Abstract
Alternatives to in-center hemodialysis as treatment for end-stage renal disease have been shown to increase patient quality of life, decrease co-morbidities and decrease financial strain on both the patient and the health care system. Focus groups (n = 6 groups with 47 participants) and survey data (n = 113) were used to ascertain perceived barriers and facilitators to alternative therapies and psychosocial and educational issues that may affect a patients' choice of modality among patients utilizing in-center dialysis, home dialysis and renal transplantation. Fear emerged as a predominant theme, both at diagnosis and when choosing a modality. Distrust of the medical system, denial and patient experiences with previous modalities were seen as barriers to care. Results imply that interventions addressing fear and providing more comprehensive pre-dialysis education may decrease barriers.
Introduction
The incidence and prevalence of end-stage renal disease (ESRD) in the United States continues to rise, creating a mounting burden on patients, caregivers and the medical system (United States Renal Data System [USRDS], 2008). Although peritoneal dialysis (PD), home hemodialysis (HD) and kidney transplantation have been shown to increase patient independence, decrease co-morbidities and increase patient quality of life overall, rates of these alternative renal replacement therapies (RRTs) remain low (Arkouche et al., 1999; Medical Education Institute, 2006; Mehrotra, Marsh, Vonesh, Peters, & Nissenson, 2005; Rubin, Fink, Plantiga, Sadler, Kliger, & Powe, 2004; USRDS, 2008; Wu et al., 2001). Rates of PD peaked in 1995 at 15% but have tapered off since then. According to 2006 prevalence data from the USRDS (2008), only 5.2% of ESRD patients are on PD, less than 2.6% are treated with home HD and only 30% have a working kidney transplant. Economically speaking, switching to or starting home therapies or receiving a kidney transplant is less expensive for both the patient and the medical system, with HD costs at $71,889 per person per year in 2006, compared to $53,327 and $24,951 for PD and transplant, respectively (Shih, Guo, Just, & Mujais, 2005; USRDS, 2008).
In the face of dramatic developments in treatment and technology and increasing patient-centered education, research has begun to focus on potential reasons for patients' reluctance to choose an alternative to in-center HD. Pre-dialysis educational programs have been shown to decrease anxiety about dialysis and have a positive effect on participants' feelings that they have the knowledge and tools to make their own choice about RRT, but these programs are not mandated and are often infrequent (Goovarts, Jadoul, & Goffin, 2005; Iacono, 2005; Klang, Bjorvell, & Cline, 1999; McLaughlin, Manns, Mortis, Hons, & Taub, 2003; Mehrotra et al., 2005). Myths abound in both patient and provider communities about PD, including perceptions that it is inappropriate for patients who are noncompliant or obese, has poor survival rates, has high infection risks, and demands that patients be totally independent (Bernadini, 2004).
Focused interviews and surveys among ESRD patients have started to explore issues of choice regarding RRT (Bernardini, 2004; Landraneau & Ward-Smith, 2006; McLaughlin et al., 2003; Tweed & Ceaser, 2005; Winkelmayer, Glynn, Levin, Owen, & Avorn, 2001; Wuerth et al, 2002). Focus groups and interviews have previously addressed patient satisfaction and quality-of-life domains (Bass et al., 1999; Rubin et al., 2004; Wu et al., 2001). PD patients gave significantly higher ratings on items such as “information given to help choose modality” and “the amount of dialysis information from staff” as compared with HD patients (Rubin et al., 2004). There were also statistically significant differences between PD and HD with regard to amount of travel required, dietary restrictions, sleep, role functioning and general quality of life, all favoring PD (Bass et al., 1999; Rubin et al., 2004).
There has been considerable research on modality choice and quality of life for ESRD patients but less is known about how patients are presented with the information, how patients may receive it based on psychosocial factors and what patients are going through physically and emotionally at the time RRT information is presented. Focus groups and survey data were used for an exploratory analysis with ESRD patients to better understand their perceptions of methods for educating newly diagnosed ESRD patients about RRT; perceptions of their disease at onset and how these perceptions may influence their choice of RRT; and perceived barriers and facilitators to alternative forms of RRT.
Methods
This project utilized a “mixed model” approach, employing both qualitative (focus group) and quantitative (survey) data within and across the stages of the research process. This approach allows the researcher to draw from the strengths and minimize the weaknesses in both quantitative and qualitative methodologies (Johnson & Onwuegbuzie, 2004). The mixed model can be viewed as a third, hybrid paradigm of research methodology, and is useful for measuring different and overlapping facets of the same research question using different research approaches (Greene, Caracelli, & Graham, 1989; Tashakkori & Teddle, 2002).
Study Sample and Recruitment
Recruitment for focus groups was performed by nephrology social workers at two dialysis clinics in North Carolina. Eligible participants were English-speaking patients on in-center and home dialysis therapies (PD or home HD) who were 18 or older. Patients eligible for home dialysis therapies who instead chose in-center HD were eligible for the in-center HD groups. Separate groups for home dialysis patients were utilized to explore the factors that made these groups more likely to choose home therapy over in-center dialysis. Participants signed consent at the time of the focus group and received a $25.00 gift card as reimbursement for time and travel.
Subjects for survey participation were recruited by nephrology social workers through five dialysis clinics in North Carolina and by one of the researchers at the kidney transplantation clinic of UNC Hospitals, which sees approximately 100 patients every month. Surveys were self-administered and completed in the clinic or at the dialysis unit. Eligible participants were English-speaking in-center or home dialysis (HD or PD) patients or kidney transplant recipients who were 18 or older. There was no reimbursement for survey participation. Eligible patients were given an informed consent explaining the study and efforts to protect patient confidentiality.
Approval by the University of North Carolina Institutional Review Board was obtained prior to the implementation of the study.
Design: Focus Groups
Focus groups were conducted between August and September 2007. The lead investigator moderated all groups. The moderator used a scripted discussion guide that was created by the study investigators. Each focus group session lasted between 60 and 90 minutes, and was audiotaped and transcribed verbatim. Questions for discussion were framed under two main themes: (a) patient experiences dealing with disease onset and RRT modalities and (b) choosing a modality. Appendix A lists the questions used in the focus groups, along with corresponding “probe” questions to keep the discussion going.
Individual recordings were transcribed and uploaded into ATLAS.ti software package (Muhr, 2005). ATLAS.ti allows researchers to more easily code, organize and interpret qualitative data. Researchers utilized the grounded theory approach, which allows the theory to emerge from the data, versus a hypothesis-driven theory (Glaser & Strauss, 1967). Grounded theory uses open coding (free form coding for words, themes, expressions, etc.) followed by axial coding, which seeks to explore categories created through the open coding process. Because this was an exploratory study, the authors utilized grounded theory to let the data “speak for itself” with the use of ATLAS.ti to supplement coding procedures and data organization.
The first and second authors used open coding to create a “base coder list” devised from their individual readings of the transcripts. All transcripts were then re-reviewed and coded by the same two members of the research team. Themes emerged in each section based on ongoing analysis using axial coding. Codes present in three or more theme sections were investigated by extracting those codes from the whole transcript and then examining codes that co-occurred within each theme section. Co-occurring codes within theme sections were reviewed and discussed by the same two coauthors for consistency and to increase inter-rater reliability. The authors were satisfied that saturation had been reached.
Design: Survey
Surveys were collected to gather quantitative data on a broader ESRD population outside the focus groups. Survey questions captured demographic data, awareness of dialysis options, pre-dialysis educational opportunities and reasons for and against alternative modality choices. The survey was developed by the co-authors, based, in part, on literature review, with consensus agreement on items to include. The survey was not validated prior to its employment.
All survey participants answered general demographics questions (education, income, insurance status, etc.), described factors around the time of their ESRD diagnosis (acute vs. chronic renal failure, length of time seen by nephrologists before renal failure) and gave their perceptions on the quantity and quality of RRT education. The remaining survey questions were divided into sections based on modality (in-center HD, home dialysis or transplant) and addressed perceived barriers to other forms of dialysis and factors influencing how they made the choice for their current modality.
Survey responses were analyzed using Stata 10.1 (StataCorp, 2007). Tabulated proportions and means were determined by complete case analysis. Continuous variables among categories of RRT were compared using one-way analysis of variance (ANOVA) if normally distributed. Kruskal-Wallis testing was employed for continuous variables not distributed normally. Categorical variables were compared using Fisher's exact test. Test statistics producing p < 0.05 were considered to be statistically significant.
Results
Focus Group Demographics
A total of 47 patients participated in 6 focus groups (Table 1). There were 12 participants on PD and 35 receiving in-center HD; no home HD patients participated. One transplant patient participated in a PD group. Four participants did not report age. One of these four also did not report education level or insurance status, and another did not report number of years on dialysis. There was an overrepresentation of female and African-American participants that was somewhat greater in the HD group, which was 70% female and 80% African American, compared to the PD group, which was 60% female and 60% African American. These differences, however, did not achieve statistical significance.
Table 1. Focus Group Participant Characteristics.
| In-Center Hemodialysis (N = 35) | Peritoneal Dialysis (N = 12) | p-Value | Total (N = 47) | |
|---|---|---|---|---|
|
| ||||
| Age, years (SD), (N = 43) | 54.6 (12.9) | 49.3 (16.3) | 0.3 | 53.1 (13.9) |
|
| ||||
| Sex (%), (N = 46) | 0.5 | |||
| Male | 10 (29.4) | 5 (41.7) | 15 (32.6) | |
| Female | 24 (70.6) | 7 (58.3) | 31 (67.4) | |
|
| ||||
| Race (%) | 0.2 | |||
| White | 6 (17.1) | 5 (41.7) | 11 (23.4) | |
| African american | 28 (80.0) | 7 (58.3) | 35 (74.5) | |
| Hispanic | 1 (2.9) | 0 | 1 (2.1) | |
|
| ||||
| Education (%), (N = 46) | 0.8 | |||
| Did not graduate high school | 9 (26.5) | 2 (16.7) | 11 (23.9) | |
| High school graduate | 10 (29.4) | 5 (41.7) | 15 (32.6) | |
| > High school education* | 15 (44.1) | 5 (41.7) | 20 (43.5) | |
|
| ||||
| Years on dialysis, median (IQR) †, (N = 46) | 4 (2, 7) | 1 (1, 3) | 0.005 | 3 (1,6) |
|
| ||||
| Insurance status (%), (N = 46) | 0.1 | |||
| Medicare | 10 (29.4) | 2 (16.7) | 12 (26.1) | |
| Medicare/Medicaid | 13 (38.2) | 2 (16.7) | 15 (32.6) | |
| Medicare/Private ins. | 8 (23.5) | 6 (50.0) | 14 (30.4) | |
| Medicare/State plan | 2 (5.9) | 0 | 2 (4.4) | |
| Other | 1 (2.9) | 2 (16.7) | 3 (6.5) | |
|
| ||||
| On transplant wait list (%) | 18 (51.4) | 8 (66.7) | 0.8 | 26 (55.3) |
| Don't know | 3 (8.6) | 1 (8.3) | 4 (8.5) | |
|
| ||||
| Previously on other modality (%) | 10 (28.6) | 10 (83.3) | 0.002 | 20 (42.6) |
Includes those who attended vocational/technical schools, college (whether or not completed) and those with graduate/professional degrees.
Median and inter-quartile range are reported as data were not normally distributed. Kruskal-Wallis test results reported.
Results with a p-value < 0.05 are considered to be statistically significant. Casewise deletion was used to account for missing data in tabulating proportions and comparisons.
Total N provided separately for instances of missing data.
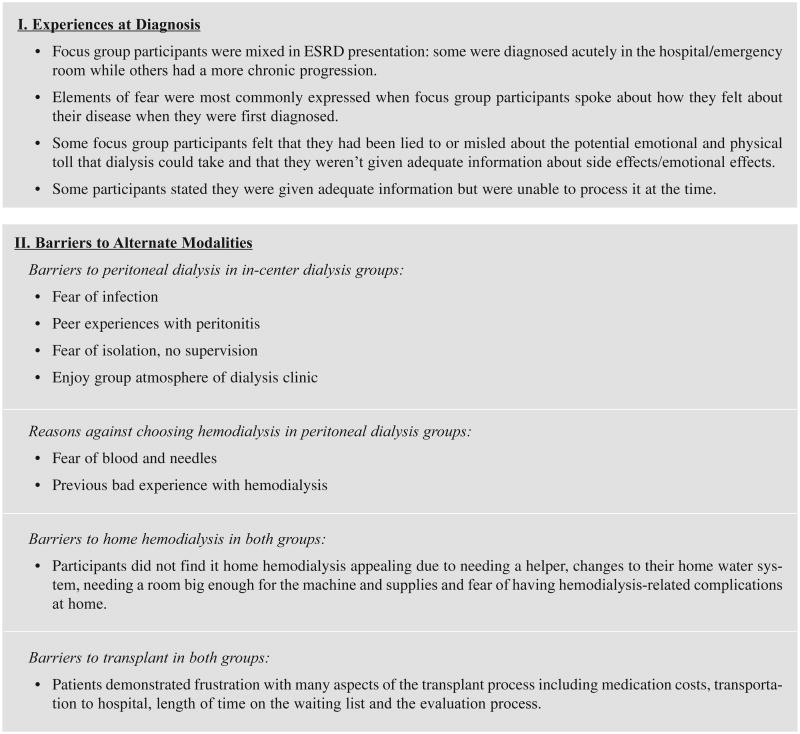
Participant age ranged from 21 to 80 years and 83% had a high school degree or higher level of education. Time on dialysis ranged from less than 1 year to 9 years. HD and PD patients differed in this regard, with PD participants having a median time on dialysis 3 years less than in-center HD participants (1 vs. 4 years, p = 0.005). Fifty-five percent reported being on the transplant waiting list. The number of patients on the transplant waiting list was greater in the PD group than the in-center HD group (66.7 vs. 52.4%, p = 0.8), although this was not statistically significant. Most notably, more than 80% of participants in the PD group previously employed in-center HD while less than 30% of participants in the in-center HD group previously received in-home therapies (p = 0.002). Main themes extracted from focus group responses are summarized in Figure 1.
Figure 1.
Summation of Focus Group Themes
Survey Demographics
Three hundred forty surveys were distributed through 4 dialysis centers and 85 surveys were distributed via the UNC kidney transplantation clinic. A total of 113 surveys were returned; 1 survey was excluded due to an excess of missing information including present modality of therapy. The remaining surveys were missing data in less than 10% of response variables except for duration of ESRD, which was missing in 18 (15.9%) respondents (7 HD, 2 PD and 9 transplant). Of the remaining 112 survey respondents, 54 had functioning renal transplants, 20 were on PD and 38 were using in-center HD. No participants were currently using home HD (Table 2).
Table 2. Survey Participant Characteristics.
| In-Center Hemodialysis (N = 38) | Peritoneal Dialysis (N = 20) | Renal Transplant (N = 54) | p-Value | Total (N = 112) | |
|---|---|---|---|---|---|
|
| |||||
| Age, yrs (SD) (N = 110) | |||||
| Sex (%) (N = 110) | 57.8 | 47.1 (16.2) | 49.3 (14.3) | 0.01 | 51.7 (15.7) |
| Male | 20 (52.6) | 9 (45.0) | 18 (33.3) | 0.2 | 42.0 |
| Female | 18 (47.3) | 11 (55.0) | 36 (66.7) | 58.0 | |
|
| |||||
| Race (%) (N = 111) | 0.7 | ||||
| White | 16 (43.2) | 8 (40.0) | 29 (53.7) | 53 (47.8) | |
| African american | 19 (51.4) | 11 (55.0) | 21 (38.9) | 51 (46.0) | |
| Hispanic | 2 (5.4) | 0 | 2 (3.7) | 4 (3.6) | |
| Pacific islander | 0 | 1 (5.0) | 1 (1.9) | 2 (1.8) | |
| Other | 0 | 0 | 1 (1.9) | 1 (0.9) | |
|
| |||||
| Education* (%) (N = 111) | |||||
| Did not graduate high school | 5 (13.2) | 1 (5.0) | 6 (11.3) | 0.8 | 12 (10.8) |
| High school graduate | 11 (29.0) | 8 (40.0) | 21 (39.6) | 40 (36.0) | |
| > High school education | 22 (57.9) | 11 (55.0) | 26 (49.1) | 59 (53.2) | |
|
| |||||
| Insurance (%) (N = 111) | |||||
| None | 1 (2.7) | 0 | 0.09 | 1 (0.9) | |
| Medicare | 7 (18.9) | 05 (25.0) | 12 (22.2) | 24 (21.6) | |
| Medicare & private ins. | 14 (37.8) | 9 (45.0) | 19 (35.2) | 42 (37.8) | |
| Medicare & Medicaid | 12 (32.4) | 4 (20.0) | 8 (14.8) | 24 (21.6) | |
| Private ins. only | 2 (5.4) | 2 (10.0) | 15 (27.8) | 19 (17.1) | |
| Other | 1 (2.7) | 0 | 0 | 1 (0.9) | |
|
| |||||
| Social security assistance (%) (N = 109) | 24 (68.6) | 10 (50.0) | 29 (53.7) | 0.3 | 63 (57.8) |
|
| |||||
| Transportation (%) | |||||
| Drive self | 15 (39.5) | 16 (80) | 34 (63.0) | <0.001 | 65 (58.0) |
| Friend/family | 11 (29.0) | 4 (20) | 19 (35.2) | 34 (36.4) | |
| Transport service | 9 (23.7) | 0 | 1 (1.9) | 10 (8.9) | |
| Public transport | 3 (7.9) | 0 | 0 | 3 (2.7) | |
|
| |||||
| Household income (%) (N = 105) | |||||
| ≤$10,000 | 7 (21.9) | 2 (10.0) | 8 (15.1) | 0.8 | 17 (16.2) |
| $10,001–30,000 | 11 (34.4) | 5 (25.0) | 14 (26.4) | 30 (28.6) | |
| $30,001–50,000 | 4 (12.5) | 6 (30.0) | 11 (20.8) | 21 (20.0) | |
| >$50,000 | 4 (12.5) | 4 (20.0) | 11 (20.8) | 19 (18.1) | |
| Do not know | 3 (9.4) | 2 (10.0) | 2 (3.8) | 7 (6.7) | |
| Do not wish to answer | 3 (9.4) | 1 (5.0) | 7 (13.2) | 11 (10.5) | |
|
| |||||
| Number in household (SD) (N = 109) | 1.42 (1.08) | 2.60 (1.98) | 1.60 (1.17) | 0.005 | 1.72 (1.38) |
|
| |||||
| Working before dialysis (%) (N = 103) | 17 (44.7) | 16 (80.0) | 36 (80.0) | 0.001 | 69 (67.0) |
|
| |||||
| Currently employed (%) (N = 111) | 5 (13.2) | 6 (30.0) | 20 (37.7) | 0.03 | 31 (27.9) |
|
| |||||
| Diabetes (%) (N = 109) | 17 (47.2) | 2 (10.0) | 17 (32.1) | 0.01 | 36 (33.0) |
|
| |||||
| Duration of ESRD, median (IQR) † (N = 94) | 2.2 (0.9, 5.5) | 3.0 (1.2, 8.3) | 6.3 (3.4, 10.7) | <0.001 | 4.4 (1.8, 9.2) |
|
| |||||
| Location of ESRD diagnosis (%) (N = 106) | |||||
| Hospital/ER | 17 (43.2) | 5 (25.0) | 14 (28.6) | 0.2 | 35 (33.0) |
| PCP in clinic | 4 (10.8) | 5 (25.0) | 11 (22.5) | 20 (18.9) | |
| Nephrologist in clinic | 14 (37.8) | 10 (50.0) | 24 (49.0) | 48 (45.3) | |
| Don't remember | 3 (8.1) | 0 | 0 | 3 (2.8) | |
|
| |||||
| Prior modality (%) | 9 (23.7) | 12 (60.0) | 46 (85.2) | <0.001 | 67 (59.8) |
Includes those who attended vocational/technical schools, college (whether or not completed) and those with graduate/professional degrees.
Median and inter-quartile range are reported as data were not normally distributed. Kruskal-Wallis test results reported. Results with a p-value < 0.05 are considered to be statistically significant. Casewise deletion was used to account for missing data in tabulating proportions and comparison. Total N provided separately for instances of missing data.
Survey participants were predominantly female (nearly 60%) and ranged in age from 18 to 86 years. On average, the HD group was older than the other two groups, with mean age 57.8 years (compared with 47.1 and 49.3 years for PD and transplant, respectively [p = 0.01]). Transplant patients, as expected, had a longer median time of ESRD diagnosis than either HD or PD patients (6.3 vs. 2.1 and 3.0 years, p < 0.001). Only 10% of PD patients carried a diagnosis of diabetes compared with 32% of transplant patients and 47% of HD patients (p = 0.01). PD and transplant patients were more likely to be employed prior to dialysis (80% in both groups) and currently employed (more than 30% of PD patients and nearly 40% of transplant patients) than HD patients, of whom less than half were employed prior to dialysis (p = 0.001) and less than 15% were currently employed (p = 0.03). Again, in this sampling of patients, as in the focus groups, far fewer HD patients had employed another modality for RRT.
After completing demographics information, patients filled out sections according to their modality (in-center dialysis, PD and kidney transplant). Responses were compared between HD and PD patients (Table 3). These survey responses were missing data in less than 10% of instances except for one question regarding patient's perception of the best form of RRT; six respondents did not answer this question, all receiving HD. Responses to the survey questions particular for each of the three groups separately are summarized in Table 4.
Table 3. Comparison of HD and PD patient survey responses.
| In-Center Hemodialysis (N = 38) | Peritoneal Dialysis (N = 20) | p-Value | |
|---|---|---|---|
|
| |||
| Prior nephrologist care (%) (N = 55) | 23 (65.7) | 15 (75.0) | 0.6 |
|
| |||
| Time under care of nephrologist (%) | |||
| 0–3 months | 1 (4.4) | 1 (6.8) | 0.2 |
| 3–6 months | 0 | 0 | |
| 6–12 months | 1 (4.4) | 1 (6.8) | |
| 1–3 years | 8 (34.8) | 1 (6.8) | |
| >3 years | 13 (56.5) | 12 (80.0) | |
|
| |||
| Discussion of modalities (%) (N = 54) | 26 (76.3) | 18 (94.7) | 0.2 |
| Don't know | 3 (8.6) | 0 | |
|
| |||
| Discussion clear (%) (N = 45) | 23 (88.5) | 17 (100.0) | 0.7 |
| Don't know | 2 (7.7) | 0 | |
|
| |||
| Classes/education (%) (N = 56) | 24 (66.7) | 17 (85.0) | 0.2 |
|
| |||
| Classes/education helpful (%) (N = 40) | 20 (90.9) | 17 (100.0) | 1 |
| Don't know | 1 (4.6) | 0 | |
|
| |||
| Type of education (%) (N = 42) | |||
| Class | 5 (13.2) | 14 (70.0) | <0.001 |
| Video | 15 (39.5) | 15 (75.0) | 0.01 |
| Literature | 20 (52.6) | 16 (80.0) | 0.05 |
| Other | 1 (2.6) | 2 (10.0) | 0.3 |
|
| |||
| Dialysis began emergently (%) (N = 56) | 19 (52.8) | 8 (40.0) | 0.4 |
|
| |||
| Met with other ESRD pts (%) (N = 56) | 5 (13.9) | 5 (25.0) | 0.5 |
| Don't know | 1 (2.8) | 1 (5.0) | |
|
| |||
| Most influential in choice (%) (N = 56) | 0.3 | ||
| Doctor | 19 (53.8) | 9 (45.0) | |
| Nurse | 1 (2.8) | 1 (5.0) | |
| Social worker | 2 (5.6) | 0 | |
| Dialysis unit employee | 0 | 0 | |
| Friend/family on dialysis | 2 (5.6) | 0 | |
| Another patient | 1 (2.8) | 0 | |
| Reading materials | 5 (13.9) | 2 (10.0) | |
| Class | 0 | 3 (15.0) | |
| Other | 6 (16.7) | 5 (25.0) | |
|
| |||
| Best option of RRT (%) (N = 52) | <0.001 | ||
| Hemodialysis (in-center) | 16 (50.0) | 0 | |
| Home hemodialysis | 1 (3.1) | 0 | |
| Peritoneal dialysis | 2 (6.3) | 15 (75.0) | |
| Kidney transplant | 13 (40.6) | 5 (25.0) | |
|
| |||
| On transplant list (%) (N = 56) | 9 (25.0) | 8 (40.0) | 0.4 |
| Don't know | 2 (5.6) | 0 | |
|
| |||
| Time on waitlist, yrs (SD) (N = 12) | 1.42 (1.07) | 2.08 (1.69) | 0.4 |
Results with a p-value < 0.05 are considered to be statistically significant.
Casewise deletion was used to account for missing data in tabulating proportions and comparison. Total N provided separately for instances of missing data.
Table 4. Survey Respondents' Responses to Treatment-Specific Questions.
| In-Center Hemodialysis (N= 38) | N(%) | Peritoneal Dialysis (N= 20) | N(%) | Renal Transplant (N= 54) | N(%) |
|---|---|---|---|---|---|
|
| |||||
| Aware of home therapy options (N = 33) | 24 (73.7) | Able to continue usual lifestyle/working | 19 (95.0) | Dialysis prior to transplantation (N = 53) | 45 (84.9) |
| Don't know | 1 (3.0) | ||||
|
| |||||
| Distance from dialysis unit (N = 35) | Distance from dialysis unit | Type of dialysis before transplantation* | |||
| <20 miles | 32 (91.4) | <20 miles | 9 (45.0) | In-center HD | 28 (62.2) |
| ≥20 miles | 2 (5.7) | ≥20 miles | 11 (55.0) | Peritoneal dialysis | 9 (20.0) |
| Don't know | 1 (2.9) | Don't know | 0 | Peritoneal dialysis and in-center HD | 7 (15.6) |
| Home HD | 1 (2.2) | ||||
|
| |||||
| Home dialysis disruptive to lifestyle (N = 35) | 18 (51.4) | In-center dialysis limiting of lifestyle | 19 (95.0) | Type transplant received (N = 47) | |
| Living related donor | 16 (34.0) | ||||
| Living non-related donor | 6 (12.8) | ||||
| Don't know | 6 (17.1) | Deceased donor | 21 (44.7) | ||
| Don't know | 4 (8.5) | ||||
|
| |||||
| Length of time on transplant list (N = 46) | |||||
| Home less sterile than dialysis center (N = 36) | 16 (44.4) | Home more sterile than dialysis center | 16 (80.0) | < 1 year | 15 (32.6) |
| Don't know | 6 (16.7) | Don't know | 2 (10.0) | >= 1 year | 29 (63.0) |
| Don't know | 2 (4.4) | ||||
|
| |||||
| Prior home therapy (v36) | 8 (22.2) | Prior in-center HD | 13 (65.0) | Mean waiting time (SD) (if not <1 year) (N = 29) | 4.0 (3.1) |
| Don't know | 1 (2.8) | ||||
|
| |||||
| Reason for switch from home therapy | Preferred type of dialysis (N = 39) | ||||
| Change in home situation | 2 (25.0) | Receive better dialysis at home (N = 18) | 17 (94.4) | Home dialysis (peritoneal or home HD) | 4 (10.3) |
| Recurrent infections | 3 (37.5) | In-center HD | 2 (5.1) | ||
| MD felt home therapy inadequate | 2 (25.0) | No preference | 1 (2.6) | ||
| No longer physically able | 1 (25.0) | Not been on both treatments | 32 (82.1) | ||
|
| |||||
| Reasons for choosing against home therapy* (N = 38) | Reasons for choosing home therapy* (N = 20) | Staff engaged in discussion of transplantation* (N = 54) | |||
| Discomfort without supervision | 12 (31.6) | Fear of needles/seeing blood | 3 (15.0) | Physician at dialysis unit | 26 (48.2) |
| Did not wish abdominal catheter | 9 (23.7) | Able to continue working | 10 (50.0) | Nurse | 19 (35.2) |
| Fear of infection/contamination | 13 (34.2) | Better for personal schedule | 17 (85.0) | Social worker | 13 (24.1) |
| Home environment not suitable | 6 (15.8) | No longer able to receive HD | 0 | Primary nephrologist | 37 (68.5) |
| Prior problem/inadequate therapy | 5 (13.2) | Knowing someone w/HD complications | 2 (10.0) | Employee at dialysis unit | 10 (18.5) |
| MD felt in-center dialysis was best | 9 (23.7) | MD felt home therapy was best | 10 (50.0) | Class | 11 (20.4) |
| Other | 10 (26.3) | Other | 5 (25.0) | Friend/family with transplant/on dialysis | 4 (7.4) |
| Reading materials | 18 (33.3) | ||||
| Other | 4 (7.4) | ||||
|
| |||||
| Time first learned about transplant | |||||
| Before starting dialysis | 23 (53.5) | ||||
| After starting dialysis | 15 (34.9) | ||||
| Don't know | 5 (11.6) | ||||
Multiple responses allowed in these categories.
Casewise deletion was used to account for missing data in tabulating proportions. Total N provided separately for instances of missing data.
Experiences at the Time of Diagnosis
Patients in both PD and HD focus groups were mixed in their entry into dialysis; several had knowledge of their disease prior to reaching end stage and others had to start dialysis acutely, even emergently. In-center HD patients reported beginning dialysis acutely more often that PD patients. One respondent stated: “I went to the hospital because I had been sick and at the hospital they told me I had a heart attack which I didn't know I'd had one … I guess they did a couple of studies on my heart and my kidneys quit working.” Another participant explained: “I just got sick at work one day … I didn't know anything. I didn't even know what dialysis was.” Others, with a longer progression, felt more prepared: “I eventually had to go on dialysis…I was sort of prepared, you know … it was not a big shock when I had to go on dialysis.” Another said: “I kept going back to the same doctor and one day he said we've got to put you on dialysis, so that's how I got on.”
Data from the distributed surveys (Table 2) indicated that the diagnosis of kidney disease in the acute hospital setting was relatively common overall (33%) and slightly more common among HD patients (42%). However, a substantial portion of total survey respondents (45.3%) reported that their nephrologist made a diagnosis of ESRD in a non-acute setting. Those using PD were slightly more likely to have been under the care of a nephrologist prior to initiating dialysis (75.0 vs. 65.7%), and a greater proportion of PD patients were followed by their nephrologists for more than 1 year (80.0 vs. 56.5%).
Elements of fear were most commonly expressed when focus group participants spoke about how they felt about their disease when they were first diagnosed. Participant responses included:
“I was afraid but I wanted to live. That's what it comes down to.”
“It scared me to death when I read on a piece of paper one day. I was here and they had on there, end-stage renal disease.”
“I was just scared about whether I was going to die or not.”
Choosing a Modality
Focus group participants were mixed in their perceptions of the ability to choose their treatment modalities. Some felt that they had no choice, and one patient reported that her family member made the decision for her. Others reported that the choice was made by a physician or due to complications of their prior modality (change from PD to HD due to poor Kt/V adequacy, change from HD to PD due to vascular access complications).
In speaking of her experiences with PD, one participant explained:
They came back to me and said I don't know why anybody told you that you couldn't do PD. There is no reason why you couldn't do it. And so then I went and had the PD surgery. But it was … sort of out of my control. That was a decision that they made. I didn't really have an option.
One participant expressed her frustration with the question of choice: “You all ask like we took this by choice. We didn't have any control over this.”
Regarding education received, some focus group participants felt that they had been lied to or misled about the potential emotional and physical toll that dialysis could take and that they were not given adequate information about side effects/emotional effects. A few participants had been diagnosed at a younger age and had a slow progression to kidney failure. They described feelings of denial and invincibility when they thought about the prospect of kidney failure. Other patients felt they had been given sufficient information but were not ready to process it: “I had a lot of information. I just didn't want to face the fact that I was going to go on dialysis.”
Some participants were given reading materials and videos explaining modality options; some participants found this helpful, but some had difficulty understanding the materials. Participant responses included:
“When my doctor sent me down there, they just put me in a room, showed me a film about people on dialysis, even my doctor didn't sit down and talk to me and tell me what was going on.”
“I read and read, and then I say well, maybe this means this, maybe that means that.”
Participants were also sensitive to the attitudes of their dialysis caregivers, and issues of distrust and misinformation influenced how they felt about dialysis staff and the staff's ability to share with them the options for therapy. Participants in several groups felt that they had been deceived by physicians who told them they would feel better, when in reality they had not felt better at all. One participant said:
I think that one of the things we all have felt that I don't think anyone has said, is the problem of people meaning to tell us or give us a misconception of how you are going to feel. I had very high expectations and I don't do that any more. I've just started to sign up for transplant, but I don't have high expectations about that either … I'm not going to set myself up for that again.
Another participant explained:
They said that, you know, you been having problems with your blood pressure for years and you're going to have to go on dialysis. And they said it's going to make you feel much better, you're going to do much better. That was the biggest lie they ever told.
This level of distrust led some patients to question the financial motivations of the dialysis health care staff. Participants in one PD group felt that PD was not mentioned as an option because it was not as profitable as in-center dialysis.
A majority of survey participants in both the HD and PD groups reported having discussions about modality choice, although this approached nearly 95% of PD patients compared to roughly 75% of HD patients. Most patients in both groups reported these discussions to be clear. Unlike focus group respondents, a majority of survey respondents reported some form of pre-dialysis education or class, which they reported to be overall helpful. Survey data showed more PD respondents reporting having a formal class (70 vs. 13.2%, p < 0.001) and having the opportunity to view a video (75 vs. 39.5%, p = 0.01). More than 75% of PD patients also reported having received literature regarding dialysis compared to only half of HD patients. Roughly 50% of participants on HD and PD named their physicians as being the most influential in their choice of therapy.
Perceived Barriers and Facilitators to Alternative Forms of RRT
Focus group participants cited fear as a motivating factor in many of their decisions, particularly in the choice to pursue dialysis and the choice of modality. Both groups reported a fear of blood and needles. For many in the PD group, these fears prompted an avoidance of HD: “When they sat down and they told me well one is your blood, and when I heard the word blood, you know, I was like, I'll take the other one, I didn't even give them a chance to tell me what the other one was.” Another person said: “Seeing your blood coming in and out… it's something that can really scare you.”
For HD groups, fear of infection, illness and isolation at home were all motivating factors for the choice of in-center dialysis, and in many situations it was the participant's own experience as a former PD patient or from hearing about bad cases of peritonitis from other dialysis patients. Three out of four HD groups had members who had previously been on PD and had bad experiences with that modality. Participants were hospitalized and often felt near death. These participants also felt that PD was more detrimental to the body and would erase any residual kidney function. Statements included:
“I didn't want to do it at home because I knew someone that had done it at home and I knew that they did catch a lot of infections and all. Most people I do know, they did catch a lot of infections at home doing it. So I said no, I don't want the risk.”
“Eventually the infections just took over her body. And I guess that's what frightened me most of all was the infections.”
“I have heard of too many people who have been on it [PD] and almost died. I will not do it.”
“I would rather have an infection in here than peritonitis. That stuff like to have killed me. It felt like I was dying.”
Members of both HD and PD groups mentioned time constraints as a reason why PD was less desirable:
“With the time like Tuesdays and Thursdays that I don't have to come here, that's great. But see, if I was doing it at home, I have to do it those days too. So that's what bothered me about it.”
“That's all you do is dialyze all day long.”
Participants who had heard about home HD in both the PD and HD groups did not find it appealing due to needing a helper, changes to their home water system, needing a room big enough for the machine and supplies and fear of “bottoming out” (dialysis-related complications) at home.
Regarding transplant, a little more than half of the focus group participants reported being on the waiting list; some patients were not sure whether they were listed and some were unable to be listed due to other medical conditions. Patients demonstrated frustration with many aspects of the transplant process including costs of medication, transportation to hospital, length of time on the waiting list and the evaluation process. Participant responses included:
“That's what it is, waiting. I may never get there, but I'm waiting.”
“I've just started to sign up and get ready for transplant, but I don't have any high expectations about that.”
“Do they realize how many people can't get there? Because if they called me today, I know good and well I can't get there. So it's just a waste of my time.”
Some patients reported having had family and friends engage in the organ donation process, although several reported potential donors being turned down. All felt that awareness in the general public of the need for organ donation was poor.
Among survey respondents, HD patients (Table 3) most commonly reported discomfort with no supervision, fear of infection and contamination and abdominal catheters as reasons for choosing HD over PD. Approximately 25% of patients reported that their physicians told them that HD was the best choice of therapy for them. Other reasons reported for choice against home dialysis included complications from prior PD, including peritonitis with subsequent peritoneal scarring and catheter complications, small children in the home, lack of dependability on home health providers and simply not being presented the option.
Among PD survey respondents (Table 4), the most common reasons for choosing PD were the ability to continue working and more suitability to their individual schedules. Some other reasons for choice of PD included less strict dietary restrictions, fewer infections while on PD and poor veins for HD access. One participant had been an HD nurse in the past and chose PD based on her experiences.
In contrast to the HD patients, half of PD patients reported that their physicians felt PD was a better modality for them. Of note, nearly all PD patients reported that they felt HD would be disruptive to their lifestyles. In contrast, only half of HD patients thought home therapy would be disruptive. Patients in the PD groups also tended to live farther away from their coordinating dialysis units, with nearly 55% traveling more than 20 miles. Less than 6% of in-center HD patients reported living more than 20 miles away (p = 0.002).
Advice to New Patients/Health Care Professionals
Although not a direct objective of the study, focus group participants were eager to discuss and suggest ways to improve education for patients approaching ESRD. Several participants described how helpful peer mentors had been in helping them cope with their own disease, or how they had mentored a patient in distress: “[The mentoree] called me a lot and she was very scared about it and all, so we talked a lot about it. And she's fine now. I think it helps knowing somebody that's on dialysis that you can talk to about it.” One participant speaking to another, stated: “You were the one talked me into going on PD. She said, ‘There's someone I want you to talk to.’ You happened to be in the center one day when I was on the other side.”
A recurring suggestion from participants was for patients to be involved in their own care and not be too dependent on the health care team. For some, this seemed driven by a lack of trust in the health care team, but for others it was motivated by a feeling that self-education would increase a patient's quality of life. Several participants felt that educating patients with kidney disease was not enough. They identified many public misconceptions of dialysis and particularly called for more education regarding transplantation. One participant stated: “‘Oh my goodness, you are getting ready to die.’ That's the biggest misconception right there.” Another said: “The general public knows nothing about [dialysis]. I think it ought to be on TV and explained somehow that there are different kinds of dialysis. And we need kidneys donated.”
Many participants asked for more education on the mechanics of how a dialysis machine works and how to read the numbers on the machine: “I could look on my machine and see sodium on there but I didn't know what I was looking at because nobody had never told me.”
Patients also mentioned that they wished they could have attended pre-dialysis educational sessions. One participant had taken the transplant class and another was signed up, but none of the participants mentioned a class about dialysis options. Participants in several groups felt that classes would have been a good idea, even in the hospital setting, and wished they had had the opportunity: “You're going to be overwhelmed. But you would have a chance to ask somebody that you could actually ask questions to.” Another said: “You know they got a certain number of people got to go on dialysis at the hospital. Why not take me into a conference room and sit down, show me some pictures, have someone come and explain what's going on?”
Discussion and Recommendations for Future Research
In our analysis, we were able to identify several factors that seemed to influence patients' decisions in choice of RRT modality. Focus group results from this study demonstrated that, regardless of modality, fear was a guiding factor both at the time of RRT initiation and when choosing a modality. Distrust of the medical system, denial and patient experiences with previous modalities were also seen as barriers to care. Participants also reported the particular merits of their chosen modality, including impact upon schedule and perceptions of sterility and quality of dialysis.
Regarding fear as a driving factor, beyond the overwhelming fear reported at time of ESRD diagnosis, focus group participants across all groups consistently mentioned fear of side effects and undesirable characteristics of opposing modalities, including visibility of blood with HD and lack of supervision with home therapies. Survey respondents reflected these same worries in their answers for why they chose one modality over the other.
The relationship between the patient and the dialysis health care team was brought up frequently in the HD focus groups. Patients had varying degrees of trust in their health care providers (physicians, nurses, dialysis technicians and social workers). Several reported feeling like they were experimental subjects and patients often questioned the motivations of both physicians and the other dialysis staff, expressing concern that the staff simply thought of their jobs as a source of money and had no concern for the patients. Respondents also felt like physicians made decisions regarding dialysis based on what would produce the most revenue. While the relationship between patients and their dialysis providers may not have a direct correlation with modality choice, it seems important to explore in future research.
Choice was also heavily influenced by the perceived impact on lifestyle and schedule. Those who chose in-center HD preferred the well-defined schedule of thrice-weekly dialysis and saw it as far more preferable than performing dialysis on a daily basis. Home dialysis participants in both the survey and focus group cohorts preferred the autonomy offered by home therapy, and this autonomy was overwhelmingly the most commonly reported reason for choosing home therapy in the survey participants.
With regard to education, an encouraging finding among survey and focus group participants was the majority had received some form of pre-dialysis education, including classes, literature and instructional videos. Both groups in survey data reported high rates of satisfaction with their education, unlike the study performed by Rubin et al. (2004), which demonstrated a greater satisfaction in domain of information provided among PD patients. However, a major distinction between the HD and PD groups in our study was the comprehensiveness of pre-dialysis education, which may correlate with Rubin et al.'s (2004) findings. As noted among survey participants, those receiving PD reported several more forms of education, which suggests that they received more formalized and possibly more detailed education. Although not statistically significant, perhaps the longer duration of pre-dialysis care under a nephrologist for home therapy participants may have contributed to the choice of PD. Alternatively, a more formalized education structure could be explained by the choice of PD and training necessary for home therapy. Regardless, one might infer that more comprehensive education programs could help patients in selecting home therapy.
Study limitations include a lack of generalizability due to the qualitative nature of the focus groups and small sample sizes. Although we had an overall response rate of 57%, response rates for PD and HD patients were low. Focus groups may have been biased to represent extremes of patient satisfaction—patients who are most and least satisfied with their therapy may be more likely to volunteer to express their opinions. Survey participants were overrepresented by transplant patients, as many of these patients were likely to complete and return their surveys while waiting for appointments.
Because many participants in both survey and focus group portions of the study were diagnosed in the hospital in an acute situation, or were diagnosed many years earlier, recall bias is highly likely and may alter our understanding of barriers to choice at initial diagnosis and further studies should focus on research and intervention at early and acute stages of kidney failure.
Our findings, although exploratory, can help guide further studies both of determinants of patient choice as well as interventions to assist in making choices and promoting home therapies. Despite a lack of statistical significance in this study, age, race and educational status may play a role in selection of modality and deserve evaluation in future research. Patients being treated with both home and in-center therapies expressed that while they often received education, many still harbored fears of treatment modalities and distrust of health care staff in delivering those modalities. Interventions guided to address specific patient fears of home therapies (peritonitis, isolation) and improving the patient–physician relationship could be targets to overcome perceived barriers. A broader educational approach that can occur even in the acute hospital setting may be another avenue to improve a patient's ability to choose and deserves further exploration.
Appendix A: Focus Group Questions and Probes
Issue A: Dealing With Disease Onset and RRT Modalities
1. What kind of information did you get about dialysis and transplant from your health care workers?
Probe
How were the different types of therapies presented to you, or were they presented to you at all? Who told you about them?
Is there anything you wish they had done or said differently?
Do you feel that your doctors/other health care workers gave you enough information to make a decision? Why or why not?
2. Think back to the time when you first found out that you were reaching end-stage kidney disease. What emotions were you going through at the time?
Probe
Who told you that you were reaching end-stage kidney disease? How did they tell you?
What did you think about dialysis before you knew you had kidney disease?
Issue B: Choosing a Modality
1. What made you decide to choose in-center hemodialysis (or PD/home HD, depending on focus group)?
Probe
What made you decide NOT to choose an alternative treatment method?
Did you feel like you were ready to make a choice?
Were there other sources you used for information in making a decision, like friends, family members or the Internet?
2. What information do you think is most important for people to have when they are trying to figure out the treatment that is right for them?
Probe
Looking back, what information could have been really useful to you that you did not get?
What would you tell someone who is approaching kidney failure and trying to decide what to next?
Contributor Information
Caroline Jennette, UNC Kidney Center, Chapel Hill, NC.
Vimal Derebail, UNC Kidney Center, Chapel Hill, NC.
Judy Baldwin, Carolina Dialysis – Carrboro, Carrboro, NC.
Sandra Cameron, Carolina Dialysis – Sanford, Sanford, NC.
References
- Arkouche W, Traeger J, Delawari E, Sibai-Galland R, Abdullah E, Galland R, et al. Twenty-five years experience with out-center hemodialysis. International Society of Nephrology. 1999;56:2269–2275. doi: 10.1046/j.1523-1755.1999.00771.x. [DOI] [PubMed] [Google Scholar]
- Bass EB, Jenckes MW, Fink NE, Cagney KA, Wu AW, Sadler JH, et al. Use of focus groups to identify concerns about dialysis. Medical Decision Making. 1999;19:287–295. doi: 10.1177/0272989X9901900307. [DOI] [PubMed] [Google Scholar]
- Bernardini J. Peritoneal dialysis: Myths, barriers, and achieving optimum outcomes. Nephrology Nursing Journal. 2004;31(5):494–498. [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine; 1967. [Google Scholar]
- Goovarts T, Jadoul M, Goffin E. Influence of a Pre-dialysis Education Programme (PDEP) on the mode of renal replacement therapy. Nephrology Dialysis Transplantation. 2005;20:1842–1847. doi: 10.1093/ndt/gfh905. [DOI] [PubMed] [Google Scholar]
- Greene JC, Caracelli VJ, Graham WF. Toward a conceptual framework for mixed-method evaluation designs. Educational Evaluation and Policy Analysis. 1989;11(3):255–274. [Google Scholar]
- Iacono SA. Predialysis anxiety: What are the concerns of patients? Journal of Nephrology Social Work. 2005;24:21–24. [Google Scholar]
- Johnson RB, Onwuegbuzie AJ. Mixed methods research: A research paradigm whose time has come. Educational Researcher. 2004;33(7):14–26. [Google Scholar]
- Klang B, Bjorvell H, Clyne N. Predialysis education helps patients choose dialysis modality and increases disease-specific knowledge. Journal of Advanced Nursing. 1999;29(4):869–876. doi: 10.1046/j.1365-2648.1999.00957.x. [DOI] [PubMed] [Google Scholar]
- Landraneau KJ, Ward-Smith P. Patients' perceptions concerning choice among renal replacement therapies: A pilot study. Nephrology Nursing Journal. 2006;33(4):397–402. [PubMed] [Google Scholar]
- McLaughlin K, Manns B, Mortis G, Hons R, Taub K. Why patients with ESRD do not select self-care dialysis as a treatment option. American Journal of Kidney Diseases. 2003;41(2):380–385. doi: 10.1053/ajkd.2003.50047. [DOI] [PubMed] [Google Scholar]
- Mehrotra R, Marsh D, Vonesh E, Peters V, Nissenson A. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. International Society of Nephrology. 2005;68:378–390. doi: 10.1111/j.1523-1755.2005.00453.x. [DOI] [PubMed] [Google Scholar]
- Medical Education Institute. Home Treatments Compared. 2006 Retrieved November, 2006, from www.homedialysis.org.
- Muhr T. User's manual for ATLAS.ti 5.0. Berlin, Germany: ATLAS.ti Scientific Software Development; 2005. [Google Scholar]
- Rubin HR, Fink NE, Plantiga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal vs. hemodialysis. Journal of the American Medical Association. 2004;291(16):697–703. doi: 10.1001/jama.291.6.697. [DOI] [PubMed] [Google Scholar]
- Shih YT, Guo A, Just PM, Mujais S. Impact of initial dialysis modality and modality switches on Medicare expenditures of end-stage renal disease patients. Kidney International. 2005;68:319–329. doi: 10.1111/j.1523-1755.2005.00413.x. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Tashakkori A, Teddle C, editors. Handbook of Mixed Methods in Social & Behavioral Research. California: SAGE Publications, Inc; 2002. [Google Scholar]
- Tweed AE, Ceasar K. Renal replacement therapy choices for pre-dialysis patients. British Journal of Nursing. 2005;14(12):659–664. doi: 10.12968/bjon.2005.14.12.18287. [DOI] [PubMed] [Google Scholar]
- United States Renal Data System. USRDS 2008 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2008. [Google Scholar]
- Winklemayer W, Glynn RJ, Levin R, Owen W, Avorn J. Late referral and modality choice in end-stage renal disease. Kidney International. 2001;60:1547–1554. doi: 10.1046/j.1523-1755.2001.00958.x. [DOI] [PubMed] [Google Scholar]
- Wuerth DB, Finkelstein SH, Schwetz O, Carey H, Kliger AS, Finkelstein FO. Patients' descriptions of specific factors leading to modality selection of chronic peritoneal dialysis or hemodialysis. Peritoneal Dialysis International. 2002;22:184–190. [PubMed] [Google Scholar]
- Wu AW, Fink NE, Cagney KA, Bass EB, Rubin HR, Meyer KB, et al. Developing a health-related quality-of-life measure for end-stage renal disease: The CHOICE health experience questionnaire. American Journal of Kidney Diseases. 2001;37(1):11–21. doi: 10.1053/ajkd.2001.20631. [DOI] [PubMed] [Google Scholar]