Abstract
Objective
The objective of this research was to identify distinct trajectories of recovery in older depressed patients in order to identify optimal samples and points for interventions.
Methods
The sample was 368 patients ages 60 years and older diagnosed with major depression and enrolled in a naturalistic treatment study and followed for up to three years.
Results
A model with four trajectory classes fit the data best: a quick recovery class (43%), a persistent moderate symptom class (27%), a persistent high symptom class (15%), and a slow recovery class (15%). Compared to patients in the quick recovery class, patients in the persistent moderate symptom class had more IADL/mobility limitations and lower levels of subjective social support. Patients in the persistent high symptom class had higher levels of perceived stress and lower levels of social support compared with those with a quick recovery. Patients in the slow recovery class had a younger age of onset compared to those in the quick recovery group. In multinomial logistic regression, levels of perceived stress and social support at baseline significantly differed across classes controlling for demographic and health variables.
Conclusions
Older patients diagnosed with major depression can have varying patterns of response to treatment. Interventions targeting those patients with higher levels of perceived stress and lower levels of subjective social support at the time of the index episode may lead to more favorable long-term trajectories.
Keywords: depression, trajectories, aged, latent class analyses, social support
Introduction
Longitudinal community studies report a high percentage of older adults with depressive symptoms or diagnosed major depression are depressed years later (Beekman et al., 2001; Denihan et al., 2000; Henderson et al., 1997; Sharma et al., 1998). Beekman et al. (1995) followed a sample of older community residents and conducted five assessments over a one-year period. Of those adults depressed at the start of the study, 32% remitted without relapse, 25% remitted but relapsed during the period, and 43% were chronically depressed. Beekman et al. (2002) also studied the six-year outcome of a cohort of depressed older adults and found a total of 32% had a severe chronic course, 23% had remitted, and 44% had an unfavorable but fluctuating course. Similar results have been reported from clinical samples (Brodaty et al., 2001; Katon et al., 2006; Lyness et al., 2002; Stek et al., 2002). Each of these clinical studies reported that most patients had a relapsing course or persistent residual symptoms. Older patients treated for depression have a high rate of symptom deterioration (Katon et al., 2006).
Much of the previous research on depression outcomes has focused on changes in symptoms or diagnoses between two points in time rather than trajectories. Trajectories offer the opportunity to chart the course of depression over a follow-up period using repeated measurements. Latent class trajectories offer an additional advantage by identifying groups or classes of patients who are similar in their individual changes in depression scores over time.
It is clear patients with late-life major depression can have varying patterns of response following an index episode, with some patients reaching remission quickly and others experiencing persistent symptoms. An understanding of the varying trajectories of depression and the variables associated with particular trajectories can be informative to clinicians and researchers in identifying optimal samples and points for interventions.
Previous research utilizing latent trajectory analyses identified distinct trajectories of depressive symptoms in community-dwelling older men and women (Byers et al., 2012; Kuchibhatla et al., 2012; Montagnier et al., 2014). In these community studies, however, a large proportion of participants had minimal or persistently low levels of depressive symptoms. In a mixed age sample of patients with clinically significant depressive symptoms selected from family practices (Gunn et al., 2013), five distinct trajectories were identified, but the majority of the participants had a mild persistent course.
Fewer studies have examined trajectories in samples of patients with major depression. Distinct short-term trajectories of major depression outcomes in patients undergoing a treatment course of antidepressants have been identified (Dew et al., 1997; Uher et al., 2010), as well as in patients during a 10 week course of electroconvulsive therapy (Cinar et al., 2010), but long term trajectories in these samples have not been reported. In a mixed-age sample from the Netherlands, five 2-year course trajectories of outpatients with a unipolar depression disorder (major depression, dysthymia or both) were identified: a rapid remission class, a slow declining symptom class, a gradual decline from severe initial depression class, a chronic moderate class, and a chronic severe class (Rhebergen et al., 2012). It is not known whether similar trajectories would be observed in older patients diagnosed with major depression. Finally, Bogner et al. (2012) identified three distinct patterns of change over one year among older patients with either major or minor depression: a class with persistent high levels of symptoms, a class with severe symptoms at baseline who improved, and a class with less severe symptoms who also improved. A total of 66% of these patients had major depression. It is not known whether additional time of follow-up would provide more information about depression course and whether the trajectories in older patients would be different if those with minor depression were not included. The outcome for major depression is generally worse than that for minor depression (Lyness et al., 2002).
The aim of this analysis was to identify distinct patterns in the course of late-life depression in a clinical sample of older adults followed for up to three years following an index episode of major depression, and to identify variables associated with these distinct depression outcomes. We hypothesized that we would identify similar patterns to those identified by Bogner et al. above (2012) – a persistent high group and a group with moderate symptoms who improved. Because all of the patients in our sample had major depression at study onset, however, we did not expect to find a group with persistent low levels of depressive symptoms.
Methods
Study Sample
The sample included 368 patients age 60 years or older who met DSM-IV criteria for major depression. The patients were recruited from both inpatient and outpatient settings and were enrolled in the Neurocognitive Outcomes of Depression in the Elderly (NCODE) study at Duke University. This longitudinal study has been described elsewhere (Steffens et al., 2007). In summary, NCODE is an ongoing guideline-based prospective naturalistic treatment study of older adults with major depression. The sample includes both incident cases as well as recurrent cases of depression recruited from both psychiatry and primary care clinics at Duke. To be eligible to be enrolled in NCODE, patients had to be free of dementia or suspected cognitive impairment. Other exclusion criteria included a diagnosis of another major psychiatric condition such as schizophrenia; any primary neurological illness; active alcohol abuse or dependence; and metal in the brain which could affect magnetic resonance imaging. All patients received treatment, primarily antidepressants, augmented with ECT or psychotherapy. That is, patients received standard care. For these analyses, data from the first three years of follow-up were included. All participants provided written consent at enrollment. The study protocol is reviewed and approved annually by the Institutional Review Board at Duke University.
Measures
Depression status was measured at each clinic visit using the Montgomery-Asburg Depression Rating Scale (MADRS) (Montgomery and Asberg, 1979). The MADRS is clinician scored and has a possible range of 0 to 60, with scores <16 generally considered partially remitted and scores <7 in full remission. Patients were followed clinically at least every three months. Besides the MADRS score, two clinical variables were of interest in these analyses: self-reported age of onset of the first episode of major depression and the number of lifetime depression spells (4+ vs. <4). These variables were collected as a part of the depression section of the Diagnostic Interview Schedule (DIS) (Robins et al., 1981) which was administered to participants. Other information about general health and cognitive and physical functioning was collected in the Duke Depression Evaluation Schedule (DDES) (Blazer and Hughes, 1991) which was administered at baseline and every twelve months following. Participants were asked about their difficulties with basic activities of daily living using items from Katz et al. (1970): eating, dressing, grooming, walking, bathing, using the toilet, and bending to pick up objects on the floor. Instrumental activities of daily living limitations were measured using six items modified from Fillenbaum et al. (1988): getting around in the neighborhood, shopping for groceries or household items, preparing meals, cleaning house, doing yard work or gardening, and keeping track of money or bills. Mobility limitations were assessed using three items from Rosow-Breslau (1966): walking one-fourth of a mile, walking up and down one flight of stairs, and taking care of or watching children. Each task was coded as 0=no difficulty and 1=some difficulty or unable to do and the number of limitations was summed. Cognitive functioning was assessed with the Mini-Mental State Examination (MMSE), with higher scores indicating better cognitive functioning (Folstein et al., 1975).
Sociodemographic variables included age, race (white vs not white), sex, marital status (married vs. not married), and years of education. Two social variables from the DDES were included in these analyses: perceived stress and social support. Perceived stress was assessed by asking how much on a scale from 1 to 10 participants rated their average stress during the past six months, with 0 indicating no stress. Subjective social support included questions about feeling useful, understood, listened to, and lonely with family and friends as well as having a role, feeling able to count on, being able to talk about deepest problems with and being satisfied with family and friends. The range of scores was 9 to 27, with higher scores indicating higher levels of subjective social support.
Statistical Analysis
We sought to identify distinct classes of patients based on their trajectories of MADRS scores following enrollment in NCODE. All available MADRS scores for the first three years post baseline were used to identify the trajectories (a range of 2-59 measures per patient). Eighty-two percent of the sample contributed eight or more MADRS scores each to the trajectories. Some patients had fewer scores because of attrition, while others had not been in the study long enough to have multiple measures.
The trajectory classes were estimated using SAS (Version 9.3) PROC TRAJ software (Jones et al., 2001). PROC TRAJ is a group-based semi-parametric mixture model used to analyze longitudinal data that identifies distinct classes of individuals who follow a distinct pattern of change over time (Andruff et al., 2009; Jones and Nagin, 2007). The trajectory classes were based on MADRS score and a variable indicating baseline MADRS score Y/N to accommodate the drop in MADRS score that naturally occurs between study entry and the next assessment, usually around three months. We estimated models with 1 to 4 trajectory classes, allowing for both quadratic and cubic terms for each class to model the function of MADRS score over time. We removed non-significant higher order terms beginning with the first class. We compared nested models in two ways – using the Bayesian Information Criteria (BIC) statistics where smaller values overall indicate a better fit, and the associated Log Bayes Factor where the difference between the BIC statistics is estimated (Jones et al., 2001). Values greater than 10 for the Log Bayes Factor are interpreted as strong evidence for the more complex model with an additional class. Patients were assigned to the class with the highest posterior probability.
We compared clinical, demographic, health and social variables across the identified classes. As a final step we estimated a multinomial logistic regression model with class membership as the dependent variable to examine the associations between the selected variables and trajectory class.
Results
The sample of patients was predominantly female, white, and married, and had on average more than 12 years of education. The mean age at baseline was 69.9 years. The mean age of onset was in mid-life (44.6 years), and a majority of the sample had more than four lifetime spells of depression. As expected from the exclusion criteria, the sample had no evidence of dementia or moderate cognitive impairment at baseline. Participants had few functional limitations at baseline enrollment, and overall, reported good levels of social support and some stress in the past six months.
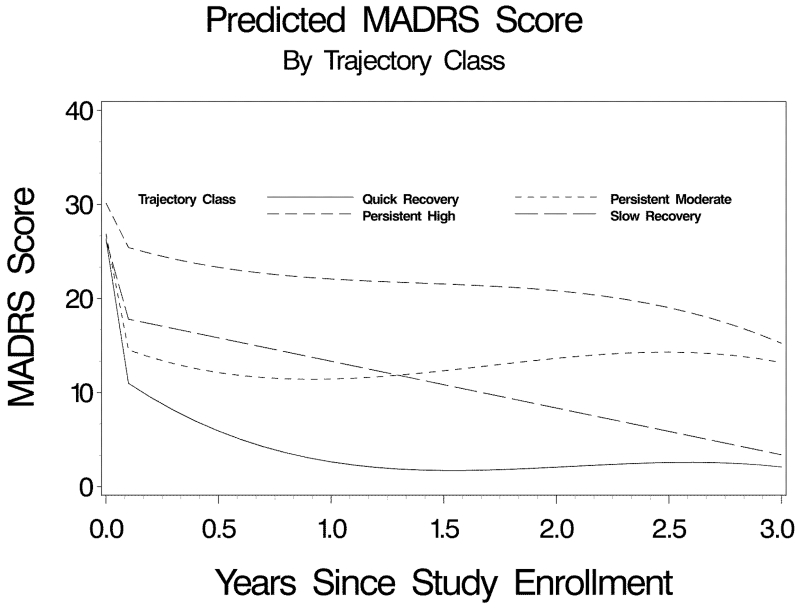
A model with four trajectory classes fit the data best. We observed that the BIC statistics decreased each time an additional class was added to the model. The Log Bayes factor (16.2) showed strong evidence for the four-class model over the three-class model. The proportions in each of the four classes were sufficient for meaningful interpretation.
The four trajectories are plotted in Figure 1. The immediate drop following enrollment reflects the adjustment for the baseline measure as previously described. The largest class in size was a quick recovery trajectory class where MADRS scores dropped after study enrollment and stayed low. Two classes showed an initial drop in MADRS score but persistent trajectories of moderate or high MADRS scores over the three years. The fourth class was a slow recovery class whose scores decreased gradually over the three year period. The trajectory for this slow recovery class was linear, while the trajectories for the other three classes showed some nonlinear properties.
Figure 1.
Predicted MADRS score by trajectory class over time (n=368)
The characteristics of the sample are shown by trajectory class in Table 1. The four classes significantly differed on their baseline MADRS score, marital status, mean years of education, mobility/IADL and ADL limitations, perceived stress, and subjective social support. Patients in the persistent high class in general had higher mean MADRS scores at baseline, fewer years of education, more functional limitations, higher levels of self-rated stress, and lower levels of perceived social support than patients in the other classes. We conducted some post hoc analyses to compare these sample characteristics in other ways. The proportion of whites and females in the slow recovery class did not differ from the proportion in the other three classes combined. A total of 37.5% of those in the slow recovery group were married compared to 56.1% of those in the other three groups (χ2[1]=6.6, p=0.01). The mean MADRS score at baseline for the persistent high group was significantly higher than the average baseline score for the other three groups (t[366]=−3.25, p=0.001). Patients in the quick recovery group had a later age of onset (t[354]=−2.44, p=0.02), more years of education (t[365]=2.73, p=0.01), fewer ADL limitations (t[356.9]=2.53, p=0.01), fewer IADL/mobility limitations (t[354.9]=4.58, p<0.001), lower perceived stress (t[359]=4.21, p<0.001, and higher levels of subjective social support (t[341.6]=−4.74, p<0.001) compared to patients in the other three groups combined. These post hoc analyses must be interpreted with caution because of the probability of a Type I error.
Table 1.
Characteristics of the sample at baseline by trajectory class (n=368)
| Total Sample (n=368) |
Quick Recovery Class (n=159) 43.2% |
Persistent Moderate Class (n=99) 26.9% |
Persistent High Class (n=54) 14.7% |
Slow Recovery Class (n=56) 15.2% |
Significance | |
|---|---|---|---|---|---|---|
| Clinical Variables | ||||||
| Mean Baseline MADRS Score (sd) |
27.0 (7.5) | 26.2 (7.6) | 27.10 (7.6) | 30.0 (7.3) | 26.2 (6.8) | F[3,364]=3.8, p=.01 |
| Mean Age of Onset (sd) |
44.6 (21.0) | 47.6 (19.8) | 44.2 (21.3) | 41.2 (20.4) | 39.6 (23.4) | F[3,352]=2.6, p=.05 |
| No. w/ Four or More Lifetime Spells (%) |
188 (52.8) | 74 (47.7) | 49 (52.1) | 32 (60.4) | 33 (61.1) | χ2[3]=4.3, p=.23 |
|
Demographic
Variables |
||||||
|
Mean Age (sd) |
69.9 (7.2) | 69.3 (6.7) | 69.3 (7.5) | 70.8 (7.8) | 69.8 (7.4) | F[3,364]=0.7, p=.57 |
| No. Women (%) | 244 (66.3) | 95 (59.8) | 68 (68.7) | 38 (70.4) | 43 (76.8) | χ2[3] =6.5, p=.09 |
| No. White (%) | 315 (85.6) | 136 (85.5) | 86 (86.9) | 48 (88.9) | 45 (80.4) | χ2[3]=1.8, p=.60 |
| No. Married (%) | 196 (53.3) | 96 (60.4) | 58 (58.6%) | 21 (38.9) | 21 (37.5) | χ2[3]=14.4, p=.002 |
| Mean Years Education (sd) |
13.5 (3.1) | 14.0 (2.8) | 13.6 (2.8) | 12.1 (4.1) | 13.4 (2.9) | F[3,363]=5.6, p=.001 |
|
Health and Social
Variables |
||||||
| Mean MMSE Score (sd) |
27.7 (2.7) | 28.0 (2.4) | 27.9 (2.5) | 27.2 (2.6) | 27.2 (3.6) | F[3,364]=2.2, p=.09 |
| Mean Mobility/IADL Difficulties (sd) |
4.1 (4.9) | 2.8 (4.1) | 4.6 (5.2) | 6.5 (5.7) | 4.5 (4.9) | F[3,353]=8.7, p<.001 |
| Mean ADL Difficulties (sd) |
0.7 (1.7) | 0.4 (1.3) | 0.6 (1.5) | 1.3 (2.5) | 0.9 (2.1) | F[3,359]=3.8, p=.01 |
| Mean Self-Rated Average Stress (sd) |
6.5 (2.1) | 6.0 (2.0) | 6.7 (1.9) | 7.3 (2.3) | 6.9 (2.1) | F[3,357]=6.9, p<.001 |
| Mean Subjective Social Support (sd) |
23.0 (3.9) | 24.1 (3.4) | 22.7 (3.8) | 20.2 (4.7) | 23.1 (3.4) | F[3,342]=13.8, p<.001 |
Sample sizes are slightly different because of missing values for some of the variables.
Table 2 presents the results of the multinomial logistic regression model showing the associations between selected covariates and trajectory class in controlled analysis using those participants with complete data (n=318). The reference group was those patients in Class 1, the quick recovery class. Patients in the persistent moderate class had more IADL/mobility limitations and lower levels of subjective social support compared to patients in the quick recovery class. Patients in the persistent high class had higher levels of perceived stress and lower levels of subjective social support compared to those in the quick recovery class. Patients in the slow recovery class had a younger age of onset compared to patients in the quick recovery class.
Table 2.
Results of the multinomial logistic regression model showing the association between selected covariates and trajectory class (n=318)
| Class 2 (26%) Persistent Moderate MADRS |
Class 3 (14%) Persistent High MADRS |
Class 4 (18%) Slower to Recover |
Wald Chi- Square [3 df] |
p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Est | Std Err | OR (95%CI) | Est | Std Err | OR (95% CI) | Est | Std Err | OR (95% CI) | |||
| Intercept | −0.30 | 3.38 | −1.66 | 4.19 | 0.06 | 3.84 | |||||
| Age | −0.01 | 0.02 | 1.00 (0.95,1.05) | 0.04 | 0.03 | 1.04 (0.98,1.11) | 0.01 | 0.03 | 1.01 (0.96,1.07) | 2.0 | .57 |
| White | 0.23 | 0.45 | 1.25 (0.52,3.04) | 0.28 | 0.61 | 1.33 (0.40,4.35) | 0.01 | 0.51 | 1.01 (0.37,2.72) | 0.4 | .94 |
| Female | 0.16 | 0.33 | 1.18 (0.62,2.22) | 0.09 | 0.48 | 1.09 (0.43,2.80) | 0.27 | 0.42 | 1.31 (0.58,2.98) | 0.5 | .91 |
| Married | 0.29 | 0.32 | 1.34 (0.72,2.49) | −0.54 | 0.44 | 0.59 (0.25,1.38) | −0.69 | 0.38 | 0.50 (0.24,1.05) | 7.5 | .06 |
| Years of Education | −0.02 | 0.06 | 0.98 (0.88,1.10) | −0.12 | 0.07 | 0.88 (0.77,1.01) | −0.02 | 0.07 | 0.98 (0.86,1.12) | 3.6 | .31 |
| Age of Onset | −0.01 | 0.01 | 0.99 (0.98,1.01) | −0.01 | 0.01 | 0.99 (0.96,1.01) | −0.02 | 0.01 | 0.98 (0.96,1.00) | 4.4 | .22 |
| Four+ Lifetime Spells |
−0.08 | 0.35 | 0.92 (0.47,1.82) | 0.29 | 0.51 | 1.34 (0.50,3.62) | −0.01 | 0.42 | 0.99 (0.44,2.24) | 0.5 | .92 |
| MMSE Score | 0.04 | 0.08 | 1.04 (0.88,1.23) | 0.05 | 0.10 | 1.05 (0.86,1.27) | −0.06 | 0.09 | 0.95 (0.80,1.13) | 1.4 | .70 |
| Basic ADL Limitations |
−0.15 | 0.15 | 0.86 (0.65,1.14) | −0.10 | 0.16 | 0.90 (0.65,1.24) | −0.03 | 0.17 | 0.97 (0.70,1.34) | 1.2 | .75 |
| IADL & Mobility Limitations |
0.10 | 0.05 | 1.11 (1.01,1.22) | 0.10 | 0.06 | 1.11 (0.98,1.25) | 0.06 | 0.06 | 1.06 (0.94,1.19) | 5.0 | .17 |
| Average Stress | 0.12 | 0.07 | 1.13 (0.98,1.30) | 0.29 | 0.10 | 1.33 (1.09,1.63) | 0.17 | 0.09 | 1.18 (1.00,1.40) | 9.4 | .02 |
| Subjective Social Support |
−0.10 | 0.04 | 0.91 (0.83,0.98) | −0.19 | 0.05 | 0.83 (0.75,0.92) | −0.01 | 0.05 | 0.99 (0.89,1.09) | 15.6 | .001 |
Reference group those in Class 1 (42%); OR=Odds Ratio; Sample size reduced because some variables had missing data;
As shown by the Wald χ2 with three degrees of freedom, the only two variables for which the overall effect across classes was significant were perceived stress and subjective social support. In post-hoc analyses, we tested within the multinomial logistic regression the hypotheses that the effects of stress and social support were equal across the classes other than quick recovery class (moderate vs. high, moderate vs. slow decline, and high vs. slow decline stress/social support). Only one of the six tests was significant: the effect of subjective social support in the persistent high group (−0.19) was significantly different from the effect in the slow to recover group (−0.01) (Wald χ2[1]=8.8, p=0.01).
A total of 50 of the 368 patients had incomplete data for one or more of the covariates of interest, resulting in a reduced sample size of 318 for the multinomial logistic regression which utilized complete case analysis. We used multiple imputation with SAS PROC MI to impute data for these patients based on five samples. The findings were essentially unchanged so we have presented our model with the reduced sample. Finally, class assignment is subject to misclassification error. That is, persons may be assigned to the class with the highest posterior probability but have some properties of other classes. To determine if this affected our conclusions, we drew five samples from each of five imputed data sets, estimating class from the multinomial probability distribution observed for each participant. We used simulated class assignment as the outcome variable and re-estimated the multinomial logistic prediction regression models. The results were essentially unchanged. Therefore, we retained the previous findings in our presentation based on class assignment to the highest posterior probability.
Discussion
We report findings of significant heterogeneity in the course of depression in late life, with social variables such as social support and stress particularly associated with recovery trajectories. Response over the initial period following the index episode may be a key predictor of depression course, and one point where interventions may be most beneficial. These findings are generally consistent with reports from a clinical trial that response in the first 3-4 weeks was a predictor of final remission (Kok et al., 2009).
Our finding that older patients clustered into distinct subgroups or classes based on their multi-year trajectories following an index episode of major depression is consistent with earlier reports in a mixed-age sample (Rhebergen et al., 2012), in a sample of patients with minor or major depression (Bogner et al., 2012), and with a sample of older patients undergoing treatment (Dew et al., 1997). Our data add to this body of knowledge in showing nonrandom variability in the long-term course of depression among a sample of older patients diagnosed with major depression and representative of older patients typically seen in clinical practice. The trajectories closely resembled those identified in other clinical samples with some patients having a chronic course and others improving. This study provides new information by estimating the percentage of patients initially diagnosed with major depression in each trajectory class. In our sample, approximately half of the patients recovered within the three-year follow up period, with over 40% making a quick recovery and an additional 15% a slower recovery. Over 40%, however, had persistent symptoms.
Our findings shown in Figure 1 appear to be consistent with those of Lyness et al (2002) that over half of older patients diagnosed with major depression had an active depression diagnosis one year later. Our three-year trajectories showed a significant proportion of patients had recovered. This recovery rate was somewhat higher than reports from longer-term studies (Brodaty et al., 2001; Stek et al., 2002), yet all these reports emphasize the chronicity of late life depression in a significant proportion of patients.
While the mean MADRS scores for each group at baseline were statistically different from each other, the scores were clinically very similar. Previous research has reported increasing levels of depression severity at baseline were associated with worse clinical outcomes (Katon et al., 2010). Our findings were consistent with this conclusion, but the majority of patients in our study had similar baseline scores and had better three-year outcomes.
Our findings of the association between stress and social support and the outcome of depression provide new information. In earlier reports from this sample, we reported that overall, psychosocial predictors were just as important as clinical and diagnostic variables in predicting depression outcome (Bosworth et al., 2002a; Bosworth et al., 2002b). We found in these analyses, however, that neither age of onset nor the number of lifetime spells of depression was differentially associated with trajectory classes. That is, these clinical variables affect depression outcome in a similar manner across classes. The finding that stress and social support are associated with the outcome of major depression in older adults is consistent with earlier reports that poor quality of social relationships is a risk factor for major depression (Teo et al., 2013) and previous reports from these data that the experience of stressful life events and greater perceived stress were associated with lower probability of remission from major depression (Zannas et al., 2012). We found that poor social support increased the probability of being in a trajectory class with persistent symptoms compared to a class with a quick recovery and that high levels of baseline stress were associated with persistent high MADRS scores but not persistent moderate scores or a slow decrease in depressive symptoms.
We do not know the mechanisms by which stress and social support affect the outcome of major depression. Stress is directly associated with depression, and strong social support has been shown to buffer these effects of stress on depression (Landerman et al., 1989) which may lead to a quicker recovery. Social support may also have direct effects which promote remission. Depression is a biologically driven disease with recurrence and subsequent remission not uncommon. Those in the quick recovery class with lower levels of stress and higher levels of social support at baseline may be responding to treatments as expected or remitting due to the natural course of the disease, while higher levels of stress and lower levels of social support in the other groups could be complicating the usual pattern of recovery. It is important to remember we are dealing with trajectory classes in these analyses and not outcomes in individual patients.
The study has some limitations. We recognize that treatment is a potential confounder in these analyses, but the diverse treatment patterns made it difficult if not impossible to adjust for the complex effects of individual medications. This was a naturalistic treatment study, however, and all patients received treatment, yet the treatments varied. Also, this sample represents the population that is typically seen in clinical practice. Of the predictors of class membership, only subjective social support and perceived stress were significant predictors of class membership. These findings may be due in part to endogeneity bias as the classes were created by these variables. Another limitation is sample attrition which is often observed in longitudinal studies and fewer measures being available for participants who more recently enrolled. Baseline in these analyses refers to the time of study enrollment at the index episode, not a sentinel event from which trajectories of depression status time can be assessed and compared.
Strengths of the research include the use of sophisticated analyses to identify distinct subgroups of patients within one group meeting criteria for a DSM diagnosis of major depression. These latent subgroups are determined through the use of measured and unmeasured variables. In this case, the measured variable was the change in MADRS score over time. Unmeasured variables could include changes in cognition, physical heath, and physical functioning, as well as social variables such as perceived stress and social support. Our naturalistic clinical sample was large and representative of patients typically seen in clinical practice.
Conclusion
Older patients diagnosed with major depression can have varying but identifiable patterns of response to treatment, with some reaching remission quickly and others experiencing a more chronic course. The optimal time for intervention may be the first several months following an index episode. Interventions targeting those patients with higher levels of perceived stress and lower levels of subjective social support at the time of the index episode may lead to more favorable long-term trajectories.
Key Points.
Older patients with major depression can have varying patterns of response following an index episode, with some patients reaching remission quickly and others experiencing persistent symptoms.
Response over the initial period may be a key predictor of depression course and one point where interventions may be most beneficial.
Interventions targeting those patients with higher levels of perceived stress and lower levels of subjective social support at the time of the index episode may lead to more favorable long-term trajectories.
Acknowledgements
This research was supported by NIMH grants R01 MH080311, R03 MH095917, R01 MH54846, and K24 MH70027. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Preliminary findings were presented at the 2010 Annual Meeting of the American Association of Geriatric Psychiatry.
Footnotes
Conflict of Interest: No disclosures to report.
Contributor Information
Celia F. Hybels, Department of Psychiatry and Behavioral Sciences, Center for the Study of Aging and Human Development, Duke University Medical Center, Box 3003, Durham, NC 27710.
Carl F. Pieper, Department of Biostatistics and Bioinformatics, Center for the Study of Aging and Human Development, Duke University Medical Center.
Dan G. Blazer, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center.
David C. Steffens, Department of Psychiatry, University of Connecticut Health Center.
References
- Andruff H, Carraro N, Thompson A, Gaudreau P. Latent class growth modeling: A tutorial. Tutorials in Quantitative Methods for Psychology. 2009;5:11–24. [Google Scholar]
- Beekman ATF, Deeg DJH, Geerlings RA, Schoevers RA, Smit JH, van Tilberg W. Emergence and persistence of late life depression: a 3-year follow-up of the Longitudinal Aging Study Amsterdam. J Affect Disord. 2001;65:131–138. doi: 10.1016/s0165-0327(00)00243-3. [DOI] [PubMed] [Google Scholar]
- Blazer D, Hughes D. Subjective social support and depressive symptoms in major depression: separate phenomena or epiphenomena. J Psychiatr Res. 1991;25(4):191–203. doi: 10.1016/0022-3956(91)90024-5. [DOI] [PubMed] [Google Scholar]
- Bogner HR, Morales KH, Reynolds CF, Cary MS, Bruce ML. Course of depression and mortality among older primary care patients. Am J Geriatr Psychiatry. 2012;20:895–903. doi: 10.1097/JGP.0b013e3182331104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosworth HB, Hays JC, George LK, Steffens DC. Psychosocial and clinical predictors of unipolar depression outcome in older adults. Int J Geriatr Psychiatry. 2002a;17:238–246. doi: 10.1002/gps.590. [DOI] [PubMed] [Google Scholar]
- Bosworth HB, McQuoid DR, George LK, Steffens DC. Time-to-remission from geriatric depression. Am J Geriatr Psychiatry. 2002b;10:551–559. [PubMed] [Google Scholar]
- Brodaty H, Luscombe G, Peisah C, Anstey K, Andrews G. A 25-year longitudinal, comparison study of the outcome of depression. Psychol Med. 2001;31:1347–1359. doi: 10.1017/s0033291701004743. [DOI] [PubMed] [Google Scholar]
- Byers AL, Vittinghoff E, Lui LY, Hoang T, Blazer DG, Covinsky KE, Ensrud KE, Cauley JA, Hillier TA, Fredman L, Yaffe K. Twenty-year depressive trajectories among older women. Arch Gen Psychiatry. 2012;69:1073–1079. doi: 10.1001/archgenpsychiatry.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinar S, Oude Voshaar RC, Janzing JGE, Birkenhäger TK, Buitelaar JK, van den Broek WW. The course of depressive symptoms in unipolar depressive disorder during electroconvulsive therapy: A latent class analysis. J Affect Disord. 2010;124:141–147. doi: 10.1016/j.jad.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Denihan A, Kirby M, Bruce I, Cunningham C, Coakley D, Lawlor BA. Three-year prognosis of depression in the community-dwelling elderly. Br J Psychiatry. 2000;176:453–457. doi: 10.1192/bjp.176.5.453. [DOI] [PubMed] [Google Scholar]
- Dew MA, Reynolds CF, Houck PR, Hall M, Buysse DJ, Frank E, Kupfer DJ. Temporal profiles of the course of depression during treatment. Predictors of pathways toward recovery in the elderly. Arch Gen Psychiatry. 1997;54:1016–1024. doi: 10.1001/archpsyc.1997.01830230050007. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh P. Mini-mental state: A practical method for grading the cognitive state of patients for clinicians. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gunn J, Elliott P, Densley K, Middleton A, Ambresin G, Dowrick C, Herrman H, Hegarty K, Gilchrist G, Griffiths F. A trajectory-based approach to understand the factors associated with persistent depressive symptoms in primary care. J Affect Disord. 2013;148:338–346. doi: 10.1016/j.jad.2012.12.021. [DOI] [PubMed] [Google Scholar]
- Henderson AS, Korten AE, Jacomb PA, MacKinnon AJ, Jorm AF, Christensen H, Rodgers B. The course of depression in the elderly: a longitudinal community-based study in Australia. Psychol Med. 1997;27:119–129. doi: 10.1017/s0033291796004199. [DOI] [PubMed] [Google Scholar]
- Jones B, Nagin D. Advances in group-based trajectory modeling and a SAS procedure for estimating them. Sociol Methods Res. 2007;35:542–571. [Google Scholar]
- Jones B, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374–393. [Google Scholar]
- Katon W, Unützer J, Russo J. Major depression: The importance of clinical characteristics and treatment response to prognosis. Depress Anxiety. 2010;27:19–26. doi: 10.1002/da.20613. [DOI] [PubMed] [Google Scholar]
- Katon WJ, Fan MY, Lin EH, Unützer J. Depressive symptom deterioration in a large primary care-based elderly cohort. Am J Geriatr Psychiatry. 2006;14:246–254. doi: 10.1097/01.JGP.0000196630.57751.44. [DOI] [PubMed] [Google Scholar]
- Kok RM, van Baarsen C, Nolen WA, Heeren TJ. Early response as predictor of final remission in elderly depressed patients. Int J Geriatr Psychiatry. 2009;24:1299–1303. doi: 10.1002/gps.2261. [DOI] [PubMed] [Google Scholar]
- Kuchibhatla MN, Fillenbaum GG, Hybels CF, Blazer DG. Trajectory classes of depressive symptoms in a community sample of older adults. Acta Psychiatr Scand. 2012;125:492–501. doi: 10.1111/j.1600-0447.2011.01801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landerman R, George LK, Campbell RT, Blazer DG. Alternative models of the stress buffering hypothesis. Am J Community Psychol. 1989;17(5):625–641. doi: 10.1007/BF00922639. [DOI] [PubMed] [Google Scholar]
- Lyness JM, Caine ED, King DA, Conwell Y, Duberstein PR, Cox C. Depressive disorders and symptoms in older primary care patients: One year outcomes. Am J Geriatr Psychiatry. 2002;10:275–282. [PubMed] [Google Scholar]
- Montagnier D, Dartigues JF, Rouillon F, Pérès K, Falissard B, Onen F. Ageing and trajectories of depressive symptoms in community-dwelling men and women. Int J Geriatr Psychiatry. 2014;29:720–729. doi: 10.1002/gps.4054. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Rhebergen D, Lamers F, Spijker J, de Graaf R, Beekman ATF, Penninx BWJH. Course trajectories of unipolar depressive disorders identified by latent class growth analysis. Psychol Med. 2012;42:1383–1396. doi: 10.1017/S0033291711002509. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff K. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Sharma VK, Copeland JRM, Dewey ME, Lowe D, Davidson I. Outcome of the depressed elderly living in the community in Liverpool: a 5-year follow-up. Psychol Med. 1998;28:1329–1337. doi: 10.1017/s0033291798007521. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Potter GG, McQuoid DR, MacFall JR, Payne ME, Burke JR, Plassman BL, Welsh-Bohmer KA. Longitudinal magnetic resonance imaging vascular changes, apolipoprotein E genotype, and development of dementia in the Neurocognitive Outcomes of Depression in the Elderly Study. Am J Geriatr Psychiatry. 2007;15:839–849. doi: 10.1097/JGP.0b013e318048a1a0. [DOI] [PubMed] [Google Scholar]
- Stek ML, van Exel E, van Tilberg W, Westendorp RGJ, Beekman ATF. The prognosis of depression in old age: outcome six to eight years after clinical treatment. Aging Ment Health. 2002;6:282–285. doi: 10.1080/13607860220142413. [DOI] [PubMed] [Google Scholar]
- Teo AR, Choi HJ, Valenstein M. Social relationships and depression: Ten-year follow-up from a nationally representative study. PlosOne. 2013;8:e62396. doi: 10.1371/journal.pone.0062396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uher R, Muthén B, Souery D, Mors O, Jaracz J, Placentino A, Petrovic A, Zobel A, Henigsberg N, Rietschel M, Aitchison KJ, Farmer A, McGuffin P. Trajectories of change in depression severity during treatment with antidepressants. Psychol Med. 2010;40:1367–1377. doi: 10.1017/S0033291709991528. [DOI] [PubMed] [Google Scholar]
- Zannas AS, McQuoid DR, Steffens DC, Chrousos GP, Taylor WD. Stressful life events, perceived stress, and 12-month course of geriatric depression: Direct effects and moderation by the 5-HTTLPR and COMT Val158Met polymorphisms. Stress. 2012;15:425–434. doi: 10.3109/10253890.2011.634263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beekman ATF, Deeg DJH, Smit JH, van Tilberg W. Predicting the course of depression in the older population: results from a community-based study in the Netherlands. J Affect Disord. 1995;34:41–49. doi: 10.1016/0165-0327(94)00103-g. [DOI] [PubMed] [Google Scholar]
- Beekman ATF, Geerlings SW, Deeg DJH, Smit JH, Schoevers RS, De Beurs E, Braam AW, Penninx BWJH, Van Tilberg W. The natural history of late-life depression. Arch Gen Psychiatry. 2002;59:605–611. doi: 10.1001/archpsyc.59.7.605. [DOI] [PubMed] [Google Scholar]
- Fillenbaum GG. Multidimensional Functional Assessment of Older Adults: The Duke Older Americans Resources and Services Procedures. Erlbaum; Hillsdale, N J: 1988. [Google Scholar]
- Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. The Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]