Abstract
Aims
Atrial fibrillation (AF) is associated with numerous cardiovascular complications. We sought to estimate the annual burden of cardiovascular complications in AF patients in French hospitals.
Methods and results
All AF patients hospitalized in France in 2012 were identified from the national public/private hospital database. Comorbid conditions and medical histories were documented using medical records dating back 5 years. Reasons for hospitalization, type of admission (emergency or otherwise), length of stay, rehabilitation transfers, and death at discharge were identified and costs of acute and rehabilitation care determined (2012 Euros). In total, 533 044 AF patients (mean age ± SD 78.0 ± 11.4 years, 47.1% women) were hospitalized in 2012 for any reason. Hospitalizations were cardiovascular-related in 267 681 patients [22.5% cardiac dysrhythmia, 18.3% heart failure, 7.1% vascular/ischaemic diseases, 6.9% stroke/transient ischaemic attack (TIA)/systemic embolism (SE), and 1.3% haemorrhages]. Patients with stroke/TIA/SE had higher rates of emergency admission (68.1%), transfer to rehabilitation unit (28.1%), and death at discharge (13.7%) than those with other cardiovascular complications, with the exception of haemorrhages, where emergency admission rates were similar. They also had longer mean lengths of stay (12.6 ± 13.2 days for acute care and 46.8 ± 42.5 days for rehabilitation). The annual total cost (acute care and rehabilitation) for all hospitalized cardiovascular events was €1.94 billion, of which heart failure represented €805 million, vascular/ischaemic diseases €386 million, stroke €362 million, cardiac dysrhythmia €341 million, and haemorrhage €48 million.
Conclusion
Half a million patients with AF were hospitalized in France in 2012. Cardiovascular-related hospitalizations involved half of these admissions, for a global burden of almost €2 billion, equivalent to 2.6% of total expenditure in French hospitals. Among these hospitalizations stroke/TIA/SE represented costly, but potentially preventable, complications.
Keywords: Burden, Cardiovascular, Atrial fibrillation, Hospitalization, Stroke
What's new?
The hospital costs of cardiovascular complications in patients with AF are substantial in France, representing 2 billion Euros.
While stroke, TIA, and SE are not the most frequent complications in AF, they have higher resource consumption. These complications require special attention because of their preventability.
Introduction
Atrial fibrillation (AF) is the most common chronic cardiac rhythm disorder, with a prevalence of between 1 and 2% in the general population.1,2 In France, between 600 000 and 1 million people are estimated to have AF.3 Atrial fibrillation has attracted much attention due to its association with substantial mortality and morbidity. Indeed, this arrhythmia is associated with numerous cardiovascular complications including ischaemic stroke, heart failure, and myocardial infarction.4 Furthermore, the use of anticoagulant therapy for stroke prevention in AF increases the risk of bleeding.4 The attributable risk of AF for stroke is 1.5% for those aged 50–59 years and 23.5% for those aged 80–90 years.5 A recent study in patients with AF estimated the 24-month cumulative incidence of stroke to be 32.1 cases per 1000, haemorrhage to be 53.1 cases per 1000, myocardial infarction to be 20.3 cases per 1000, and chest pain to be 45.3 cases per 1000.6
Rehabilitation care contributes a high number of hospital stays after acute care for a stroke; one-third of patients (with AF or not) were admitted for rehabilitation after a stroke event.7 However, no data are available on the global burden of AF and its cardiovascular complications in France. The objectives of this study were to describe the characteristics of patients with AF hospitalized in France in 2012 and to estimate the annual burden of this arrhythmia and of cardiovascular complications in hospitalized patients with AF, at national and regional levels.
Methods
In this retrospective analysis, we used data from the Programme de médicalization des systèmes d'information (PMSI). The PMSI consists of five comprehensive databases that record diagnoses and procedures for most day-care and inpatient stays in private and public hospitals in France. Information from two of these databases was used. PMSI-MCO (Médecine chirurgie obstétrique, Medicine, Surgery, Obstetric) was used to identify patients and PMSI-SSR (Soins de suite et de réadaptation, post-acute care and functional rehabilitation) was used to identify medical and rehabilitation procedures during hospitalization and physical and cognitive dependence.
The study population comprised adults (≥18 years) with a diagnosis of AF or atrial flutter (ICD-10 code I48) coded in the principal diagnosis (i.e. the health problem that justified admission to hospital), the related diagnosis (i.e. potential chronic disease or health state during hospital stay), or the significantly associated diagnosis (i.e. comorbidity or associated complication) who were hospitalized for any reason from 1 January to 31 December 2012. Patient information (demographics, coexisting medical conditions, and medical history) was described using data collected in their hospital records since 1 January 2007. Individualized risk stratification was done retrospectively using the CHA2DS2-VASc [Cardiac failure or dysfunction, Hypertension, Age ≥75 (Doubled), Diabetes, Stroke [Doubled]-Vascular disease, Age 65–74, and Sex category (Female)] score for stroke and the HAS-BLED [Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio (INR), Elderly, Drugs/alcohol concomitantly] score for bleeding. A modified version (excluding labile international normalized ratio and ‘antithrombotic drug therapy’) is presented as not all components of the HAS-BLED score were available.
For AF complications occurring in 2012, data from acute and rehabilitation stays were collected and analysed.
Statistical analysis
Qualitative variables are described using counts and percentages and continuous quantitative variables as means and standard deviations (SDs). Comparisons were made using non-parametric tests as appropriate: the Wilcoxon W and Kruskal–Wallis tests were used for comparing values between two independent groups and the χ2 test for comparing categorical data. Costs of acute stays were determined using diagnosis-related groups and corresponding tariffs (2012 Euros). Regarding the costs of rehabilitation, stays were valuated using the Activity Value Indicator (AVI) points system for each week per patient. The AVI points obtained for each week per patient are deducted from an algorithm formula taking into account the specific parameters correlated to the patient's care.8 The mean costs per patient (including both acute and rehabilitation stays) were estimated for each cardiovascular complication. All analyses were performed using SAS software version 9.2 (Cary, NC, USA).
Results
Patient characteristics and reasons for hospitalization
In France in 2012, 533 044 patients were hospitalized for AF as the principal, related, or associated diagnosis. The mean ± SD age of the population was 78.0 ± 11.4 years, 53.2% were ≥80 years, and 47.1% were women (Table 1). The prevalence of hypertension was 70.2 and 24.2% had diabetes mellitus. Overall, 50.2% of patients were hospitalized for a cardiovascular reason, most commonly for a cardiac dysrhythmia (22.5%), followed by heart failure (18.3%), vascular/ischaemic diseases (7.1%), stroke/transient ischaemic attack (TIA)/systemic embolism (SE) (6.9%), and haemorrhages (1.3%) (Table 2).
Table 1.
Patient baseline characteristics
| All patients (n = 533 044) | |
|---|---|
| Mean age (years) | 78.0 ± 11.4 |
| Median (Q1–Q3) | 80 (72–86) |
| Minimum, maximum | 18–110 |
| Age ≥80 years | 53.2 |
| Women | 47.1 |
| Coexisting conditions (%) | |
| Alcohol-related diagnosis | 6.1 |
| Anaemia | 23.8 |
| Cancer | 19.0 |
| Diabetes mellitus | 24.2 |
| Dyslipidaemia | 27.8 |
| Hypertension | 70.2 |
| Inflammatory disease | 9.8 |
| Liver failure | 4.7 |
| Lung disease | 22.5 |
| Neurological disease | 10.4 |
| Obesity | 17.6 |
| Renal failure | 22.8 |
| Thyroid disease | 13.4 |
| Cardiovascular history (%) | |
| Stroke | 8.1 |
| Ischemic | 6.3 |
| Haemorrhagic | 1.1 |
| Unspecified | 1.7 |
| Major haemorrhage | 2.4 |
| Intracranial | 0.5 |
| Gastrointestinal | 1.0 |
| Any severe bleeding | 1.1 |
| TIA | 3.0 |
| SE | 3.1 |
| Vascular disease | 17.7 |
| Myocardial infarction | 8.0 |
| Peripheral arterial disease | 9.8 |
| Occlusions | 4.4 |
| Other ischaemic heart disease | 22.1 |
| AF symptoms present | 7.3 |
| Heart failure (including dyspnoea) | 29.5 |
| Cardiac dysrhythmia | 7.6 |
| Abnormal cardiac conduction | 16.3 |
| Valvular disease/surgery | 13.8 |
| Risk scores | |
| Stroke: CHA2DS2-VASc | 4.0 ± 1.8 |
| Haemorrhage: HAS-BLED | 2.2 ± 1.1 |
CHA2DS2-VASc, Cardiac failure or dysfunction, Hypertension, Age ≥75 (Doubled), Diabetes, Stroke (Doubled)-Vascular disease, Age 65–74, and Sex category (Female); HAS-BLED, Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio (INR), Elderly, Drugs/alcohol concomitantly
Table 2.
Reason for hospitalization (n = 533 044 patients) (patients may have several hospitalizations)
| Reason for hospitalization | Hospital stays, n (%) | Patients, n (%) |
|---|---|---|
| Number of patients | 833 127 | 533 044 |
| Cardiovascular reason | 347 862 (41.8) | 267 681 (50.2)a |
| Cardiac dysrhythmia | 138 939 (16.7) | 119 930 (22.5)a |
| Haemorrhage | 7485 (0.9) | 7013 (1.3)a |
| Heart failure | 120 310 (14.4) | 97 622 (18.3)a |
| Stroke/TIA/SE | 39 156 (4.7) | 36 320 (6.9)a |
| Vascular/ischaemic diseases | 41 972 (5.0) | 37 670 (7.1)a |
| Non-cardiovascular reason | 485 265 (58.2) | 369 515 (69.3)a |
| Cancer | 29 588 (3.6) | 25 894 (4.9)a |
| Digestive disease | 42 539 (5.1) | 37 864 (7.1)a |
| Ophthalmology | 13 893 (1.7) | 11 401 (2.1)a |
| Pneumology | 74 415 (8.9) | 63 750 (12.0)a |
| Rheumatology | 28 737 (3.4) | 26 810 (5.0)a |
| Other non-cardiovascular reason | 296 093 (35.5) | 203 796 (38.2)a |
Data given as number (%).
aPatients may have several hospitalizations.
Resource use and costs
Resource use
Of the cardiovascular-related hospitalizations, 44.9% required emergency admission. The mean length of stay (LOS) in acute care was 8.2 ± 9.3 days. In the 15.8% of patients who required transfer to a rehabilitation unit, the LOS for rehabilitation was 32.0 ± 28.5 days.
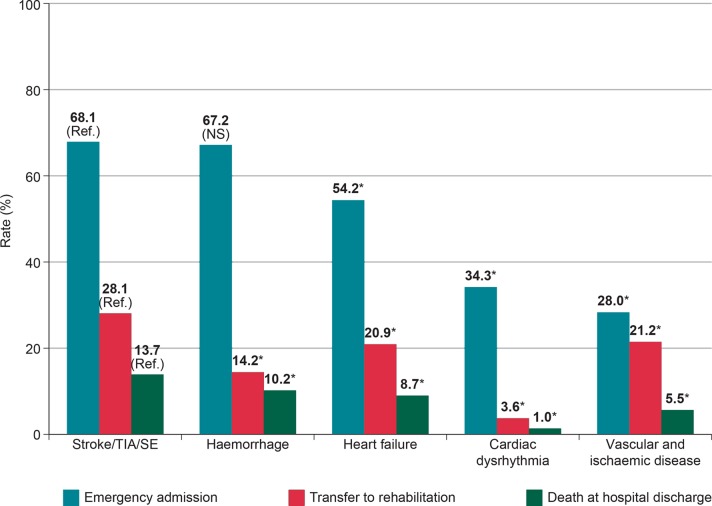
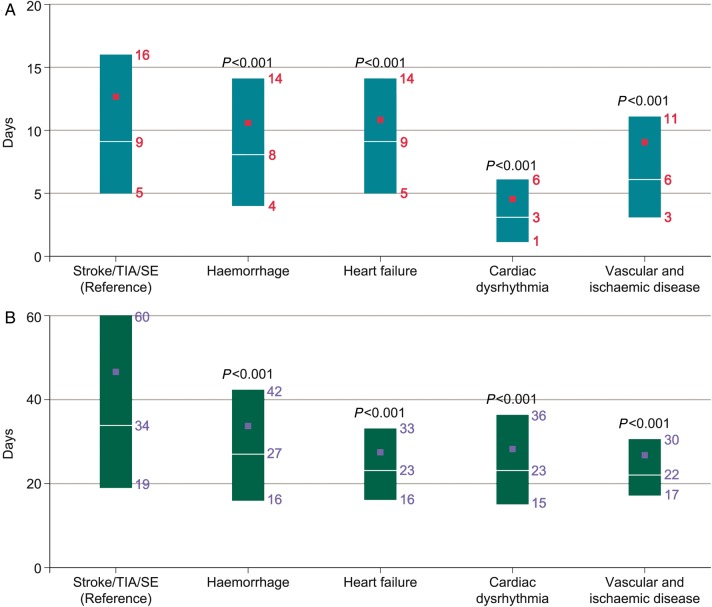
A total of 50 165 patients (9.4%) died during hospitalization, of which 17 066 (34.0%) were cardiovascular deaths. Of the cardiovascular complications, patients with stroke/TIA/SE showed significantly higher rates (P < 0.0001) of emergency admission, transfer to rehabilitation, and death at hospital discharge compared with patients with heart failure, cardiac dysrhythmia, or vascular/ischaemic diseases, but not for patients with haemorrhages (Figure 1). The length of stay was longer for patients with stroke/TIA/SE than for other cardiovascular complications, for both acute care (median: 9.0; Q1–Q3: 5.0–16.0) (Figure 2A) and rehabilitation care (median: 34.0; Q1–Q3: 19.0–30.0) (Figure 2B). In hospitalized patients with AF who had a stroke, 74.9% required emergency admission to hospital and 34.2% required rehabilitation in hospital (Table 3).
Figure 1.
Emergency admission, transfer to rehabilitation unit, and death at hospital discharge according to type of cardiovascular complication (*P < 0.0001 vs. stroke/TIA/SE; NS: non-significant difference vs. stroke/TIA/SE). SE, systemic embolism; TIA, transient ischaemic attack.
Figure 2.
Length of hospital stay for (A) acute care and (B) rehabilitation, according to the type of cardiovascular complication. Horizontal white lines indicate median; rectangles indicate Q1–Q3; solid squares indicate mean. SE, systemic embolism; TIA, transient ischaemic attack.
Table 3.
Resource use and in-hospital death for patients hospitalized for a stroke, TIA, or SE
| Stroke |
TIA (n = 5194) | SE (n = 5725) | ||||
|---|---|---|---|---|---|---|
| All types (n = 25 401) | Ischaemic (n = 19 909) | Haemorrhagic (n = 4228) | Unspecified (n = 1615) | |||
| Emergency admission, n (%) | 20 419 (74.9) | 16 113 (76.4) | 3106 (68.9) | 1200 (72.7) | 4240 (79.1) | 1996 (30.5) |
| Length of acute stay (days) | ||||||
| Mean ± SD | 14 ± 14 | 14 ± 13 | 15 ± 17 | 12 ± 12 | 7 ± 7 | 11 ± 13 |
| Median (Q1–Q2) | 11 (6–17) | 11 (6–17) | 10 (4–19) | 9 (5–16) | 6 (4–10) | 8 (3–14) |
| Rehabilitation stay, n (%) | 8694 (34.2) | 6921 (34.8) | 1392 (32.9) | 412 (25.5) | 431 (8.3) | 968 (16.9) |
| Length of rehabilitation stay (days) | ||||||
| Mean ± SD | 48 ± 43 | 48 ± 43 | 51 ± 46 | 43 ± 39 | 33 ± 31 | 38 ± 36 |
| Median (Q1–Q2) | 35 (20–62) | 35 (20–62) | 37 (22–65) | 32 (18–56) | 26 (15–38) | 28 (16–47) |
| Death at discharge, n (%) | 4242 (16.7) | 2614 (13.1) | 1334 (31.6) | 294 (18.2) | 69 (1.3) | 590 (10.3) |
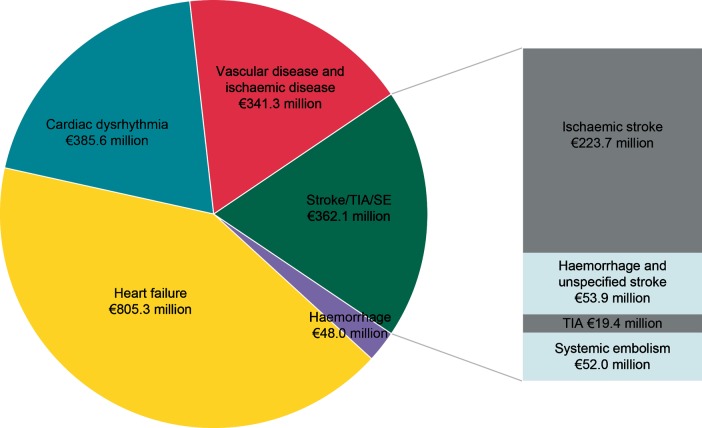
Global costs
The overall costs for the management of cardiovascular complications were €1.94 billion. Heart failure represented €805 million (41.5%), cardiac dysrhythmia €386 million (19.9%), stroke/TIA/SE €362 million (18.7%), vascular/ischaemic diseases €341 million (17.6%), and haemorrhages €48 million (2.5%) (Figure 3). Hospitalization for AF symptoms as the principal diagnosis was collected in the cardiac dysrhythmia group, and represented 5674 stays (5433 patients) for a total amount of €9.5 million in 2012. Acute care was provided in public hospitals for 75.0% of patients and rehabilitation care for 66.2% of patients (Table 4). These rates increased to 88.8 and 75.2%, respectively, for patients with stroke/TIA/SE.
Figure 3.
Distribution of cardiovascular hospitalization costs in AF patients in 2012 in France (€1.94 billion). AF, atrial fibrillation; SE, systemic embolism; TIA, transient ischaemic attack.
Table 4.
Global cost (€1.94 billion) of cardiovascular hospitalizations in 2012
| Hospitalization costs in 2012 | All cardiovascular complications (n = 267 681) | Stroke/TIA/SE (n = 36 320) | Haemorrhage (n = 7013) | Heart failure (n = 95 655) | Cardiac dysrhythmia (n = 116 890) | Vascular/ischaemic diseases (n = 36 444) |
|---|---|---|---|---|---|---|
| Acute care | €1 619 418 327 | €236 282 000 | €40 245 062 | €682 869 176 | €360 665 441 | €299 356 648 |
| Treatment in public hospitals (% patients) | 75.0 | 88.8 | 88.4 | 81.2 | 67.3 | 67.3 |
| Rehabilitation care | €322 906 651 | €125 785 587 | €7 731 816 | €122 454 928 | €24 958 238 | €41 976 082 |
| Treatment in public hospitals (% patients) | 66.2 | 75.2 | 72.8 | 64.3 | 67.4 | 59.4 |
| All hospital care | €1 942 324 978 | €362 067 587 | €47 976 878 | €805 324 105 | €385 623 679 | €341 332 729 |
SE, systemic embolism; TIA, transient ischaemic attack.
Mean costs per patient per event
In patients hospitalized for a cardiovascular complication, those with stroke/TIA/SE had the highest mean cost per patient (€10 094), followed by vascular/ischaemic diseases (€9366), heart failure (€8419), haemorrhages (€6841), and cardiac dysrhythmia (€3299). Haemorrhagic stroke had a higher mean cost per patient (€12 748) than ischaemic stroke (€11 234), SE (€9087), unspecified stroke (€8108), and TIA (€3734).
Discussion
A total of 533 044 patients with AF were hospitalized in France in 2012 (841 per 100 000 inhabitants), half for a cardiovascular reason, and 53.2% were among the very elderly (≥80 years). Consequently the annual burden for cardiovascular complications related to AF is huge, costing nearly €2 billion, and equivalent to 2.6% of the total expenditure of French hospitals in 2012. To our knowledge, this is the first national cost-of-illness estimate for AF complications in France. It can, however, be measured against UK data, where 0.9–2.4% of the UK healthcare budget was allocated to AF in 2000, and against US data, where $6.65 billion was attributed to AF hospitalizations in 2005.9 Previously, based on 2000 data from France, Jeantet et al.10 estimated the cost of treatment for the first two episodes of AF to be €305 million.
The results from this study show that the use of healthcare resources in patients with AF is substantial: 45% of patients were hospitalized as an emergency admission and the mean LOS in acute care exceeded 1 week. Of the cardiovascular complications, stroke/TIA/SE required the greatest use of healthcare resources (i.e. emergency admission, transfer to rehabilitation unit, and LOS) and cost the most per patient. Hence, minimizing the risk of stroke in patients with AF is vital, not only from a healthcare perspective but also from an economic perspective. Ischaemic stroke is also a largely avoidable complication in the presence of effective anticoagulant prophylaxis. As a previous study reported, before the introduction of non-vitamin K oral antagonists (NOACs), a quarter of patients with AF in France received no antithrombotic therapy, 50.7% were treated with a vitamin K antagonist, 19.9% with aspirin, and 4.3% with clopidogrel (with or without aspirin).11 Vitamin K antagonists require close monitoring to maintain treatment within the target therapeutic range, but data from the primary care setting demonstrate that barely half of the patients receiving vitamin K antagonist therapy have a well-controlled international normalized ratio.12 Non-vitamin K oral antagonists offer a new therapeutic approach for the prevention of stroke and SE and are cost-effective when compared with warfarin.13,14 In addition, recent studies have shown that patients on NOACs have a significantly shorter LOS in hospital compared with patients receiving warfarin.1,15,16 A re-evaluation of our findings when NOACs are more widely used in France may thus be of interest.
The high rate of emergency admissions for stroke reflects an inappropriate use of resources in France, especially as only a small percentage of patients are admitted direct to acute stroke centres.17 This finding may explain the higher rate of patients with strokes managed in public hospitals (where most emergency units are located) as opposed to private hospitals. A similar relationship can be observed for haemorrhage and heart failure. The use of healthcare resources in the 36 320 patients with stroke/TIA/SE was generally homogenous, but with a few notable exceptions. Although often thought of as benign, four-fifths of AF patients with a TIA were admitted to hospital as emergencies, and the mean acute LOS exceeded a week. While this could potentially be viewed as a poor use of resources, the general public is appropriately encouraged to attend the emergency department if they experience early signs suggestive of stroke, and often the transient nature of the symptom may not be apparent at the time of presentation. Furthermore, the long LOS for TIA in patients with AF may be related to the patient's age or their social situation, which cannot be evaluated in our study, but is similar to that reported in a Spanish study (mean 8 days vs. 7.3 days, respectively).18
The rate of death at discharge was also considerably higher for patients with haemorrhagic stroke when compared with the other cardiovascular complications. This finding is concert with recent data showing that patients with haemorrhagic stroke were at greater risk of dying within the first 30 days of the event when compared with those with ischaemic stroke.19 Despite the substantial costs related to stroke in the study population, additional costs correspond to a global cardiac disease. Many aspects of the current care for AF patients set apart treatment ‘strategies', while an approach that takes into account all aspects of their cardiac profile may achieve better clinical outcomes. Optimizing the management of these patients, including the use of evidence-based cardiac medications, particularly for heart failure associated with AF, will ultimately reduce the healthcare costs in these patients.
Strengths and limitations
The principal strength of this study was the use of the French PMSI database, which contains information on all public and private hospital stays in France. This medico-administrative database has also been used for epidemiological and medico-economic purposes in many medical fields, including studies assessing the incidence of stroke and haemorrhage.6,20 Analyses from the PMSI database allow ‘real-world’ research that would not be feasible if conducted in a prospective manner. The reports contained in the PMSI database are coded under the responsibility of the head physician at each medical unit and with the quality support of a dedicated department in each hospital; coding may, however, have been performed by a more junior member of staff. External quality controls are also conducted by insurers, as hospital financial resources are directly related to the coded information.
Nevertheless, some limitations must be acknowledged. Only the burden of hospitalizations has been taken in account in our study, which also underestimated some factors. First, in everyday clinical practice, patients with non-major complications (e.g. mild bleeding) are not systematically hospitalized, and may therefore be under-reported in our study. Secondly, the absence of consultation and prescription data in community care is a limitation, but is small relative to the cost of hospitalization for cardiovascular complications. Indeed, in the future it may be possible to address the burden of disease in France using a national health insurance database, which contains both hospital and community care reimbursement data. Finally, our analysis included all AF diagnoses, irrespective of whether it was the primary reason for hospitalization or a coexisting condition. In a proportion of heart failure admissions, for example, AF may be a co-morbidity that has only a small impact on the costs of admission, and thus we may have overestimated the costs attributed to AF in this analysis.
Conclusion
Atrial fibrillation-related cardiovascular complications pose a substantial economic burden in French hospitals, and emphasize the need to minimize the risk of cardiovascular events in this population.
Funding
The work was supported by Bristol-Myers Squibb and Pfizer.
Conflict of interest: F.-E.C. and A.-F.G.: employee of Bristol-Myers Squibb; G.C., A.V., and L.F.: consulting fees from Bristol-Myers Squibb and Pfizer; and A.S.: grants from Bristol-Myers Squibb.
Acknowledgements
The authors thank Sophie Rushton-Smith, PhD, for editorial assistance on this manuscript.
References
- 1. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370–75. [DOI] [PubMed] [Google Scholar]
- 2. Wilke T, Groth A, Mueller S, Pfannkuche M, Verheyen F, Linder R, et al. Incidence and prevalence of atrial fibrillation: an analysis based on 8.3 million patients. Europace 2013;15:486–93. [DOI] [PubMed] [Google Scholar]
- 3. Charlemagne A, Blacher J, Cohen A, Collet JP, Dievart F, de Groote P, et al. Epidemiology of atrial fibrillation in France: extrapolation of international epidemiological data to France and analysis of French hospitalization data. Arch Cardiovasc Dis 2011;104:115–24. [DOI] [PubMed] [Google Scholar]
- 4. Piccini JP, Hammill BG, Sinner MF, Hernandez AF, Walkey AJ, Benjamin EJ, et al. Clinical course of atrial fibrillation in older adults: the importance of cardiovascular events beyond stroke. Eur Heart J 2014;35:250–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983–8. [DOI] [PubMed] [Google Scholar]
- 6. Cotte FE, Chaize G, Kachaner I, Gaudin AF, Vainchtock A, Durand-Zaleski I. Incidence and cost of stroke and hemorrhage in patients diagnosed with atrial fibrillation in France. J Stroke Cerebrovasc Dis 2014;23:e73–83. [DOI] [PubMed] [Google Scholar]
- 7. Schnitzler A, Woimant F, Nicolau J, Tuppin P, de Peretti C. Effect of rehabilitation setting on dependence following stroke: an analysis of the French inpatient database. Neurorehabil Neural Repair 2014;28:36–44. [DOI] [PubMed] [Google Scholar]
- 8. Grelier S, Thetio M, Quentin V, Achache V, Sanchez N, Leroux V, et al. Risk assessment analysis of the future technical unit dedicated to the evaluation and treatment of motor disabilities. Ann Phys Rehabil Med 2011;54:73–87. [DOI] [PubMed] [Google Scholar]
- 9. Wolowacz SE, Samuel M, Brennan VK, Jasso-Mosqueda JG, Van Gelder IC. The cost of illness of atrial fibrillation: a systematic review of the recent literature. Europace 2011;13:1375–85. [DOI] [PubMed] [Google Scholar]
- 10. Jeantet M, Losay J, Cassinat G, Andral J, Guize L, de Pouvourville G. Paroxysmal atrial fibrillation in community medicine: management intentions and cost estimates. Arch Mal Coeur Vaiss 2001;94:1103–9. [PubMed] [Google Scholar]
- 11. Sabouret P, Depret-Bixio L, Cotte FE, Marie P, Bedira N, Blin P. Sex differences in stroke prevention in atrial fibrillation in French primary care. Results of the AFIGP (Atrial Fibrillation In General Practice) Database. Clin Res Cardiol 2014;103:887–93. [DOI] [PubMed] [Google Scholar]
- 12. Cotte FE, Benhaddi H, Duprat-Lomon I, Doble A, Marchant N, Letierce A, et al. Vitamin K antagonist treatment in patients with atrial fibrillation and time in therapeutic range in four European countries. Clin Ther 2014;36:1160–8. [DOI] [PubMed] [Google Scholar]
- 13. Lanitis T, Cotte FE, Gaudin AF, Kachaner I, Kongnakorn T, Durand-Zaleski I. Stroke prevention in patients with atrial fibrillation in France: comparative cost-effectiveness of new oral anticoagulants (apixaban, dabigatran, and rivaroxaban), warfarin, and aspirin. J Med Econ 2014;17:587–98. [DOI] [PubMed] [Google Scholar]
- 14. Chevalier J, Delaitre O, Hammes F, de Pouvourville G. Cost-effectiveness of dabigatran versus vitamin K antagonists for the prevention of stroke in patients with atrial fibrillation: a French payer perspective. Arch Cardiovasc Dis 2014;107:381–90. [DOI] [PubMed] [Google Scholar]
- 15. Laliberte F, Pilon D, Raut MK, Nelson WW, Olson WH, Germain G, et al. Hospital length of stay: is rivaroxaban associated with shorter inpatient stay compared to warfarin among patients with non-valvular atrial fibrillation? Curr Med Res Opin 2014;30:645–53. [DOI] [PubMed] [Google Scholar]
- 16. Cowper PA, Pan W, Anstrom K, Stafford J, Lopes R, Davidson-Ray L, et al. Apixaban reduces hospitalization in patients with atrial fibrillation: an analysis of the effect of apixaban therapy on resource use in the apixaban for reduction in stroke and other thromboembolic events in atrial fibrillation. J Am Coll Cardiol 2013;61:10_S. [Google Scholar]
- 17. Leys D, Cordonnier C, Debette S, Hacke W, Ringelstein EB, Giroud M, et al. Facilities available in French hospitals treating acute stroke patients: comparison with 24 other European countries. J Neurol 2009;256:867–73. [DOI] [PubMed] [Google Scholar]
- 18. Alvaro LC, Lopez-Arbeloa P, Cozar R. Hospitalizations for acute cerebrovascular accidents and transient ischemic attacks in Spain: temporal stability and spatial heterogeneity, 1998–2003. Rev Calid Asist 2009;24:16–23. [DOI] [PubMed] [Google Scholar]
- 19. Henriksson KM, Farahmand B, Asberg S, Edvardsson N, Terent A. Comparison of cardiovascular risk factors and survival in patients with ischemic or hemorrhagic stroke. Int J Stroke 2012;7:276–81. [DOI] [PubMed] [Google Scholar]
- 20. Heng C, Rybarczyk-Vigouret MC, Michel B. Anticoagulant-related hospital admissions: serious adverse reactions identified through hospital databases. Pharmacoepidemiol Drug Saf 2015;24:144–51. [DOI] [PubMed] [Google Scholar]