Abstract
Purpose
To evaluate concordance between Breast Imaging Reporting and Data System (BI-RADS®) assessments and management recommendations for breast MRI in community practice.
Materials and Methods
Breast MRI data were collected from four regional Breast Cancer Surveillance Consortium registries from 2005–2011 for women aged 18–79 years. This study was HIPPA-compliant; each registry received approval or waiver of consent from their respective IRBs. Assessments and recommendations were compared to determine concordance according to BI-RADS guidelines. Concordance was compared by assessment category, as well as by year of examination and clinical indication.
Results
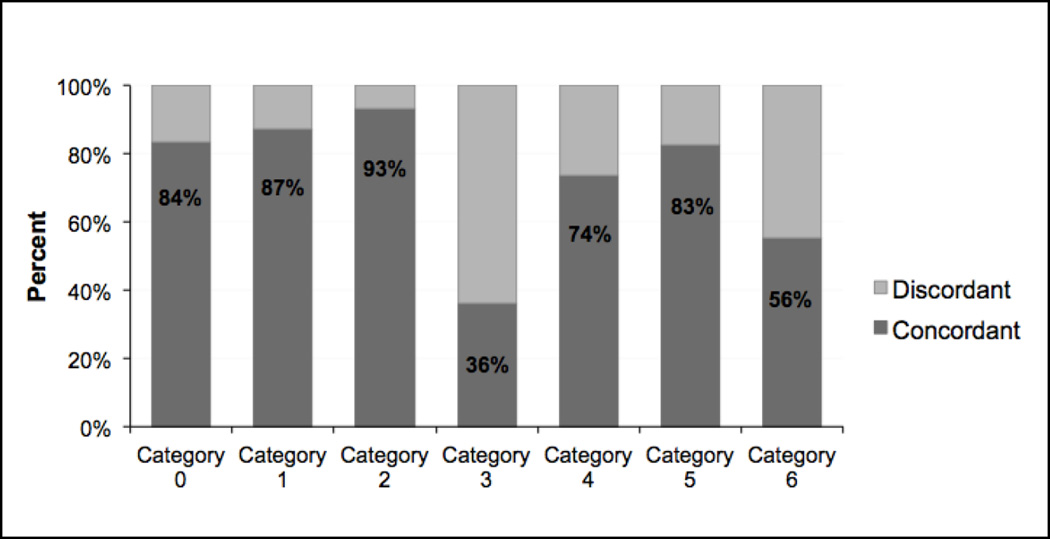
8,283 MRI examinations were included in the analysis. Concordance was highest (93%; 2475/2657) in examinations with a BI-RADS category 2 (benign) assessment. Concordance was also high in examinations with category 1 (negative) (87%; 1669/1909), 0 (incomplete) (84%; 348/417), 5 (highly suggestive of malignancy) (83%; 208/252), and 4 (suspicious) (74%; 734/993) assessments. Examinations with category 3 (probably benign) and 6 (known malignancy) assessments had the lowest concordance rates (36%; 302/837 and 56%; 676/1218, respectively). The most frequent discordant recommendation for a category 3 assessment was routine follow-up. The most frequent discordant recommendation for a category 6 assessment was biopsy. Concordance of assessments and management recommendations differed across clinical indications (p<0.0001), with the lowest concordance in examinations for disease extent.
Conclusion
Breast MRI BI-RADS management recommendations were most concordant for negative, benign, suspicious, and highly suspicious assessments. Lower concordance for assessments of probably benign and known malignancy and for examinations performed for disease extent highlight areas for interventions to improve breast MRI reporting.
Keywords: Breast cancer, Breast magnetic resonance imaging, Breast Imaging Reporting and Data System, Quality assurance
INTRODUCTION
Magnetic resonance imaging (MRI) has become a key tool for the detection and characterization of breast carcinoma. It is currently the most sensitive imaging modality for identifying breast cancer and detects malignancy that is occult to clinical examination, mammography, and ultrasound (1–3). This has led to a rapid increase in breast MRI use in the U.S. over the past decade (4–6).
In recognition of the importance of standardizing breast MRI reporting, the American College of Radiology (ACR) expanded the Breast Imaging Reporting and Data System (BI-RADS) in 2003 to include breast MRI (7). This MRI section was recently updated in 2013 (8). Similar to the well-established BI-RADS for mammography, the MRI lexicon provides a common framework for reporting imaging findings and directing next steps in patient care. A key component of this reporting system is a defined assessment system, with categories numbered 0 to 6 based on the likelihood of malignancy, and a corresponding clinical management recommendation to be used with each assessment category.
Prior multi-institution studies of mammography in community practice demonstrated inconsistencies between the use of BI-RADS assessment categories and expected clinical management recommendations (9–11). These studies evaluated mammograms performed shortly after the introduction of BI-RADS for mammography (12) and their results provided important feedback for better understanding and improving clinical practice.
Given the relatively recent introduction of the breast MRI BI-RADS lexicon, the utilization patterns of MRI BI-RADS assessment categories and whether they are used with concordant management recommendations in community practice are largely unknown. To our knowledge, no study to date addresses this clinical issue. Discordance between assessments and recommendations could have significant influence on patient care, potentially leading to unnecessary work-up or to delayed cancer diagnosis. Furthermore, the validity of performance audits and research utilizing clinical databases often relies on the appropriate use of the standardized BI-RADS reporting system. The purpose of this study was to evaluate the concordance between breast MRI BI-RADS assessments and clinical management recommendations across a diverse, national sample of imaging facilities in the United States.
METHODS
Study Population
The Breast Cancer Surveillance Consortium (BCSC) is comprised of regional registries across the United States, each consisting of multiple facilities. Data from the registries are pooled and stored centrally at the Statistical Coordinating Center in Seattle, Washington. The BCSC was developed by the National Cancer Institute’s Division of Cancer Control and Population Sciences in an effort to enhance the understanding of breast cancer surveillance practices throughout the United States (http://breastscreening.cancer.gov). This collaborative effort allows for evaluation of large samples of patients, radiologists, and imaging facilities across diverse geographic and practice settings. In a comparison with 2000 Census data, the patient population of counties served by BCSC was shown to be a broadly representative cross-section of the national population (13).
Breast MRI data for this study was available from four BCSC registries: Group Health Cooperative (Western Washington), San Francisco, Vermont, and North Carolina. Each registry received approval for active or passive consenting processes or a waiver of consent by their respective institutional review boards. All procedures were compliant with the Health Insurance Portability and Accountability Act, and all sites hold U.S. Public Health Service Certificates of Confidentiality, which provide the highest degree of identity protection for participating women and health care providers (14).
Data Analysis
We identified all MRI examinations performed from 2005 through 2011 in women 18 to 79 years of age. Examinations were excluded from the analysis if an assessment was missing or a recommendation was missing. Examinations with a recommendation of “Other” or “Follow-up MRI” with no specified follow-up time were also excluded because the BI-RADS defined recommendation category (i.e. short-interval follow-up MRI and routine follow-up MRI) could not be determined from the available recommendation data in these cases.
We quantified 1) the number of examinations assigned each BI-RADS assessment, 2) the number of examinations assigned specific management recommendations, and 3) the proportion of examinations with concordant assessment-recommendation pairings according to the MRI BI-RADS guidelines.
The seven BI-RADS assessment categories are defined as follows: 0 (Incomplete, need additional imaging evaluation); 1 (Negative); 2 (Benign); 3 (Probably benign); 4 (Suspicious), 5 (Highly suggestive of malignancy); and 6 (Known biopsy-proven malignancy). Where available, for each examination, assessments were recorded at the breast-level. Otherwise, they were recorded at the examination-level. For examinations at the breast-level with more than one assessment, a single highest order examination-level assessment was assigned according to the following hierarchy from most to least severe: BI-RADS Category 5, 4, 0, 3, 6, 2, 1.
The recommendation for each examination was recorded independently of the assessment. If there was one recommendation in an examination, this one was used. If there were multiple recommendations in an examination, the most severe recommendation was assigned. The recommendation hierarchy from most to least severe of the nine recommendation options extracted from the BCSC database was: 1) Biopsy (MRI-guided biopsy, FNA, Needle biopsy, Surgical excision); 2) Targeted ultrasound-if negative MRI-guided biopsy; 3) Additional imaging or clinical follow-up miscellaneous; 4) Targeted ultrasound- not otherwise specified; 5) Targeted ultrasound- if negative follow-up MRI; 6) Short term follow-up MRI (<12 months); 7) Take appropriate action- Category 6; 8) Routine follow-up MRI (≥12 months); 9) Routine mammographic or clinical follow-up.
Table 1 lists assessment-recommendation pairings that were defined as concordant for the analysis. Concordance rates for each BI-RADS assessment were determined for the whole cohort. In addition, concordance was determined by year of examination (2005–2008 vs. 2009–2011) and by clinical indication for examination (Screening, Diagnostic, Extent of disease, Short interval follow-up, and Other). Differences in concordance were assessed using the Pearson’s chi-squared test. All computations were performed using SAS statistical software version 9.3 (SAS Institute). A two-sided p-value <0.05 was considered statistically significant for all comparisons.
TABLE 1.
Definitions for assigning concordance between BI-RADS assessments and recommendations
| BI-RADS Assessment |
Definition of BI-RADS Category |
Concordant Recommendations a |
|---|---|---|
| Category 0 | Incomplete, Need Additional Imaging Evaluation |
Targeted ultrasound NOS Targeted ultrasound- if negative follow-up MRI b Targeted ultrasound- if negative MRI-guided biopsy b Additional Imaging or Clinical follow-up NOS |
| Category 1 | Negative | Routine mammographic or clinical follow-up Routine Follow-up MRI (≥12 months) |
| Category 2 | Benign | Routine mammographic or clinical follow-up Routine Follow-up MRI (≥12 months) |
| Category 3 | Probably Benign | Short interval follow-up MRI (<12 months) Targeted ultrasound- if negative follow-up MRI b |
| Category 4 | Suspicious Abnormality |
Biopsy (MRI-guided biopsy, FNA, CNB, Surgical excision) Targeted ultrasound- if negative MRI-guided biopsy b |
| Category 5 | Highly Suggestive of Malignancy |
Biopsy (MRI-guided biopsy, FNA, CNB, Surgical excision) Targeted ultrasound- if negative MRI-guided biopsy b |
| Category 6 | Known Biopsy- proven Malignancy |
Take appropriate action- Category 6 |
Abbreviations: NOS = Not Otherwise Specified; FNA = Fine Needle Aspiration; CNB = Core Needle Biopsy
Recommendation options within the Breast Cancer Surveillance Consortium database
Recommendation may be concordant with more than one assessment category
RESULTS
MRI Characteristics
A total of 14,412 breast MRI examinations were completed during the study period. Of these, we excluded 1,069 (7%) due to missing an assessment, 4,557 (32%) due to missing a recommendation, and 503 (4%) because the only recommendation(s) was “Other” (n=356) and/or “Follow-up MRI” with no specified follow-up time (n=142).
The final study sample included 8,283 examinations in 6,230 women from 39 individual facilities across the four regional registries. The number of facilities contributing 1–10, 11–49, and 50 or more MRI examinations was 20 (51%), 4 (10%), and 15 (39%), respectively. Table 2 summarizes the characteristics of the patients and examinations. The majority of examinations (63%; 5199/8283) were in patients between 40 and 59 years of age. The most common indication for MRI was “Screening” (33%; 2741/8283), followed by “Diagnostic” (31%; 2525/8283).
TABLE 2.
Characteristics of MRI Examinations
| Characteristic | N |
|---|---|
| Year | |
| 2005 | 724 (8.7) |
| 2006 | 1074 (13.0) |
| 2007 | 1355 (16.4) |
| 2008 | 1114 (13.4) |
| 2009 | 1109 (13.4) |
| 2010 a | 2103 (25.4) |
| 2011 a | 804 (9.7) |
| Age group | |
| 18–39 | 885 (10.7) |
| 40–49 | 2408 (29.1) |
| 50–59 | 2791 (33.7) |
| 60–69 | 1627 (19.6) |
| 70–79 | 572 (6.9) |
| Indication for exam | |
| Screening | 2741 (33.1) |
| Diagnostic b | 2525 (30.5) |
| Extent of disease | 1198 (14.5) |
| Short interval follow-up | 452 (5.5) |
| Other c | 530 (6.4) |
| Missing | 837 (10.1) |
| Total | 8283 |
Note—Data in parentheses are percentages of total (N=8283) examinations
One registry only contributes data in 2010–2011; One registry has no data in 2011.
“Diagnostic” includes Additional evaluation of recent non-MRI breast imaging, Evaluation of a breast problem, Recurrence vs scar
“Other” includes Response to neoadjuvant chemotherapy, Evaluation of breast implants, and Other.
Concordance of Assessments and Recommendations
The overall concordance between BI-RADS assessments and management recommendations across all examinations was 77%. Figure 1 shows the concordance of recommendations for each assessment category. Table 3 further demonstrates the association between each assessment category and each management recommendation.
FIGURE 1.
Concordance Rate by Assessment Category
TABLE 3.
Concordance of BI-RADS Assessments and Recommendations
| BI-RADS Assessment Category | |||||||
|---|---|---|---|---|---|---|---|
| Recommendation | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
| Routine mammo or clinical follow-up | 13 | 1633* | 2278* | 151 | 21 | 6 | 87 |
| Routine follow-up MRI | 1 | 36* | 197* | 83 | 2 | 0 | 0 |
| Take appropriate action - Cat 6 | 4 | 3 | 5 | 19 | 12 | 8 | 676* |
| Short-term follow-up MRI | 2 | 1 | 11 | 294* | 12 | 3 | 18 |
| Targeted US; if neg, follow-up MRI | 21* | 1 | 0 | 8* | 8 | 1 | 1 |
| Ultrasound, not otherwise specified | 235* | 7 | 22 | 137 | 180 | 19 | 37 |
| Additional imaging or clinical follow-up | 68* | 213 | 109 | 103 | 24 | 7 | 4 |
| Targeted US; if neg, MRI-guided biopsy | 24* | 0 | 1 | 4 | 94* | 8* | 7 |
| Biopsy | 49 | 15 | 34 | 38 | 640* | 200* | 388 |
| Total (denominator) | 417 | 1909 | 2657 | 837 | 993 | 252 | 1218 |
| Percentage concordant | 83.5% | 87.4% | 93.2% | 36.1% | 73.9% | 82.5% | 55.5% |
Abbreviations: mammo = mammography; US = ultrasound; neg.=negative
Highlighted numbers reflect the recommendations that are concordant with BI-RADS assessment.
Concordance between assessments and recommendations was highest among examinations assigned a BI-RADS assessment category of 2 (benign), with a concordant management recommendation given 93% (2475/2657) of the time. The next highest concordance was seen in examinations with BI-RADS assessment categories of 1 (negative) (87%; 1669/1909), 0 (incomplete) (84%; 348/417), 5 (highly suggestive of malignancy) (83%; 208/252), and 4 (suspicious) (74%; 734/993). Assessments and recommendations were the least concordant among examinations assigned BI-RADS assessment categories of 3 (probably benign) and 6 (known malignancy). These demonstrated overall concordances of 36% (302/837) and 56% (676/1218), respectively.
In total, 64% (535/837) of MRI examinations with a BI-RADS assessment of category 3 (probably benign) had a discordant recommendation. Of these examinations, 28% (151/535) were due to a discordant recommendation of “Routine mammography or clinical follow-up” and 26% (137/535) were due to a discordant recommendation of “Ultrasound”. Of MRI examinations with a BI-RADS assessment of category 6 (known malignancy), 44% (542/1218) had a discordant recommendation; the majority (72%; 388/542) were due to a discordant recommendation of “Biopsy”.
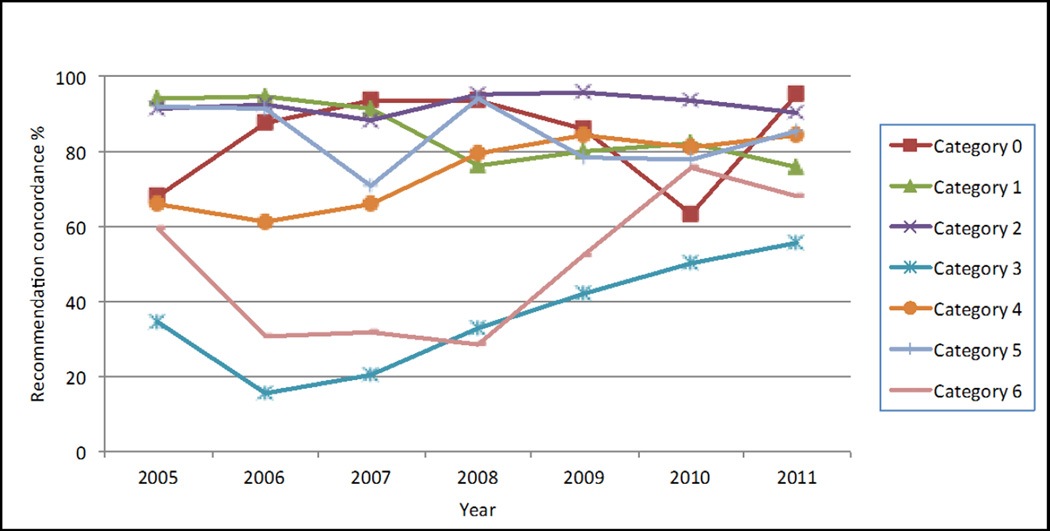
Examination Year and Indication
Figure 2 depicts the percent concordance by BI-RADS assessment category over time. BI-RADS assessment categories 3 (probably benign) and 6 (known malignancy), which had the lowest overall concordance, both demonstrated improvement in concordance over time. Concordance for category 6 assessments improved from 60% in 2005 to 68% in 2011. Concordance for category 3 assessments improved from 34% in 2005 to 56% in 2011. However, concordance for both of these assessment categories remained relatively low (<70%) compared to the concordance for other BI-RADS assessment categories.
FIGURE 2.
Recommendation concordance (%) by BI-RADS assessment and year.
The overall concordance across all examinations was higher for MRIs performed in 2009–2011 (80%) compared to those performed in 2005–2008 (75%), Table 4. This difference was statistically significant (p<0.0001), and remained significant after controlling for clinical indication. However, additional analysis indicated that this was mainly driven by one of the four registries and there was no statistically significant difference when this registry was removed (p=0.25).
TABLE 4.
Concordance of BI-RADS Assessments and Recommendations by Age group and Indication
| Percent Concordant | |
|---|---|
| Year of Examination | |
| 2005–2008 | 74.7% (3187/4267) |
| 2009–2011 | 80.3% (3225/4016) |
| p for difference* | P<0.0001 |
| Indication for exam | |
| Extent of disease | 72.5% (869/1198) |
| Diagnostic | 75.8% (1913/2525) |
| Screening | 82.2% (2253/2741) |
| Other | 82.3% (436/530) |
| Short follow-up | 89.8% (406/452) |
| p for difference* | p<0.0001 |
p-value based on Pearson chi-squared test
Differences in concordance by indication for examination were also statistically significant (p<0.0001). The lowest concordance was seen for extent of disease evaluations among newly diagnosed cancer patients (73%; 869/1198).
DISCUSSION
We evaluated concordance between BI-RADS assessments and clinical management recommendations for breast MRI examinations across multiple imaging facilities in U.S. community practice settings. We found that most breast MRI assessments were associated with concordant recommendations in keeping with BI-RADS guidelines. However, there was high discordance in the reporting of recommendations for examinations with assessments of category 3 (probably benign) and category 6 (known malignancy). Although we found improvement in concordance for these categories over time, it has remained low for these assessments.
BI-RADS assessment categories for breast MRI have been shown to be reliable predictors of the risk of malignancy (15, 16). However, appropriate care of women undergoing breast imaging relies on providing the concordant clinical management recommendation for each reported assessment. The importance of this concordant pairing of assessments and recommendations has been emphasized in more recent editions of the ACR BI-RADS manual (7, 8).
The high concordance in the reporting of recommendations for BI-RADS assessment categories of 0 (incomplete), 2 (benign), 4 (suspicious) and 5 (highly suggestive of malignancy) in this study reflects that community radiologists are performing well and using BI-RADS as intended in these scenarios. However, low concordance for BI-RADS assessment category 3 (probably benign) and category 6 (known malignancy) indicates that there is a need for further improvement and continuing education. This is particularly important given that the BI-RADS assessment category and its associated management recommendation have become the standard by which clinicians determine the disposition of their patients who undergo breast imaging. Furthermore, consistent reporting is important for accurate data collection for both auditing and research purposes.
We found the lowest concordance among MRI examinations with a BI-RADS category 3 (probably benign) assessment, with the concordant recommendation of “short-interval follow-up” given in only 36% of cases. Early studies on mammography reporting practices in the community similarly found that less than half of category 3 assessments received the expected clinical management recommendations (9–11). The category 3 assessment has often been a source of confusion and uncertainty for radiologists, and this may be particularly true for MRI, where there are limited data regarding the types of findings that should be assigned a category 3 assessment. At the time of our study, the 2003 BI-RADS atlas was in use, and stated that “data are becoming available” and that “at the present time, most approaches are intuitive” regarding MRI category 3 assessment (7). The recently introduced 2013 BI-RADS atlas acknowledges that “the use of category 3 assessment at MRI remains intuitive for radiologists” (8). Nevertheless, recent studies have shown a low malignancy rate (0.6–1.8%) for MRI-detected lesions assessed as BI-RADS category 3, supporting the concordant recommendation of short-interval follow-up for these findings (17–19).
We also found inconsistencies with BI-RADS category 6 (known malignancy) assessments, with a concordant recommendation given only 56% of the time. The most common discordant recommendation was biopsy. This may in part be due to misunderstanding by radiologists about the appropriate use of the category 6 assessment. In a patient with known malignancy, if there are any additional suspicious findings that warrant biopsy, the BI-RADS category 4 (suspicious) or 5 (highly suggestive of malignancy) assessment should supersede a category 6 despite the presence of a known malignancy. This is clinically significant because if an examination with additional suspicious or highly suspicious findings is assigned a category 6 assessment, multifocal or multicentric cancers could potentially be missed prior to surgery. The recently published 2013 edition of BI-RADS has been updated to further clarify this issue (8, 20). Specifically, it states that in patients with known breast cancer, “the single overall assessment should be based on the most immediate action needed. If a finding or findings are identified for which tissue diagnosis is recommended, then a category 4 or 5 assessment should be rendered.” Our analysis included MRI examinations performed only up to 2011, prior to the publication of the 2013 BI-RADS atlas. It will be important to observe whether these new refinements in 2013 edition lead to a better understanding and use of BI-RADS by radiologists and to improved concordance of assessments and recommendations over time.
Across all clinical indications, we found the lowest concordance in MRI examinations performed for evaluation of disease extent in women with newly diagnosed breast cancer. This is expected, given the low concordance for examinations assigned a BI-RADS category 6 (known malignancy) assessment, and the reasons for discordance for this clinical indication likely parallel those for the known malignancy assessment.
There are limitations to our study. First, nearly one-third of MRI examinations were excluded from the analysis due to missing recommendations. The primary reason for this was that the recommendation data for many examinations could not be extracted from some facilities by their respective registries, mainly due to the type of software used by these facilities to record examination assessments and recommendations. GIven the number of excluded examinations, the study population could be less representative of the community as a whole. However, we would not expect concordance at these facilities to be much different than concordance at included facilities, since exclusion was due to a somewhat random factor (software issues). In addition, since this impacted all examinations of the affected facilities, we would not expect the exclusions to introduce much bias to the data.
A second limitation of our study is that we did not have the ability to review the complete details and text of the MRI reports. Instead, we worked with assessment and recommendation data already extracted by the regional registries and pooled at the central BCSC statistically coordinating center. Although the structure of the BI-RADS reporting system should ideally limit a radiologist’s reliance on additional free text, having access to the entirety of the reports may have allowed us to gather potentially useful information about the reasons for assigning discordant recommendations and decipher possible sources of confusion. It is important to note that, while we did not have these additional details from individual radiology reports, the rigorous coding procedures during the initial data collection process are what enable the analysis of such broad and large national datasets.
In summary, we found high concordance between MRI BI-RADS assessments and management recommendations in community practice for assessment categories 0, 1, 2, 4, and 5, but lower concordance for categories 3 (probably benign) and 6 (known malignancy). Across clinical indications, the lowest concordance was seen in examinations performed for extent of disease. Although there has been some increase in concordance for breast MRI examinations over time, further improvements in BI-RADS reporting are needed. More accurate use of concordant MRI BI-RADS assessments and management recommendations will enable radiologists to communicate more effectively with referring providers and facilitate appropriate patient care, and educational efforts and training should target observed areas of inconsistency.
Advances in Knowledge
Concordance between MRI BI-RADS assessments and management recommendations was lowest for examinations with assessment categories of 3 (probably benign) and 6 (known malignancies).
Concordance was highest for examinations with assessment categories of 0 (incomplete), 1 (negative), 2 (benign), 4 (suspicious), and 5 (highly suggestive of malignancy).
The MRI examination clinical indication with the lowest concordance was evaluation of disease extent for newly diagnosed breast cancers.
Implications for Patient Care
Improved use of concordant MRI BI-RADS assessments and management recommendations will facilitate appropriate patient care and enable radiologists to communicate more effectively with referring providers.
Summary statement.
In summary, we found high concordance between MRI BI-RADS assessments and management recommendations in community practice for assessment categories 0, 1, 2, 4, and 5, but lower concordance for categories 3 (probably benign) and 6 (known malignancy).
Acknowledgments
Funding support: This work was supported by a National Cancer Institute-funded Program Project (P01CA154292) and the Breast Cancer Surveillance Consortium (HHSN261201100031C). Vermont Breast Cancer Surveillance System data collection was also supported by U54CA163303. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. We thank the participating women, mammography facilities, and radiologists for the data they have provided for this study. A list of the BCSC investigators and procedures for requesting BCSC data for research purposes are provided at http://breastscreening.cancer.gov/. AYL was supported in part by the RSNA Resident Research Grant (RR1328).
REFERENCES
- 1.Kuhl CK. Current status of breast MR imaging. Part 2. Clinical applications. Radiology. 2007;244(3):672–691. doi: 10.1148/radiol.2443051661. [DOI] [PubMed] [Google Scholar]
- 2.Sung JS, Dershaw DD. Breast magnetic resonance imaging for screening high-risk women. Magnetic resonance imaging clinics of North America. 2013;21(3):509–517. doi: 10.1016/j.mric.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 3.Brasic N, Wisner DJ, Joe BN. Breast MR imaging for extent of disease assessment in patients with newly diagnosed breast cancer. Magnetic resonance imaging clinics of North America. 2013;21(3):519–532. doi: 10.1016/j.mric.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Stout NK, Nekhlyudov L, Li L, et al. Rapid increase in breast magnetic resonance imaging use: trends from 2000 to 2011. JAMA internal medicine. 2014;174(1):114–121. doi: 10.1001/jamainternmed.2013.11958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wernli KJ, DeMartini WB, Ichikawa L, et al. Patterns of breast magnetic resonance imaging use in community practice. JAMA internal medicine. 2014;174(1):125–132. doi: 10.1001/jamainternmed.2013.11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao K, Stewart AK, Winchester DJ, Winchester DP. Trends in contralateral prophylactic mastectomy for unilateral cancer: a report from the National Cancer Data Base, 1998–2007. Annals of surgical oncology. 2010;17(10):2554–2562. doi: 10.1245/s10434-010-1091-3. [DOI] [PubMed] [Google Scholar]
- 7.American College of Radiology. ACR Breast Imaging Reporting and Data System (BI-RADS), Breast Imaging Atlas. 4th. Reston, Va: American College of Radiology; 2003. [Google Scholar]
- 8.American College of Radiology. ACR Breast Imaging Reporting and Data System (BI-RADS), Breast Imaging Atlas. 5th. Reston, Va: American College of Radiology; 2013. [Google Scholar]
- 9.Taplin SH, Ichikawa LE, Kerlikowske K, et al. Concordance of breast imaging reporting and data system assessments and management recommendations in screening mammography. Radiology. 2002;222(2):529–535. doi: 10.1148/radiol.2222010647. [DOI] [PubMed] [Google Scholar]
- 10.Geller BM, Barlow WE, Ballard-Barbash R, et al. Use of the American College of Radiology BI-RADS to report on the mammographic evaluation of women with signs and symptoms of breast disease. Radiology. 2002;222(2):536–542. doi: 10.1148/radiol.2222010620. [DOI] [PubMed] [Google Scholar]
- 11.Lehman C, Holt S, Peacock S, White E, Urban N. Use of the American College of Radiology BI-RADS guidelines by community radiologists: concordance of assessments and recommendations assigned to screening mammograms. AJR American journal of roentgenology. 2002;179(1):15–20. doi: 10.2214/ajr.179.1.1790015. [DOI] [PubMed] [Google Scholar]
- 12.American College of Radiology (ACR) Illustrated breast imaging reporting and data system (BI-RADS) Reston, Va: American College of Radiology; 1993. [Google Scholar]
- 13.National Cancer Institute. Bethesda, MD: National Cancer Institute, National Institutes of Health, U.S. Department of Health and Human Services; 2004. Apr, Breast Cancer Surveillance Consortium: Evaluating Screening Performance in Practice. NIH Publication No. 04-5490. Available at: http://breastscreening.cancer.gov/espp.pdf. [Google Scholar]
- 14.Carney PA, Geller BM, Moffett H, et al. Current medicolegal and confidentiality issues in large, multicenter research programs. American journal of epidemiology. 2000;152(4):371–378. doi: 10.1093/aje/152.4.371. [DOI] [PubMed] [Google Scholar]
- 15.Mahoney MC, Gatsonis C, Hanna L, DeMartini WB, Lehman C. Positive predictive value of BI-RADS MR imaging. Radiology. 2012;264(1):51–58. doi: 10.1148/radiol.12110619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gutierrez RL, DeMartini WB, Eby PR, Kurland BF, Peacock S, Lehman CD. BI-RADS lesion characteristics predict likelihood of malignancy in breast MRI for masses but not for nonmasslike enhancement. AJR American journal of roentgenology. 2009;193(4):994–1000. doi: 10.2214/AJR.08.1983. [DOI] [PubMed] [Google Scholar]
- 17.Eby PR, Demartini WB, Peacock S, Rosen EL, Lauro B, Lehman CD. Cancer yield of probably benign breast MR examinations. Journal of magnetic resonance imaging : JMRI. 2007;26(4):950–955. doi: 10.1002/jmri.21123. [DOI] [PubMed] [Google Scholar]
- 18.Weinstein SP, Hanna LG, Gatsonis C, Schnall MD, Rosen MA, Lehman CD. Frequency of malignancy seen in probably benign lesions at contrast-enhanced breast MR imaging: findings from ACRIN 6667. Radiology. 2010;255(3):731–737. doi: 10.1148/radiol.10081712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bahrs SD, Baur A, Hattermann V, et al. BI-RADS(R) 3 lesions at contrast-enhanced breast MRI: is an initial short-interval follow-up necessary? Acta radiologica. 2014;55(3):260–265. doi: 10.1177/0284185113501304. [DOI] [PubMed] [Google Scholar]
- 20.Edwards SD, Lipson JA, Ikeda DM, Lee JM. Updates and revisions to the BI-RADS magnetic resonance imaging lexicon. Magnetic resonance imaging clinics of North America. 2013;21(3):483–493. doi: 10.1016/j.mric.2013.02.005. [DOI] [PubMed] [Google Scholar]