Abstract
Aim:
The study aimed at evaluating the clinical efficacy of articaine over lidocaine in the surgical removal of impacted mandibular third molars.
Objective:
The objectives were to compare the onset of anesthesia, pain during injection, during the procedure and after the procedure, compare the duration of anesthesia, and need for re-anesthesia.
Materials and Methods:
A prospective study was conducted on 70 subjects planned for surgical removal of mandibular third molars. Subjects were randomly administered one of two local anesthetics. The anesthetic agent used was unknown for the patient and the observer who performed the measurements.
Results:
The differences in latency with 4% articaine (56.57 ± 9.8 s) and with 2% lignocaine (88.26 ± 12.87 s), pain during procedure for articaine 1.31 ± 0.87 and for lignocaine 2.60 ± 1.06, pain after procedure was 0.89 ± 0.58 for articaine and 1.31 ± 1.05 for lignocaine, and mean duration of anesthetic effect for articaine was 231 ± 57.15 min and 174.80 ± 37.02 min for lignocaine, which was statistically significant. For re-anesthesia, 6 out of 35 patients needed re-anesthesia at the frequency of 8.57% for articaine and 13 out of 35 patients needed re-anesthesia at a frequency of 18.57% for lignocaine.
Conclusion:
The results proved that articaine had a significant faster onset of action and longer duration of action when compared to lignocaine. Hence, the pain experienced by the patients during and after the surgical procedure was significantly less. The study was concluded that articaine is a safe alternative to lignocaine, which is potent and effective in minor surgical procedures such as removal of mandibular third molars.
Keywords: Articaine hydrochloride, impacted third molars, lignocaine hydrochloride, local anesthesia
INTRODUCTION
Local anesthetics form the mainstay of pain control techniques in dentistry. They are chemicals that block the nerve conduction in a specific, temporary, and reversible manner without affecting the patient's consciousness.[1] Despite the significant limitations of cocaine such as its low therapeutic index, the risk of addiction and potentially lethal arrhythmias, it has been the drug of choice for surgical and dental pain control until the beginning of 20th century. In 1904, Alfred Einhorn synthesized procaine that became the main local anesthetic in medicine and dentistry and in 1943 Nils Lofgren synthesized lidocaine which was the first amide anesthetic prepared for local application.[1] Lidocaine was widely used and was considered the gold standard.[2] The potency of lidocaine is presently regarded as the standard for comparison with other local anesthetics. The latent period of lidocaine action varies from 2 to 3 min with an approximate duration of its anesthetic effect for 2% solutions with epinephrine as vasoconstrictor of 85 min at pulp level and 180 min in soft tissues.[3] Lidocaine is the most widely used local anesthetic agent for pain control because of its pharmacokinetic characteristics and low toxicity compared with other anesthetics and hence make it safe for use in dental practice.[4] In 1969, articaine hydrochloride was synthesized by Rusching et al. with the name of carticaine and was first marketed in Germany in 1976. By 1983, the drug was available practically in all of Europe and Canada, though it was not approved in the United States until March 2000.[3] Articaine was available as a 4% solution with epinephrine 1:100,000. The advantage of articaine over other local anesthetic is its potency due to its high liposolubility attributed to the thiopene ring in its molecule.[3] The long duration of action and its superior diffusion through bony tissue makes it comparable to long acting local anesthetics. Since the introduction of articaine, a number of studies compared it to other local anesthetics. Malamed et al. reported articaine to be a safe local anesthetic after comparing the drug with 2% lidocaine and epinephrine 1:100,000 and can be used in both adults and children.[5] Articaine is outstanding as the local anesthetic indicated for dental procedures and control of postoperative pain.
Therefore, the aim of this study was to compare the clinical efficacy of 4% articaine with 1:100,000 epinephrine over 2% lidocaine in 1:80,000 epinephrine for the application of inferior alveolar nerve block during the surgical removal of impacted third molars.
MATERIALS AND METHODS
This study was conducted in the Department of Oral and Maxillofacial Surgery, from 2010 to 2011. The Institutional Scientific Review Board and the Ethics Committee approved the protocol of this study. The present in vivo study was conducted to evaluate pain, onset, and duration of 4% articaine with 1:100,000 epinephrine (Septanest; Septodont; France) and 2% lignocaine with 1:80,000 epinephrine (Lignospan Special; Septodont; France) in the surgical removal of mandibular third molars, and the frequency of re-anesthesia, if any required. Seventy patients in the age group of 18–45 years were selected for the study. The patients were randomly administered one of the two local anesthetics. The anesthetic used was unknown for the patient and the observer who performed the measurements.
Inclusion criteria
Subjects between 18 and 45 years of age
Prophylactic removal of third molars
Acute pericoronitis in relation to lower third molar region
Dental decay in relation to third molars.
Exclusion criteria
Any known or suspected allergies or sensitivities to any of the local anesthetics solutions included in the study or any ingredients in anesthetic solutions
Pregnancy and lactation
Single isolated impacted tooth
Patient having systemic disorder like diabetes, hypertension, cardiac, or neurological disorder
Reduced mouth opening (mouth opening above 30 mm was considered normal).
The patient received a regional anesthetic blockade of buccal, lingual, and inferior alveolar nerve with 1.7 ml of anesthetic solution. Additional volume of the solution would be infiltrated if the patient complained of pain during the surgery. The removal of lower third molars followed a standard surgical technique. Postoperatively antibiotic capsule amoxicillin 500 mg (TID), tablet metronidazole 400 mg (TID), and for postoperative pain tablet ibuprofen 400 mg (BID) for 5 days were prescribed. Patients were instructed to continue the medication.
Parameters evaluated were as follows:
The onset of anesthetic agent duration was determined both subjectively and objectively by loss of sensitivity of inferior lip, the corresponding half of the tongue, and the buccal mucosa
The quality of anesthesia provided by the local anesthetic agent during surgery was evaluated by the visual analog scale (VAS) with 0 anchored by no pain and 10 anchored by worst pain imaginable
Duration of surgery after anesthetic administration, which was determined by the period between the first incision and last suture
The duration of postoperative anesthesia on soft tissues, represented by the lack of sensibility of the mucosa, tongue, and inferior lip. The patients recorded the moment that all soft tissue sensation returned to normal.
RESULTS
All data were analyzed by using the Statistical Program of Social Science (SPSS Inc., Chicago, IL, USA). Independent t-test and Chi-square test using the SPSS version 12.0.
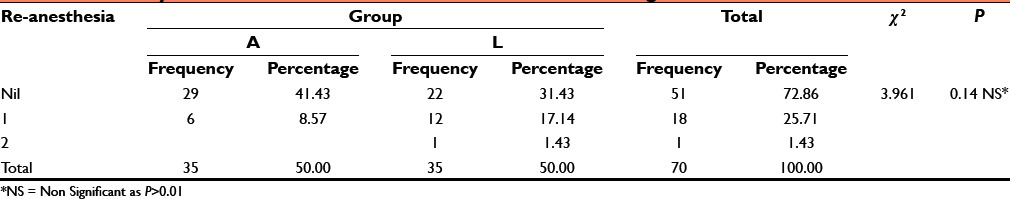
The mean anesthetic latency in the onset of anesthesia for articaine was 56.57 ± 9.82 s versus 88.26 ± 12.87 s for lignocaine with the difference being statistically significant [Table 1]. The mean duration of surgery was 33.93 ± 18.41 min for articaine and 31.03 ± 12.53 for lignocaine with no significant differences between the two groups [Table 1]. Subjective pain (during administration of anesthesia, pain during procedure, and pain after procedure) was evaluated with VAS scoring. VAS score for recording pain during administration of anesthesia for articaine was 0.97 ± 0.92, whereas for lignocaine it was 1.26 ± 1.74, with P = 0.393 (P > 0.01), which was nonsignificant [Table 1]. VAS score for pain during procedure using articaine was 1.31 ± 0.87 and 2.60 ± 1.06 for lignocaine with P < 0.01, which was highly significant [Table 1]. VAS score for pain after procedure was 0.89 ± 0.58 for articaine and 1.31 ± 1.05 for lignocaine with P = 0.039, which was significant [Table 1]. The mean duration of anesthetic effect for articaine was 231 ± 57.15 min and 174.80 ± 37.02 min for lignocaine with P < 0.01, which was highly significant [Table 1]. 6 out of 35 patients needed re-anesthesia at the frequency of 8.57% for articaine and 13 out of 35 patients needed re-anesthesia at frequency of 18.57% for lignocaine [Table 2].
Table 1.
Summary of values for comparison of clinical efficacy between articaine and lignocaine
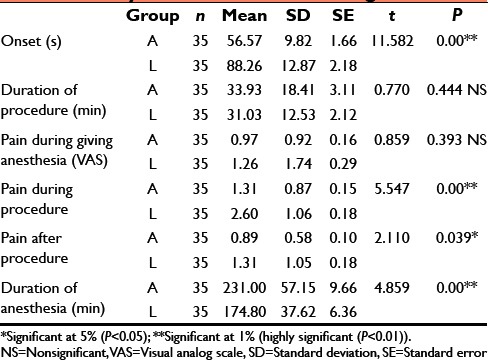
Table 2.
Summary of values for re-anesthesia between articaine and lignocaine
DISCUSSION
Management of pain during oral surgical procedures has always been a challenge and area of continued interest. Number of local anesthetic agents have been assessed for their efficacy in pain control and hence supremacy over the existing local anesthetics. Articaine is emerging local anesthetic which due to its comparable safety and potency has been studied extensively and being compared with lignocaine. The administration of local anesthetics into skin or oral mucous membrane is frequently uncomfortable. Many factors are attributed to this discomfort, including the speed of injection, volume of solution, density of tissue, and lot of psychology. The acidic pH of the anesthetic solutions plays a significant role in provoking discomfort during local anesthetic administration. The pH of plain local anesthetic solution is approximately 5.5; vasoconstrictor containing solution is about 4.5. The addition of substances such as sodium bicarbonate or carbon dioxide to the anesthetic that alkalinize the solution should make the drug administration more comfortable. Moreover, at a higher pH anesthetic has a rapid onset of action and great potency. The difference in chemical structure of articaine from that of other local anesthetics is due to the substitution of the aromatic ring with a thiophenic ring, and the presence of an additional ester ring, which gives articaine increased liposolubility and intrinsic potency, as well as greater plasma protein binding versus other commonly used local anesthetic. These differential characteristics are in turn clinically reflected by a shorter latency and increased duration of anesthesia, as well as superior bony tissue diffusion. The latency of an anesthetic depends on a number of factors, such as the intrinsic properties of the drug substance used, and the anesthetic technique employed. It is a known fact that latency is directly influenced by the corresponding pKa value; smaller pKa values being associated to shorter latency. Accordingly, 4% articaine (pKa = 7.8) would at least in theory present a shorter latency than 2% lidocaine (pKa = 7.9). In 1993, Vähätalo et al.[6] conducted a double blind study to compare the anesthetic properties of articaine hydrochloride with 1:200,000 epinephrine and lidocaine with 1:80,000 epinephrine for maxillary infiltration anesthesia. The latency time was 187 s (±66) for articaine and 201 s (±88) for lignocaine, and there were no statistically significant difference in onset and duration of anesthesia between articaine with epinephrine 1:200,000 and lignocaine with epinephrine 1:80,000. Miyoshi et al.[7] compared the potency of four local anesthetics on dental pulp with 4% articaine and concluded that articaine showed quicker onset than lidocaine. In 2000, Malamed et al.[5] compared the safety and efficacy of 4% articaine with epinephrine 1:100,000 with 2% lidocaine with epinephrine 1:100,000 and found that 4% articaine with epinephrine 1:100,000 was well tolerated and also provided clinically effective pain relief during most dental procedures and had a time of onset and duration of anesthesia appropriate for clinical use and comparable to those observed for other commercially available local anesthetics. Costa et al.[8] carried out a study to compare the onset and duration of pulpal anesthesia by maxillary infiltration using 2% lidocaine with 1:100,000 epinephrine, 4% articaine with 1:200,000 epinephrine, and 4% articaine with 1:100,000 epinephrine using an electric pulp tester and reported that both articaine solutions produced shorter onset and longer duration of pulpal anesthesia by maxillary infiltration when compared to lidocaine. Sierra-Rebolledo et al.[3] carried out a comparative study on the anesthetic efficacy of 4% articaine versus 2% lidocaine, both with epinephrine 1:100,000, in truncal block of the inferior alveolar nerve during the surgical extraction of impacted lower third molars and found out that 4% articaine offers better clinical performance than 2% lidocaine, particularly in terms of latency and duration of the anesthetic effect but statistically no significant differences in anesthetic efficacy were recorded between the two solutions. Kalia et al.[9] did a study to compare the onset and duration of anesthesia of 4% articaine with epinephrine (1:100,000) versus 2% lidocaine with epinephrine during exodontias and concluded that there were some significant differences between 4% articaine and 2% lidocaine in terms of subjective and objective symptoms and onset of pulpal anesthesia. The result showed that 4% articaine had longer duration and onset of anesthesia as compared to 2% lidocaine. Sreekumar and Bhargava[10] conducted a study to compare the onset and duration of action of soft tissue and pulpal anesthesia with three different volumes 0.6 ml, 0.9 ml, and 1.2 ml of 4% articaine with 1:100,000 epinephrine in maxillary anesthesia and concluded that maxillary infiltration anesthesia with articaine and epinephrine has a faster onset, a greater success rate, and a longer duration with volume of 1.2 ml. Bhagat et al.[11] did a study to compare the anesthetic efficacy of both 4% articaine and 2% lignocaine with epinephrine in the truncal block of the inferior alveolar nerve during surgical removal of the impacted mandibular third molars and concluded that 4% articaine has better anesthetic efficacy as compared to 2% lignocaine. Our results coincide with this study, since the latency was shorter for articaine when compared to lidocaine. The recorded latencies for both anesthetic substances were shorter than reported by other authors. The possible reason can be measured latency from the moment of needle withdrawal from the patient soft tissues, technique of nerve block and other local factors. In our study, the latency of articaine was 56.57 s versus 88.26 s in the case of lidocaine. The difference between the two anesthetic solutions was significant as P < 0.01. The duration of the effect of an anesthetic is proportional to its degree of protein binding. However, the duration of the effect of the local anesthetic is also dependent on the injection site or concentration of vasoconstrictor present in the anesthetic solution, among other factors. Articaine has one of the greatest protein binding percentages of all amide local anesthetics, comparable only to ultra-long action substances such as bupivacaine, ropivacaine, and ethidocaine. Oliveira et al.[12] conducted a study to evaluate the onset of action of pulpal and soft tissue anesthesia, and pain experience after buccal and palatal infiltrative injections with 4% articaine with 1:100,000 adrenaline, and 2% lignocaine with 1:100,000 adrenaline and found that there were no significant differences between articaine and lignocaine in relation to palatal pain sensitivity although articaine had increased duration of pulpal anesthesia over lignocaine. Batista da Silva et al.[13] conducted a prospective study to compare the anesthetic efficacy of 4% articaine and 2% lidocaine both with 1:100,000 epinephrine concentration administered as inferior mandibular nerve block and revealed that the duration of anesthesia for lignocaine was 135.5–184.5 min and 145.75–198.75 min for articaine. Articaine promoted higher anesthesia success and longer duration of anesthesia than lidocaine for most of the teeth. Shruthi et al.[14] conducted a study to compare the efficacy of articaine with that of lidocaine and found out that articaine has similar efficacy as that of lignocaine with slightly longer duration and can be used as an alternative to lignocaine in the third molar surgery.
In our study, the duration of articaine anesthetic effect varied from 155 to 330 min (1.2–5.5 h, respectively). Duration of anesthesia for lignocaine is 174.80 min (mean) and for articaine 231.0 min (mean) respectively. These values are significant as the result shows the P < 0.01. These values are comparable to the values reported in literature. In our study, a clinical evaluation of the efficacy of the two anesthetic solutions was made by comparing the need for re-anesthesia during dental surgery. In 19 cases out of 70, another dose of the anesthetic solution had to be administered via either the intrapulpal or intraligamentary technique. The number of repeat anesthetic procedures was greater when using 2% lidocaine. The difference between the frequencies of re-anesthesia in between two anesthetic solutions was not significant.
“Pain is an unpleasant emotional experience usually incited by a noxious stimulus and transmitted over a specialized neural network to the central nervous system where it is interpreted as such.” Subjective evaluation of local anesthetics used in this study done by the use of VAS, in which patient was instructed to score pain on a scale of 0–10 during injection, during procedure, and after procedure. Nusstein et al.[15] conducted a study to compare the pain on injection, heart rate increase, and postinjection pain of the intraligamentary injection of 4% articaine with 1:100,000 epinephrine and 2% lidocaine with 1:100,000 epinephrine administered with a computer-controlled local anesthetic delivery system and concluded that the intraligamentary injection of 4% articaine with 1:100,000 epinephrine was similar to 2% lidocaine with 1:100,000 epinephrine for injection pain and postinjection pain in the mandibular first molar when administered with a computer-controlled local anesthetic delivery system. Kanaa et al.[2] did a comparative study of the efficacy of buccal infiltration with 4% articaine and 2% lidocaine (both with 1:100,000 epinephrine) in securing mandibular first molar pulpal anesthesia and concluded that mandibular buccal infiltration is more effective with 4% articaine with epinephrine when compared to 2% lidocaine with epinephrine, but both injections were associated with mild discomfort. García-Gómez et al.[16] conducted a comparative study to calculate the possible effect of two anesthetics articaine with epinephrine in 1:100,000 and lignocaine with epinephrine in 1:100,000 on the postoperative pain after surgical removal of lower third molars and concluded that the articaine with epinephrine in 1:100,000 concentration is useful for the surgical removal of lower third molar where more surgical complexity and long duration of procedure was expected. Moore et al.[17] compared the efficacy of 4% articaine HCl with 1:100,000 epinephrine to 4% articaine HCl 1:200,000 epinephrine in providing effective local anesthesia and hemostasis for periodontal surgery, and reported that in patients undergoing periodontal surgery 4% articaine anesthetic formulations containing epinephrine (1:100,000 or 1:200,000) provided excellent surgical pain control. Overman[18] did a literature review on characteristics of articaine such as safety and effectiveness for incorporating it into dental hygiene practice and concluded that articaine was superior to the existing anesthetics and it provided an alternative option for pain control in dental hygiene practice. Sumer et al.[19] did a study to investigate the pain on injection of articaine with adrenaline, prilocaine with phenylpressin, and lidocaine with adrenaline and concluded that there were mild or no injection pain for all the anesthetic administrations. Tortamano et al.[20] compared the anesthetic efficacy of 4% articaine with 1:100000 epinephrine and 2% lidocaine with 1:100,000 epinephrine during pulpectomy in patients with irreversible pulpitis in mandibular posterior teeth with conventional inferior alveolar nerve block and concluded that articaine had a higher success rate than lidocaine regarding the pain absence during pulpectomy. Kanaa et al.[21] carried out a study to compare mandibular tooth pulpal anesthesia and reported discomfort following lidocaine inferior alveolar nerve block with and without supplemental articaine buccal infiltration and concluded that articaine buccal infiltration was more successful than inferior alveolar nerve block alone and more comfortable also. Trullenque-Eriksson and Guisado-Moya[1] compared bupivacaine 0.5% and articaine 4% with an epinephrine concentration of 1:200,000 in extraction of bilaterally symmetrical mandibular third molars and reported that articaine seems to be a more appropriate anesthetic for the extraction of mandibular third molars due to the shorter duration of anesthetic effect in soft tissues, lower pain during the immediate postoperative period, and personal preference. In our study, we used VAS using the marking 0–10 where 0 score showing the no pain and 10 showing the maximum pain, which cannot be bearable. In our study of subjective pain on the VAS score, 4% articaine rated significantly better than 2% lignocaine showing less pain during the procedure and after the procedure, but there was no significant difference in pain during administration of anesthesia. Pain during procedure revealed significant results as P < 0.01, as well as pain after procedure also having significant P = 0.039 value with 4% articaine with 1:100,000 epinephrine.
CONCLUSION
In our comparative study, results showed that 4% articaine had a significant faster onset and longer duration of action when compared to 2% lignocaine. Hence, the pain experienced by the patients during and after the surgical procedure was significantly less. From our study, we concluded that 4% articaine is a safe alternative to 2% lignocaine, which is potent and effective in minor surgical procedures such as removal of mandibular third molars.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Trullenque-Eriksson A, Guisado-Moya B. Comparative study of two local anesthetics in the surgical extraction of mandibular third molars: bupivacaine and articaine. Med Oral Patol Oral Cir Bucal. 2011;16:e390–6. doi: 10.4317/medoral.16.e390. [DOI] [PubMed] [Google Scholar]
- 2.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine and lidocaine mandibular buccal infiltration anesthesia: a prospective randomized double-blind cross-over study. J Endod. 2006;32:296–8. doi: 10.1016/j.joen.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 3.Sierra-Rebolledo A, Delgado-Molina E, Berini-Aytés L, Gay-Escoda C. Comparative study of the anesthetic efficacy of 4% articaine versus 2% lidocaine in inferior alveolar nerve block during surgical extraction of impacted lower third molars. Med Oral Patol Oral Cir Bucal. 2007;12:E139–44. [PubMed] [Google Scholar]
- 4.Malamed SF. Handbook of Local Anesthesia. 5th ed. St. Louis: Mosby; 2004. [Google Scholar]
- 5.Malamed SF, Gagnon S, Leblanc D. Efficacy of articaine: a new amide local anesthetic. J Am Dent Assoc. 2000;131:635–42. doi: 10.14219/jada.archive.2000.0237. [DOI] [PubMed] [Google Scholar]
- 6.Vähätalo K, Antila H, Lehtinen R. Articaine and lidocaine for maxillary infiltration anesthesia. Anesth Prog. 1993;40:114–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Miyoshi T, Aida H, Kaneko Y. Comparative study on anesthetic potency of dental local anesthetics assessed by the jaw-opening reflex in rabbits. Anesth Prog. 2000;47:35–41. [PMC free article] [PubMed] [Google Scholar]
- 8.Costa CG, Tortamano IP, Rocha RG, Francischone CE, Tortamano N. Onset and duration periods of articaine and lidocaine on maxillary infiltration. Quintessence Int. 2005;36:197–201. [PubMed] [Google Scholar]
- 9.Kalia V, Supreet, Kaur R. Comparative evaluation of onset and duration of anesthesia of 4% articaine versus 2% lidocaine with epinephrine 1:1,00,000 during exodontia. Indian J Compr Dent Care. 2011;1:19–24. [Google Scholar]
- 10.Sreekumar K, Bhargava D. Comparison of onset and duration of action of soft tissue and pulpal anesthesia with three volumes of 4% articaine with 1:100,000 epinephrine in maxillary infiltration anesthesia. Oral Maxillofac Surg. 2011;15:195–9. doi: 10.1007/s10006-011-0275-8. [DOI] [PubMed] [Google Scholar]
- 11.Bhagat MJ, Narayan V, Muthusekhar MR, Jain AR. Comparative study of the anesthetic efficacy of 4% articaine versus 2% Lignocaine in the inferior alveolar nerve block during the surgical extraction of impacted mandibular third molars. Univ Res J Dent. 2014;4:108–14. [Google Scholar]
- 12.Oliveira PC, Volpato MC, Ramacciato JC, Ranali J. Articaine and lignocaine efficiency in infiltration anaesthesia: a pilot study. Br Dent J. 2004;197:45–6. doi: 10.1038/sj.bdj.4811422. [DOI] [PubMed] [Google Scholar]
- 13.Batista da Silva C, Berto LA, Volpato MC, Ramacciato JC, Motta RH, Ranali J, et al. Anesthetic efficacy of articaine and lidocaine for incisive/mental nerve block. J Endod. 2010;36:438–41. doi: 10.1016/j.joen.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 14.Shruthi R, Kedarnath N, Mamatha N, Rajaram P, Bhadrashetty D. Articaine for surgical removal of impacted third molar; a comparison with lignocaine. J Int Oral Health. 2013;5:48–53. [PMC free article] [PubMed] [Google Scholar]
- 15.Nusstein J, Berlin J, Reader A, Beck M, Weaver JM. Comparison of injection pain, heart rate increase, and postinjection pain of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system. Anesth Prog. 2004;51:126–33. [PMC free article] [PubMed] [Google Scholar]
- 16.García-Gómez FA, Martín JF. Effects of local anaesthetics in postsurgical pain in third molar surgery. Dentum. 2006;6:67–9. [Google Scholar]
- 17.Moore PA, Doll B, Delie RA, Hersh EV, Korostoff J, Johnson S, et al. Hemostatic and anesthetic efficacy of 4% articaine HCl with 1:200,000 epinephrine and 4% articaine HCl with 1:100,000 epinephrine when administered intraorally for periodontal surgery. J Periodontol. 2007;78:247–53. doi: 10.1902/jop.2007.060314. [DOI] [PubMed] [Google Scholar]
- 18.Overman PR. Articaine: a new alternative in dental hygiene pain control. J Dent Hyg. 2007;81:66. [PubMed] [Google Scholar]
- 19.Sumer M, Misir F, Celebi N, Muglali M. A comparison of injection pain with articaine with adrenaline, prilocaine with phenylpressin and lidocaine with adrenaline. Med Oral Patol Oral Cir Bucal. 2008;13:E427–30. [PubMed] [Google Scholar]
- 20.Tortamano IP, Siviero M, Costa CG, Buscariolo IA, Armonia PL. A comparison of the anesthetic efficacy of articaine and lidocaine in patients with irreversible pulpitis. J Endod. 2009;35:165–8. doi: 10.1016/j.joen.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 21.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. Int Endod J. 2009;42:238–46. doi: 10.1111/j.1365-2591.2008.01507.x. [DOI] [PubMed] [Google Scholar]


