Abstract
Despite the lack of placebo-controlled trials, glucocorticoids are considered the mainstay of initial treatment for idiopathic inflammatory myopathy and myositis-associated interstitial lung disease. Glucocorticoid-sparing agents are often given concomitantly with other immunosuppressive agents, particularly in patients with moderate or severe disease. First-line conventional immunosuppressive drugs include either methotrexate or azathioprine, and when they fail, more aggressive therapy includes mycophenolate mofetil, tacrolimus or cyclosporine, intravenous immunoglobulin, rituximab, or cyclophosphamide, used alone or in various combinations. Further investigations are required to assess the role of more novel therapies in the treatment of myositis and myositis-associated interstitial lung disease.
Keywords: dermatomyositis, idiopathic inflammatory myopathy, myositis, polymyositis, treatment
Idiopathic inflammatory myopathies (IIMs) are a group of heterogeneous, systemic rheumatic diseases that include adult polymyositis (PM), adult dermatomyositis (DM), myositis associated with another connective tissue disease or cancer, juvenile myositis (juvenile DM and juvenile PM) and inclusion body myositis.
Treatment of IIM has been challenging and there are currently no standard therapeutic guidelines. The reasons include a low incidence and prevalence, considerable phenotypic clinical heterogeneity, and the small number of randomized, double-blind controlled clinical trials that have been completed [1–4].
Agents used for the management of myositis include glucocorticoids and traditional immunosuppressive or immunomodulatory agents such as methotrexate, azathioprine, mycophenolate mofetil (MMF), cyclosporine, tacrolimus and intravenous immunoglobulin (IVIg). As treatment of refractory IIM is difficult, there has been growing interest in evaluating novel therapies such as newer biologics that target various pathways implicated in disease pathogenesis. Novel classification schemes for IIM based on serologic and histopathologic features may also enhance trial design and treatment choices [5,6]. Previously, outcome measures in myositis trials were poorly standardized and based on varying muscle strength and functional assessments. However, the past several years have heralded the introduction of consensus and data-driven core set measures to assess myositis disease activity and damage. In particular, two international groups, the International Myositis Assessment and Clinical Studies Group and the Pediatric Rheumatology International Trials Organization, have defined and validated consensus core set measures for assessing disease activity and damage in adult and pediatric populations [7–9]. Such outcome measures along with active international initiatives to develop both data- and consensus-driven response criteria will assist in studying both standard and novel therapies in a more systematic and rigorous fashion [10]. In this article, the authors review the immunomodulatory and immunosuppressive approaches in treating IIM, including both conventional therapeutic agents as well as more novel therapies in both PM and DM. Treatment of necrotizing autoimmune myopathy or overlap syndromes is the same as PM/DM. Inclusion body myositis is resistant to standard immunomodulatory or immunosuppressive therapy.
Glucocorticoid therapy
Despite the lack of controlled clinical trials, glucocorticoids remain the mainstay of initial treatment of IIM. Glucocorticoids normalize serum muscle enzymes and improve or preserve muscle strength [11]. They are generally initiated with prednisone at a dose of 1 mg/kg/day, often in divided doses and generally not exceeding 80 mg daily. After 4–6 weeks of high-dose oral glucocorticoid therapy, the prednisone dose is slowly tapered to the minimum effective dose using the general guideline of tapering the existing dose by 20–25% every month. When the daily prednisone dose reaches 5–10 mg/day, the tapering is frequently held for total duration of therapy from 6 to 12 months.
Patients with severe disease manifestations such as marked weakness, severe dysphagia or rapidly progressive interstitial lung disease require pulse intravenous methylprednisolone (1000 mg daily for three consecutive days) followed by the high-dose oral glucocorticoid regimen given above [12]. These patients generally should be started on a steroid-sparing immunosuppressive drug.
Although the total duration of oral glucocorticoid therapy is generally 9–12 months, approximately 50% of patients with IIM fail to completely respond to glucocorticoids alone [5]. In a retrospective cohort study of 113 patients with IIMs, many of those who responded to glucocorticoid monotherapy did not regain normal muscle strength and/or flared when glucocorticoids were tapered [11]. Although a lack of initial response or disease worsening on glucocorticoid therapy should lead to a re-assessment for myositis diagnosis, steroid myopathy or an unrecognized malignancy needs to be considered. A repeat muscle biopsy may be necessary to confirm the diagnosis. In the follow-up assessment of myositis patients, it is important that muscle strength be carefully monitored as a more clinically reliable indicator of treatment response than the levels of serum muscle enzymes such as the creatine kinase (CK). However, in many instances, the CK remains an excellent biomarker of myositis disease activity.
Although some patients with milder disease can be treated with glucocorticoid monotherapy, most of the myositis patients will require the addition of another immunosuppressive drug due to refractory disease, repeated disease flares, or to reduce the dose and duration of glucocorticoid therapy and associated side effects. Regardless of the choice of initial therapy, early treatment is associated with less muscle damage [11].
Methotrexate & azathioprine
The first-line conventional immunosuppressive drug is generally methotrexate or azathioprine. Methotrexate is a folate antimetabolite that irreversibly binds to and inhibits dihydrofolate reductase, resulting in inhibition of DNA synthesis, repair and replication. Methotrexate can be administered orally or subcutaneously and the dose can be titrated up to 25 mg/week, if necessary. There are no placebo-controlled clinical trials of methotrexate in PM or DM. However, a randomized, open-label, assessor-blind, international multicenter clinical trial is ongoing in Europe to assess the efficacy and safety of combined methotrexate/glucocorticoid therapy as compared with glucocorticoid therapy alone [13,14]. Several retrospective studies have suggested the efficacy of methotrexate in PM and DM patients, even in those where initial glucocorticoid monotherapy had failed [11,15]. In a retrospective cohort study of 55 glucocorticoid-refractory IIM patients, methotrexate use was associated with a partial response in 31 and a complete response in 9 [11]. Although methotrexate is not specifically used to treat myositis-associated interstitial lung disease (MA-ILD), pulmonary toxicity leading to pneumonitis is rare but may present a diagnostic challenge in a myositis patient with underlying ILD; so, it should be used cautiously [16]. Methotrexate toxicity monitoring should include a complete blood count to assess for bone marrow suppression, along with assessment of liver enzymes and renal function.
Azathioprine is a derivative of mercaptopurine that inhibits purine metabolism, thus interfering with cellular replication. In a controlled double-blind trial, 16 patients with PM received 60 mg of prednisone daily plus either azathioprine (2 mg/kg/ day) or placebo for a period of 3 months [2]. There was no difference in muscle strength or CK between the two groups after 3 months. But in those patients receiving combination therapy, functional status was better and they required lower maintenance doses of prednisone 3 years later [17]. Some retrospective case series have suggested the efficacy for azathioprine in treating MA-ILD [18,19]. In a series of 70 patients with MA-ILD, azathioprine treatment in 25 patients was associated with clinical improvement [19]. Controlled comparisons have suggested that azathioprine and methotrexate have similar efficacy [11,20]. In a more recent study, survival at 10 years was higher in patients initially treated with methotrexate as compared with those receiving azathioprine, but this was not confirmed in multivariable modeling for the full follow-up period [21]. In contrast, another retrospective study in PM and DM patients showed that azathioprine was associated with improved survival [22]. Although methotrexate is usually considered as the first immunosuppressive agent in the treatment of IIM, azathioprine is preferred in patients with liver disease, those unwilling to abstain from alcohol or in the aforementioned case of MA-ILD. Azathioprine is given orally starting at 50 mg/day with dose escalation by 25–50 mg increments every 1–2 weeks up to 1.5 mg/kg/day. If the response is inadequate after 2–3 months of therapy, the dose can be increased up to 2 or 2.5 mg/kg/day. The azathioprine target dose is lower in patients with renal insufficiency. Monitoring parameters should assess bone marrow suppression, liver enzyme abnormalities and renal dysfunction. Azathioprine toxicity also includes flu-like reactions with fever, gastrointestinal symptoms and pancreatitis. The US FDA recommends screening for thiopurine methyltransferase deficiency prior to treatment with azathioprine.
In a randomized, crossover study of 30 patients with refractory IIM, including those who previously had inadequate treatment responses to either methotrexate or azathioprine alone, a combination of oral methotrexate and azathioprine was beneficial [23].
Mycophenolate mofetil
MMF, a prodrug of mycophenolic acid, is a reversible inhibitor of inosine monophosphate dehydrogenase, thus inhibiting guanosine nucleotide synthesis that, in turn, results in inhibition of T and B lymphocyte proliferation. Use of MMF in inflammatory myopathies has been reported in several small case series [24–27]. In an open study in seven patients with PM and DM refractory to steroid and/or immunosuppressants, MMF combined with IVIg resulted in complete remission [28]. Case series and uncontrolled studies have suggested the efficacy of MMF in treating refractory cutaneous DM [29,30].
Over the past decade, MMF has gained popularity in the management of MA-ILD. Two small case series suggested the efficacy with MMF in treating connective tissue disease-related ILD (CTD-ILD) [31,32]. In another case series of four patients with DM-associated ILD on prednisone, the addition of MMF led to resolution of dyspnea and normalization of the pulmonary function tests (PFTs) in three patients after 1 year of follow-up, along with improvement in the diffusing lung capacity (DLCO) in another patient [33]. In the largest cohort of CTD-ILD, 125 patients (32 with PM or DM) treated with MMF for a median of 897 days showed significant improvements in forced vital capacity (FVC) at 52, 104 and 156 weeks and DLCO at 52 and 104 weeks [34]. There were trends toward statistically significant FVC% and DLCO% improvement among patients with PM or DM at 52, 104 and 156 weeks.
MMF is administered orally starting at 250–500 mg twice daily and increased by 250–500 mg increments every 1–2 weeks to the target dose of 1500–3000 mg/day. A lower dose is recommended in patients with renal insufficiency.
Cyclosporine & tacrolimus
T lymphocytes have been suggested as therapeutic targets in MA-ILD. In one study, infiltrating lymphocytes in MA-ILD patients revealed activated CD8+ T-cells [35]. In a recent study, a decrease in regulatory T-cells in interstitial pneumonitis was noted in rheumatic disease [36]. Use of tacrolimus and cyclosporine has been reported in inflammatory myopathies, particularly those with coexisting ILD [37–42].
Cyclosporine is a calcineurin inhibitor that inhibits the production and release of IL-2 and IL-2–induced activation of T lymphocytes. In a retrospective controlled study of 14 patients with DM and acute/subacute interstitial pneumonia, combination therapy with glucocorticoids and cyclosporine (4 mg/kg/day) within 12 days from diagnosis improved both PFTs and high-resolution computed tomography (HRCT) findings [39]. In another retrospective study of eight anti-Jo-1 positive PM patients with ILD who received oral cyclosporine, progression on HRCT was not significantly different, compared to that in subjects treated with cyclophosphamide [40].
Tacrolimus is a second-generation calcineurin inhibitor that binds to an intracellular protein, FKBP-12, resulting in inhibition of T-cell activation. In a case series of eight patients with myositis (six with anti-Jo-1 and two with anti-signal recognition particle auto-antibodies; five with ILD), tacrolimus therapy resulted in an improvement in muscle strength and CK in all patients and in PFT parameters in three of five patients with ILD [42]. In a follow-up report, 13 patients with anti-synthetase–associated ILD (12 with anti-Jo-1 and 1 with anti-PL-12 auto-antibodies) received tacrolimus for an average of 51 months and showed significant improvement in muscle strength, CK and all PFT parameters [43]. In a more recent observational clinical study of 16 PM and 15 DM patients, tacrolimus led to an improvement in muscle strength and CK, 2–4 months after the initiation of therapy [44]. In three small series of patients with MA-ILD, tacrolimus use was beneficial in patients who had been refractory to cyclosporine [37,44,45]. Tacrolimus has been used as a first-line glucocorticoid-sparing agent [46], but its use is generally reserved for patients with refractory disease due to concerns about its toxicity profile.
Cyclophosphamide
Cyclophosphamide, an alkylating agent, is generally reserved for myositis patients with severe or rapidly progressive interstitial lung disease, features of overlapping systemic vasculitis or those refractory to several other second-line agents. The reasons include a paucity of reports suggesting efficacy in the primary disease and concern about its serious side effects, particularly an increased risk of malignancy [47].
Use of cyclophosphamide in MA-ILD has been reported in a few case reports and small series [48–50]. In a series of 17 patients with MA-ILD, patients received monthly intravenous cyclophosphamide (300–800 mg/m2 monthly) for at least 6 months, in addition to daily prednisone [48]. In 11 of the 17 patients, dyspnea improved and of 7 patients who required supplemental oxygen, 6 later discontinued its use. Twelve patients showed improvements in vital capacity of at least 10% or demonstrated at least a 10-point reduction in a quantitative HRCT score.
Intravenous immunoglobulin
IVIg is an immunomodulatory agent thought to suppress inflammatory or immune-mediated processes. IVIg demonstrated efficacy in DM in a double-blind, controlled trial in 15 patients with refractory DM [3]. In another prospective open-label trial with 35 patients with PM, treatment with IVIg was associated with a significant clinical improvement in 70% of the patients, with stable efficacy reported in half of the patients, 3 years after stopping IVIg [51]. An alternative subcutaneous form of IVIg was associated with promising results in a small series of seven patients (four with DM and three with PM) [52]. Subcutaneous IVIg was administered by a programmable pump and the patient’s usual IVIg monthly dose was divided into equal doses given subcutaneously at weekly intervals. All patients showed significant improvement in muscle strength, CK and quality of life, and were able to discontinue the immunosuppressive agents and reduce their maintenance prednisone dose. Few case reports have suggested that IVIg may be effective in the treatment of MA-ILD [53,54]. The 2012 American Academy of Neurology guidelines support using IVIg for refractory DM, but there is insufficient evidence to support or refute its use in PM [55].
IVIg is usually administered as infusions of 2 g/kg monthly, but the dose or interval can be changed based on the disease severity and response to therapy. A major advantage of IVIg is that it is safe in the setting of an active infection and can be used concomitantly with other immunosuppressive agents. The high cost of IVIg may influence decisions on its long-term use. Therefore, IVIg is generally reserved for patients with refractory disease or severe dysphagia, or as a salvage therapy in patients with severe and progressive MA-ILD resistant to conventional immunosuppressive therapy.
Rituximab
Rituximab, a B-cell depleting agent, is a monoclonal antibody that targets the CD20 antigen on B-cells. Several small case reports have suggested its in refractory IIM [56–60]. In a small, open-label, uncontrolled pilot trial in six treatment-resistant DM patients, rituximab therapy (4 weekly intravenous doses) was associated with major clinical improvement in muscle strength and rash [61]. In another small, open-label trial of rituximab in four patients with refractory PM, all patients demonstrated normalization of muscle strength and significant decline in CK levels [62]. However, in another open-label trial of rituximab in eight patients with adult DM, skin disease (skin scores based on Dermatomyositis Skin Severity Index) and CK levels did not significantly change from those at baseline and only three patients showed modest improvement in muscle strength [63].
In the largest randomized, double-blind, controlled clinical trial in IIM (the Rituximab in Myositis [RIM] trial), 195 patients (75 with PM, 72 with DM and 48 with juvenile dermatomyositis; all refractory to glucocorticoid therapy and at least one immunosuppressive drug) were randomized to receive two 1-g rituximab infusions either at baseline or 8 weeks later [1]. The primary endpoint was the time to achieve the International Myositis Assessment and Clinical Studies Group definition of improvement (DOI) that was compared between the two groups (receiving rituximab early and late, respectively). Although the group receiving early rituximab demonstrated no faster response to therapy than the group treated later (thus failing to meet the primary outcome), the DOI was met by 83% of this refractory group of myositis patients with a median time to achieving the DOI of 20 weeks. Rituximab also showed a significant steroid-sparing effect as the mean prednisone dose decreased from 20.8 mg at baseline to 14.4 mg daily at the end of the trial. Moreover, patients who initially met the DOI and who were subsequently re-treated with rituximab after a disease flare also responded to re-treatment. Rituximab therapy was generally well tolerated and the most common adverse events were infections. Additional analysis of the RIM study data demonstrated that the presence of anti-synthetase and anti-Mi-2 auto-antibodies along with juvenile DM subset, and lower disease damage were strong predictors of clinical improvement [64].
The efficacy data of rituximab specific to MA-ILD is limited to case reports and case series [58,59]. In a recent retrospective study of 50 patients with severe, progressive ILD (10 with MA-ILD), rituximab therapy was associated with a median improvement in FVC of 6.7% (p < 0.01) and stability of the DLCO (0% change; p < 0.01) in the 6–12-month period after rituximab therapy [65]. Among the CTD-ILD patients assessed in this study, the best outcome was noted in patients with MA-ILD, as 5 of the 10 (50%) MA-ILD patients showed an increase in their FVC by >10% and/or the DLCO by >15%, compared to 4 out of 22 (18.2%) patients with other CTD-ILDs (p = 0.096). In a more recent retrospective study in Europe, 24 patients with anti-synthetase syndrome and severe ILD with more than 12 months follow-up (median 52 months) post-rituximab therapy were identified [66]. The median percentage of predicted FVC, forced expiratory volume in 1 second and DLCO increased by 24, 22 and 17%, respectively, following rituximab therapy. HRCT findings (expressed as a percentage of total lung volume involvement) showed a median of 34% reduction in ILD extent following B-cell depleting therapy. Muscle strength (evaluated by manual muscle testing of eight muscle groups [MMT8]) also improved post-rituximab therapy and the CK significantly dropped as well. The best results (>30% improvement in all three PFT parameters) were observed in seven patients with a disease duration of <12 months and/or an acute onset/exacerbation of ILD. Since 10 of the 12 patients with acute disease also received cyclophosphamide, this study is difficult to interpret, as the response attributable to rituximab alone cannot be inferred. Of note, there were 7 deaths among the 34 rituximab-treated patients and 6 of the 7 deaths were related to infection (3 subjects had Pneumocystis jirovecii pneumonia).
Rituximab is usually administered as two 1-g doses 2 weeks apart, but the interval may vary. The decision on additional courses of rituximab therapy is generally made on a case-by-case basis. All patients should be screened for hepatitis B prior to therapy and high-risk patients require hepatitis C screening. Patients with a history of recovery from prior hepatitis B infection need to be monitored closely for clinical and laboratory evidence of HBV reactivation during rituximab therapy and for 1–2 years thereafter. Some suggest periodic monitoring of peripheral B-cell flow cytometry to assess for the return of CD20-positive B-cells.
Anti-TNF agents
Anti-TNF agents, etanercept and infliximab, have been used for the treatment of IIMs, but the outcomes have been mixed and their efficacy is yet to be established. In a series of five patients with DM resistant to steroid and cytotoxic therapy, etanercept therapy (25 mg subcutaneously twice a week for at least 3 months) was associated with worsening muscle weakness, elevation of muscle enzyme levels and unchanged rash in all patients [67]. After the discontinuation of etanercept, patients improved with the combination of methotrexate and azathioprine therapy. In contrast, in a more recent randomized, double-blind, controlled trial of etanercept (50 mg subcutaneously weekly for 52 weeks) in 16 DM patients, etanercept therapy was associated with a significantly longer median time to treatment failure and a significantly lower average prednisone dose after week 24 [68]. Given the small number of patients in this study, further studies are needed to clarify the role of etanercept in IIM.
A few anecdotal reports suggested the efficacy of infliximab in IIM [69–71], but a follow-up report of two patients initially responding showed that they worsened later and resuming infliximab was associated with anaphylaxis and the development of anti-dsDNA auto-antibodies [72]. In a larger retrospective series of eight patients with refractory DM or PM, infliximab therapy was associated with improved motor strength, but only a partial decline in serum CK [73]. In a more recent pilot study of 13 patients with refractory IIM, infliximab therapy (four infusions of 5 mg/kg body weight over 14 weeks) was not effective, with no patient showing improvement in muscle strength [74]. An unpublished randomized controlled trial of infliximab in IIM also failed to demonstrate efficacy [75]. A multicenter, open-label, controlled trial of infliximab combined with weekly methotrexate in patients with PM or DM was terminated prematurely because of a low inclusion rate and high drop-out due to disease progression and the infusion reactions [76].
In general, anti-TNF therapy is not routinely used in myositis, given the negative studies as well as the recent reports suggesting its potential for inducing PM and DM [77–80].
Adrenocorticotropic hormone gel
Adrenocorticotropic hormone (ACTH) gel is a long-acting, full-sequence ACTH that includes other proopiomelanocortin peptides. Melanocortin receptors are widely distributed in peripheral cells and their activation by natural or synthetic ligands is thought to have anti-inflammatory and immunomodulatory effects [81].
In a recent retrospective case review, five patients with refractory myositis (three DM, two PM) received ACTH gel subcutaneous injections of 80 U (1 ml) twice weekly (four patients) or once weekly (one patient) for 12 weeks. All patients showed improvement in muscle strength as well as resolution of rash [82]. All patients tolerated the ACTH gel therapy well, and no major side effects occurred.
ACTH gel has been an FDA-approved treatment for PM and DM since 1952 and its approval was retained by the FDA in 2010. Therefore, some clinical rheumatologists are considering ACTH gel in refractory IIM patients or those who are unable to tolerate the glucocorticoid-related side effects. However, the clinical efficacy of ACTH gel has not been established and an open-label clinical trial is underway to evaluate the efficacy and safety of ACTH gel in refractory PM and DM [83]
Tocilizumab
Since the approval of tocilizumab, an antagonist of the IL-6 receptor, for rheumatoid arthritis, there has been growing interest in assessing the potential efficacy of this biologic agent in other systemic rheumatic diseases including IIMs. Mononuclear inflammatory cells in IIM implicate the production of pro-inflammatory cytokines such as IL-6, which is overexpressed in the serum of IIM patients [84,85]. While IL-1α, IL-1β, TGF β1–3 and the type I interferon signature are the dominant cytokines expressed in the muscle tissue of patients with IIMs, IL-6 is also observed [86].
In the first report of tocilizumab therapy in IIMs, two patients with refractory PM demonstrated improvement in the serum CK level and MRI of their thigh muscles [87]. There were no adverse events except for a mild elevation of serum low-density lipoprotein in one patient. In another more recent report, a 32-year-old Japanese patient with an overlap syndrome, including features of DM (proximal muscle weakness, heliotrope rash and Gottron’s sign) and systemic sclerosis, initially responded to high-dose prednisolone therapy, but later had worsened muscle weakness and serum CK elevation [88]. Trials of cyclosporine, intravenous cyclophosphamide, IVIg and tacrolimus followed by methotrexate and adalimumab in combination were ineffective or partially effective, and he subsequently developed inflammatory arthritis associated with anti-cyclic citrullinated peptide positivity. Tocilizumab therapy led to resolution of skin rash and improvement in arthritis 1 month later, along with gradual improvement in the muscle weakness and serum CK elevation, allowing glucocorticoid dose tapering.
An investigator-initiated, randomized, multicenter, double-blind, controlled trial is ongoing to assess the efficacy of tocilizumab and its potential role in refractory adult PM and DM, with the University of Pittsburgh as the coordinating center [89].
Abatacept
CD28 and CTLA-4, costimulatory molecules, are up-regulated in the muscle of PM and DM patients [90,91]. Abatacept, which targets CD80 and CD86 on antigen presenting cells, was successful in a refractory PM [92] patient, while a child with severe recalcitrant juvenile dermatomyositis with ulcerative skin disease and progressive calcinosis responded well to combination therapy with abatacept and sodium thiosulfate [93]. In another case report from Japan, abatacept therapy was associated with a favorable outcome in the treatment of refractory anti-signal recognition particle–positive myositis [94]. In a more recent report from Europe, a patient with severe myositis in overlap with rheumatoid arthritis, peripheral vasculitis and ILD, who had been refractory to many conventional and biologic therapies, responded well to abatacept and showed good control of myositis [95]. An ongoing clinical trial (ARTEMIS) is underway to further assess the efficacy of abatacept in refractory IIM.
Alemtuzumab
Alemtuzumab, a humanized monoclonal antibody, binds the cell-surface glycoprotein CD52 on B and T lymphocytes, monocytes, macrophages and NK cells, interfering with T-cell signaling, thus leading to alteration in the number and properties of both B- and T-cells.
In a report, a single course of alemtuzumab (120 mg over 4 days) was associated with rapid improvement in muscle strength in a 48-year-old woman with refractory anti-Jo-1 positive PM, ILD and pulmonary artery hypertension [96]. Unfortunately, there was no improvement in the respiratory function following alemtuzumab and sildenafil therapy and the patient died 1 year later.
Sifalimumab
There is growing evidence that type I interferon (IFN-α/-β)-mediated innate immunity may be involved in the pathogenesis of IIMs. In a study of 67 patients with DM, PM and other myopathies, clusters of genes known to be induced by IFN-α/-β were overexpressed in DM patients (n = 14) as compared to controls [97]. A follow-up study from the same group showed similar findings of overexpression of type I interferon genes including IFI27, IFI44L, RSAD2 and IFI44 [98]. In another study, a striking interferon signature with increased levels of interferon-regulated cytokines was noted in DM serum samples, both of which correlated with disease activity [99]. Using peripheral blood samples and clinical data from 56 patients with adult or juvenile DM, the type I interferon gene and chemokine signature and serum levels of IL-6 correlated with each other and with myositis disease activity [100].
A recent Phase Ib randomized, double-blinded, controlled, multicenter clinical trial evaluated sifalimumab in PM and DM [101] and found the drug therapy to be associated with suppression of the interferon signature in blood and muscle tissue, which correlated with clinical improvement.
Conclusion
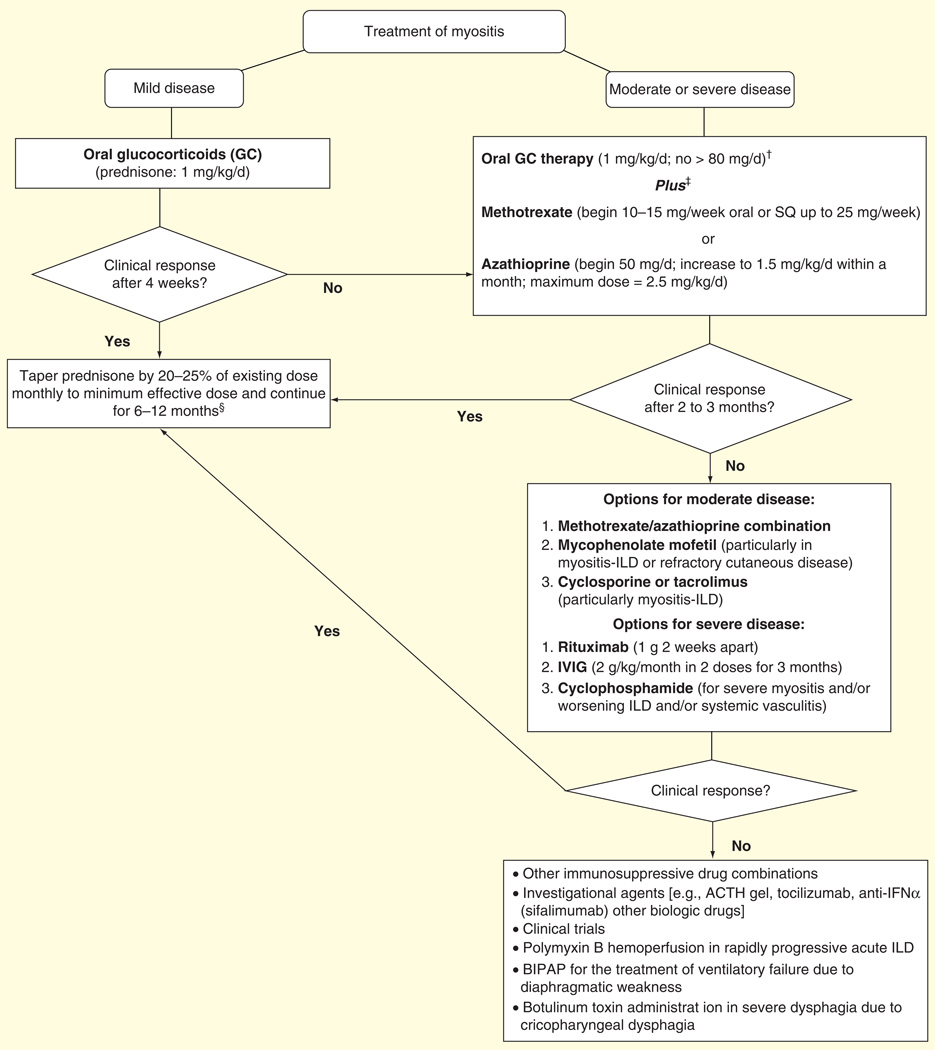
Despite the lack of placebo-controlled trials, systemic glucocorticoids are considered the mainstay of initial treatment of the IIMs, specifically PM and DM. Glucocorticoid-sparing agents, either methotrexate or azathioprine, are often begun concomitantly with glucocorticoids, particularly in patients with moderate or severe disease and presenting to tertiary care centers. If these agents fail, other conventional or biologic immunosuppressive or immunomodulatory agents are sequentially used alone or in various combinations (Table 1 & Figure 1).
Table 1.
Immunosuppressive and immunomodulatory drugs used in the treatment of inflammatory myopathy.
| Drug | Dose | Level of evidence for use in inflammatory myopathy |
|---|---|---|
| Glucocorticoids | Begin at 1 mg/kg/day, often in divided doses and generally not exceeding 80 mg daily. Taper by 20–25% of the existing dose monthly until 5–10 mg/day is reached. Hold tapering for a total duration of therapy of 6–12 months |
Retrospective studies [11] |
| Methotrexate | Begin at 10–15 mg/week (oral or subcutaneous), increase to 25 mg/week | Retrospective uncontrolled cohort studies [11,14,15] |
| Azathioprine | Begin at 50 mg/day (oral) with dose escalation by 25–50 mg increments every 1–2 weeks up to 1.5 mg/kg/day. Increase up to 2–2.5 mg/kg/day in severe cases |
Retrospective uncontrolled cohort studies [2,17–19] |
| Mycophenolate mofetil |
Begin at 250–500 mg twice daily (oral) and increase by 250–500 mg increments every 1–2 weeks to a target dose of 1500–3000 mg/day |
Retrospective uncontrolled studies [24–34] |
| Cyclosporine | Begin at 50 mg twice daily, increase up to 100–150 mg twice daily | Retrospective controlled study [39] |
| Tacrolimus | Begin at 1 mg twice daily, increase to reach trough level of 5–10 ng/ml | Retrospective controlled studies [37,42–46] |
| Cyclophosphamide |
Begin at 50–75 mg/day (oral), working up to 1.5–2 mg/kg/day | Prospective uncontrolled studies on myositis-ILD [47–50] |
| IVIg | Begin at 1–2 g/kg/month over 1–2 days, continue for 3–6 months depending on response |
Double-blind, placebo- controlled trial [3] |
| Rituximab | Two 1-g doses 2 weeks apart, but the interval may vary | Double-blind, controlled trial (improvement in the definition of improvement) [1] |
ILD: Interstitial lung disease; IVIg: Intravenous immunoglobulin.
Figure 1. Therapeutic approach to inflammatory myopathy.
†For the initial treatment of severe disease (marked weakness, dysphagia or rapidly progressive ILD), consider pulse intravenous methylprednisolone (1 g daily for three consecutive days) before oral or intravenous GC therapy.
‡For patients on combination of high-dose GC plus another immunosuppressive agent, add prophylaxis against Pneumocystis jirovecii (e.g., trimethoprim–sulfamethoxazole double strength [160 mg/800 mg] three-times weekly).
§Duration of therapy with GC-sparing agents may be extended to 1–2 years based on clinical response.
ACTH: Adrenocorticotropic hormone; BIPAP: Bilevel positive airway pressure; GC: Glucocorticoid; ILD: Interstitial lung disease; IVIg: Intravenous immunoglobulin.
Expert commentary
Traditional therapy for IIMs includes systemic glucocorticoids and conventional immunosuppressive or immunomodulatory agents. However, the treatment of refractory IIMs can be difficult. Some of the immunosuppressive agents are more appropriately used when certain manifestations predominate, such as MMF for MA-ILD and refractory cutaneous disease and tacrolimus or cyclosporine for MA-ILD. Various combinations have been studied, such as methotrexate and azathioprine, but others can be considered as well, such as tacrolimus and MMF or methotrexate and MMF in patients with refractory IIM.
There is growing interest in investigating novel drugs including newer biologics that target various pathways involved in the pathogenesis of myositis. Over the last decade, there have been several small case series and a limited number of clinical trials attempting to evaluate the efficacy of biologic agents in IIMs, even though data remains limited.
Five-year view
Additional well-designed controlled trials are required to develop an evidence-based approach for the treatment of IIM and MA-ILD. Novel schemes for classification of IIMs based on serologic and histopathologic features can provide guidelines for enrolling subjects. Emerging, validated consensus core set measures will further assist in assessing myositis disease activity and damage and studying novel therapies in a more rigorous fashion in future clinical trials. Further investigations are required to assess the role of novel therapies such as ACTH gel, anti-IL6 (tocilizumab), anti-IFN-α (sifalimumab), inhibition of T-cell costimulation (abatacept), along with alemtuzumab (a humanized monoclonal antibody which binds CD52 on B and T lymphocytes), fingolimod (a sphingosine-1-phosphate receptor modulator that traps T lymphocytes in the lymphoid organs), eculizumab (which targets C5 and inhibits the cleavage of C5 to C5a and C5b-9) and basiliximab (a monoclonal antibody that blocks the IL-2 receptor alpha chain on T and B lymphocytes).
Key issues.
Despite the lack of controlled trials, systemic glucocorticoids are considered the mainstay of initial treatment of inflammatory myopathies (IIMs) and myositis-associated interstitial lung disease.
Glucocorticoid-sparing agents, either methotrexate or azathioprine, are often started concomitantly with systemic glucocorticoids, particularly in IIM patients with moderate or severe disease.
In patients who do not show adequate response to systemic glucocorticoids combined with methotrexate or azathioprine, other conventional or biologic immunosuppressive or immunomodulatory agents are sequentially used alone or in various combinations.
The treatment of refractory IIMs can be challenging, and efficacy data on novel drugs including biologic agents remains limited.
Acknowledgments
Financial
R Aggarwal has received research grants from Pfizer, Mallinckrodt and Genentech. CV Oddis has received research grants from Genentech, Mallinckrodt, and Novartis.
Footnotes
competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
Papers of special note have been highlighted as:
• of interest
•• of considerable interest
- 1. Oddis CV, Reed AM, Aggarwal R, et al. Rituximab in the treatment of refractory adult and juvenile dermatomyositis and adult polymyositis: a randomized, placebo-phase trial. Arthritis Rheum. 2013;65(2):314–324. doi: 10.1002/art.37754.• This manuscript summarizes the results of the largest randomized, double-blind, controlled clinical trial in idiopathic inflammatory myopathy (the Rituximab in Myositis [RIM] trial)
- 2.Bunch TW, Worthington JW, Combs JJ, et al. Azathioprine with prednisone for polymyositis A controlled, clinical trial. Ann Intern Med. 1980;92(3):365–369. doi: 10.7326/0003-4819-92-3-365. [DOI] [PubMed] [Google Scholar]
- 3.Dalakas MC, Illa I, Dambrosia JM, et al. A controlled trial of high-dose intravenous immune globulin infusions as treatment for dermatomyositis. N Engl J Med. 1993;329(27):1993–2000. doi: 10.1056/NEJM199312303292704. [DOI] [PubMed] [Google Scholar]
- 4.Miller FW, Leitman SF, Cronin ME, et al. Controlled trial of plasma exchange and leukapheresis in polymyositis and dermatomyositis. N Engl J Med. 1992;326(21):1380–1384. doi: 10.1056/NEJM199205213262102. [DOI] [PubMed] [Google Scholar]
- 5.Troyanov Y, Targoff IN, Tremblay JL, et al. Novel classification of idiopathic inflammatory myopathies based on overlap syndrome features and autoantibodies: analysis of 100 French Canadian patients. Medicine (Baltimore) 2005;84(4):231–249. doi: 10.1097/01.md.0000173991.74008.b0. [DOI] [PubMed] [Google Scholar]
- 6.Koenig M, Fritzler MJ, Targoff IN, et al. Heterogeneity of autoantibodies in 100 patients with autoimmune myositis: insights into clinical features and outcomes. Arthritis Res Ther. 2007;9(4):R78. doi: 10.1186/ar2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rider LG, Werth VP, Huber AM, et al. Measures of adult and juvenile dermatomyositis, polymyositis, and inclusion body myositis: physician and patient/parent global activity, manual muscle testing (MMT), health assessment questionnaire (HAQ)/childhood health assessment questionnaire (C-HAQ), childhood myositis assessment scale (CMAS), myositis disease activity assessment tool (MDAAT), disease activity score (DAS), short form 36 (SF-36), child health questionnaire (CHQ), physician global damage, myositis damage index (MDI), quantitative muscle testing (QMT), myositis functional index-2 (FI-2), myositis activities profile (MAP), inclusion body myositis functional rating scale (IBMFRS), cutaneous dermatomyositis disease area and severity index (CDASI), cutaneous assessment tool (CAT), dermatomyositis skin severity index (DSSI), skindex, and dermatology life quality index (DLQI) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S118–S157. doi: 10.1002/acr.20532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oddis CV, Rider LG, Reed AM, et al. International consensus guidelines for trials of therapies in the idiopathic inflammatory myopathies. Arthritis Rheum. 2005;52(9):2607–2615. doi: 10.1002/art.21291. [DOI] [PubMed] [Google Scholar]
- 9.Isenberg DA, Allen E, Farewell V, et al. International consensus outcome measures for patients with idiopathic inflammatory myopathies Development and initial validation of myositis activity and damage indices in patients with adult onset disease. Rheumatology (Oxford) 2004;43(1):49–54. doi: 10.1093/rheumatology/keg427. [DOI] [PubMed] [Google Scholar]
- 10.Aggarwal R, Rider LG, Ruperto N, et al. A consensus hybrid definition using a conjoint analysis is proposed as response criteria for minimal and moderate improvement in adult polymyositis and dermatomyositis clinical trials. Arthritis and Rheum. 2014;64(10 Suppl) [Google Scholar]
- 11.Joffe MM, Love LA, Leff RL, et al. Drug therapy of the idiopathic inflammatory myopathies: predictors of response to prednisone, azathioprine, and methotrexate and a comparison of their efficacy. Am J Med. 1993;94(4):379–387. doi: 10.1016/0002-9343(93)90148-i. [DOI] [PubMed] [Google Scholar]
- 12.Bolosiu HD, Man L, Rednic S. The effect of methylprednisolone pulse therapy in polymyositis/dermatomyositis. Adv Exp Med Biol. 1999;455:349–357. doi: 10.1007/978-1-4615-4857-7_54. [DOI] [PubMed] [Google Scholar]
- 13.Combined treatment of methotrexate + glucocorticoids versus glucocorticoids alone in patients with polymyositis and dermatomyositis (Prometheus) Available from: https://clinicaltrials.gov/ct2/show/NCT00651040.
- 14. Available from: http://clinicaltrials.gov/ct2/show/NCT00651040?term=methotrexate+myositis&rank=1.
- 15.Newman ED, Scott DW. The use of low-dose oral methotrexate in the treatment of polymyositis and dermatomyositis. J Clin Rheumatol. 1995;1(2):99–102. doi: 10.1097/00124743-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Saravanan V, Kelly CA. Reducing the risk of methotrexate pneumonitis in rheumatoid arthritis. Rheumatology (Oxford) 2004;43(2):143–147. doi: 10.1093/rheumatology/keg466. [DOI] [PubMed] [Google Scholar]
- 17.Bunch TW. Prednisone and azathioprine for polymyositis: long-term followup. Arthritis Rheum. 1981;24(1):45–48. doi: 10.1002/art.1780240107. [DOI] [PubMed] [Google Scholar]
- 18.Marie I, Hachulla E, Chérin P, et al. Interstitial lung disease in polymyositis and dermatomyositis. Arthritis Rheum. 2002;47:614–622. doi: 10.1002/art.10794. [DOI] [PubMed] [Google Scholar]
- 19.Douglas WW, Tazelaar HD, Hartman TE, et al. Polymyositis-dermatomyositis-associated interstitial lung disease. Am J Respir Crit Care Med. 2001;164:1182–1185. doi: 10.1164/ajrccm.164.7.2103110. [DOI] [PubMed] [Google Scholar]
- 20.Miller J, Walsh Y, Saminaden S, et al. Randomised double blind controlled trial of methotrexate and steroids compared with azathioprine and steroids in the treatment of idiopathic inflammatory myopathy. J Neurol Sci. 2002;199(Suppl 01):S53. [Google Scholar]
- 21.Schiopu E, Phillips K, MacDonald PM, et al. Predictors of survival in a cohort of patients with polymyositis and dermatomyositis: effect of corticosteroids, methotrexate and azathioprine. Arthritis Res Ther. 2012;14(1):R22. doi: 10.1186/ar3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu KH, Wu YJ, Kuo CF, et al. Survival analysis of patients with dermatomyositis and polymyositis: analysis of 192 Chinese cases. Clin Rheumatol. 2011;30(12):1595–1601. doi: 10.1007/s10067-011-1840-0. [DOI] [PubMed] [Google Scholar]
- 23.Villalba L, Hicks JE, Adams EM, et al. Treatment of refractory myositis: a randomized crossover study of two new cytotoxic regimens. Arthritis Rheum. 1998;41(3):392–399. doi: 10.1002/1529-0131(199803)41:3<392::AID-ART3>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 24.Pisoni CN, Cuadrado MJ, Khamashta MA, et al. Mycophenolate mofetil treatment in resistant myositis. Rheumatology (Oxford) 2007;46(3):516–518. doi: 10.1093/rheumatology/kel336. [DOI] [PubMed] [Google Scholar]
- 25.Rowin J, Amato AA, Deisher N, et al. Mycophenolate mofetil in dermatomyositis: is it safe? Neurology. 2006;66(8):1245–1247. doi: 10.1212/01.wnl.0000208416.32471.c0. [DOI] [PubMed] [Google Scholar]
- 26.Majithia V, Harisdangkul V. Mycophenolate mofetil (CellCept): an alternative therapy for autoimmune inflammatory myopathy. Rheumatology (Oxford) 2005;44(3):386–389. doi: 10.1093/rheumatology/keh499. [DOI] [PubMed] [Google Scholar]
- 27.Schneider C, Gold R, Schäfers M, Toyka KV. Mycophenolate mofetil in the therapy of polymyositis associated with a polyautoimmune syndrome. Muscle Nerve. 2002;25(2):286–288. doi: 10.1002/mus.10026. [DOI] [PubMed] [Google Scholar]
- 28.Danieli MG, Calcabrini L, Calabrese V, et al. Intravenous immunoglobulin as add on treatment with mycophenolate mofetil in severe myositis. Autoimmun Rev. 2009;9(2):124–127. doi: 10.1016/j.autrev.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 29.Edge JC, Outland JD, Dempsey JR, Callen JP. Mycophenolate mofetil as an effective corticosteroid-sparing therapy for recalcitrant dermatomyositis. Arch Dermatol. 2006;142(1):65–69. doi: 10.1001/archderm.142.1.65. [DOI] [PubMed] [Google Scholar]
- 30.Gelber AC, Nousari HC, Wigley FM. Mycophenolate mofetil in the treatment of severe skin manifestations of dermatomyositis: a series of 4 cases. J Rheumatol. 2000;27(6):1542–1545. [PubMed] [Google Scholar]
- 31.Saketkoo LA, Espinoza LR. Experience of mycophenolate mofetil in 10 patients with autoimmune-related interstitial lung disease demonstrates promising effects. Am J Med Sci. 2009;337(5):329–335. doi: 10.1097/MAJ.0b013e31818d094b. [DOI] [PubMed] [Google Scholar]
- 32.Swigris JJ, Olson AL, Fischer A, et al. Mycophenolate mofetil is safe, well tolerated, and preserves lung function in patients with connective tissue disease-related interstitial lung disease. Chest. 2006;130(1):30–36. doi: 10.1378/chest.130.1.30. [DOI] [PubMed] [Google Scholar]
- 33.Morganroth PA, Kreider ME, Werth VP. Mycophenolate mofetil for interstitial lung disease in dermatomyositis. Arthritis Care Res (Hoboken) 2010;62(10):1496–1501. doi: 10.1002/acr.20212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fischer A, Brown KK, Du Bois RM, et al. Mycophenolate mofetil improves lung function in connective tissue disease-associated interstitial lung disease. J Rheumatol. 2013;40(5):640–646. doi: 10.3899/jrheum.121043.• This paper reviews the largest cohort of connective tissue disease-related interstitial lung disease, 125 patients (32 with polymyositis or dermatomyositis [DM]) treated with mycophenolate mofetil.
- 35.Yamadori I, Fujita J, Kajitani H, et al. Lymphocyte subsets in lung tissues of interstitial pneumonia associated with untreated polymyositis/dermatomyositis. Rheumatol Int. 2001;21:89–93. doi: 10.1007/s00296-001-0146-y. [DOI] [PubMed] [Google Scholar]
- 36.Katagiri A, Morimoto S, Nakiri Y, et al. Decrease in CD4+CD25+ and CD8+CD28 + T cells in interstitial pneumonitis associated with rheumatic disease. Mod Rheumatol. 2008;18:562–569. doi: 10.1007/s10165-008-0090-8. [DOI] [PubMed] [Google Scholar]
- 37.Takada K, Nagasaka K, Miyasaka N. Polymyositis/dermatomyositis and interstitial lung disease: a new therapeutic approach with T-cell-specific immunosuppressants. Autoimmunity. 2005;38:383–392. doi: 10.1080/08916930500124023. [DOI] [PubMed] [Google Scholar]
- 38.Kotani T, Makino S, Takeuchi T, et al. Early intervention with corticosteroids and cyclosporin A and 2-hour postdose blood concentration monitoring improves the prognosis of acute/subacute interstitial pneumonia in dermatomyositis. J Rheumatol. 2008;35:254–259. [PubMed] [Google Scholar]
- 39.Kotani T, Takeuchi T, Makino S, et al. Combination with corticosteroids and cyclosporin-A improves pulmonary function test results and chest HRCT findings in dermatomyositis patients with acute/ subacute interstitial pneumonia. Clin Rheumatol. 2011;30:1021–1028. doi: 10.1007/s10067-011-1713-6. [DOI] [PubMed] [Google Scholar]
- 40.Ingegnoli F, Lubatti C, Ingegnoli A, et al. Interstitial lung disease outcomes by high-resolution computed tomography (HRCT) in Anti-Jo1 antibody-positive polymyositis patients: a single centre study and review of the literature. Autoimmun Rev. 2012;11:335–340. doi: 10.1016/j.autrev.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 41.Qushmaq KA, Chalmers A, Esdaile JM. Cyclosporin A in the treatment of refractory adult polymyositis/dermatomyositis: population based experience in 6 patients and literature review. J Rheumatol. 2000;27:2855–2859. [PubMed] [Google Scholar]
- 42.Oddis CV, Sciurba FC, Elmagd KA, Starzl TE. Tacrolimus in refractory polymyositis with interstitial lung disease. Lancet. 1999;353:1762–1763. doi: 10.1016/S0140-6736(99)01927-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilkes MR, Sereika SM, Fertig N, et al. Treatment of antisynthetase-associated interstitial lung disease with tacrolimus. Arthritis Rheum. 2005;52:2439–2446. doi: 10.1002/art.21240. [DOI] [PubMed] [Google Scholar]
- 44.Mitsui T, Kuroda Y, Ueno S, Kaji R. The effects of FK506 on refractory inflammatory myopathies. Acta Neurol Belg. 2011;111(3):188–194. [PubMed] [Google Scholar]
- 45.Ochi S, Nanki T, Takada K, et al. Favorable outcomes with tacrolimus in two patients with refractory interstitial lung disease associated with polymyositis/ dermatomyositis. Clin Exp Rheumatol. 2005;23:707–710. [PubMed] [Google Scholar]
- 46.Labirua-Iturburu A, Selva-O’Callaghan A, Martínez-Gómez X, et al. Calcineurin inhibitors in a cohort of patients with antisynthetase-associated interstitial lung disease. Clin Exp Rheumatol. 2013;31:436–439. [PubMed] [Google Scholar]
- 47.Cronin ME, Miller FW, Hicks JE, et al. The failure of intravenous cyclophosphamide therapy in refractory idiopathic inflammatory myopathy. J Rheumatol. 1989;16(9):1225–1228. [PubMed] [Google Scholar]
- 48.Yamasaki Y, Yamada H, Yamasaki M, et al. Intravenous cyclophosphamide therapy for progressive interstitial pneumonia in patients with polymyositis/dermatomyositis. Rheumatology (Oxford) 2007;46:124–130. doi: 10.1093/rheumatology/kel112. [DOI] [PubMed] [Google Scholar]
- 49.Kameda H, Nagasawa H, Ogawa H, et al. Combination therapy with corticosteroids, cyclosporin A, and intravenous pulse cyclophosphamide for acute/subacute interstitial pneumonia in patients with dermatomyositis. J Rheumatol. 2005;32:1719–1726. [PubMed] [Google Scholar]
- 50.Mok CC, To CH, Szeto ML. Successful treatment of dermatomyositis-related rapidly progressive interstitial pneumonitis with sequential oral cyclophosphamide and azathioprine. Scand J Rheumatol. 2003;32:181–183. doi: 10.1080/03009740310002542. [DOI] [PubMed] [Google Scholar]
- 51.Cherin P, Pelletier S, Teixeira A, et al. Results and long-term followup of intravenous immunoglobulin infusions in chronic, refractory polymyositis: an open study with thirty-five adult patients. Arthritis Rheum. 2002;46(2):467–474. doi: 10.1002/art.10053. [DOI] [PubMed] [Google Scholar]
- 52.Danieli MG, Pettinari L, Moretti R, et al. Subcutaneous immunoglobulin in polymyositis and dermatomyositis: a novel application. Autoimmun Rev. 2011;10(3):144–149. doi: 10.1016/j.autrev.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 53.Suzuki Y, Hayakawa H, Miwa S, et al. Intravenous immunoglobulin therapy for refractory interstitial lung disease associated with polymyositis/dermatomyositis. Lung. 2009;187:201–206. doi: 10.1007/s00408-009-9146-6. [DOI] [PubMed] [Google Scholar]
- 54.Bakewell CJ, Raghu G. Polymyositis associated with severe interstitial lung disease: remission after three doses of IV immunoglobulin. Chest. 2011;139:441–443. doi: 10.1378/chest.10-0360. [DOI] [PubMed] [Google Scholar]
- 55.Patwa HS, Chaudhry V, Katzberg H, et al. Evidence-based guideline: intravenous immunoglobulin in the treatment of neuromuscular disorders: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2012;78(13):1009–1015. doi: 10.1212/WNL.0b013e31824de293. [DOI] [PubMed] [Google Scholar]
- 56.Mahler EA, Blom M, Voermans NC, et al. Rituximab treatment in patients with refractory inflammatory myopathies. Rheumatology (Oxford) 2011;50(12):2206–2213. doi: 10.1093/rheumatology/ker088. [DOI] [PubMed] [Google Scholar]
- 57.Valiyil R, Casciola-Rosen L, Hong G, et al. Rituximab therapy for myopathy associated with anti-signal recognition particle antibodies: a case series. Arthritis Care Res (Hoboken) 2010;62(9):1328–1334. doi: 10.1002/acr.20219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brulhart L, Waldburger JM, Gabay C. Rituximab in the treatment of antisynthetase syndrome. Ann Rheum Dis. 2006;65(7):974–975. doi: 10.1136/ard.2005.045898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lambotte O, Kotb R, Maigne G, et al. Efficacy of rituximab in refractory polymyositis. J Rheumatol. 2005;32(7):1369–1370. [PubMed] [Google Scholar]
- 60.Arlet JB, Dimitri D, Pagnoux C, et al. Marked efficacy of a therapeutic strategy associating prednisone and plasma exchange followed by rituximab in two patients with refractory myopathy associated with antibodies to the signal recognition particle (SRP) Neuromuscul Disord. 2006;16(5):334–336. doi: 10.1016/j.nmd.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 61.Levine TD. Rituximab in the treatment of dermatomyositis: an open-label pilot study. Arthritis Rheum. 2005;52(2):601–607. doi: 10.1002/art.20849. [DOI] [PubMed] [Google Scholar]
- 62.Mok CC, Ho LY, To CH. Rituximab for refractory polymyositis: an open-label prospective study. J Rheumatol. 2007;34(9):1864–1868. [PubMed] [Google Scholar]
- 63.Chung L, Genovese MC, Fiorentino DF. A pilot trial of rituximab in the treatment of patients with dermatomyositis. Arch Dermatol. 2007;143(6):763–767. doi: 10.1001/archderm.143.6.763. [DOI] [PubMed] [Google Scholar]
- 64.Aggarwal R, Bandos A, Reed AM, et al. Predictors of clinical improvement in rituximab-treated refractory adult and juvenile dermatomyositis and adult polymyositis. Arthritis Rheumatol. 2014;66(3):740–749. doi: 10.1002/art.38270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Keir GJ, Maher TM, Ming D, et al. Rituximab in severe, treatment-refractory interstitial lung disease. Respirology. 2014;19:353–359. doi: 10.1111/resp.12214.• Recent retrospective study of 10 patients with severe, progressive myositis-associated interstitial lung disease in which rituximab therapy was associated with improvement.
- 66.Andersson H, Sem M, Lund MB, et al. Long-term experience with rituximab in anti-synthetase syndrome-related interstitial lung disease. Rheumatology (Oxford) 2015 doi: 10.1093/rheumatology/kev004. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 67.Iannone F, Scioscia C, Falappone PC, et al. Use of etanercept in the treatment of dermatomyositis: a case series. J Rheumatol. 2006;33(9):1802–1804. [PubMed] [Google Scholar]
- 68.Muscle Study Group. A randomized, pilot trial of etanercept in dermatomyositis. Ann Neurol. 2011;70(3):427–436. doi: 10.1002/ana.22477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hengstman GJ, van den Hoogen FH, Barrera P, et al. Successful treatment of dermatomyositis and polymyositis with anti-tumor-necrosis-factor-alpha: preliminary observations. Eur Neurol. 2003;50(1):10–15. doi: 10.1159/000070852. [DOI] [PubMed] [Google Scholar]
- 70.Selva-O’Callaghan A, Martínez-Costa X, Solans-Laque R, et al. Refractory adult dermatomyositis with pneumatosis cystoides intestinalis treated with infliximab. Rheumatology (Oxford) 2004;43(9):1196–1197. doi: 10.1093/rheumatology/keh285. [DOI] [PubMed] [Google Scholar]
- 71.Anandacoomarasamy A, Howe G, Manolios N. Advanced refractory polymyositis responding to infliximab. Rheumatology (Oxford) 2005;44(4):562–563. doi: 10.1093/rheumatology/keh539. [DOI] [PubMed] [Google Scholar]
- 72.Hengstman GJ, van den Hoogen FH, van Engelen BG. Treatment of dermatomyositis and polymyositis with anti-tumor necrosis factor-alpha: long-term follow-up. Eur Neurol. 2004;52(1):61–63. doi: 10.1159/000079547. [DOI] [PubMed] [Google Scholar]
- 73.Efthimiou P, Schwartzman S, Kagen LJ. Possible role for tumour necrosis factor inhibitors in the treatment of resistant dermatomyositis and polymyositis: a retrospective study of eight patients. Ann Rheum Dis. 2006;65(9):1233–1236. doi: 10.1136/ard.2005.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dastmalchi M, Grundtman C, Alexanderson H, et al. A high incidence of disease flares in an open pilot study of infliximab in patients with refractory inflammatory myopathies. Ann Rheum Dis. 2008;67(12):1670–1677. doi: 10.1136/ard.2007.077974. [DOI] [PubMed] [Google Scholar]
- 75.Coyle K, Pokrovnichka A, French K. A randomized double blind placebo controlled trial of infliximab in patients with polymyositis and dermatomyositis. Arthritis Res. 2008;58:S293. [Google Scholar]
- 76.Hengstman GJ, De Bleecker JL, Feist E. Open-label trial of anti-TNF-alpha in dermato- and polymyositis treated concomitantly with methotrexate. Eur Neurol. 2008;59(3–4):159–163. doi: 10.1159/000114036. [DOI] [PubMed] [Google Scholar]
- 77.Riolo G, Towheed TE. Anti-tumor necrosis factor inhibitor therapy-induced dermatomyositis and fasciitis. J Rheumatol. 2012;39(1):192–194. [PubMed] [Google Scholar]
- 78.Klein R, Rosenbach M, Kim EJ, et al. Tumor necrosis factor inhibitor-associated dermatomyositis. Arch Dermatol. 2010;146(7):780–784. doi: 10.1001/archdermatol.2010.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ishikawa Y, Yukawa N, Ohmura K, et al. Etanercept-induced anti-Jo-1-antibody-positive polymyositis in a patient with rheumatoid arthritis: a case report and review of the literature. Clin Rheumatol. 2010;29(5):563–566. doi: 10.1007/s10067-009-1370-1. [DOI] [PubMed] [Google Scholar]
- 80.Brunasso AM, Scocco GL, Massone C. Dermatomyositis during adalimumab therapy for rheumatoid arthritis. J Rheumatol. 2010;37(7):1549–1550. doi: 10.3899/jrheum.091413. [DOI] [PubMed] [Google Scholar]
- 81.Catania A, Lonati C, Sordi A, et al. The melanocortin system in control of inflammation. Scientific World Journal. 2010;10:1840–1853. doi: 10.1100/tsw.2010.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Levine T. Treating refractory dermatomyositis or polymyositis with adrenocorticotropic hormone gel: a retrospective case series. Drug Des Devel Ther. 2012;6:133–139. doi: 10.2147/DDDT.S33110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Acthar in treatment of refractory dermatomyositis and polymyositis. Available from: https://clinicaltrials.gov/ct2/show/NCT01906372.
- 84.Lepidi H, Frances V, Figarella-Branger D, et al. Local expression of cytokines in idiopathic inflammatory myopathies. Neuropathol Appl Neurobiol. 1998;24(1):73–79. doi: 10.1046/j.1365-2990.1998.00092.x. [DOI] [PubMed] [Google Scholar]
- 85.Gabay C, Gay-Croisier F, Roux-Lombard P, et al. Elevated serum levels of interleukin-1 receptor antagonist in polymyositis/dermatomyositis A biologic marker of disease activity with a possible role in the lack of acute-phase protein response. Arthritis Rheum. 1994;37(12):1744–1751. doi: 10.1002/art.1780371206. [DOI] [PubMed] [Google Scholar]
- 86.Lundberg I, Ulfgren AK, Nyberg P, et al. Cytokine production in muscle tissue of patients with idiopathic inflammatory myopathies. Arthritis Rheum. 1997;40(5):865–874. doi: 10.1002/art.1780400514. [DOI] [PubMed] [Google Scholar]
- 87.Narazaki M, Hagihara K, Shima Y. Therapeutic effect of tocilizumab on two patients with polymyositis. Rheumatology (Oxford) 2011;50(7):1344–1346. doi: 10.1093/rheumatology/ker152. [DOI] [PubMed] [Google Scholar]
- 88. Kondo M, Murakawa Y, Matsumura T, et al. A case of overlap syndrome successfully treated with tocilizumab: a hopeful treatment strategy for refractory dermatomyositis? Rheumatology (Oxford) 2014;53(10):1907–1908. doi: 10.1093/rheumatology/keu234.• A recent report of a Japanese patient with an overlap syndrome, including features of DM and systemic sclerosis, in whom tocilizumab therapy led to resolution of skin rash and improvement in the muscle weakness and serum creatine kinase elevation.
- 89.Tocilizumab in the treatment of refractory polymyositis and dermatomyositis (TIM) Available from: https://clinicaltrials.gov/ct2/show/NCT02043548.
- 90.Murata K, Dalakas MC. Expression of the costimulatory molecule BB-1, the ligands CTLA-4 and CD28, and their mRNA in inflammatory myopathies. Am J Pathol. 1999;155(2):453–460. doi: 10.1016/s0002-9440(10)65141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nagaraju K, Raben N, Villalba ML, et al. Costimulatory markers in muscle of patients with idiopathic inflammatory myopathies and in cultured muscle cells. Clin Immunol. 1999;92(2):161–169. doi: 10.1006/clim.1999.4743. [DOI] [PubMed] [Google Scholar]
- 92.Musuruana JL, Cavallasca JA. Abatacept for treatment of refractory polymyositis. Joint Bone Spine. 2011;78(4):431–432. doi: 10.1016/j.jbspin.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 93.Arabshahi B, Silverman RA, Jones OY, Rider LG. Abatacept and sodium thiosulfate for treatment of recalcitrant juvenile dermatomyositis complicated by ulceration and calcinosis. J Pediatr. 2012;160(3):520–522. doi: 10.1016/j.jpeds.2011.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Maeshima K, Kiyonaga Y, Imada C, et al. Successful treatment of refractory anti-signal recognition particle myopathy using abatacept. Rheumatology (Oxford) 2014;53(2):379–380. doi: 10.1093/rheumatology/ket251. [DOI] [PubMed] [Google Scholar]
- 95.Kerola AM, Kauppi MJ. Abatacept as a successful therapy for myositis—a case-based review. Clin Rheumatol. 2015;34(3):609–612. doi: 10.1007/s10067-014-2507-4. [DOI] [PubMed] [Google Scholar]
- 96.Thompson B, Corris P, Miller JA, et al. Alemtuzumab (Campath-1H) for treatment of refractory polymyositis. J Rheumatol. 2008;35(10):2080–2082. [PubMed] [Google Scholar]
- 97.Greenberg SA, Pinkus JL, Pinkus GS, et al. Interferon-alpha/beta-mediated innate immune mechanisms in dermatomyositis. Ann Neurol. 2005;57(5):664–678. doi: 10.1002/ana.20464. [DOI] [PubMed] [Google Scholar]
- 98.Walsh RJ, Kong SW, Yao Y, et al. Type I interferon-inducible gene expression in blood is present and reflects disease activity in dermatomyositis and polymyositis. Arthritis Rheum. 2007;56(11):3784–3792. doi: 10.1002/art.22928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Baechler EC, Bauer JW, Slattery CA, et al. An interferon signature in the peripheral blood of dermatomyositis patients is associated with disease activity. Mol Med. 2007;13(1–2):59–68. doi: 10.2119/2006-00085.Baechler. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bilgic H, Ytterberg SR, Amin S, et al. Interleukin-6 and type I interferon-regulated genes and chemokines mark disease activity in dermatomyositis. Arthritis Rheum. 2009;60(11):3436–3446. doi: 10.1002/art.24936. [DOI] [PubMed] [Google Scholar]
- 101. Higgs BW, Zhu W, Morehouse C, et al. A phase 1b clinical trial evaluating sifalimumab, an anti-IFN-α monoclonal antibody, shows target neutralisation of a type I IFN signature in blood of dermatomyositis and polymyositis patients. Ann Rheum Dis. 2014;73(1):256–262. doi: 10.1136/annrheumdis-2012-202794.• A recent Phase Ib double-blinded, controlled clinical trial of sifalimumab in polymyositis and DM, showing clinical improvement correlating with suppression of the interferon signature in blood and muscle tissue.