Abstract
Background
Prior research has shown that high-risk census tracts for out-of-hospital cardiac arrest (OHCA) can be identified. High-risk neighborhoods are defined as having a high incidence of OHCA and a low prevalence of bystander cardiopulmonary resuscitation (CPR). However, there is no consensus regarding the process for identifying high-risk neighborhoods.
Objective
We propose a novel summary approach to identify high-risk neighborhoods through three separate spatial analysis methods: Empirical Bayes (EB), Local Moran’s I (LISA), and Getis Ord Gi* (Gi*) in Denver, Colorado.
Methods
We conducted a secondary analysis of prospectively collected Emergency Medical Services data of OHCA from January 1, 2009 to December 31, 2011 from the City and County of Denver, Colorado. OHCA incidents were restricted to those of cardiac etiology in adults ≥18 years. The OHCA incident locations were geocoded using Centrus. EB smoothed incidence rates were calculated for OHCA using Geoda and LISA and Gi* calculated using ArcGIS 10.
Results
A total of 1102 arrests in 142 census tracts occurred during the study period, with 887 arrests included in the final sample. Maps of clusters of high OHCA incidence were overlaid with maps identifying census tracts in the below the Denver County mean for bystander CPR prevalence. Five census tracts identified were designated as Tier 1 high-risk tracts, while an additional 7 census tracts where designated as Tier 2 high-risk tracts.
Conclusion
This is the first study to use these three spatial cluster analysis methods for the detection of high-risk census tracts. These census tracts are possible sites for targeted community-based interventions to improve both cardiovascular health education and CPR training.
Keywords: Out-of-hospital cardiac arrest, Cardiopulmonary resuscitation, Geographic information systems, Spatial statistics, Public health interventions
1. Introduction
Approximately 420,000 out-of-hospital cardiac arrests (OHCA) occur each year in the United States.1 Research has found that survival rates from OHCA vary widely based on the location where the event occurs.2,3 An important variable in the survival of an OHCA is the victim’s timely receipt of bystander cardiopulmonary resuscitation (CPR), yet only a minority of all OHCA patients receive bystander CPR.4 Bystander CPR is an important link in the American Heart Association’s chain of survival for OHCA. For every 30 people who receive bystander CPR, one additional life will be saved.3 However, recent research has shown that the chance of receiving bystander CPR and surviving after an OHCA can vary drastically from city to city (e.g. 0.2% in Detroit to 16% in Seattle).5,6
Although there is geographic variation in OHCA survival between cities, there is also variation at the neighborhood (census tract) level.7 Bystander CPR prevalence also appears to cluster within cities.8 Using geographic information systems (GIS) and spatial cluster analysis, neighborhoods can be identified as “high-risk,” defined as having higher than expected incidence of OHCA, with corresponding low prevalence of bystander CPR.9,10 The utility of identifying these neighborhoods is the ability to maximize public health resources by tailoring CPR training and cardiac arrest educational programs to neighborhoods that are most in need.11
There are multiple methods for detecting clusters or areas that have statistically significant auto-correlation (e.g., spatial scan statistic12 and Kernel Density13). Each method has its own unique advantages and limitations. Currently, however, there is no consensus regarding the process for identifying these high-risk neighborhoods. As a result, the primary objective of this study was to propose a novel summary approach to identify census tracts using the intersection of three separate spatial analysis methods: Empirical Bayes (EB), Local Moran’s I (LISA) and Getis Ord Gi* (Gi*).
2. Methods
2.1. Data
This study is a secondary analysis of the Cardiac Arrest Registry to Enhance Survival (CARES) dataset for Denver City and County, Colorado. CARES is a secure, standardized, web-based data management system housed at Emory University, funded by the Centers for Disease Control and Prevention (CDC) and the American Heart Association that catalogs every out-of-hospital cardiac arrest of presumed cardiac etiology for which Emergency Medical Services (EMS) provides care. As of 2011, 40 U.S. cities from 25 US states contribute data to CARES. CARES collects a limited number of standardized data elements from the time of 911 call, event characteristics (e.g. location of arrest, witnessed versus unwitnessed arrests, and presumed etiology), resuscitation-specific information (e.g. whether resuscitation was attempted, bystander initiated CPR information, who initiated defibrillation, initial cardiac rhythm, return of spontaneous circulation [ROSC], and prehospital survival status), demographics of the patient (e.g. name, age, date of birth, address of event, sex, and race/ethnicity), emergency department and hospital outcome (e.g. discharge from hospital and neurological status). Further details on the CARES dataset can be found elsewhere.4
The CARES data is submitted with a daily upload of records from Denver EMS’s electronic patient-care record system. Data entry checks have been embedded in the software to help minimize errors and enhance the accuracy of the data collection process. The EMS agency also electronically queries its electronic patient-care record to ensure that all of its resuscitation efforts are reported.
All OHCA events were geocoded (the process of assigning geographic coordinates, e.g., latitude and longitude) based on address information from the CARES registry and each location assigned to a census tract using ArcMap 10.1 (ESRI, Redlands, CA). Census tract level demographic and socio-economic data from the 2010 decennial census were used in conjunction with Census 2010 geographic boundary shapefiles.14 The geocoded OHCA events were joined with demographics for its corresponding census tract. The resulting geographic shapefile contained both CARES registry data (age, race, gender, witnessed arrest, and arrest location) and census data (race, median household income, poverty status, and educational attainment).
2.2. Study population
All adult (≥18 years old) OHCA patients that had a resuscitation attempted by EMS between January 1, 2009 and December 31, 2011 were eligible for inclusion. During the study period 1102 arrests occurred in 142 census tracts in the City and County of Denver, with the final sample including 887 arrests. Arrests were excluded from the final dataset if the address occurred outside of the study area (City and County of Denver; n = 66) or the event occurred in a jail (n = 3), a hospital or health facility (n = 18), or nursing home or “other” location (n = 128), as these locations would presumably have rapid access to bystander CPR.
2.3. Study area
The city and county of Denver has a population of 600,158. It has a consolidated city and county government comprising 78 statistical neighborhoods defined by the Denver Regional Council of Governments (DRCOG) made up of 144 Census Tracts.14 Census tracts are administrative units that have been used as “proxies” for neighborhoods in community and neighborhood level analysis because they are designed to represent social and economically homogenous groups of approximately 2,500 to 8000 persons.15,16 Two census tracts (Tract 9800 and Tract 9801) were removed entirely from the study area because of their designation as industrial areas by the census with resultant population counts of zero. The resulting study area is comprised of 142 census tracts.
2.4. Statistical analysis
2.4.1. Three statistical methods for high-risk neighborhood identification
Neighborhoods were defined as potentially high-risk if the census tract was identified in at least 2 of the 3 spatial analysis methods (EB smoothed OHCA incidence, LISA, and Gi*), and the crude prevalence of bystander CPR was below the mean for CPR prevalence. Because census tract populations can vary dramatically within a county, it is important to reduce the variability that can occur with different base populations. As a result, the Empirical Bayes smoothing method was used to calculate OHCA incidence to compensate for the variability created by differences in base populations. Two additional spatial statistic methods (Local Moran’s I and Gi* statistic) were used to identify clusters of high or low incidence of OHCA. These two spatial statistics allow a census tract’s OHCA incidence to be compared to the OHCA incidence of neighboring census tracts, something that cannot be done with either crude or Empirical Bayes smoothed OHCA incidence rates. Each analysis was run separately, and then the results triangulated to determine the census tracts that appeared in at least two out of the three methods for hot spot analysis and overlapped with census tracts that were below the mean of those receiving bystander CPR. Tier 1 census tracts were identified in all three spatial OHCA clustering methods and tier 2 was identified in 2 out of 3 spatial analysis methods.
2.4.2. Calculation of crude OHCA Incidence for 2009–2011
The incidence of OHCA was determined by dividing the total number of OHCA events in a census tract by the total number of adults 18 years and older that lived in a specific census tract. Because the data incorporated three years, the denominator (population of adults 18 years and older) was multiplied by three.
2.4.3. Crude bystander CPR prevalence
The majority of census tracts had either zero instances or extremely low numbers of bystander CPR occurrence, during the 3-year time period. Based on prior research,9 we used only the crude aggregate bystander CPR prevalence for the 3-year time period. The crude percentages of bystander CPR prevalence were calculated for each census tract by dividing the total number of OHCA victims who received bystander CPR in each census tract by the total number of OHCA incidents over the 3-year time period.
2.4.4. Empirical Bayes smoothed OHCA rates
The EB smoothed OHCA rates were calculated for the three-year study period using the number of OHCA events in each census tract divided by the tract population using the smoothing tool in GeoDa 0.9.9.15, a freely available spatial statistics software package (http://geodacenter.asu.edu).17 The EB smoother adjusted values toward the mean of the observed data with the amount of shrinkage toward the mean being inversely proportional to the size of the overall at risk population.18,19 Census tracts with large populations experienced smaller amounts of adjustment toward the mean than census tracts with small populations. Smoothed data values are therefore stabilized in areas with small populations with unstable rates which accounts for the geographic “small numbers” problem.20 The EB smoothed OHCA rates were categorized into quintiles. Census tracts were defined as high-risk if the EB smoothed OHCA rates were in the top quintile.
2.4.5. Local Moran’s I statistic (LISA)
The LISA measured the similarity between census tracts and calculated values both within and across geographic boundaries while additionally identifying spatial outliers.21,22 The LISA calculates local index values, z-scores, and p-values. The z-scores and p-values measure the computed local index value and provide a measure of statistical significance. Census tracts with statistically significant positive z-scores indicate areas surrounded by areas with similar OHCA rates – either similarly high or similarly low (positive spatial autocorrelation). These are designated “High–High” (HH) or “Low–Low” (L-L) in the maps. Conversely, census tracts with statistically significant negative z-scores indicate areas surrounded by dissimilar values (negative spatial autocorrelation). These are designated as “High–Low” (HL) or “Low–High” (LH) in the maps.
The LISA was calculated using first order polygon contiguity in the ArcMap 10.1 Spatial Statistics toolbox. First order polygon contiguity designated that only neighboring census tracts that shared a boundary would influence the calculation for each census tract. The LISA statistics were run on the crude OHCA incidence by census tract. Clusters with high OHCA incidence (areas that have incidence values of similar magnitude) for the aggregated study period were identified as “Hot Spots” while clusters of features with low incidence are referred to as “Cold Spots.” Clusters of census tracts with high OHCA were those with significant p-value ≤0.5.
2.5. Getis-Ord Gi* statistic (Gi* statistic)
The Gi* statistic identified areas where incidents with either high or low values cluster spatially by looking at each census tract within the context of its neighboring census tract.23,24 Unlike LISA, the Gi* statistic did not identify the similarity of values to their surrounding neighbors. We calculated Gi* using the Cluster and Outlier Analysis tool from the Mapping Clusters toolset of the ArcGIS 10.1 Spatial Statistics Tools toolbox. The crude OHCA incidence by census tracts was analyzed using first order polygon contiguity which designated that only neighboring census tract that shared a boundary would influence the value calculation for each census tract. The z-scores and their associated p-values indicated the statistical significance with which the census tract was part of a spatial cluster of high or low values. The higher the z-score the more intense the clustering of high values (hot spot); the smaller the z-score the more intense the clustering of low values (cold spots). Census tracts with z-scores greater than 1.96 were chosen as high OHCA clusters.
3. Results
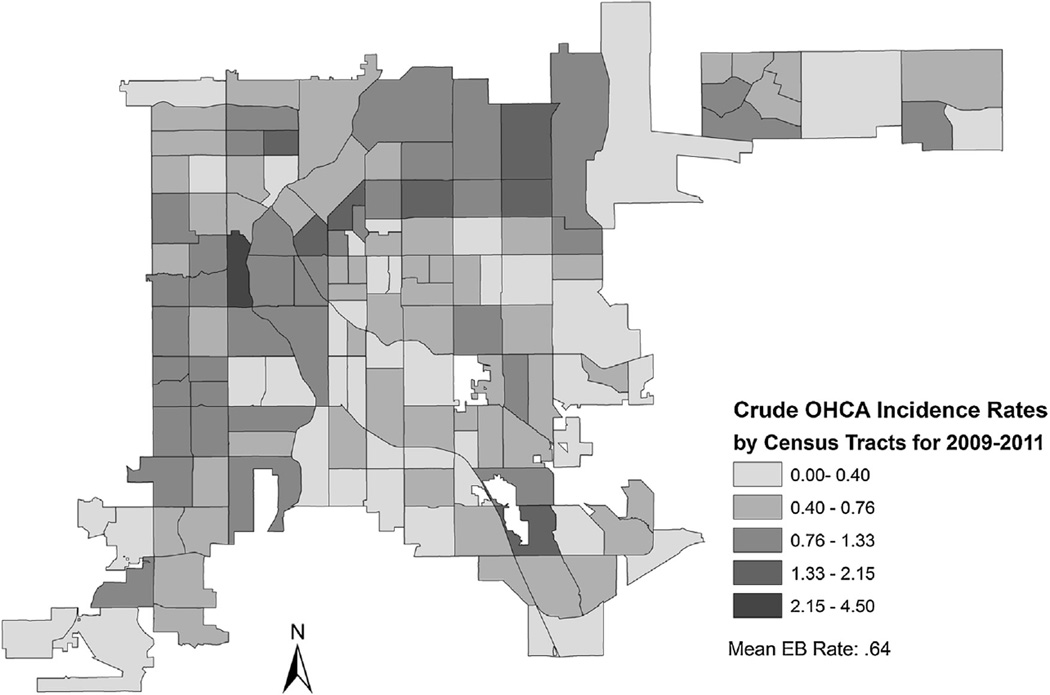
A total of 1102 arrests in 142 census tracts occurred during the study period, with 887 arrests included in final sample. Of the 887 arrests, 17.5% (n = 155) of the cardiac arrest victims received bystander CPR. The mean crude OHCA incidence for Denver County was 0.67 per 1000 people and the mean CPR prevalence was 19.0%. All 12 of the identified high-risk census tracts had a crude OHCA incidence that was higher than the Denver County mean. Fig. 1 shows the distribution of crude OHCA incidence during the three-year study period. Table 1 describes the baseline demographics and characteristics of the 887 OHCA events.
Fig. 1.
Incidence of Cardiac Arrest by Census Tract.
Table 1.
Characteristics of study sample.
| 2009–2011 OHCA Descriptive Statistics (n = 887) |
n (%) | |
|---|---|---|
| Mean age | 60.9 years | |
| Race | Hispanic | 99 (11.2) |
| White | 276 (31.1) | |
| Black | 117 (13.2) | |
| Asian | 10 (1.2) | |
| American Indian | 10 (1.2) | |
| Native Hawaiian | 2 (0.1) | |
| Unknown | 373 (42.0) | |
| Bystander CPR | Lay person medical provider | 15 (1.7) |
| Lay person family member | 78 (8.8) | |
| Layperson | 62 (7.0) | |
| EMS personnel | 59 (6.6) | |
| First responder | 558 (63.0) | |
| Responding EMS personnel | 108 (12.2) | |
| Arrest after EMS arrived | 7 (0.7) | |
| AED used | Yes | 236 (26.6) |
| No | 80 (9.0) | |
| Present but not used | 264 (29.8) | |
| Unknown | 307 (34.6) | |
| Survival to discharge | Discharged alive | 94 (10.6) |
| Died in hospital | 167 (18.8) | |
| Patient made DNR | 14 (1.6) | |
| Unknown | 2 (0.2) | |
| Not applicable | 610 (68.8) | |
| Neurological outcome | Good cerebral performance | 71 (8.0) |
| Moderate cerebral disability | 20 (2.3) | |
| Severe cerebral disability | 4 (0.5) | |
| Coma, vegetative state | 2 (0.1) | |
| Not applicable | 790 (89.1) |
3.1. OHCA results
3.1.1. EB smoothed OHCA incidence analysis
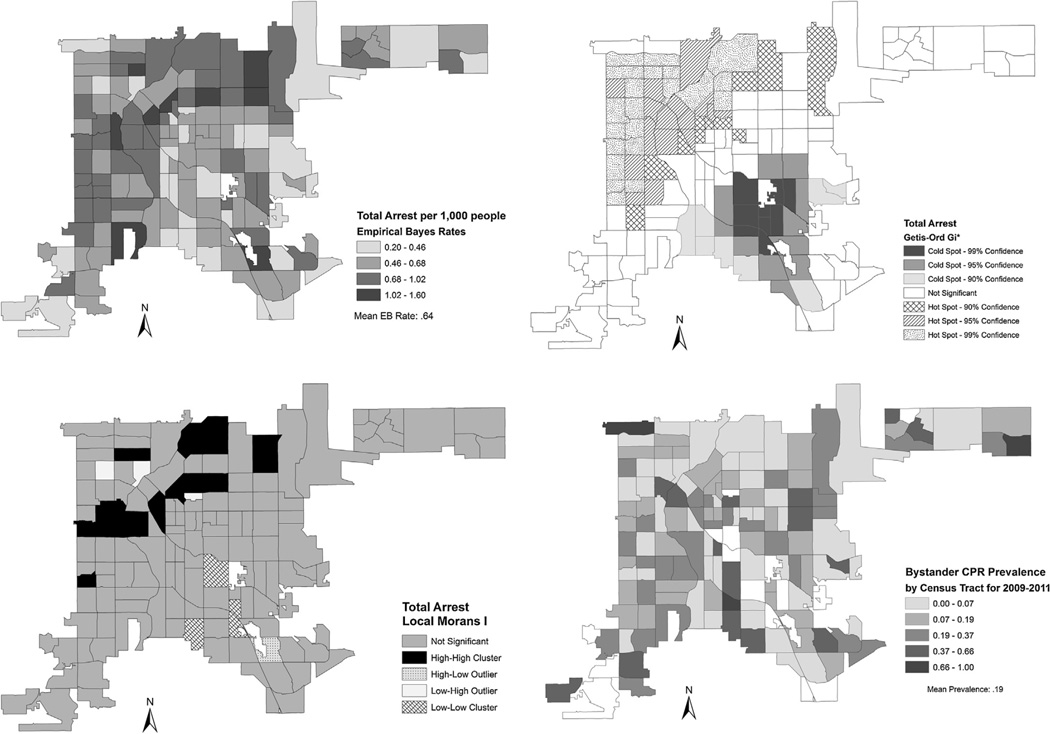
The EB smoothed OHCA rates ranged from 0.20 to 1.60/1000 people. There were 9 census tracts that were in the highest quintile (1.02–1.60/1000) and were considered high OHCA incidence census tracts (Fig. 2a).
Fig. 2.
Cardiac Arrest Incidence Using Empirical Bayes, Getis-Ord, Local Moran’s I and Crude Bystander CPR.
3.1.2. Local Moran’s I analysis
LISA identified 17 census tracts with high rates of OHCA incidence. The majority of the 17 census tracts identified by LISA as clusters of high OHCA incidence (16 out of 17) were categorized by ArcGIS as HH (high clusters neighboring with other census tract with high clusters). The remaining 1 census tract designated as having a cluster of high OHCA incidence was categorized as HL (high clusters neighboring with census tracts with clusters of low incidence of OHCA). All 16 of these LISA designated HH census tracts were located in the northeastern to northwestern part of the City and County of Denver. The HL designated tract was located in the southern portion of Denver County (Fig. 2b).
3.1.3. Gi* analysis
The Gi* analysis identified 48 clusters of census tracts with a high rate of OHCA incidence. Eleven census tracts were in the 90% significance level, 16 were in the 95% significance level and 21 were identified in the 99% significance level. Fourteen out of the 48 census tracts were the same tracts identified by LISA in northern Denver (Fig. 2c).
3.2. Bystander CPR results
3.2.1. Crude bystander CPR prevalence
Crude bystander CPR prevalence ranged from 0 to 1. Prevalence below the mean for Denver County (0.19) was used to identify census tracts with the lowest bystander CPR prevalence Fig. 2d. Seventy-one census tracts were identified as having low prevalence of bystander CPR using this method.
3.2.2. High-risk census tracts
Using three spatial analysis techniques, we identified tier 1 and tier 2 areas with relatively high rates of cardiac arrest, and relatively low prevalence of bystander CPR. Tier 1 neighborhoods were identified in all three spatial analysis methods, while tier 2 neighborhoods were identified in two out of three spatial analysis methods. Fig. 3 shows the twelve high-risk neighborhoods that were identified using this approach. Table 2 lists the socioeconomic- demographic data for each neighborhood as compared to the mean for the City and County of Denver. The neighborhoods comprised primarily of Latino and African-American residents with a median household income ranging from $8015 to $57,689.
Fig. 3.
Tier 1 and 2 High-Risk Census Tracts.
Table 2.
Characteristics of high-risk neighborhoods.
| Neighborhood | Tract ID | Total arrest crude rate per 1000 |
Total arrest EB rate per 1000 |
Bystander CPR crude prevalence |
% White | % African American |
% Hispanic | Median age, years |
Median household income ($) |
% of High School Grad or higher |
|---|---|---|---|---|---|---|---|---|---|---|
| Tier 1 | ||||||||||
| Sunnyside | 11.01 | 1.58 | 1.09 | 0.13 | 19.8 | 5.6 | 72.9 | 31.4 | 32,769 | 60.8 |
| Five Points | 24.03 | 1.40 | 1.08 | 0.09 | 36.4 | 31.5 | 27.8 | 32.5 | 31,195 | 78.8 |
| Sun Valley | 8 | 1.59 | 4.50 | 0.00 | 21.6 | 24.6 | 39.0 | 16.1 | 8015 | 63.5 |
| West Colfax | 7.02 | 1.20 | 1.00 | 0.15 | 18.1 | 3.5 | 77.3 | 27.7 | 31,380 | 74.5 |
| Westwood | 45.03 | 1.33 | 1.02 | 0.00 | 15.0 | 0.0 | 80.4 | 27.1 | 31,500 | 45.8 |
| Tier 2 | ||||||||||
| Northeast Park Hill | 41.02 | 1.75 | 1.31 | 0.15 | 11.6 | 59.0 | 24.6 | 34.0 | 28,867 | 75.7 |
| Skyland | 36.03 | 2.00 | 1.39 | 0.08 | 22.1 | 46.2 | 20.5 | 37.9 | 42,396 | 86.2 |
| Elyria Swansea | 35 | 0.98 | 0.86 | 0.00 | 11.3 | 7.8 | 78.8 | 26.6 | 28,528 | 47.1 |
| Whittier | 23 | 1.17 | 0.98 | 0.14 | 38.3 | 40.2 | 16.3 | 32.4 | 39,432 | 84.9 |
| Lincoln Park | 19.01 | 1.22 | 0.92 | 0.17 | 35.1 | 22.2 | 36.0 | 27.3 | 17,373 | 66.5 |
| Sunnyside | 4.01 | 1.03 | 0.86 | 0.17 | 42.2 | 2.3 | 51.8 | 34.8 | 35,469 | 81.1 |
| Villa Park | 9.04 | 1.06 | 0.90 | 0.08 | 15.7 | 0.3 | 83.9 | 29.3 | 24,907 | 57.0 |
| Denver County | 0.67 | 0.64 | 0.19 | 52.7 | 10.4 | 31.5 | 33.7 | 49,091 | 85.1 |
4. Discussion
This is the first study to utilize a novel summary approach to identify high-risk OHCA neighborhoods. This combination approach uses the strengths of three separate analytical spatial clustering methods in order to identify areas which were hot spots for cardiac arrest, and were below the mean for bystander CPR prevalence. Consistent with prior research,7–10,25 these neighborhoods were comprised of lower-income, primarily African-American and Latino residents.
This type of spatial analysis may change how public health resources are targeted throughout the country. Rather than blanketing a city with CPR training, our research shows that neighborhoods can be identified where the need is greatest, and the potential impact of targeted CPR training could be most effective. Prior research has shown that neighborhoods comprising lower-income, African-American residents are most at risk for not receiving bystander CPR.25 Our research takes this one step further by identifying specific neighborhoods within Denver County that should be targeted for community-based CPR training interventions. We found that the Lincoln Park neighborhood was considered high-risk. This area has a high proportion of white residents, and would not have been identified by as a target for CPR training if we had only focused on lower-income, African-American neighborhoods. This highlights the importance of using data to drive systematic, targeted training in the highest-risk neighborhoods.
Our work has significant policy implications. There is a growing body of evidence for targeting training when resources are limited (e.g. CPR training), including a recent Science Advisory from the American Heart Association.11 We believe that this novel, systematic spatial analytical approach may be a new manner in which high-risk neighborhoods can be identified. This type of hot spot analysis could also be important in identifying high-risk neighborhoods for other acute, time-sensitive conditions such as myocardial infarction and stroke. Although the majority of research identifies disease-specific conditions, we could presumably integrate these maps in order to fully understand the health and wellness of our neighborhoods. This more complete picture of health, driven by GIS-based analyses, would allow us to design and implement targeted neighborhood-based interventions that would improve both morbidity and mortality in these areas.
There are some limitations to this study. We used census tract as a proxy for neighborhood. This allowed us to examine the underlying demographics and composition of these areas. Future research could use community-based land use surveys to identify true neighborhoods within an area. We also chose to use three common spatial analysis methods. Each of these methods has its own strengths and weaknesses. Therefore, we decided to use a summary approach that would allow us to draw conclusions based on triangulating these three methodologies, rather than just picking one. Also, the bystander CPR prevalence within Denver County is below the national average, so the applicability of the results may be of concern. However, this is actually a strength of the triangulated approach to identify high-risk census tracts. Even in a city which has a high bystander CPR prevalence (e.g. Seattle), this method can be used to identify those census tracts that fall below the average bystander CPR prevalence within Seattle which may be target areas for CPR education and training. Finally, we did not separate OHCA events by public or private events. However, prior data has shown that more than 80% of events occur at home.4 It is possible that certain areas could be high-risk given that they have larger daytime populations (e.g. busy downtown district). However, the majority of the high-risk neighborhoods that we identified were in fact residential primarily.
5. Conclusion
Using a novel summary approach, we have identified high-risk neighborhoods in the City and County of Denver. This research allows us to triangulate areas based on multiple spatial analytical approaches, with the idea that a truly high-risk neighborhood will be identified using all three methods. Future research will need to be conducted to test the effectiveness of a community-based CPR intervention targeted to the highest-risk neighborhoods we have identified. Ultimately, this type of targeted approach to CPR training focuses on the areas where the impact can be greatest. This may serve as a model for other public health conditions.
Acknowledgments
This study was supported by NIH/NCATS Colorado CTSI Grant Number UL1 TR001082. Contents are the authors’ sole responsibility and do not necessarily represent official NIH views. Dr. Haukoos is supported by AHRQ grants R01AI106057, R01HS021749, and K02HS017526. Dr. Magid currently receives grant funding from the Agency for Healthcare Research and Quality (AHRQ), National Health Lung and Blood Institute (NHLBI), National Institute on Aging (NIA), National Center for Advancing Translational Science (NCATS), American College of Cardiology Foundation (ACCF), Amgen, and the Patient Centered Outcome Research Institute (PCORI).
Footnotes
A Spanish translated version of the summary of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2014.08.029.
Conflict of interest statement
No conflicts of interest to declare.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e92. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 4.McNally B, Robb R, Mehta M, et al. Out-of-Hospital Cardiac Arrest Surveillance – Cardiac Arrest Registry to Enhance Survival (CARES), October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;31:1–19. [PubMed] [Google Scholar]
- 5.Dunne RB, Compton S, Zalenski RJ, Swor R, Welch R, Bock BF. Outcomes from out-of-hospital cardiac arrest in Detroit. Resuscitation. 2007;72:59–65. doi: 10.1016/j.resuscitation.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Rea TD, Crouthamel M, Eisenberg MS, Becker LJ, Lima AR. Temporal patterns in long-term survival after resuscitation from out-of-hospital cardiac arrest. Circulation. 2003;108:1196–1201. doi: 10.1161/01.CIR.0000087403.24467.A4. [DOI] [PubMed] [Google Scholar]
- 7.Sasson C, Keirns CC, Smith D, et al. Small area variations in out-of-hospital cardiac arrest: does the neighborhood matter? Ann Intern Med. 2010;153:19–22. doi: 10.1059/0003-4819-153-1-201007060-00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Root ED, Gonzales L, Persse DE, Hinchey PR, McNally B, Sasson C. A tale of two cities: the role of neighborhood socioeconomic status in spatial clustering of bystander CPR in Austin and Houston. Resuscitation. 2013;84:752–759. doi: 10.1016/j.resuscitation.2013.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sasson C, Cudnik MT, Nassel A, et al. Identifying high-risk geographic areas for cardiac arrest using three methods for cluster analysis. Acad Emerg Med. 2012;19:139–146. doi: 10.1111/j.1553-2712.2011.01284.x. [DOI] [PubMed] [Google Scholar]
- 10.Sasson C, Keirns CC, Smith DM, et al. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation. 2011;82:674–679. doi: 10.1016/j.resuscitation.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sasson C, Meischke H, Abella BS, et al. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–1350. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
- 12.Kuldorff M. A spatial scan statistic. Commun Stat Theory Methods. 1997;26:1487–1496. [Google Scholar]
- 13.Waller L, Gotway C. Applied spatial statistics for public health data. New York: Wiley; 2004. [Google Scholar]
- 14.U.S. Census Bureau: State and County QuickFacts. [accessed May 20];2012 http://quickfacts.census.gov/qfd/states/39/3918000.html.
- 15.Krieger N. Place, space, and health: GIS and epidemiology. Epidemiology. 2003;14:384–385. doi: 10.1097/01.ede.0000071473.69307.8a. [DOI] [PubMed] [Google Scholar]
- 16.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57:186–199. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anselin L, Syabri I, Kho Y. GeoDa: an introduction to spatial data analysis. Geogr Anal. 2006;38:5–22. [Google Scholar]
- 18.Hayward RA, Heisler M, Adams J, Dudley RA, Hofer TP. Overestimating outcome rates: statistical estimation when reliability is suboptimal. Health Serv Res. 2007;42:1718–1738. doi: 10.1111/j.1475-6773.2006.00661.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using stata. 2nd. College Station: Stata Press; 2008. [Google Scholar]
- 20.Cromley E, McLafferty S. GIS and public health. 2nd. New York, NY: The Guilford Press; 2012. [Google Scholar]
- 21.Anselin L. Local indicators of spatial association – LISA. Geogr Anal. 1995;27:93–115. [Google Scholar]
- 22.Anselin L. Exploring spatial data with GeoDa: a workbook. Urbana-Champaign: University of Illinois; 2004. [Google Scholar]
- 23.Li H, Calder CA, Cressie NAC. Beyond Moran’s I: testing for spatial dependence based on the spatial autoregressive model. Geogr Anal. 2007;39:357–375. [Google Scholar]
- 24.Li H, Calder CA, Cressie NAC. One-step estimation of spatial dependence parameters: properties and extensions of the APLE statistic. J Multivariate Anal. 2012;105:68–84. [Google Scholar]
- 25.Sasson C, Magid DJ, Chan P, et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]