Tick paralysis is caused by a neurotoxin produced in the tick's salivary gland.1 It has been described to occur when a gravid female tick transmits the neurotoxin during feeding.2 Typically, ascending weakness begins within 2 to 7 days, which may lead to respiratory failure and death. Rarely, acute ataxia without paralysis is the presenting symptom.3 Herein, we describe a case of acute-onset ataxia and tremulousness from the bite of a male tick.
Case report.
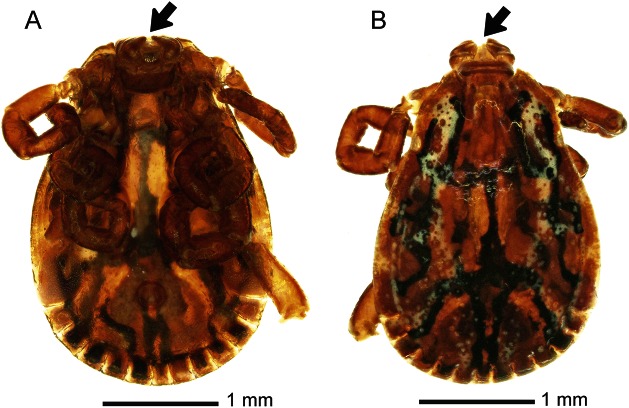
An 82-year-old male farmer presented with sudden onset of unsteadiness associated with dizziness, nausea, and vomiting upon standing up after gardening for several hours. Medical history was significant for childhood polio with residual bilateral foot drop, Type 2 diabetes, bilateral lower extremity polyneuropathy, atrial fibrillation with pacemaker implantation, dyslipidemia, and hypertension. Neurologic examination revealed a coarse bilateral hand tremor at rest that worsened with movement, and a jaw tremor. Cranial nerves were intact except for loss of smooth pursuit bilaterally, and he was initially noted to have a transient deficit in adducting the right eye, which resolved within the next 12 hours on repeated examination. He had bilateral foot drop and slight weakness in multiple muscles, none different from his baseline. There was bilateral loss of vibration sense to the knees, loss of proprioception to the ankles, and loss of pain, temperature, and light touch to the midcalf. Vibration sense was decreased in the arms to the elbow, with other sensory modalities decreased to the wrist, none different from baseline. Muscle stretch reflexes were absent in the ankles and reduced (1+) elsewhere. Plantar responses were flexor. Cerebellar testing revealed markedly ataxic finger-to-nose and heel-to-shin movements. His gait was wide-based and ataxic, and he was unable to walk or stand without assistance. Head CT with CT angiography showed no evidence of cerebellar stroke or other abnormalities. Brain MRI was precluded because of the pacemaker. Head CT, repeated 1 day later, was again unremarkable. Ataxia and tremulousness persisted without abatement. On hospital day 3, a tick was discovered attached to the right anterior thigh, with a 1-cm round, raised erythematous base. Within 24 hours of tick removal, the ataxia and tremor completely resolved. The tick was identified as an adult male American dog tick, Dermacentor variabilis, which, when examined microscopically, was missing the hypostome and chelicerae, and the tick was slightly engorged (figure, A and B). The absence of tick mouth parts and skin erythema are evidence of attachment to this patient.
Figure. American dog tick.
(A) Ventral and (B) dorsal views of the male American dog tick (Dermacentor variabilis) removed from the patient. Arrows indicate where the missing mouthparts were previously located.
Discussion.
Tick paralysis is a rare neurologic condition attributed to a gravid female tick transmitting a neurotoxin to its host during feeding.2 In children, tick paralysis presents as acute ataxia followed by ascending weakness.4 There are few published reports of adult tick paralysis. Review of the 14 published adult cases (age range 22–86 years) revealed that, in adults, the typical neurologic symptoms are muscle weakness (50%), areflexia (36%), ascending paralysis (21%), ataxia (14%), bulbar palsy (14%), and ophthalmoparesis (7%).5–7,e1–e6 Vomiting and tremulousness as symptoms have not been previously reported. The female American dog tick, D variabilis, is a common cause of tick paralysis.5 Female ticks require multiple days of feeding to become fully engorged, whereas male ticks may feed little, if at all; there have not been published reports to date indicating that males of this species can cause tick paralysis. This case presents a rare observation demonstrating that a male tick can cause neurologic disease, and in this patient, the neurologic manifestation was severe ataxia and tremor rather than the classic and well-known pattern of tick paralysis.
Supplementary Material
Footnotes
Supplemental data at Neurology.org/nn
Author contributions: Dr. Yambem, Dr. Tsao: case concept and design. Dr. Carter, Dr. Hickling, Mr. Carlson, Ms. Collins: acquisition of data. Dr. Yambem, Dr. Tsao: analysis and interpretation. Dr. Tsao, Dr. Jacewicz: critical revision of the manuscript for important intellectual content. Dr. Tsao, Dr. Jacewicz: case supervision.
Disclaimer: The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Veterans Affairs.
Study funding: No targeted funding reported.
Disclosure: C. Carter and O. Yambem report no disclosures. T. Carlson received research support from the Shelby County Health Department. G.J. Hickling received speaker honoraria from the University of Georgia Athens, received research support from NSF. K. Collins reports no disclosures. M. Jacewicz is on the editorial board for Merck Manual of Medical Therapeutics. J. Tsao is on the editorial board for Neurology®: Clinical Practice, receives publishing royalties from Springer, received research support from Wounded, Ill & Injury Directorate, US Navy Bureau of Medicine and Surgery, University of Tennessee Health Science Center. Go to Neurology.org/nn for full disclosure forms. The Article Processing Charge was paid by Department of Neurology, University of Tennessee Health Science Center.
References
- 1.Hall-Mendelin NS, Craig SB, Hall RA, et al. Tick paralysis in Australia caused by Ixodes holocyclus. Ann Trop Med Parasitol 2011;105:95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diaz JH. Ticks, including tick paralysis. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practice of Infectious Diseases, 7th ed Philadelphia: Churchill Livingstone Elsevier; 2009:3649–3662. [Google Scholar]
- 3.Engin A, Elaldi N, Bolayir E, Dokmetas I, Bakir M. Tick paralysis with atypical presentation: isolated, reversible involvement of the upper trunk of brachial plexus. Emerg Med J 2006;23:e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felz MW, Smith CD, Swift TR. A six-year-old girl with tick paralysis. N Engl J Med 2000;342:90–94. [DOI] [PubMed] [Google Scholar]
- 5.Laufer CB, Chiota-McCollum N. A case of subacute ataxia in the summertime: tick paralysis. J Gen Intern Med 2015;30:1225–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris JB, Goonetilleke A. Animal poisons and the nervous system: what the neurologists need to know. J Neurol Neurosurg Psychiatry 2004;75:iii40–iii46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bane A. A 60-year-old Ethiopian farmer diagnosed with tick paralysis at Adera Medical Center. Ethiop Med J 2014;52:143–146. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.