Abstract
We investigated the range and frequency of significant adverse events (AEs) in use of pharmacopuncture and acupuncture using large-scale, single-center safety data as evidence supporting safety of acupuncture with pharmacopuncture, used extensively in Asia, is scarce. Status reports (nurse records in ambulatory and inpatient care units, and administrative event records) as a part of an internal audit at a Korean Medicine hospital specializing in the treatment of musculoskeletal disorders, patient complaints filed through the hospital website, and medical records of patients visiting from December, 2010 (inception of internal audit) to October, 2014 were retrospectively reviewed. A total 80,523 patients (5966 inpatients and 74,557 outpatients) visited during this period. Inpatients received an average 31.9 ± 20.7 acupuncture, 23.0 ± 15.6 pharmacopuncture, and 15.4 ± 11.3 bee venom pharmacopuncture sessions, and outpatients were administered 8.2 ± 12.2 acupuncture, 7.8 ± 11.5 pharmacopuncture, and 10.0 ± 12.3 bee venom sessions, respectively. AEs associated with acupuncture/pharmacopuncture were forgotten needle (n = 47), hypersensitivity to bee venom (n = 37), presyncopic episode (n = 4), pneumothorax (n = 4), and infection (n = 2). Most cases were mild requiring little or no additional intervention and leaving no sequelae. Although serious AEs including infection (n = 2) and anaphylaxis associated with bee venom treatment (n = 3) were also reported, incidence was rare at 0.002% in infection and 0.019% in anaphylaxis. Incidence of AEs associated with acupuncture/pharmacopuncture treatment was low, and most cases were not serious. Still, however rare, avoidable AEs can and should be prevented through education and corrective action. Further prospective studies on the effect of error reduction strategies on incidence of adverse effects are warranted.
INTRODUCTION
Musculoskeletal disorders, especially low back and neck pain, are the main reasons for complementary and alternative medicine (CAM) consultation and use.1,2 According to a 2008 survey,3 86% of the South Korean population was estimated to have used Korean medicine treatment at least once, and 45.8% within the preceding 12 months. Among recipients of Korean medicine treatment, 53.4% had received them for musculoskeletal or connective tissue disorders.3
Acupuncture is licensed in 39 states in the U.S., and is the 3rd most frequented CAM treatment for back pain.1 The U.S. Food and Drug Administration estimates that 9 to 12 million acupuncture treatments are performed each year in the U.S., equaling $500 million in annual revenue.4 Due to heightened public interest in acupuncture, various new methods of acupuncture are being developed and employed. Pharmacopuncture is a relatively new acupuncture technique that combines the 2 most frequently used Korean medicine treatment forms: acupuncture and herbal medicine. Herbal medicine extracts are administered directly to acupuncture points for mechanical and chemical stimulation, thereby maximizing acupuncture point access and expanding the treatment window.5,6
Despite paucity of large-scale studies or reports on pharmacopuncture usage in clinical practice, its use can be indirectly gauged from its high production rate and multitude of related research. Approximately 200 herbal preparation types for injection are produced by pharmaceutical companies in China,7 and pharmacopuncture is covered by some private insurance companies, including traffic accident insurance, in Korea. Most colleges of Korean medicine have incorporated pharmacopuncture into their curriculum, and the government-funded research institution sector has also taken on an active role in pharmacopuncture research.8 A 2006 review showed that 438 pharmacopuncture studies have been published as of August, 2006 in the Acupuncture, a Korea National Research Foundation-certified journal, which constitutes 34.6% of total 1268 articles published since its foundation.9 Clinical use of pharmacopuncture for musculoskeletal problems in Korea can be inferred from a retrospective review of medical records of postspine operative pain patients treated at 2 spine-specialty Korean medicine hospitals. Of 702 patients reviewed, 69% were treated with pharmacopuncture. Considering that acupuncture, which is covered by Korean national health insurance, was used in 88% of patients, it can be deduced that the use of pharmacopuncture is comparable to that of acupuncture.10
Most previous studies on acupuncture safety are systematic reviews (SRs) or surveys,11–14 and U.S., German, British, Korean, and Japanese reports place AE incidence at 0.671% to 11.4%, with the most common acupuncture-related AEs being pain, bleeding, fatigue, and hematoma.14–17 Two prospective studies of the acupuncture practitioners in the U.K. reported no serious AEs in 66,000 treatment sessions.11,18 An SR of acupuncture safety investigated nearly a quarter of a million treatments in 9 prospective studies, and the most serious AEs were 2 cases of pneumothorax and 2 of broken needle.19 Odsberg et al20 reported no serious AEs in almost 9300 acupuncture treatment sessions conducted by Swedish physiotherapists.
Although acupuncture safety has been rigorously studied in previous literature, there are no such corresponding large-scale clinical investigations on pharmacopuncture safety which is unbefitting to its widespread use. The objectives of this study are, in light of increasing pharmacopuncture use, to determine the range and frequency of significant AEs in combined use of pharmacopuncture and acupuncture compared to acupuncture alone, and to provide large-scale, single-center safety data on bee venom pharmacopuncture, whose safety is already supported by a large body of evidence, as preliminary data for basic clinical safety guidelines of acupuncture and pharmacopuncture practice.
MATERIALS AND METHODS
Study Population and Sampling
Retrospective Review of Electronic Medical Records and Event Reports
We retrospectively reviewed internal audit event monitoring records including relevant status reports (nurse records in ambulatory and inpatient care units, and administrative event records), patient complaints filed through the hospital website, and medical records of all patients treated between December, 2010 and October, 2014 at a Korean Medicine hospital certified by the Korean Ministry of Health & Welfare to specialize in the treatment of spinal disorders.
Data on the number of patients receiving acupuncture/pharmacopuncture treatment and frequency and type of acupuncture/pharmacopuncture treatment sessions were collected from electronic medical records. Audit records were reviewed for AEs that may be associated with treatment (e.g., acupuncture, pharmacopuncture, moxibustion, cupping, Chuna spinal manipulation, herbal medicine, conventional medicine, injection, and physical therapy) and patient management-related accidents (e.g., fall injury, bedsore), and categorized accordingly. Of reported AEs, those related to acupuncture and/or pharmacopuncture were retrieved. Electronic medical records (doctor records, nurse records, lab results, and imaging data such as X-rays and MRIs) of relevant patients were analyzed.
Nurse Records
The nursing staff is divided into 6 outpatient and 5 inpatient units. Each unit consists of 4 to 5 nurses, including a head nurse for each unit, and the outpatient units are staffed with a total 33 nurses (including registered and auxiliary nurses), and inpatient ward with 27. There are additional heads of departments, and of the entire nursing staff. Inpatient ward nurses check patient status 5+ times a day, and ambulatory care unit nurses meet with patients at least twice per visit before and after treatment, permitting close observation of any unexpected or unintended reactions. All significant AEs (regardless of causal relationship with treatments), patient complaints, management records, physician briefings, and transfers to other physicians or institutions are recorded and reported daily. The reports are shared with head nurses and doctors at weekly meetings.
Patients are informed of treatment contents to be introduced to the patient's treatment regimen and related AEs prior to administration by attending physician and attending nurse, and instructions on how to respond to AE occurrence after treatment by counselling (head) nurse. AEs of delayed onset presenting out of hospital grounds can be reported by the patient or guardian using the 24 hour hotline for consultation with the call duty doctor, reported upon visit to the in-hospital ER, or filed through the hospital website, and this information is also compiled by the nursing staff. It can be reasonably inferred that most AEs are covered through extensive exposure and contact means available to patients and a systematic reporting system. A weekly status reports consists of 1380 Korean words on average.
Physician and Nurse Patient Management
The hospital employs a patient management policy where physicians are encouraged to call patients who have been noncompliant with treatment for a prolonged period of time and nurses no-show patients for clinical follow-up and quality assurance means. Although such calls are not specifically for patient safety evaluation, nonreturning patients are so provided with an additional opportunity to report and/or ask about potential AEs.
AE Analysis
Two specially trained Korean medicine doctors individually analyzed AEs associated with acupuncture and/or pharmacopuncture, then reached agreement on difference of opinion through discussion. Demographic information of patients experiencing AEs (inpatient/outpatient department, sex, age, and comorbidities), test type, and results relevant to AE diagnosis were collected in addition to AE symptoms, severity, causality, any concomitant interventions for AE treatment, and additional follow-ups.
AE Frequency
For comparison with previously reported AE incidence of acupuncture and pharmacopuncture/bee venom treatment, frequency was categorized in accordance with the European Commission guidelines for AEs of medicinal products (very common [≥1/10], common [≥1/100 to <1/10], uncommon [≥1/1000 to ≤1/100], rare [≥1/10,000 to ≤1/1000]; very rare [≤1/10,000], and not known).21
AE Severity
The severity of the adverse event was classified into 3 levels following Spilker AE classification (mild: does not significantly impair daily activities [function] nor require additional medical intervention; moderate: significantly impairs daily activities [function], and may require additional medical intervention but resolves afterwards; severe: serious AE that requires intense medical intervention, and leaves sequelae).22
AE Causality
Causality was determined using the WHO-UMC causality scale.23 Hypersensitivity to bee venom was classified into local and systemic reactions, and systemic reactions were recategorized using Mueller 4-level classification.24 Bee venom concentration, total number of bee venom treatments, and vital signs were reviewed through medical charts.
Statistical Analysis
All statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC. In descriptive statistics, continuous variables are given as mean ± SD, and categorical data are given as frequency and percentage (%).
Ethics Statement
The study was approved by the Institutional Review Board (IRB) of Jaseng Hospital of Korean Medicine in Seoul, Korea (IRB approval number: KNJSIRB2016-002).
RESULTS
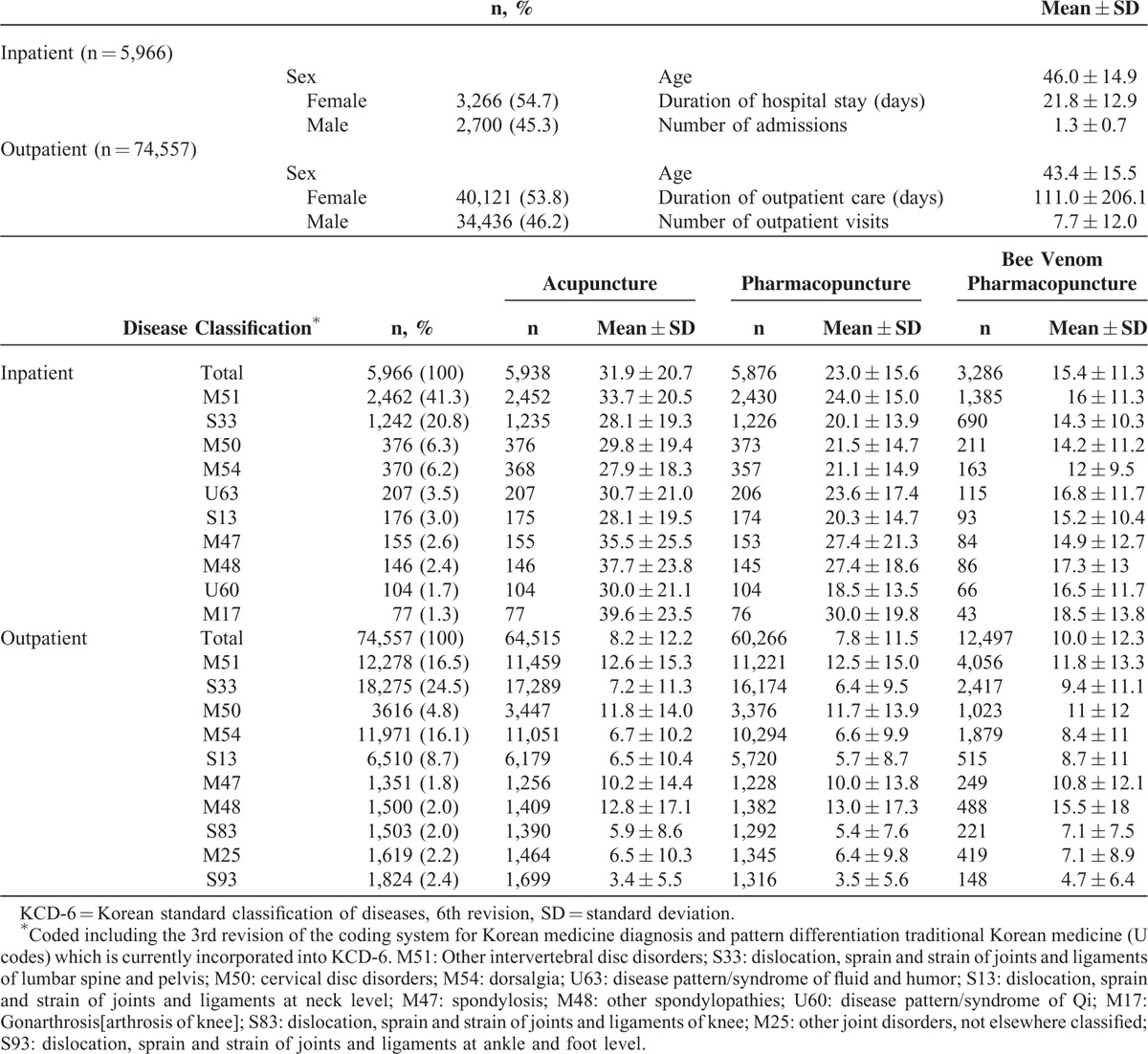
A total 80,523 patients (5966 inpatients, and 74,557 outpatients) were treated between December, 2010 and October, 2014. The percentage of inpatients receiving acupuncture, pharmacopuncture (including bee venom), and bee venom was 100%, 98%, and 55%, respectively, and that of outpatients was 87%, 81%, and 17%, respectively. Most patients visited the hospital for the disease classification codes M51 (other intervertebral disc disorders), or S33 (dislocation, sprain and strain of joints, and ligaments of lumbar spine and pelvis). Patients received 31.9 ± 20.7 acupuncture treatment sessions for the duration of inpatient care, and 8.2 ± 12.2 sessions in ambulatory care. Inpatients were administered 23.0 ± 15.6 pharmacopuncture sessions, and outpatients, 7.8 ± 11.5 sessions, while bee venom was administered for 15.4 ± 11.3 and 10.0 ± 12.3 sessions in inpatients and outpatients, respectively, showing that inpatients received more intensive treatment within a shorter time frame (Table 1).
TABLE 1.
Use of Acupuncture and Pharmacopuncture by Patient Disease Classification According to the KCD-6 (n = 80,523)
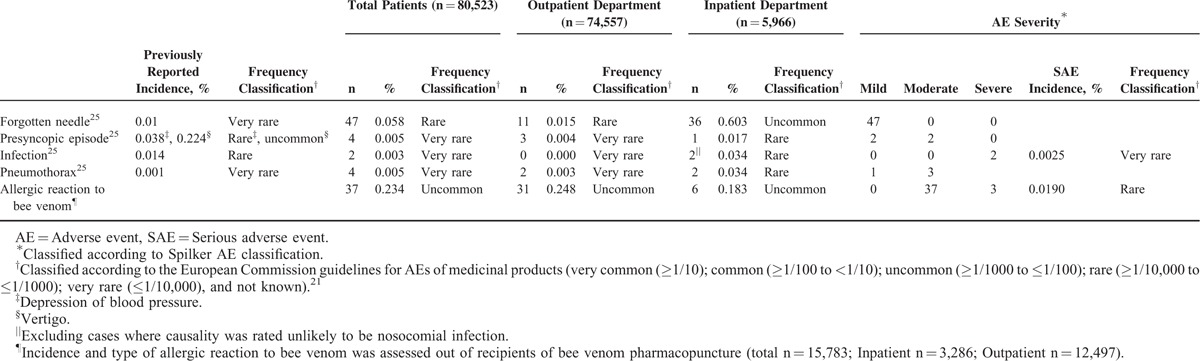
The main AEs associated with acupuncture/pharmacopuncture treatment were forgotten needle, presyncopic episode (depression of blood pressure or vertigo), infection, pneumothorax, and hypersensitivity to bee venom. The most frequently reported events were forgotten needle and hypersensitivity to bee venom. All cases of forgotten needle did not require additional medical intervention. Severe AEs consisted of 3 cases of hypersensitivity to bee venom and 2 cases of infection, and were rare. Most AEs were more common in inpatients with the exception of hypersensitivity to bee venom, which had higher incidence in ambulatory care (Table 2).
TABLE 2.
AEs Associated With Acupuncture or Pharmacopuncture (Out of Total n = 80,523)
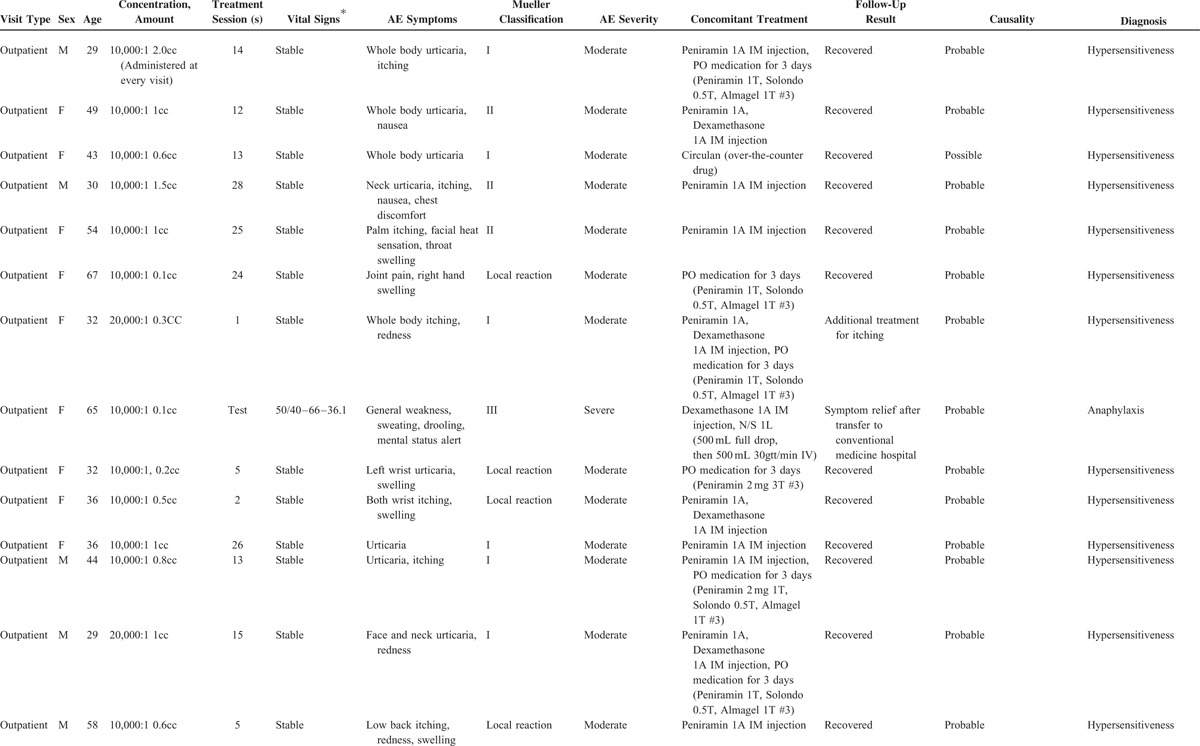
Eleven males and 16 females, aged 44.5 ± 14.8 years, presented with hypersensitivity to bee venom. The average number of treatment sessions before adverse event presentation was 11.6 ± 9.2 sessions, excluding cases with positive skin tests or not recorded. Of 37 cases of bee venom hypersensitivity, 34 were classified as hypersensitiveness and of moderate AE severity, and 3 cases were classified as anaphylactic and of severe AE severity. Most were prescribed immunosuppressive agents such as phenylamine and dexamethasone, and anaphylactic patients were administered epinephrine. The majority recovered within 24 hours, while 5 were transferred to other hospitals for additional medical attention. Three transfers were for additional medical intervention for anaphylaxis, and 2 were due to delayed onset with symptoms surfacing after operating hours of conventional ambulatory care unit sharing facilities with the Korean medicine hospital. None of the patients expired (Table 3 ).
TABLE 3.
Adverse Events Associated With Bee Venom Pharmacopuncture
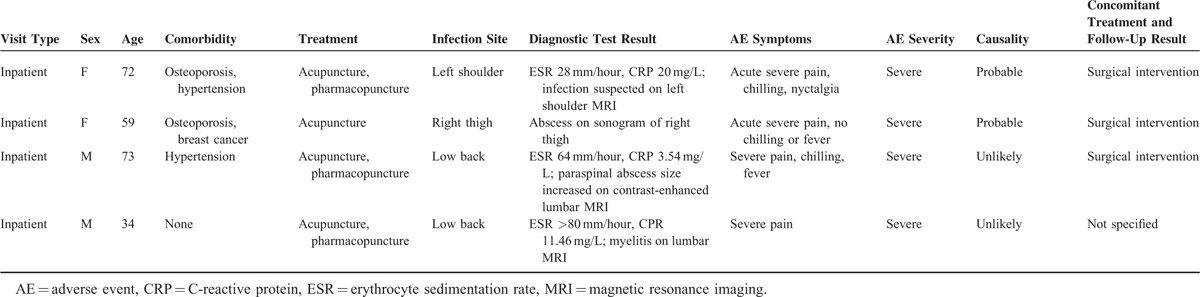
Four patients were suspected of infection, all of which were inpatients and mostly geriatrics. Blood tests were conducted upon suspicion of infection, and erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels were elevated in all 4 patients. Imaging results of MRs or ultrasound also confirmed infection in all 4 patients. Most patients presented with severe pain, accompanied with subjective symptoms of fever and chills. All cases were classified as severe, requiring antibiotics and surgery. Whereas causality was rated as probable in 2 of the 4 cases to be nosocomial infections, it was rated unlikely for the other 2 patients. Signs of infection were visible on MRIs taken before admission and acupuncture/pharmacopuncture treatment, and ESR and CRP levels showed elevation in blood tests at admission in the 2 patients for whom attribution was considered unlikely. These cases were therefore judged to be infections occurring prior to hospitalization (Table 4).
TABLE 3 (Continued).
Adverse Events Associated With Bee Venom Pharmacopuncture
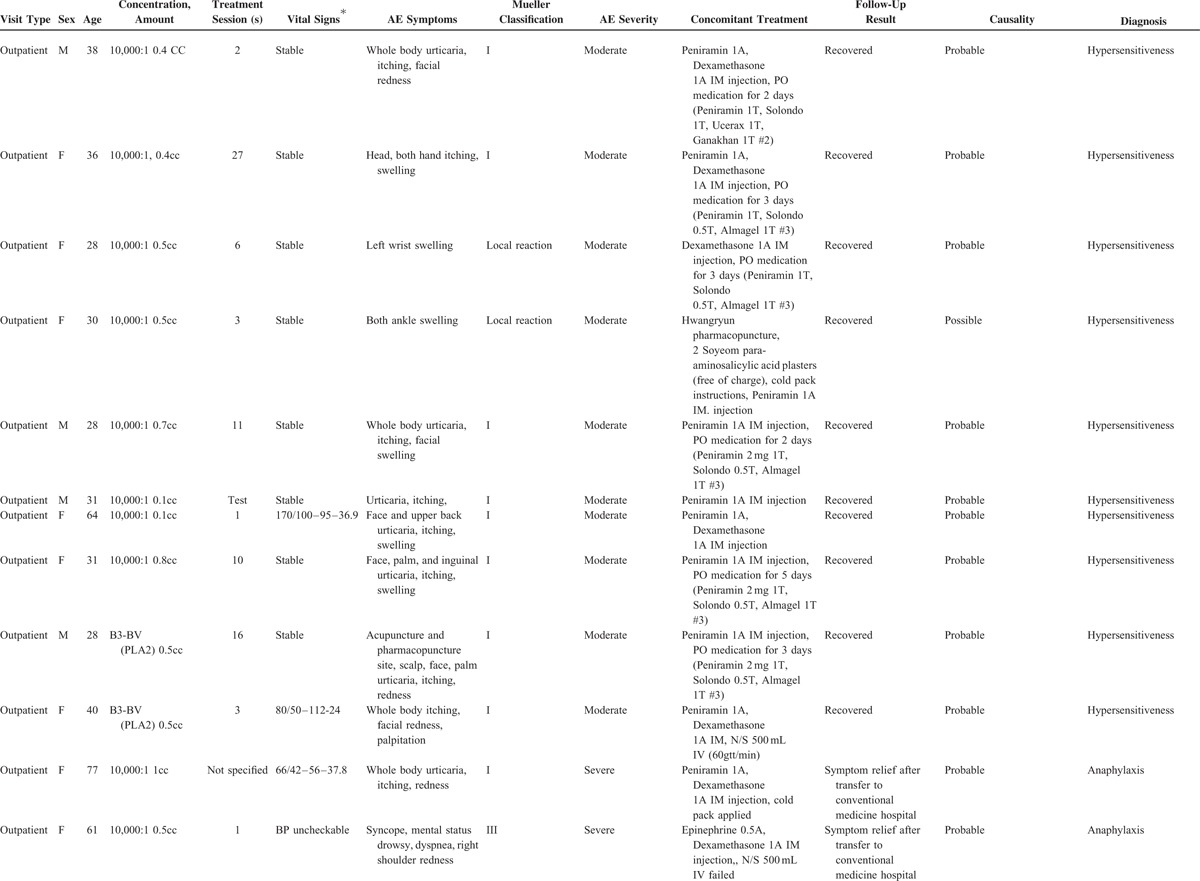
TABLE 4.
Infection Associated With Acupuncture or Pharmacopuncture
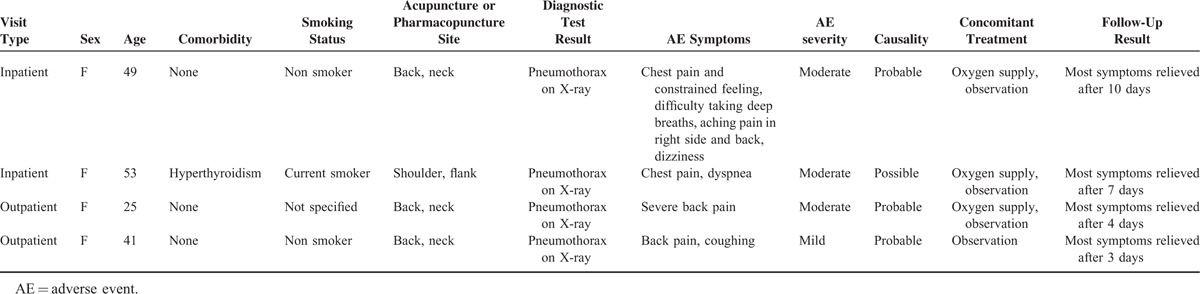
All 4 of the pneumothorax cases were slender and female, and most were diagnosed based on clinical symptoms and X-ray. These patients had received acupuncture treatment in the upper thoracic and cervical areas: 2 as inpatients, and 2 as outpatients. Pneumothorax was suspected upon complaints of acute pain shortly after treatment. Dyspnea was not observed in some patients. Most recovered fully within 10 days upon observation and simple oxygen supply without intubation (Table 5).
TABLE 3 (Continued).
Adverse Events Associated With Bee Venom Pharmacopuncture
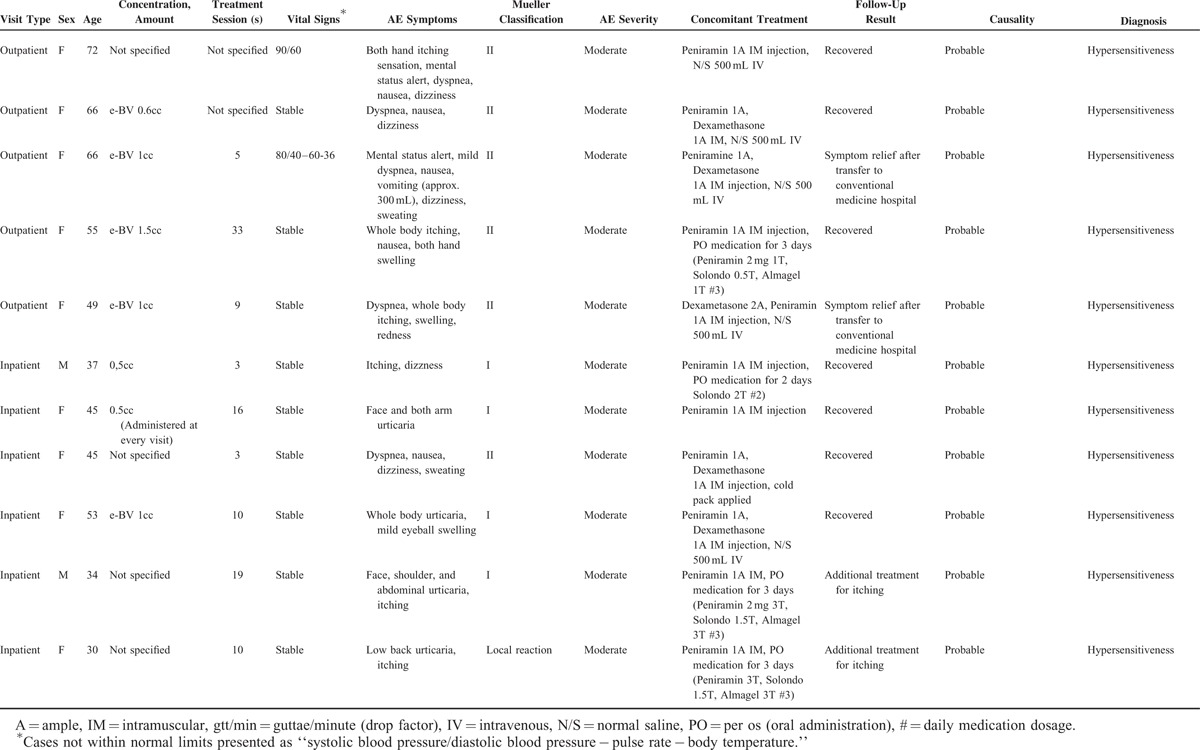
TABLE 5.
Pneumothorax Associated With Acupuncture or Pharmacopuncture
DISCUSSION
This study reports patterns of use and safety of acupuncture and pharmacopuncture in a population of 80,523 patients with musculoskeletal disorders. Main AEs associated with acupuncture/pharmacopuncture reported over the 4-year period were forgotten needle, presyncopic episode, infection, pneumothorax, and hypersensitivity to bee venom. Of these, the most frequently reported AEs were forgotten needle and hypersensitivity to bee venom, and the most severe were anaphylaxis due to bee venom and infection. However, severe AEs were rare and not fatal, nor did they leave sequelae. The acupuncture/pharmacopuncture safety results of our study are similar to those of a prospective observational study on acupuncture safety in 229,230 patients as shown in Table 2.25 Presyncopic episode and infection was less common in the current population, while forgotten needle and pneumothorax was slightly more common, but difference was not large. These results imply that incorporation of pharmacopuncture in acupuncture practice does not increase risk of AE.
Hypersensitivity to Bee Venom
Although a literature search was conducted for further information on pharmacopuncture safety, single intervention studies on pharmacopuncture are scarce and most are on bee venom. Clinical symptoms of bee venom hypersensitivity range from minor problems such as skin rashes, hives, and diarrhea to potentially fatal systemic problems such as dyspnea, arrhythmia, and hypotension.26 A recent SR on risks associated with bee venom therapy using 12 databases from inception to June 2014 without language restriction27 reported that of 6 audits and cohort studies on bee venom pharmacopuncture, 3 studies covered populations larger than 300 and reported AE incidence at 48/374 (12.83%; 48 cases of local reactions),28 11/32,000 (0.03%; 11 cases of systemic reactions),29 and 361/2765 (13.00%; 361 cases of systemic reactions).30 Also, in a meta-analysis of bee venom AE occurrence compared to normal saline in 4 randomized controlled trials, bee venom showed a 261% increased relative risk. In this study, 37 patients (0.234%) presented with bee venom hypersensitivity, of which 3 were anaphylactic. The relatively low incidence rate of anaphylaxis resulting in no significant sequelae or deaths may be attributed to swift administration of antihistamines such as phenylamine, glucocorticoids such as dexamethasone, or epinephrine as indicated upon presentation of hypersensitivity symptoms.
Infection
Acupuncture and pharmacopuncture are usually administered at acupuncture points in the same region, making differentiation of causal relationship highly difficult. Most invasive treatments for musculoskeletal disorders are administered around the site of the pain, and aggravation of pain may suggest infection or alternatively be a natural progression or fluctuation of disease. Although ESR and CRP are useful indicators of inflammation, many disease processes entail inflammation, and rise in acute phase proteins is not disease-specific (e.g., infection).31 For instance, while ESR and CRP values persistently elevated >15 days postsurgery strongly suggest infection, normal ESR and/or CRP values cannot be taken to exclude this diagnosis.32 Close observation and medical attention is necessary for patients susceptible to infection from immune deficiency or old age. Especially as all infections were serious AEs requiring corrective surgery and avoidable,12,33 error reduction strategies to prevent infection need to be implemented and tested.
Pneumothorax
Previous investigations on pneumothorax associated with acupuncture report incidence of 0.0014%34 and 0.001%.25 Norheim and Fonnebo33 reported the highest estimate to date with 33 possible cases of acupuncture-induced pneumothorax from questionnaires of doctors and acupuncturists. Pneumothorax was more common in our population than previous clinical observations, with an incidence of 0.005%. Although many patients reporting with this complication are predisposed to secondary pneumothorax,35 the disparity in incidence of the current population is probably due to difference in chief complaints, as those included were primarily musculoskeletal, especially spinal, and acupuncture was accordingly frequently applied to upper thoracic areas. Although pneumothorax was considered a serious AE in previous studies,19,25 symptoms were transient and subsided within a week of observation and simple oxygen supply without chest intubation or surgery in most patients in this study.
Presyncopic Episode and Forgotten Needle
Presyncopic episodes were less common in our data, which may be due, at least in part, to widespread prior exposure of Asian patients to acupuncture. As moderate presyncopic AEs were mostly fall injuries following presyncopic episodes, precaution on the part of both staff and patient is needed. Although forgotten needle cases were mild events not requiring additional medical intervention, they were highly common and should be avoided as they indicate malpractice or negligence.
The most significant strength of this study is that it is the 1st large-scale report of AEs associated with acupuncture and pharmacopuncture treatment. Data reliability was enhanced by crosschecking internal audits (status reports) and electronic medical records. Inpatients and outpatients were also separately analyzed as subgroups for distinctive trends by visit type and environment, in addition to AE incidence, severity classification, causality, symptoms, concomitant treatment, and follow-up results for comprehensive evaluation.
Limitations of this study are mainly due to its retrospective nature. This study lacks comparator populations and information on potential confounders such as risk factors were not collected. Data collection relied on voluntary reporting of patient and medical personnel, and considering for efficiency and clarity, the reporting format and range of AEs were kept relatively simple. There is the possibility that less severe events may not have been reported if the patient or practitioner did not regard it to be a problem as Koreans using Korean medicine may be more familiar or lenient toward treatment and regard minor AEs to be part of the treatment process. Due to the possibility of “missed AEs,” these results warrant careful interpretation, especially regarding minor AEs which have high incidence in previous reports but may have been underrepresented in this study.
Although in cases where the patient visits an outside clinic/hospital or receives no treatment for AEs it would be difficult for the event to be included in internal audits unless the patient or guardian voluntarily reports to the hospital, it is customary for musculoskeletal treatment to be continued for a period of time as opposed to a one-off session. As shown in Table 1, inpatients received medical care daily for an average hospital stay of 21 days and outpatients visited the hospital 7.7 times over a period of 111 days on average, and as the attending physician and attending nurse check patient condition at each treatment session, AEs associated with the previous visit should be included for internal reporting. In addition, as these records were documented for internal monitoring purposes, and even in cases where patient or medical personnel was reluctant to disclose the event, it is unlikely that significant AEs which require further treatment or may have other consequences for the patient would have gone unrecognized by the patient, guardian, and all staff members. To ensure unbiased systematic reporting of AEs and to be of wider external validity, future studies may consider a regional reporting network of private and public, conventional, and Korean medicine-based health care facilities. An additional limitation is that due to high correlation in method and usage of acupuncture and pharmacopuncture, respective causal relationships of AE are not clear.
Although CAM treatment is generally regarded to be safe, evidence on its safety is lacking. Safety reports hold considerable importance as they may help dictate future practice for AE prevention. Quarterly hospital analyses of AEs displayed a decreasing time-trend (not shown), possibly reflecting error reduction through education and corrective action as a result of internal auditing. For example, a standardized communication system of the number and location of needles between medical personnel was devised to prevent forgotten needles as part of continuous internal quality improvement efforts. Also, education sessions on hand sanitization and alcohol and povidone-iodine use were conducted to lower possibility of infection, as were sessions of appropriate needle retention and removal method in high-risk acupuncture points for pneumothorax. Bee venom skin tests have been shown to be an insufficient indicator of AEs with numerous cases occurring after several treatment sessions, and consequently current clinical instructions focus on regular examination of general patient condition and appropriate course of action upon AE occurrence as opposed to prevention. AE prevention is sought instead through development and manufacture of PLA2- and histamine-free bee venom products.
These results suggest that AEs after acupuncture/pharmacopuncture treatment may have low incidence and reported events were mostly of minor nature. Still, however rare or minor, avoidable AEs can and should be prevented through education and corrective action. Further prospective studies on the effect of error reduction strategies on incidence of adverse effects in a systemized reporting system using standardized terminology such as WHO adverse reaction terminology are warranted.
Acknowledgments
The authors thank the Standardization Project of Korean Medicine Acupuncture funded by the Korean Ministry of Health & Welfare through the Korea Promotion Institute for Traditional Medicine Industry (3243–302) for the support.
Footnotes
Abbreviations: CAM = complementary and alternative medicine, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, FDA = Food and Drug Administration, SR = systematic review.
This study was supported by the Standardization Project of Korean Medicine Acupuncture funded by the Korean Ministry of Health & Welfare through the Korea Promotion Institute for Traditional Medicine Industry (3243–302).
The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA 1998; 280:1569–1575. [DOI] [PubMed] [Google Scholar]
- 2.Cherkin DC, Deyo RA, Sherman KJ, et al. Characteristics of visits to licensed acupuncturists, chiropractors, massage therapists, and naturopathic physicians. J Am Board Fam Pract 2002; 15:463–472. [PubMed] [Google Scholar]
- 3.Korea Institute of Oriental Medicine, Institute of Korean Medicine Education & Evaluation, Health Insurance Review & Assessment Service, Yonsei University Department of Health Administration, Seoul National University College of Nursing. A survey on the use of traditional Korean medicine. 2008; 11-1351000-000223-01. [Google Scholar]
- 4.Lytle C. An Overview of Acupuncture. Washington, D.C.: United States Department of Health and Human Services, Health Sciences Branch, Division of Life Sciences, Office of Science and Technology, Center for Devices and Radiological Health, Food and Drug Administration; 1993. [Google Scholar]
- 5.Luna SP, Angeli AL, Ferreira CL, et al. Comparison of pharmacopuncture, aquapuncture and acepromazine for sedation of horses. Evid Based Complement Alternat Med 2008; 5:267–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strudwick MW, Hinks RC, Choy ST. Point injection as an alternative acupuncture technique – an exploratory study of responses in healthy subjects. Acupunct Med 2007; 25:166–174. [DOI] [PubMed] [Google Scholar]
- 7.Seoul National University Natural Products Research Institute, Center for collaborative research on traditional Korean and Chinese drugs. Survey on Injections of Traditional Chinese Drug. Seoul: Science and Technology Policy Institute; 1995. [Google Scholar]
- 8.Year Book of Traditional Korean Medicine Publishing Committee. 2013 Year Book of Traditional Korean Medicine. Daejeon: Kumkang Printing, Pusan National University School of Korean Medicine, Korea Institute of Oriental Medicine, The Association of Korean Medicine; 2014. [Google Scholar]
- 9.Baik S, Ahn J, Kim Y, et al. Type analysis of pharmacopuncture papers published in the Journal of Korean Acupuncture and Moxibustion. J Korean Acupunct Moxibust Soc 2006; 23:19–27. [Google Scholar]
- 10.Choi HS, Chi EH, Kim MR, et al. Demographic characteristics and medical service use of failed back surgery syndrome patients at an integrated treatment hospital focusing on complementary and alternative medicine: a retrospective review of electronic medical records. Evid Based Complement Alternat Med 2014; 2014:714389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White A, Hayhoe S, Hart A, et al. Adverse events following acupuncture: prospective survey of 32,000 consultations with doctors and physiotherapists. BMJ 2001; 323:485–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macpherson H, Scullion A, Thomas KJ, et al. Patient reports of adverse events associated with acupuncture treatment: a prospective national survey. Qual Saf Health Care 2004; 13:349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melchart D, Weidenhammer W, Streng A, et al. Prospective investigation of adverse effects of acupuncture in 97,733 patients. Arch Intern Med 2004; 164:104–105. [DOI] [PubMed] [Google Scholar]
- 14.Yamashita H, Tsukayama H. Safety of acupuncture practice in Japan: patient reactions, therapist negligence and error reduction strategies. Evid Based Complement Alternat Med 2008; 5:391–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ernst G, Strzyz H, Hagmeister H. Incidence of adverse effects during acupuncture therapy – a multicentre survey. Complement Ther Med 2003; 11:93–97. [DOI] [PubMed] [Google Scholar]
- 16.Lao L, Hamilton GR, Fu J, et al. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med 2003; 9:72–83. [PubMed] [Google Scholar]
- 17.MacPherson H, Thomas K, Walters S, et al. A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional acupuncturists. Acupunct Med 2001; 19:93–102. [DOI] [PubMed] [Google Scholar]
- 18.MacPherson H, Thomas K, Walters S, et al. The York acupuncture safety study: prospective survey of 34,000 treatments by traditional acupuncturists. BMJ 2001; 323:486–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ernst E, White AR. Prospective studies of the safety of acupuncture: a systematic review. Am J Med 2001; 110:481–485. [DOI] [PubMed] [Google Scholar]
- 20.Odsberg A, Schill U, Haker E. Acupuncture treatment: side effects and complications reported by Swedish physiotherapists. Complement Ther Med 2001; 9:17–20. [DOI] [PubMed] [Google Scholar]
- 21.European Commission: Enterprise and Industry Directorate-General. A guideline on summary of product characteristics. http://ec.europa.eu/health/files/eudralex/vol-2/c/smpc_guideline_rev2_en.pdf 2009. Accessed April 23, 2016. [Google Scholar]
- 22.Spilker B. Interpretation of adverse reactions. In:. Guide to Clinical Trials 1991; New York: Raven Press, Ltd, 565–587. [Google Scholar]
- 23.World Health Organization. The use of the WHO-UMC system for standardized case causality assessment. http://who-umc.org/Graphics/24734.pdf 2005. Accessed April 23, 2016. [Google Scholar]
- 24.Mueller HL. Diagnosis and treatment of insect sensitivity. J Asthma Res 1966; 3:331–333. [DOI] [PubMed] [Google Scholar]
- 25.Witt CM, Pach D, Brinkhaus B, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed 2009; 16:91–97. [DOI] [PubMed] [Google Scholar]
- 26.Cianferoni A, Novembre E, Mugnaini L, et al. Clinical features of acute anaphylaxis in patients admitted to a university hospital: an 11-year retrospective review. Ann Allergy Asthma Immunol 2001; 87:27–32. [DOI] [PubMed] [Google Scholar]
- 27.Park JH, Yim BK, Lee JH, et al. Risk associated with bee venom therapy: a systematic review and meta-analysis. PLoS One 2015; 10:e0126971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choi S, Choi S, Oh S. A clinical report of localized itching after treatment with sweet bee venom. J Pharmacopunct 2010; 13:103–108. [Google Scholar]
- 29.Hwang Y, Lee B. Clinical study of anaphylaxis on bee venom acupuncture. J Korean Acupunct Moxibust Soc 2000; 17:149–159. [Google Scholar]
- 30.Kwon G, Koh H. The clinical observation of immune response by Korean bee venom therapy. J Korean Acupunct Moxibust Soc 2000; 17:169–174. [Google Scholar]
- 31.Stuart J, Whicher JT. Tests for detecting and monitoring the acute phase response. Arch Dis Child 1988; 63:115–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lazennec JY, Fourniols E, Lenoir T, et al. Infections in the operated spine: update on risk management and therapeutic strategies. Orthop Traumatol Surg Res 2011; 97 (6 Suppl):S107–S116. [DOI] [PubMed] [Google Scholar]
- 33.Norheim AJ, Fonnebo V. Adverse effects are more than occasional case reports: results from questionnaires among 1,135 randomly selected doctors, and 197 acupuncturists. Complement Ther Med 1996; 4:8–13. [Google Scholar]
- 34.Umlauf R. Analysis of the main results of the activity of the acupuncture department of faculty hospital. Acupunct Med 1988; 5:16–18. [Google Scholar]
- 35.Bodner G, Topilsky M, Greif J. Pneumothorax as a complication of acupuncture in the treatment of bronchial asthma. Ann Allergy 1983; 51:401–403. [PubMed] [Google Scholar]


