Abstract
Early diagnosis was the main way to improve the survival rate of lung cancer patients. At present, the methods to diagnose lung cancer were varied, but early diagnosis of lung cancer was still difficult. In experimental and clinical studies, lung cancer related tumor markers were helpful to the early diagnosis of lung cancer. So far, there were many studies about lung cancer related tumor markers in China, but the subjects in these studies were almost the Han population. There were few studies about the Uygur population. Xinjiang was a multi-ethnic region in China, the ratios of Han and Uygur population were 40% and 45%, respectively. Xinjiang also was a high incidence area of lung cancer in China. The purpose of this study was to research the application of 6 tumor markers in Uygur and Han lung cancer patients in XinJiang, China.
The study collected 342 cases who were diagnosed as lung cancer in Tumor Hospital Affiliated to XinJiang Medical University from May 2012 to December 2012. Serum concentrations of squamous cell carcinoma (SCC), cytokeratin fragment 19 (CYFRA21-1), carcino-embryonic antigen (CEA), carbohydrate antigen 125 (CA125), precursor of gastrin-releasing peptide (Pro-GRP), and neuron-specific enolase (NSE) were tested for every patient before radiation, chemotherapy, or surgery. The serum concentrations of SCC, CYFRA21-1, CEA, CA125, and Pro-GRP were assayed using the micro-particle luminescence analysis testing by the Abbott ARHCITECT i2000SR immunoanalyzer. NSE was assayed by the electrochemical luminescence analysis testing using Roche Cobas E601 electrochemical luminescence analyzer.
Serum levels of SCC were different between 2 ethnic populations, smoking should be the influence factor to create the difference. Cluster analysis showed that the NSE and Pro-GRP were helpful to identify small cell lung cancer (SCLC), and CEA, CA125, SCC, CYFRA21-1 were beneficial to diagnose non-small cell lung cancer (NSCLC). The compare of diagnosis value about serum tumor markers also proved the result of cluster analysis. No matter SCLC or NSCLC, the positives rate of all tumor markers were increasing as clinical stage advancing. Pro-GRP had higher positive rate than NSE in limited stage of SCLC. CA125 had the highest positive rate in I and II stage of NSCLC, and CYFRA21-1 had the highest positive rate in III and IV stage of NSCLC. CEA and CA125 were beneficial to diagnose adenocarcinoma, CYFRA21-1, and SCC identified squamous cell cancer better.
Only SCC level was higher in Han population than Uygur population because of the differences of smoking constituent ratio between 2 populations. So, it could be unified to research the application value of the 6 indicators for the Han and Uygur population. Then, we suggested a primary diagnostic utility of 6 commonly by lung cancer biomarkers in both the Han and Uygur populations in Xinjiang Uygur Autonomous Region of People's Republic of China.
INTRODUCTION
Lung cancer was the world's most common malignant tumor, the fatality ratio in the cities was in the first place, as high as 90%.1,2 In United States, lung cancer mortality accounted for 28% in all cancer deaths, in China the constituent ratio was also more than 20%.3–5 The 5-year survival rate was 10%, the early accurate diagnosis could effectively improve the survival rate of lung cancer patients. The clinical diagnosis of lung cancer included pathologic and clinical stage. Clinicians relied mainly on clinical symptoms and signs, imaging examination, tumor markers, genetic testing, and pathological examination to make the diagnosis for lung cancer. Clinical signs and symptoms of lung cancer tended to be complicated and non-specificity, Bari et al6 studied 1300 cases of lung cancer and lung cancer suspected benign disease to conclude that symptoms were nonspecific. If it was found that the suspicious lung cancer related symptoms when physical examination, patients were recommended to do image examination.7 Radiographic inspection of lung cancer was the main test method, but it was more difficult to diagnose the small nodules. Once suspicious lung nodules were found by imaging, then there was the need for histopathology related inspection, including bronchoscopy, percutaneous lung biopsy, and mediastinum microscopy. But these histopathological examinations were invasive; there was the risk of injury and the presence of false negative result.8
Experimental and clinical studies have shown that tumor markers were useful to diagnose lung tumor. Compared with the imaging and histopathological examination, tumor markers were tested by an inexpensive and simple detection method which was less invasive and traumatic. Previous research has widely reported that the meaningful tumor markers of lung cancer including squamous cell carcinoma (SCC), cytokeratin fragment 19 (CYFRA21-1), carcino-embryonic antigen (CEA), carbohydrate antigen 125 (CA125), precursor of gastrin-releasing peptide (Pro-GRP), and neuron-specific enolase (NSE). The tumor markers had considerable clinical significance for diagnosis and prognosis of lung cancer.9–13
Xinjiang Uygur Autonomous Region was located in the northwestern border of China and was the largest province in China with a population of 21.8 million in 2011, which covered 1.66 million square kilometers. According to the latest census data from the National and Xinjiang local Statistics Bureau (2011), the total population of China was 1.37 billion, in which 91.51% was Han ethnic, 0.76% was Uygur ethnic. Xinjiang was a multi-ethnic area with a much larger percentage of Uygur (46.2%) and smaller percentage of Han (40.1%) than in whole China. Xinjiang also was one of the high incidence areas of lung cancer in China.14
The purpose of this study was to research the application of 6 tumor markers in Uygur and Han lung cancer patients in XinJiang by a retrospective study.
METHODS
Patient
Specimens were collected from May 2012 to December 2012 in the tumor hospital affiliated to XinJiang Medical University which were diagnosed to lung cancer finally, some of the patients were found to have some pulmonary mass during health examination, others were transferred to the hospital from other primary hospital and general hospital because of an unclear diagnosis. All tumor markers were determined before patients received any radiation, chemotherapy, and surgery. The study included 342 cases that met the criteria, including 187 Han and 155 Uygur cases. The clinical stages of non-small cell lung cancer (NSCLC) referenced to the revision of International Cancer Alliance (UICC) and American Joint Committee on Cancer (AJCC) in 2003, NSCLC was divided into I and II, III and IV stages. Small cell lung carcer (SCLC) was divided into limited and extensive stage according to the staging system of the Veterans Hospital. The research related to human had been complied with all the relevant national regulations, institutional policies, and in accordance with the tenets of the Helsinki Declaration, and had been approved by The Tumor Hospital Affiliated to Xinjiang Medical University institutional review board.
Tumor Markers Assay
Serum concentrations of SCC, CYFRA21-1, CEA, CA125, Pro-GRP, and NSE were assayed in all patients. The serum concentrations of SCC, CYFRA21-1, CEA, CA125, and Pro-GRP were assayed by the micro-particle chemiluminescence analysis using the Abbott ARCHITECT i2000SR immuno analyser (USA). NSE was assayed by the electrochemical luminescence using Roche Cobas E601 analyzer (Switzerland). All test procedures were performed according to the equipment operation procedure, calibration solution and reagents were original kits from manufacturer. The reference interval of these tumor markers were that: CAl25 0 – 35 U/mL, CYFRA21–1 0 – 3.3 ng/mL, CEA 0 – 5 μg/L, NSE 0 – 15.2 ng/mL, Pro-GRP 0 – 40 pg/mL, SCC 0 – 1.5 ng/mL.
Statistical Analysis
For quantitative data, if consistented with normal distribution, the mean and standard deviation were used to describe. If it was abnormal distribution data, the median was used to describe. Differences were evaluated by t test in different groups. Positive rate was compared by chi-square test. In addition, hierarchical clustering analysis was performed to classify the 6 indicators. All statistical analysis was used SPSS18.0 software. Statistical significance was defined as P < 0.05.
RESULTS
Patient Characteristics
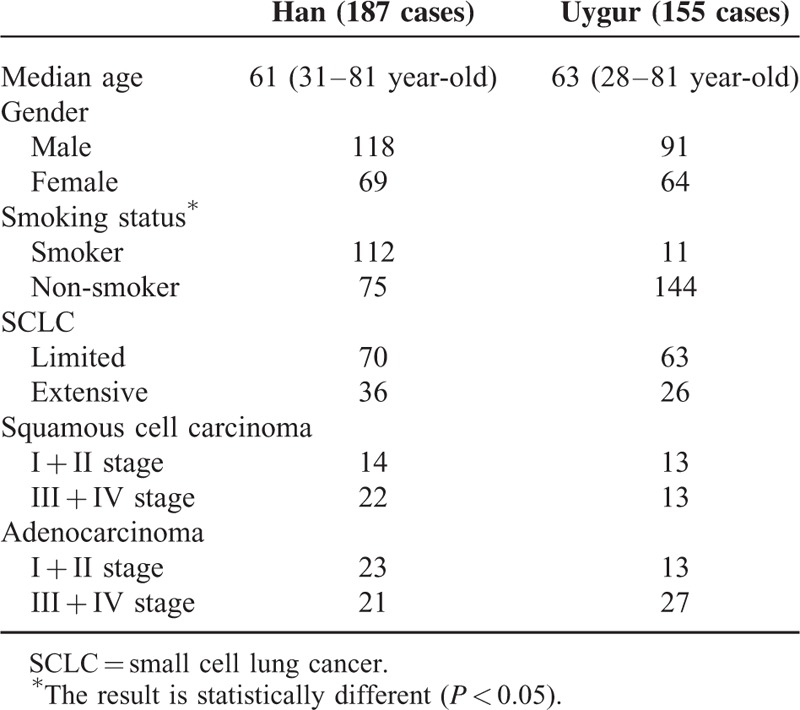
A total of 342 cases enrolled in the trial including 195 cases of SCLC and 147 cases of NSCLC. NSCLC included 62 squamous cell carcinoma and 85 adenocarcinoma cases. Age ranged from 28 to 81 years old, the median age was 6 years old. Clinical characteristics of patients were shown on Table 1.
TABLE 1.
The Clinical Characteristics of 342 Cases Lung Cancer Patients in 2 Populations
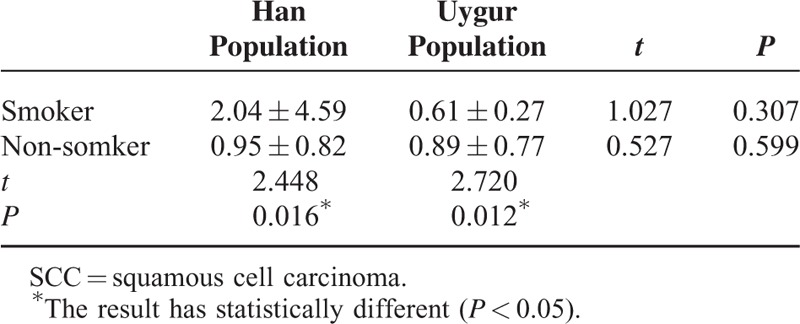
Serum Level of Tumor Markers
The levels of 6 tumor markers were compared with different gender, age, nationality, smoking status, and so on, the results were shown on Table 2. For gender and age, the levels of all 6 tumor markers had no statistically significant. SCC levels were higher in smokers than non-smokers and also higher in the Han than the Uygur. So, we speculated that smoking should be the influence factor to create the difference between Han and Uygur population. In order to confirm that the difference of the smoking ratio in 2 populations created the differences of SCC. The SCC was compared between different smoking statuses in 2 populations; the result was shown on Table 3. So, it was sure that smoking was the confounding factor to create the difference between Han and Uygur population.
TABLE 2.
The Compare of Serum Tumor Markers Level
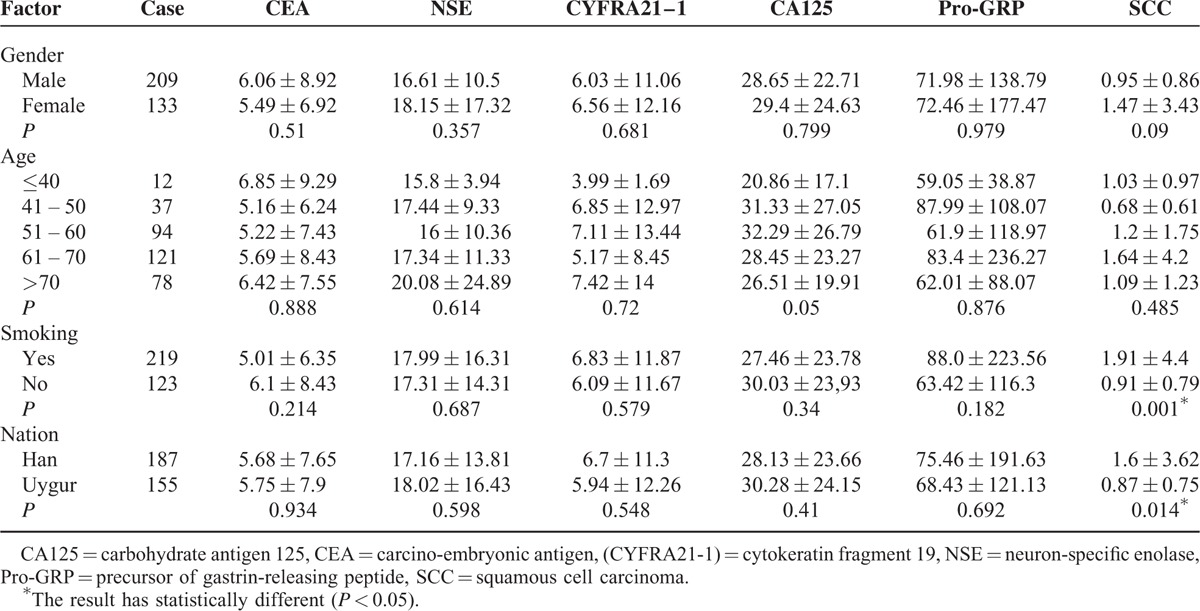
TABLE 3.
The Compare of SCC in Different Smokers Between 2 Populations
When 1 or more in 6 tumor markers exceeded the reference value, the results were considered as the positive, the different positive ratios also were compared with different gender, nationality, and smoking status, the results were shown on Table 4, all of them had no statistic difference.
TABLE 4.
The Positive Rate of Serum Tumor Markers Within Subgroups
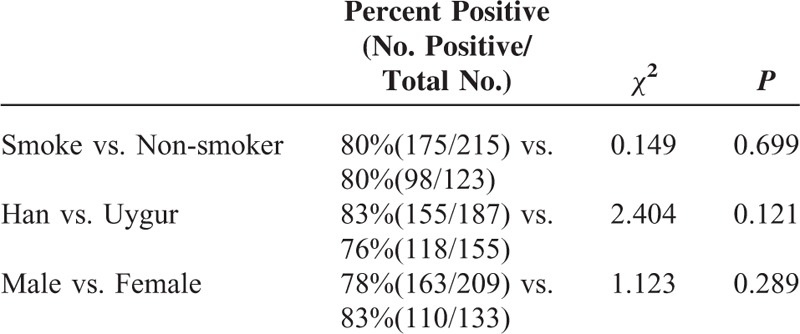
Combined with the results on Tables 2–4, it could be unified to research the application value of the 6 indicators for the Han and Uygur population.
The Application Value of the 6 Tumor Marker in Xinjiang Population
Cluster Analysis About 6 Tumor Markers
Cluster analysis was performed using the 342 cases of lung cancer to cluster analysis the 6 tumor markers, the 6 tumor markers were automatically divided into 2 types using SPSS18.0 software when no pre-determined clustering kinds of cases. The clustering histogram was shown in Figure 1. In Figure 1, NSE and Pro-GRP were 1 category and the other 4 tumor markers were the second category. It was consistent with the fact that Pro-GRP and NSE were more useful for SCLC while the other 4 markers were better to detect NSCLC.
FIGURE 1.
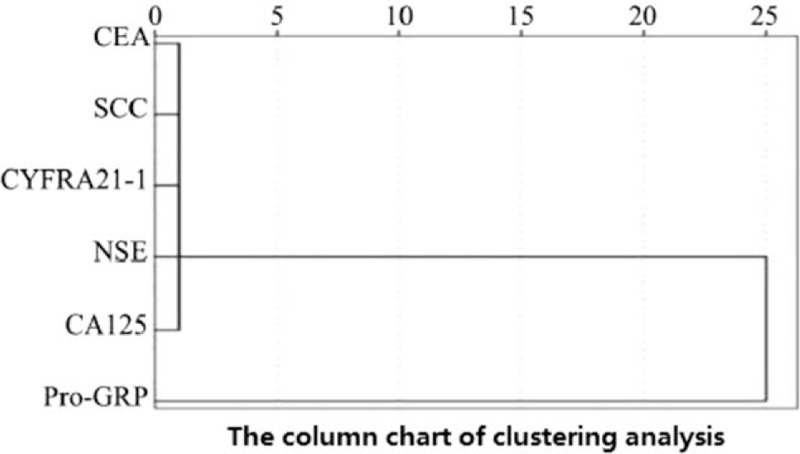
The clustering analysis column of 6 lung cancer tumor markers.
The Diagnosis Value of Serum Tumor Markers
The positive rate of each individual tumor marker to diagnose the lung cancer types (SCLC and NSCLC) was shown in Figure 2.
FIGURE 2.
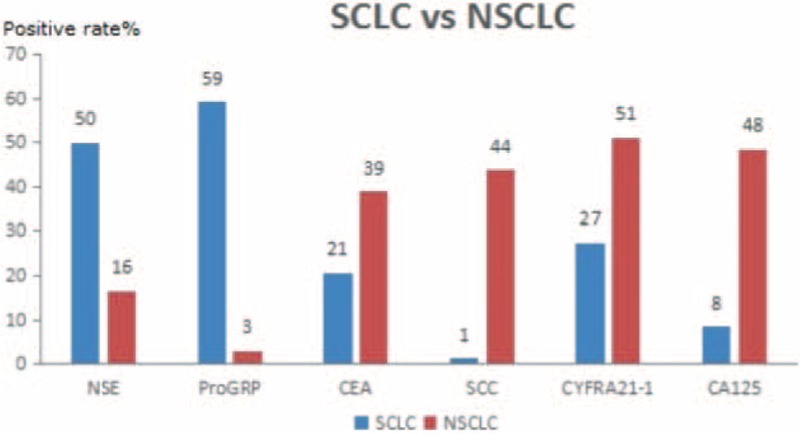
Sensitivity of 6 tumor markers for diagnosis of SCLC and NSCLC.
For positive rate, the most suitable diagnostic indicators were NSE and Pro-GRP for SCLC patients, but CEA, CA125, CYFRA 21-1, and SCC were more better compared with NSE and Pro-GRP for NSCLC patients. The results were consistent with the result of cluster analysis.
In addition, Pro-GRP had lower false positive rate than NSE in SCLC patients, since NSE had higher positive ratio in NSCLC patients (the positive of NSE was 16% compared with 3% of Pro-GRP in NSCLC). In NSCLC patients, CA125 and SCC had lower false positive rate than CEA and CYFRA21-1, also because of the higher positive in SCLC patients (the positive ratios of CEA and CYFRA21-1 were 21% and 27%, compared with 1% and 8% of SCC and CA125).
Then, further to discuss the relationship between 6 tumor markers and clinical stage of lung cancer (in Figures 3 and 4). For SCLC, Pro-GRP, and NSE had the same positive rate to diagnose the extensive stage, but Pro-GRP had higher positive rate than NSE to detect limited stage. CA125 has the highest positive rate for I and II stage of NSCLC, and CYFRA21-1 has the highest positive rate for III and IV stage of NSCLC.
FIGURE 3.
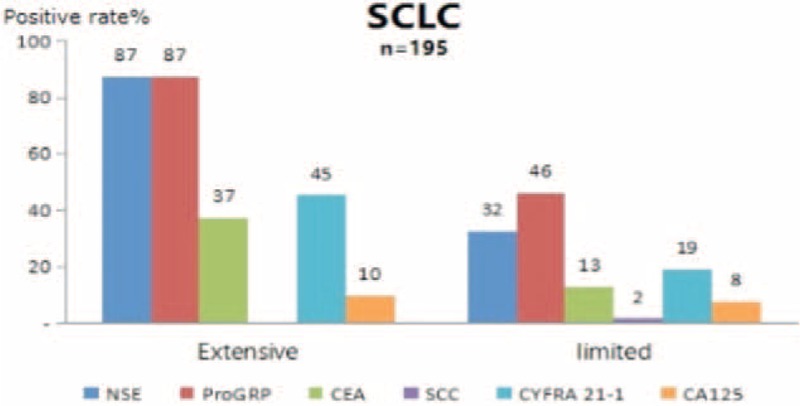
Sensitivity of 6 tumor markers for diagnosis of SCLC in different clinical stages.
FIGURE 4.
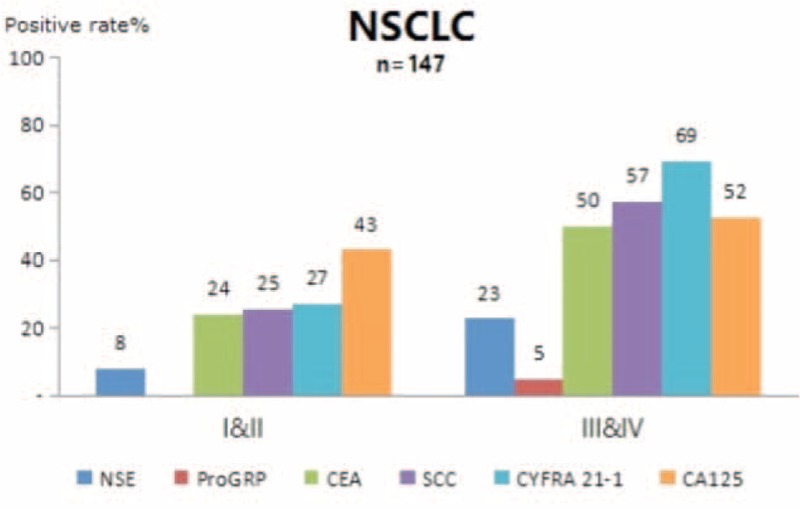
Sensitivity of 6 tumor markers for diagnosis of NSCLC in different clinical stages.
At last, in this study, NSCLC was divided into adenocarcinoma and squamous cell carcinoma, CEA, CA125, CYFRA21-1, and SCC were used to identified the 2 histopathological type (in Figure 5), CEA and CA125 had higher positive rate for adenocarcinoma, CYFRA21-1, and SCC had higher positive rate in squamous cell carcinoma.
FIGURE 5.
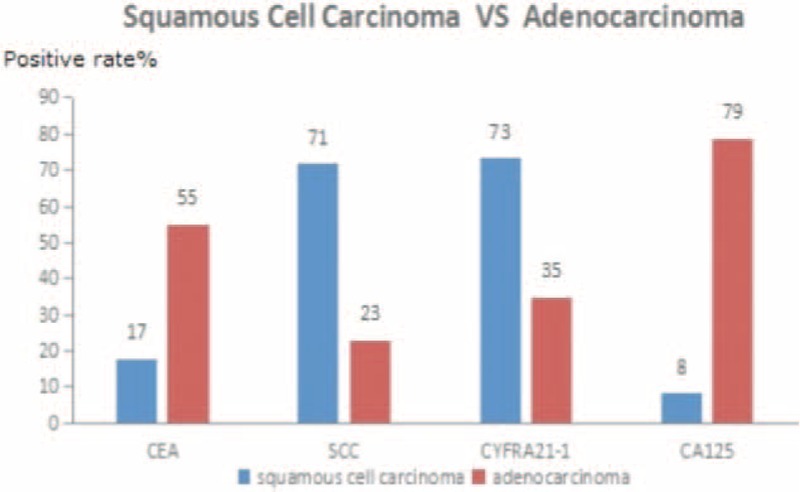
Sensitivity of 6 tumor marker for squamous cell carcinoma and adenocarcinoma.
DISCUSSION
In this retrospective study, the levels of 6 tumor markers were evaluated in the patients which diagnosed as lung cancer. Firstly, the clinical characteristics of the Han and Uygur patients have been compared, only the smoking status had a significantly difference between the Han and Uygur population. Early stage patients for both SCLC and NSCLC (including I/II stage and limited stage) were more common than advanced stage patients, SCLC patients were more common than NSCLC patients, adenocarcinoma was more common than squamous cell carcinoma. These patient distributions were not typical in the all lung cancer populations as reported in many studies. This study was performed in the top specialized tumor hospital in the Xinjiang area. The early stage, SCLC, and adenocarcinomas patients, which were difficult to diagnose and treat, were transferred to this hospital from other primary hospital and general hospital in order to better diagnosis and treatment.
The levels of tumor markers in lung cancer patients had no differences in different gender and age groups. Only SCC had statistically differences in different nationality and smoking groups. For the nation, SCC was obviously higher in Han than Uygur patients, the percentage of smokers in Han population was also higher than Uygur population. So, we speculated that smoking should be the confounding factor to create the difference between Han and Uygur population. Further analysis, there was not difference in smoker between Han and Uygur population, also in non-smoker between Han and Uygur population. So, it was sure that smoking was the confounding factor to create the difference between Han and Uygur population. Removed the confounding factor, we could think that SCC had no difference between 2 nations. So, it could be unified to research the application value of the 6 indicators for the Han and Uygur population.
The report to evaluate lung cancer related tumor markers by cluster analysis was rare, this study firstly analyzed the 6 tumor markers by cluster analysis, which revealed 2 clusters, the first including NSE and Pro-GRP, the second including CEA, CA125, SCC, CYFRA21–1. These results were consistent with the reports in this and other studies about lung cancer related tumor markers.
For both SCLC and NSCLC, the positive rates of every tumor markers were higher along with increasing clinical stage.15–16 For SCLC, the most suitable diagnostic markers were NSE and Pro-GRP, and the 2 indicators had highest positive rate in extensive stage, Pro-GRP was better than NSE in ability to detect limited disease. So, we could view that Pro-GRP was helpful to diagnose the clinical stage.17
For NSCLC, the positive rates were higher in squamous cell carcinoma than adenocarcinoma, for the squamous cell carcinoma of lung cancer, SCC and CYFRA21–1 were better diagnostic indicators. For adenocarcinoma, CEA and CA125 were useful, but the diagnostic value was lower than SCC and CYFRA21–1 for squamous cell carcinoma. CA125 had the highest positive rate in I and II stage of NSCLC, CYFRA21–1 had the highest positive rate in III and IV stage of NSCLC. All of these also consistented with the previous reports.18–19
In summary, we suggested a diagnostic utility of 6 commonly using lung cancer biomarkers in both the Han and Uygur populations in Xinjiang province of People's Republic of China: for a suspected lung cancer patients who could find a pulmonary mass though image examination such as X-ray examination, CT scanning, Magnetic Resonance Imaging, and so on, NSE and Pro-GRP were helpful for the diagnosis of SCLC; Pro-GRP was useful for the diagnosis clinical stage of SCLC. And CEA, CA125, SCC, CYFRA21–1 could be used for diagnosis NSCLC. CEA and CA125 were beneficial to diagnosis adenocarcinoma, CYFRA21–1 and SCC are squamous cancer, CA125 and CYFRA21–1 were beneficial for the diagnosis clinical stage of NSCLC.
Footnotes
Abbreviations: CA125 = carbohydrate antigen 125, CEA = carcino-embryonic antigen, CYFRA21–1 = cytokeratin fragment 19, NSCLC = non-small cell lung cancer, NSE = neuron-specific enolase, Pro-GRP = precursor of gastrin-releasing peptide, SCC = squamous cell carcinoma, SCLC = small cell lung cancer.
FYC and FM contributed equally to the work.
The material contained in the manuscript has not been previously published and is not being concurrently submitted elsewhere.
The authors have no financial conflicts of interest to dislcose.
REFERENCES
- 1.You-sheng MAO, Yan-ning GAO, Jie HE, et al. Association of molecular biology of lung cancers and their metastasis and prognosis. Chin J Oncol 2006; 8:632–634. [PubMed] [Google Scholar]
- 2.Anthony, Malcolm V Brock, Jean G Ford, et al. Epidemiology of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of chest physicians evidence-based clinical practice guidelines. Chest 2013; 143 Suppl 5:e1S–e29S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brenda K Edwards, Anne-Michelle Noone, Angela B Mariotto, et al. Annual report to the nation on the status of cancer, 1975-2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast or prostate cancer. Cancer 2014; 120:1290–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denise Riedel Lewis, David P Check, Neil E Caporaso, et al. U.S. lung cancer trends by histologic type. Cancer 2014; 120:2883–2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng-Ming Chen, Richard Peto, Andri Iona, et al. Emerging tobacco-related cancer risks in China: a nationwide, prospective study of 0.5 million adults. Cancer 2015; 121 Suppl 17:3097–3106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bari S, Stock DA, Mclver A, et al. Symptoms in lung cancer: do they help the diagnosis? Thorax 2005; 60:314–315.15790987 [Google Scholar]
- 7.Henschke CI, Yankelevitz DF. CT screening for lung cancer: update. Oncologist 2008; 13:65–78. [DOI] [PubMed] [Google Scholar]
- 8.Yang YJ, Cheng DY, Fang X, et al. The clinical diagnosis value of fibro-optic bronchoscope examination combined with tumor marker determination to lung cancer. J Sichuan Univ (Med Ed) 2007; 38:312–315. [PubMed] [Google Scholar]
- 9.Li CS, Cheng BC, Ge W, et al. Clinical value of CYFRA21-1, NSE, CA15-3, CA19-9 and CA125 assay in the elderly patients with pleural effusions. Blackwell Publishing Ltd Int J Clin Pract 2007; 61:444–448. [DOI] [PubMed] [Google Scholar]
- 10.Rafael Molina. ProGRP: A new biomarker for small cell lung cancer. EJCMO 2009; 1:25–32. [Google Scholar]
- 11.Hui-jie Yang, Ying Gu, Chu Chen, et al. Diagnostic value of pro-gastrin-releasing peptide for small cell lung cancer: a meta-analysi. Clin Chem Lab Med 2011; 49:1039–1046. [DOI] [PubMed] [Google Scholar]
- 12.April Scott, Ravi Salgia. Biomarkers in lung cancer: from early detection to novel therapeutics and decision making. Biomark Med 2008; 2:577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rong Wang, Guoqing Wang, Nan Zhang, et al. Clinical evaluation and cost-effectiveness analysis of serum tumor markers in lung cancer. Biomed Res Int 2013; 2013:195692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Xiumei, Wu Tao, Zhao Yan, et al. Disease composition analysis on malignant tumor inpatients in a hospital of Xinjiang from 2010 to2013. Chin Med Rec 2014; 15:60–62. [Google Scholar]
- 15.Rafael Molina, Jose Maria Auge, Jose Miguel Escudero, et al. Mucins CA 125, CA 19-9, CA 15-3 and TAG72-3 as tumor markers in patients with lung cancer: comparison with CYFRA 21-1, CEA, SCC and NSE. Tumor Biol 2008; 29:71–80. [DOI] [PubMed] [Google Scholar]
- 16.Zhao W, Yu H, Han Z, et al. Clinical significance of joint detection of serum CEA, SCCA, and bFGF in the diagnosis of lung cancer. Int J Clin Exp Pathol 2015; 8:9506–9511. [PMC free article] [PubMed] [Google Scholar]
- 17.Hirose T. Are levels of pro-gastrin-releasing peptide or neuron-specific enolase at relapse prognostic factors after relapse in patients with small-cell lung cancer. Lung Cancer 2010; 10:10–16. [DOI] [PubMed] [Google Scholar]
- 18.Cedrés S, Nuñez I, Longo M, et al. Serum tumor markers CEA, CYFRA21-1, and CA-125 are associated with worse prognosis in advanced non-small-cell lung cancer (NSCLC). Clin Lung Cancer 2011; 12:172–179. [DOI] [PubMed] [Google Scholar]
- 19.Wang B, He YJ, Tian YX, et al. Clinical utility of haptoglobin in combination with CEA, NSE and CYFRA21-1 for diagnosis of lung cancer. Asian Pac J Cancer Prev 2014; 15:9611–9614. [DOI] [PubMed] [Google Scholar]


