Abstract
Purpose
To investigate whether changes in physical activity (PA) impact sedentary behavior (SB) during a lifestyle intervention.
Design
Randomized trial.
Setting/participants
Participants (n=204) with low PA and high sedentary leisure screen time from the Chicago area.
Intervention
Participants were randomized to either increase PA (iPA) or decrease sedentary leisure (dSED). The intervention consisted of decision support, coaching, and financial incentives. For iPA participants, the goal was at least 60 min/day of self-reported moderate-to-vigorous-intensity PA (MVPA). For dSED participants the goal was less than 90 min/day of sedentary leisure screen time.
Measures
Daily accelerometer-based measures of SB and bout-corrected MVPA.
Analysis
Linear mixed-effects models were fit to estimate the effect of the intervention on MVPA and total SB and to estimate the effect of daily changes in MVPA on daily SB.
Results
iPA participants increased their bout-corrected MVPA by 14 min/day (p<.001) and decreased total SB by 18 min/day (p<.001). dSED participants did not significantly change their PA or their total SB. On days when participants exercised, each 10 minute bout of MVPA was associated with a 6 minute decrease in SB on the same day (p<.001).
Conclusion
In an intervention study designed to increase MVPA, participants who increase their time spent exercising will obtain much of this time by reducing their SB.
Keywords: accelerometry, compensation, exercise, MVPA
Indexing Key Words: Manuscript format: research, Research purpose: modeling/relationship testing, Study design: randomized trial, Outcome measure: behavioral, Setting: local community, Health focus: fitness/physical activity, Strategy: skill building/behavior change, Target population age: adults, Target population circumstances: geographic location
PURPOSE
A sedentary lifestyle and physical inactivity are well-established risk factors for heart disease, cancer and diabetes.1–5 In light of these links to adverse health outcomes and the continued increase in the prevalence of overweight and obesity in the United States, sedentary behaviors have emerged as an important target for health promotion and obesity and disease prevention efforts,6–8 complementing long-standing efforts to increase levels of moderate- to vigorous-intensity physical activity (MVPA).9–11 Despite calls to improve these health behaviors, U.S. adults average almost 8 hours per day in sedentary behaviors12 and 26% report no leisure time physical activity (PA).13
Few studies have examined the longitudinal relationship between objectively-measured MVPA and sedentary behavior within the context of a lifestyle intervention trial. This relationship is important because health risk behaviors tend to co-occur and become more numerous as social disadvantage increases.14, 15 Interdependencies among these bundled behaviors are poorly understood, making it difficult to know whether a lifestyle intervention that improves one risk behavior will have positive or negative effects on other behaviors in the bundle.16 Sometimes the behavioral synergy is positive, as when reducing television watching also reduces the paired intake of high calorie foods.17 At other times, the synergy is negative, as when quitting smoking leads to overeating and weight gain.18
In this study we examined whether an intervention designed to increase PA may produce the tag-along benefit of decreasing sedentary behavior and, likewise, that an intervention designed to decrease sedentary behavior may synergistically increase PA. Such positive substitutive effects among clustered behaviors are predicted by behavioral choice theory.19, 20 Conversely, if increasing physical activity causes fatigue that, in turn, has the unintended negative consequence of also increasing sedentary behavior, the health benefits of increased PA could be offset. Improving our understanding of the relationship between sedentary behavior and PA in an intervention designed to change these behaviors can help inform the design of lifestyle interventions so that increases in PA are not compensated for and undercut by increases in sedentary behavior.
There are a number of mechanisms that could drive the relationship between PA and sedentary behavior. One argument is that exercise participation may incidentally result in an increase in sedentary behavior by causing fatigue and reducing the drive to be active in non-exercise periods.21 Another possibility is that adults who exercise regularly may generally have more energy, or have enhanced feelings of vigor, resulting in less sedentary behavior.22, 23 These two arguments do not necessarily oppose one another as adults who tend to be active and sit less overall, may be more sedentary on days when they exercise more than usual. A third possibility is that greater exercise time may simply displace sitting time.24
Several cross-sectional studies that have reported on the relationship between PA and sedentary behavior have used self-report measures and have found equivocal associations.25–28 A notable exception is Craft et al.29 who used objectively measured data from accelerometers and found no differences in sedentary behavior between women who were active and those who were not. However the cross-sectional designs of these studies do not provide information on the effect of changes in PA on sedentary behavior over time as would be observed in an intervention study.
Studies examining the relationship between changes in PA and sedentary behavior in the context of an exercise intervention include Lee and King,30 who investigated changes in sedentary behavior in two PA interventions among older adults based on a self-reported weekly activities questionnaire. In both interventions, they found no changes in sedentary behavior even though participants in the PA conditions increased their MVPA. De Cocker et al.31 found that intervention participants in a PA promotion trial who increased their pedometer step counts also significantly decreased their sitting time, although the decrease in sitting time—18 minutes/day, was not particularly large and sitting time was assessed by self-report. Gilson et al.32 found no changes in sedentary behavior (as measured by self-report) among participants randomized to a walking intervention. Similarly, Kozey-Keadle et al.33 also found no significant changes in sedentary time (measured using an activity monitor) in participants randomized to an exercise intervention. These results suggest that PA and sedentary behavior may be distinct behaviors with different determinants.7, 34
The aim of the current study is to examine how changes in PA over time affect sedentary behavior in the context of an intervention study using a wearable accelerometer to estimate sedentary behavior and PA. Two hypotheses are tested, a between-subjects hypothesis and a within-subjects hypothesis. The between-subjects hypothesis is that individuals who are more active during the course of the study will be less sedentary. The within-subjects hypothesis is that on days when individuals engage in more MVPA than usual (regardless of how active they tend to be overall), they will be more sedentary in order to compensate for the additional energy expenditure. Analyses are performed at the day-level in order to investigate these hypotheses.
Information from this analysis will help inform the designs of PA intervention studies. For example, if the association between time spent engaging in MVPA and sedentary behavior is negative or independent, then PA intervention studies may not need to be concerned with unintended increases in sedentary behavior. Conversely, if the association is positive, then studies may need to be designed that target both sedentary behavior and MVPA.
METHODS
Design
The data come from the Make Better Choices (MBC) study, a randomized lifestyle intervention of adults designed to test competing hypotheses about the optimal way to promote healthy lifestyle change among four risk behaviors: high saturated fat intake, low fruit and vegetable intake, low PA, and high sedentary leisure screen time behavior. These behaviors were chosen so that there were two eating behaviors and two activity behaviors which were a combination of low-rate healthy behaviors (PA; fruit and vegetable consumption) and high-rate unhealthy behaviors (sedentary behavior; saturated fat consumption). In the MBC study, sedentary leisure screen time behavior was defined as non-work-related sedentary behavior that took place in front of a screen (e.g. television, movies, recreational internet use, and video games).
Sample
Table 1 reports the baseline characteristics of the 204 participants of the MBC study. This was a relatively young, well-educated sample, consisting of mostly White and African American women. Details on the design and methods of the MBC study can be found elsewhere.20, 35 Briefly, adults aged 21 to 60 years from the Chicago area were recruited through community advertisements. To be eligible, individuals needed to self-report engaging in all four risk behaviors: (i) intake of fewer than 5 fruits/vegetables daily; (ii) greater than 8% caloric intake from saturated fat; (iii) less than 60 minutes/day of MVPA; and (iv) greater than 90 minutes/day of sedentary leisure screen time behavior.
Table 1.
Characteristics of study participants
| Total (n=204) | Decrease Sedentary Behavior (n=109) | Increase Physical Activity (n=95) | p-value for difference | |
|---|---|---|---|---|
| Age | 33 (11) | 33 (12) | 33 (10) | .85 |
| BMI* | 28.2 (7.1) | 27.7 (6.3) | 28.9 (7.9) | .22 |
| Female No. (%) | 157 (77) | 82 (75) | 75 (79) | .53 |
| Ethnicity No. (%) | ||||
| Asian/Pacific islander | 24 (12) | 12 (11) | 12 (13) | |
| Black/African American | 47 (23) | 18 (17) | 29 (31) | |
| Caucasian | 109 (53) | 65 (60) | 44 (46) | .16 |
| More than one race | 6 (3) | 3 (3) | 3 (3) | |
| Hispanic/Latino | 18 (9) | 11 (10) | 7 (7) | |
| Education No. (%) | ||||
| Associate/some college or less | 61 (30) | 27 (24.8) | 34 (35.8) | |
| Bachelor’s degree | 46 (23) | 23 (21) | 23 (24) | .11 |
| Some graduate school or greater | 97 (48) | 59 (54) | 38 (40) | |
| Marital Status No. (%) | ||||
| Married or living with partner | 81 (40) | 47 (43) | 34 (36) | |
| Single/Separated/Divorced | 123 (60) | 62 (57) | 61 (64) | .29 |
| Baseline Sedentary (hrs/day)† | 9.1 (1.6) | 9.1 (1.6) | 9.0 (1.5) | .65 |
| Baseline MVPA (min/day)† | 32.8 (24.9) | 31.3 (24.1) | 34.4 (25.6) | .15 |
| Baseline MVPA bouts (min/day)† | 10.6 (19.2) | 10.0 (19.2) | 11.2 (19.2) | .36 |
All values are mean (SD) unless otherwise noted
two participants were missing BMI
adjusted for accelerometer wear time
Candidates who self-reported all 4 risk behaviors were enrolled in a 2-week baseline phase in which they wore an accelerometer, recorded diet and activity on a handheld device, and uploaded their data daily. Those candidates who displayed all 4 risk behaviors, based on the handheld device and accelerometer results, were randomized (stratified by sex) into one of four treatment groups which targeted one activity behavior and one diet behavior: Group 1) increase MVPA, decrease saturated fat; Group 2) increase MVPA, increase fruits and vegetables; Group 3) decrease sedentary leisure screen time, decrease saturated fat; Group 4) decrease sedentary leisure screen time, increase fruits and vegetables.
The MBC study was approved by the institutional review boards of the University of Illinois at Chicago and Northwestern University. All participants provided informed consent. Figure 1 diagrams participant flow through the trial.
Figure 1.
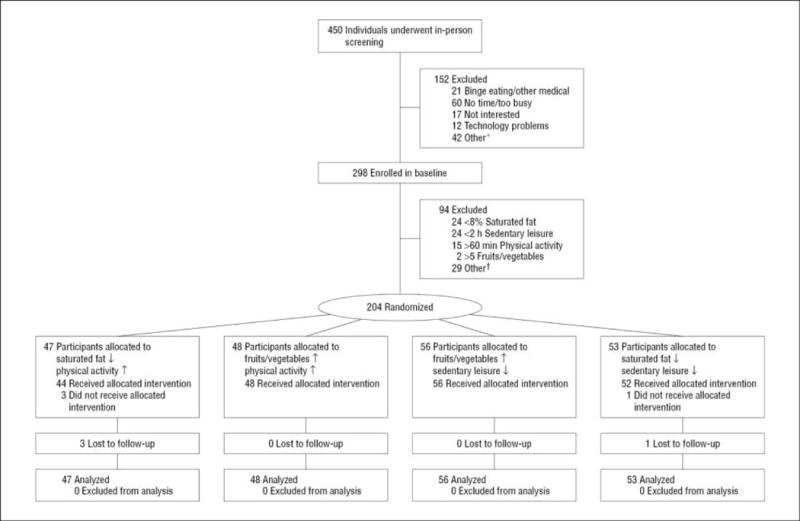
CONSORT flow diagram. *Other at screening includes no personal computer/landline, substance abuse, required but did not receive physician approval for blood pressure, and ineligible due to recent lifestyle change. †Other at baseline includes incomplete data during baseline recording, unreliable recording/compliance/communication, and required but did not receive physician approval for blood pressure. ↑Indicates increase; ↓, decrease. Adapted from “Multiple Behavior Changes in Diet and Activity,” by B. Spring, K. Schneider, G. McFadden, J. Vaughn, A.T. Kozak, M. Smith, A.C. Moller, L.H. Epstein, A. DeMott, D. Hedeker, J. Siddique, D.M. Lloyd-Jones, 2012, Archives of Internal Medicine, 172, p. 790, Figure 1. Copyright 2012 by the American Medical Association. Adapted with permission.
Intervention
The intervention phase of the study was three weeks and consisted of decision support, remote behavioral coaching, and financial incentives to achieve the goals for the two targeted behaviors to which the participant was randomized: 5 fruit/vegetable servings, saturated fat intake less than 8% of calories, MVPA of at least 60 min/day, or sedentary leisure screen time behavior less than 90 min/day. Decision support consisted of a goal thermometer on the handheld device that displayed each participant’s progress towards their goal for that day. Goals were based on self-reported behaviors and were daily in order to encourage real-time self-monitoring and awareness.36 Physical activity and sedentary behavior goals were based on self-report because the accelerometer technology at the time did not allow for real-time feedback via wireless transmission of data. The self-reported MVPA goal of 60 min/day exceeds that of PA guidelines and was chosen in recognition of the fact that participants tend to overestimate their PA. Had self-monitoring by accelerometer been possible, an MVPA goal closer to the recommended U.S. guideline of 30 min/day would likely have been chosen.11
For the first week of treatment (week 3 of the study), daily goals were set midway between the baseline behavior and the ultimate daily goal. Participants were expected to reach their behavioral targets during week 4 and to maintain them during week 5. During the three treatment weeks, participants wore an accelerometer and communicated as needed with their coaches via telephone or e-mail, per preference, to overcome challenges. Some common challenges for participants randomized to decrease sedentary behavior included not knowing how to relax/reduce stress without television. Common challenges for those randomized to increase MVPA included exercising in very hot or very cold weather. Participants could earn a $175 incentive for meeting the goals for both targeted behaviors during the treatment phase.
For the purposes of this paper—where the focus is on MVPA and sedentary behavior—treatment groups 1 and 2 are combined into an increase PA (iPA) group and treatment groups 3 and 4 are combined into a decrease sedentary leisure screen time behavior (dSED) group. It should be noted that while participant goals were based on their own self-reported behaviors, all of the analyses reported in this manuscript use results from the accelerometer.
Measures
Activity monitor
MBC participants wore an Actigraph accelerometer (model 7164; Actigraph, LLC, Pensacola, Florida) throughout the 2-week baseline phase and the 3-week treatment phase. This uniaxial Actigraph measures and processes vertical acceleration as counts, providing an indication of the amount and intensity of PA.37 Data were recorded in 1-minute epochs. The Actigraph 7164 has been validated for the measurement of both sedentary behavior and PA.12, 38
Participants were instructed to secure the accelerometer to their waist with an adjustable belt worn over or under clothing from the time they woke up until bedtime and to take it off during water-based activities (e.g. bathing, swimming).
Data reduction and determination of sedentary behavior and physical activity
Non-wear time was defined as intervals of at least 60 consecutive minutes of zero counts, with allowance for up to 2 consecutive minutes of observations of 1–100 counts/min. Periods of non-wear were defined as ending when count levels exceeded 100 counts/min or when 3 consecutive minutes of observation were between 1 and 100 counts/min. Wear time was determined by subtracting non-wear time from 24 hours. A day was considered a “valid monitoring day” if daily wear time exceeded ten hours.39
Bout-corrected MVPA, rather than total MVPA is the PA outcome measure because sustained MVPA was the targeted behavior of the iPA group and Federal PA guidelines state that MVPA should be accumulated in bouts of at least 10 minutes in order to qualify towards the goal of 150 minutes per week.11 Using cut-points developed by Freedson et al,38 daily minutes of bout-corrected MVPA were calculated as the number of accelerometer counts greater than 1951 counts/min that occurred in bouts of 10 consecutive minutes or more, with allowance for 1–2 minutes of counts below 1951 counts/min.40 Daily time spent in sedentary behavior was estimated as the amount of time accumulated below 100 counts/min during periods when the monitor was worn.12
Analysis
The first analysis assessed the effect of the MBC intervention on both sedentary behavior and MVPA separately. These analyses used linear mixed-effects models41 where the outcome was either daily minutes of bout-corrected MVPA or daily hours of sedentary behavior as measured by the accelerometer. Fixed effects included an indicator variable for the first week of treatment, an indicator variable for the last two weeks of treatment, and their interaction with the iPA condition. Models controlled for weekend, accelerometer wear time, gender, and age. To account for correlated observations on the same subject, random intercept and time effects were included in the models. In these models, the focus of inference is on the fixed time effects which measure change from baseline and also the fixed time by treatment interaction terms which measure the difference in change from baseline between the two treatment groups.
The second set of analyses investigated how daily changes in MVPA affect daily amounts of sedentary behavior. Here, the dependent variable was daily minutes of sedentary behavior and we used linear mixed-effects models controlling for weekend, accelerometer wear time, gender and age. Daily MVPA was a covariate in this model which was decomposed into between-subject and within-subject effects,42 namely,
| (Equation 1) |
where is the MVPA for person i on day j, and is the average MVPA for person i within a treatment phase (baseline, week 3, or weeks 4–5). Both terms on the right hand side of Equation 1 were entered into the regression model in order to estimate two effects. The term on the right hand side of Equation 1 is an estimate of a participant’s usual activity. Those participants who tend to be more active during the study will have higher values of . The term on the right hand side of Equation 1 measures how much on a given day a participant deviated from their usual activity level. Even participants who tend to be inactive (as measured by low values of ) will still have some days when they are more active than usual (as measured by a high value of . Conversely, there will be participants who are very active who will have days when they are not active at all. The regression coefficient on estimates the effect of usual activity level on sedentary behavior. The coefficient on estimates the effect on sedentary behavior when a participant is more or less physically active than usual. If both regression coefficients are not significantly different from one another, both terms on the right hand side of Equation 1 are replaced with in the model, and the resulting estimate is the effect of daily MVPA on sedentary behavior. All statistical analysis were performed using StataSE Version 13 (StataCorp LP, College Station, TX).
RESULTS
As shown in Table 1, during the two-week baseline period, the average number of hours of sedentary behavior was 9.1 hours per day. Average total MVPA was 33 minutes per day and bout-corrected MVPA averaged 11 minutes per day.
Table 2 shows accelerometer metadata based on days when the accelerometer was worn for 10 or more hours. Compliance was good, with participants wearing the device 5 to 6 days out of the week (including at least one weekend) throughout the study. Average wear time was approximately 14 hours per day.
Table 2.
Accelerometer adherence measures by treatment phase and intervention condition
| Baseline (2 weeks) | Trt Week 3 | Trt Weeks 4 & 5 | ||||
|---|---|---|---|---|---|---|
| Decrease SED | Increase PA | Decrease SED | Increase PA | Decrease SED | Increase PA | |
| No. ten hour days | 10.7 | 11.0 | 5.7 | 6.6 | 10.5 | 11.4 |
| No. ten hour days (total) | 1063 | 1004 | 560 | 584 | 1078 | 1017 |
| No. weekend (Sat & Sun) days | 2.7 | 2.6 | 1.4 | 1.6 | 2.5 | 3.1 |
| No. weekend days (total) | 264 | 235 | 137 | 143 | 262 | 274 |
| Wear time hours | 14.4 | 14.5 | 14.4 | 14.3 | 14.3 | 14.7 |
| Wear time hours (total) | 15305 | 14549 | 8072 | 8372 | 15368 | 14925 |
Note: Values above only include days where the accelerometer was worn for 10 hours or more.
All values are means unless noted.
PA, physical activity.
SED, sedentary behavior;
Table 3 displays estimated mean bout-corrected MVPA (min/day) and sedentary behavior (hours/day) based on the linear mixed-effects models. These models control for wear time, weekend day, gender and age so that the results at baseline are slightly different from those reported in Table 1. Examining the results for bout-corrected MVPA, participants in the dSED condition increased their minutes of bout-corrected MVPA between baseline and week 3 by 1 minute (ns) while those in the iPA condition increased their minutes of bout-corrected MVPA by 11 minutes (p<.001). The difference in change scores between the two treatment groups at week 3 was significant (p<.001). By the end of the intervention period, participants in the dSED condition still had not significantly changed their bout-corrected MVPA while those in the iPA condition had increased their MVPA from baseline by 14 minutes per day (p<.001). The difference in change scores between baseline and the end of treatment remained significantly different between the two treatment groups (p<.001).
Table 3.
Physical activity and sedentary behavior predicted daily means (SE) by treatment phase and intervention condition.
| MVPA bouts (min/day) | Sedentary behavior (hrs/day) | |||||
|---|---|---|---|---|---|---|
| Decrease SED | Increase PA | Trt Diff | Decrease SED | Increase PA | Trt Diff | |
| Baseline (2 weeks) | 12.9 (1.2) | 12.9 (1.2) | 9.3 (0.1) | 9.3 (0.1) | ||
| Week 3 | 13.8 (1.4) | 23.5 (1.4) | 9.2 (0.1) | 9.0 (0.1) | ||
| Change from baseline to week 3 | 0.9 (1.1) | 10.7 (1.1)* | −9.7 (1.5)* | −0.1 (0.1) | −0.3 (0.1)* | 0.2 (0.1) |
| Weeks 4 & 5 | 14.3 (1.3) | 26.7 (1.3) | 9.2 (0.1) | 9.0 (0.1) | ||
| Change from baseline to weeks 4 & 5 | 1.4 (0.9) | 13.9 (0.9)* | −12.4 (1.2)* | −0.1 (0.1) | −0.3 (0.1)* | 0.2 (0.1) |
Note: Models controlled for accelerometer wear time, weekend day, gender, and age. Results above are weekday means.
MVPA bouts, Moderate + Vigorous activity accumulated in bouts
p<.001. Only estimates in the rows labeled “Change” were assessed for statistical significance
Looking at the results for sedentary behavior in Table 3, participants in the dSED condition decreased their hours of sedentary behavior between baseline and week 3 by 0.1 hours, approximately 6 minutes (ns) while those in the iPA condition decreased their minutes of sedentary behavior by 0.3 hours, approximately 18 minutes (p<.001). The difference in change scores between the two treatment groups was not significant (p=.2). By the end of the intervention period, participants in the dSED condition still had not significantly changed their sedentary behavior while those in the iPA condition had decreased their sedentary behavior from baseline by approximately 18 minutes per day (p<.001). The difference in change scores between baseline and the end of treatment was not significantly different between the two treatment groups.
Table 4 reports the results of the analyses examining the effect of MVPA on sedentary behavior. When fitting the model that decomposed MVPA into between- and within-subject effects as in Equation 1, the regression coefficients on these two effects were not significantly different from one another (p=.26). Therefore, reported are the results of a model that only uses bout-corrected MVPA in its raw form as a covariate.
Table 4.
Results from a regression model predicting daily minutes of sedentary behavior
| Variable | Coefficient | Lower 95% CI | Upper 95% CI | p-value |
|---|---|---|---|---|
| MVPA bouts (min) | −0.6 | −0.7 | −0.5 | <.001 |
| Weekend | −22.0 | −26.6 | −17.5 | <.001 |
| Wear hours | 40.1 | 39.1 | 41.1 | <.001 |
| Male | 18.8 | 8.8 | 28.7 | <.001 |
| Age | −1.6 | −2.4 | −0.8 | <.001 |
| Intercept | 559.3 | 549.1 | 569.4 | <.001 |
The regression coefficient for minutes of MPVA bouts in Table 4 is equal to −0.6. Thus, on a given day, each additional 10 minute bout of MPVA is associated with a 6 minute decrease in sedentary behavior on the same day (p<.001). Weekend, wear time, female gender, and age were also significant, as they were in the models reported in Table 3. Sedentary behavior is lower on weekends, and among women. Daily sedentary behavior increases by 40 minutes for each additional hour of wear time and decreases by about 2 minutes per each additional year of age.
DISCUSSION
This study investigated the effects of a lifestyle intervention on MVPA and sedentary behavior using data from 204 ethnically diverse men and women who wore an accelerometer for 5 weeks. Those participants randomized to the iPA condition significantly increased their bout-corrected MVPA and significantly decreased their sedentary behavior. Participants randomized to the dSED condition did not significantly change either behavior. There was a significant difference in MVPA change scores between the iPA and dSED conditions but no significant difference in sedentary behavior change scores between the two conditions. The difference in sedentary behavior change scores was small, and this between-subjects comparison is less powerful than comparisons within a treatment condition.
We found that, on a given day, there is a significant inverse relationship between MVPA and sedentary behavior such that an increase in MVPA is associated with a decrease in sedentary behavior. Thus, the data support the notion that increasing MVPA does not increase time spent in sedentary behavior. This is the largest study that we are aware of to investigate the longitudinal relationship between PA and sedentary behavior in an intervention setting, using accelerometer-based measures to estimate sedentary time and physical activity.
The analysis which treated MVPA as a covariate in the model predicting sedentary behavior sheds some light on why those participants in the iPA condition were able to change both behaviors even though sedentary behavior was not targeted by the coaches. On a given day, for every additional 10-minute bout of MVPA, sedentary behavior decreased by 6 minutes. Thus, there is tradeoff between MVPA and sedentary behavior. This is counter to the hypothesis that the relationship between these two behaviors would move in the same direction. It had been hypothesized that on days when participants exercised more, they would also sit more in order to compensate for the additional energy expenditure. Instead, we observed a tradeoff which suggests that participants found the additional time to exercise by taking away from time that they had previously spent engaged in sedentary behavior, an optimal outcome for health.
While the change in sedentary behavior among participants in the iPA condition was significant, the amount of change itself was relatively minor compared to the total daily sedentary time, amounting to only an 18 minute per day decrease from the 9 hours per day observed at baseline. Nevertheless, recent findings indicate that reallocating time spent sedentary to MVPA is the most potent health enhancing behavior in terms of reducing CVD risk biomarkers, with 2–25% improvement per 30 minutes of reallocation.43 These cardioprotective effects may derive both from the beneficial effects of increasing MPVA and from reducing the adverse effects of prolonged sedentary time. Notably, it was only the iPA intervention that produced beneficial effects on both outcomes. The dSED intervention, in contrast, did not significantly change either sedentary time or MVPA. An alternative and feasible approach to PA intervention that is attracting attention is to increase light-intensity PA.44, 45 In addition to having potential direct beneficial effects on cardiovascular health, light-intensity PA covaries inversely with sedentary time, such that light activity usually displaces sedentary behavior.
Although the MBC study consisted of four treatment groups, for our analyses we collapsed over the diet conditions so that we only had two treatment groups: dSED and iPA. In order to investigate whether the dietary components of the study interacted with the activity components, we conducted a sensitivity analysis which included all 4 treatment groups rather than collapsing over the two dietary groups. For the analyses of sedentary behavior, there were no significant interactions between the diet and activity groups. That is, change in sedentary behavior at week 3 and at the end of treatment did not differ based on the targeted dietary behavior. For the analyses of MVPA, change in the dSED group at week 3 and at the end of treatment did not differ significantly by diet group. In the iPA Group, there was no significant difference in change scores by diet group at week 3, but there was a 6 minute difference in change from baseline between the increase fruits and vegetables group (11 minute increase) and the decrease saturated fat group (17 minute increase). With only one significant small difference across the two activity behaviors and two follow-up time points, we chose to continue using the collapsed treatment groups but note that this interaction between a targeted unhealthy eating behavior and a targeted healthy activity behavior is an area worthy of further investigation.
We also investigated several additional models which looked at the relationship between sedentary behavior and MVPA by treatment group and time and found that this relationship did not differ by treatment group, nor did it change over time. These results suggest that participants in an intervention study obtain time for MPVA by reducing sedentary behavior and that they continue to do so at the same rate even when their levels of MPVA increase.
The current study has several limitations that should be noted. A cut-point of 100 counts/min was used to define sedentary behavior. Although this is the standard accelerometer criterion for defining sedentary behavior12 it has been noted that the 100 counts/min cut-point may underestimate sedentary behavior and miss changes in sedentary behavior.46 Also, MBC participants in the dSED condition were instructed to decrease specific discretionary leisure sedentary screen time activities (e.g. watching TV, playing video games) rather than total sedentary time. This intervention approach was adopted to avoid interfering with necessary or valuable work, school, or social activities and discretionary leisure screen time was considered a high-prevalence unhealthy behavior with less value to the participant than non-screen time sedentary behavior. Participants in the dSED condition could, without penalty, replace sedentary leisure screen time behaviors with non-screen activities such as reading a book or talking on the phone. Based on self-report, participants in the dSED condition did significantly decrease time spent in targeted sedentary leisure screen time.35 However, the accelerometer was unable to detect this change as it could not distinguish between leisure screen time and other voluntary sedentary behaviors such as reading. As a result, the analyses of accelerometry-derived activity measures reported here were only able to detect the effect of the interventions on total sedentary time rather than the targeted outcome (sedentary leisure screen time behavior) and the analyses were only able to determine the relationship between MVPA and total (rather than leisure screen time) sedentary behavior. A final limitation is the short-term nature of the MBC study. It is not clear how the relationship between MVPA and sedentary behavior might change over a longer intervention or after the end of active treatment.
The fact that an exercise intervention did not cause participants to sit more is encouraging and suggests that the effectiveness of an exercise intervention on improved health is not necessarily compromised by a compensatory increase in sitting. Instead, increases in PA resulted in a decrease in sedentary behavior, likely due to a reallocation of the time spent in the two categories of activity behaviors. Additional studies extending the present results to other populations (children, old, overweight/obese) would strengthen the conclusions of this study. It would also be of value to understand the relationship between PA and sedentary behavior when both behaviors are targeted for intervention at the same time. Since intervening to increase MVPA does not result in a substantial reduction in total time spent sedentary, even though it might selectively decrease unnecessary sitting, separate simultaneous interventions designed to decrease sedentary time are warranted.
SO WHAT? Implications for Health Promotion Practitioners and Researchers.
What is already known on this topic?
A sedentary lifestyle and physical inactivity are well-established risk factors for heart disease, cancer and diabetes. The few studies that have examined the relationship between physical activity and sedentary behavior have found equivocal associations. These studies were mostly cross-sectional and used self-reported measures. It was unknown whether an intervention designed to increase physical activity will result in an increase in sedentary behavior or whether it will produce the complementary benefit of a decrease in sedentary behavior.
What does this article add?
This study examines how changes in physical activity over time affect sedentary behavior in the context of a longitudinal intervention study. Physical activity and sedentary behavior were measured objectively, using wearable accelerometers. Increases in physical activity were associated with small but significant decreases in sedentary behaviors.
What are the implications for health promotion practice or research?
The results suggest that the effectiveness of an exercise intervention on improved health will not necessarily be compromised by a compensatory increase in sitting. Interventions that seek to change both sedentary behavior and physical activity may need to target both behaviors.
Acknowledgments
The Make Better Choices trial was supported by NIH grant R01 HL075451. Dr. Siddique’s effort was supported by NIH grant K07 CA154862-01. Dr. Craft’s effort was supported by NIH grant K07 CA134936-01A1.
References
- 1.Danaei G, Ding EL, Mozaffarian D, et al. The Preventable Causes of Death in the United States: Comparative Risk Assessment of Dietary, Lifestyle, and Metabolic Risk Factors. PLoS Med. 2009 Apr;6(4) doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grontved A, Hu FB. Television Viewing and Risk of Type 2 Diabetes, Cardiovascular Disease, and All-Cause Mortality A Meta-analysis. Jama-Journal of the American Medical Association. 2011 Jun 15;305(23):2448–2455. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting Time and Mortality from All Causes, Cardiovascular Disease, and Cancer. Med Sci Sports Exerc. 2009 May;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Hong YL, Labarthe D, et al. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction The American Heart Association’s Strategic Impact Goal Through 2020 and Beyond. Circulation. 2010 Feb 2;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 5.Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012 Nov;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 6.Neuhaus M, Eakin EG, Straker L, et al. Reducing occupational sedentary time: a systematic review and meta-analysis of evidence on activity-permissive workstations. Obes Rev. 2014 Oct;15(10):822–838. doi: 10.1111/obr.12201. [DOI] [PubMed] [Google Scholar]
- 7.Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults’ sedentary behavior determinants and interventions. Am J Prev Med. 2011 Aug;41(2):189–196. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 8.Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obes Rev. 2014 Nov;15(11):905–919. doi: 10.1111/obr.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007 Aug 28;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 10.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007 Aug 28;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 11.United States. 2008 physical activity guidelines for Americans : be active, healthy, and happy! Washington, DC: U.S. Dept. of Health and Human Services; 2008. Department of Health and Human Services. [Google Scholar]
- 12.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008 Apr 1;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Prevalence and trends data 2013: Behavioral Risk Factor Surveillance System. 2015 [Google Scholar]
- 14.Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. Am J Prev Med. 2004 Aug;27(2 Suppl):18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 15.Spring B, Moller AC, Coons MJ. Multiple health behaviours: overview and implications. Journal of Public Health. 2012 Mar;34:I3–I10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spring B, King AC, Pagoto SL, Van Horn L, Fisher JD. Fostering multiple healthy lifestyle behaviors for primary prevention of cancer. Am Psychol. 2015 Feb-Mar;70(2):75–90. doi: 10.1037/a0038806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999 Oct 27;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 18.Aubin HJ, Farley A, Lycett D, Lahmek P, Aveyard P. Weight gain in smokers after quitting cigarettes: meta-analysis. Br Med J. 2012 Jul 10;:345. doi: 10.1136/bmj.e4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bickel WK, Vuchinich RE. Reframing health behavior change with behavioral economics. Mahwah, N.J.: Lawrence Erlbaum; 2000. [Google Scholar]
- 20.Spring B, Schneider K, McFadden HG, et al. Make Better Choices (MBC): Study design of a randomized controlled trial testing optimal technology-supported change in multiple diet and physical activity risk behaviors. BMC Public Health. 2010 Sep 29;:10. doi: 10.1186/1471-2458-10-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rowland TW. The biological basis of physical activity. Med Sci Sports Exerc. 1998 Mar;30(3):392–399. doi: 10.1097/00005768-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Osei-Tutu KB, Campagna PD. The effects of short- vs. long-bout exercise on mood, VO2max, and percent body fat. Prev Med. 2005 Jan;40(1):92–98. doi: 10.1016/j.ypmed.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 23.Puetz TW. Physical activity and feelings of energy and fatigue: epidemiological evidence. Sports Med. 2006;36(9):767–780. doi: 10.2165/00007256-200636090-00004. [DOI] [PubMed] [Google Scholar]
- 24.Serrano-Sanchez JA, Marti-Trujillo S, Lera-Navarro A, Dorado-Garcia C, Gonzalez-Henriquez JJ, Sanchis-Moysi J. Associations between Screen Time and Physical Activity among Spanish Adolescents. PLoS One. 2011 Sep 1;6(9) doi: 10.1371/journal.pone.0024453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bauman A, Ainsworth BE, Sallis JF, et al. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ) Am J Prev Med. 2011 Aug;41(2):228–235. doi: 10.1016/j.amepre.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Burton NW, Khan A, Brown WJ, Turrell G. The association between sedentary leisure and physical activity in middle-aged adults. Br J Sports Med. 2012 Aug;46(10):747–752. doi: 10.1136/bjsm.2010.081430. [DOI] [PubMed] [Google Scholar]
- 27.Patel AV, Bernstein L, Deka A, et al. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010 Aug 15;172(4):419–429. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Proper KI, Cerin E, Brown WJ, Owen N. Sitting time and socio-economic differences in overweight and obesity. Int J Obes (Lond) 2007 Jan;31(1):169–176. doi: 10.1038/sj.ijo.0803357. [DOI] [PubMed] [Google Scholar]
- 29.Craft LL, Zderic TW, Gapstur SM, et al. Evidence that women meeting physical activity guidelines do not sit less: An observational inclinometry study. International Journal of Behavioral Nutrition and Physical Activity. 2012 Oct 4;:9. doi: 10.1186/1479-5868-9-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee RE, King AC. Discretionary time among older adults: How do physical activity promotion interventions affect sedentary and active behaviors? Ann Behav Med. 2003 Spr;25(2):112–119. doi: 10.1207/S15324796ABM2502_07. [DOI] [PubMed] [Google Scholar]
- 31.De Cocker KA, De Bourdeaudhuij IM, Brown WJ, Cardon GM. The effect of a pedometer-based physical activity intervention on sitting time. Prev Med. 2008 Aug;47(2):179–181. doi: 10.1016/j.ypmed.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 32.Gilson ND, Puig-Ribera A, McKenna J, Brown WJ, Burton NW, Cooke CB. Do walking strategies to increase physical activity reduce reported sitting in workplaces: a randomized control trial. Int J Behav Nutr Phys Act. 2009;6:43. doi: 10.1186/1479-5868-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kozey-Keadle S, Staudenmayer J, Mavilia M, Lyden K, Braun B, Freedson P. Changes in Sedentary Time and Physical Activity in Response to an Exercise Training and/or Lifestyle Intervention. Journal of Physical Activity & Health. 2013 doi: 10.1123/jpah.2012-0340. [DOI] [PubMed] [Google Scholar]
- 34.Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010 Dec;85(12):1138–1141. doi: 10.4065/mcp.2010.0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spring B, Schneider K, McFadden G, et al. Multiple Behavior Changes in Diet and Activity A Randomized Controlled Trial Using Mobile Technology. Arch Intern Med. 2012 May 28;172(10):789–796. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective Techniques in Healthy Eating and Physical Activity Interventions: A Meta-Regression. Health Psychol. 2009 Nov;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 37.John D, Freedson P. ActiGraph and Actical Physical Activity Monitors: A Peek under the Hood. Med Sci Sports Exerc. 2012;44:S86–S89. doi: 10.1249/MSS.0b013e3182399f5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998 May;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Masse LC, Fuemmeler BF, Anderson CB, et al. Accelerometer data reduction: A comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc. 2005 Nov;37(11):S544–S554. doi: 10.1249/01.mss.0000185674.09066.8a. [DOI] [PubMed] [Google Scholar]
- 40.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, Mcdowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008 Jan;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 41.Hedeker DR, Gibbons RD. Longitudinal data analysis. Hoboken, N.J.: Wiley-Interscience; 2006. [Google Scholar]
- 42.Neuhaus JM, Kalbfleisch JD. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics. 1998 Jun;54(2):638–645. [PubMed] [Google Scholar]
- 43.Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014 Feb 1;179(3):323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 44.Healy GN, Dunstan DW, Shaw JE, Zimmet PZ, Owen N. Objectively measured sedentary time and light-intensity physical activity are independently associated with components of the metabolic syndrome: the AusDiab study. Diabetologia. 2007 Sep;50:S67–S68. [Google Scholar]
- 45.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively Measured Sedentary Time, Physical Activity, and Metabolic Risk The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008 Feb;31(2):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 46.Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of Wearable Monitors for Assessing Sedentary Behavior. Med Sci Sports Exerc. 2011 Aug;43(8):1561–1567. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]


