Abstract
Background/Objectives
Geriatricians may be more effective and efficient in their management of elderly patients than other physicians. This study compared patient outcomes and measures of efficiency for hospitalized elderly patients managed by geriatricians and other physicians.
Design
Secondary data analysis using a system that integrates clinical and financial information for inpatient and outpatient services delivered throughout the University of Pittsburgh Medical Center (UPMC). Propensity scores were developed based on patient socio-demographic and clinical characteristics and used to match patients based on the attending physician’s specialty (a geriatrician (n=701) or a non-geriatrician (n=11,549)). Multivariate analyses using generalized estimating equations methods were performed.
Setting
Two UPMC hospitals in Pittsburgh, PA.
Participants
Patients age 65 and older who were admitted in 2002 and had a medical diagnosis related group (DRG).
Measurements
Patient outcomes (inpatient mortality, 30-day mortality, readmissions) and efficiency measures (length of stay, total costs and surplus, which is the difference between hospital costs and payment received for an admission).
Results
Elderly patients managed by geriatricians were significantly older (p<.01), more likely to be male (p<.01), and had a higher number of diagnoses (p<.01). Propensity scores successfully balanced patient characteristics managed by the two groups. Patients of geriatricians had lower inpatient mortality (p=.04), shorter length of stay (p<.01), lower costs per admission (p<.01) and greater surplus (p<.01). In multivariate analyses, there were not significant differences in patient outcomes, but patients of geriatricians had significantly shorter length of stay, lower costs per admission and generated more surplus for the hospitals.
Conclusion
Geriatricians were more efficient than other PCPs in managing hospitalized elderly patients with medical DRGs frequently managed by geriatricians. This efficiency did not compromise patient outcomes.
Keywords: quality of care, efficiency, geriatric medicine
INTRODUCTION
The Medicare system is on the brink of crisis. Medicare spending is expected to grow by 6.4% annually from 2008 through 2018(1) and, as a share of GDP, it is projected to double from 3.2 percent in 2008 to 6.4 percent by 2030(2) In part, this growth is due to aging of the “baby boomers”, whose 79 million members will roughly double the number of Medicare eligible Americans by 2030(1) and comprise 20 percent of the United States population. Moreover, the fastest growing segment of this population will be those over age 85, whose per capita Medicare expenditures are double those of people aged 65–74.(1) The 2011 Annual Report of the Board of Trustees projected that Medicare will not be insolvent until 2024, but this estimate is predicated on the unlikely assumption that Medicare payments for physician services will be reduced by approximately 30% in 2012.(3)
In addition to concerns about rising costs, there is concern about health care quality. McGlynn and colleagues demonstrated that patients receive only about 55 percent of guideline recommended care for their conditions.(4) While the rate for community dwelling elderly is similar, the quality of care for geriatric conditions is lower than that provided for general medical conditions.(5)
A major goal of health care reform is to identify ways to control costs while maintaining or improving the quality of care. One approach might be to increase the number of geriatricians, physicians trained to care for older patients. Currently, there are only about 7,000 physicians with active certification in geriatric medicine, and fewer than 4 certified geriatricians in the United States per 10,000 people age 75 and older.(6) Moreover, the ratio is deteriorating because <1% of graduates from US medical schools choose geriatrics as a career focus and almost half of geriatrics training slots go unfilled.(6)
Among the many reasons for the dearth of geriatricians is the belief that geriatric practices lose money and require financial support.(7) This reflects the fact that geriatricians generally care for patients who are older, have more comorbidity, and are more likely to have impairments of cognition and mood and thus require more time and resources to care for than the average Medicare patient. Yet, reimbursement for such patients is not commensurate with the increased cost. Thus, hospitals have traditionally subsidized geriatrics practices. Some have suggested that “downstream revenue” more than offsets such subsidy,(8, 9) but it is unclear whether downstream revenue exceeds the associated cost and, with hospitals under increased pressure to cut costs, it becomes increasingly important to examine the fiscal aspect of geriatrics.
Due to their training, geriatricians may be more effective and efficient in managing elderly patients. While the medical approach to younger patients is generally (and appropriately) reactive, addressing symptoms as they appear, the geriatric approach is more proactive in patient assessment and management, aiming to identify each patient’s risk factors early and address them before they result in additional problems and deterioration. Although the literature shows that geriatricians are less likely to prescribe inappropriate medications to the elderly, (10) there are few studies documenting that geriatricians provide higher quality care and still fewer that examine the resulting financial component of such care
To fully understand the impact of geriatrics, it is important to look at care across all settings. To date, the focus has been primarily on outpatient geriatric clinics. However, it is possible that the financial losses in the outpatient setting are offset by reduced utilization of other costly healthcare resources (e.g., emergency room visits and hospital admissions). While these will become increasingly important with changes in healthcare financing, the vast majority of older adults remain in the fee for service setting. Thus, the purpose of this study was to compare patient outcomes and measures of efficiency for hospitalized patients managed by geriatricians and other specialties of attending physicians. The inpatient services represent approximately 30 percent of all health care costs,(1) the largest proportion for a single setting. Our hypotheses were that having a geriatrician as the attending physicians for elderly patient in the hospital would result in: 1) reduced length of stay, 2) less costly admissions, 3) fewer readmissions, 4) better patient outcomes. Each of these is important, regardless of whether the setting is fee for service or managed care.
METHODS
Study Population
The study sample comprised a cohort of patients discharged from January 1st, 2002 to December 31st, 2002 from two hospitals in Pittsburgh, Pennsylvania that are part of the University of Pittsburgh Medical Center (UPMC). One hospital is a large academic medical center that utilized a hospitalist model for both geriatricians and non-geriatricians, while the other is a large affiliated community hospital that utilized a more traditional non-hospitalist model for both geriatricians and non-geriatricians. This time period was selected because it was prior to a change in the health system that resulted in very different models at the two hospitals that would no longer permit the comparisons that were the focus of this study. Subsequent to this time period, there has been much more cross over between physicians at the two hospitals and cultural integration as a result of mergers in the health system. Thus, in more recent data, it is more difficult to analytically discern the effect of the geriatrician attending physician.
All patients included were 65 years or older at the time of admission and had a medical diagnosis related group (DRG) as identified on the Medicare website. The admissions with a DRG 014 (specific cerebrovascular disorders except transient ischemic attacks) were excluded from the analysis as they were treated by a separate group of attending physicians. The analysis also excluded patients participating in clinical research. We further limited our analyses to those patients who had as their attending either a board-certified geriatrician or another primary care physician certified in either internal medicine or family practice. This was done because multiple DRGs common among the specialists’ patients were uncommon among the geriatricians’ and primary care physicians’ patients (e.g. cardiac catheterization), thus limiting our ability to adequately control for these differences in the analyses.
Data Sources
The data were extracted from the UPMC’s Medical Archival System (MARS), which was developed in 1987 to improve health care by integrating the computer systems that supported medical care. The MARS system captures information on all patients seen at UPMC hospitals and long-term care facilities and at most physician offices and outpatient clinics, including laboratory and radiology data. All records obtained on a single patient at any given time are linked via a unique patient identifier. Patients who cross facilities or billing areas are linked through a Master Patient Index maintained in an OracleTM database. In addition, a minimum of three demographic items are stored with each record. This strengthens linkages and facilitates searching for common patient characteristics within clinical and financial records. A second, logically separated MARS database stores financial transactions that can be combined with corresponding clinical data.(11) Data for this study included information for each admission on patient demographics, health insurance status, clinical diagnoses (verified by electronic chart review), payment, and total costs.
Outcome Measures
There were seven outcomes included in the study. The three patient outcomes included inhospital mortality, 30-day mortality, and readmission within 30 days after discharge to any of UPMC’s 12 hospitals, which represent two-thirds of the hospitals in the Pittsburgh metropolitan area. The four measures of cost and efficiency were length of stay, total cost for the admission, cost per day, and surplus from the cost of the hospital stay for the admission. 30-day mortality was defined as death within 30 days of the discharge date. Costs were defined as the dollar amount of resources utilized to provide all aspects of patient care including direct and indirect costs. Hospital costs excluded physicians' fees. Costs were calculated using the ratio of cost-to-charge (RCC) for the patients' charges in a given department. In our institution, RCCs are updated each fiscal year. A step-down method is used to allocate indirect costs to direct cost centers. In this method, the indirect department that receives the least amount of services from other indirect departments and provides the most service to other departments allocates its costs first. A similar analysis is conducted to determine the order of cost allocation for each remaining indirect department. Overhead costs are allocated based on specific statistics. For example housekeeping costs are allocated to other cost centers based on square footage, while billing department costs are allocated based on gross charges. The methodology used was validated in 2002 at one of the study hospitals.(12) Cost per day was calculated as total cost divided by length of stay. Surplus was defined as the difference between payment received by the hospital for the admission and total costs for the admission.
Main Independent Variable
The variable of interest was the specialty of the attending physician for the hospital stay. An attending physician was classified as a geriatrician if she/he completed a fellowship in geriatric medicine.
Covariates
Covariates were used to control for factors that may affect the outcomes, including age, gender, race, marital status, health insurance status, geographic area, major comorbidities, the number of diagnoses at admission, hospital where admitted, being transferred from other hospitals, admission type, being a readmission, and season of admission. The measure of comorbidity used was the modified Charlson Comorbidity Index(13) to which we added comorbidities that are common among geriatric populations, including falls, malnutrition, delirium, dehydration, anemia, fractures, and selected psychiatric diagnoses.1 Instead of using a comorbidity score to represent conditions identified in the data in the year prior to the admission, an indicator variable for each comorbidity in the modified Charlson Comorbidity Index was used because different comorbidities may affect outcomes differently. In addition, the number of diagnoses at discharge was used to capture patient severity. Patients transferred from other hospitals tend to be sicker and an indicator for transfer status was entered in the models. We also included an indicator for being admitted from a nursing home. Three admission types were included: elective, urgent, and emergent. Being a readmission was defined as an admission with a prior hospital admission within 30 days of the current discharge date.
Statistical Analysis
Descriptive analysis was conducted between the outcomes, covariates, and the exposure, whether a patient was cared by a geriatrician. Pearson’s chi-square tests and t tests were performed for categorical variables and continuous variables, respectively.
A propensity score matching was performed between admissions cared for by a geriatrician (geriatrician admission) and those cared for by other physicians (non-geriatrician admission) so that the two groups were balanced in the observed variables. First, a propensity score was predicted for each admission based on a GEE model on whether the attending physician of an admission was a geriatrician, using a logit link and a binomial family. The independent variables included the set of covariates listed above. Each geriatrician admission was then matched to a non-geriatrician admission with the closest propensity score to that of the geriatrician admission. If there were several non-geriatrician admissions with the closest propensity score to that of a geriatrician admission, one non-geriatrician admission was randomly selected. Once a non-geriatrician admission was matched, it was removed from the matching process. After the propensity score matching, the balance between geriatrician admissions and the matched non-geriatrician admissions were checked for all the covariates.
Four regression analyses were carried out: regression not adjusting for other covariates, regression controlling for the aforementioned covariates, regression based on the admissions matched by propensity score and adjusting for the covariates remaining unbalanced after matching, and regression controlling for the deciles of propensity score and the set of covariates. All the regression models incorporated the lack of independence between admissions of the same patient using generalized estimating equations (GEE) with appropriate link functions, distribution families, and an exchangeable working correlation structure.(14, 15) A logit link and a binomial family were used for in-hospital mortality, 30-day mortality, and readmission within 30 days, while length of stay, total cost of an admission, and cost per day were modeled using a log link and a Gaussian family as the distributions of these two outcomes were skewed to the right. An identity link and a Guassian family were employed to model surplus.
Marginal effects of having a geriatrician as the attending physician on length of stay, total cost, and surplus, were computed to ease the interpretation. The standard errors of marginal effects were calculated using the delta method.(16) A significance level of 0.05 was adopted for all the statistical inferences. All the analyses were conducted using STATA Version 10 (StataCorp LP, College Station, Texas).
A number of sensitivity analyses were conducted to evaluate the robustness of the results. Since some patients had long length of stays, we repeated analyses excluding those with a length of stay greater than 30 days. Because of concerns that inpatient deaths could be driving length of stay results, we conducted a time to discharge analysis using Cox-proportional hazard models to censor those who died in the hospital. We also repeated the length of stay, total cost, cost per day, and surplus analyses excluding the subset of the sample that died in the hospital. To explore the possibility that those admitted from the nursing home could influence results beyond what was controlled for in the propensity score and multivariate analyses, we ran sensitivity analyses excluding these individuals. Our results were robust to these sensitivity analyses. We report the results that include those patients who died in the hospital or were admitted from a nursing home, but exclude those with length of stay greater than 30 days, which were more common among patients who did not have a geriatrician as their attending physician.
RESULTS
Our sample included 701 patients who had a geriatrician as their attending physician and 5,600 patients whose attending physician was a non-geriatric primary care physician. Compared to the primary care physicians’ patients, the geriatricians’ patients were significantly older, less likely to be male, less likely to be black or another minority, less likely to be married and more likely to reside in Allegheny County (Table 1). They had a significantly higher number of comorbid conditions in the year prior to their admission, particularly geriatric conditions, and more diagnoses while in the hospital. The geriatricians’ patients were also significantly less likely to be received in transfer from another hospital, and more likely to be admitted from a nursing home. In bivariate analyses, the geriatricians’ patients had significantly shorter average length of stay, lower costs per admission, greater costs per day and larger surplus than the primary care physicians’ patients (Table 2). There were not significant differences in the percent readmitted within 30 days, in-hospital mortality or 30 day mortality. Nine of the ten most frequent DRGs were identical between the two groups. The 10 most frequent DRGs captured 47 percent of the geriatricians’ patients and 44 percent of the primary care physicians’ patients (Table 3).
Table 1.
Patient Demographic and Clinical Characteristics before Propensity Score Matching ┼
| Characteristics | Patients Cared by Geriatricians (n=701) | Patients Cared by Primary Care Physicians (n=5,600) | P Value |
|---|---|---|---|
| Age, median (range), years | 84(65–99) | 79(65–99) | <0.01 |
| Age, mean (± SD), years | 82.98(6.97) | 78.91(7.73) | <0.01 |
| Male, N (%) | 191(27) | 1,986(35) | <0.01 |
| Race, N (%) | |||
| White | 566(81) | 4,077(73) | <0.01 |
| Black | 128(18) | 1,388(25) | <0.01 |
| Other or unknown | 7(1) | 135(2) | 0.02 |
| Married, N (%) | 227(32) | 2,108(38) | 0.01 |
| Modified Charlson Comorbidity | 2(0–11) | 2(0–13) | 0.04 |
| Index, median (range) | |||
| Modified Charlson Comorbidity | 2.62(1.81) | 2.44(1.93) | 0.02 |
| Index, mean (± SD) | |||
| Number of diagnoses, median (range) | 8(1–25) | 7(1–25) | <0.01 |
| Number of diagnoses, mean (±SD) | 8.64(3.58) | 7.8(3.48) | <0.01 |
| Comorbidities, N. (%) | |||
| Myocardial infarction | 109(16) | 799(14) | 0.36 |
| Congestive heart failure | 194(28) | 1,681(30) | 0.20 |
| Peripheral vascular disease | 39(6) | 366(7) | 0.32 |
| Cerebrovascular disease | 83(12) | 533(10) | 0.05 |
| Dementia | 38(5) | 110(2) | <0.01 |
| Chronic pulmonary disease | 159(23) | 1,722(31) | <0.01 |
| Rheumatologic disease | 18(3) | 155(3) | 0.76 |
| Peptic ulcer disease | 11(2) | 168(3) | 0.03 |
| Mild liver disease | 7(1) | 98(2) | 0.14 |
| Diabetes | 142(20) | 1,453(26) | <0.01 |
| Diabetes with complications | 21(3) | 219(4) | 0.23 |
| Hemiplegia | 2(0) | 35(1) | 0.27 |
| Renal disease | 14(2) | 186(3) | 0.06 |
| Any malignancy | 42(6) | 377(7) | 0.46 |
| Metastatic tumor | 21(3) | 177(3) | 0.81 |
| Severe liver disease | 2(0) | 52(1) | 0.08 |
| HIV and Aids | 0(0) | 1(0) | 0.72 |
| Falls | 71(10) | 464(8) | 0.10 |
| Malnutrition | 75(11) | 323(6) | <0.01 |
| Delirium | 107(15) | 267(5) | <0.01 |
| Dehydration | 238(34) | 1,580(28) | <0.01 |
| Anemia | 195(28) | 1,205(22) | <0.01 |
| Fractures | 31(4) | 97(2) | <0.01 |
| Psychiatric disorders | 72(10) | 234(4) | <0.01 |
| Hospital transfer, N. (%) | 16(2) | 270(5) | <0.01 |
| Admission from nursing home, | 217(31) | 1,081(19) | <0.01 |
| N. (%) | |||
| Being a readmission, N. (%) | 108(15) | 936(17) | 0.38 |
| Admission Type, N. (%) | |||
| Elective | 28(4) | 136(2) | 0.01 |
| Urgent | 58(8) | 813(15) | <0.01 |
| Emergent | 615(88) | 4,651(83) | <0.01 |
| Season of Admission, N. (%) | |||
| Spring | 184(26) | 1,378(25) | 0.34 |
| Summer | 146(21) | 1,314(23) | 0.12 |
| Fall | 178(25) | 1,418(25) | 0.97 |
| Winter | 193(28) | 1,490(27) | 0.60 |
| Primary Insurance, N. (%) | |||
| Medicare | 546(78) | 3,838(69) | <0.01 |
| Medicare Advantage | 126(18) | 1,425(25) | <0.01 |
| Medicaid | 2(0) | 33(1) | 0.31 |
| Medicaid HMO | 6(1) | 34(1) | 0.43 |
| Private | 17(2) | 238(4) | 0.02 |
| Self-pay | 4(1) | 32(1) | 1.00 |
| Geographic area, N. (%) | |||
| Allegheny County | 650(93) | 5,011(89) | 0.01 |
| The rest of the MSA | 33(5) | 335(6) | 0.17 |
| Outside the MSA | 18(3) | 254(5) | 0.02 |
The characteristics are at the admission level.
Table 2.
Patient Outcomes Before Propensity Score Matching ┼
| Outcome | Patients Cared by Geriatricians (n=701) | Patients Cared by Primary Care Physicians (n=5,600) | P Value |
|---|---|---|---|
| Length of Stay, median (range), days | 3(1–27) | 4(1–30) | <0.01 |
| Length of Stay, mean (± SD) | 4.13(3.25) | 4.9(3.83) | <0.01 |
| Readmission within 30 days, N. (%) | 109(16) | 993(18) | 0.15 |
| In-hospital mortality, N. (%) | 24(3) | 258(5) | 0.15 |
| 30-day mortality | 77(11) | 610(11) | 0.94 |
| Cost, median (range), US $ | 3,812(614–53,556) | 4,242(195–92,445) | 0.01 |
| Cost, mean (± SD) | 5,163(5,137) | 5,913(5,723) | <0.01 |
| Cost per day, median (range), US $ | 1,178(540–4,549) | 1,133(39–12,465) | <0.01 |
| Cost per day, mean (± SD), US $ | 1,314(495) | 1,268(532) | 0.03 |
| Net revenue, median (range), US $ | 717(-53,556-47,301) | 98(-73,473–62,659) | <0.01 |
| Net revenue, mean (± SD) | 590(4,807) | −220(4,239) | <0.01 |
The characteristics are at the admission level.
Table 3.
10 Most Common DRGs in Sample
| Geriatrician | Other Primary Care | ||
|---|---|---|---|
| DRG | % | DRG | % |
| Heart failure and shock | 8.1% | Heart failure and shock | 9.8% |
| Simple pneumonia & pleurisy; age>17 w/ complications, comorbidities | 7.1% | Simple pneumonia & pleurisy; age>17 w/ complications, comorbidities | 5.4% |
| Nutritional & miscellaneous metabolic disorders | 5.7% | Nutritional & miscellaneous metabolic disorders | 5.3% |
| Respiratory infections & inflammations | 5.1% | Esophagitis, gastroenteritis & miscellaneous digestive disorders, age >17 w/ complications, comorbidities | 4.1% |
| GI hemorrhage w/ complications, comorbidities | 4.7% | GI hemorrhage w/ complications, comorbidities | 3.9% |
| Chronic obstructive pulmonary disease | 4.0% | Kidney & urinary tract infections; age >17 w/ complications, comorbidities | 3.8% |
| Kidney & urinary tract infections; age >17 w/ complications, comorbidities | 4.0% | Chronic obstructive pulmonary disease | 3.7% |
| Cardiac arrhythmia & conduction disorder w/ complications, comorbidities | 3.3% | Respiratory infections & inflammations | 3.2% |
| Esophagitis, gastroenteritis & miscellaneous digestive disorders, age >17 w/ complications, comorbidities | 3.0% | Cardiac arrhythmia & conduction disorder w/ complications, comorbidities | 2.6% |
| Cellulitis age >17 w/ complications, comorbidities | 2.0% | Septicemia age >17 | 2.1% |
| Total for top 10 DRGs | 47.1% | 43.8% |
The propensity score matching eliminated the demographic differences in the patient population (online appendix), with the exception of the percent married. The geriatricians’ patients still had more comorbidities on average, particularly delirium and psychiatric diagnoses. Differences in average length of stay cost per admission, cost per day and surplus remained significant after propensity score matching.
Appendix.
Patient Demographic and Clinical Characteristics after Propensity Score Matching ┼
| Characteristics | Patients Cared by Geriatricians (n=701) | Patients Cared by Primary Care Physicians (n=701) | P Value |
|---|---|---|---|
| Age, median (range), years | 84(65–99) | 84(65–99) | 1.00 |
| Age, mean (± SD), years | 82.98(6.97) | 83.36(7.08) | 0.31 |
| Male, N (%) | 191(27) | 178(25) | 0.43 |
| Race, N (%) | |||
| White | 566(81) | 577(82) | 0.45 |
| Black | 128(18) | 118(17) | 0.48 |
| Other or unknown | 7(1) | 6(1) | 0.78 |
| Married, N (%) | 227(32) | 187(27) | 0.02 |
| Modified Charlson Comorbidity | 2(0–11) | 2(0–12) | 0.45 |
| Index, median (range) | |||
| Modified Charlson Comorbidity | 2.62(1.81) | 2.42(1.77) | 0.03 |
| Index, mean (± SD) | |||
| Number of diagnosis, median (range) | 8(1–25) | 8(1–24) | 0.03 |
| Number of diagnosis, mean (±SD) | 8.64(3.58) | 8.32(3.53) | 0.09 |
| Comorbidities, N (%) | |||
| Myocardial infarction | 109(16) | 88(13) | 0.11 |
| Congestive heart failure | 194(28) | 224(32) | 0.08 |
| Peripheral vascular disease | 39(6) | 51(7) | 0.19 |
| Cerebrovascular disease | 83(12) | 72(10) | 0.35 |
| Dementia | 38(5) | 30(4) | 0.32 |
| Chronic pulmonary disease | 159(23) | 169(24) | 0.53 |
| Rheumatologic disease | 18(3) | 23(3) | 0.43 |
| Peptic ulcer disease | 11(2) | 16(2) | 0.33 |
| Mild liver disease | 7(1) | 7(1) | 1.00 |
| Diabetes | 142(20) | 151(22) | 0.55 |
| Diabetes with complications | 21(3) | 8(1) | 0.01 |
| Hemiplegia | 2(0) | 2(0) | 1.00 |
| Renal disease | 14(2) | 21(3) | 0.23 |
| Any malignancy | 42(6) | 39(6) | 0.73 |
| Metastatic tumor | 21(3) | 10(1) | 0.05 |
| Severe liver disease | 2(0) | 2(0) | 1.00 |
| HIV and Aids | 0(0) | 1(0) | 0.32 |
| Falls | 71(10) | 67(10) | 0.72 |
| Malnutrition | 75(11) | 70(10) | 0.66 |
| Delirium | 107(15) | 73(10) | 0.01 |
| Dehydration | 238(34) | 229(33) | 0.61 |
| Anemia | 195(28) | 190(27) | 0.76 |
| Fractures | 31(4) | 31(4) | 1.00 |
| Psychiatric disorders | 72(10) | 43(6) | <0.01 |
| Hospital transfer, N (%) | 16(2) | 19(3) | 0.61 |
| Admission from nursing home, N (%) | 217(31) | 218(31) | 0.95 |
| Being a readmission, N (%) | 108(15) | 102(15) | 0.65 |
| Admission Type, N (%) | |||
| Elective | 28(4) | 25(4) | 0.67 |
| Urgent | 58(8) | 68(10) | 0.35 |
| Emergent | 615(88) | 608(87) | 0.58 |
| Season of Admission, N (%) | |||
| Spring | 184(26) | 162(23) | 0.17 |
| Summer | 146(21) | 159(23) | 0.40 |
| Fall | 178(25) | 195(28) | 0.30 |
| Winter | 193(28) | 185(26) | 0.63 |
| Primary Insurance, N (%) | |||
| Medicare | 546(78) | 551(79) | 0.75 |
| Medicare Advantage | 126(18) | 128(18) | 0.89 |
| Medicaid | 2(0) | 2(0) | 1.00 |
| Medicaid HMO | 6(1) | 1(0) | 0.06 |
| Private | 17(2) | 15(2) | 0.72 |
| Self-pay | 4(1) | 4(1) | 1.00 |
| Geographic area, N (%) | |||
| Allegheny County | 650(93) | 657(94) | 0.46 |
| The rest of the MSA | 33(5) | 30(4) | 0.70 |
| Outside the MSA | 18(3) | 14(2) | 0.47 |
| Length of Stay, median (range), days | 3(1–27) | 4(1–24) | <0.01 |
| Length of Stay, mean (± SD) | 4.13(3.25) | 5.17(4.07) | <0.01 |
| Readmission within 30 days, N (%) | 109(16) | 122(17) | 0.35 |
| In-hospital mortality, N (%) | 24(3) | 34(5) | 0.18 |
| 30-day mortality | 77(11) | 89(13) | 0.32 |
| Cost, median (range), US $ | 3,812(614–53,556) | 4,340(520–44,649) | 0.02 |
| Cost, mean (± SD) | 5,163(5,137) | 6,027(5,299) | <0.01 |
| Cost per day, median (range), US $ | 1,178(540–4,549) | 1,112(168–12,465) | <0.01 |
| Cost per day, mean (± SD), US $ | 1,314(495) | 1,247(617) | 0.02 |
| Net revenue, median (range), US $ | 717(−53,556−47,301) | 256(−24,452−21,327) | 0.03 |
| Net revenue, mean (± SD) | 590(4,807) | −256(4,243) | <0.01 |
The characteristics are at the admission level.
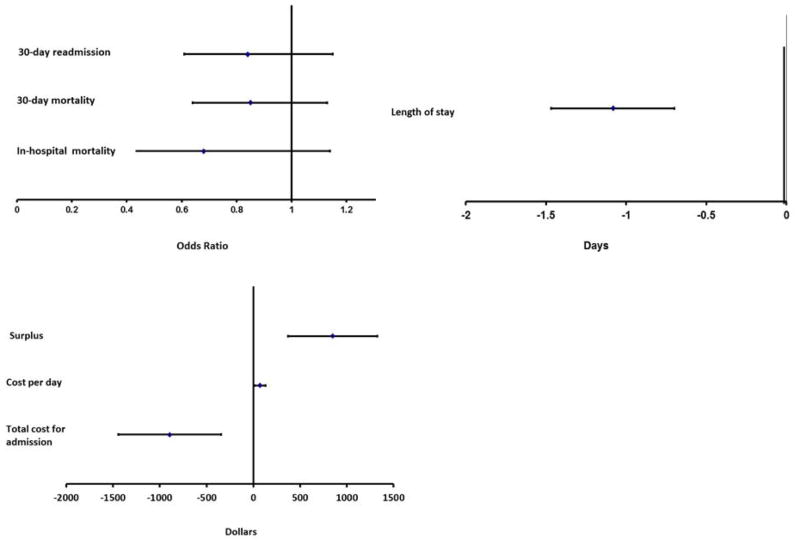
Figures 1a though 1c present the multivariate analyses results comparing the effect of having a geriatrician instead of a primary care specialty physician as the attending physician. The results are presented for each of the outcomes assessed. We present the results for the propensity score matching method; the other analytic approach produced substantively similar results. While not reaching statistical significance the geriatricians’ patients had lower in-hospital mortality, lower 30-day mortality, and were less likely to be readmitted within 30 days. The average length of stay for the geriatrician’s patients was an estimated 1.1 days shorter. The total cost of admission for each patient of the geriatricians was $895 less than that for each patient of the primary care physicians. There was less consistency in estimates for the cost per day between the estimation approaches than for other outcomes. Two modeling approaches showed no significant differences while the matched pairs approach suggested that geriatricians had higher daily costs. Compared to primary care specialties, having a geriatrician as the attending physician was associated with a greater surplus for the hospital ($850 per admission).
Figure 1. Marginal Effect of Geriatricians on Mortality, Length of Stay and Readmissions.
Figure 1a. Marginal Effect of Geriatricians on Readmissions and Mortality
Figure 1b. Marginal Effect of Geriatricians on Hospital Length of Stay
Figure 1c. Marginal Effect of Geriatricians on Financial Measures
DISCUSSION
This study examined clinical and financial outcomes for patients admitted to two hospitals in Pittsburgh, PA in 2002 and assessed whether having a geriatrician as the attending physician was associated with patient outcomes. We found that, as compared to patients of a non-geriatrician, patients of a geriatrician experienced shorter lengths of stay and lower costs without an adverse impact on outcomes for DRGs frequently managed by primary care physicians and geriatricians. In fact, although not statistically significant, outcomes for patients of geriatricians tended to be superior. The lower costs appeared to be completely driven by shorter length of stay rather than by lower per day costs. Thus, method of hospital reimbursement will determine whether savings from shorter length of stay benefit the hospital (DRGs), payer (per diem), or integrated delivery system, accountable care organization, or other provider organization (capitation, episodes of care or other bundled payments). The study design did not permit assessment of the impact of such care on functional status. These findings are consistent with the literature on inpatient geriatric evaluation, which shows shorter length of stay compared to being managed by general internists,(17) greater improvements in function and a greater likelihood of discharge to home.(18, 19)
These analyses do not provide information on the mechanisms by which geriatricians achieve these results. One possibility is that patients of geriatricians are more likely to be admitted from the nursing home, which must hold their bed for 15 days. This facilitates discharge back to the nursing home and could reduce their length of stay relative to other patients being discharged to a nursing home. While we did find that the patients of geriatricians were more likely to be admitted from the nursing home, this did not explain the observed results. First, the patients admitted from nursing homes had a longer average length of stay than those admitted from the community. In addition, our results were robust to excluding from the multivariate analyses those patients admitted from nursing homes (data not shown).
A second possible explanation for our findings is that geriatricians identify diagnoses that are frequently not looked for or are missed by doctors without geriatric training and, by recognizing these problems, it is possible to avoid or mitigate declines in elder hospitalized patients and thus shorten length of stay. In our sample, patients who had geriatricians as their attending physician were more likely to be diagnosed with malnutrition, delirium, anemia, dehydration, and psychiatric problems. These diagnoses were included in the calculation of propensity scores and multivariate analyses. It is possible that these differences in diagnoses were due to systematic differences in assessment and coding practices rather than true differences in disease burden. If this is the case, our multivariate analyses potentially over adjusted for differences in case-mix, but similar results were observed when such adjustments were not included.
Many of the patients managed by geriatricians in the hospital were also managed by them in the outpatient setting. Although this is also the case for patients of non-geriatricians, it is possible that the patients of the geriatricians are better managed in the outpatient setting and thus experience fewer complications in the hospital. Alternatively, shorter hospitalization may occur if geriatricians focus on the primary reason a patient is hospitalized and request fewer tests and consultations than do other physicians, either because they prefer doing them in the outpatient setting or because they may lead to procedures inconsistent with patient preferences.
This study has several strengths. It included every patient over age 65 years who was discharged from two large hospitals for a full year. It included both a large academic, referral-based hospital, which utilized a hospitalist model for both geriatricians and non-geriatricians, and a large community-based hospital, which utilized a more traditional, non-hospitalist model for geriatricians and non-geriatricians. The results are strengthened by their consistency across both hospitals and models and by the use of propensity adjustment for clinical status as well as adjustment for other potential confounders. The study also has a number of limitations. First, it included only two hospitals. As such, the results may not be generalizable to hospitals in other communities. Second, we excluded patients referred for specialist care (e.g. cardiac catheterization or stent placement), which are not commonly handled by generalists (geriatricians or non-geriatricians), which could limit the generalizability of our results. Third, we captured only readmissions to the original hospital or another UMPC hospital, which comprise two-thirds of the hospitals in the Pittsburgh area. Based on national Medicare data about the site of rehospitalizations,(20) we estimate that we capture at least 90 percent of readmissions. Fourth, the data are from 2002. This time period was selected because it was prior to one of the hospital’s complete integration into the UPMC health system, which would greatly complicate the opportunity to examine consistency across the two hospitals and models.
It should be noted that this analysis is likely an underestimate of the true value of geriatricians to society. This study was limited to the inpatient setting, focusing on patients over age 65 who were admitted to the hospital. It does not capture whether geriatricians are better able to prevent hospitalizations among complex elderly patients nor does it assess whether geriatricians are better able to maintain the functional status of their patients than other provider specialties. Geriatricians experience adverse selection in their patients in the outpatient setting, providing care to elderly patients who are complex, have high needs and are high cost, while more functional elderly patients continue to receive care from internists and other physician specialties. As a result, the throughput in geriatric practices is low and the overhead is high as structures are put into place to meet the needs of their patients. While outpatient geriatric clinics have been shown to produce favorable patient outcomes(21–23), they frequently do not break even financially (9, 24); Thus, geriatrics outpatient practices are frequently subsidized by hospitals which are increasingly interested in knowing the value of this investment. Because many studies focus on downstream revenue rather than on net revenue, it is not clear whether the hospital made or lost money. This study shows that, as compared with non-geriatrician primary care providers, geriatricians generate a greater surplus for the hospital by successfully reducing length of stay without compromising patient outcomes. It thus may contribute useful information in beginning to construct a more comprehensive business model for geriatrics. While surplus from inpatient admissions can offset the costs of the outpatient clinics, however, it remains unknown whether it does so completely.
Acknowledgments
We thank Anna Marano, MHA, MBA and David W. Young, DBA for their assistance in the development of the methodology to calculate hospital costs and surplus and review of the initial study findings.
This work was supported in part by funding by the Jewish Healthcare Foundation and the RAND-University of Pittsburgh Health Institute (RUPHI), both in Pittsburgh, PA
Footnotes
A complete list of ICD-9 diagnosis codes used to identify these conditions is available from the authors upon request.
Presented at the 2010 AcademyHealth Annual Research Meeting
Conflict of Interest Disclosures:
| Elements of Financial/Personal Conflicts |
* Author 1 MES |
Author 2 MIS |
Author 3 HL |
Author 4 NMR |
||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | ||||
| Grants/Funds | X | X | X | X | ||||
| Honoraria | X | X | X | X | ||||
| Speaker Forum | X | X | X | X | ||||
| Consultant | X | X | X | X | ||||
| Stocks | X | X | X | X | ||||
| Royalties | X | X | X | X | ||||
| Expert Testimony | X | X | X | X | ||||
| Board Member | X | X | X | X | ||||
| Patents | X | X | X | X | ||||
| Personal Relationship | X | X | X | X | ||||
Author Contributions:
All authors contributed to the drafting and approved the final version to be published and participated in the interpretation of the results.
MES, MIS, NMR: conception and design of the study. MIS, NMR: acquisition of data. MES, HL: statistical analysis.
Sponsor’s Role:
The sponsors had no involvement in any aspect of the research or manuscript preparation.
Contributor Information
Melony E. Sorbero, Policy Researcher, RAND Corporation, Pittsburgh, PA.
Melissa I. Saul, Clinical Data Scientist, Department of Biomedical Informatics, School of Medicine, University of Pittsburgh, Pittsburgh, PA.
Hangsheng Liu, Associate Policy Researcher, RAND Corporation, Boston, MA.
Neil M. Resnick, Chief, Division of Geriatric Medicine, University of Pittsburgh, Pittsburgh, PA.
References
- 1.MedPAC. A Data Book: Healthcare Spending and the Medicare Program. Washington, DC: 2010. [Google Scholar]
- 2.2009 Annual Report of the Boards of Trustees of the Federal Hosptial Insurance and Fenderal Supplementary Medical Insurance Trust Funds. Washington, DC: 2009. [Google Scholar]
- 3.2010 Annual Report of the Boards of Trustees of the Federal Hosptial Insurance and Federal Supplementary Medical Insurance Trust Funds. Washington, DC: 2010. [Google Scholar]
- 4.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. The New England journal of medicine. 2003 Jun 26;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 5.Wenger NS, Solomon DH, Roth CP, et al. The quality of medical care provided to vulnerable community-dwelling older patients. Annals of internal medicine. 2003 Nov 4;139(9):740–747. doi: 10.7326/0003-4819-139-9-200311040-00008. [DOI] [PubMed] [Google Scholar]
- 6.American Geriatrics Society Geriatrics Workforce Policy Studies Center. Documenting the Development of Geriatric Medicine. 2010 [cited 2010 June 10 2010]; Available from: http://www.adgapstudy.uc.edu/figs.cfm.
- 7.Boult C, Counsell SR, Leipzig RM, et al. The urgency of preparing primary care physicians to care for older people with chronic illnesses. Health affairs (Project Hope) May;29(5):811–818. doi: 10.1377/hlthaff.2010.0095. [DOI] [PubMed] [Google Scholar]
- 8.Dang S, Baker G, Lipschitz DA. Financial effect of a hospital outpatient senior clinic on an academic medical center. Journal of the American Geriatrics Society. 2002 Oct;50(10):1621–1628. doi: 10.1046/j.1532-5415.2002.50452.x. [DOI] [PubMed] [Google Scholar]
- 9.McAtee RE, Crandall D, Wright LD, et al. Senior health clinics: are they financially viable? Journal of the American Geriatrics Society. 2009 Jul;57(7):1293–1299. doi: 10.1111/j.1532-5415.2009.02314.x. [DOI] [PubMed] [Google Scholar]
- 10.Pugh MJ, Rosen AK, Montez-Rath M, et al. Potentially inappropriate prescribing for the elderly: effects of geriatric care at the patient and health care system level. Medical care. 2008 Feb;46(2):167–173. doi: 10.1097/MLR.0b013e318158aec2. [DOI] [PubMed] [Google Scholar]
- 11.Yount R, Vries J, Councill C. The medical archival retrieval system: An information retrieval system based on distributed parallel processing. Information Processing and Management. 1991;27:1–11. [Google Scholar]
- 12.Rubin FH, Williams JT, Lescisin DA, et al. Replicating the Hospital Elder Life Program in a community hospital and demonstrating effectiveness using quality improvement methodology. Journal of the American Geriatrics Society. 2006 Jun;54(6):969–974. doi: 10.1111/j.1532-5415.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- 13.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of clinical epidemiology. 1992 Jun;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 14.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 15.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986 Mar;42(1):121–130. [PubMed] [Google Scholar]
- 16.Oehlert GW. A Note on the Delta Method. The American Statistician. 1992;46(1):27–29. [Google Scholar]
- 17.Pawlson LG. Hospital length of stay of frail elderly patients. Primary care by general internists versus geriatricians. Journal of the American Geriatrics Society. 1988 Mar;36(3):202–208. doi: 10.1111/j.1532-5415.1988.tb01801.x. [DOI] [PubMed] [Google Scholar]
- 18.Rubenstein LZ, Josephson KR, Wieland GD, et al. Effectiveness of a geriatric evaluation unit. A randomized clinical trial. The New England journal of medicine. 1984 Dec 27;311(26):1664–1670. doi: 10.1056/NEJM198412273112604. [DOI] [PubMed] [Google Scholar]
- 19.Stuck AE, Siu AL, Wieland GD, et al. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993 Oct 23;342(8878):1032–1036. doi: 10.1016/0140-6736(93)92884-v. [DOI] [PubMed] [Google Scholar]
- 20.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009 Apr 2;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 21.Burns R, Nichols LO, Martindale-Adams J, et al. Interdisciplinary geriatric primary care evaluation and management: two-year outcomes. Journal of the American Geriatrics Society. 2000 Jan;48(1):8–13. doi: 10.1111/j.1532-5415.2000.tb03021.x. [DOI] [PubMed] [Google Scholar]
- 22.Coleman EA, Grothaus LC, Sandhu N, et al. Chronic care clinics: a randomized controlled trial of a new model of primary care for frail older adults. Journal of the American Geriatrics Society. 1999 Jul;47(7):775–783. doi: 10.1111/j.1532-5415.1999.tb03832.x. [DOI] [PubMed] [Google Scholar]
- 23.Rubenstein LZ, Stuck AE, Siu AL, et al. Impacts of geriatric evaluation and management programs on defined outcomes: overview of the evidence. Journal of the American Geriatrics Society. 1991 Sep;39(9 Pt 2):8S–16S. doi: 10.1111/j.1532-5415.1991.tb05927.x. discussion 17S–18S. [DOI] [PubMed] [Google Scholar]
- 24.Goodwin JS. Developing a geriatric business plan for an academic medical center. Journal of the American Geriatrics Society. 2002 Apr;50(4):755–760. doi: 10.1046/j.1532-5415.2002.50174.x. [DOI] [PubMed] [Google Scholar]