Abstract
Background
Diffuse parenchymal lung diseases (DPLDs) are common. An accurate diagnosis is essential due to differences in etiology, cli nicopathologic features, therapeutic options and prognosis. Transbronchial lung biopsies (TBLB) are often limited by small specimen size, crush artifact and other factors. Transbronchial lung cryobiopsies (TBLC) are under investigation to overcome these limitations.
Methods
We conducted a retrospective study of 56 patients in a single, tertiary-care academic center in order to compare the yield of both techniques when performed in the same patient. Patients underwent flexible bronchoscopy using moderate sedation with TBLB followed by TBLC in the most radiographically abnormal areas. Clinical data and post-procedural outcomes were reviewed, with a final diagnosis made utilizing a multidisciplinary approach.
Results
The mean age was 60 and 53.6% were male. Co-morbidities included COPD (14%) and prior malignancy (48%). The number of TBLB specimens ranged from 1–10 per patient (mean 4) and size varied from 0.1–0.8 cm. The number of TBLC specimens ranged from 1–4 per patient (mean 2) and size ranged from 0.4–2.6 cm. Both techniques provided the same diagnosis in 26 patients (46.4%). An additional 11 (19.6%) patients had a diagnosis established by adding TBLC to TBLB. Compared to TBLB, TBLC had a higher diagnostic yield in patients with hypersensitivity pneumonitis and interstitial lung disease. Only two patients required video-assisted thoracoscopic surgery (VATS) to establish a diagnosis. Complications included pneumothorax (19.6%) and massive hemoptysis (1.8%).
Conclusions
TBLC used with TBLB can improve the diagnostic yield of flexible bronchoscopy in patients with DPLD.
Keywords: Bronchoscopy, transbronchial biopsy, cryobiopsy, diffuse parenchymal lung disease
INTRODUCTION
Diffuse parenchymal lung diseases (DPLD) comprise a heterogeneous group of over 200 pulmonary disorders that contribute to diffuse and often patchy involvement of the bilateral lung parenchyma. (1) Estimated to occur in up to 15% of the general pulmonary clinic population, DPLDs are characterized by broad differences in etiology, clinicopathologic features, therapeutic options and prognosis. (2) An accurate diagnosis is therefore essential to guide therapy.
A multidisciplinary approach to DPLD is critical. As guidelines suggest, the patients’ clinical presentation, laboratory data and pulmonary function testing is reviewed in conjunction with a radiologist. In cases where high-resolution computed tomographic scans of the chest are inconclusive, biopsies may be required. Surgical lung biopsies have been long considered the gold standard for diagnosis of DPLD. However, not all patients can safely undergo surgery. Bronchoscopic biopsies, especially cryobiopsies, may fit into the diagnostic algorithm in these scenarios.
Transbronchial forceps have been traditionally used for procuring parenchymal biopsies for diagnostic purposes, despite a lower diagnostic yield for conventional forceps estimated at 29% in one study (3). The diagnostic yield is traditionally low in patients with idiopathic pulmonary fibrosis (IPF). Limitations of TBLB include small specimen size, sampling errors, and artifacts. While surgical lung biopsy remains the gold standard for definitive diagnosis, it cannot be safely performed in many patients due to respiratory impairment and medical co-morbidities.
Cryoprobes have been used in the field of bronchoscopy since the 1970s. (4) Initially used for therapeutic tumor debulking and later for “cryorecanalization” of airways, cryobiopsies have been increasingly performed over the past decade for obtaining parenchymal specimens. (5, 6) These biopsies are obtained by utilizing the Joule-Thomson effect, whereby the probe is cooled by release of compressed gas at high flow. The gas, typically carbon dioxide (CO2) or nitric oxide (NO), expands due to the sudden difference in pressure relative to the atmosphere, causing a drop in temperature at the tip of the probe. Adjacent tissue becomes attached to the frozen probe. (7) Purported advantages of the biopsy technique include larger specimens with less artifact. (8, 9) However, the specific etiologies by which cryoprobes routinely improve diagnostic yield are unknown. The aim of this study is to report our experience with TBLC in the diagnosis of patients with DPLD, and to compare the yield of TBLB and TBLC when performed simultaneously in the same patient.
MATERIALS AND METHODS
We performed a retrospective study on all patients who underwent TBLC at our institution between March 2013 and June 2014. All procedures were performed at Yale-New Haven Hospital, a tertiary care academic medical center. Written informed consent was obtained for bronchoscopy with biopsies from all patients. Approval for the study was obtained from the Yale University Human Investigation Committee (HIC# 1406014160).
Our definition of DPLD included diffuse alveolar filling abnormalities or interstitial disease identified by thoracic CT scans obtained as part of the patient’s clinical evaluation. These included traditionally characterized interstitial lung diseases as well as parenchymal disease felt possibly due to drug- or radiation-pneumonitis, autoimmune disease, and others. Patients were typically referred by hospitalists or other pulmonologists who were guiding the patients’ evaluation. Pertinent clinical data at the time of the procedure included age, gender, medical history, medication use and smoking status (Table 1). A number of patients had been followed and then referred for biopsy by expert clinicians specializing in ILD. In these cases, the patient often did not have a definitive prior diagnosis but worsening symptoms and radiographs prompted the request for bronchoscopy. Patients underwent flexible bronchoscopy using moderate sedation with fluoroscopy to guide conventional TBLB and TBLC. Biopsies were not performed if a patient’s platelet count was less than 50,000/uL, the INR was > 1.5, or if they were on medications predisposing to an increased risk of bleeding (Clopidogrel; Warfarin).
Table 1.
Clinical Characteristics of patients undergoing TBLC.
| Clinical Characteristic | |
|---|---|
| Age (SD) | 60 (12) |
| Male gender | 30 (54%) |
| Procedure as outpatient | 38 (68%) |
| Past Medical History | |
| Obstructive lung disease | 16 (28%) |
| ILD | 16 (28%) |
| Pneumothorax | 2 (4%) |
| Autoimmune Disease | 8 (14%) |
| Malignancy | 27 (48%) |
| Heart Disease | 8 (14%) |
| Tobacco Use | |
| Current | 6 (11%) |
| Former | 34 (61%) |
| Never | 16 (29%) |
Procedural Technique
All procedures were performed by a single interventional pulmonologist in a procedure center using conscious sedation with midazolam and fentanyl. Oral anesthesia was accomplished using 1% atomized lidocaine and 2% lidocaine gel. Additional atomized 1% lidocaine was administered with a spray catheter (Olympus PW-6C-1) through the bronchoscope during the procedure. Supplemental oxygen was provided and patients had spontaneous respiration without the support of an artificial airway or assisted ventilation. The nurse and physician monitored the patient throughout the procedure, a technician helped with specimen processing, and anesthesiology was not present.
The bronchoscope (1T180, Olympus, Japan) was introduced orally and an airway inspection was performed. Patients routinely underwent bronchoalveolar lavage (BAL) to assess for infection. Endobronchial biopsies were performed if the mucosa appeared abnormal. Thereafter, fluoroscopy was used to perform parenchymal biopsies. TBLB were performed throughout all lobes in one hemithorax for up to 10 visible specimens. Subsequently, TBLC were performed in the area of the lung that was most radiographically abnormal, as determined by the bronchoscopist. The cryoprobe (2.4 mm diameter, ERBE, Tubingen, Germany) was advanced through the working channel of the bronchoscope and advanced into the parenchyma similar to TBLB forceps. A 4–5 second freeze was performed, after which the bronchoscope and cryoprobe were concurrently withdrawn from the patient. The specimen was removed from the probe into saline and subsequently transferred to formalin. Typically only one biopsy was performed, although up to four were performed if the specimen was visibly inadequate. The bronchoscope was then re-advanced into the airways to assess for and remove blood prior to completion of the procedure. A post-procedural chest x-ray was routinely performed.
Post-Procedural Review
The final clinical diagnosis (Table 2) for each patient was established by a multidisciplinary review of the radiographic diagnosis, the pathologic diagnosis determined by both TBLB and TBLC specimens, and clinical data obtained from the medical records. The patients diagnosed with malignancy in this study did not have a discrete nodule or mass but rather ground glass opacities, non-specific nodules or interstitial changes that would be consistent with lymphangitic spread. For analysis, we separated sarcoidosis, hypersensitivity pneumonitis (HP), organizing pneumonia (OP), malignancy and drug reaction due to their relative numbers and diagnostic yield noted in this study. The broader general term “ILD” encompasses other types of ILD, such as but not exclusively non-specific interstitial pneumonia (NSIP) and usual interstitial pneumonia (UIP). In the former group, with the exception of malignancy, steroids are often a mainstay of therapy. In other types of ILD, including fibrotic NSIP and UIP, steroids are often not useful. Thus, this division of subgroups may be helpful clinically.
Table 2.
Diagnostic Yield for Various DPLDs using TBLB and TBLC.
| Clinical Diagnosis | TBLB and TBLC Similar and Diagnostic | TBLB Diagnostic TBLC Non-Diagnostic |
TBLB Non-Diagnostic TBLC Diagnostic |
Neither TBLB nor TBLC Diagnostic |
|---|---|---|---|---|
| ILD* | 4 | 0 | 3 | 3 |
| OP | 6 | 2 | 1 | 0 |
| HSP | 1 | 0 | 2 | 0 |
| Sarcoid | 1 | 0 | 1 | 1 |
| Malignancy | 5 | 0 | 0 | 0 |
| Drug Reaction | 5 | 1 | 1 | 0 |
| Other** | 4 | 1 | 3 | 11 |
| Total (56) | 26 | 4 | 11 | 15*** |
ILD = Interstitial lung disease; OP = organizing pneumonia; HSP = hypersensitivity pneumonitis
“Other” includes both infectious and non-infectious pneumonias (n=10), normal pathology (n=3), GVHD, hemophagocytic syndrome, extramedullary hematopoiesis, cardiac amyloidosis (no pulmonary involvement), and ABPA. Although biopsies did not reveal a specific diagnosis in 11 of the “other” patients, the diagnosis was made by microbiologic data from BAL or exclusion of other diseases by bronchoscopy.
Of the 15 patients without a clear diagnosis by pathology, only 2 underwent VATS to confirm a diagnosis. Others were diagnosed with bronchoscopic and clinical data.
All radiographs were initially read by a number of radiologists, For this study, CT scans were re-reviewed by an independent, blinded radiologist.. This radiologist was asked to provide a diagnosis based on our sub-groups. Whereas the pathologic diagnosis was also initially provided by a number of pathologists, all samples were re-reviewed by an independent, blinded pulmonary pathologist. The pathologist was asked to determine if the ultimate pathologic diagnosis was defined by TBLB specimens alone, TBLC specimens alone, both TBLB and TBLC, or neither TBLB and TBLC. The non-diagnostic specimens, comprising the latter group, were those in which no specific entity was identified using both biopsy techniques. These included normal parenchyma, non-specific inflammation or non-specific fibrosis. The final clinical diagnosis then incorporated the reviews by the radiologist, pathologist and two investigators (AR, JP) who reviewed the patients’ medical records.
Post-procedural complications were reviewed. The presence of a pneumothorax was acutely assessed by post-procedure radiography. Massive hemoptysis was defined as that requiring therapy beyond application of topical iced saline or epinephrine during the procedure. All charts were reviewed six months following the bronchoscopy to assess for delayed complications.
RESULTS
A total of 56 patients were identified who fulfilled study criteria. The mean age of patients was 60 years, and 53.6% of patients were male. Despite cell count, cultures, cytology and flow cytometry (CD4:CD8 ratio) sent for BAL fluid, results were suggestive of the final clinical diagnosis in 19 cases (34%). The number of TBLB specimens recorded by pathology ranged from 1–10 (average 4) and size per biopsy varied from 0.1–0.8 cm. The number of TBLC ranged from 1–4 per patient (average 2) and the size ranged from 0.4–2.6 cm. Our mean of 4 TBLBs obtained per patient is consistent with recommendations for 4–6 transbronchial biopsies for optimal yield in patients with DPLDs. (10,11)
Of the 56 patients, 45 (80.4%) had a definitive pathologic diagnosis. Both techniques provided the same diagnosis in 26 (46.4% of all cases). An additional 15 (27%) patients had a diagnosis made by only one of the techniques. Whereas 4/56 (7.1%) diagnoses were made only by TBLB, an additional 11/56 (19.6%) diagnoses were established using TBLC. Six patients were diagnosed with infectious processes as a result of bronchoscopy and four had non-specific inflammation. The clinicians caring for the patients determined that all but two patients (96.4%) had clinical diagnoses established by these methods. The other two patients (3.6%) required video-assisted thoracoscopic surgery (VATS) to establish the definitive diagnosis [UIP (Usual Interstitial Pneumonia)/IPF and GVHD (Graft versus Host Disease)].
Compared to TBLB, TBLC had a higher diagnostic yield in patients with non-specific interstitial lung disease (ILD) and hypersensitivity pneumonitis (HP). Specimens obtained by TBLC were larger and had less crush artifact, similar to previous studies. Complications included pneumothorax in 11/56 patients (19.6%) and hemoptysis. Given that cryobiopsies were performed immediately after transbronchial biopsies without an intervening chest radiograph, the pneumothorax may have been caused by either biopsy technique. However, this rate is higher than our traditional pneumothorax rate of less than 2%, suggesting the higher rate was due TBLC. Interestingly, in our study, the rate of pneumothorax did not correlate with a prior history of COPD, or the number or size of biopsies performed per patient. One patient had significant hemoptysis that was managed with iced saline, topical lidocaine with epinephrine, and Fogarty balloon occlusion. No patient required intubation, and there were no procedure-related deaths.
DISCUSSION
Diffuse parenchymal lung disease causes significant morbidity and mortality. When radiographs are insufficient and histology is felt necessary, clinicians are challenged to determine the most appropriate invasive tests. Clinician perceptions are often that TBLB will be insufficient and surgical lung biopsy too risky, thus creating a clinical conundrum. The advent of TBLC has generated enthusiasm as an advance over these techniques, providing a higher diagnostic yield than TBLB with less complications than surgery.
In our study, although BAL was routinely performed, it suggested a diagnosis a minority of the time. The reliability of TBLB is felt to be disease-specific. Whereas malignancy, sarcoidosis and post-transplant pathologic processes are often reliably diagnosed with TBLB, the diagnostic yield is lower for drug toxicity, hypersensitivity pneumonitis, and certain interstitial lung diseases [Usual Interstitial Pneumonia (UIP) and non-specific interstitial pneumonia (NSIP)]. (12) On the other hand, surgical lung biopsies have higher morbidity. Kreider, et al. detailed a 10.7% incidence of hospital re-admission, 5.9% incidence of postoperative mechanical ventilation, 4.4% incidence of mortality, and 19.1% overall incidence of complications following VATS for ILD. They performed a meta-analysis and identified a composite 4.5% rate of mortality in 2223 patients. Overall, patients requiring oxygen, pre-operative ventilation and those with pulmonary hypertension had higher complications. (13)
Previous, mostly retrospective, studies have investigated the use of TBLC for evaluating DPLD, including ILD and the post-transplant population (Table 3). Some investigators use flexible bronchoscopy and moderate sedation whereas others have used general anesthesia, intubation or rigid bronchoscopy. Similarly, some studies have used only cryobiopsies and not conventional forceps biopsies whereas others have not compared forceps to cryobiopsy specimens in the same “per-patient” analysis.
Table 3.
Existing literature regarding use of TBLC as of June 2015.
| Authors | Date | Disease | N | Procedure | Outcome | Complications |
|---|---|---|---|---|---|---|
| Hagmeyer, et al. | 01/2015 | ILD | 32 | General anesthesia Rigid bronchoscopy |
72% definitive diagnosis | Bleeding Severe 53% Mod 25% Pneumothorax 19% |
| Griff, et al. | 11/2014 | DPLD | 52 | Flexible bronchoscopy | 79% diagnostic yield | No bleeding > 3 minutes Pneumothorax 0% |
| Hernandez-Gonzalez, et al. | 11/2014 | ILD | 33 | Flexible bronchoscope | 79% yield | Bleeding Grade 1 9% Grade 2 21% |
| Pajares, et al. | 8/2014 | ILD | 77 | Intubated for TBLC Flexible bronchoscope | TBLC yield higher than TBLB (54.1 vs 29.1%; p=0.038) | Bleeding Grade 1 30.8% Grade 2 56.5% Pneumothorax 7.7% |
| Fruchter, et al. | 7/2014 | ILD | 75 | Flexible bronchoscopy (Only TBLC performed) | 73/75 had abnormal tissue | Bleeding 4% Pneumothorax 2.6% |
| Poletti, et al. | 3/2014 | DPLD | 176 | Unclear | 80% specific pathologic pattern | Bleeding 0% Pneumothorax 23% |
| Casoni, et al. | 2/2014 | ILD | 69 | Rigid bronchoscopy | 76% specific pathologic pattern | Bleeding 1.4% Pneumothorax 28% Death (1 IPF exacerbation) |
| Fruchter, et al. | 12/2013 | Immuno-suppressed | 15 | Flexible bronchoscopy | 80% change in management | Bleeding 6.7% Pneumothorax 0% |
| Kropski, et al. | 11/2013 | DPLD | 25 | Intubated patients | 80% diagnostic yield | Bleeding 0% Pneumothorax 0% |
| Fructer, et al. | 5/2013 | Post-transplant | 40 | Flexible bronchoscopy | Improved yield over TBLB | Bleeding 2.5% Pneumothorax 0% |
| Yarmus, et al. | 3/2013 | Post-transplant | 21 | Rigid and flexible bronchoscopy | TBLC specimens larger and less artifact | Bleeding Grade 1 52.4% |
| Babiak, et al. | 08/2009 | ILD | 41 | Intubated patients Flexible bronchoscopy | Improved yield over TBLB | Bleeding 0% Pneumothorax 4.9% |
Table 3 References In Chronological Order :
1. Hagmeyer L, Theegarten D, Wohlschlager J et al. The role of transbronchial cryobiopsy and surgical lung biopsy in the diagnostic algorithm of interstitial lung disease. Clin Respir J. 2015 Jan 26
2. Griff S, Schonfeld N, Ammenwerth W et al. Diagnostic yield of transbronchial cryobiopsy in non-neoplastic lung disease: a retrospective case series. BMC Pulm Med 2014 Nov 3; 14 (1):171.
3. Hernandez-Gonzalez. Cryobiopsy in the Diagnosis of Diffuse Interstitial Lung Disease: Yield and Cost-Effectiveness Analysis. Arch Bronconeumol. 2014 Nov 3.
4. Pajares V, Puzo C, Castillo D et al. Diagnostic yield of transbronchial cryobiopsy in interstitial lung disease: a randomized trial. Respirology. 2014 Aug;19(6):900–6.
5. Fruchter O, Fridel L, El Raouf BA, et al. Histological diagnosis of interstitial lung diseases by cryo-transbronchial biopsy. Respirology. 2014 Jul;19(5):683–8.
6. Poletti V, Casoni GL, Gurioli C et al. Lung cryobiopsies: a paradigm shift in diagnostic bronchoscopy ? Respirology. 2014 Jul;19(5):645–54.
7. Casoni GL, Tomassetti S, Cavazza A et al. Transbronchial Lung Cryobiopsy in the Diagnosis of Fibrotic Interstitial Lung Diseases. PLos One. 2014 Feb 28; 9(2): e86716
8. Fruchter O, Fridel L, Rosengarten D et al. Transbronchial cryobiopsy in immunocompromised patients with pulmonary infiltrates: a pilot study. Lung 2013 Dec;191(6):619–24.
9. Kropski JA, Pritchett JM, Mason WR et al. Bronchoscopic Cryobiopsy for the Diagnosis of Diffuse Parenchymal Lung Disease. PLos One. 2013 Nov 12;8(11):e78674.
10. Fruchter O, Fridel L, Rosengarten D et al. Transbronchial cryo-biopsy in lung transplantation patients: first report. Respirology.2013 May;18(4):669–73
11. Yarmus L, Akulian J, Gilbert C et al. Cryoprobe transbronchial lung biopsy in patients after lung transplantation: a pilot safety study. Chest. 2013;143(3):621–6.
12. Babiak A, Hetzel J, Krishna G et al. Transbronchial Cryobiopsy: A New Tool for Lung Biopsies. Respiration 2009;78:203–208
Initial experiments determined that activation time and probe size influenced the quantity of tissue obtained by biopsy. (14) In general, compared to TBLB, TBLC specimens are larger, contain more alveoli and have less artifact. (15) In a prospective randomized study by Pajares, et al, the histologic diagnosis was attained significantly more frequently with cryobiopsies than conventional transbronchial biopsies (74.4% vs 34%). (3) Using a multidisciplinary approach to final diagnoses, including radiographic and clinical data, the final diagnostic yield using cryobiopsies was superior to conventional transbronchial biopsies (51 vs 29%). Surgical biopsies were avoided in at least 50% of cases in this study as a result of TBLC. Similarly, in a study by Hagmeyer, et al., 72% of patients were diagnosed using TBLC and did not require surgical lung biopsy. In those who underwent surgical biopsy (n=8), the diagnosis was made in 75%. Following a multidisciplinary review including the surgical biopsies, TBLC showed a strong congruence with the final diagnosis in 78% of patients, an approximate congruence in 19% and no congruence in 3%. (16)
Our study contributes to the literature by emphasizing the complementary role of TBLB and TBLC performed using flexible bronchoscopy and moderate sedation. By performing both techniques in the same patient, we attempt to identify which patients may benefit from the use of the combined techniques. Furthermore, by including patients with idiopathic, exposure-related, connective-tissue disease related and other types of DPLD, we incorporate many disease processes not previously investigated with the TBLC technique. Finally, we performed an independent review of all radiographs and pathologic specimens while incorporating clinical information to establish a final diagnosis based on multidisciplinary investigation.
Although not powered to determine a statistical significance for individual disease processes, our study suggests that TBLC offers an improved diagnostic yield compared to conventional TBLB for patients with suspected ILD and granulomatous diseases such as hypersensitivity pneumonitis and sarcoidosis. These results are similar to those obtained by Babiak, et al (6), who investigated many types of diffuse parenchymal disease, and those investigating ILD shown in Table 3. In contrast, the diagnostic yield of TBLC in patients with diffuse malignancy was not different than TBLB in our investigation. Cases of organizing pneumonia or drug-induced pneumonitis were often diagnosed by both techniques, although the additive process improved the overall yield.
As noted previously, many patients in our study were referred by ILD sub-specialists for bronchoscopy. A prior diagnosis of ILD was suggested in the history by 16 patients (28% of the patient population in this study). Most patients were now referred for progressive radiographic or clinical symptoms that raised questions about their previous diagnosis. Given that many patients with ILD are initially classified by clinical and radiographic findings without biopsies, and that many diseases are progressive by nature, our study demonstrates the potential role of a non-surgical biopsy technique in this scenario.
Our complication rate is similar to that published in the literature. The most troublesome complication was pneumothorax given its rate is significantly higher than that historically obtained by TBLB. There are several explanations, including the larger samples obtained and learning curve of the procedure. Whether a shorter freeze and thaw time or smaller probe would lessen this incidence requires clarification in the future. We experienced bleeding that grossly appeared more frequent and potentially more significant than that due to TBLB. One patient experienced significant bleeding requiring Fogarty balloon occlusion. However, no other patients required any intervention beyond iced saline and topical lidocaine with epinephrine. No patients required intubation as a result of hemoptysis. That being said, additional investigation is required to determine if this procedure is safe when performed by large numbers of bronchoscopists, including those not trained in interventional pulmonology.
As noted previously and demonstrated in Table 3, the approach to performing TBLC varies, including the setting (bronchoscopy arena versus operating room), sedation (moderate sedation and a cooperative patient versus a deeply sedated patient), method of bronchoscopy (flexible versus rigid), and measures to treat complications such as hemoptysis. Although this study did not compare these issues, it was performed using a simple, standard bronchoscopic approach that is easy to replicate. Flexible bronchoscopy performed in a bronchoscopy suite with moderate sedation (fentanyl and midazolam) is less expensive than that performed in an operating room with anesthesiology. Depending on the institution, this approach may be beneficial when scheduling constraints are prominent in the OR. Disadvantages to this approach focus mostly on the risk of complications, namely massive hemoptysis. Although some authors use rigid bronchoscopy and/or preemptively insert endobronchial blockers, we approached TBLC as any other diagnostic procedure. We had nursing, standard monitoring, and equipment available if necessary (intubation equipment, endobronchial blockers, Fogarty balloons). We found that we did not require additional preparation.
Limitations of this study include its retrospective design, performance in a single institution, number of patients and number of operators. The use of TBLC was initiated in our institution at the suggestion of pathology and this study reports our initial experience. We did not compare pathologic results to a surgical gold standard and thus base the diagnostic yield on the new technique (TBLC) compared to our conventional method of biopsy (TBLB). Furthermore, the number of specimens obtained was not consistent for every patient and the location of biopsies was based on the bronchoscopists’ interpretation of radiographic disease severity rather than biopsies consistently being performed in a defined lobe or subsegment. When only one sample was obtained by TBLC, the pathologic diagnosis was undoubtedly limited to the location of the biopsy and did not necessarily reflect the diffuse process. Despite these limitations, our institutional practice has changed with the availability of TBLC. Our algorithm for diagnosing DPLD typically includes a multidisciplinary conference. When the clinical evaluation and imaging fail to provide a diagnosis that strongly supports a particular disease process, bronchoscopy with BAL, TBLB and TBLC is typically performed. Thoracoscopic biopsies are then considered if the patient is a surgical candidate and the diagnosis remains in question. As our experience continues to increase, we hope to answer the many questions that exist regarding TBLC. Future studies need to define patients most likely to benefit, the technical aspects most likely to improve yield while minimizing complications, and the impact of this algorithm on the clinical management of patients with DPLD.
CONCLUSIONS
Patients with DPLD represent a diagnostic challenge. TBLB are often limited by small size and artifact whereas the morbidity of surgical procedures makes clinicians hesitant to pursue this approach in many patients. We believe that further refinement in the use of TBLC may improve the yield of flexible bronchoscopy in DPLDs, thus improving clinical care and avoiding potentially more invasive surgical procedures. Following a multidisciplinary review of a patients clinical and radiographic presentation, we believe that TBLC may be additive to conventional TBLB, but additional studies are required to determine which patients benefit the most from this approach.
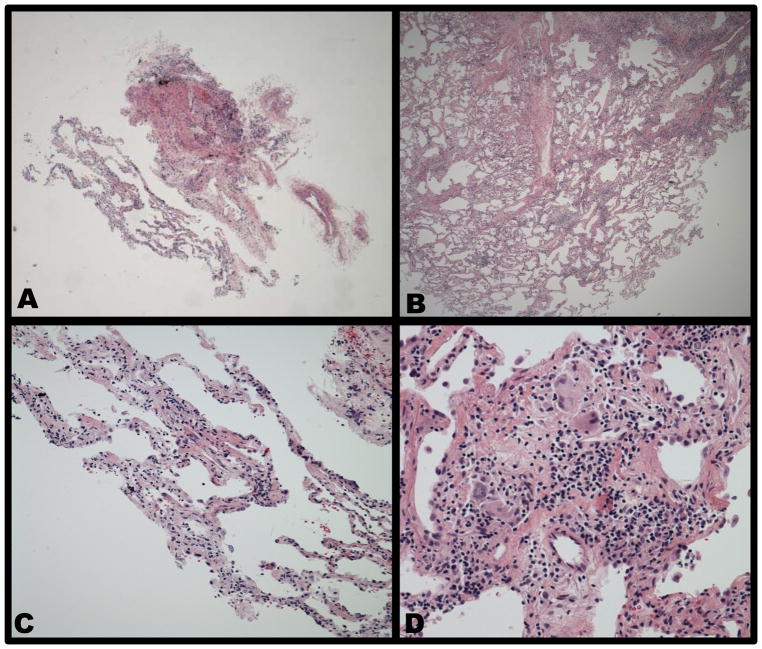
Figure 1. Representative pathology specimens.
(A) This low power demonstrates tissue adequacy obtained by TBLB. (B) This same power in the same patient demonstrates the relative amount of tissue obtained by TBLC. (C) This high power image of TBLB in the same patient demonstrates only non-specific inflammation. (D). This high power specimen obtained by TBLC in the same patient demonstrates ill-defined granulomas with a background of patchy lymphocytes and plasma cells.
Footnotes
Conflicts of Interest: None
References
- 1.Maher TM. A Clinical Approach to Diffuse Parenchymal Lung Disease. Immunol Allergy Clin North Am. 2012 Nov;32(4):453–72. doi: 10.1016/j.iac.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Maher TM. Diffuse parenchymal lung disease. Medicine. 2012;40:314–21. [Google Scholar]
- 3.Pajares V, Puzo C, Castillo D, et al. Diagnostic yield of transbronchial cryobiopsy in interstitial lung disease: a randomized trial. Respirology. 2014 Aug;19(6):900–6. doi: 10.1111/resp.12322. [DOI] [PubMed] [Google Scholar]
- 4.Poletti V, Casoni GL, Gurioli C, et al. Lung cryobiopsies: a paradigm shift in diagnostic bronchoscopy ? Respirology. 2014 Jul;19(5):645–54. doi: 10.1111/resp.12309. [DOI] [PubMed] [Google Scholar]
- 5.Hetzel J, Hetzel M, Hasel C, et al. Old Meets Modern : The use of traditional cryoprobes in the age of molecular biology. Respiration. 2008;76:193–197. doi: 10.1159/000135934. [DOI] [PubMed] [Google Scholar]
- 6.Babiak A, Hetzel J, Krishna G, et al. Transbronchial Cryobiopsy: A New Tool for Lung Biopsies. Respiration. 2009;78:203–208. doi: 10.1159/000203987. [DOI] [PubMed] [Google Scholar]
- 7.Poletti V, Benzaquen S. Transbronchial cryobiopsy in diffuse parenchymal lung disease. A new star in the horizon. Sarcoidosis Vasc Diffuse Lung Dis. 2014 Oct 20;31(3):178–81. [PubMed] [Google Scholar]
- 8.Fruchter O, Fridel L, El Raouf BA, et al. Histological diagnosis of interstitial lung diseases by cryo-transbronchial biopsy. Respirology. 2014 Jul;19(5):683–8. doi: 10.1111/resp.12296. [DOI] [PubMed] [Google Scholar]
- 9.Sunna R. Chapter 33 : Cryotherapy and Cryodebridement. In: Ernst A, Herth FJF, editors. Principles and Practice of Interventional Pulmonology. Springer; New York: 2013. [Google Scholar]
- 10.[Guideline] British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax. 2001 Mar;56(Suppl 1):i1–21. doi: 10.1136/thorax.56.suppl_1.i1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.British Thoracic Society. The diagnosis, assessment and treatment of dffuse parenchymal lung disease in adults. Thorax. 1999;54(Suppl 1):S1–30. doi: 10.1136/thx.54.suppl_1.s1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gal AA. Use and Abuse of Lung biopsy. Adv Anat Pathol. 2005;12:195–202. doi: 10.1097/01.pap.0000175116.40294.83. [DOI] [PubMed] [Google Scholar]
- 13.Kreider ME, Hansen-Flaschen J, Ahmad NN, et al. Complications of video-assisted thoracoscopic lung biopsy in patients with interstitial lung disease. Ann Thorac Surg. 2007 Mar;83(3):1140–4. doi: 10.1016/j.athoracsur.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Franke KJ, Szyrach M, Nilius G, et al. Experimental Study on Biopsy sampling using new flexible cryoprobes: Influence of activation time, probe size, tissue consistency and contact pressure of the probe on the size of the biopsy specimen. Lung. 2009 Aug;187(4):253–9. doi: 10.1007/s00408-009-9156-4. [DOI] [PubMed] [Google Scholar]
- 15.Griff S, Schonfeld N, Ammenwerth W, et al. Diagnostic yield of transbronchial cryobiopsy in non-neoplastic lung disease: a retrospective case series. BMC Pulm Med. 2014;14( 1):171. doi: 10.1186/1471-2466-14-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hagmeyer L, Theegarten D, Wohlschlager J, et al. The role of transbronchial cryobiopsy and surgical lung biopsy in the diagnostic algorithm of interstitial lung disease. Clin Respir J. 2015 Jan 26; doi: 10.1111/crj.12261. [DOI] [PubMed] [Google Scholar]