Abstract
Postoperative small bowel obstruction (SBO) is a common complication of appendectomy. This study aimed to assess risk factors for SBO following appendectomy.
This retrospective cohort study used the 2006 to 2008 Taiwan National Health Insurance Research Database. We evaluated adult patients with acute appendicitis who underwent open (OA) or laparoscopic appendectomy (LA) between January 1, 2006 and December 31, 2008. Excluded were patients with a history of abdominal surgery and SBO before the index operation, or abdominal surgery between the appendectomy and initial diagnosis of bowel obstruction as an identifiable cause of SBO. Factors thought to influence postoperative SBO were highlighted. The OA and LA cohorts were matched by propensity score, and the hazard ratios (HRs) and 95% confidence interval (CIs) of SBO were calculated.
We enrolled 11,289 patients who underwent OA, and 11,289 matched controls who underwent LA. OA patients had significant risk of adhesive SBO compared with the LA group (adjusted HR: 1.7, 95% CI: 1.11–2.63). Further analysis revealed that that female sex (adjusted HR: 1.79, 95% CI: 1.17–2.72), CCI score of 1 or ≥2 (adjusted HR: 3.16, 95% CI: 1.76–5.67; adjusted HR: 4.03, 95% CI: 1.57–10.34), complicated appendicitis (adjusted HR: 1.68, 95% CI: 1.05–2.69), treatment in district hospitals increased risk of adhesive SBO.
Female sex, complicated appendicitis, more comorbidities, and treatment in district hospitals are factors associated with a risk of SBO after appendectomy. Our findings confirmed that a laparoscopic approach is better than an open approach.
INTRODUCTION
Appendicitis is a common problem that is typically treated with an appendectomy.
Laparoscopic appendectomy has been used as a more favorable minimally invasive method compared with an open procedure because of its clinical advantages, including less pain, shorter hospital stay, and less risk of wound infection, as demonstrated by randomized trials; however, LA is also associated with an increased risk of intra-abdominal abscess, an increased risk of serious vascular injury and bowel perforation, and higher hospital costs,1,2
Following appendectomy, adhesions subsequently may cause a small bowel obstruction (SBO). Previous studies reported differences in the rate of postappendectomy SBO, and conveyed conflicting recommendations,3,4 Studies addressing this question are small single-center retrospective studies, in which observations have been confounded by previous abdominal surgery and loss to follow-up, or included only patients who underwent an open appendectomy,5,6 We matched the open and laparoscopic appendectomy cohorts by propensity score to reduce the selection bias. From a population-based register database, we could exclude other possible surgical etiologies of SBO. In addition, we did not encounter the problem of loss to follow-up that may be more prevalent in a single institution. The purpose of our study was to determine the true risk and predictors of postappendectomy SBO.
METHODS
The National Health Insurance Program in Taiwan is a universal health care system established in 1995 that covers 99% of this country's population of 25.58 million people.
The data used in this analysis originated from the National Health Insurance Research Database (NHIRD). This database contains all claims data (from 1996 to 2012) for 25 million beneficiaries randomly selected in 2000. The database contains encrypted patient identification numbers, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), which codes for diagnoses and procedures; prescription drug details; dates of admission and discharge; and basic socio-demographic information, including sex and birth date.
A retrospective cohort study was conducted with 2 study groups: a laparoscopic appendectomy (LA) group and an open appendectomy (OA) group. Hospitalized adult patients with a discharge diagnosis of acute appendicitis (International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes 540, 540.0, 540.1, and 540.9, 542) between January 2006 and December 2008 were selected from the NHIRD.
Patients with a history of abdominal surgery and small bowel obstruction before the index operation, or abdominal surgery between the appendectomy and initial diagnosis of bowel obstruction as an identifiable cause of small bowel obstruction (ICD-9-CM codes: 560, 568) were excluded. The claims data from 1996 to 2006 were used to confirm that none of the enrolled patients had undergone any abdominal operation, nor had any of them had a small bowel obstruction before 2006. In our study, patients younger than 18 years of age were also excluded.
Demographic data including age, sex, Charlson comorbidity index score (CCI score), surgical methods (open or laparoscopic), pathology, and hospital status were collected. Person-years (PY) of follow-up time were calculated for each person until SBO diagnosis, death, withdrawal from the insurance system, or the end of 2008.
To decrease selection bias, we matched the open and laparoscopic appendectomy cohorts by propensity score. Propensity-score matching was used to reduce selection bias because it can bundle many confounding covariates that may be present in an observational study with this number of variables. In our study, propensity scores were computed by modeling a logistic regression model with the dependent variable as the odds of diagnosis of open appendectomy (vs. laparoscopic), and the independent variables as the age of surgery, sex, Charlson comorbidity index score (CCI score), pathology, and hospital status. Subsequently, an SAS matching macro “%OneToManyMTCH” proposed by proceeding of the 29th SAS Users Group international (SUGI) was used in this study.7 It allows propensity score matching from 1-to-1 to 1-to-N based on specification from the user. The macro makes “best” matches first and “next-best” matches next, in a hierarchical sequence until no more matches can be made. Each control is selected at most once. The final matched-pair samples contain both closely matched individual pairs and balanced case and control groups. After propensity score matching, 11,289 patients who underwent LA, and 11,289 patients who underwent OA were selected as the study sample.
The data retrieval from the register did not include patient or hospital identification. No individual patient medical records have been studied, and results are presented only for groups. No individual patient can be identified; thus, no approval from the ethics committee was required or obtained.
Statistical Analyses
All statistical analyses were performed by using the SAS 9.3.1 statistical package (SAS Institute Inc, Cary, NC). We used Pearson χ2 tests to compare differences in the baseline characteristics, Charlson comorbidity index score (CCI score), surgical methods (open or laparoscopic), pathology, and hospital status between LA and OA groups before and after propensity score matching. The incidence rate was calculated as the number of SBO cases identified during the follow-up, divided by the total person-years for each group by sex, age, and follow-up months.
Moreover, stratified Cox proportional hazard regression stratified by 0 to 3 month and 3 month–3 years was performed to calculate the risk of SBO between LA and OA groups during the follow-up period. A Kaplan–Meier analysis was used to calculate the cumulative incidence rates of SBO between 2 cohorts, and the log-rank test was used to analyze the differences between the survival curves. A 2-sided P value <0.05 was considered statistically significant.
RESULTS
Before the propensity score matching, a total of 40,326 patient records were sampled. We identified 11,317 patients (28.1%) who had undergone laparoscopic appendectomy based on insurance claims data collected between the years of 2006 and 2008.
The demographic characteristics were different in age distribution, sex distribution, Charlson comorbidity index score, pathology, and hospital status (Table 1) for patients in the LA group versus the OA group. Compared with patients in the OA group, patients in the LA group were younger on average (39.06 years of age vs. 40.03 years of age, P <0.0001), and had a lower Charlson comorbidity index score (P <0.0001). In addition, the LA group had a smaller proportion of female patients (47.98% vs. 52.02%, P <0.0001), more patients with simple appendicitis (84.24% vs. 78.34%, P <0.0001), and more patients treated in medical centers (48.05% vs. 28.83%, P < 0.0001).
TABLE 1.
Demographic Characteristics and Clinical Information of Patients in OA and LA Groups From 2006 to 2008 in Taiwan and Matched by Propensity Score

Among patients who met the eligibility criteria for this study, 11,289 patients who underwent LA, and 11,289 patients who underwent OA were selected.
After propensity, all of the P values of variables were >0.05, demonstrating that there was no significant difference in average age, age stratification, sex, CCI score, severity of acute appendicitis, and hospital status.
We compared the differences in the risk of developing postappendectomy SBO between the OA and LA groups with regard to age, sex, and follow-up year. SBO incidence was significantly greater in the OA group (34.95 per 10,000 person-years) than in the LA group (22.59 per 10,000 person-years) (P = 0.0472).
No significant differences in the incidence of SBO were noted in LA patients 18 to 35 years of age, 35 to 50, and 50 years or older (P = 0.0524, P = 0.1208, and P = 0.9636, respectively) compared with patients of similar age in the OA group (Table 2).
TABLE 2.
Risk of Small Bowel Obstruction in Patients After OA or LA

Although in all groups of patients 18 to 35 years of age, 35 to 50, and 50 years or older, patients who had undergone OA had a greater incidence of SBO than did those who had undergone LA (28.38 vs. 13.35 per 10,000 person-years; 31.34 vs. 14.91 per 10,000 person-years; 54.93 vs. 54.1 per 10,000 person-years); however, there was no statistically significant difference.
Patients ≥50 years of age exhibited the highest incidence of SBO, and patients 35 to 50 years of age the second highest among patients in both the LA and OA groups.
Male and female patients having undergone OA had a greater incidence of SBO than did those in the LA group (27.09 vs. 14.09; 43.48 vs. 31.69 per 10,000 person-years); however, there was no statistically significant difference, P = 0.08, 0.2468, respectively.
The greatest incidence of SBO occurred within 3 months postoperatively, and there was a significant difference between the OA and LA groups (117.29 vs. 41.20 per 10,000 person-years P = 0.0028).
In the follow-up time periods of 3 months to 3 years, patients in the OA group had an incidence of SBO similar to that of patients in the LA group (19.99 vs. 18.1, P = 0.7308) (Table 2).
The ratio of the slopes of the curves describing cumulative incidence of SBO over time for patients in the OA group versus that of those in the LA group is constant. It also corresponds to the assumption of proportional hazards in the Cox regression (Figure 1).
FIGURE 1.
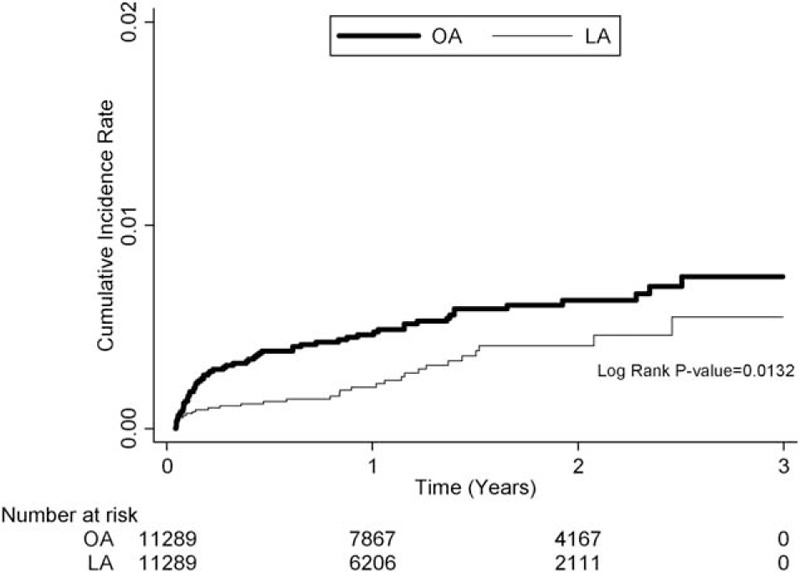
The ratio of the slopes of the curves describing cumulative incidence of SBO over time for patients in the open appendectomy (OA) group versus that of those in the laparoscopic appendectomy (LA) group is constant.
Patients who underwent open appendectomy (adjusted HR of 1.7, 95% CI, 1.11–2.63), female patients (adjusted HR of 1.79, 95% CI, 1.17–2.72), those with a CCI score = 1 or ≧2 (adjusted HR of 3.16, 95% CI, 1.76–5.67; adjusted HR of 4.03, 95% CI, 1.57–10.34), patients who underwent appendectomy in a district hospital, and those with complicated appendicitis (adjusted HR of 1.68, 95% CI, 1.05–2.69) had a significantly greater cumulative hazard rate (Table 3).
TABLE 3.
Crude and Adjusted Hazard Ratios of Cox Proportional Hazard Regressions and 95% Confidence Interval for the Development of Small Bowel Obstruction During 3 Years for the Study Cohort

DISCUSSION
In our study, the incidence of SBO in populations who had undergone OA and LA was 34.95 per 10,000 person-years, and 22.59 per 10,000 person-years, respectively. The incidence ratio 1.55 (95% CI = 1.01–2.38), P = 0.0472, OA vs. LA) indicated the significant difference in the incidence of SBO after laparoscopic versus open appendectomy. Leung et al8 enrolled 1777 patients, and found 0.0069 cases per person-year by using data from an adult hospital in the Calgary Health Region. Using the National Library of Medicine MEDLINE database to identify all reports related to the incidence and risk factors associated with adhesive SBO, Barmparas et al9 reported a similar rate of adhesive SBO after open or laparoscopic appendectomy (1.3% vs. 1.4%).
From the Swedish National Patient Register database, Andersson10 concludes that laparoscopic appendectomy leads to fewer adhesions and is therefore expected to lower.
The risk of this long-term complication; however, neither of these studies excluded those patients who had undergone abdominal surgery before or after appendectomy.
Due to the unique Taiwan's National Health Insurance (NHI) system providing universal coverage and guaranteed equal access to health care services, patients being admitted to other hospitals for SBO are ascertained, and patients receiving any medical care are not lost to follow-up in this nationwide population-based study.
In our study, the risk of SBO was related not only to the surgical approach, but also to sex, hospital status, severity of initial appendicitis, and comorbidities.
Open surgery seems to increase the risk of SBO at least 4-fold compared with laparoscopic surgery for most of the abdominal surgical procedures studied.11 The laparoscopic approach appears to decrease the risk of adhesion formation by 45% as well as decreasing the need for adhesion-related reintervention to 0.8% after appendectomy.12 A recent study by Isaksson et al13 found a significant difference in the rate of postoperative SBO: 1.0% in the open group, and 0.4% in the laparoscopic group (P = 0.015). Our findings were similar and the overall incidence of SBO after laparoscopic appendectomy was significantly less than after open appendectomy (22.59 vs. 34.95 per 10,000 person-years). Although LA is associated with a greater incidence of intra-abdominal abscess after operation than is OA,14 however the influence of intra-abdominal abscess on small bowel obstruction is not obvious in this study.
Andersson5 found that of all patients undergoing appendectomy, those 20 to 39 years of age had the lowest risk for SBO requiring surgery, while patients >70-year old had a 2-fold higher risk compared with patients <20-year old.
From the Scottish National Health Service medical record linkage database, Parker et al15 reported that patients ≥16 years of age undergoing an appendectomy were at higher risk for readmission directly related to adhesions over the following 5 years, when compared with young patients, those <16 years of age.
However, our data showed that age is not an independent risk factor for SBO. Differences in age stratification between studies, and selection bias in patient groups account for differences in study conclusions.
The role of sex in the development of SBO is still controversial and is not conclusive. Riber et al16 examined the role of sex in patients undergoing open appendectomy, and found that female patients had an almost 4-fold higher overall risk for SBO requiring surgical intervention. In contrast, Andersson5 found that female patients were at a slightly lower risk for developing this complication [adjusted hazard ratio 0.8 (0.8–0.9)] in a similar population. In our study, woman had higher risk of subsequent small bowel obstruction after appendectomy. Occult etiology causing SBO such as subclinical pelvic inflammatory pelvic disease, endometriosis, or inflammation of adnexa may be misdiagnosed as adhesive small bowel obstruction.
Such misdiagnosis may be the reason why woman exhibited a higher risk of postappendectomy small bowel obstruction in a population-based study.
Charlson comorbidity index (CCI) has been used to predict outcome in many kinds of surgery and treatment modalitities.17,18Although preoperative comorbidities were not very common in our study groups, with only 6.25% of patients having CCI score ≥1. Our study still confirmed that a high comorbidity burden was associated with increased risk of small bowel obstruction after appendectomy. Disorders that may influence bowel motility may be more common in a population with higher CCI scores. Application of the CCI to the population undergoing appendectomy is a strong predictor of subsequent small bowel obstruction.
Not only the type of surgery, but also the extent of peritoneal damage resulting from surgical trauma, dissection, infection, or inflammation could be a risk factor for bowel obstruction.19 Complicated appendicitis results in increased risk of postoperative intra-abdominal infection, increased surgical complexity with a larger rough surface, and inflammation. Therefore, disease severity can play an important role in the development of small bowel obstruction.
High-volume hospitals and experienced surgeons had significantly better surgical outcomes.20,21 In our study, approximately 91% of patients who underwent appendectomy did so in a medical center or regional hospital. Our results showed that patients in district hospitals had increased risk of postappendectomy small bowel obstruction. Although laparoscopic appendectomy is safe, even in the case of complicated appendicitis22 and when performed in a low-volume setting.23 A high volume of appendectomies and consequently a high degree of experience may be important in reducing postoperative small bowel obstruction.
The identification of high-risk patient subgroups may assist in the development of strategies to prevent adhesions, and in the proffering of preoperative advice on adhesion risk.24 The large, nationwide, population-based data set from Taiwan allowed us to examine risk factors for the development of SBO with a low risk of selection bias. The large sample size enhanced our statistical power as well as the precision of risk appraisal.
This population-based study has still some limitations. First, several suspected risk factors for SBO were not available from the insurance data, such as nonsurgical abdominal pathology, including subclinical gynecologic pathology, abdominal trauma, or intra-abdominal infection. Thus, the lack of access to this information might have resulted in some degree of bias. Second, the database did not include information regarding the severity of SBO. Some patients may have sustained only mild self-limited partial bowel obstruction, and may have been treated in the ER or OPD. Thus, they would not have been enrolled into our study. Third, the diagnosis of adhesive small bowel obstruction was based on ICD-9-CM diagnosis code only. Our study lacks the imaging findings to confirm diagnoses, thus allowing potential misclassification of disease.
CONCLUSION
An open surgical approach, female sex, CCI score ≥1, complicated appendicitis, and appendectomy in a district hospital were factors associated with a higher risk of postoperative SBO. The benefits of the minimally invasive approach may extend well beyond the postoperative period. Thus, clinicians managing patients with acute appendicitis, especially those patients who have risk factors, should be aware of the potential for the development of SBO.
Footnotes
Abbreviations: CCI = Charlson comorbidity index, LA = laparoscopic appendectomy, NHIRD = National Health Insurance Research Database, OA = open appendectomy, SBO = small bowel obstruction.
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institutes (Registered number 99213). The interpretation and conclusions contained herein do not represent those of Bureau of National Health Insurance, Department of Health or National Health Research Institutes.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Ohtani H, Tamamori Y, Arimoto Y, et al. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg 2012; 16:1929–1939. [DOI] [PubMed] [Google Scholar]
- 2.Wei B, Qi CL, Chen TF, et al. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc 2011; 25:1199–1208. [DOI] [PubMed] [Google Scholar]
- 3.Duron JJ, Hay JM, Msika S, et al. Prevalence and mechanisms of small intestinal obstruction following laparoscopic abdominal surgery: a retrospective multicenter study. French Association for Surgical Research. Arch Surg 2000; 135:208–212. [DOI] [PubMed] [Google Scholar]
- 4.Zbar RI, Crede WB, McKhann CF, et al. The postoperative incidence of small bowel obstruction following standard, open appendectomy and cholecystectomy: a six-year retrospective cohort study at Yale-New Haven Hospital. Conn Med 1993; 57:123–127. [PubMed] [Google Scholar]
- 5.Andersson RE. Small bowel obstruction after appendicectomy. Br J Surg 2001; 88:1387–1391. [DOI] [PubMed] [Google Scholar]
- 6.Khairy GA, Afzal MF, Murshid KR, et al. Post appendectomy small bowel obstruction. Saudi Med J 2005; 26:1058–1060. [PubMed] [Google Scholar]
- 7.Parsons LS (2004) Performing a 1:N case-control match on propensity score (Poster presented at the 29th Annual SAS® Users Group International Conference, Montreal, Canada), pp 9–12, May, Poster 165–29. http://www2.sas.com/proceedings/sugi29/toc.html#front Accessed August 19, 2011. [Google Scholar]
- 8.Leung TT, Dixon E, Gill M, et al. Bowel obstruction following appendectomy: what is the true incidence? Ann Surg 2009; 250:51–53. [DOI] [PubMed] [Google Scholar]
- 9.Barmparas G, Branco BC, Schnüriger B, et al. The incidence and risk factors of post-laparotomy adhesive small bowel obstruction. J Gastrointest Surg 2010; 14:1619–1628. [DOI] [PubMed] [Google Scholar]
- 10.Andersson RE. Short-term complications and long-term morbidity of laparoscopic and open appendicectomy in a national cohort. Br J Surg 2014; 101:1135–1142. [DOI] [PubMed] [Google Scholar]
- 11.Angenete E, Jacobsson A, Gellerstedt M, et al. Effect of laparoscopy on the risk of small-bowel obstruction: a population-based register study. Arch Surg 2012; 147:359–365. [DOI] [PubMed] [Google Scholar]
- 12.Ouaïssi M, Gaujoux S, Veyrie N, et al. Post-operative adhesions after digestive surgery: their incidence and prevention: review of the literature. J Visc Surg 2012; 149:104–114. [DOI] [PubMed] [Google Scholar]
- 13.Isaksson K, Montgomery A, Moberg AC, et al. Long-term follow-up for adhesive small bowel obstruction after open versus laparoscopic surgery for suspected appendicitis. Ann Surg 2014; 259:1173–1177. [DOI] [PubMed] [Google Scholar]
- 14.Yong JL, Law WL, Lo CY, et al. A comparative study of routine laparoscopic versus open appendectomy. JSLS 2006; 10:188–192. [PMC free article] [PubMed] [Google Scholar]
- 15.Parker MC, Wilson MS, Menzies D, et al. The SCAR-3 study: 5-year adhesion-related readmission risk following lower abdominal surgical procedures. Colorectal Dis 2005; 7:551–558. [DOI] [PubMed] [Google Scholar]
- 16.Riber C, S⊘e K, J⊘rgensen T, et al. Intestinal obstruction after appendectomy. Scand J Gastroenterol 1997; 32:1125–1128. [DOI] [PubMed] [Google Scholar]
- 17.Birim O, Kappetein AP, Bogers AJ. Charlson comorbidity index as a predictor of long-term outcome after surgery for nonsmall cell lung cancer. Eur J Cardiothorac Surg 2005; 28:759–762. [DOI] [PubMed] [Google Scholar]
- 18.Shi HY, Hwang SL, Lee IC, et al. Trends and outcome predictors after traumatic brain injury surgery: a nationwide population-based study in Taiwan. J Neurosurg 2014; 121:1323–1330. [DOI] [PubMed] [Google Scholar]
- 19.Di Saverio S, Coccolini F, Galati M, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2013 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg 2013; 8:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang CM, Yin WY, Wei CK, et al. The combined effects of hospital and surgeon volume on short-term survival after hepatic resection in a population-based study. PLoS One 2014; 9: e86444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brusselaers N, Mattsson F, Lagergren J. Hospital and surgeon volume in relation to long-term survival after oesophagectomy: systematic review and meta-analysis. Gut 2014; 63:1393–1400. [DOI] [PubMed] [Google Scholar]
- 22.Yeom S, Kim MS, Park S, et al. Comparison of the outcomes of laparoscopic and open approaches in the treatment of periappendiceal abscess diagnosed by radiologic investigation. J Laparoendosc Adv Surg Tech A 2014; 24:762–769. [DOI] [PubMed] [Google Scholar]
- 23.Cawich SO, Mohanty SK, Simpson LK, et al. Is laparoscopic appendectomy safe when performed in a low volume setting? Int J Biomed Sci 2014; 10:31–35. [PMC free article] [PubMed] [Google Scholar]
- 24.Attard JA, MacLean AR. Adhesive small bowel obstruction: epidemiology, biology and prevention. Can J Surg 2007; 50:291–300. [PMC free article] [PubMed] [Google Scholar]


