Abstract
Objectives
To determine whether sharing laboratory charge and personal utilization information with physicians can reduce laboratory test orders and expenditures, thereby decreasing the overutilization of laboratory testing.
Methods
This was a prospective study. By querying our electronic medical records, we calculated the median laboratory charges per patient/per day (PP/PD) and median laboratory tests ordered PP/PD for the resident general internal medicine and hospitalist services. For 10 weeks, we shared this team-based information with physicians with weekly updates. We calculated total laboratory charges for the 10 most common discharge diagnoses to capture laboratory charges for entire episodes of care.
Results
During the intervention, the mean number of laboratory tests ordered PP/PD by resident service decreased from 5.56 to 5.17 (−0.389, P <0.001); the mean charge PP/PD decreased from $488 to $461 (−$27, P < 0.001). The hospitalist service decreased the number of laboratory tests ordered PP/PD from 3.54 to 3.36 (−0.18, P = 0.77) and the mean charge PP/PD decreased from $331 to $301 (−$30, P = 0.96). The statistically significant decline in laboratory charges persisted after controlling for the 10 most common discharge diagnoses. Compared with the 3-month period before the study began, physicians in the 10-week intervention period ordered 1464 fewer laboratory tests, resulting in a $188,000 reduction in charges and a 3% to 4% reduction in utilization.
Conclusions
Informing physicians of the charges for laboratory tests and their personal utilization patterns can reduce the number of laboratory tests ordered and laboratory expenditures, especially for physicians in training.
Keywords: cost analysis, decision making, healthcare costs, physician decision support, laboratory utilization
Healthcare costs in the United States are increasing at an alarming rate, threatening both the ability of the health-care system to adequately provide care for the population and the nation’s fiscal solvency. From 2002 to 2009, hospital expenditures increased an average of 5.2%/year.1 Although charges for physician professional fees increased 5.1% from 2003 through 2006, charges for laboratory testing increased at a faster rate of 14.2% during that same period.2 Similarly, from 2000 to 2010, the number of diagnostic laboratory tests ordered for Medicare patients increased by 89%, but the volume of major surgeries, office visits, and nursing facility care increased only 35% for the same population.3 The value of these increasing diagnostic expenditures is unclear because considerable geographic variation in practice patterns signals that overutilization is likely occurring.4-6 In addition, some evidence suggests laboratory utilization does not affect clinical outcomes.7,8 For hypertension control, James et al demonstrated that laboratory utilization decreased and patient outcomes were unchanged in the capitation model versus a fee-for-service model.9 In routine presurgical assessments, 93% of tests are not indicated and numerous professional groups recommend against routine testing.10-13 Even many physicians acknowledge that some routine preoperative tests are unnecessary but perform them nevertheless, citing practice tradition, medicolegal worries, concerns about delays, lack of awareness of the evidence base, and patient insistence.14,15 Because physicians’ decisions drive 80% of healthcare costs,16 providers play a leading role in curtailing overutilization. Fortunately, 99% of primary care physicians endorse the need for cost containment, and 96% believe that physicians play a role in controlling costs.17 Unfortunately, physicians often believe themselves to be unprepared for this task. Cost containment and cost-effectiveness have not been a traditional part of residency training,18 and physicians are frequently unaware of the costs of tests they order.19 Furthermore, the real pressures of patient expectations and defensive medicine encourage test ordering.20,21 The opposite pressures to reduce laboratory costs are not generally felt nor are they routinely tracked on an individual physician basis. If physicians were armed with details of their own spending patterns, however, they could feel empowered to decrease spending because they could point toward measurable differences and reduced costs, counteracting the pressures that encourage ordering. Moreover, providing utilization and spending data could encourage a regression to the mean because physicians who order disproportionately more tests would be confronted with their outlier status.
It is not known whether confronting physicians with the “financial harms” of their spending habits in combination with social pressure would curtail their use of laboratory tests to conform to a new norm. To address this question, we conducted a prospective study of resident and hospitalist physicians.
Methods
Study Setting and Participants
Inspired by the Choosing Wisely campaign,22 our study was conceived, initiated, and directed by residents with support of the Section on General Internal Medicine faculty. We conducted the study at a large academic medical center, and our institutional review board approved the study protocol. All internal medicine residents and all hospitalists on general medicine services who cared for approximately 120 patients daily were included in this study.
Each of the 3 resident teaching teams was structured with 1 faculty member from either general internal medicine or infectious diseases, 1 senior internal medicine resident, and 2 interns caring for up to 16 patients per team. Each member of the team was capable of ordering or discontinuing laboratory tests independent of other team members, but the majority of orders were placed by interns. By contrast, hospitalists worked as individual providers, with approximately 70 patients distributed equally among colleagues. When hospitalists supervised a resident teaching team, they were counted as part of the academic service tally. The structure of all teams remained constant during the entire study period, but individual team members changed monthly (resident teams) or weekly (hospitalist teams). Resident team members changed every 4 weeks having 2 days overlap with new resident teams transferring from subspecialty services, outpatient rotations, or possibly other general medicine teaching teams as per the usual rotation schedule. Most residents were exposed to our study intervention for only 4 weeks, but a minority was exposed for 8 weeks. Hospitalists worked 7 days on, 7 days off, with new hospitalists transferring from a previous hospitalist general medicine service, general medicine teaching service, and subspecialty service as per their usual schedule; the majority were exposed to our study for several weeks.
Intervention
From October 2013 through December 2013, we posted in the physician workrooms two items: the charges for the most commonly ordered laboratory tests (Fig. 1) and each team’s mean laboratory tests ordered per patient/per day (PP/PD) and mean laboratory charges PP/PD for the prior week with the previous weeks’ values for comparison. In addition, we presented these same two pieces of information at resident educational conferences (which occurred four times per week). Sunday through Saturday constituted the week, and updates were presented and posted every Tuesday of the study period. Hospitalists were invited to the morning report, served as attending physicians on resident teaching teams, and worked in the same physician workrooms where data were posted. No formal education regarding appropriateness, indications, or high-value care was given.
Fig. 1.
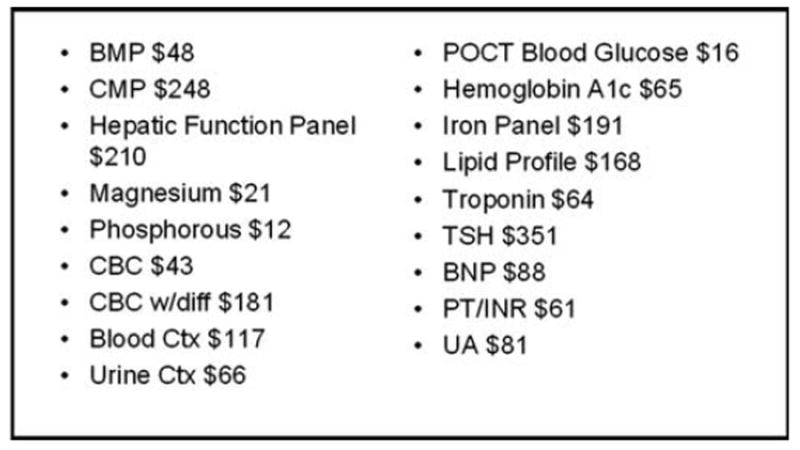
Laboratory charge information for the 18 most commonly ordered laboratory tests displayed to providers at educational conferences and posted in physician workrooms. BMP, basic metabolic panel; BNP, brain natriuretic peptide; CMP, comprehensive metabolic panel; CBC, complete blood count; CBC w/diff, CBC with differential; Ctx, culture; INR, international normalized ratio; POCT, point of care; PT, prothrombin time; TSH, thyroid-stimulating hormone; UA, urinalysis.
Data Measurement
We queried the electronic medical records (EMRs) to obtain the number of laboratory tests ordered for all inpatient resident general medicine and hospitalist services in our study. Laboratory tests ordered as prespecified “panels” (eg, a basic metabolic panel [BMP]) were counted as one laboratory test each. Laboratory tests obtained from emergency department and intensive care unit stays were excluded. Charges for each laboratory test were obtained from the finance department based on the current year’s master charge sheet in effect as of October 2013. The actual cost of each test within our institution was deemed too difficult to calculate given variations in material and manpower involved and therefore charges were measured as a correlator.
Outcome Measures
Our primary outcomes of interest were the number of laboratory tests ordered PP/PD and the laboratory charges PP/PD in the intervention period compared with the 3-month control period before the intervention. Secondary outcomes included the mean charge per laboratory test to determine whether physicians were selectively choosing less expensive tests and specific laboratory tests ordered to assess any change. We also tracked the total laboratory charges per total episode of care for the 10 most common discharge diagnosis-related groups (DRGs) during our study period.
Statistical Analysis
For each patient, we calculated the total laboratory charge per day, the number of tests per day, and the mean charge per laboratory test. We summarized these variables both by time period (intervention vs baseline control) and by provider specialty (resident teaching service vs hospitalists). Because the distribution of the charges was skewed to the right, we log transformed the charges for the regression modeling. To determine whether there were significant changes in the total laboratory test charges per patient, the number of tests per patient and the mean charge per laboratory test after the intervention was implemented, we used linear mixed models with random intercepts. These models account for the correlation within each provider’s multiple measurements over time. Models were created and stratified by the type of provider and the 10 most common DRGs. Lastly, to determine whether the changes in the charges were affected by DRGs, we added a model that adjusted for the top 10 DRGs. All of the analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC), and a P value of <0.05 was considered to denote significance for all of the outcomes.
Results
During the 3-month control period before the intervention was implemented, resident services ordered a mean of 5.56 laboratory tests PP/PD generating laboratory charges of $488 PP/PD. Hospitalists ordered a mean of 3.54 tests PP/PD, generating charges of $332 PP/PD. No significant changes over time (increases or decreases) in charges or laboratory tests ordered were seen for either number of tests ordered or charges (P = 0.85 and P = 0.58, respectively) during the control period.
During the intervention period, the mean number of laboratory tests ordered PP/PD by resident service decreased by −0.39 (P < 0.001) and the mean charge PP/PD decreased −$27 (P < 0.001; Figs. 2 and 3). On the hospitalist service, we observed no significant change in the laboratory tests ordered PP/PD (−0.18, P = 0.77) or the mean charge PP/PD (−$30, P = 0.96). For hospitalists the mean charge per laboratory test decreased slightly, from $91.84 to $88.53 (−$3.31, P = 0.0007) but did not change for the resident teaching services ($1.70, P = 0.95).
Fig. 2.
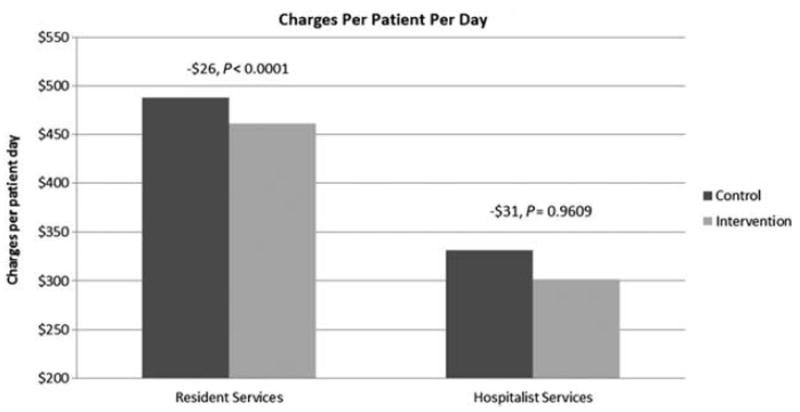
Charges per patient per day on all services during control and intervention.
Fig. 3.
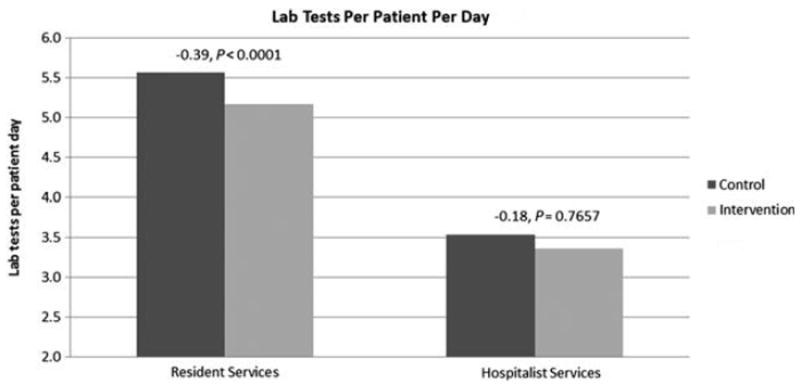
Tests per patient per day on all services during control and intervention.
The Table shows the 10 most commonly ordered laboratory tests during the study period. During the intervention period, resident physicians ordered relatively fewer complete blood counts (CBCs) with differentials in favor of the less expensive CBC without differentials, and fewer comprehensive metabolic panels (CMPs) in favor of the less expensive BMPs.
Table.
Specific laboratory tests ordered
| Specific laboratory tests ordered ($) | Laboratory tests/patient/day
|
||
|---|---|---|---|
| Baseline | Pilot | P | |
| General medicine | |||
| CBC ($43) | 0.885 | 0.960 | 0.001 |
| CBC w-diff ($181) | 0.511 | 0.312 | <0.0001 |
| BMP ($48) | 0.983 | 1.012 | 0.971 |
| CMP ($248) | 0.423 | 0.272 | <0.0001 |
| POCT glucose ($16) | 0.688 | 0.673 | 0.424 |
| Magnesium ($21) | 0.857 | 0.750 | <0.0001 |
| Phosphorous ($12) | 0.687 | 0.629 | 0.003 |
| Blood culture ($117) | 0.120 | 0.120 | 0.921 |
| Hemglobin A1c ($65) | 0.031 | 0.029 | 0.663 |
| Hepatic function ($210) | 0.024 | 0.025 | 0.676 |
| Ratio CBC w-diff/CBC+CBC w-diff | 36.614 | 24.536 | <0.0001 |
| Ratio CMP/BMP+CMP | 30.079 | 21.157 | <0.0001 |
| Hospitalists | |||
| CBC ($43) | 0.679 | 0.607 | <0.0001 |
| CBC w-diff ($181) | 0.486 | 0.393 | <0.0001 |
| BMP ($48) | 0.817 | 0.721 | <0.0001 |
| CMP ($248) | 0.390 | 0.301 | <0.0001 |
| POCT glucose ($16) | 0.622 | 0.540 | <0.0001 |
| Magnesium ($21) | 0.524 | 0.478 | 0.001 |
| Phosphorous ($12) | 0.360 | 0.291 | <0.0001 |
| Blood culture ($117) | 0.120 | 0.105 | 0.019 |
| Hemoglobin A1c ($65) | 0.026 | 0.028 | 0.504 |
| Hepatic function ($210) | 0.020 | 0.015 | 0.063 |
| Ratio CBC w-diff/CBC+CBC w-diff | 41.709 | 39.308 | 0.044 |
| Ratio CMP/BMP+CMP | 32.310 | 29.419 | 0.005 |
BMP, basic metabolic panel; CBC, complete blood count; CMP, comprehensive metabolic panel; POCT, point-of-care testing; w-diff, with differential.
To control for possible changes in case mix affecting our results, we examined the mean laboratory charges for the 10 most common DRGs during the study period. After adjusting for these DRGs, the overall decreases in the number of laboratory tests ordered PP/PD and laboratory charges PP/PD remained statistically significant (P < 0.001 and P < 0.01, respectively).
Compared with the 3-month baseline control period, during the 10-week intervention period, physicians ordered 1464 fewer laboratory tests, resulting in $188,000 fewer charges. Overall, this represents a 3% to 4% reduction in charges. In the resident teams, which experienced the greatest decline, the reduction in utilization was 4% to 5%.
Discussion
Educating physicians at an academic medical center about how many laboratory tests they ordered and tests’ related charges, significantly decreased the number of tests ordered among internal medicine residents but not among hospitalist physicians. During the 10-week study period, resident services decreased charges PP/PD by $27 on the internal medicine resident services, but this did not change among hospitalists. The degree of change may have been more marked in the resident groups because of team-based decision making, pressure toward the norm, and greater exposure to the intervention at educational conferences. Although both hospitalists and internal medicine residents saw the charge information posted in physician workrooms, the hospitalists did not routinely attend the resident educational conferences at which the information also was shared, limiting their exposure. In addition, hospitalists may have felt less peer pressure because they were tracked as a group and their individual performance was not recorded. Interventions that target an entire health system may yield greater results. Feldman et al embedded the cost of laboratory tests in a hospital’s electronic health record, ensuring that all healthcare providers saw the cost of a laboratory test at the time it was ordered.23 Their study documented a greater reduction in laboratory utilization than we observed, likely because of the most consistent nature of the exposure (every time someone ordered a laboratory test) and the equal nature of exposure (every ordering provider exposed when they ordered a test).
During this study, physicians ordered fewer tests, which we hypothesize reduced overutilization; residents reduced their laboratory ordering by 0.39 laboratory test PP/PD, which is consistent with the previous literature.24-29 We also hypothesized that the tests physicians ordered were less expensive, as reflected in a decrease of $3.31 mean charge per laboratory test PP/PD for the hospitalist service. This result may not have occurred in the resident services because of an overall decrease in laboratory test ordering. For example, if during the control period a typical patient had a CMP ($248) and then two subsequent BMPs ($48 each) drawn over a hospitalization, the mean charge would be lower than for a patient who had only one CMP and one BMP drawn. This was also reflected in the specific laboratory tests ordered, because we observed physicians ordering fewer expensive laboratory panels in favor of more targeted testing. Although the number of both CBCs and BMPs ordered actually increased on the resident team during our study, the much larger decrease in the more expensive CBC with differential and CMPs more than offset this increase. This is consistent with findings of Feldman et al, who showed that when confronted with the costs, providers choose a BMP over a CMP, although they did not see a trend for CBC with differential versus no differential.23
A reasonable concern is that laboratory test ordering may simply have been delayed and the length of stay prolonged; therefore, artificially decreasing the charges PP/PD and laboratory tests PP/PD by increasing the denominator. Total laboratory charges for entire episodes of care decreased for most diagnoses, and the decreases were statistically significant for respiratory failure, however.
Our hypothesis is that with the ability to see changes in a rolling weekly format, provider teams and individuals felt empowered and obligated to drive change. Social cognitive theory states that individuals are compelled to conform to their peers. In the context of this study, having the information increased the knowledge needed to perform differently, also known as behavioral capability, and updating team-based charge totals weekly set expectations.24 Furthermore, giving physicians cost information allows them to more effectively select the highest yield test at the lowest cost and avoid low-yield tests. Teams were tracked in parallel; therefore, personal and peer pressure may have been exerted on outliers to decrease their ordering habits. Because all providers on the team were capable of ordering and discontinuing laboratory tests, decisions regarding laboratory testing were most likely made through both shared team decision making and individual decisions. After the study was complete, one of the authors (B.T.) learned that residents had spontaneously enacted a variety of methods to support appropriate laboratory utilization, including resident-organized primary literature and guideline reviews of testing indications, ad hoc team discussions, and individual efforts by senior residents and attending physicians to personally discontinue unnecessary laboratory tests before phlebotomy rounds. These new discussions regarding the appropriateness of laboratory tests likely led to more appropriate laboratory test ordering as interns received guidance from peers and senior team leaders. As such, it was likely a combination of the previously unknown knowledge of laboratory costs and spending habits in combination with peer pressure that led to the changes in our study. Hawthorne effect (observer effect) also may have contributed.
Significant efforts have been made in a variety of scenarios to decrease overutilization. Successful “top down” approaches have included structuring Computerized Physician Order Entry to prohibit recurrent laboratory tests and hospital-wide committees to enforce education in best practices.25,26 Other initiatives that empowered providers, such as displaying reimbursement data in the EMR and providing department-specific spending trends at educational conferences, have shown efficacy as well.27
Our study demonstrates that a house officer–led “bottom up” approach of giving individual teams their utilization data and laboratory charge information can lead to change. This strategy has been described before by Han et al and others, but often in conjunction with monetary or other incentives and targeting a specific set of laboratory tests instead of all laboratory testing.28,29 Furthermore, our efforts required no formal education and no intensive efforts to gather the data because they were already being collected as part of routine care, which is unique compared with many studies. As such, this model should be relatively easy to implement elsewhere. This intervention was led by residents, highlighting the important role that physicians-in-training can play in cost containment and is supported by other resident-led studies.28 Spending patterns during physician training correlate with spending habits during practice,30 so a program such as ours is an ideal framework from which to create lifelong habits of more appropriate test ordering.
Our study has limitations. We conducted the study on the general internal medicine inpatient services at a single large academic medical center, which may limit its generalizability to smaller hospital settings or subspecialty care services. We used a historical control group, and seasonal variations may have affected our data; however, we observed no prior trend in laboratory use or charges during the control period, suggesting that seasonal variation or a maturation effect of residents was unlikely. Similarly, our analysis of laboratory utilization for the most common discharge diagnoses would be unaffected by seasonal variations in case mix. Although the resident teaching services did show statistically significant improvement in the study period, they continued to maintain a higher baseline of utilization. This may be because residents are still learning and order tests out of an abundance of caution or inexperience or are ordering tests to further delineate a diagnosis that would not necessarily be needed as inpatient; it is likely a combination of the these and other factors. This higher starting point gave the residents more room for improvement, which may have biased the results. Lastly, we did not track comorbidities, which may affect the number of laboratory tests ordered; however, our large sample size makes it unlikely that comorbidities were unevenly distributed.
The total number of laboratory tests averted during the 10-week study period was approximately 1400 and represents less patient discomfort, less physician time spent ordering or analyzing unnecessary data, and actual financial savings. Which party actually accrues that savings depends on the payment structure. Most insurers pay a lump sum per DRG; therefore, any cost savings would benefit the hospital and any patients who pay co-insurance. Some insurers and those without insurance are billed using a fee-for-service model. In such cases, fewer laboratory tests would mean savings for both patients and insurers. Six months after we presented our results to the chief medical officer and the chair of internal medicine at our institution, laboratory charges were placed within the EMR as part of the basic order itself for the 50 most common laboratory tests ordered at our institution. The sustainability of these changes is unknown at this time.
Conclusions
We recommend making laboratory charge data easily available to providers through the EMR or paper or electronic distribution and by empowering providers with their individually or team-based utilization data. Given rising healthcare costs and known overutilization of diagnostic testing within internal medicine, methods are needed to reduce healthcare waste in a provider-driven way. This intervention shows that increased provider a wareness and accountability of laboratory test ordering habits can reduce the number of tests ordered and reduce costs.
Key Points.
Overutilization is a key contributor to the unsustainable increases to the cost of medical care.
Physicians are directly in control of these expenditures, but they lack knowledge about costs and their own spending habits.
By making laboratory cost data and physician spending habits directly available to physicians in a timely, updated manner, physicians can be compelled to decrease unnecessary utilization, therby decreasing costs.
Acknowledgments
N.F.F. has received compensation via the Wake Forest University School of Medicine Data Analysis Unit for participation in data monitoring boards, statistical analysis, and endpoint committees.
Footnotes
To purchase a single copy of this article, visit sma.org/southern-medical-journal.
The remaining authors have no financial relationships to disclose and no conflicts of interest to report.
References
- 1.Centers for Medicare & Medicaid Services. [June 6, 2014];National Health Expenditure Fact Sheet. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet.html. Published May 2014.
- 2.Duszak R. Medical imaging: is the growth boom over? [June 6, 2014]; http://www.acr.org/~/media/ACR/Documents/PDF/Research/Brief%2001/PolicyBriefHPI092012.pdf. Published October 2012.
- 3.Doherty B. Facts challenge physicians’ views on Medicare spending. [June 1, 2014]; http://advocacyblog.acponline.org/2012/07/facts-challenge-physicians-views-on.html. Published July 2012.
- 4.Ashton CM, Petersen NJ, Souchek J, et al. Geographic variations in utilization rates in Veterans Affairs hospitals and clinics. N Engl J Med. 1999;340:32–39. doi: 10.1056/NEJM199901073400106. [DOI] [PubMed] [Google Scholar]
- 5.Welch WP, Miller ME, Welch HG, et al. Geographic variation in expenditures for physicians’ services in the United States. N Engl J Med. 1993;328:621–627. doi: 10.1056/NEJM199303043280906. [DOI] [PubMed] [Google Scholar]
- 6.Qaseem A, Alguire P, Dallas P, et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012;156:147–149. doi: 10.7326/0003-4819-156-2-201201170-00011. [DOI] [PubMed] [Google Scholar]
- 7.Daniels M, Schroeder SA. Variation among physicians in use of laboratory tests. II. Relation to clinical productivity and outcomes of care. Med Care. 1977;15:482–487. doi: 10.1097/00005650-197706000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Powell EC, Hampers LC. Physician variation in test ordering in the management of gastroenteritis in children. Arch Pediatr Adolesc Med. 2003;157:978–983. doi: 10.1001/archpedi.157.10.978. [DOI] [PubMed] [Google Scholar]
- 9.Murray JP, Greenfield S, Kaplan SH, et al. Ambulatory testing for capitation and fee-for-service patients in the same practice setting: relationship to outcomes. Med Care. 1992;30:252–261. doi: 10.1097/00005650-199203000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Vogt AW, Henson LC. Unindicated preoperative testing: ASA physical status and financial implications. J Clin Anesth. 1997;9:437–441. doi: 10.1016/s0952-8180(97)00060-3. [DOI] [PubMed] [Google Scholar]
- 11.American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Practice advisory for preanesthesia evaluation: a report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2002;96:485–496. doi: 10.1097/00000542-200202000-00037. [DOI] [PubMed] [Google Scholar]
- 12.Card R, Sawyer M, Degnan B, et al. Health Care Guideline: Perioperative Protocol. 7. Bloomington, MN: Institute for Clinical Systems Improvement; 2014. [Google Scholar]
- 13.Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518–528. doi: 10.1097/SLA.0b013e318265bcdb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown SR, Brown J. Why do physicians order unnecessary preoperative tests? A qualitative study Fam Med. 2011;43:338–343. [PubMed] [Google Scholar]
- 15.Blair M. Survey: physicians are aware that many medical tests and procedures are unnecessary, see themselves as solution. [September 9, 2014]; http://www.rwjf.org/en/about-rwjf/newsroom/newsroom-content/2014/04/surveyVphysicians-are-aware-that-many-medical-tests-and-procedu.html. Published May 1, 2014.
- 16.Berndtson K. Managers and physicians come head to head over cost control. Healthc Financ Manage. 1986;40:23–24. 28–29. [PubMed] [Google Scholar]
- 17.Horn DM, Koplan KE, Senese MD, et al. The impact of cost displays on primary care physician laboratory test ordering. J Gen Intern Med. 2014;29:708–714. doi: 10.1007/s11606-013-2672-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Varkey P, Murad MH, Braun C, et al. A review of cost-effectiveness, cost-containment and economics curricula in graduate medical education. J Eval Clin Pract. 2010;16:1055–1062. doi: 10.1111/j.1365-2753.2009.01249.x. [DOI] [PubMed] [Google Scholar]
- 19.Tek Sehgal R, Gorman P. Internal medicine physicians’ knowledge of health care charges. J Grad Med Educ. 2011:3182–187. doi: 10.4300/JGME-D-10-00186.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oboler SK, Prochazka AV, Gonzales R, et al. Public expectations and attitudes for annual physical examinations and testing. Ann Intern Med. 2002;136:652–659. doi: 10.7326/0003-4819-136-9-200205070-00007. [DOI] [PubMed] [Google Scholar]
- 21.Hermer LD, Brody H. Defensive medicine, cost containment, and reform. J Gen Intern Med. 2010;25:470–473. doi: 10.1007/s11606-010-1259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choosing Wisely. [October 13, 2014]; http://www.choosingwisely.org.
- 23.Feldman LS, Shihab HM, Thiemann D, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013;173:903–908. doi: 10.1001/jamainternmed.2013.232. [DOI] [PubMed] [Google Scholar]
- 24.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 25.May TA, Clancy M, Critchfield J, et al. Reducing unnecessary inpatient laboratory testing in a teaching hospital. Am J Clin Pathol. 2006;126:200–206. doi: 10.1309/WP59-YM73-L6CE-GX2F. [DOI] [PubMed] [Google Scholar]
- 26.Kim JY, Dzik WH, Dighe AS, et al. Utilization management in a large urban academic medical center: a 10-year experience. Am J Clin Pathol. 2011;135:108–118. doi: 10.1309/AJCP4GS7KSBDBACF. [DOI] [PubMed] [Google Scholar]
- 27.Stuebing EA, Miner TJ. Surgical vampires and rising health care expenditure: reducing the cost of daily phlebotomy. Arch Surg. 2011;146:524–527. doi: 10.1001/archsurg.2011.103. [DOI] [PubMed] [Google Scholar]
- 28.Han SJ, Saigal R, Rolston JD, et al. Targeted reduction in neurosurgical laboratory utilization: resident-led effort at a single academic institution. J Neurosurg. 2014;120:173–177. doi: 10.3171/2013.8.JNS13512. [DOI] [PubMed] [Google Scholar]
- 29.Axt-Adam P, van der Wouden JC, van der Does E. Influencing behavior of physicians ordering laboratory tests: a literature study. Med Care. 1993;31:784–794. doi: 10.1097/00005650-199309000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Chen C, Petterson S, Phillips R, et al. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312:2385–2393. doi: 10.1001/jama.2014.15973. [DOI] [PubMed] [Google Scholar]


