Abstract
Early menarche is strongly associated with adulthood obesity; however, the relationship between age at menarche and cardiovascular disease (CVD) in Korean women remains poorly understood. Here, we investigated the association between early menarche and risk factors for developing CVD during adulthood using a nationwide population database.
In total, 12,336 women (weighted n = 17,483,406; weighted age, 45.7 years) who participated in the Korean National Health and Nutrition Examination Survey 2010 to 2013 were included in this study. Participants were scored using the National Cholesterol Education Program Adult Treatment Panel III criteria for metabolic syndrome. Risk of CVD was estimated using the 10-year Framingham Coronary Heart Disease Risk Point Scale (10-year FRS).
Early menarche (≤11 years) was reported in 5.2% (weighted n = 917,493) of subjects. The weighted prevalences of metabolic syndrome and ≥20% 10-year FRS were 23.6% [95% confidence interval (95% CI), 22.7–24.6] and 7.7% (7.1–8.3), respectively. Women with early menarche reported a significantly higher body mass index and waist circumference, along with a higher prevalence of hypertension, diabetes, and metabolic syndrome than those with later menarche (≥13 years). Furthermore, the prevalence of women with a ≥10% or ≥20% 10-year FRS was higher in those with early menarche than in other groups after adjusting for age, smoking, education level, and menstruation. Logistic regression analyses controlling for these and other confounding factors revealed odds ratios of 2.29 (95% CI = 1.25–4.19) and 1.78 (0.96–3.30) for ≥10% and ≥20% 10-year FRS in women with early menarche, respectively, compared with those in the latest menarche group (≥17 years).
Taken together, this nationwide study revealed that women with early menarche are at increased risks of metabolic syndrome and CVD. Early menarche may therefore represent an important marker for early preventive interventions.
INTRODUCTION
Although total cardiovascular disease (CVD) mortality rates have been decreasing steadily over the past 3 decades, CVD remains the leading cause of death in Korea, with crude mortality rates for women exceeding those of men since 1992.1 Many studies have suggested that modification of risk factors for CVD, such as smoking, hypertension, and dyslipidemia, may be responsible for the decrease in CVD mortality in developed countries.2 However, among women, several other independent risk factors have been associated with an increased risk of CVD, including hormonal status, such as menarche, gestation, and menopause.3
Menarche, the onset of first menstruation in girls, represents a distinct event in puberty. Because reproduction requires a sufficient energy supply to maintain gestation, metabolic status, which is indicative of energy reservoirs, may be a logical signal driving the onset and timing of menarche in women.3 In recent decades, the age at menarche has decreased steadily worldwide, including in Korea.4 There is growing evidence that women who experienced menarche at an early age are at increased risks of obesity, type 2 diabetes (T2DM), CVD, and all-cause mortality in later adult life.5–7
Although previous studies have suggested associations between early menarche and T2DM, obesity, and metabolic syndrome in both pre- and postmenopausal women in Korea,8,9 these studies have been limited in scale. Our hypothesis was that CVD risk varies according to menarcheal ages. Accordingly, the purpose of our study was to test this hypothesis by comparing the risk factors associated with CVD, namely the component of metabolic syndrome and its prevalence, and subsequently an index of CVD risk factors, including the 10-year Framingham Coronary Heart Disease Risk Point Scale (10-year FRS) and investigate the associations of those according to the age at menarche in Korean women.
METHODS
Study Design and Participants
Study Population
The survey target population was all noninstitutionalized South Korean civilian individuals aged 1 year or older. The study population and survey methods have been described previosuly.10 Briefly, KNHANES surveys have been conducted triennially between 1998 and 2005, and then annually since 2007. The KNHANES (2010–2013) uses a stratified, multistage probability sampling units that were based on geographic area, gender, and age, which were determined by the household registries of the 2005 National Census Registry. The sample design of the KNHANES has changed annually, and combination of any consecutive year could be representative national sample since 2007. The total target population consisted of 18,291 women aged ≥19 years (13,918 in KNHNES V; 2010–2012, and in 4373 in 2013), of whom 33,552 people (25,534 in KNHNES V; 2010–2012, and in 8018 in 2013) completed the survey. The institutional review board of Ilsan Paik Hospital, Republic of Korea (No. 2015-12-008) approved this study. We excluded information from 3701 individuals aged 1 to 18 years, and information from 12,366 women had participated in the laboratory examination were included in the final analyses. KNHANES includes a standardized health interview using well-established questions to determine the demographic and socioeconomic characteristics of all subjects, including menstruation history. Age at menarche was defined as age at the first menstrual period, as determined on the basis of a participant's response to the survey question “At what age did you have your first menstrual period (menarche)?” Age at menarche was defined as the age at the start of menstruation by counting age in full. Women reported their age at menarche in single years and were classified for this study as having an age at menarche of ≤11, 12, 13, 14, 15, 16, or ≥17 years. Specific age to define early menarche is not definitive but various from 9 to 12 years depend on population and design of each study.4,7,11,12 In this study, we assumed that early menarche could be defined to first 5th percentiles of the observed distribution of age at menarche in our population. Women who smoked regularly during the previous 12 months were classified as current smokers. Heavy alcoholic drinking was defined as drinking 20 g or more of pure alcohol per day within the last year. Regular exercise was defined as moderate exercise 5 or more times per week or strenuous exercise 3 or more times per week, sustained for at least 30 minutes per session.
Sample Size
In the KNHNES, the target population, at which the survey is aimed, comprises noninstitutionalized citizens residing in Korea. The sampling was conducted by a multi-stage clustered probability design: primary sampling unit, households, and individuals. The sample size was 12,336 women. The statistical power was calculated using a variety of equations after the study had been conducted because the sample was collected before calculating the sample size.13 This statistical power is based on the prevalence of women with 10-year FRS ≥10% as an outcome between groups with early menarche and others. Using this value and assuming a significance level of 5%, the power of the test was 97.8%.
Definition of Metabolic Syndrome and Assessment of CVD Risk
Metabolic syndrome was defined according to the criteria of the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATPIII) guidelines.14 Under these guidelines, the presence of any 3 of the following 5 factors is required for a diagnosis of metabolic syndrome: waist circumference (WC) ≥90 cm in men or ≥80 cm in women, hypertriglyceridemia (triglyceride, TG ≥150 mg/dL), low high-density lipoprotein cholesterol level (HDL ≤50 mg/dL for women), elevated blood pressure (BP) (systolic BP ≥130 mm Hg and/or diastolic BP ≥85 mm Hg, or current use of antihypertensive drugs), and impaired fasting plasma glucose level (≥100 mg/dL or use of glucose-lowering medication). The 10-year FRS scores, incorporating age, total cholesterol (TC), smoking status, HDL-C level, and systolic BP, stratified by gender, were used to predict the 10-year absolute risk of developing coronary heart disease.14 To calculate the score for an individual, a point value was assigned for each risk factor.
Statistical Analysis
All data are presented as weighted means and 95% confidence intervals (CIs) or standard error of mean (SEM) unless otherwise specified. To represent the Korean population, we used sample weight provided by the Korean Center for Disease Control on the basis of Korean National Census Registry data in 2005 as the reference population.10 Analysis of covariance (ANCOVA) was used to compare the weighted age-adjusted anthropometric, clinical, laboratory characteristics and the prevalence of abdominal obesity, hypertension, diabetes, metabolic syndrome, or those with ≥10% or 20% of 10-year FRS according to age at menarche. A CI was calculated for each parameter using the value of alpha = 0.05. The Bonferroni method was also used to determine significant differences between groups as a posthoc test. Confounding factors were controlled for in the analyses as required, depending on the outcome response of interest. Logistic regression analyses were performed to determine the odds ratios (ORs) for age at menarche with age ≥17 years as the reference assuming linear relationships between age at menarche and obesity, hypertension, diabetes, and risk of CVD, with 17 years of age as the reference group (Table 1). The likelihood ratio test was used to measure the goodness-of-fit of the model. All analyses were performed using IBM SPSS Statistics 21 (IBM, Armonk, NY).
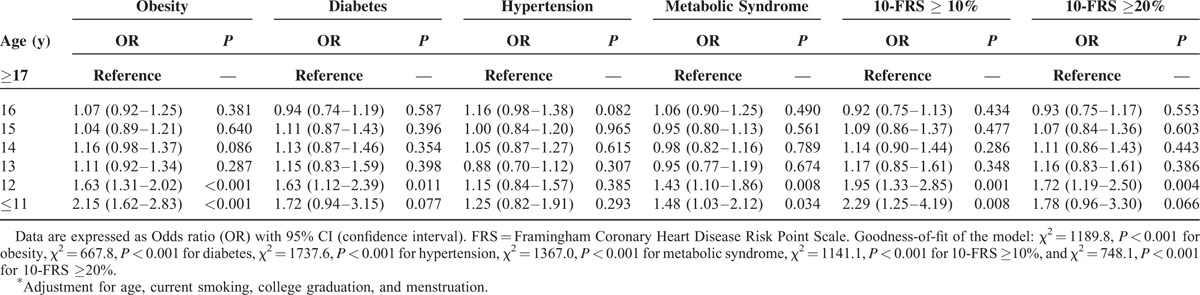
TABLE 1.
Logistic Regression Analyses for the Presence of Obesity, Diabetes, Metabolic Syndrome, and Framingham Risk With Age at Menarche∗
RESULTS
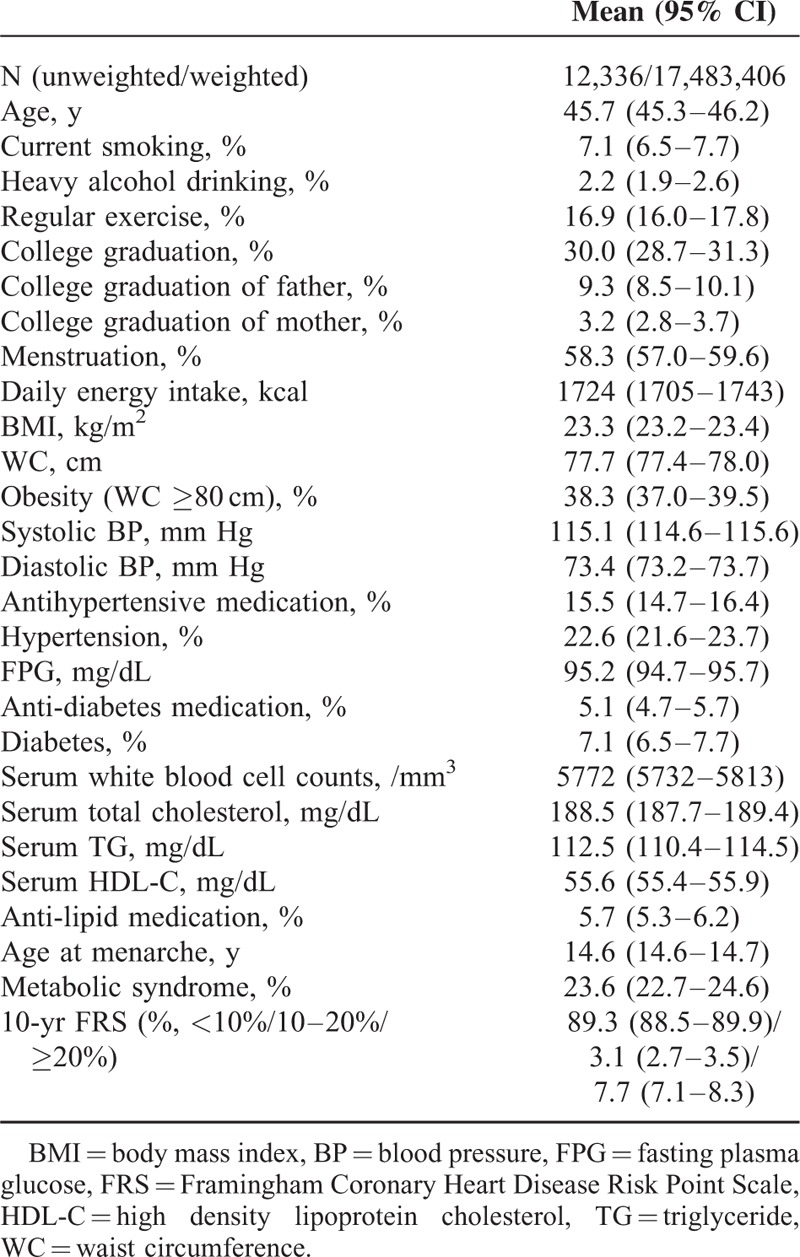
A total of 12,336 women (weighted n = 17,483,406) aged 45.7 years (95% CI, 45.3–46.2 years) and with a BMI of 23.3 kg/m2 (23.2–23.4 kg/m2) were included in this study. Anthropometric, clinical, and laboratory characteristics are presented in Table 2. The mean (SEM) age at menarche was 14.61 years (0.03) self-reported and rounded down to the nearest whole year. Among the study participants, 508 women reported menarche at ≤11 years of age, 1138 at 13 years of age, 1867 at 13 years of age, 2257 at 14 years of age, 2086 at 15 years of age, 1664 at 16 years of age, and 2816 at ≥17 years; the mean age at the time of the survey increased along with increasing age at menarche (mean 30.9, 34.2, 39.1, 42.3, 46.7, 53.0, and 59.7 years, respectively). For the purposes of this study, early menarche was defined as menarche at or before 11 years of age, accounting for 5.2 % (weighted n = 917,493) of all women in this analysis. The weighted, age-adjusted prevalence of metabolic syndrome and 10-year FRS ≥20% for this group were 23.6% (95% CI, 22.7–24.6) and 7.7% (7.1–8.3), respectively.
TABLE 2.
Weighted Clinical Characteristics of Korean Women
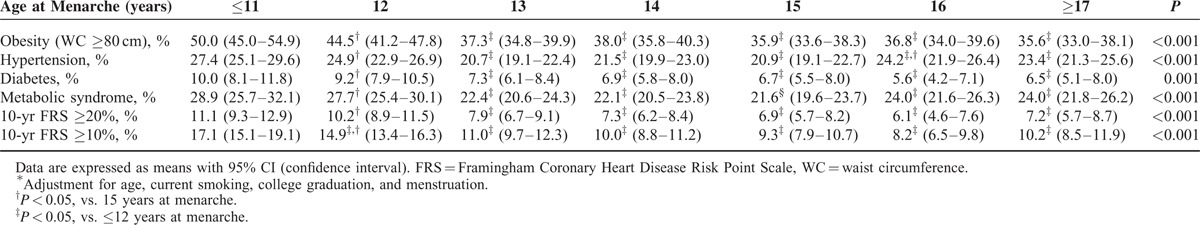
The weighted, age-adjusted demographics, and clinical characteristics of all study participants by age at menarche are summarized in Table 3. Women with early menarche were younger, more likely to have a higher education level, as well as higher parental education levels, and more likely to be smokers and being menstruation across age at menarche categories. In addition, women with early menarche were more likely to exhibit a higher BMI, WC, and white blood cell counts, relative to the other groups. The prevalences of hypertension, diabetes, and metabolic syndrome were higher in women with early menarche than in women with menarche at age 13 years or older (all Ptrend < 0.01). Both ≥10% and ≥20% 10-year FRS exhibited linear decreases in relation to age at menarche between 12 and 16 years of age. These tendencies toward higher prevalences of abdominal obesity, hypertension, diabetes, metabolic syndrome, and 10-year FRS ≥10% or ≥20% from ≤12 to ≥17 years of ages at menarche showed statistically significant after adjusting for age, smoking, college graduation, and menstruation (Table 4). Although the prevalence of metabolic syndrome in women with menarche at age 17 years (25.1%, 95% CI = 22.9–27.3) higher than those at age 15 years (21.5%, 19.5–23.6) in posthoc analysis in weighted age-adjusted comparison (P = 0.019; Table 3), the statistical significance was lost after adjustment for confounding factors (P = 0.113; Table 4).
TABLE 3.
Weighted Age-Adjusted Clinical Characteristics in Korean Adult Women by Age at Menarche
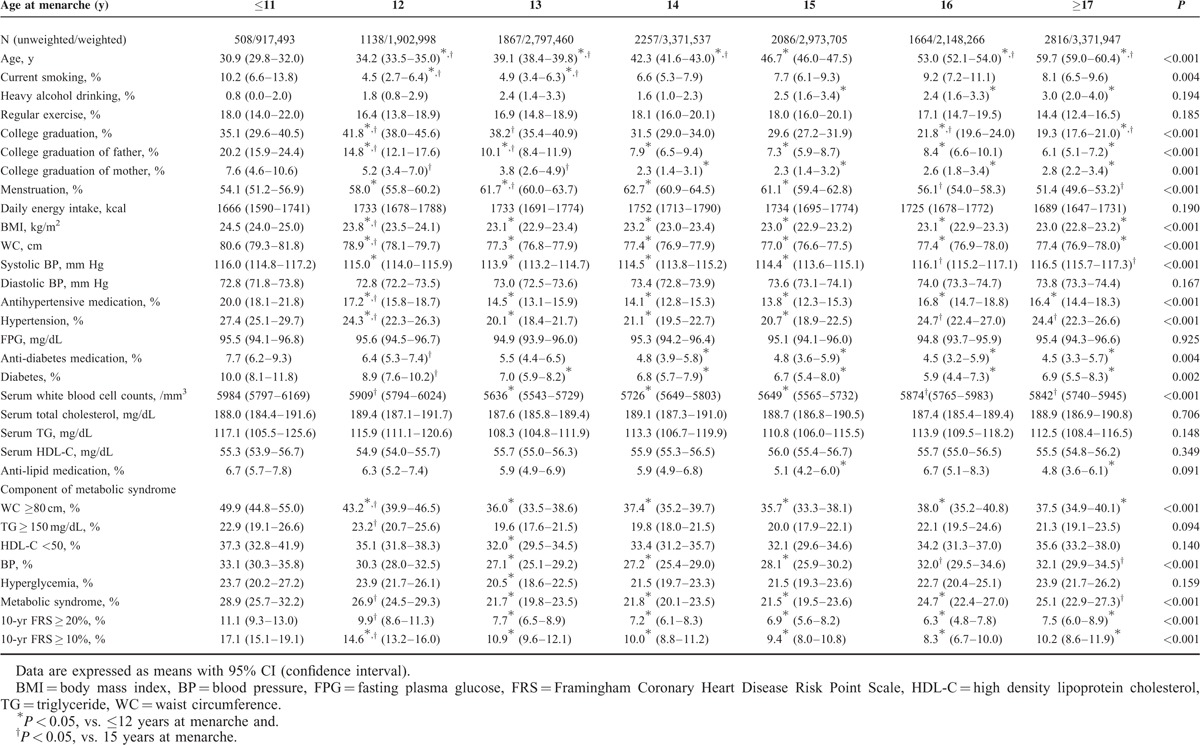
TABLE 4.
Weighted-Adjusted Clinical Characteristics in Korean Adult Women by Age at Menarche∗
Logistic regression analysis of age at menarche, in which age was treated as a categorical variable, grouping by year, revealed association with presence of obesity, diabetes, and metabolic syndrome, and 10-year FRS in groups of menarcheal age 12 and ≤11 years old compared with reference group age ≥17 years old: a strong association between early menarche (age ≤11 years) and increased risks of obesity (OR, 2.15, 95% CI 1.62–2.83), diabetes (1.72, 0.94–3.15), hypertension (1.25, 0.82–1.91), metabolic syndrome (1.48, 1.03–2.12), and ≥10% 10-year FRS (2.29, 1.25–4.19) compared with those in the latest menarche group (≥17 years), after adjusting for age, smoking, college graduation, and menstruation (Table 1).
DISCUSSION
In this nationwide survey, we observed that early menarche, that is, menarche at or before 11 years of age, was associated with higher prevalences of obesity, diabetes, and metabolic syndrome, along with an increased risk of CVD with age. In particular, the adjusted risk of CVD, that is, a ≥10% Framingham 10-yr risk score, was associated with women with early menarche relative to those in the latest menarche group (≥17 years) (OR, 2.29, 95% CI = 1.25–4.19, P = 0.008). Even after adjusting for age, smoking, college graduation, and menstruation, the prevalences of abdominal obesity, hypertension, diabetes, metabolic syndrome, and a ≥10% or 20% 10-year FRS were higher in women with earlier menarche than those undergoing menarche at ages 13 to 17 years. Taken together, these findings suggest a significantly increased risk of CVD in women who experience earlier menarche, independent of various potential confounders.
Several studies have examined the association between age at menarche and risk of CVD. Although a relationship between early menarche and adult obesity has been observed in other studies, it is uncertain whether early menarche increases the risk of CVD later in life of Korean women. The data presented here are in strong agreement with population studies that showed increased risks of abdominal obesity, diabetes,15 and metabolic syndrome16 in women experiencing menarche at an earlier age. The results of our study are also consistent with those of a recent meta-analysis,17 which found that earlier menarche was associated with a higher risk of all-cause mortality. However, despite these strong associations, contradictory findings have also been reported, with disagreements in terms of outcomes confounded by smoking,18 premenarcheal obesity,19 and other vascular outcomes by different measures.17 A large prospective study of women in the UK found that the relative risks for coronary heart disease were 1.27 (95% CI, 1.22–1.31) for menarche at age ≤10 years compared with 1.23 (1.16–1.30) for menarche at age ≥17 years, and showed the U-shaped relationship of age at menarche with the magnitudes of these associations similar across all subgroups for outcomes such as coronary heart disease, cerebrovascular disease, and hypertension, after adjusting for cofactors such obesity, smoking, and socioeconomic status.7 Although women with late menarche (≥17 years of age) tended to be elder and have higher prevalence of hypertension and lower level of HDL-C than those with menarche at 15 years age in this study (Table 3), the prevalence of metabolic syndrome or ≥10% or 20% 10-year FRS was not different after adjustment for confounding factors (Table 4). These differences in the relationship between age at menarche and risk of CVD may be reflective of the difference of individual study populations, with variability seen in the mean age at menarche among populations, cultural groups, socioeconomic status, and outcomes variables. Other factors, such as differences in statistical methods and adjustment for confounding factors, are also likely to have affected the outcomes.
Previous findings from the Kangwha cohort study (1985–2005) investigating the relationship between reproductive factors and the risk of CVD mortality in 3257 postmenopausal Korean women (mean age, 66.8 ± 8.3 years) observed a 51% reduction in mortality associated with coronary heart disease in women with early menarche (<17 years of age at menarche) compared with those with menarche at 17 years old, after controlling for confounding factors, such as age at enrollment, BMI, drinking status, smoking status, education, and occupation.12 However, the mean age at menarche was 17.6 ± 1.7 years and only included women born before 1930 in that study, thereby avoiding the trend of decreasing age at menarche by several decades. This distinction is important, as it has been reported that age at menarche in Korean girls has been decreasing at a rate of 0.726 years per decade since the period of 1925 to 1934 (R2 = 0.600; 95% CI, −0.745 to −0.706; P < 0.01) due to economic development and nutritional sufficiency, consistent with trends seen in many western countries.4 As shown in this study, the age at menarche was decreased along the women's age with statistical significance reflecting the decreasing secular trend of menacheal age (Table 3, P for tend <0.01). Compared with previous study,12 most of women in this study had born after Korean War and during the economic development in Korea (1950–1970). The novelty of our study stems from its recent, large sample size, which is reflective of the Korean population as a whole, and its sufficient statistical power to identify groups at an increased risk of CVD.
Age at menarche is associated with a variety of biological and socioeconomic factors during childhood as well as early life of infancy, such as weight gain in the first few weeks to months of life and throughout childhood obesity influenced by gestational diabetes or weight gain, breast feeding, genetic inheritance, individual behaviors, natural environment, and chemical exposures, parents’ education level, or psychological factors.3,20,21 Among them, there are growing body of evidence suggesting the relationship between weight gain in early life and subsequent childhood obesity and early menarche. The Cardiovascular Risk in Young Finns Study (n = 794) found that early menarche predicted high BMI in adult after adjustment for other risk factors for CVD, but this association was lost after adjustment for premenarcheal BMI in the analysis of women with measurement of baseline BMI (n = 341).19 And, higher weight gain at ages of 3 and 5 years associated with obesity in adolescent in 468 French adolescents (ages, 8–17 years),22 and higher fat mass in adults was predicted by excess weight gain between ages 2 and 11 years in 1917 Finnish adults.23 In other aspect of childhood obesity, studies from Project Viva, prospective, cohort study of pregnant women and their children, found that rapid weight gain against length in the early life (≤6 months) was associated with obesity in children at age 3 years. More-rapid increases in weight for length in the first 6 months of life were associated with sharply increased risk of obesity at 3 years of age.24 Collectively, these findings suggested that obesity or weight gain in the first 6 months of life associated with childhood obesity, and that could cause the early menarche later. With those studies, early menarche seems to be a risk marker of increased risk of CVD in adult as a consequence of obesity at early life or childhood.19,25 Therefore, these time-sequencing relationships remain to be defined by well-constructed, prospective studies in Korea. Here, we also observed a strong association between age of menarche and parental education levels, consistent with a previous study.26
Several mechanisms may collectively explain the association between early menarche and increased risk of CVD, namely abdominal obesity, hypertension, diabetes, and metabolic syndrome. Menarche is followed by an increase in adiposity, and early menarche is associated with increased obesity and insulin resistance in adolescence, which may persist into adulthood.19,27 Leptin, an important signal of energy sufficiency, modulates the release of gonadotropin-releasing hormone (GnRH) from the hypothalamus. Insulin also affects GnRH release, along with the subsequent development of the reproductive system.28 Given these effects, insulin or lower cord blood leptin level or leptin resistance in childhood is thought to play an important role in the onset of menarche and the increased risk of CVD in later in life.29,30 As the KNHANES data did not include details regarding the BMI of women during childhood, we were unable to determine whether higher childhood BMI drives the association between age at menarche and CVD risk in adulthood. Other factors, such as higher levels of female sex hormones, abdominal obesity, and insulin resistance, have been associated with inflammation and atherosclerosis,31 consistent with the higher levels of white blood cells seen in this study; however, the causal relationship between age at menarche and CVD remains uncertain.
There are several limitations to our study. The main limitation of our study is its cross-sectional design: this study establishes association at most, not causality in discovering etiologic factors of disease but can help identify preliminary relationships that other analytic designs may explore further studies. And we were unable to collect any anthropometric data at childhood as well as follow-up data, as menarche, which could affect age of menarche and adverse health outcome of later life.32 Second, because age at menarche was assessed by recall, we should consider about the actual age of menarche of women in this study. However, it has been shown that age at menarche has a high correlation with prospectively assessed childhood data.33,34 We also did not include the parity of women as a confounding factor. Although the relationship between the duration of exposure to estrogen and CVD mortality is not fully understood, we did control for menopause as a confounding factor in this analysis. To verify the role of estrogen exposure in the development of CVD, additional studies will be necessary, with researchers controlling for confounding factors, such as parity, gestational events, and hormonal withdrawal or replacement. Despite these limitations, we found a meaningful association between early menarche and obesity, diabetes, metabolic syndrome, and an increased risk for CVD in Korean women broadly representative of the Korean population as a whole. Longitudinal studies that allow for clinical intervention are needed to confirm the effect of early menarche on the morbidity or mortality associated with CVD.
Our findings strengthen the association of early menarche with increased risk factors for CVD in Korean women, with earlier age at menarche potentially serving as an independent risk factor for CVD in adult women. Strategies for comprehensive intervention for girls at menarche during early adolescence may therefore be needed to prevent CVD in adulthood in Korean women.
Footnotes
Abbreviations: KNHANES = Korea National Health and Nutrition Examination Survey, CVD = cardiovascular disease, SEM = standard error of the mean, ANCOVA = analysis of covariance, CI = confidence interval, WHO = World Health Organization, NCEP-ATPIII = the National Cholesterol Education Program Adult Treatment Panel, 10-yr FRS = 10-year Framingham Coronary Heart Disease Risk Point Scale, BMI = body mass index, WC = waist circumference, BP = blood pressure, TG = triglyceride, HDL-C = high density lipoprotein-cholesterol, FPG = fasting plasma glucose, eGFR = estimation of glomerular filtrationrate, OR = odds ratio.
The Priority Research Centers Program through the National Education, Science, and Technology (2010-0020224) supported this study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We especially thank PhD, Sung-Cheol Yun (Division of Biostatistics, Center for Medical Research and Information, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea) for recommendation about statistical analysis.
The authors report no conflicts of interest.
REFERENCES
- 1.Lee SW, Kim HC, Lee HS, et al. Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J 2015; 45:202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim HJ, Kim Y, Cho Y, et al. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998-2012. Int J Cardiol 2014; 174:64–72. [DOI] [PubMed] [Google Scholar]
- 3.Mishra GD, Cooper R, Kuh D. A life course approach to reproductive health: theory and methods. Maturitas 2010; 65:92–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahn JH, Lim SW, Song BS, et al. Age at menarche in the Korean female: secular trends and relationship to adulthood body mass index. Ann Pediatr Endocrinol Metab 2013; 18:60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elks CE, Ong KK, Scott RA, et al. Age at menarche and type 2 diabetes risk the epic-interact study. Diabetes Care 2013; 36:3526–3534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prentice P, Viner R. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes 2013; 37:1036–1043. [DOI] [PubMed] [Google Scholar]
- 7.Canoy D, Beral V, Balkwill A, et al. Age at menarche and risks of coronary heart and other vascular diseases in a large UK cohort. Circulation 2015; 131:237–244. [DOI] [PubMed] [Google Scholar]
- 8.Lim SW, Ahn JH, Lee JA, et al. Early menarche is associated with metabolic syndrome and insulin resistance in premenopausal Korean women. Eur J Pediatr 2016; 175:97–104. [DOI] [PubMed] [Google Scholar]
- 9.Hwang E, Lee K, Cho Y, et al. Association between age at menarche and diabetes in Korean post-menopausal women: results from the Korea National Health and Nutrition Examination Survey. Endocr J 2015; 62:897–905. [DOI] [PubMed] [Google Scholar]
- 10.Won JC, Hong JW, Kim JM, et al. Increased prevalence of albuminuria in individuals with higher range of impaired fasting glucose: the 2011 Korea National Health and Nutrition Examination Survey. J Diabetes Complications 2015; 29:50–54. [DOI] [PubMed] [Google Scholar]
- 11.Cesario SK, Hughes LA. Precocious puberty: a comprehensive review of literature. J Obstet Gynecol Neonatal Nurs 2007; 36:263–274. [DOI] [PubMed] [Google Scholar]
- 12.Chang HS, Odongua N, Ohrr H, et al. Reproductive risk factors for cardiovascular disease mortality among postmenopausal women in Korea: the Kangwha Cohort Study. Menopause 2011; 18:1205–1212. [DOI] [PubMed] [Google Scholar]
- 13.Rosner B. Fundamentals of Biostatistics. Vol 10. 7th ed.2011; Boston, MA: Brooks/Cole Cengage Learning, 381–390. [Google Scholar]
- 14.Wilson PW, D’Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation 1998; 97:1837–1847. [DOI] [PubMed] [Google Scholar]
- 15.Stöckl D, Döring A, Peters A, et al. Age at menarche is associated with prediabetes and diabetes in women (aged 32–81 years) from the general population: the KORA F4 Study. Diabetologia 2012; 55:681–688. [DOI] [PubMed] [Google Scholar]
- 16.Akter S, Jesmin S, Islam M, et al. Association of age at menarche with metabolic syndrome and its components in rural Bangladeshi women. Nutr Metab (Lond) 2012; 9:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charalampopoulos D, McLoughlin A, Elks CE, et al. Age at menarche and risks of all-cause and cardiovascular death: a systematic review and meta-analysis. Am J Epidemiol 2014; 180:29–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gallagher LG, Davis LB, Ray RM, et al. Reproductive history and mortality from cardiovascular disease among women textile workers in Shanghai, China. Int J Epidemiol 201; 40:1510–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kivimäki M, Lawlor DA, Smith GD, et al. Association of age at menarche with cardiovascular risk factors, vascular structure, and function in adulthood: the Cardiovascular Risk in Young Finns study. Am J Clin Nutr 2008; 87:1876–1882. [DOI] [PubMed] [Google Scholar]
- 20.Trasande L, Cronk C, Durkin M, et al. Environment and obesity in the National Children's Study. Environ Health Perspect 2009; 117:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oken E, Taveras EM, Kleinman KP, et al. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol 2007; 196:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ylihärsilä H, Kajantie E, Osmond C, et al. Body mass index during childhood and adult body composition in men and women aged 56-70 y. Am J Clin Nutr 2008; 87:1769–1775. [DOI] [PubMed] [Google Scholar]
- 23.Botton J, Heude B, Maccario J, et al. Postnatal weight and height growth velocities at different ages between birth and 5 y and body composition in adolescent boys and girls. Am J Clin Nutr 2008; 87:1760–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perng W, Rifas-Shiman SL, Kramer MS, et al. Early weight gain, linear growth, and mid-childhood blood pressure a prospective study in project viva. Hypertension 2016; 67:301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taveras EM, Rifas-Shiman SL, Belfort MB, et al. Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics 2009; 123:1177–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Braithwaite D, Moore DH, Lustig RH, et al. Socioeconomic status in relation to early menarche among black and white girls. Cancer Causes Control 2009; 20:713–720. [DOI] [PubMed] [Google Scholar]
- 27.Remsberg KE, Demerath EW, Schubert CM, et al. Early menarche and the development of cardiovascular disease risk factors in adolescent girls: the Fels Longitudinal Study. J Clin Endocrinol Metab 2005; 90:2718–2724. [DOI] [PubMed] [Google Scholar]
- 28.Gamba M, Pralong FP. Control of GnRH neuronal activity by metabolic factors: the role of leptin and insulin. Mol Cell Endocrinol 2006; 254:133–139. [DOI] [PubMed] [Google Scholar]
- 29.Dreyfus J, Jacobs DR, Mueller N, et al. Age at Menarche and cardiometabolic risk in adulthood: the coronary artery risk development in young adults study. J Pediatr 2015; 167:344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mantzoros CS, Rifas-Shiman SL, Williams CJ, et al. Cord blood leptin and adiponectin as predictors of adiposity in children at 3 years of age: a prospective cohort study. Pediatrics 2009; 123:682–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sell H, Habich C, Eckel J. Adaptive immunity in obesity and insulin resistance. Nat Rev Endocrinol 2012; 8:709–716. [DOI] [PubMed] [Google Scholar]
- 32.Abdullah A, Wolfe R, Stoelwinder J, et al. The number of years lived with obesity and the risk of all-cause and cause-specific mortality. Int J Epidemiol 2011; 40:985–996. [DOI] [PubMed] [Google Scholar]
- 33.Must A, Phillips S, Naumova E, et al. Recall of early menstrual history and menarcheal body size: after 30 years, how well do women remember? Am J Epidemiol 2002; 155:672–679. [DOI] [PubMed] [Google Scholar]
- 34.Casey V, Dwyer J, Coleman K, et al. Accuracy of recall by middle-aged participants in a longitudinal study of their body size and indices of maturation earlier in life. Ann Hum Biol 1991; 18:155–166. [DOI] [PubMed] [Google Scholar]


