Introduction
Tranexamic acid (TXA) is a synthetic derivative of the amino acid, lysine. Conventionally used orally or intravenously, topical administration of TXA has the ability to reduce bleeding with minimal systemic absorption and, in turn, reduce the risk of systemic side effects. Previous clinical trials found that topical TXA reduces blood loss in cardiac, orthopedic, and otolaryngologic surgery.1 However, the hemostatic role of topical TXA for the skin has not been fully established. We describe a case of an elderly female with locally advanced basal cell carcinoma (BCC) of the scalp that was managed conservatively. The bleeding from the tumor was reduced with the aid of topical TXA.
Case report
A 96-year-old Chinese woman was first seen at our dermatology tertiary center 7 years ago. She presented with a growth on her right frontal scalp. She had a medical history of hypertension but was otherwise healthy. Apart from prolonged sun exposure when she was younger, she did not have any other significant risk factors for skin malignancies. On examination, there was a 3- × 2-cm pigmented plaque on the right frontal scalp with erosion. There was no lymphadenopathy. A skin biopsy was done, and histology confirmed the diagnosis of nodular BCC. Despite counseling the patient and her family regarding the risk of progression of the tumor without surgical treatment, they decided to opt for conservative management. She had regular wound dressing done by her family doctor but was subsequently lost to follow-up. She was admitted earlier this year to a nursing home because of severe dementia, and her family could not cope. On examination, the nodular BCC on her anterior scalp had increased in size and measured 6 × 4.5 cm with ulceration and bled easily on contact (Fig 1). Despite progression of the scalp BCC, her family declined any form of surgery or radiotherapy. Regular wound dressing was done at the nursing home with nonadherent lipidocolloid dressing with cadexomer iodine powder. However, the size of the tumor progressively increased over the next 3 months to 7 × 6 cm with increased vascularity and bleeding (Fig 2). This development was a cause for concern, as there was difficulty in wound dressing and the bleeding was affecting the patient adversely.
Fig 1.
May 2015. A 6- × 4.5-cm nodular BCC of the right anterior scalp.
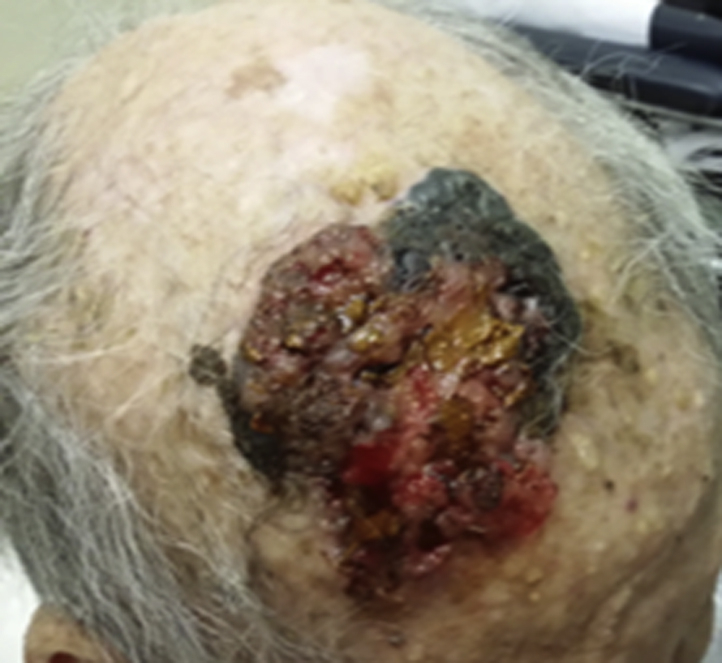
Fig 2.

August 2015. Increased size, vascularity, and bleeding of the scalp tumor.
To achieve hemostasis, 500 mg topical TXA (derived from crushed TXA tablets) was applied to the wound daily. After a month of applying topical tranexamic, the scalp tumor remained stable in size. Vascularity and bleeding of the tumor were significantly reduced (Fig 3). Wound dressing was continued with topical TXA, 500 mg once a day, and was eventually decreased to every other day with good hemostatic effect. No systemic side effects were encountered during the course of the treatment.
Fig 3.

September 2015. After 1 month of topical TXA, resulting in reduced vascularity and bleeding of the scalp tumor.
Discussion
Although there are topical curative therapies for patients with low-risk superficial BCC, such as 5-fluorouracil and imiquimod,2, 3 there is no evidence of these therapies being effective for locally advanced BCC. In our case, there are various medical and ethical complexities, such as the advanced nature of the disease, patient's cognitive decline, and her family decision for comfort care only. The primary aim in this case would be palliative wound care. Bleeding is a common and distressing symptom in these patients with advanced cutaneous malignancies, and this is usually caused by local vessel damage or invasion. Various modalities are described in the literature for local hemostasis of these patients with cutaneous malignancies such as dressings, cauterization, and radiotherapy.4 Our case describes the successful hemostasis of a bleeding skin malignancy using topical TXA as an alternative. The mechanism in which topical TXA helps in hemostasis is similar to its effects when administered systematically. TXA inhibits local fibrinolysis by blocking binding sites of plasminogen, preventing the conversion of plasminogen into plasmin.5 Topical TXA is efficacious in reducing blood loss in surgeries such as knee arthroplasties and cardiac and otolaryngologic surgery.6, 7, 8 In terms of safety profile, a recent meta-analysis of these studies involving topical TXA did not show increased risk of thromboembolic events such as myocardial infarction, stroke, pulmonary embolism, or deep vein thrombosis compared with the control groups involved.1
Topical TXA is a promising therapeutic option for the hemostasis of locally advanced BCC or other skin malignancies, especially with palliative intent in patients who are unsuitable for surgery or radiotherapy. This observation underlines the need for larger studies to evaluate the efficacy and safety of topical TXA as an adjunct to control bleeding of tumors.
Acknowledgments
The authors thank the staff of Villa Francis Home of the Aged, Singapore.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Ker K., Beecher D., Roberts I. Topical application of tranexamic acid for the reduction of bleeding. Cochrane Database Syst Rev. 2013;(7):CD010562. doi: 10.1002/14651858.CD010562.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gross K., Kircik L., Kricorian G. 5% 5-Fluorouracil cream for the treatment of small superficial basal cell carcinoma: efficacy, tolerability, cosmetic outcome, and patient satisfaction. Dermatol Surg. 2007;33:433–439. doi: 10.1111/j.1524-4725.2007.33090.x. [DOI] [PubMed] [Google Scholar]
- 3.Quirk C., Gebauer K., De'Ambrosis B., Slade H.B., Meng T.C. Sustained clearance of superficial basal cell carcinomas treated with imiquimod cream 5%: results of a prospective 5-year study. Cutis. 2010;85(6):318–324. [PubMed] [Google Scholar]
- 4.Pereira J., Phan T. Management of bleeding in patients with advanced cancer. Oncologist. 2004;9(5):561–570. doi: 10.1634/theoncologist.9-5-561. [DOI] [PubMed] [Google Scholar]
- 5.Cesarman-Maus G., Hajjar K. Molecular mechanisms of fibrinolysis. Br J Haematol. 2005;129(3):307–321. doi: 10.1111/j.1365-2141.2005.05444.x. [DOI] [PubMed] [Google Scholar]
- 6.Alshryda S., Mason J., Sarda P. Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total knee replacement: a randomised controlled trial (TRANX-K) J Bone Joint Surg Am. 2013;95(21):1961–1968. doi: 10.2106/JBJS.L.00907. [DOI] [PubMed] [Google Scholar]
- 7.Albirmawy O.A., Saafan M.E., Shehata E.M., Basuni A.S., Eldaba A.A. Topical application of tranexamic acid after adenoidectomy: a double-blind, prospective, randomized, controlled study. Int J Pediatr Otorhinolaryngol. 2013;77(7):1139–1142. doi: 10.1016/j.ijporl.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 8.Abul-Azm A., Abdullah K.M. Effect of topical tranexamic acid in open heart surgery. Eur J Anaesthesiol. 2006;23(5):380–384. doi: 10.1017/S0265021505001894. [DOI] [PubMed] [Google Scholar]


