the CPI.
3) Covariates and potential confounders
Poverty Income ratio (PIR)
PIR (as a percentage of poverty line) was considered as a confounder while conducting the multivariate regression analyses for the total population and an effect modifier in the stratified analysis. As a percentage of the poverty line, it was categorized as 0–130 (poor: food stamp eligible) (Siega-Riz, Kranz, Blanchette, Haines, Guilkey, & Popkin, 2004), 131–299 (near poor), and 300 or more (not poor). While SES is usually conceptualized with several measures (including education and occupation), we focused on the financial aspect of SES for the purpose of this study. However, a sensitivity analysis was done to look at potential effect modification by education (<High School (HS), HS, >HS), controlling for PIR. Another sensitivity analysis assessed effect modification by presence or absence of chronic diseases.
Other covariates
Additional control covariates included age, gender, and ethnicity (Non-Hispanic Whites, Non-Hispanic black, Hispanic, Other), years of education attained, degree of urbanization of the geographical area in which households were selected (i.e., Metropolitan Statistical Area-central city, MSA- suburban, and rural). We also considered dummy variables for year of the survey. In addition, we considered individual-level lifestyle and health factors, which were adjusted in all models. These lifestyle variables included two binary variables: current smoking status and low physical activity (response of “rarely or never” on the question: “How often do you exercise vigorously enough to work up a sweat?”). Self-rated and doctor-rated health based on the following questions was used: (A) In general, would you say that your health is: (1) excellent, (2) very good, (3) good, (4) fair, (5) poor; (B) Has a doctor ever told you that you have any of these conditions? (diabetes, high blood pressure, heart disease, cancer, osteoporosis, high blood cholesterol, stroke). This variable was measured on a scale of 0 to 2 (0: none; 1: one chronic condition; 2: two or more) and was included as two dummy variables in the models.
Statistical Analysis
First, we described the characteristics of the study sample taking into account the complex sampling design for variance estimation. In particular, we accounted for stratification by geographic location, degree of urbanization, and socioeconomic characteristics. We used sampling weights that compensate for variable probabilities of selection, differential response rates, and possible deficiencies in the sampling frame. Failure to account for sample design tends to yield underestimated standard errors of parameters, and hence increases the risk of rejecting true null hypotheses. Differences in means between groups were tested using ANOVA and t-tests. Associations between categorical variables were tested using χ2 tests.
Multivariate linear regression analyses were conducted to test the effects of the price indices (FFPI and FVPI) on our continuous outcomes (dietary intakes and quality, and BMI). Further, in the case of FFCI, a count model was estimated. Poisson regression was attempted first and the deviance goodness of fit statistic for over-dispersion was estimated. Given that it was highly significant, a more conservative model was used, namely the negative-binomial model, which does not have the assumption of mean count being equal to its variance, as is the case in the poisson model. In addition, stratified analyses were carried out to test whether these associations varied across income categories. Design complexity was taken into account using STATA survey-related commands and specifying PSUs, strata and weights. Control for all potential confounders described earlier was done, with both food prices (FFPI and FVPI) included in all models. Effect modification by PIR was concluded based on a statistically significant interaction term between food price indices (FVPI and FFPI) or FPIj×PIR introduced into the model. In all tests, a p-value < 0.05 was considered as statistically significant. However, regarding interaction terms, we used p <0.1 due to their lower power compared to main effects in the models (Selvin, 2004). For binary outcome variables, logistic regression models were run controlling for the same confounding variables and stratifying for PIR in part of the analysis. Price indices were transformed and entered as standardized z-scores in all logistic models, to enhance comparability and for ease of interpretation. Our analysis controlled for region in addition to survey year and other potential confounders to assess the extent to which unobserved determinants of food consumption intake and weight outcomes across regions may bias our results. All analyses were conducted using STATA release 9.0 (STATA, 2005).
RESULTS
Characteristics of study population
Table 1 shows characteristics of our full study population and by PIR category. Overall, study subjects had a mean age of 39.8 (± 0.25), 13.3 (± 1.0) years of education, 51% were female, 74% were non-Hispanic white, the highest proportion lived in the South (36%), and 47% lived in suburban areas. Close to one third had low physical activity, 27% were current smokers, 12% reported their health as being fair or poor and 29% reported at least one chronic condition. Average BMI was in the overweight range (26.1±0.1) and the overall prevalence of obesity was 18.2%. Mean HEI and aMED were 63.1 (range: 21–99) and 3.5 (range:0–9), respectively. On average, subjects consumed 2.49 items over a period of 48-hours from a FF restaurant. 46.4% of study subjects reported consuming at least one FF item over that same period.
Table 1.
Characteristics of study population by category of poverty income ratio (PIR); CSFII 1994–96
| All | Poverty Income Ratio (PIR)a |
|||
|---|---|---|---|---|
|
0–130 Poor |
131–299 Near Poor |
300+ Non-poor |
||
| N=7,331 | N=1,616 | N=2,713 | N=3,002 | |
| (proportion ± SEM) | ||||
| Age (years) | ||||
| 20–34 | 37.6±0.8 | 51.9±2.8 | 41.4±1.3 | 29.7±1.1* |
| 35–54 | 47.4±0.7 | 35.8±2.5 | 44.2±1.1 | 53.8±1.2 |
| 55–65 | 15.0±0.6 | 12.3±1.0 | 14.3±0.8 | 16.5±0.9 |
| Female | 51.0±0.7 | 58.4±2.6 | 50.7±0.7 | 48.9±0.9* |
| Ethnicity | ||||
| Non-Hispanic white | 74.0±2.0 | 48.7±4.2 | 71.3±2.9 | 84.3±1.3* |
| Non-Hispanic black | 11.4±1.1 | 22.3±3.5 | 13.3±2.1 | 6.3±0.6 |
| Hispanic | 10.1±1.7 | 22.8±3.5 | 10.8±2.2 | 5.3±1.0 |
| Other | 4.5±0.5 | 6.1±1.1 | 4.5±0.7 | 4.0±0.7 |
| Region | ||||
| Northeast | 19.3±2.0 | 20.3±3.3 | 16.8±1.9 | 21.1±2.6 |
| Midwest | 22.2±1.0 | 20.2±1.8 | 22.0±1.1 | 23.1±1.5 |
| South | 36.0±2.7 | 33.2±3.3 | 39.3±3.3 | 34.0±3.3 |
| West | 22.4±2.5 | 26.3±2.7 | 21.8±2.8 | 21.7±3.1 |
| Urbanization | ||||
| MSA-inner city | 32.9±1.8 | 43.4±3.4 | 33.6±2.1 | 29.0±2.5* |
| MSA-suburbs | 46.6±1.8 | 30.2±2.7 | 42.3±2.0 | 55.6±2.6 |
| Rural | 20.4±1.1 | 26.4±2.4 | 24.1±1.6 | 15.4±1.6 |
| Current smoker | 27.1±0.6 | 36.8±2.6 | 30.0±1.1 | 21.6±1.1* |
| Low physical activity | 32.6±0.9 | 40.5±2.0 | 33.8±1.2 | 28.9±1.4* |
| Self-rated health | ||||
| Excellent | 25.3±0.8 | 18.3±1.6 | 24.1±1.2 | 28.5±1.2* |
| Very good | 34.7±1.0 | 23.0±1.7 | 35.8±1.8 | 37.5±1.0 |
| Good | 28.0±0.7 | 33.2±1.4 | 27.7±1.1 | 26.5±0.9 |
| Fair | 9.7±0.4 | 18.8±1.1 | 10.0±0.9 | 6.5±0.6 |
| Poor | 2.3±0.2 | 6.6±0.9 | 2.3±0.3 | 1.0±0.2 |
| Number of Chronic conditions | ||||
| None | 71.6±0.9 | 69.3±1.4 | 73.8±1.0 | 70.6±1.2* |
| One | 18.8±0.7 | 18.7±1.2 | 17.5±0.8 | 20.1±0.9 |
| Two or more | 9.5±0.5 | 12.0±0.9 | 9.4±0.8 | 9.4±0.8 |
| Body Mass Index ≥30 kg/m2 | 18.2±0.7 | 23.9±1.6 | 18.2±1.0 | 16.4±0.9* |
| (Mean±SEM) | ||||
| Education (years) | 13.3±1.0 | 11.4±0.2 | 12.8±0.1 | 14.3±0.1* |
| Diet quality indicesb | ||||
| Healthy Eating Index (HEI) | 63.1±0.2 | 59.0±0.6 | 62.1±0.3 | 65.2±0.2* |
| Alternative Mediterranean Diet Score (aMED) |
3.5±0.0 | 3.0±0.1 | 3.4±0.0 | 3.8±0.0* |
| Body Mass Index (kg/m2) | 26.1±0.1 | 26.8±0.2 | 26.0±0.2 | 25.9±0.1* |
| Fast food consumption indexc | ||||
| Count index over 48-hrs | 2.49±0.10 | 2.59±0.44 | 2.46±0.11 | 2.48±0.11* |
| Binary index over 48-hrs | 46.4±1.08 | 40.17±1.83 | 47.76±1.36 | 47.19±1.53* |
| Food price indices ($) | ||||
| FFPI | 2.770±0.017 | 2.801±0.019 | 2.757±0.019 | 2.770±0.017* |
| Range | 2.249, 3.213 | |||
| FVPI | 0.725±0.007 | 0.728±0.009 | 0.722±0.007 | 0.727±0.007* |
| Range | 0.570, 0.952 | |||
P<0.05 for design-based χ2 test for categorical variables or ANOVA test for continuous variables.
Poverty income ratio is computed as percentage of poverty line. It was categorized as 0–130 (poor: food stamp eligible (Siega-Riz et al., 2004), 131–299 (medium SES), and 300 or more (High SES).
See Appendix A for more details about computations of diet quality indices.
The count index consisted of number of food items consumed at fast food restaurants over the two 24-hr recall period. The binary index (% yes) is the proportion of subjects who reported consuming at least one items at a fast food restaurant during that period.
In general, subjects in non-poor PIR categories compared to the lowest level tended to be older, male, non-Hispanic White, living in the suburbs or highly educated. In addition, lower proportions were current smokers, had a low physical activity level, reported fair or poor health, or listed two or more chronic conditions. Obesity prevalence was lowest in the non-poor and the same was observed for BMI and the two diet quality indices (HEI and aMED). Among the poorest income category (PIR<130), a higher consumption level at FF restaurants was observed when compared to the other categories (count index). However, the binary index exhibited a different pattern whereby a higher proportion among the middle and non-poor categories reported foods eaten at FF restaurants compared to the lowest PIR category. Finally, food price indices varied across PIR groups, with the poorest categories being exposed to the highest prices and the middle category to the lowest. All associations, except for that between FFCI and PIR, were statistically significantly different across PIR (p<0.05).
Multivariate linear associations between food prices and study outcomes
Table 2 shows the results from the multivariate linear and negative binomial regression analyses for the effect of the two price indices (FFPI and FVPI) on diet quality indicators and other outcomes considered for total population as well as stratified by PIR. Our finding for the total population suggested that increasing FFPI by $1 was associated with a drop in percent saturated fat from total energy intake by 1.1 percentage points, an increase in fiber intake by 2.8 grams per day as well as an increased in aMED score by 0.49 points (out of 10) (p<0.05). The association between FFPI and fiber intake was stronger and statistically significant only among the near poor though FFPI*PIR did not indicate effect modification by income (p>0.10). The relationship between FFPI and aMED was in contrast stronger among the poor, with a significant FFPI*PIR interaction term. However, none of the stratum-specific associations in that case were significant (p>0.05). Unexpectedly, higher FVPI were also associated with improved dietary quality in the total adult population. In fact, every $1 increase in FVPI was associated with 1777 mg. lower sodium consumption, 141 mg. lower cholesterol intake, as well as 10.8 points more on the HEI overall diet quality index. Unlike FFPI, $1 increase in FVPI was associated with a significant reduction in BMI (β=-3.9, p<0.05).
Table 2.
Multivariate linear and negative binomialc regression modelsa of the effect of fast food and fruits and vegetables price indices on diet quality indicators and indices and on fast food consumption indices, stratified by poverty income ratio (PIR) (N=7,331); CSFII 1994–96
| All PIR groups | Poverty Income Ratio (PIR) | |||||||
|---|---|---|---|---|---|---|---|---|
| 0–130 Poor |
131–299 Near poor |
300+ Non-poor |
||||||
| N=7,331 | N=1,616 | N=2,713 | N=3,002 | |||||
| Beta (SEE) | ||||||||
|
Diet quality indicators |
||||||||
| Energy (kcal/d) | ||||||||
| FFPI | 55.8 | (137.5) | 217.9 | (225.0) | 178.3 | (213.0) | −107.6 | (144.2) |
| FVPI | −669.2 | (438.7) | 848.6 | (963.2) | −608.8 | (582.4) | −815.5 | (346.7)* |
| Fat (% kcal) | ||||||||
| FFPI | −2.2 | (1.4) | −1.7 | (2.2) | −2.0 | (2.4) | −2.5 | (1.5) |
| FVPI | −4.5 | (4.1) | −6.7 | (6.6) | −9.2 | (6.4) | 1.0 | (4.4) |
|
Saturated fat (% kcal) |
||||||||
| FFPI | −1.1 | (0.5)* | −0.7 | (1.2) | −1.3 | (0.9) | −1.0 | (0.5) |
| FVPI | −2.4 | (1.6) | −1.8 | (3.3) | −5.4 | (2.5)* | −0.7 | (1.8) |
| Cholesterol (mg/d) | ||||||||
| FFPI | 16.6 | (26.5) | 55.6 | (50.3) | 29.4 | (54.1) | −0.45 | (27.4) |
| FVPI | −141.4 | (67.6)* | 76.5 | (183.4) | −201.4 | (172.9) | −143.5 | (69.5) |
| Sodium (mg/d) | ||||||||
| FFPI | 15.1 | (252.0) | 374.7 | (522.7) | 65.0 | (428.4) | −66.4 | (290.7) |
| FVPI | −1777.4 | (804.1)* | 1491.9 | (2207.4) | −1624.1 | (1152.0) | −2254.8 | (728.5)* |
| Sugar (g/d) | ||||||||
| FFPI | 5.1 | (6.7) | 26.7 | (15.4) | 5.4 | (7.5) | −1.6 | (9.5) |
| FVPI | −28.1 | (20.3) | 18.2 | (48.2) | −20.3 | (23.1) | −37.1 | (24.4)d |
| Dairy products (g/d) | ||||||||
| FFPI | 4.1 | (39.3) | 51.8 | (64.2) | −5.2 | (56.2) | 4.6 | (43.3) |
| FVPI | −129.1 | (118.1) | −75.3 | (195.5) | −132.7 | (150.9) | −129.7 | (108.4) |
| Calcium (mg/d) | ||||||||
| FFPI | −13.7 | (68.9) | 144.3 | (131.1) | 29.1 | (109.1) | −80.1 | (84.7) |
| FVPI | −292.2 | (233.5) | 290.0 | (484.4) | −227.5 | (282.1) | −384.3 | (208.2) |
| Fiber (g/d) | ||||||||
| FFPI | 2.8 | (1.1)* | 1.3 | (3.3) | 5.7 | (1.9)* | 0.7 | (1.6) |
| FVPI | −1.7 | (3.9) | 18.0 | (7.5)* | −5.1 | (5.7) | −1.1 | (4.3) |
|
Fruits and Vegetables (g/d) |
||||||||
| FFPI | 43.7 | (38.8) | −54.8 | (84.8) | 80.4 | (63.6) | 42.4 | (44.6) |
| FVPI | 96.6 | (99.1) | 363.3 | (254.8) | 172.8 | (138.5) | 9.6 | (110.8) |
| Diet quality indicesb | ||||||||
| HEI | ||||||||
| FFPI | 3.16 | (1.53) | −0.2 | (3.9) | 4.3 | (2.6) | 2.9 | (1.7) |
| FVPI | 10.77 | (5.08)* | 7.0 | (8.9) | 14.9 | (8.3) | 10.2 | (6.4) |
| aMED | ||||||||
| FFPI | 0.49 | (0.22)* | 0.7 | (0.5) | 0.4 | (0.3) | 0.4 | (0.3)d |
| FVPI | 0.41 | (0.84) | 1.5 | (1.2) | 0.08 | (1.0) | 0.8 | (1.0) |
|
Fast food consumption index (FFCI)c |
||||||||
| FFPI | −0.29 | (0.30) | 0.2 | (0.6) | −0.4 | (0.3) | −0.5 | (0.3)d |
| FVPI | −0.79 | (0.82) | −3.6 | (1.5)* | 0.0 | (0.7) | −0.8 | (1.1) |
|
Body Mass Index (kg/m2) |
||||||||
| FFPI | 0.6 | (1.0) | 3.6 | (1.7) | 0.4 | (1.8) | −0.3 | (1.1) |
| FVPI | −3.9 | (1.8)* | −9.8 | (5.7) | −6.8 | (2.8)* | −0.8 | (2.0) |
p<0.05 for null hypothesis that β=0, Wald test.
All models were adjusted for: survey year, proximity to price geocode (two dummy variables and four price indices × dummy var. interactions), age, sex, ethnicity, education, urbanization, region, smoking status, physical activity status, self-rated health and number of chronic conditions. Models with all PIR groups were adjusted for PIR categories. Models with FFPI were adjusted for FVPI and vice versa.
Fast Food Consumption Index: This index consisted of number of food items consumed at fast food restaurants over the two 24-hr recall period.
See Appendix A for more details about computations of diet quality indices.
Interaction term PIR ×FPI in a separate model indicates that this stratum-specific β is significantly different from the other strata at a type I error of 0.10.
PIR-stratified multivariate linear associations between food prices and study outcomes
Stratified multivariate linear and negative binomial regression analyses (Table 2) indicated that the effect of FFPI on dietary intake and quality varied somewhat across income groups. First, the positive effect of FFPI on fiber intake was statistically significant only and was largest in magnitude among the middle income category. It is important to bear in mind when assessing differences in significance levels across the stratified samples that the non-poor sample size was almost twice that of the poor sample size (3,002 versus 1,600). Several other associations between FFPI and dietary intake (e.g. aMED and FFCI) were modified by income as indicated by significant interaction term FFPI*PIR, though stratum-specific associations were not statistically significant.
As for FVPI, while it was expected to be inversely associated with diet quality, the opposite pattern was found for the total population as well as in stratum-specific associations. For instance, a higher FV price was associated with reduced energy and sodium intakes among the non-poor income groups; but higher fiber intake and lower FFCI among the poor (p<0.05). Finally, increased FVPI was associated with reduced BMI particularly among the near-poor income category, though interaction between FVPI and PIR was not significant.
Multivariate logistic regression association with selected binary outcomes: stratified by PIR
Table 3 shows results from multivariate logistic regression analyses of the association between food price indices expressed as z-scores and several binary outcomes including obesity, improved diet quality (upper quintile of HEI and aMED) and consumption of foods at FF restaurants within any of the two 24-hr recalls. Our findings suggested that while FF prices had only borderline significant association with FF consumption (OR: 0.89; 95% CI: 0.78, 1.02), FVPI was positively associated with improved dietary quality based on aMED score among the poor income category (OR=2.22; 95% CI: 1.22, 4.03), as well as a marked reduction in the proportion obese, particularly among the near poor (OR:0.82; 95%CI: 0.67, 0.99). PIR was a significant effect modifier in the relationship between FVPI and obesity (p<0.10 for interaction term FVPI*PIR).
Table 3.
Multivariate logistic regression modelsa of the effect of fast food, fruits and vegetables price indices (per 1 SD) on risk of obesity, high quality diet and consumption of fast foods stratified by poverty income ratio (PIR)---OR (95%CI): CSFII 1994–96
| All PIR groups | Poverty Income Ratio (PIR) | |||||||
|---|---|---|---|---|---|---|---|---|
| 0–130 Poor |
131–299 Near poor |
300+ Non-poor |
||||||
| N=7,331 | N=1,616 | N=2,713 | N=3,002 | |||||
| FFCI (yes vs. no)b | ||||||||
| FFPI (z-score) | 0.89 | (0.78, 1.02) | 0.99 | (0.74, 1.35) | 0.89 | (0.77, 1.04) | 0.87 | (0.74, 1.02) |
| FVPI (z-score) | 0.95 | (0.85, 1.07) | 0.79 | (0.60, 1.02) | 1.02 | (0.86, 1.21) | 0.94 | (0.81, 1.08) |
|
HEIc (>80th perc.) |
||||||||
| FFPI (z-score) | 1.00 | (0.87, 1.16) | 1.00 | (0.70, 1.45) | 0.95 | (0.71, 1.26) | 1.04 | (0.88, 1.22) |
| FVPI (z-score) | 1.16 | (0.99, 1.36) | 1.06 | (0.68, 1.67) | 1.23 | (0.89, 1.70) | 1.14 | (0.93, 1.39) |
|
aMEDc (>80th perc.) |
||||||||
| FFPI (z-score) | 1.07 | (0.91, 1.25) | 1.47 | (0.82, 2.62) | 0.96 | (0.75, 1.22) | 1.10 | (0.89, 1.36) |
| FVPI (z-score) | 1.11 | (0.92,1.35) | 2.22 | (1.22, 4.03)* | 1. 23 | (0.92, 1.65) | 1.00 | (0.81, 1.25) |
| Obesity (BMI≥30) | ||||||||
| FFPI (z-score) | 1.07 | (0.88, 1.31) | 1.18 | (0.87, 1.59) | 1.04 | (0.77, 1.40) | 1.04 | (0.80, 1.36) |
| FVPI (z-score) | 0.88 | (0.76, 1.04) | 0.77 | (0.51, 1.17) | 0.82 | (0.67, 0.99)* | 0.95 | (0.74, 1.22)d |
p<0.05 for null hypothesis that β=0, Wald test.
All models were adjusted for: survey year, proximity to price geocode (two dummy variables and four price indices × dummy var. interactions), age, sex, ethnicity, education, urbanization, region, smoking status, physical activity status, self-rated health and number of chronic conditions. Models with all PIR groups were adjusted for PIR categories. Models with FFPI were adjusted for FVPI and vice versa.
Fast Food Consumption Index: This index consisted of number of food items consumed at fast food restaurants over the two 24-hr recall period. In part of the analysis, this index was used as a binary variable (0 : no consumption; 1: at least one item consumed over the two 24-hr recall period).
See Appendix A for more details about computations of diet quality indices. In this analysis, the upper quintile of each index was considered as the main outcome.
Interaction term PIR ×FPI in a separate model indicates that this stratum-specific β is significantly different from the other strata at a type I error of 0.10.
DISCUSSION
This is one of few studies contributing to the growing literature on contextual and environmental socio-economic effects on dietary patterns and obesity, and the first to examine the impact of FFPI and FVPI on FF consumption, dietary intakes and overall dietary quality among a nationally representative sample of US adults. Although it is complex to assess individuals’ dietary intakes which are believed to be affected by the interactions of many factors at multiple levels, our main findings indicate that the variations in food prices are generally associated with dietary intakes in a manner that conforms to economic models, though that was only observed in the case of fast food prices. For example, when FFPI were increased, overall diet quality became higher. Further, higher FFPI was associated with higher fiber and lower saturated fat intake. In contrast, FVPI did not conform to that model as its increase was not associated with poorer dietary quality but in general followed the patterns observed for FFPI. In addition, FVPI was associated with a reduction in BMI and in the prevalence of obesity. Examining differences in price effects across income groups, we found several differential effects, including a stronger association between FFPI and fiber as well as between FVPI and BMI among the near-poor. In addition, significant association in the direction of improving dietary quality was found between FVPI , FFCI and fiber intakes particularly among the poor income category. However, none of those food price and income interactions were significant at a type I error level of 0.10. In contrast, the protective effect of FVPI on obesity was shown to be mostly confined to the near poor income category with a statistically significant interaction between FVPI and PIR.
Differential price sensitivity across income groups may reflect differences in ability to translate economic conditions into behavior changes. Whether this is due to individual knowledge and beliefs or to other environmental factors such as access to alternative food stores, or because the intakes of many poor individuals’ might have been affected by some related federal nutrition programs such food stamps needs to be investigated further. Further, other factors, such as access to food stores may be important factors in meeting the dietary guidelines, especially in poor neighborhoods. Supermarket availability has been associated with more fruit and vegetable intake, more healthful diets, and lower rates of obesity (Laraia, Siega-Riz, Kaufman, & Jones, 2004; Morland, Diez Roux, & Wing, 2006; Morland, Wing, Diez Roux, & Poole, 2002). Indeed, several studies show that low- versus high-income neighborhoods have significantly fewer available supermarkets (Alwitt, 1997; Moore & Diez Roux, 2006; Morland, Wing, & Diez Roux, 2002; Powell, Slater, Mirtcheva, Bao, & Chaloupka, 2007b; Shaffer, 2002). Thus, public policies should take the full food environment into account in order to develop successful strategies to encourage consumption of healthier foods (Jetter & Cassady, 2006).
Our study has several strengths in making contributions to the existing literature regarding the determinants of people’s eating behaviors. First, it extended findings from previous reports that showed significant associations between food prices and various outcomes of interest (Chou et al., 2004; Lakdawalla et al., 2005; Powell et al., 2007a; Sturm & Datar, 2005). . Second, we made use of a large nationally representative dataset with a wealth of social, demographic, psychosocial and nutritional information. Third, we assessed income differentials in the associations between food prices and food choices and BMI among US adults. In fact, a recent review (French, 2005) pointed to some emerging evidence that more motivated subgroups may account for most of the change in the aggregate-level environmental impact (Jeffery et al., 1994) and that higher-need groups, such as low-income populations, may not be equally influenced by such structural changes. Fourth, we examined the effects of FF and FV prices on FFCI directly using a standardized food coding system applied to two 24 hour recalls.
Despite its strengths, our study has its limitations. First, our findings were based on cross-sectional data which restricts our ability to ascertain causal effects. Second, food price indices are based on city-level prices for each survey year. Further, we were unable to geocode the households in the CSFII below the MSA/county level. Ideally, price geocodes should match each individual’s more proximate neighborhood community. To our knowledge, more proximate price data are not available on a national scale. In addition, with respect to the price data, our FV price index was limited to a relatively small number of items available in the ACCRA database and may not be representative of all of the most commonly consumed FVs. This may be responsible for some of our unexpected findings for the FVPI. However, a possible explanation is that low food prices in general can be related to overconsumption. Another limitation may be residual confounding by access variables such as concentration of FF restaurants and large supermarkets at the geocode level considered. Some of our inconsistent findings regarding price effects on dietary intakes (e.g. the effect of FVPI on sodium and cholesterol) may be explained by lack of access of the lower income groups to other dietary alternatives, which if controlled for, might have yielded different results. In those neighborhoods, a small decrement in the price of FV may be insufficient to influence overall dietary quality.
While increasing interventions to promote intake of FVs have been carried out over the past few decades, few studies have addressed environmental, national policy, and/or pricing interventions to encourage healthy eating (Glanz & Hoelscher, 2004). The latter can be defined as efforts aiming at improving the health of all people through better nutrition, not just small groups of motivated or high-risk individuals (Glanz, Lankenau, Foerster, Temple, Mullis, & Schmid, 1995; Glanz & Mullis, 1988). By influencing availability, access, price, and information/education about healthy eating, especially FVs, policies are able to reach entire populations.
The financial and political feasibility of subsidizing or taxing specific food prices as a strategy to promote healthier food choices is a legitimate concern. Our study results suggest that raising (taxing) the price of FFs would be a potentially effective strategy to improve a number of important dietary intake measures, particularly overall diet quality. However, such a tax would raise equity concerns. A reduction (subsidy) in FVPI may be important in helping improve Americans’ FV consumption and their dietary quality although these are not detected in our present study, which may be due to the limitations of the available national data sets. Future longitudinal studies with detailed food price data at the community or neighborhood levels as well as information regarding accessibility to various food stores and restaurants are needed to fully understand the impacts of food prices on people’s dietary intake and their risk of developing obesity. Continued research on the importance of food prices and food price-related policies and programs deserves ongoing attention considering the obesity crisis in the United States.
Supplementary Material
Acknowledgments
This study was supported by the National Research Initiative of the USDA Cooperative State Research, Education and Extension Service, grant number #2005-35215-15372.
Footnotes
Contributions of each author:
MAB: Conceptualization, plan of analysis, data management and statistical analysis, write-up of manuscript.
LMP: Conceptualization, plan of analysis, help with statistical analysis, write-up of parts of the manuscript, revision of the manuscript.
YW: Conceptualization, plan of analysis, help with statistical analysis, write-up of parts of the manuscript, revision of the manuscript.
Contributor Information
May A. Beydoun, Email: mbaydoun@jhsph.edu.
Lisa Powell, Email: powelll@uic.edu.
Youfa Wang, Email: ywang@jhsph.edu.
REFERENCES
- Ajani UA, Lotufo PA, Gaziano JM, Lee IM, Spelsberg A, Buring JE, et al. Body mass index and mortality among US male physicians. Ann Epidemiol. 2004;14(10):731–739. doi: 10.1016/j.annepidem.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Alwitt LF, Donley TD. Retail stores in poor urban neighborhoods. Journal of Consumer Affairs. 1997;31(1):139–164. [Google Scholar]
- Andrieu E, Darmon N, Drewnowski A. Low-cost diets: more energy, fewer nutrients. Eur J Clin Nutr. 2006;60(3):434–436. doi: 10.1038/sj.ejcn.1602331. [DOI] [PubMed] [Google Scholar]
- Cade J, Upmeier H, Calvert C, Greenwood D. Costs of a healthy diet: analysis from the UK Women’s Cohort Study. Public Health Nutr. 1999;2(4):505–512. doi: 10.1017/s1368980099000683. [DOI] [PubMed] [Google Scholar]
- Chou SY, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23(3):565–587. doi: 10.1016/j.jhealeco.2003.10.003. [DOI] [PubMed] [Google Scholar]
- Darmon N, Briend A, Drewnowski A. Energy-dense diets are associated with lower diet costs: a community study of French adults. Public Health Nutr. 2004;7(1):21–27. doi: 10.1079/phn2003512. [DOI] [PubMed] [Google Scholar]
- Darmon N, Ferguson E, Briend A. Do economic constraints encourage the selection of energy dense diets? Appetite. 2003;41(3):315–322. doi: 10.1016/s0195-6663(03)00113-2. [DOI] [PubMed] [Google Scholar]
- Darmon N, Ferguson EL, Briend A. A cost constraint alone has adverse effects on food selection and nutrient density: an analysis of human diets by linear programming. J Nutr. 2002;132(12):3764–3771. doi: 10.1093/jn/132.12.3764. [DOI] [PubMed] [Google Scholar]
- Darmon N, Ferguson EL, Briend A. Impact of a cost constraint on nutritionally adequate food choices for French women: an analysis by linear programming. J Nutr Educ Behav. 2006;38(2):82–90. doi: 10.1016/j.jneb.2005.11.028. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. Fat and sugar: an economic analysis. J Nutr. 2003;133(3):838S–840S. doi: 10.1093/jn/133.3.838S. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. Obesity and the food environment: dietary energy density and diet costs. Am J Prev Med. 2004;27(3 Suppl):154–162. doi: 10.1016/j.amepre.2004.06.011. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005a;82(1 Suppl):265S–273S. doi: 10.1093/ajcn/82.1.265S. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Darmon N. Food choices and diet costs: an economic analysis. J Nutr. 2005b;135(4):900–904. doi: 10.1093/jn/135.4.900. [DOI] [PubMed] [Google Scholar]
- Freedman DM, Ron E, Ballard-Barbash R, Doody MM, Linet MS. Body mass index and all-cause mortality in a nationwide US cohort. Int J Obes (Lond) 2006;30(5):822–829. doi: 10.1038/sj.ijo.0803193. [DOI] [PubMed] [Google Scholar]
- French SA. Public health strategies for dietary change: schools and workplaces. J Nutr. 2005;135(4):910–912. doi: 10.1093/jn/135.4.910. [DOI] [PubMed] [Google Scholar]
- French SA, Jeffery RW, Story M, Breitlow KK, Baxter JS, Hannan P, et al. Pricing and promotion effects on low-fat vending snack purchases: the CHIPS Study. Am J Public Health. 2001a;91(1):112–117. doi: 10.2105/ajph.91.1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001b;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Jeffery RW, Snyder P, Eisenberg M, Sidebottom A, et al. Pricing strategy to promote fruit and vegetable purchase in high school cafeterias. J Am Diet Assoc. 1997;97(9):1008–1010. doi: 10.1016/S0002-8223(97)00242-3. [DOI] [PubMed] [Google Scholar]
- Glanz K, Hoelscher D. Increasing fruit and vegetable intake by changing environments, policy and pricing: restaurant-based research, strategies, and recommendations. Prev Med. 2004;39 Suppl 2:S88–S93. doi: 10.1016/j.ypmed.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Glanz K, Lankenau B, Foerster S, Temple S, Mullis R, Schmid T. Environmental and policy approaches to cardiovascular disease prevention through nutrition: opportunities for state and local action. Health Educ Q. 1995;22(4):512–527. doi: 10.1177/109019819502200408. [DOI] [PubMed] [Google Scholar]
- Glanz K, Mullis RM. Environmental interventions to promote healthy eating: a review of models, programs, and evidence. Health Educ Q. 1988;15(4):395–415. doi: 10.1177/109019818801500403. [DOI] [PubMed] [Google Scholar]
- Howarth NC, Huang TT, Roberts SB, Lin BH, McCrory MA. Eating patterns and dietary composition in relation to BMI in younger and older adults. Int J Obes (Lond) 2006 doi: 10.1038/sj.ijo.0803456. [DOI] [PubMed] [Google Scholar]
- Howarth NC, Huang TT, Roberts SB, McCrory MA. Dietary fiber and fat are associated with excess weight in young and middle-aged US adults. J Am Diet Assoc. 2005;105(9):1365–1372. doi: 10.1016/j.jada.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Howarth NC, Murphy SP, Wilkens LR, Hankin JH, Kolonel LN. Dietary energy density is associated with overweight status among 5 ethnic groups in the multiethnic cohort study. J Nutr. 2006;136(8):2243–2248. doi: 10.1093/jn/136.8.2243. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, French SA, Raether C, Baxter JE. An environmental intervention to increase fruit and salad purchases in a cafeteria. Prev Med. 1994;23(6):788–792. doi: 10.1006/pmed.1994.1135. [DOI] [PubMed] [Google Scholar]
- Jetter KM, Cassady DL. The availability and cost of healthier food alternatives. Am J Prev Med. 2006;30(1):38–44. doi: 10.1016/j.amepre.2005.08.039. [DOI] [PubMed] [Google Scholar]
- Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101(1):28–34. doi: 10.1016/S0002-8223(01)00008-6. quiz 35-26. [DOI] [PubMed] [Google Scholar]
- Lakdawalla D, Philipson T, Bhattacharya J. Welfare-Enhancing Technological Change and the Growth of Obesity. American Economic Review. 2005;95(2):253–257. doi: 10.1257/000282805774670266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laraia BA, Siega-Riz AM, Kaufman JS, Jones SJ. Proximity of supermarkets is positively associated with diet quality index for pregnancy. Prev Med. 2004;39(5):869–875. doi: 10.1016/j.ypmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- McCullough ML, Feskanich D, Rimm EB, Giovannucci EL, Ascherio A, Variyam JN, et al. Adherence to the Dietary Guidelines for Americans and risk of major chronic disease in men. Am J Clin Nutr. 2000;72(5):1223–1231. doi: 10.1093/ajcn/72.5.1223. [DOI] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health. 2006;96(2):325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am J Public Health. 2002;92(11):1761–1767. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- Popkin BM, Duffey K, Gordon-Larsen P. Environmental influences on food choice, physical activity and energy balance. Physiol Behav. 2005;86(5):603–613. doi: 10.1016/j.physbeh.2005.08.051. [DOI] [PubMed] [Google Scholar]
- Powell LM, Auld C, Chaloupka FJ, O’ Malley P, Johnston LD. Access to fast food and food prices: relationship with fruit and vegetable consumption and overweight among adolescents. Advances in Health Economics and Health Services Research. 2007a;17:23–48. [PubMed] [Google Scholar]
- Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007b doi: 10.1016/j.ypmed.2006.08.008. In press. [DOI] [PubMed] [Google Scholar]
- Schroder H, Marrugat J, Covas MI. High monetary costs of dietary patterns associated with lower body mass index: a population-based study. Int J Obes (Lond) 2006;30(10):1574–1579. doi: 10.1038/sj.ijo.0803308. [DOI] [PubMed] [Google Scholar]
- Selvin S. Statistical Analysis of Epidemiologic Data. Oxford University Press; 2004. [Google Scholar]
- Shaffer A. The persistence of L.A.’s grocery gap: The need for a new food policy and approach to market development.: Center for Food and Justice, Urban and Environmental Policy Institute (UEPI) Occidental College; 2002. [Google Scholar]
- Siega-Riz AM, Kranz S, Blanchette D, Haines PS, Guilkey DK, Popkin BM. The effect of participation in the WIC program on preschoolers’ diets. J Pediatr. 2004;144(2):229–234. doi: 10.1016/j.jpeds.2003.10.052. [DOI] [PubMed] [Google Scholar]
- STATA. Statistics/Data Analysis: Release 9. Texas: Stata Corporation; 2005. [Google Scholar]
- Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059–1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, et al. Diet and overall survival in elderly people. Bmj. 1995;311(7018):1457–1460. doi: 10.1136/bmj.311.7018.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Agriculture. Data (CD-ROM) and documentation for the 1994–96 Continuing Survey of Food Intakes by Individuals (CSFII)-Diet and Health Knowledge Survey. National Technical Information Service Accession; 1994–96. [Google Scholar]
- Wang Z, Patterson CM, Hills AP. A comparison of self-reported and measured height, weight and BMI in Australian adolescents. Aust N Z J Public Health. 2002;26(5):473–478. doi: 10.1111/j.1467-842x.2002.tb00350.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.