Abstract
Objective
A causal relationship between removal of circumflex iliac nodes distal to the external iliac nodes (CINDEIN) and lower leg edema has been recently suggested. The aim of this study was to elucidate the incidence of CINDEIN metastasis in cervical cancer.
Methods
A retrospective chart review was carried out for 531 patients with cervical cancer who underwent lymph node dissection between 1993 and 2014. CINDEIN metastasis was pathologically identified by microscopic investigation. After 2007, sentinel lymph node biopsy was performed selectively in patients with non-bulky cervical cancer. The sentinel node was identified using 99mTc-phytate and by scanning the pelvic cavity with a γ probe.
Results
Two hundred and ninety-seven patients (55.9%) underwent CINDEIN dissection and 234 (44.1%) did not. The percentage of International Federation of Gynecology and Obstetrics stage IIb to IV (42.4% vs. 23.5%, p<0.001) was significantly higher in patients who underwent CINDEIN dissection than those who did not. CINDEIN metastasis was identified in 1.9% overall and in 3.4% of patients who underwent CINDEIN dissection. For patients with stage Ia to IIa disease, CINDEIN metastasis was identified in 0.6% overall and in 1.2% of patients who underwent CINDEIN dissection. Of 115 patients with sentinel node mapping, only one (0.9%) had CINDEIN detected as a sentinel node. In this case, the other three lymph nodes were concurrently detected as sentinel lymph nodes.
Conclusion
CINDEIN dissection can be eliminated in patients with stage Ia to IIa disease. CINDEIN might not be regional lymph nodes in cervical cancer.
Keywords: Circumflex Iliac Node, Leg Edema, Lymph Node Excision, Quality of Life, Uterine Cervical Neoplasms
INTRODUCTION
Uterine cervical cancer is the third most commonly diagnosed cancer among women worldwide. Cervical cancer is the fourth leading cause of death from cancer, accounting for 8% (275,100) of total cancer deaths among women in 2008 [1]. In the United States, an estimated 12,900 new cases are expected to be diagnosed and 4,100 are expected to die of cervical cancer in 2015 [2]. Radical hysterectomy with pelvic lymphadenectomy is the preferred treatment for International Federation of Gynecology and Obstetrics (FIGO) stage Ia2, Ib, and IIa lesions [3] and conventional pelvic lymphadenectomy includes removal of the circumflex iliac nodes distal to the external iliac nodes (CINDEIN). CINDEIN are also called circumflex iliac nodes [4], distal external iliac lymph nodes [5], suprafemoral nodes [6], and suprainguinal nodes [7].
Lower leg lymphedema is the most frequent complication after pelvic lymphadenectomy [8,9]. Lymphedema is a chronic generally incurable ailment that requires life-long care and attention, along with psychological support [10]. The median age at diagnosis of cervical cancer is 49 years [11], which means that the remaining lifespan of such young women is much longer than those with other malignancies. In 2007, Abu-Rustum and Barakat [4] suggested a causal relationship between CINDEIN dissection and lower leg lymphedema.
Clinical significance of CINDEIN dissection should be reviewed from the following two points at least: (1) incidence of CINDEIN metastasis and (2) incidence of CINDEIN identified as sentinel lymph nodes. In this study, we investigate these incidences and propose a novel template of pelvic lymph node dissection (PLND) with significant reduction in leg edema.
MATERIALS AND METHODS
1. Patients
A total of 1,027 patients with cervical cancer were treated in the Division of Gynecologic Oncology, Hokkaido Cancer Center, Japan from January 1993 to December 2014. Five hundred and thirty-five patients underwent surgical treatment with PLND but medical records concerning lymph node site were missing in four patients. Finally, 531 patients were included in this study.
2.Surgery
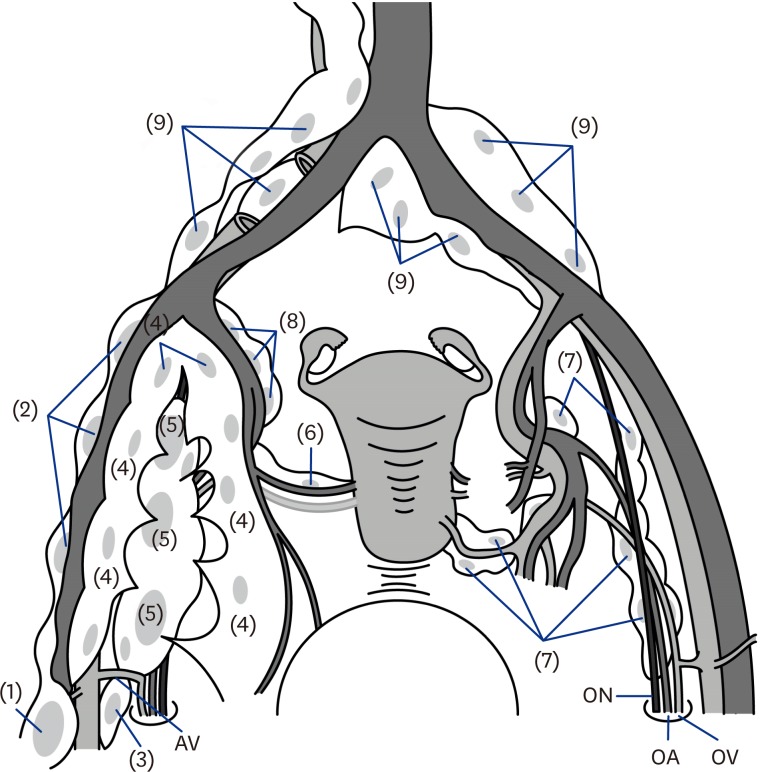
The patients underwent radical hysterectomy, radical trachelectomy or less radical surgery and lymph node dissection. Lymph node dissection included PLND and para-aortic lymph node dissection. Nine pelvic lymph node sites were classified: CINDEIN, external iliac nodes (EIN), circumflex iliac nodes to distal obturator nodes (CINDON), internal iliac nodes (IIN), obturator nodes (ON), cardinal ligament nodes (CLN), sacral nodes (SN), parametrial nodes (PN), and common iliac nodes (CIN).
The definitions of each site are as follows: EIN are located outside a lateral iliac artery and below the level of bifurcation of the common iliac artery. CINDEIN are the most distal EIN. IIN are located on the anterior side of a medial iliac artery below the level of bifurcation of the common iliac artery, between both iliac arteries, and ON are located on the anterior side of an obturator nerve and under the IIN. CINDON are the most distal ON, being located below an anonymous vein. CLN are located on the posterior side of an obturator nerve and usually might be called deep ON or inferior gluteal nodes. SN are located inside medial iliac artery and might be called hypogastric nodes. PN are located along the uterine artery or uterine vein. CIN are located between the level of bifurcation of the common iliac artery and the level of bifurcation of the aorta. They include lymph nodes in the presacral area. Fig. 1 shows the locations of the lymph node sites defined above. During the study period, an aspect of the management of cervical cancer shifted at our institution, with the transitional period happening around 2007. Before 2007, PLND included removal of CINDEIN. After this time, the institutional preference gradually started to eliminate CINDEIN dissection from routine PLND because a causal relationship between CINDEIN dissection and lower leg lymphedema had been suggested [4].
Fig. 1.
Grouping and nomenclature of retroperitoneal lymph nodes. (1) Circumflex iliac nodes distal to the external iliac node; (2) external iliac nodes; (3) circumflex iliac nodes to distal obturator node; (4) internal iliac nodes; (5) obturator nodes; (6) parametrial nodes; (7) cardinal ligament nodes; (8) sacral nodes; (9) common iliac nodes. A.V., anonymous vein; O.A., obturator artery; O.N., obturator nerve; O.V., obturator vein.
3. Sentinel lymph node navigation methods
From 2007 to 2014, 115 patients were subjected to lymphoscintigraphy to detect sentinel lymph nodes. At 20 hours before surgery, each 0.2 mL of 99mTc-phytate (148 MBq) was injected into the subepithelial area of the uterine cervix at the four quadrants: 0, 3, 6, and 9 o’clock positions. Four hours later, lymphoscintigraphy was performed to confirm sentinel node detection. If bilateral clear imaging was not available, blue dye (patent blue) was injected into the cervix during surgery. Intraoperatively, sentinel lymph nodes were scanned with a γ probe (Navigator GPS, Furuno Electric Co. Ltd., Nishinomiya, Japan) and nodes with more than 10-fold counts above the background were identified.
RESULTS
Table 1 shows the clinicopathological characteristics of the 531 patients included in this study. Their median age was 46 years (range, 21 to 79 years). A total of 28 patients (5.3%) were in FIGO stage Ia, 308 (58.0%) in stage Ib, 159 (29.9%) in stage II, 22 (4.1%) in stage III, and 14 (2.6%) in stage IV. Three hundred and forty-six patients (65.2%) had squamous cell carcinoma. Ninety patients (16.9%) received neoadjuvant chemotherapy. One hundred and forty-five patients (27.3%) had lymph node metastasis. The median number of lymph nodes removed was 48.
Table 1. Clinical characteristics of 531 patients with cervical cancer treated with lymph node dissection.
| Characteristic | Value |
|---|---|
| Age (yr) | 46 (21–79) |
| FIGO stage | |
| Ia | 28 (5.3) |
| Ib1 | 255 (48.0) |
| Ib2 | 53 (10.0) |
| IIa | 14 (2.6) |
| IIb | 145 (27.3) |
| III | 22 (4.1) |
| IV | 14 (2.6) |
| Tumor histology | |
| Squamous cell carcinoma | 346 (65.2) |
| Adenocarcinoma | 132 (24.9) |
| Adenosquamous carcinoma | 42 (7.9) |
| Others | 11 (2.1) |
| Chemotherapy before surgery | |
| No | 441 (83.1) |
| Yes | 90 (16.9) |
| Parametrial involvement | |
| Negative | 361 (68.0) |
| Positive | 158 (29.8) |
| Not available | 12 (2.3) |
| Lymph node metastasis | |
| Negative | 386 (72.7) |
| Positive | 145 (27.3) |
| Sentinel lymph node biopsy | |
| Not performed | 416 (78.3) |
| Performed | 115 (21.7) |
| Para-aortic lymphadenectomy | |
| Not performed | 291 (54.8) |
| Performed | 240 (45.2) |
| No. of lymph nodes removed | |
| Total | 48 (1–143) |
| Pelvic lymph node | 44 (1–126) |
| Para-aortic lymph node | 0 (0–64) |
Values are presented as median (range) or number (%).
FIGO, International Federation of Gynecology and Obstetrics.
Table 2 shows the characteristics of the patients with or without CINDEIN dissection. Two hundred and ninety-seven patients (55.9%) underwent CINDEIN dissection and 234 (44.1%) did not. The percentage of FIGO stage IIb to IV (42.4% vs. 23.5%, p<0.001) and lymph node metastasis (31.7% vs. 21.8%, p=0.011) was significantly higher in patients who underwent CINDEIN dissection than those who did not.
Table 2. Characteristics of the patients with or without CINDEIN dissection.
| Characteristic | CINDEIN-dissection surgery (n=297) | CINDEIN-sparing surgery (n=234) | p-value |
|---|---|---|---|
| Age (yr) | 47.6±11.2 | 47.0±12.7 | 0.55 |
| FIGO stage | |||
| Ia–IIa | 171 (57.6) | 179 (76.5) | |
| IIb–IV | 126 (42.4) | 55 (23.5) | |
| Histology | 0.12 | ||
| SCC | 202 (68.0) | 144 (61.5) | |
| NSCC | 95 (32.0) | 90 (38.5) | |
| Parametrial involvement | 0.21 | ||
| Positive | 95 (32.0) | 63 (26.9) | |
| Negative/not available | 202 (68.0) | 171 (73.1) | |
| Lymph node metastasis | 0.011 | ||
| Positive | 94 (31.7) | 51 (21.8) | |
| Negative | 203 (68.3) | 183 (78.2) |
Values are presented as mean±SD or number (%).
CINDEIN, circumflex iliac nodes distal to the external iliac node; FIGO, International Federation of Gynecology and Obstetrics; NSCC, non-squamous cell carcinoma; SCC, squamous cell carcinoma.
Table 3 shows the incidence of lymph node metastasis according to nodal sites. CINDEIN metastasis was observed in 1.9% of patients included in this study and in 3.4% of patients who had CINDEIN pathologically examined. While CINDEIN metastasis was observed in five (5.6%) of 90 patients who received neoadjuvant chemotherapy, it was observed in only five (1.1%) of 441 patients who did not. As for patients with stage Ia to IIa disease, CINDEIN metastasis was observed in 0.6% overall and in 1.2% of patients who had CINDEIN pathologically examined.
Table 3. Incidence of lymph node metastasis according to each subclassified site.
| LN site | All the cases included in this study (N1=531) | Cases of stage Ia–IIa disease (N2=350) | ||||||
|---|---|---|---|---|---|---|---|---|
| No. of patients with metastatic LNs (n1) | No. of patients who had the relevant LNs removed (N1') | Metastatic rate 1* (%) | Metastatic rate 2† (%) | No. of stage Ia–IIa patients with metastatic LNs (n2) | No. of stage Ia–IIa patients who had the relevant LNs removed (N2') | Metastatic rate 3‡ (%) | Metastatic rate 4§ (%) | |
| CIN | 37 | 471 | 7.0 | 7.9 | 11 | 304 | 3.1 | 3.6 |
| IIN | 69 | 519 | 13.0 | 13.3 | 25 | 341 | 7.1 | 7.3 |
| EIN | 40 | 481 | 7.5 | 8.3 | 11 | 308 | 3.1 | 3.6 |
| ON | 81 | 516 | 15.3 | 15.7 | 29 | 341 | 8.3 | 8.5 |
| CINDEIN | 10 | 297 | 1.9 | 3.4 | 2 | 171 | 0.6 | 1.2 |
| CINDON | 6 | 396 | 1.1 | 1.5 | 2 | 246 | 0.6 | 0.8 |
| SN | 22 | 452 | 4.1 | 4.9 | 8 | 286 | 2.3 | 2.8 |
| CLN | 33 | 478 | 6.2 | 6.9 | 9 | 312 | 2.6 | 2.9 |
| PN | 21 | 518 | 4.0 | 4.1 | 8 | 340 | 2.3 | 2.4 |
CIN, common iliac node; CINDEIN, circumflex iliac nodes distal to the external iliac node; CINDON, circumflex iliac nodes to distal obturator node; CLN, cardinal ligament node; EIN, external iliac node; IIN, internal iliac node; LN, lymph node; ON, obturator node; PN, parametrial node; SN, sacral node.
*n1/N1 (N1=531). †n1/N1'. ‡n2/N2 (N2=350). §n2/N2'.
Table 4 shows clinical characteristics of 10 patients who had CINDEIN metastasis. Nine (90%) had FIGO stage II to IV disease. Five (50%) received neoadjuvant chemotherapy and eight (80%) had positive parametrial involvement. Nine (90%) had multiple lymph node metastases and only one (10%) had single lymph node metastasis.
Table 4. FIGO stage and pathological findings of 10 cases with CINDEIN metastasis.
| Case | Age (years) | FIGO stage | Histology | NAC | Parametrial involvement | Positive tumor marker | No. of resected LNs | No. of metastatic LNs | Site of metastatic LN other than CINDEIN | Outcome | OS (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 51 | 2B | SCC | Performed | Negative | SCC 18.9 ng/mL | 31 | 2 | IIN | DID | 105 |
| 2 | 36 | 2A2 | SCC | Performed | Positive | SCC 7.3 ng/mL | 11 | 4 | EIN | DOD | 23 |
| 3 | 46 | 2B | SCC | Performed | Positive | SCC 11.7 ng/mL | 34 | 2 | EIN | DOD | 18 |
| 4 | 50 | 2B | Ad | Not performed | Positive | CEA 144.7 ng/mL | 59 | 8 | CIN, EIN, ON | NED | 104 |
| 5 | 71 | 4B | SCC | Not performed | NA | SCC 10.8 ng/mL | 11 | 11 | EIN, IIN, ON | DOD | 50 |
| 6 | 57 | 2B | SCC | Not performed | Positive | - | 37 | 1 | None | NED | 116 |
| 7 | 56 | 2B | SCC | Not performed | Positive | SCC 94.5 ng/mL | 125 | 121 | PAN, CIN, EIN, IIN, ON, CLN, SN | DOD | 27 |
| 8 | 45 | 4B | Ad | Performed | Positive | CA-125 8,601 U/mL | 41 | 31 | PAN, CIN, EIN, IIN, ON, CLN | DOD | 32 |
| 9 | 65 | 3B | Ad | Performed | Positive | - | 36 | 15 | PAN, CIN, EIN, IIN, ON, CLN, SN | DOD | 8 |
| 10 | 50 | 1B1 | SCC | Not performed | Positive | SCC 2.7 ng/mL | 79 | 3 | CINDON | NED | 10 |
FIGO, International Federation of Gynecology and Obstetrics; Ad, adenocarcinoma; CA-125, cancer antigen 125; CEA, carcinoembryonic antigen; CIN, common iliac node; CINDEIN, circumflex iliac nodes distal to the external iliac node; CINDON, circumflex iliac nodes to distal obturator node; CLN, cardinal ligament node; DID, died of intermittent disease; DOD, died of disease; EIN, external iliac node; IIN, internal iliac node; LN, lymph node; NA, not available; NAC, neoadjuvant chemotherapy; NED, no evidence of disease; ON, obturator node; OS, overall survival; PAN, para-aortic node; SCC, squamous cell carcinoma; SN, sacral node.
Table 5 shows the results of sentinel lymph node mapping. Detection rate of sentinel nodes on the right or left side (at least unilateral) was 87.0%. Bilaterally positive detection was available in 70.4% of cases. The most frequent type of sentinel lymph nodes detected was ON; 52.2% (left side) and 54.8% (right side) were detected in patients with sentinel lymph node navigation. The second most frequent site was IIN. Only one case (0.9%) had CINDEIN detected as a sentinel lymph node. However, the other lymph nodes, including ON, CLN, and PN, were concurrently detected as sentinel lymph nodes. After postoperative pathological examination in this case, we found that maximum tumor size was 44 mm and parametrial involvement was positive but lymph node metastasis was negative.
Table 5. Detection rates of sentinel lymph nodes according to each subclassified site.
| Site | Detection rate (%) | |
|---|---|---|
| Left | Right | |
| Common iliac node | 6.1 | 7.0 |
| Internal iliac node | 23.5 | 25.2 |
| External iliac node | 5.2 | 7.0 |
| Obturator node | 52.2 | 54.8 |
| Circumflex iliac nodes distal to the external iliac node | 0 | 0.9 |
| Circumflex iliac nodes to distal obturator node | 0.9 | 0 |
| Sacral node | 0 | 0 |
| Cardinal ligament node | 2.6 | 0.9 |
| Parametrial node | 5.2 | 4.3 |
| Any lymph node (at least unilateral) | 87 | |
| Any lymph node (bilateral) | 70.4 | |
DISCUSSION
CINDEIN dissection has been conventionally performed as a part of the whole procedure of pelvic lymphadenectomy. However, lymphadenectomy should be tailored to maximize its therapeutic effect and minimize its adverse effects. CINDEIN dissection should be reviewed based on the following three points.
First, CINDEIN dissection might be closely associated with postoperative complications. Since it was suggested that CINDEIN dissection is a plausible etiology of lower leg lymphedema [4], the causal relationship between removal of CINDEIN and lower leg lymphedema was confirmed in cervical cancer [6], endometrial cancer [12,13], and gynecological malignancies [14,15]. We previously reported a sharp decline in the occurrence of lower leg edema after the introduction of CINDEIN-sparing lymphadenectomy into our routine practice. While lymphadenectomy including CINDEIN dissection resulted in >30% occurrence of lower leg edema, CINDEIN-sparing full lymphadenectomy could keep the occurrence of lower leg edema under 10% [13]. CINDEIN are the first intrapelvic lymph nodes that mainly drain lymphatic fluid from the leg. The location of CINDEIN is the most specific among other pelvic lymph nodes, which may explain the increased occurrence of lower leg lymphedema when CINDEIN are removed.
Second, the metastatic rate of CINDEIN is low. Previous studies showed that the percentage of CINDEIN metastasis was 0% to 2.6% in patients with FIGO stage up to IIb [16,17], and 4.0% to 10.1% in patients with pN1 disease [5,7,17]. In our study, the percentage of CINDEIN metastasis was 1.9% in all patients and 3.4% in patients who underwent removal of CINDEIN. As for patients with FIGO stage Ia to IIa disease, the percentage of CINDEIN metastasis was 0.6% in all patients and 1.2% in patients who underwent removal of CINDEIN. It should be noted that the rate of patients who had unfavorable prognostic factors was significantly higher in patients who underwent CINDEIN dissection than those who did not. If all patients underwent removal of CINDEIN, actual rate of CINDEIN metastasis would not have exceeded 3% in all patients included in our study and 1% in patients with stage Ia to IIa disease. Ninety percent of patients with CINDEIN metastasis had multiple lymph node metastases and 80% had positive parametrial involvement. Yin et al. [17] showed that CINDEIN metastases were strongly correlated with metastases of the obturator, external iliac, and IIN [17]. They found that 94% of patients with CINDEIN metastasis were associated with multiple sites of pelvic lymph node metastases, which was compatible with our results. The origin of CINDEIN metastases might not be direct metastases from primary tumor in the cervix, but indirect metastases through regional lymph nodes including the obturator, external iliac, and IIN.
Third, CINDEIN might not be regional lymph nodes in cervical cancer. Several studies reported that CINDEIN are seldom identified as sentinel lymph nodes in cervical cancer [18,19,20,21]. Ouldamer et al. [21] conducted a meta-analysis to determine the frequency of unusual localizations of sentinel lymph nodes in patients with early cervical cancer. In their study, a total of 3,012 sentinel lymph nodes from 1,301 patients were examined. Of these nodes, 83.7% were found in classic areas of the pelvis (i.e., obturator, external iliac, and internal iliac), 6.6% in the common iliac area, 4.3% in the parametrial area, 2.0% in the para-aortic area, 1.3% in the presacral area, 0.2% in the hypogastric area, 0.07% in the inguinal area, and 0.07% in the cardinal ligament (inferior gluteal) area. In this study, only one case (0.9%) had CINDEIN detected as sentinel lymph nodes. However, ON, CLN, and PN were concurrently detected as sentinel lymph nodes in this case. It is possible that the accumulation of 99mTc-phytate in CINDEIN is not caused by direct transition from the cervix, but indirect transition through regional lymph nodes including the ON, CLN, and PN.
These suggest the validity of omitting CINDEIN dissection in the treatment of early cervical cancer. A limitation of the present study was its retrospective observational design. CINDEIN dissection or neoadjuvant chemotherapy was performed at the discretion of the attending physician, which might have had an influence on incidence of CINDEIN metastasis. The rate of CINDEIN metastasis might have been overestimated by selection bias that CINDEIN dissection was closely associated with unfavorable prognostic factors. In contrast, the rate of CINDEIN metastasis might have been underestimated by incorporating subjects with neoadjuvant chemotherapy. Several studies have suggested that CINDEIN dissection is associated with increased occurrence of postoperative lower leg edema. It might be difficult to conduct a further study to validate the incidence of CINDEIN metastasis in cervical cancer because such a study needs CINDEIN dissection. From this point of view, the present manuscript could offer clinical significance to the treatment in early-stage cervical cancer.
In conclusion, CINDEIN might not be regional lymph nodes in cervical cancer. If possible, CINDEIN should be preserved in patients with cervical cancer because preservation of CINDEIN might result in a reduction in the incidence of postoperative lower-extremity lymphedema.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 3.NCCN Clinical Guideline in Oncology. Cervical cancer version 2, 2015 [Internet] Fort Washington, PA: National Comprehensive Cancer Network; c2016. [cited 2016 Apr 13]. Available from: http://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. [Google Scholar]
- 4.Abu-Rustum NR, Barakat RR. Observations on the role of circumflex iliac node resection and the etiology of lower extremity lymphedema following pelvic lymphadenectomy for gynecologic malignancy. Gynecol Oncol. 2007;106:4–5. doi: 10.1016/j.ygyno.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman MS, Parsons M, Gunasekaran S, Cavanagh D. Distal external iliac lymph nodes in early cervical cancer. Obstet Gynecol. 1999;94:391–394. doi: 10.1016/s0029-7844(99)00310-5. [DOI] [PubMed] [Google Scholar]
- 6.Ohba Y, Todo Y, Kobayashi N, Kaneuchi M, Watari H, Takeda M, et al. Risk factors for lower-limb lymphedema after surgery for cervical cancer. Int J Clin Oncol. 2011;16:238–243. doi: 10.1007/s10147-010-0171-5. [DOI] [PubMed] [Google Scholar]
- 7.Matsumoto K, Yoshikawa H, Yasugi T, Onda T, Nakagawa S, Yamada M, et al. Distinct lymphatic spread of endometrial carcinoma in comparison with cervical and ovarian carcinomas. Cancer Lett. 2002;180:83–89. doi: 10.1016/s0304-3835(01)00803-5. [DOI] [PubMed] [Google Scholar]
- 8.Kodama J, Seki N, Ojima Y, Nakamura K, Hongo A, Hiramatsu Y. Risk factors for early and late postoperative complications of patients with endometrial cancer. Eur J Obstet Gynecol Reprod Biol. 2006;124:222–226. doi: 10.1016/j.ejogrb.2005.06.027. [DOI] [PubMed] [Google Scholar]
- 9.Konno Y, Todo Y, Minobe S, Kato H, Okamoto K, Sudo S, et al. A retrospective analysis of postoperative complications with or without para-aortic lymphadenectomy in endometrial cancer. Int J Gynecol Cancer. 2011;21:385–390. doi: 10.1097/IGC.0b013e3182094e09. [DOI] [PubMed] [Google Scholar]
- 10.International Society of Lymphology The diagnosis and treatment of peripheral lymphedema. Consensus document of the International Society of Lymphology. Lymphology. 2003;36:84–91. [PubMed] [Google Scholar]
- 11.National Cancer Institute Surveillance, Epidemiology, and End Results. SEER stat fact sheets: cervix uteri cancer [Internet] Bethesda, MD: National Cancer Institute; 2015. [cited 2016 Apr 13]. Available from: http://seer.cancer.gov/statfacts/html/cervix.html. [Google Scholar]
- 12.Todo Y, Yamamoto R, Minobe S, Suzuki Y, Takeshi U, Nakatani M, et al. Risk factors for postoperative lower-extremity lymphedema in endometrial cancer survivors who had treatment including lymphadenectomy. Gynecol Oncol. 2010;119:60–64. doi: 10.1016/j.ygyno.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Todo Y, Yamazaki H, Takeshita S, Ohba Y, Sudo S, Minobe S, et al. Close relationship between removal of circumflex iliac nodes to distal external iliac nodes and postoperative lower-extremity lymphedema in uterine corpus malignant tumors. Gynecol Oncol. 2015;139:160–164. doi: 10.1016/j.ygyno.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Hareyama H, Hada K, Goto K, Watanabe S, Hakoyama M, Oku K, et al. Prevalence, classification, and risk factors for postoperative lower extremity lymphedema in women with gynecologic malignancies: a retrospective study. Int J Gynecol Cancer. 2015;25:751–757. doi: 10.1097/IGC.0000000000000405. [DOI] [PubMed] [Google Scholar]
- 15.Hareyama H, Ito K, Hada K, Uchida A, Hayakashi Y, Hirayama E, et al. Reduction/prevention of lower extremity lymphedema after pelvic and para-aortic lymphadenectomy for patients with gynecologic malignancies. Ann Surg Oncol. 2012;19:268–273. doi: 10.1245/s10434-011-1863-4. [DOI] [PubMed] [Google Scholar]
- 16.Sakuragi N, Satoh C, Takeda N, Hareyama H, Takeda M, Yamamoto R, et al. Incidence and distribution pattern of pelvic and paraaortic lymph node metastasis in patients with Stages IB, IIA, and IIB cervical carcinoma treated with radical hysterectomy. Cancer. 1999;85:1547–1554. doi: 10.1002/(sici)1097-0142(19990401)85:7<1547::aid-cncr16>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 17.Yin YJ, Li HQ, Sheng XG, Li XL, Wang X. Distribution pattern of circumflex iliac node distal to the external iliac node metastasis in stage IA to IIA cervical carcinoma. Int J Gynecol Cancer. 2014;24:935–940. doi: 10.1097/IGC.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 18.Levenback C, Coleman RL, Burke TW, Lin WM, Erdman W, Deavers M, et al. Lymphatic mapping and sentinel node identification in patients with cervix cancer undergoing radical hysterectomy and pelvic lymphadenectomy. J Clin Oncol. 2002;20:688–693. doi: 10.1200/JCO.2002.20.3.688. [DOI] [PubMed] [Google Scholar]
- 19.Ogawa S, Kobayashi H, Amada S, Yahata H, Sonoda K, Abe K, et al. Sentinel node detection with (99m)Tc phytate alone is satisfactory for cervical cancer patients undergoing radical hysterectomy and pelvic lymphadenectomy. Int J Clin Oncol. 2010;15:52–58. doi: 10.1007/s10147-009-0010-8. [DOI] [PubMed] [Google Scholar]
- 20.Rob L, Strnad P, Robova H, Charvat M, Pluta M, Schlegerova D, et al. Study of lymphatic mapping and sentinel node identification in early stage cervical cancer. Gynecol Oncol. 2005;98:281–288. doi: 10.1016/j.ygyno.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 21.Ouldamer L, Marret H, Acker O, Barillot I, Body G. Unusual localizations of sentinel lymph nodes in early stage cervical cancer: a review. Surg Oncol. 2012;21:e153–7. doi: 10.1016/j.suronc.2012.04.003. [DOI] [PubMed] [Google Scholar]