Abstract
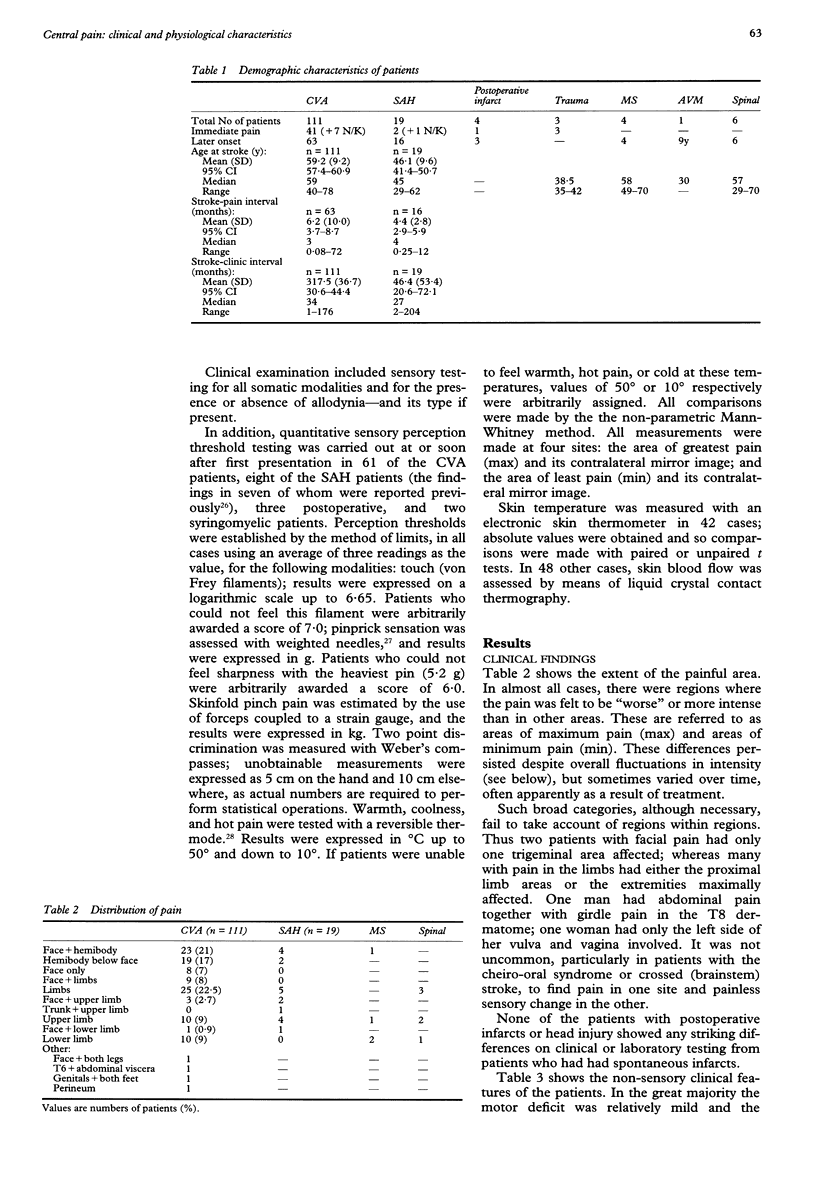
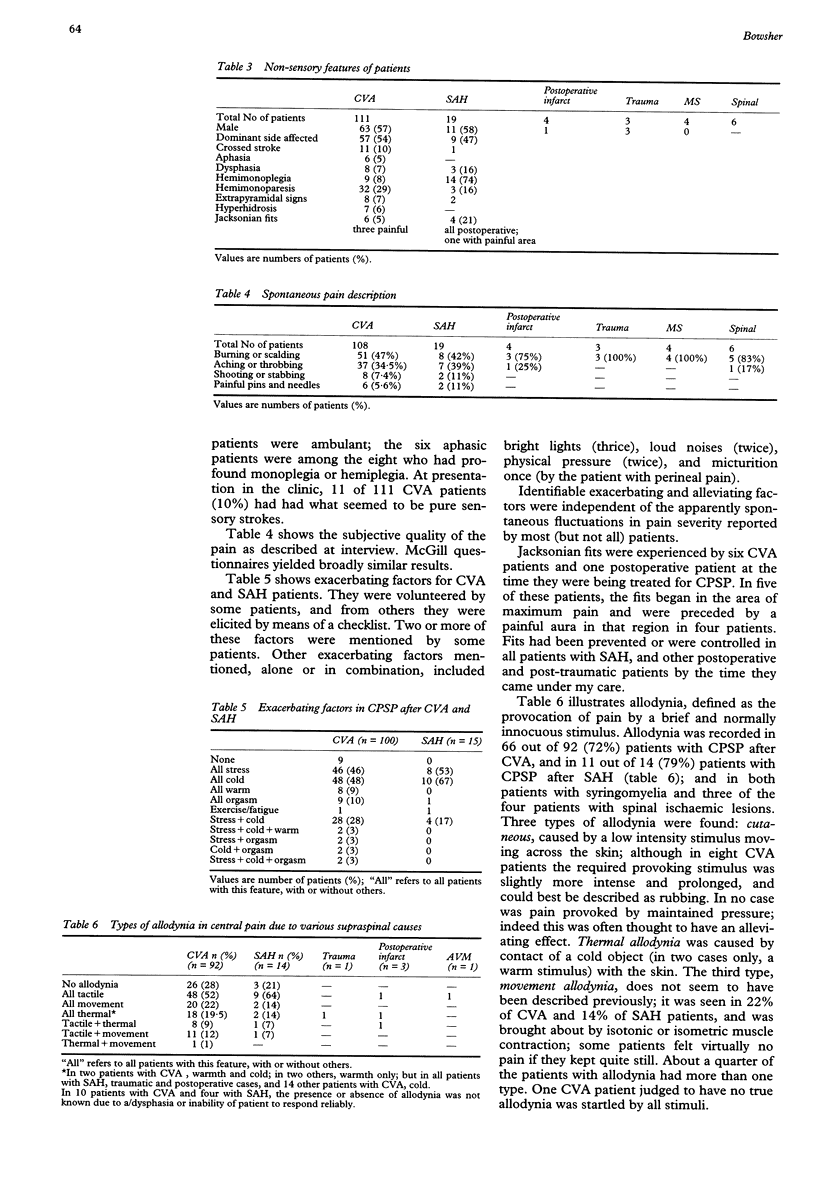
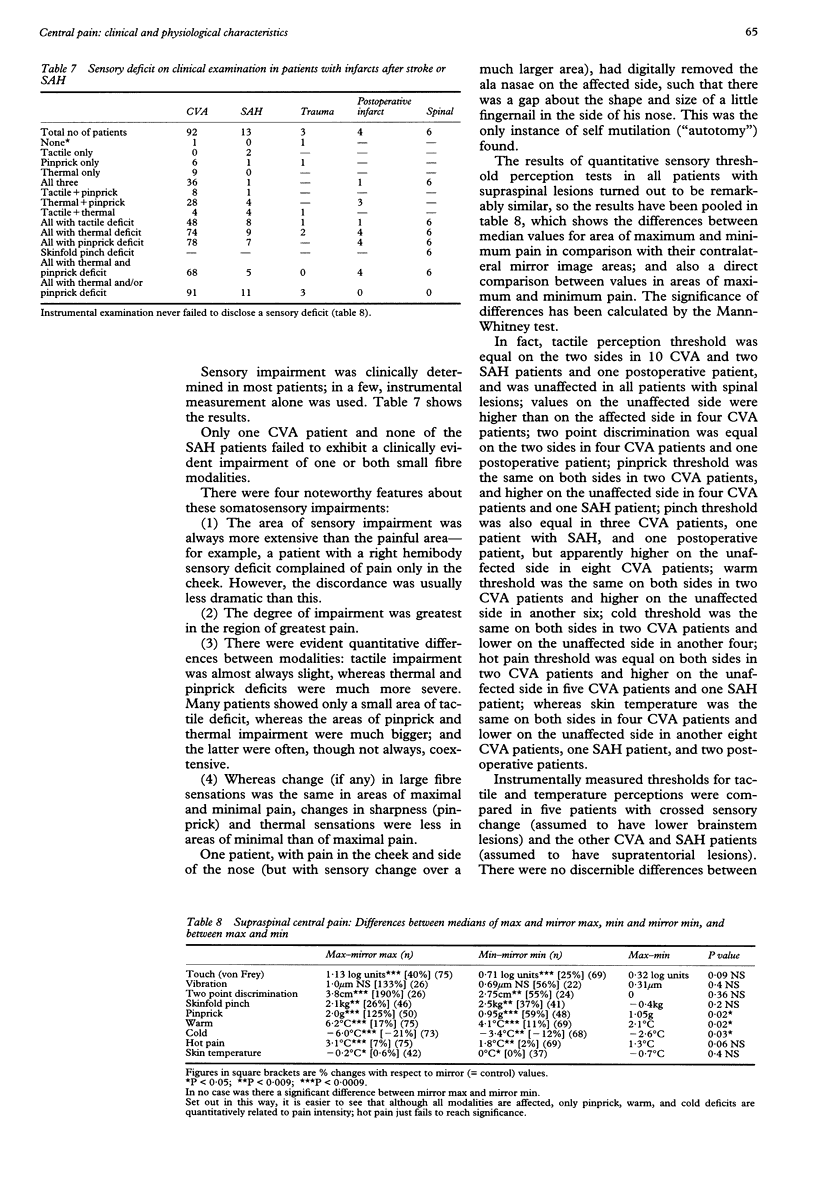
OBJECTIVES--To study the clinical and pathophysiological features of central pain due to damage to the CNS. METHODS--156 patients (mostly with ischaemic strokes, some with infarct after subarachnoid haemorrhage and other cerebral conditions; one with bulbar and others with spinal pathology) with central pain have been investigated clinically and varying numbers instrumentally with respect to quantitative somatosensory perception thresholds and autonomic function. RESULTS--Pain onset was immediate in a minority; and from a week or two up to six years in > 60%. For those with supraspinal ischaemic lesions, the median age of onset was 59; dominant and non-dominant sides were equally affected. Two thirds of the patients had allodynia, including a previously undescribed movement allodynia apparently triggered from group I afferents. Most patients exhibited autonomic instability in that their pain was increased by physical and emotional stress and alleviated by relaxation; cutaneous blood flow and sweating may also be affected. Pain occurred within a larger area of differential sensory deficit. The critical deficit seems to be for thermal and pinprick sensations, which were more pronounced in areas of greatest than in areas of least pain; whereas low threshold mechanoceptive functions, if affected, did not vary between areas of greatest and least pain. Skinfold pinch (tissue damage) pain thresholds were only slightly affected in supraspinal cases, but greatly increased in patients with spinal lesions; thermal (heat) pain did not show this dissociation. CONCLUSION--The pathogenetic hypothesis which seems best to fit the findings is that there is up regulation or down regulation of receptors for transmitters, possibly mainly noradrenergic, over time.
Full text
PDF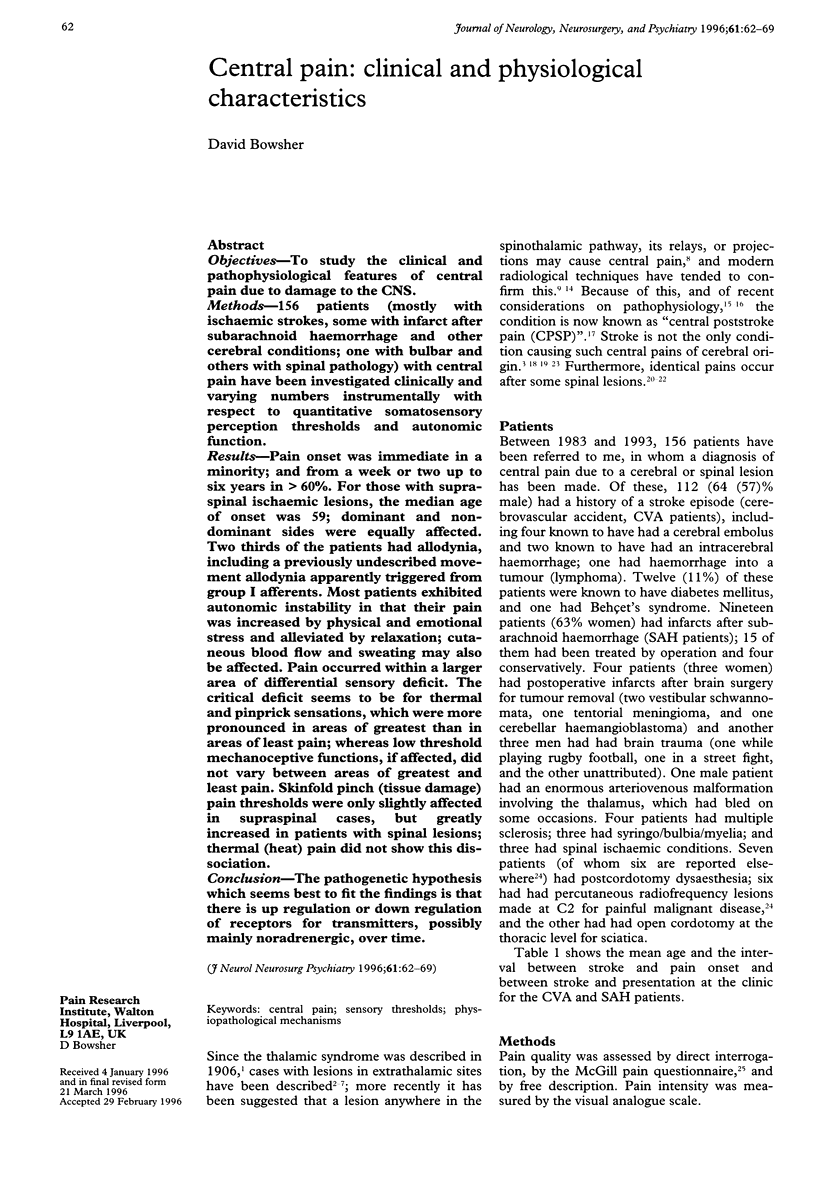

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersen G., Vestergaard K., Ingeman-Nielsen M., Jensen T. S. Incidence of central post-stroke pain. Pain. 1995 May;61(2):187–193. doi: 10.1016/0304-3959(94)00144-4. [DOI] [PubMed] [Google Scholar]
- Berić A., Dimitrijević M. R., Lindblom U. Central dysesthesia syndrome in spinal cord injury patients. Pain. 1988 Aug;34(2):109–116. doi: 10.1016/0304-3959(88)90155-8. [DOI] [PubMed] [Google Scholar]
- Boivie J., Leijon G., Johansson I. Central post-stroke pain--a study of the mechanisms through analyses of the sensory abnormalities. Pain. 1989 May;37(2):173–185. doi: 10.1016/0304-3959(89)90128-0. [DOI] [PubMed] [Google Scholar]
- Bowsher D. R., Foy P. M., Shaw M. D. Central pain complicating infarction following subarachnoid haemorrhage. Br J Neurosurg. 1989;3(4):435–441. doi: 10.3109/02688698909002829. [DOI] [PubMed] [Google Scholar]
- Bowsher D. Acute herpes zoster and postherpetic neuralgia: effects of acyclovir and outcome of treatment with amitriptyline. Br J Gen Pract. 1992 Jun;42(359):244–246. [PMC free article] [PubMed] [Google Scholar]
- Bowsher D. Neurogenic pain syndromes and their management. Br Med Bull. 1991 Jul;47(3):644–666. doi: 10.1093/oxfordjournals.bmb.a072498. [DOI] [PubMed] [Google Scholar]
- Bowsher D. Sensory consequences of stroke. Lancet. 1993 Jan 16;341(8838):156–156. doi: 10.1016/0140-6736(93)90015-9. [DOI] [PubMed] [Google Scholar]
- Bowsher D. The management of central post-stroke pain. Postgrad Med J. 1995 Oct;71(840):598–604. doi: 10.1136/pgmj.71.840.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A. W., MacFarlane I. A., Bowsher D., Campbell J. A. Weighted needle pinprick sensory thresholds: a simple test of sensory function in diabetic peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1992 Jan;55(1):56–59. doi: 10.1136/jnnp.55.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig A. D., Bushnell M. C. The thermal grill illusion: unmasking the burn of cold pain. Science. 1994 Jul 8;265(5169):252–255. doi: 10.1126/science.8023144. [DOI] [PubMed] [Google Scholar]
- De Salles A. A., Bittar G. T., Jr Thalamic pain syndrome: anatomic and metabolic correlation. Surg Neurol. 1994 Feb;41(2):147–151. doi: 10.1016/0090-3019(94)90113-9. [DOI] [PubMed] [Google Scholar]
- Eide P. K., Jørum E., Stenehjem A. E. Somatosensory findings in patients with spinal cord injury and central dysaesthesia pain. J Neurol Neurosurg Psychiatry. 1996 Apr;60(4):411–415. doi: 10.1136/jnnp.60.4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruhstorfer H., Lindblom U., Schmidt W. C. Method for quantitative estimation of thermal thresholds in patients. J Neurol Neurosurg Psychiatry. 1976 Nov;39(11):1071–1075. doi: 10.1136/jnnp.39.11.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GARCIN R., LAPRESLE J. [2d personal observation of a sensory syndrome of the thalamic type with cheiro-oral topography caused by localized lesion of the thalamus]. Rev Neurol (Paris) 1960 Nov;103:474–481. [PubMed] [Google Scholar]
- Gonzales G. R., Herskovitz S., Rosenblum M., Foley K. M., Kanner R., Brown A., Portenoy R. K. Central pain from cerebral abscess: thalamic syndrome in AIDS patients with toxoplasmosis. Neurology. 1992 May;42(5):1107–1109. doi: 10.1212/wnl.42.5.1107. [DOI] [PubMed] [Google Scholar]
- Ho K. L. Uncommon causes of the lateral medullary syndrome. Report of a case of metastatic carcinoma. Arch Neurol. 1980 Oct;37(10):669–670. doi: 10.1001/archneur.1980.00500590093018. [DOI] [PubMed] [Google Scholar]
- Hommel M., Besson G., Pollak P., Borgel F., Le Bas J. F., Perret J. Pure sensory stroke due to a pontine lacune. Stroke. 1989 Mar;20(3):406–408. doi: 10.1161/01.str.20.3.406. [DOI] [PubMed] [Google Scholar]
- Kameyama M. Vascular lesions of the thalamus on the dominant and nondominant side. Appl Neurophysiol. 1976;39(3-4):171–177. doi: 10.1159/000102492. [DOI] [PubMed] [Google Scholar]
- Korpelainen J. T., Sotaniemi K. A., Myllylä V. V. Asymmetric sweating in stroke: a prospective quantitative study of patients with hemispheral brain infarction. Neurology. 1993 Jun;43(6):1211–1214. doi: 10.1212/wnl.43.6.1211. [DOI] [PubMed] [Google Scholar]
- Lahuerta J., Bowsher D., Lipton S., Buxton P. H. Percutaneous cervical cordotomy: a review of 181 operations on 146 patients with a study on the location of "pain fibers" in the C-2 spinal cord segment of 29 cases. J Neurosurg. 1994 Jun;80(6):975–985. doi: 10.3171/jns.1994.80.6.0975. [DOI] [PubMed] [Google Scholar]
- Leijon G., Boivie J., Johansson I. Central post-stroke pain--neurological symptoms and pain characteristics. Pain. 1989 Jan;36(1):13–25. doi: 10.1016/0304-3959(89)90107-3. [DOI] [PubMed] [Google Scholar]
- Lenz F. A., Dostrovsky J. O., Tasker R. R., Yamashiro K., Kwan H. C., Murphy J. T. Single-unit analysis of the human ventral thalamic nuclear group: somatosensory responses. J Neurophysiol. 1988 Feb;59(2):299–316. doi: 10.1152/jn.1988.59.2.299. [DOI] [PubMed] [Google Scholar]
- Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975 Sep;1(3):277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- Michel D., Laurent B., Convers P., Garcia-Larrea L., Le Bas J. F., Mauguiere F., Schott B. Douleurs corticales. Etude clinique, électrophysiologique et topographique de 12 cas. Rev Neurol (Paris) 1990;146(6-7):405–414. [PubMed] [Google Scholar]
- Nurmikko T., Bowsher D. Somatosensory findings in postherpetic neuralgia. J Neurol Neurosurg Psychiatry. 1990 Feb;53(2):135–141. doi: 10.1136/jnnp.53.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurmikko T., Wells C., Bowsher D. Pain and allodynia in postherpetic neuralgia: role of somatic and sympathetic nervous systems. Acta Neurol Scand. 1991 Aug;84(2):146–152. doi: 10.1111/j.1600-0404.1991.tb04923.x. [DOI] [PubMed] [Google Scholar]
- Pelser H., van Gijn J. Spinal infarction. A follow-up study. Stroke. 1993 Jun;24(6):896–898. doi: 10.1161/01.str.24.6.896. [DOI] [PubMed] [Google Scholar]
- Rétif J., Brihaye J., Vanderhaegen J. J. Syndrome douloureux "thalamique" et lésion pariétale. A propos de trois observations de tumeur à localisation pariétale, s'étant accompagnées de douleurs spontanées de l'hémicorps controlatéral. Neurochirurgie. 1967 May-Jun;13(3):375–384. [PubMed] [Google Scholar]
- Schmahmann J. D., Leifer D. Parietal pseudothalamic pain syndrome. Clinical features and anatomic correlates. Arch Neurol. 1992 Oct;49(10):1032–1037. doi: 10.1001/archneur.1992.00530340048017. [DOI] [PubMed] [Google Scholar]
- Stenuit A., Retif J. Syndrome thalamique de Dejerine-Roussy: présentation d'une observation et discussion. Rev Med Brux. 1984 Jan;5(1):21–25. [PubMed] [Google Scholar]
- Stoodley M. A., Warren J. D., Oatey P. E. Thalamic syndrome caused by unruptured cerebral aneurysm. Case report. J Neurosurg. 1995 Feb;82(2):291–293. doi: 10.3171/jns.1995.82.2.0291. [DOI] [PubMed] [Google Scholar]
- Vestergaard K., Nielsen J., Andersen G., Ingeman-Nielsen M., Arendt-Nielsen L., Jensen T. S. Sensory abnormalities in consecutive, unselected patients with central post-stroke pain. Pain. 1995 May;61(2):177–186. doi: 10.1016/0304-3959(94)00140-A. [DOI] [PubMed] [Google Scholar]
- Yarnitsky D., Ochoa J. L. Release of cold-induced burning pain by block of cold-specific afferent input. Brain. 1990 Aug;113(Pt 4):893–902. doi: 10.1093/brain/113.4.893. [DOI] [PubMed] [Google Scholar]



