Abstract
Corazón Sano y Feliz is a hypertension management intervention developed to address deficiencies in the management of hypertensive patients in Guatemala. From 2007 to 2009, Corazón Sano y Feliz was pilot-tested in the community of Mixco. Corazón Sano y Feliz comprises a clinical risk assessment and treatment component implemented primarily by nurses, and a health education component implemented by community health workers. To accomplish our secondary objective of determining Corazon Sano y Feliz's potential for change at the patient level, we implemented a one-group pretest-posttest study design to examine changes in clinical measures, knowledge and practices between baseline and the end of the 6-month intervention. Two nurses and one physician set up a hypertension clinic to manage patients according to risk level. Twenty-nine community health workers were trained in CVD risk reduction and health promotion and in turn led six educational sessions for patients. Comparing baseline and 6-month measures, the intervention achieved significant improvements in mean knowledge and behaviour (increase from 54.6 to 59.1 out of a possible 70 points) and significant reductions of mean systolic and diastolic blood pressure (27.2 and 7.7 mmHg), body mass index (from 26.5 to 26.2 kg/m2) and waist circumference (89.6–88.9 cm). In this pilot study we obtained preliminary evidence that this community-oriented hypertension management and health promotion intervention model was feasible and achieved significant reduction in risk factors. If scaled up, this intervention has the potential to substantially reduce CVD burden.
Keywords: cardiovascular health promotion, hypertension control, diabetes, community-based intervention
INTRODUCTION
In low and middle-income countries, cardiovascular diseases (CVD) have become the most frequent cause of death and disease burden (Ebrahim and Smith, 2001; Yusuf et al., 2001; Reddy, 2004). In Guatemala, the percentage of deaths attributed to CVD increased in recent decades: from 7% in 1986 to 17% in 2009, representing the second cause of death in the country (Ministry of Public Health, Guatemala, 2009). It is projected that the prevalence of CVD will increase due to the increase in life expectancy and the adoption of unhealthy lifestyles. Hypertension will contribute to a significant proportion of the future deaths related to CVD. Globally, 51% of stroke and 45% of ischaemic heart disease deaths are attributable to high systolic blood pressure (WHO, 2002; Lopez et al., 2006).
Despite the benefits of effective drug treatment (Lloyd-Jones et al., 2005) and the existence of clinical practice guidelines (Chobanian et al., 2003), hypertension control remains suboptimal worldwide (Beckett et al., 2008). The situation is particularly notorious in developing countries where the health system is for the most part oriented to the acute care of infectious diseases and maternal and child health. As a result, serious deficiencies in the management of hypertension have been identified (McKinstry et al., 2006). For example, in Guatemala, measurement of blood pressure is seen as a secondary task and is not systematically done. As a result, hypertension is not often diagnosed and treated at primary health care facilities (Mendoza-Montano et al., 2008).
A significant proportion of the morbidity and mortality caused by CVD could be prevented by cost-effective interventions at the health system level, and through wide population-based strategies that include timely and sustained lifestyle interventions (WHO, 2007; Beaglehole et al., 2008). The primary care level constitutes the most important component of the health care delivery system in Guatemala; interventions at this level provide a unique opportunity to carry out screening for risk detection, stratification and management (Mendoza-Montano et al., 2008).
A major limitation of current clinical guidelines for CVD prevention and control is that they focus on single risk factors (Fahey et al., 2006). A global cardiovascular risk approach that takes into account several risk factors is more cost-effective than one that uses only blood pressure thresholds to measure risk. The global risk of an individual can be a useful guide for making clinical decisions; the risk stratification approach is particularly suitable to health services with limited resources, where saving the greatest number of lives at lowest cost is imperative (Lim et al., 2007; Greenland et al., 2010). The World Health Organization (WHO) has developed risk charts for different regions of the world that define the global risk of a cardiovascular event in the next 10 years on the basis of age, sex, systolic blood pressure, total cholesterol, the presence of diabetes and tobacco consumption. Studies have shown high agreement in risk characterization between a non-laboratory-based risk prediction method and the classic laboratory-based risk charts.
Therefore, the global risk factor approach and other cost-effective clinical strategies should be put in practice to achieve hypertension control. However, there are other factors contributing to the sub-optimal control of hypertension in developing countries which include limited formal education, little knowledge about the importance, causes, and control of hypertension among patients, and poor patient relationships with overburdened health professional. As a result, the involvement of community health workers (CHWs) has been recommended as an effective way of responding to these barriers that underserved populations face, as well as to improve health outcomes (Love et al., 1997; CDC, 2003). In the case of patients with hypertension, CHWs can facilitate access to care, and enhance compliance with treatment regimens (Morisky et al., 1983). In many settings, CHWs have worked with medical care teams to take on significant patient follow-up responsibilities including phone calls and home visits (Perez and Martinez, 2008; Pinto et al., 2011). In some cases, CHWs assist in monitoring blood glucose and blood pressure, and provide social support to patients and families (Corkery et al., 1997; AADE, 2003; Fedder et al., 2003).
The impact of CHWs on hypertension control has been demonstrated in a number of studies. In a family-based home health education intervention delivered by CHWs, coupled with clinician training in Karachi, Pakistan, there was a SBP reduction of 10.8 mmHg when followed up at 2 years; this reduction was significantly greater than either the health education or clinician training alone (Jafar et al., 2009). In a volunteer-run, community-based BP-monitoring programme in senior centres in New York City, participants showed on average a 3.9 mmHg reduction in SBP at 6 months, and participants with baseline SBP >160 mmHg showed an average reduction of 20.9 mmHg (Truncali et al., 2010). Evidence for public health interventions to improve hypertension control rates through patient or physician education in Guatemala is lacking.
The US National Heart, Lung and Blood Institute (NHLBI) developed a programme called ‘Health for Your Heart’ (Salud Para Su Corazón-SPSC in Spanish) aimed at increasing knowledge about CVD risk factors and heart-healthy behaviours among Hispanic populations in the USA (Alcalay et al., 1999; Balcazar et al., 2001). The programme has a heart-healthy curriculum designed for training CHWs to teach community residents about preventing risk factors and adopting healthy behaviours (NHLBI, 2000).
In a combined clinical and health promotion study in community health centres in the US-Mexico border region using SPSC, participants showed changes in heart-healthy behaviour at 6 and 12 months and significant changes in LDL cholesterol and triglyceride levels, but significant reductions in blood pressure were not observed (Balcazar et al., 2006; Medina et al., 2007; Balcazar et al., 2009).
The hypertension management intervention model described in this article called Corazón Sano y Feliz (Happy and Healthy Heart in English) was developed with the aim of addressing deficiencies in the screening, assessment and management of hypertensive patients in primary health care centres of Guatemala, incorporating as a core clinical component the WHO global CVD risk prediction charts mentioned above (WHO, 2007). In addition, the programme was developed to address educational and cultural barriers of patients incorporating a health promotion strategy based on the SPSC model.
From 2007 to 2009, we conducted a study in Mixco, Guatemala to pilot Corazon Sano y Feliz. The aim of the pilot study was to assess the feasibility of implementing the intervention model in the primary health care (PHC) system of Guatemala. The main purpose of this article is to: (i) describe the core components of Corazon Sano y Feliz; (ii) present strategies used in its pilot implementation; and (iii) discuss lessons learned during the implementation and evaluation of the pilot study, and share implications for its future implementation. Our secondary purpose is to present changes in patient knowledge and clinical outcomes for participants as preliminary evidence of the Corazon Sano y Feliz effectiveness.
The development and pilot-testing of Corazón Sano y Feliz was part of the Pan American Cardiovascular Initiative (PACI), which was a joint initiative of the US National Heart, Lung and Blood Institute (NHLBI), and the Pan American Health Organization (PAHO) both of which provided technical and funding support to Corazón Sano y Feliz. PACI included similar projects in communities of Argentina and Chile. The study was conducted in partnership with the Ministry of Health, local authorities and members of the community who were involved from the outset.
METHODS
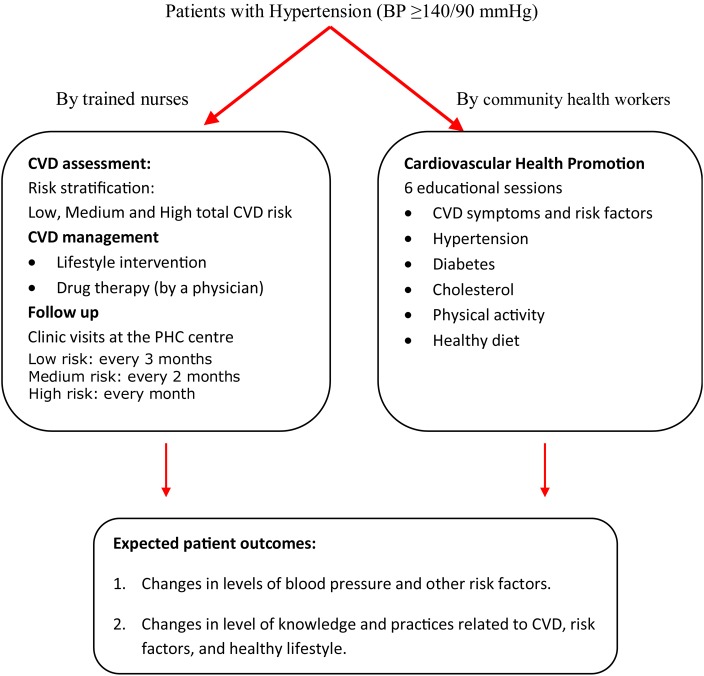
Corazón Sano y Feliz is a hypertension management model for individuals with high blood pressure and other risk factors comprising a risk assessment and clinical management component implemented primarily by nurses with support and supervision from physicians, and a health promotion component implemented by trained CHWs (Figure 1).
Fig. 1:
Clinical and health promotion components of Corazon Sano y Feliz.
The details of the core components of Corazon Sano y Feliz are the following.
CVD assessment and clinical management of patients
The clinical component applied the World Health Organisation (WHO) global cardiovascular risk guidelines (WHO, 2007), to patients who had been detected to have hypertension. The WHO guidelines employ simple CVD risk assessment tools that do not require laboratory analysis and use non-invasive parameters to stratify CVD risk. The clinical management was based on the total CVD risk restricting anti-hypertensive medication to those patients at high total CVD risk. Therefore, the minimum infrastructure and equipment that the PHC centres needed to implement the guidelines were: adequate space, blood pressure monitors, glucometer and glucose strips for diabetes screening, weight scales for assessment of body mass index and basic office supplies. In addition, a group of well-trained health workers (nurses and physicians) were needed. Corazon Sano y Feliz relied mostly on nurses for patient assessment and management because many PHC settings in Guatemala do not have a physician available to deliver clinical care.
The CVD assessment and clinical management included the following activities.
Capacity enhancement of professional health workers
The capacity enhancement of physicians and nurses was accomplished through workshops providing methods for total CVD risk assessment, management and follow-up of patients. The core of the training was based on the WHO CVD risk prediction chart and management guidelines (see below for details of the charts and algorithms). Principal content areas included in the workshops were: CVD risk stratification, promotion of healthy diets, promotion of regular physical activity, medication treatment algorithms and indications for nurses to refer patients to PHC physicians or to a higher level of care.
Detection, CVD risk assessment, clinical management and follow-up
Detection of hypertensive individuals
The programme was designed primarily for assessment and management of CVD risk in hypertensive individuals. Nurses measured blood pressure in individuals ≥40 years; and those with SBP <140 received a brief lifestyle counselling session. Individuals with SBP ≥140 were advised to enrol in the intervention study for further assessment and management.
CVD risk assessment
The assessment of patients was based on simple, non-invasive variables. When patients returned to the PHC centre for Visit 1, a nurse took a second blood pressure measurement to confirm hypertension. If confirmed, the nurse assessed the following CVD risk factors: blood glucose, body mass index (BMI), waist circumference, tobacco consumption and age.
The total CVD risk stratifications were based on the simple WHO CVD risk prediction charts (WHO, 2007), which did not require laboratory analysis and used easy-to-measure parameters: sex, age, blood pressure, presence or absence of diabetes, and tobacco use. The chart indicates total 10-year risk of a fatal or non-fatal cardiovascular event (myocardial infarction or stroke) for the WHO Latin American Region, sub-region AMR D (which includes Guatemala). According to the 10-year risk of a CVD event, patients are stratified as follows:
This stratification guided health providers to establish the type of treatment, the need for drug use and the frequency of scheduled visits to the clinic of patients.
Clinical management
The management and follow-up algorithm was also based on the WHO clinical guidelines. The clinical protocols guide the health workers in formulating an individualized care plan for each patient based on his/her total CVD risk. Nurses provided all patients counselling on healthy dietary changes, smoking cessation and physical activity to reduce CVD risk. The dietary counselling emphasized the reduction of salt, fatty and sugary food and alcohol intake and advocated the consumption of lean meats, fruit and vegetables. The counselling on physical activity encouraged patients to do at least 30 min of moderate-intensity physical activity on most (and preferably all) days of the week. The nurses asked patients about tobacco use at every visit. A staff physician could be consulted for serious changes in patient's medical conditions or for drug therapy. The anti-hypertensive drug therapy consisted of prescribing a thiazide diuretic and was restricted to patients classified with high total CVD risk. As part of the overall management, nurses invited patients to participate in the health promotion sessions conducted by CHWs.
Follow-up
The nurses made two follow-up visits (Visits 2 and 3) for each patient. The frequency of the visits depended on the total CVD risk of patients. At each of the two follow-up visits, the nurses measured levels of CVD risk factors and reassessed smoking status, physical activity, dietary practices and review of health goals. Based on this information, the nurses, with the advice of a physician, reviewed progress made to continue or change drug treatment.
Cardiovascular health promotion
The health promotion component of the programme was offered to all participants and had the aim of improving knowledge and the uptake of healthy behaviours. The theoretical underpinning for the health education component is the Health Belief Model (Becker, 1974), recognizing the importance of culturally appropriate materials delivered by community peers (SPSC, 2006).
This component was comprised of the following activities.
Training of CHWs
The training was designed to provide CHWs with the knowledge and abilities necessary to teach community residents about preventing CVD and adopting healthy behaviours and was based on the 10 educational sessions of the Manual Corazon Sano y Feliz, originally developed by NHLBI as part of the programme ‘Health for Your Heart’ described in the Introduction. The Manual includes educational sessions about CVD symptoms, risk factors, blood pressure, diabetes, high blood cholesterol, physical activity, health diet, weight control and smoking cessation.
Cardiovascular health promotion sessions
Patients participated in a series of group health promotion sessions conducted and delivered by CHWs. The content of the health promotion sessions was also based on the curriculum of the Corazón Sano y Feliz Manual. Family members or friends of patients were welcome to participate in the sessions to support enrolled patients with lifestyle changes as well as to communicate the need for CVD prevention in their households.
Pilot study design and measures
The pilot study was conducted and designed with the primary objective of assessing the feasibility of implementing the Corazon Sano y Feliz core components.
Geographic location
The pilot study was implemented in the municipality of Mixco, which is a typical low-income urban community of Guatemala. Mixco is located 18 kilometres south of Guatemala City with an urban population of ∼400 000. This setting was selected because it had adequate health infrastructure, a functional group of CHWs, and was accessible. In Mixco, the Ministry of Health operated one primary care level health centre and six health posts. Most of the activities of the pilot study were carried out within the physical space of the PHC centre.
Pilot study implementation
The pilot study was implemented in two phases:
Phase 1 (September 2007–July 2008) included: adaptation and validation of the Manual for CHW training, capacity enhancement of nurses and physicians to apply risk stratification and management algorithms, and carrying out the CHW training in cardiovascular health promotion.
Phase 2 (January–November 2009) was the actual recruitment, assessment, management and health promotion of patients (shown in Figure 1):
The pilot implementation was based on a logic framework to facilitate the assessment of the extent to which the implementation of Corazon Sano y Feliz was feasible. The implementation process was assessed by observation by study researchers, review of study reports, and interviews with nurses and CHWs, which served to compare the study as it was originally envisioned to how it was operationalised, and reasons for adaptation were documented (Summary Box) (Table 1).
Table 1:
Logical framework
| Objectives | Activities | Indicators | Expected result | Assumptions | |
|---|---|---|---|---|---|
| Clinical component | To provide adequate CVD risk assessment and clinical management to hypertensive individuals contributing to the improvement of quality of life for patients participating in the project. | Capacity enhancement of professional health workers through workshops providing methods for total CVD risk assessment, management and follow-up of patients. | 90% of doctors and nurses at the health centre make use of algorithms for detection, evaluation and management of risk factors, according to the absolute CVD risk. | 75% of patients with hypertension have positive changes in the levels of hypertension and other CVD risk factors. | Nurses and physicians have the time and commitment to perform programme related activities. |
| Patients with hypertension and diabetes are less likely to suffer complications associated with CVD. | There is availability of drugs for the treatment of hypertension patients. | ||||
| Nurses measure blood pressure and other risk factors in individuals. | Hypertensive patients make follow-up visits and sessions of promotion and prevention. | ||||
| Nurses stratify total CVD risk based on the WHO CVD risk prediction chart, using easy to measure parameters. | |||||
| Cardiovascular health promotion component | To improve knowledge and uptake of healthy behaviours of patients with hypertension by training CHW to conduct follow-ups and encouraging the adoption of healthy diets, physical activity and avoidance of tobacco consumption. | Selection and training of CHWs. | CHWs are actively involved in promoting the activities of care and prevention of CVD conducted by PHC centres. | CHWs incorporate the knowledge gained in their everyday practices. | Health districts demonstrates willingness to integrate CHW prevention and promotion of CVD. |
| Health promotion educational sessions delivered by CHWs for hypertensive patients. | 100% of patients with hypertension have a greater knowledge of CVD and its risk factors. | CHWs transmit their acquired knowledge to their communities. | There is interest in working in cardiovascular prevention and promotion within CHWs. | ||
| 60% of patients with hypertension incorporate at least one healthy habit at the end of the intervention. | 100% of patients with hypertension incorporate the knowledge gained in their everyday practices. | CHWs and patients with hypertension have minimum skills (reading and writing) to appropriate and convey concepts. | |||
| 100% of patients with hypertension are sensitized towards adoption of healthy habits. | Patients with hypertension transmits the acquired knowledge to their closest referents. | CHWs and patients with hypertension have nourishing diets and environmental conditions necessary for appropriate healthy practices. |
Data collection and analysis
To accomplish our secondary objective of determining Corazon Sano y Feliz's potential for change at the patient-level, nurses captured the following clinical measures at baseline, at intermediate visits to the clinic and at 6 months:
Blood pressure, measured three times with a calibrated automated device (Omron HEM-, 737Intelli Sense; Omron Healthcare, Vernon Hills, IL, USA) in the sitting position after 5 min of rest, and 1 min between each measurement.
Body weight (kg), measured using a calibrated scale.
Height (m), measured using a standardized stadiometer.
Body mass index (BMI), calculated as weight (kg)/height2 (m2). Overweight was classified as having BMI of 25 kg/m2 or greater.
Waist circumference (in centimetres, cm), measured following the protocol used in the Diabetes Prevention Programme (Diabetes Prevention Programme).
Abdominal obesity: >80 cm for women, >90 cm for men (Ministry of Health guidelines).
Blood glucose was measured in samples obtained randomly (some patients were fasting and some were non-fasting) with glucometers.
Knowledge and practices data were collected with a questionnaire administered by our research team to each CHW before and after their training, and to patients at baseline and 6 months after the intervention. The questionnaire used the My Knowledge and Family Habits Scale, a 70-item, self-reported, valid and reliable instrument, which has been used in other studies (Balcazar et al., 2006; Medina et al., 2007).
The potential for change was analysed using a one-group pretest-posttest study design to examine changes in clinical measures, knowledge, and practices between baseline and at the end of the 6-month intervention. Comparison of socio-demographic characteristics at baseline stratified by risk level was conducted to characterize the patient population. A test of significance for difference in socio-demographic characteristics between risk level groups was conducted using X2 analysis for categorical variables and one-way analysis of variance for continuous variables. This same analysis was also conducted at baseline for differences in patient characteristics by sex.
For comparisons in clinical measures, knowledge, and behaviour at baseline and 6 months, a paired two-sided t-test was conducted. The significance level for all tests was set at p = 0.05. All statistical analyses were conducted using STATA 12. We also conducted a sub-group analysis among low- and medium-risk patients treated with lifestyle intervention only.
RESULTS
Phase 1 (adaptation of educational materials and training of health personnel)
Adaptation and validation of the Manual
The beginning of the health promotion component entailed the adaptation and validation of the Manual Su Corazón, Su Vida to the local conditions of Mixco. We hired a specialist in communication science who conducted four focus group discussions (FGD), each with seven to eight members of the community with similar characteristics to the study target population. Participants in the FGD included teachers from a local school, housewives, the social worker from the PHC Centre, officers from the Municipality and a midwife from the Community of Mixco. The adaptation and validation did not require very extensive changes to the original Manual since cultural and socio-economic conditions of the population of Mixco are similar to those of the U.S. Latino population from which the original manual originated. The main product of the FGD was the validated version of the Manual that was renamed Manual Corazon Sano y Feliz.
Capacity enhancement of nurses and physicians
The capacity enhancement of nurses and physicians was accomplished through three workshops delivered by our research team at the PHC centre of Mixco taking advantage of time regularly allotted for continuing education of professional staff. The workshops were delivered to 5 physicians and 10 nurses working at the PHC Centre and at the 6 health posts of Mixco. No formal evaluation was conducted to assess change of knowledge and practices among the participants but the health workers expressed their willingness to collaborate with the pilot study despite their multiple occupations. However, in the implementation it was noticed that the health professionals were not performing all that work as patients were not reaching the CHWs. For this reason two nurses were hired to carry out the patient assessment and management.
CHW recruitment and training
We recruited 29 CHWs (27 women, mean age = 31 years and 2 men, mean age = 25) who were already collaborating with the Mixco PHC centre and active in the community but with no previous training in CVD. With the exception of two CHWs who had studied to be auxiliary nurses, all of the others' highest level of study was equivalent to middle school (through eighth grade). The project was presented to the CHWs before training. Emphasis was placed on the project objectives and the required commitment.
The training was based on the Manual Corazon Sano y Feliz and its methodological implementation was followed almost to the letter, no substantial changes were made to the training schedule. From the beginning, each CHW was motivated by giving them the tools needed to work with the community: a sphygmomanometer, a glucometer, a tape measure for the waist and the instruments bag. This equipment was suggested by those who participated in the validation process of the manual in light of the economic conditions of the promoters, and because it could be used at the health centre. Training sessions were conducted every 15 days at the Mixco PHC centre lasting ∼2 h. CHW attendance at these sessions was constant throughout the period, and they rarely missed them.
Phase 2 (clinical care and cardiovascular health promotion for hypertensive patients)
Patient detection and recruitment
Two strategies were used to detect and recruit hypertensive individuals in a 5-month period:
(i) Opportunistic screening of patients attending the PHC centre any day for any condition, and (ii) screening during two health fairs in strategic locations on weekends.
The ‘snowball effect’ resource was also used to invite people to the programme. CHWs and patients themselves referred the project activities and invited local people to participate.
Baseline characteristics of participants by cardiovascular risk level are presented in Table 2, as patients were stratified by risk level at the beginning of the study. A total of 85 patients were enrolled during a 5-month period, between January and May 2009, and 78 were followed up for 6 months. Seven patients were dropped from the study for failure to return for follow-up visits. Thirty-one patients were stratified as having low CVD risk, 22 had medium risk and 25 had high risk. The majority of patients (71%) were women. The mean age of participants was 61 years with a significant difference (p < 0.001) between low-, medium- and high-risk groups, with low-risk patients being on average 10 years younger. Over half of low- and medium-risk patients' highest level of schooling was complete primary school and for high-risk patients 68% had completed secondary school. Thirty-seven patients (47%) had diabetes; only four of these patients had a diagnosis before recruitment; 33 were diagnosed upon entering the study. Forty-five patients were overweight and 63 (81%) had abdominal obesity, with women being significantly more likely to be abdominally obese than men (p < 0.001). Only two low-risk patients reported that they smoked. According to our management algorithm, the 53 patients with low and medium risk were treated just with healthy lifestyle counselling, and the 25 high-risk patients were treated with healthy lifestyle counselling plus anti-hypertensive drug therapy.
Table 2:
Baseline characteristics of patients participating in Corazón Sano y Feliz in Mixco, Guatemala by global cardiovascular risk level
| Global cardiovascular risk level |
p-value | |||
|---|---|---|---|---|
| Low risk n = 31 (39.7%) |
Medium n = 22 (28.2%) |
High n = 25 (32.1%) |
||
| Mean age in years (±SD) | 54.1 ± 9.1 | 66.5 ± 9.5 | 64.6 ± 10.7 | p < 0.001 |
| Female | 22 (71.0%) | 14 (63.6%) | 18 (72.0%) | p = 0.80 |
| Education level | p = 0.14 | |||
| Complete elementary | 16 (51.6%) | 12 (57.1%) | 8 (32.0%) | |
| Complete secondary | 13 (41.9%) | 9 (42.9%) | 17 (68.0%) | |
| Higher education | 2 (6.5%) | 0 | 0 | |
| Disease status | ||||
| Type 2 diabetes mellitus | 12 (41.4%) | 11 (50.0%) | 14 (56.0%) | p = 0.56 |
| Overweight/obesity | ||||
| Patients with BMI ≥ 25 kg/m2 | 17 (60.7%) | 13 (59.1%) | 15 (60.0%) | p = 0.99 |
| Patients with abdominal obesity | 26 (83.9%) | 17 (77.3%) | 22 (88.0%) | p = 0.61 |
| Tobacco use | 2 (6.5%) | 0 | 0 | p = 0.21 |
Risk factor assessment, clinical management and follow-up of patients
These activities were carried out by two previously-trained nurses at the PHC centre of Mixco on Saturdays. Initially, opening the study's clinic on Saturday had not been considered, but through recommendations made by health authorities and CHWs, it was decided to work on that day to provide participation opportunities for those who worked during weekdays, especially men. During the time the project was implemented on Saturdays, the clinic operated as a clinic for hypertension and diabetes. According to the Corazón Sano y Feliz protocols, at Visit 1 nurses assessed blood pressure and other risk factors, and stratified patients' total CVD risk. Treatment was based on total CVD risk (see above), restricting anti-hypertension drug therapy to high-risk individuals. For effective treatment, we had to secure a special supply of thiazide diuretics given the usual lack of these medications in the Guatemalan PHC system. According to clinical protocols, all patients had two follow-up visits to the clinic; and as part of the comprehensive management, nurses invited all patients to participate in the health promotion activities delivered by the CHWs.
Cardiovascular health promotion
Although it was originally envisioned to have at least three meeting places throughout the city of Mixco, this had to be reconsidered as it was very difficult to coordinate and synchronize the education sessions of the various groups. For this reason, it was jointly decided by CHWs and professionals to have a single place in a room contiguous to the PHC centre and a designated day to hold the health promotion sessions. For delivering the sessions, groups consisting of three CHWs were organized. Training sessions were held every 2 weeks. Patients' training included just 6 educational sessions from the Manual, and not all 10 because the CHWs felt that several topics were repeated, particularly the one related to a healthy diet. In accordance, the following topics were prioritized: Session 1 (general introduction to cardiovascular risk), Session 4 (high blood pressure control), Session 7 (take care of your diabetes), Session 3 (physical activity) and Session 6 (maintain a healthy weight). The CHWs had the role of organizing and conducting two cycles of the six sessions because the recruitment of patients was done gradually. All patients participated in at least three sessions; 44 patients (56%) attended all six sessions.
Changes in patient knowledge and clinical outcomes
Changes in clinical measures and knowledge and behaviour scores at baseline and at 6-month follow-up are presented in Table 3, both for all participating patients (n = 78), and separately for the sub-group of lifestyle-only participants (n = 53). The mean SBP and DBP of patients at baseline (Visit 1) were 160.1 ± 16.5 mmHg and 91.1 mmHg (SD: 8.8). The mean SBP and DBP measured at 6 months were 132.8 (SD: 15.1) and 83.4 (SD: 6.4) mmHg, showing a significant reduction of 27.2 and 7.7 mmHg of SBP and DBP from the mean baseline level (p < 0.0001). At 6 months, 48 patients (60%) had reduced their blood pressure to normal levels (<140/90 mmHg). There were also small but statistically significant reductions in mean weight (from 145.2 ± SD to 143.9 pounds, p = 0.02), mean BMI (from 26.5 to 26.2 kg/m2, p = 0.01) and mean waist circumference (from 89.6 to 88.9 cm, p = 0.02) between baseline and 6 months. On average, patients increased their composite knowledge and behaviour score from 54.6 to 59.1 out of a possible 70 points (p < 0.0001) comparing their pre- and post-test scores.
Table 3:
Baseline to posttest (6 months) differences in health outcomes and knowledge and behaviour for study participants receiving medication and lifestyle treatment
| Clinical measure | n | Mean (SD) at baseline | Mean (SD) at 6 months | t-test | p-value |
|---|---|---|---|---|---|
| Systolic blood pressure, mmHg | |||||
| All patients | 78 | 160.1 (16.5) | 132.8 (15.1) | 14.11 | p < 0.0001 |
| Lifestyle treatment only | 53 | 152.3 (12.2) | 129.4 (12.5) | 11.26 | p < 0.0001 |
| Diastolic blood pressure, mmHg | |||||
| All patients | 78 | 91.1 (8.8) | 83.4 (6.4) | 7.28 | p < 0.0001 |
| Lifestyle treatment only | 53 | 91.2 (8.4) | 82.7 (6.2) | 6.70 | p < 0.0001 |
| Weight, pounds | |||||
| All patients | 78 | 145.2 (21.7) | 143.9 (22.0) | 2.50 | p = 0.02 |
| Lifestyle treatment only | 53 | 147.7 (20.8) | 146.6 (21.3) | 1.55 | p = 0.13 |
| BMI, kg/m2 | |||||
| All patients | 75 | 26.5 (4.9) | 26.2 (4.7) | 2.55 | p = 0.01 |
| Lifestyle treatment only | 50 | 26.7 (5.2) | 26.5 (5.0) | 1.56 | p = 0.12 |
| Waist circumference, cm | |||||
| All patients | 77 | 89.6 (8.8) | 88.9 (8.7) | 2.41 | p = 0.02 |
| Lifestyle treatment only | 52 | 89.6 (9.0) | 88.9 (8.9) | 1.80 | p = 0.08 |
| Knowledge/behaviour scores | |||||
| All patients | 78 | 54.6 (6.2) | 59.1 (8.1) | −5.10 | p < 0.0001 |
| Lifestyle treatment only | 53 | 54.7 (6.8) | 59.6 (9.1) | −4.45 | p < 0.0001 |
The sub-group of low- and medium-risk participants who were not given blood-pressure-lowering medications (n = 53), showed significant reductions in SBP (from 152.3 to 129.4 mmHg; p < 0.0001) and DBP (from 91.2 to 82.7 mmHg, p < 0.0001) between baseline and 6 months. For these participants, mean knowledge and behaviour scores also changed significantly, increasing from 54.7 to 59.6 (p < 0.0001). We did not observe significant changes in BMI, waist circumference and body weight. At 6 months, the risk classification of patients showed a reduction compared with the classification at baseline. Fifty-seven patients (73%) were found to be low risk, eighteen (23%) were medium risk and three (4%) were high risk (Table 3).
DISCUSSION
Corazon Sano y Feliz was successfully implemented in the PHC centre of Mixco, Guatemala. The pilot implementation took advantage of community and health authorities' interest in the project, the existing infrastructure and human resources at the PHC centre, and that there were a group of CHWs already active in the community. During the intervention study, we carried out most of the activities envisioned within the logical framework and its operational plan. The objectives, subject population and chronogram were not significantly altered during the pilot study implementation. However, some methodological strategies were adjusted because either the conditions demanded it or because it was demonstrated that the change would favour implementation.
One of the main contributors to the success of the pilot study was the focus on implementing strong partnerships. From the beginning, the study investigators worked in close collaboration with the Ministry of Health, involving both national and local authorities. At the national level, partnership with the Programme of Chronic Diseases of the Ministry of Health was instrumental in obtaining necessary authorizations and approvals. At the local level, collaboration with authorities of the Mixco Health District permitted sufficient space for the CHW training and allowed for the opening and functioning of the clinic on Saturdays. Another key partnership was established with the Municipality of Mixco, which organized health fairs to recruit patients, provided a meeting room contiguous to the health centre for education sessions, and supported physical activity group sessions.
In our study we obtained a patient population with higher-than-average education levels when compared with a typical cross section of the population, potentially due to self-selection to participate in the education sessions. For scaling up the intervention more broadly to the Guatemalan population, it will be important to also offer cardiovascular health education to a non-literate population. Study participants demonstrated a high level of enthusiasm for participating and only seven patients did not continue after baseline. In fact, low- and medium-risk patients often came to the health centre even more frequently than they were requested to return for follow-up, and the health centre became almost like a social gathering place on Saturdays. Over two-thirds of the patients were women despite the concerted effort to include equal numbers of men and women by opening the health centre on Saturdays. Had the programme only been offered during weekdays, it is likely that even fewer men would have participated.
Despite the overall success of the pilot study, we encountered a number of barriers. One of them was the heavy workload of health personnel. Initially, their day-to-day work obligations impeded dedication to study activities. This barrier was overcome by hiring and paying a salary supplement to two nurses for working extra hours on Saturdays. This finding is important for considering the replication of Corazón Sano y Feliz in other regions of the country. Health authorities will need to allocate resources to provide incentives to scale up the inclusion of CVD risk reduction in primary care services. The additional hours that are needed to train health personnel also translate to an initial investment by government programmes. Another important barrier that the study faced initially was the lack of medications at the health centre. Future implementation of Corazón Sano y Feliz will also require that health authorities commit resources to supply primary care facilities with essential medications to treat hypertension and diabetes.
As indicated in the Introduction, our secondary purpose was to present changes in patient knowledge and clinical outcomes. The pilot study showed significant reductions in blood pressure levels and other risk factors comparing baseline and 6-month measurements, and increased levels of knowledge and practices related to CVD for 78 hypertensive patients. While we observed statistically significant changes, not all measures showed significant change to be of public health importance. For those patients who only received lifestyle modification, we also observed significant reductions in blood pressure, which indicates that risk classification may be an adequate approach for determining who should be provided medication.
The average SBP reduction (27.2 mmHg) was greater than average reductions in SBP reported in other community-based interventions (Balcazar, et al, 2001; Jafar, et al, 2009; Truncali, et al, 2010). This is likely due to the higher baseline SBP level in our population (160.1 mmHg) and by the fact that we included mostly newly-diagnosed patients. As high-risk patients received anti-hypertension medication we consider that the observed reduction in blood pressure is likely to be an effect of drug therapy. In our study, the reduction in blood pressure may also be attributed to reduced salt intake and increased physical activity, both of which were themes included in the education sessions, however these measures were not captured. Physical activity was also promoted through the walking sessions organized by the municipality. Consistent with other studies in which SPSC has been used (Balcazar, et al, 2006; WHO, 2007), participants demonstrated a significant improvement in heart-healthy behaviour and knowledge.
However, our results should be interpreted with caution as the study had a number of limitations. We did not make use of a more sophisticated study design, which could have included a control group and longer patient follow-up. Due to not having a control group, it is possible that the observed changes are in part due to measurement bias and increasing familiarity with the procedure. The primary inclusion criterion for individual study participants was hypertension, which means that non-hypertensive high-risk patients could be missed. Socio-demographic covariates were not controlled for and a simple paired t-test analysis was conducted comparing baseline and 6-month clinical measures. The study was small and was only implemented in one health centre. The study did not capture variables that could explain what the dramatic reductions in systolic and diastolic blood pressure seen in the sub-group not receiving medication were due to. For the high-risk sub-group that received medication, treatment adherence was not documented; this variable would have been valuable to document the extent to which blood pressure reduction was associated with anti-hypertensive drugs. It was not possible to measure changes in blood glucose levels because not all patients had fasting glucose levels measured at baseline.
In future research, we recommend: including a comparison group, including patients with hypertension and/or type 2 diabetes in order to capture high-risk patients that may not have high blood pressure, systematic monitoring of glucose levels in which patients are fasting at baseline and follow-up, follow-up with patients for a longer period to determine whether their lifestyle modification persists, and separating out the analysis of diet, physical activity and medication use to determine which components of the intervention are most effective. Social support and self-efficacy are also important measures to include in future analysis of disease management and control.
Lessons learned and policy implications
Given the results from this study we conclude that it is practical and feasible to implement a community-based, hypertension management intervention in low-resource, urban settings in Guatemala. We consider that the involvement of the municipal government, Ministry of Health and community members allowed for implementation of this project. It is important to adapt the intervention to the socio-economic, cultural and health infrastructure contexts in distinct settings; this project specifically captured women and literate populations and it will be important to expand the reach to men and non-literate populations in the future. In future analyses it will be important to include measures beyond those used in this study to more precisely assess the relative contribution of education and clinical components of hypertension management interventions.
The experience of Corazón Sano y Feliz in Mixco has implications for health policy and research both within Guatemala and for the region. Key aspects of the clinical component have been incorporated into recent Ministry of Health guidelines for the treatment of hypertension. In 2011, Corazón Sano y Feliz was adapted for a study implemented in government health centres in San José, Costa Rica and Tuxtla Gutierrez, Chiapas in México for patients with hypertension and type 2 diabetes, using a more robust study design with intervention and comparison groups. Future projects and studies will contribute to the evidence base about the feasibility and impact of similar CVD interventions, an area of increasing importance due to the rising burden of CVD morbidity and mortality in developing countries.
SUPPLEMENTARY DATA
Supplementary data are available at Health Promotion International online.
FUNDING
The authors acknowledge the two sponsoring organisations: the National Heart, Lung and Blood Institute (NHLBI) and the Pan American Health Organization (PAHO) for the financial and technical support provided for the implementation of the pilot study.
Supplementary Material
REFERENCES
- Alcalay R., Alvarado M., Balcazar H., Newman A., Huerta E. (1999) Salud Para Su Corazón: a community-based Latino cardiovascular disease prevention and outreach model. Journal of Community Health, 24, 359–379. [DOI] [PubMed] [Google Scholar]
- American Association of Diabetes Educators. (2003) Position statement: diabetes community health workers. Diabetes Education, 29, 818–824. [Google Scholar]
- Balcazar H., Alvarado M., Alcalay R., Schindeldecker M., Newman E., Huerta E., et al. (2001) Salud Para Su Corazón: evaluating cardiovascular health outreach activities in the Latino community. Medicine of the Americas, 2, 4–11. [Google Scholar]
- Balcázar H., Alvarado M., Cantu F., Pedregon V., Fulwood R. A. (2009) Promotora de Salud model for addressing cardiovascular disease risk factors in the US-Mexico border region. Preventing Chronic Diseases, 6, A02. [PMC free article] [PubMed] [Google Scholar]
- Balcázar H., Luna-Hollen M., Medina A., Pedregon V., Alvarado M., Fulwood R. (2006) The North Texas Salud para su Corazón Promotor/a outreach program: an enhanced dissemination initiative. The Health Education Monograph Series, 22, 19–27. [Google Scholar]
- Beaglehole R., Epping-Jordan J., Patel V. (2008) Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet, 372, 940–999. [DOI] [PubMed] [Google Scholar]
- Becker M. H. (1974) The Health Belief Model and sick-role behavior. Health Education Monographs, 2, 409–419. [Google Scholar]
- Beckett N. S., Peters R., Fletcher A. E., Staessen J. A., Liu L., Dumitrascu D., et al. (2008) HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. New England Journal of Medicine, 358, 1887–1898. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Department of Health and Human Services. (2003) Community Health Workers and Promotores de Salud: Critical Connections in Communities. http://www.cdc.gov/diabetes.comm.
- Chobanian A. V., Bakris G. L., Black H. R., Cushman W. C., Green L. A., Izzo J. L., et al. (2003) National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Journal of the American Medical Association, 289, 2560–2572. [DOI] [PubMed] [Google Scholar]
- Corkery E., Palmer C., Foley M. E., Schechter C. B., Fisher L., Roman S. H. (1997) Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population . Diabetes Care, 20, 254–257. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Lifestyle Resource Core Wing R, Gillis B. The Diabetes Prevention Program's Lifestyle Change Program, Manual of Operations http://www.bsc.gwu.edu/dpp/index.htmlvdoc.
- Ebrahim S., Smith G. D. (2001) Exporting failure? Coronary heart disease and stroke in developing countries. International Journal of Epidemiology, 30, 201–205. [DOI] [PubMed] [Google Scholar]
- Fahey T., Schroeder K., Ebrahim S. (2006) Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database of Systematic Review, CD005182. [DOI] [PubMed] [Google Scholar]
- Fedder D., Chang R. J., Curry S., Nichols G. (2003) The effectiveness of a community health worker outreach program on healthcare utilization of West Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethnicity and Disease, 13, 22–27. [PubMed] [Google Scholar]
- Greenland P., Alpert J. S., Beller G. A., Benjamin E. J., Budoff M. J., Faya Z. A., et al. (2010) ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology, 56, 2–54. [DOI] [PubMed] [Google Scholar]
- Jafar T. H., Hatcher J., Poulter N., Islam M., Hashmi S., Qadri Z., et al. (2009) Community-based interventions to promote blood pressure control in a developing country. Annals of Internal Medicine, 151, 593–601. [DOI] [PubMed] [Google Scholar]
- Lim S. S., Gaziano T. A., Gakidou E., Reddy K. S., Farzadfar F., Lozano R., Rodgets A. (2007) Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet, 370, 2054–2062. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D. M., Evans J. C., Levy D. (2005) Hypertension in adults across the age spectrum: current outcomes and control in the community. Journal of the American Medical Association, 294, 466–472. [DOI] [PubMed] [Google Scholar]
- Lopez A. D., Mathers C. D., Ezzati M., Jamison D. T., Murray C. J. (2006) Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet, 367, 1747–1757. [DOI] [PubMed] [Google Scholar]
- Love M. B., Gardner K., Legion V. (1997) Community health workers: who they are and what they do. Health Education and Behaviour, 24, 510–522. [DOI] [PubMed] [Google Scholar]
- McKinstry B., Hanley J., Heaney D., McCloughan L., Elton R., Webb D. J. (2006) Impact on hypertension control of a patient-held guideline: a randomised controlled trial. British Journal of General Practice, 56, 842–847. [PMC free article] [PubMed] [Google Scholar]
- Medina A., Balcázar H., Luna-Hollen M., Nkoma E., Soto L., Mas F. (2007) Promotores de Salud: educating Hispanic communities on heart-healthy living. American Journal of Health Education, 38, 194–202. [Google Scholar]
- Mendoza Montano C., Estrada K., Chavez A., Ramírez-Zea M. (2008) Perceptions, knowledge and beliefs about prevention of cardiovascular diseases in Villa Nueva, Guatemala. Prevention and Control, 3, 1–9. [Google Scholar]
- Ministry of Public Health (2009) National Epidemiological Bulletin No. 26. Guatemala. [Google Scholar]
- Morisky D. E., Levine D. M., Green L. W., Shapiro S., Russell R. P., Smith C. R. (1983) Five-year blood pressure control and mortality following health education for hypertensive patients. American Journal of Public Health, 73, 153–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez L., Martinez J. (2008) Community health workers: social justice and policy advocates for community health and well-being. American Journal of Public Health, 98, 11–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto R., Bulhoes da Silva S., Soriano R. (2011) Community health workers in Brazil's unified health system: a framework of their praxis and contributions to patients health behaviors. Social Science and Medicine, 30, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy K. S. (2004) Cardiovascular disease in non-western countries. New England Journal of Medicine, 350, 2438–2440. [DOI] [PubMed] [Google Scholar]
- SPSC (2006) Health Promotion Practice, January 2006, Vol. 7, No. 1, 68–77.
- Su Corazón, Su Vida: Manual for Health Promoters. (2000) Bethesda MD: National Heart, Lung, and Blood Institute; http://hp2010.nhlbihin.net/salud/pa/session2/teaching/index.htm (Accessed 22 May 2009). [Google Scholar]
- The World Health Report 2002 (2002) World Health Organization; Geneva. [Google Scholar]
- Truncali A., Dumanovsky T., Stollman H., Angell S. Y. (2010) Keep on track: a volunteer-run community-based intervention to lower blood pressure in older adults. Journal of the American Geriatric Society, 58, 1177–1183. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2007) Prevention of Cardiovascular Disease: Guidelines for Assessment and Management of Total Cardiovascular Risk. World Health Organization, Geneva. [Google Scholar]
- Yusuf S., Reddy S., Ounpuu S., Anand S. (2001) Global burden of cardiovascular diseases: Part I: General considerations, the epidemiological transition, risk factors, and impact of urbanization. Circulation, 104, 2746–2753. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.