Abstract
Background:
Peroral endoscopic myotomy (POEM) is a novel method of treating achalasia of the esophagus. Very little data are available to guide the anesthesia providers caring for these patients. The anesthetic challenges are primarily related to the risk of pulmonary aspiration. There is also a potential risk of pneumomediastinum, pneumoperitoneum, subcutaneous, or submucosal emphysema, as a result of carbon dioxide tracking into the soft tissues surrounding the esophagus and lower esophageal sphincter.
Methods:
In this retrospective study, electronic charts of 24 patients who underwent POEM over 18 months were reviewed. Demographic data, fasting status, relevant aspiration risks, anesthetic technique, and postoperative care measures were extracted.
Results:
Fasting times for both solids and liquids were variable. None of the patients underwent preprocedural esophageal emptying. Standard induction and intubation were performed in 16, rapid sequence induction (RSI) with cricoid pressure in seven, and modified rapid sequence without application of cricoid pressure in one of the patients. One of the patients aspirated at induction, and the procedure was aborted. However, the procedure was performed successfully after a few weeks, this time a RSI with cricoid pressure was chosen.
Conclusion:
As there are no guidelines for the perioperative management of patients presenting for POEM presently, certain recommendations can be made. Preprocedural esophageal emptying should be considered in patients considered as high-risk, although cultural factors might preclude such an approach. Induction and intubation in a semi-reclining position might be useful. Although debatable, use of RSI with cricoid pressure should be strongly considered.
Keywords: Achalasia, aspiration, cricoid pressure, peroral endoscopic myotomy, pneumomediastinum, pneumoperitoneum, subcutaneous emphysema, submucosal emphysema
INTRODUCTION
Achalasia (Latin and Greek origin), literally translates into absence of relaxation. However, in reality, the absence of relaxation of the affected esophageal segment is not absolute. With the advent of high-resolution esophageal manometry, more accurate prediction of bolus movement and clinically relevant esophageal dysfunction has become possible.[1]
Anesthesia providers have delivered perioperative care to patients presenting with achalasia over many decades for a variety of procedures. These include Heller myotomy (laparoscopic, thoracoscopic, or open), endoscopic Botox injection, and balloon dilation. Peroral endoscopic myotomy (POEM) is a relatively new procedure, with endoscopists and anesthesia providers across the world on a learning curve.[2] Although the first POEM was performed in 1980, technological advances have contributed to the recent surge in its popularity.[3] As a result, more anesthesia providers are likely to encounter these patients in their daily practice. As the experience accumulates, anesthesia providers delivering care in freestanding endoscopy centers might be called to cater to the needs of these patients. Presently, two research groups have published their anesthesia experience with POEM.[4,5] At the hospital of the University of Pennsylvania, Philadelphia, 24 such procedures have been performed in the last 18 months. A dedicated team of anesthesiologists with extensive experience in gastroenterological endoscopy provided the anesthesia care. In addition to evaluating our experience with providing perioperative care to these patients, a systematic review on the subject is provided.
METHODS
After obtaining the approval from the institutional review board, electronic charts of 24 patients presenting for POEM between April 11, 2014, and July 30, 2015, were reviewed. All the procedures were performed by a single endoscopist. The demographics, type of anesthesia, medications administered, fasting status, American Society of Anesthesiology physical status, type of induction, airway management, anesthesia maintenance, anesthesia duration, procedure duration, and any unexpected events were noted.
RESULTS
A brief overview of the 24 patients is presented in Table 1. The last patient developed significant aspiration during induction and, as a result, the procedure was aborted at the first attempt. It was performed successfully few weeks later with no adverse effects. However, on the second occasion, a rapid sequence induction (RSI) technique with cricoid pressure was used. In all, standard induction and intubation was performed in 16, RSI with cricoid pressure in 7, and modified rapid sequence without application of cricoid pressure in one of the patients. As can be inferred from the table, some of the patients had a history that might have necessitated RSI and intubation. There was no consistent relation between the presumed aspiration risk and the use of RSI with cricoid pressure. In our series, none of the patients had preprocedural esophageal emptying. The duration of fasting for liquids and solids was variable as detailed in Table 1.
Table 1.
Relevant details of all the patients who underwent POEM
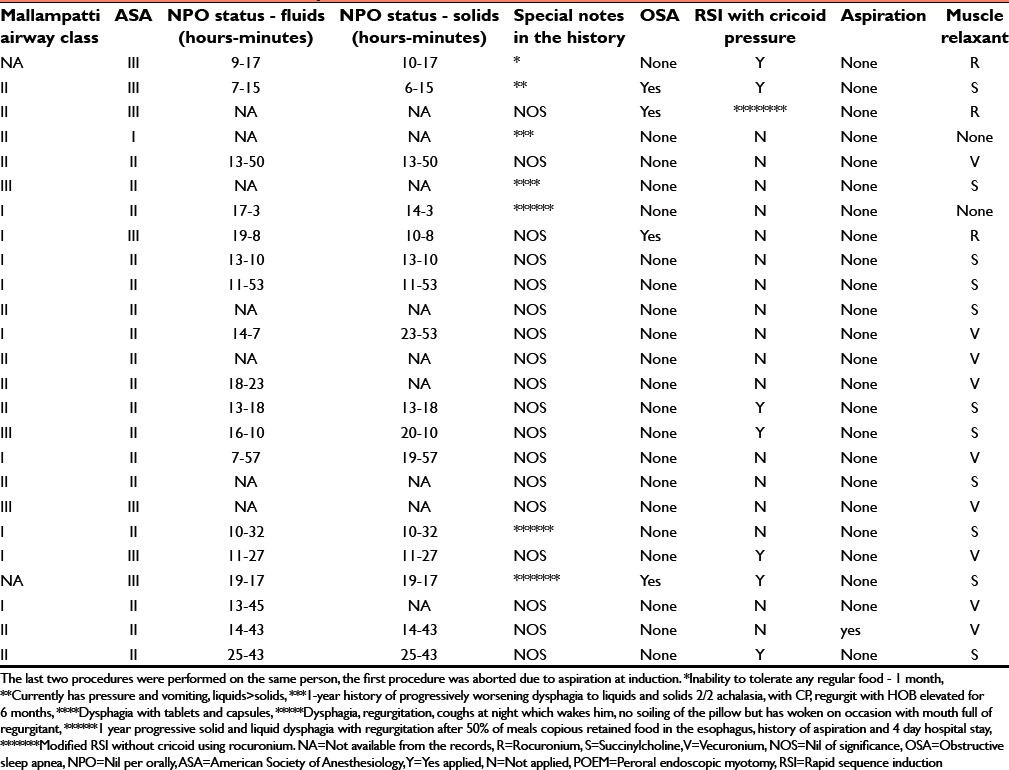
Table 2 indicates the demographics of the 24 patients who underwent the procedure. The anesthesia maintenance included total intravenous anesthesia (TIVA) in six patients, inhalational (desflurane or sevoflurane) in 16 patients, and combined (intravenous and inhalational) in 2 patients. The patient who aspirated at first procedural attempt received TIVA. Figure 1 is a bar diagram representing the mean opioid requirements. Both fentanyl and remifentanil requirements are modest indicating relative painless nature of the procedure.
Table 2.
Demographic characteristics of 24 consecutive patients who underwent peroral endoscopic myotomy
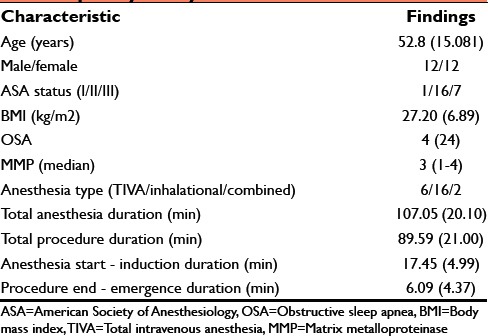
Figure 1.
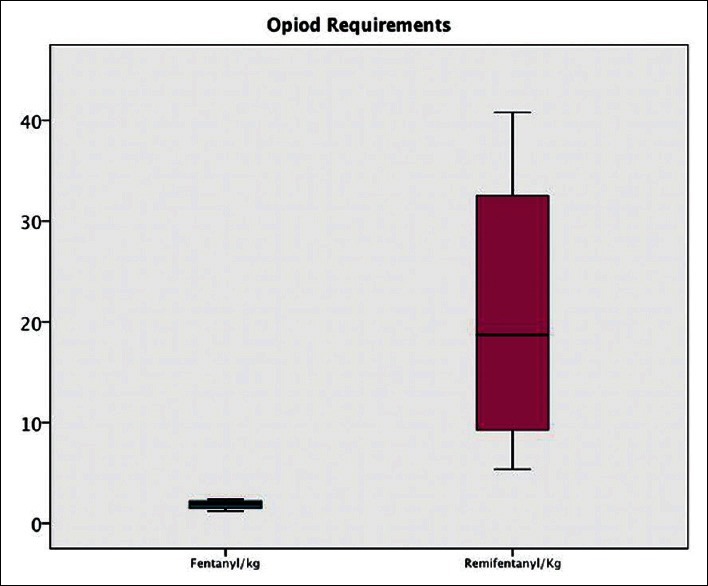
Bar diagram indicating the opioid requirements in 24 patients who underwent peroral endoscopic myotomy; remifentanil microgram/kg median values 19.46 (25–75 percentiles) (10.34–24.88) and fentanyl microgram/kg median 2.63 (1.90–4.23)
DISCUSSION
The only anesthesia-related complication in our series of 24 consecutive procedures was an aspiration in a single patient at induction. Currently, there are no guidelines regarding the airway management in patients presenting for POEM. As a matter of fact, there is almost no anesthesia literature available on the anesthetic care and practical aspects of management of POEM. Although it is crucial that aspiration needs to be avoided in all patients administered sedation or general anesthesia, it still occurs with an incidence of 3/10,000 anesthetics.[6] With very limited published data available, it is impossible to make any specific recommendations for prevention of this dreadful complication in patients presenting for POEM.
The first publication concerning the anesthetic management of POEM consisted of 28 consecutive procedures.[4] In this case series, the authors had adapted preprocedural endoscopic clearance of esophageal contents using a large channel endoscope, as a means of reducing the aspiration risk. None of their patients aspirated. Some of the anesthesia providers used cricoid pressure at induction as a matter of choice. A major endoscopy center in the USA probably did not see much merit with such a practice and allowed clear fluids for at least 48 hours before the procedure.[5] In patients considered to be at higher risk of aspiration (documented by significant food retention in the esophagus in a preprocedural esophagoduodenoscopy), a longer clear fluid regime was recommended. They used RSI with cricoid pressure for intubation. There were no documented cases of pulmonary aspiration in this prospective observational study involving 52 patients.
In our series of 24 patients, there was one patient who experienced pulmonary aspiration at induction. The procedure was aborted and safely completed a few weeks later. Considering that pulmonary aspiration can have significant morbidity and definite mortality, this issue needs to be given careful consideration. In fact, many of the patients in our series had a recent history that would have rendered a RSI and intubation more appropriate. Nevertheless, use of the RSI technique was not consistent. Recent skepticism surrounding the use of RSI with cricoid pressure might have played a part in this decision.[7,8]
Based on the experience in our practice and the two publications referenced, it might be appropriate to recommend preprocedural suctioning in selected patients who can tolerate it. Ability to tolerate an awake or sedated esophagoduodenoscopy might depend on the local culture. Induction and intubation in semi-reclined position might be another option. Considering that moderate to deep sedation for endoscopy is normally administered in this position with minimal risk of aspiration, such a practice might reduce the risk of aspiration. Cricoid pressure may be administered in the same position, if deemed appropriate. Considering that the esophageal contents are unlikely to be under pressure, any risk of esophageal damage due to cricoid pressure is remote.
Upper gastrointestinal endoscopic procedures including advanced procedures are commonly performed under deep sedation without intubation.[9,10] Most of these procedures including endoscopic retrograde pancreatography (ERCP) can be safely performed without recourse to endotracheal intubation. However, POEM is a unique procedure wherein procedural challenges are different than a standard advanced endoscopic procedure (like ERCP or endoscopic ultrasound). Other than a need to provide a still patient to the endoscopist to facilitate performance of this delicate endoscopic procedure, possibility of carbon dioxide leaking into various tissue spaces should be borne in mind. Pneumomediastinum, pneumoperitoneum, subcutaneous, and submucosal emphysema are possible. Apart from keeping a high index of suspicion, preparedness to manage such a complication is mandatory.
As reflected by the small doses of opioid used in our practice, the procedure in itself is not stimulating. As a result, adequate hypnotic effect (for example by using propofol) and analgesia with a short-acting opioid is sufficient. Postprocedure pain is usually not a factor with these procedures. Patients are generally kept overnight to monitor for any complications. As expertise is gained, such a requirement might be unnecessary on a routine basis.
Limitations
As with any retrospective study, nonavailability of complete data is a limitation. When the data are entered in the charts, the clinician is unlikely to consider the possibility of their future review for research purposes. The number of patients available for inclusion is small. As POEM is a new endoscopic interventional procedure, worldwide experience is extremely limited.
CONCLUSIONS
In spite of the stated limitations, our retrospective analysis and the review is likely to provide much-needed safety information for anesthesiologists and gastroenterologists willing to take the challenge of performing POEM. Preprocedural esophageal emptying under sedation, although difficult to implement, should be considered. RSI and intubation with the application of cricoid pressure must be adapted in patients at risk, as judged by the history and investigations. Induction and intubation in a semi-reclined position might reduce the risk of aspiration. Use of carbon dioxide (instead of air) for is mandatory to mitigate the effects of possible pneumomediastinum, pneumoperitoneum, subcutaneous, or submucosal emphysema.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Fox M, Hebbard G, Janiak P, Brasseur JG, Ghosh S, Thumshirn M, et al. High-resolution manometry predicts the success of oesophageal bolus transport and identifies clinically important abnormalities not detected by conventional manometry. Neurogastroenterol Motil. 2004;16:533–42. doi: 10.1111/j.1365-2982.2004.00539.x. [DOI] [PubMed] [Google Scholar]
- 2.Kumbhari V, Khashab MA. Peroral endoscopic myotomy. World J Gastrointest Endosc. 2015;7:496–509. doi: 10.4253/wjge.v7.i5.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8–10. doi: 10.1016/s0016-5107(80)73249-2. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka E, Murata H, Minami H, Sumikawa K. Anesthetic management of peroral endoscopic myotomy for esophageal achalasia: A retrospective case series. J Anesth. 2014;28:456–9. doi: 10.1007/s00540-013-1735-0. [DOI] [PubMed] [Google Scholar]
- 5.Yang D, Pannu D, Zhang Q, White JD, Draganov PV. Evaluation of anesthesia management, feasibility and efficacy of peroral endoscopic myotomy (POEM) for achalasia performed in the endoscopy unit. Endosc Int Open. 2015;3:E289–95. doi: 10.1055/s-0034-1391965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdulla S. Pulmonary aspiration in perioperative medicine. Acta Anaesthesiol Belg. 2013;64:1–13. [PubMed] [Google Scholar]
- 7.Bhatia N, Bhagat H, Sen I. Cricoid pressure: Where do we stand? J Anaesthesiol Clin Pharmacol. 2014;30:3–6. doi: 10.4103/0970-9185.125683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sinha AC. Cricoid pressure: An enigma wrapped in a mystery or a hand wrapped around a throat. If I can't disprove a lie, does it become the truth? J Anaesthesiol Clin Pharmacol. 2014;30:1–2. doi: 10.4103/0970-9185.125682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goudra BG, Singh PM, Sinha AC. Outpatient endoscopic retrograde cholangiopancreatography: Safety and efficacy of anesthetic management with a natural airway in 653 consecutive procedures. Saudi J Anaesth. 2013;7:259–65. doi: 10.4103/1658-354X.115334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goudra BG, Singh PM, Penugonda LC, Speck RM, Sinha AC. Significantly reduced hypoxemic events in morbidly obese patients undergoing gastrointestinal endoscopy: Predictors and practice effect. J Anaesthesiol Clin Pharmacol. 2014;30:71–7. doi: 10.4103/0970-9185.125707. [DOI] [PMC free article] [PubMed] [Google Scholar]


