Abstract
Introduction
Numerous studies have demonstrated that plasma transforming growth factor-β1 (TGF-β1) may be involved in the pathogenesis of atrial fibrillation (AF), but some discrepancy remained. We performed a meta-analysis to evaluate the association between the plasma level of TGF-β1 and the risk of AF.
Methods
Published clinical studies evaluating the association between the plasma level of TGF-β1 and the risk of AF were retrieved from PubMed and EMBASE databases. Two reviewers independently evaluated the quality of the included studies and extracted study data. Subgroup analysis and sensitivity analysis were performed to evaluate for heterogeneity between studies.
Results
Of the 395 studies identified initially, 13 studies were included into our analysis, with a total of 3354 patients. Higher plasma level of TGF-β1 was associated with increased risk of AF when evaluated as both a continuous variable (SMD 0.67; 95%CI 0.29–1.05) and a categorical variable (OR 1.01, 95% CI 1.01–1.02).
Conclusions
This meta-analysis suggests an association between elevated plasma TGF-β1 and new onset AF. Additional studies with larger sample sizes are needed to further investigate the relationship between plasma TGF-β1 and the occurrence of AF.
Introduction
Atrial fibrillation (AF) is the most common sustained arrhythmia with debilitating consequences such as stroke and heart failure. It is also associated with an increase in overall mortality [1,2,3]. Animal models and studies on patients with AF have confirmed that the development of AF is associated with both structural and electrical remodeling of the atria [4]. Patients with chronic AF have significant myocardial interstitial fibrosis which contributes to the occurrence and perpetuation of AF [5, 6]. Transforming growth factor-β1 (TGF-β1) is an important factor in fibrosis [7]. It is involved in the process of cell proliferation, apoptosis and migration. It promotes the differentiation of cardiac fibroblasts and production of extracellular matrix such as collagen, fibronectin, and protein polysaccharide which leads to cardiac fibrosis [8]. In transgenic mouse models, the activation of TGF-β1 promotes atrial fibrosis and the development of AF [9]. On the other hand, the inhibition of TGF-β1 by pirfenidone (PFD) can significantly reduce the extent of atrial fibrosis [10]. These findings have prompted clinical studies on the relationship between plasma TGF-β1 levels and the development of AF in humans. However, the results generated have been inconsistent. Therefore, we conducted a comprehensive meta-analysis to evaluate the available evidence of whether high plasma TGF-β1 levels are related to the risk of having AF.
Methods
Search strategy
Articles were identified by searching PubMed and Embase online databases for articles published up until November 2015. The key terms used are ‘TGF-β1’, ‘transforming growth factor-β1’, ‘transforming growth factor-beta1’, ‘transforming growth factor’ and ‘atrial fibrillation’. We manually searched the bibliographies of original papers and abstracts of the scientific sessions of the past 3 years. In addition, we sought the assistance from potential experts in the field to assess the quality of included articles. We evaluated the titles, abstracts and reference lists of all articles to identify potentially relevant studies.
Trial selection and inclusion criteria
Two reviewers (J. L. and Y. Y.) evaluated the titles and abstracts of all eligible studies. The full text of relevant studies was retrieved and assessed accordingly based on the inclusion criteria. Any disagreements on whether to include any study between the two investigators were resolved through joint review and discussions.
For inclusion, eligible trials should meet the following criteria: (1) the study design was case-control, prospective or retrospective cohort studies; (2) human subjects; (3) included the characteristics of study patients; (4) clearly defined endpoint events, such as AF occurrence or recurrence; (5) evaluated the plasma TGF-β1 levels of AF patients and non-AF patients; (6) reported the plasma level of TGF-β1 using [mean ± standard deviation (SD)] and odds ratio (OR) or hazard ratio (HR) of AF incidence and the corresponding 95% confidence interval (CI) for TGF-β1 levels.
Data extraction
Two independent reviewers (J. L. and Y. Y.) extracted data from included studies using a standard data extraction form. Information on authors and published journals were removed and then independently evaluated according to the described inclusion criteria. Relevant data were extracted from the manuscripts. We extracted and analyzed the plasma concentration of TGF-β1 expressed as mean ± SD from each primary study. Adjusted OR values were selected for the analysis. Additional data collected included study characteristics (first author’s last name, publication year, study design, sample size, AF definition, follow-up duration, end-point events) and patients baseline characteristics (age, sex, BMI, smoking, mean left atria diameter, left ventricular ejection fraction, the presence of CAD, hypertension, diabetes and medication).
Quality assessment
The two investigators (J. L. and Y. Y.) independently evaluated the quality of the eligible studies based on the guidelines by the Evidence-Based Medicine Working Group [11] and the United States Preventive Task Force [12]. Each study was judged in accordance to the 10-item STROBE checklist. We appraised the quality of studies according to the following characteristics: (1) the inclusion and exclusion criteria are clearly defined; (2) sample selection is clearly described; (3) involved population is representative of study sample; (4) the patients’ follow-up period is adequate; (5) reports loss of follow-up; (6) clinical and demographic variables are complete; (7) the definition of AF is clearly defined; (8) the outcomes and outcome assessment are clearly defined; (9) temporality (evaluation of plasma TGF-β1 levels at baseline) and (10) adjustment of possible confounders on the multivariate analysis, especially for categorical variable. If any of the characteristics was not described, we assumed that it had not been performed.
Statistical analysis
All continuous variables were presented as (mean ± SD). The standard mean difference (SMD) was used to analyze the results in our meta-analysis. SMD method was used as different unit of measurements were presented for TGF-β1 levels. As the studies included in this meta-analysis may have used either a continuous or categorical variable for TGF-β1 levels, we performed a separate meta-analysis for both types of variables to evaluate the association between TGF-β1 levels and the occurrence of AF. The HR values in multivariate Cox proportional hazards model in each primary study were directly considered as OR values. I2 derived from the chi-square test was used to evaluate the heterogeneity across the studies included. I2 of ≤50% indicates that there was no significant heterogeneity [13]. A fixed effects model was used if no significant heterogeneity was found. When pooled effect resulted in significant heterogeneity, the random effects model was used. We conducted random effects meta-analysis using the inverse variance heterogeneity method. In addition, we also performed subgroup analysis based on the patients’ age (≤50y or >50y), study design (cohort study or case control study), duration of follow-up (<12 months or ≥12 months), sample size (<100 or ≥100) and left ventricular ejection fraction (LVEF) (<50% or ≥50%). Sensitivity analysis was performed by sequentially removing each individual study. We assessed for publication bias by constructing a funnel plot. Two-tailed p value of <0.05 was considered statistically significant. All statistical analyses were performed with Review Manager Version 5.3.
Results
Search results
Data retrieval and study selection was shown in the flow chart (Fig 1). A total of 395 studies were found using our search criteria. After reviewing title and abstract of each study, we excluded 356 articles because they were either unrelated, review articles or basic science research papers. Then, we evaluated the remaining 39 studies in detail. Of these 39 studies, we excluded 26 studies because: 1 had duplicate data, 17 did not provide the plasma TGF-β1 levels, 6 did not provide (mean ± SD) data of TGF-β1 or OR/HR values, 1 did not provide baseline characteristics of patients and 1 had no control group. Finally, the remaining 13 studies were included into our meta-analysis.
Fig 1. Flow chart of study selection.

SD, standard deviation.
Study characteristics
We included 13 studies with a total of 3354 patients of which 1154 patients have AF and 2200 patients have no AF. The main features of the studies are exhibited in Table 1, and the patients’ baseline characteristics are summarized in Table 2. Confounding factors used in multivariate analysis are shown in Table 3. Out of the 13 included studies, 6 studies[14–19] demonstrated that AF patients had higher plasma TGF-β1 levels, regardless of whether it was new-onset AF or recurrent AF, but the remaining 7[20–26] presented no significant correlation between plasma TGF-β1 levels and occurrence of AF. 12[14–26] studies in which the plasma TGF-β1 levels was expressed as (mean ± SD) were analyzed using TGF- β1 as a continuous variable. 4[15, 19, 25, 26] studies with OR/HR values in which the plasma TGF-β1 levels was analyzed as a categorical variable had been included in a separate analysis. Of the 13 included studies, 3 studies [15, 19, 25] analyzed TGF-β1 levels as both a continuous variable and categorical variable.
Table 1. General data of studies included in meta-analysis.
| Investigator (year) | Location | Patients number (n) | Study population | Design type | Mean follow-up | Endpoint | Duration of AF | Quality score |
|---|---|---|---|---|---|---|---|---|
| Wang 2010 | China | 540 | Patients who were newly diagnosed essential hypertensive and none of them received anti-hypertensive treatment. | Case control study | During hospitalization | The occurrence of AF was determined by 12-lead electrocardiography (ECG) and/or 24-h Holter monitoring. | NA | 7 |
| Wu 2013 | Taiwan | 46 | Nonparoxysmal AF patients who underwent catheter ablation. | Cohort study | 10.9 ± 7.4 months | The clinically documented recurrence of atrial arrhythmias or repeat ablation procedures. An AF recurrence was defined as an episode lasting >1 minute and was confirmed by ECG 3 months after the ablation. | 71.3±58.1 months | 9 |
| On 2009 | Korea | 76 | Patients who underwent both the open heart operation for mitral valvular heart disease and the surgical maze procedure for AF. | Cohort study | 12 months | The primary end point of the study was the persistence of AF after the maze procedure with cryoablation. | 3.4 years | 8 |
| Xiao 2010 | China | 38 | Patients with RHD who underwent valve replacement surgery. | Case control study | During hospitalization | The occurrence of AF. The patients were divided into 3 groups: the sinus rhythm group, the paroxysmal AF group, and the chronic AF group (AF lasting ≥6 months). | NA | 7 |
| Zhao 2014 | China | 90 | VHD patients, comprising pathological changes in the mitral or aortic valves, or both, who underwent valve replacement surgery | Case control study | During hospitalization | The occurrence of AF. (Persistent AF:AF lasting >6 month and paroxysmal AF: recurrent AF that terminated spontaneously in <7 days.) | NA | 7 |
| Kim 2009 | Korea | 74 | Patients with persistent AF who underwent external electrical cardioversion. | Cohort study | 13.2 ± 11.0 months | AF recurrence after successful cardioversion. | NA | 8 |
| Mira 2013 | China | 80 | Patients with AF. | Case control study | During hospitalization | The occurrence of AF. Patients were divided into paroxysmal AF group and persistent AF group according to whether they could convert to sinus rhythm spontaneously. | NA | 7 |
| Lin 2015 | China | 112 | Patients with a history of essential hypertensive. | Case control study | During hospitalization | AF was determined by 12-lead electrocardiography (ECG) and/or 24-h Holter monitoring. Persistent AF: AF lasting >6 month. | 13.12±9.96 years | 7 |
| Kimura 2014 | Japan | 44 | AF patients who received an initial catheter ablation | Cohort study | 9.7 ± 2.4 months | AF recurrence was defined as a documented AF for more than 30 seconds after three months of a blanking-period. | 53±29 months | 8 |
| Shim 2013 | Korea | 575 | Patients with AF who underwent radiofrequency catheter ablation. | Cohort study | 15 ± 7 months | If any ECG documented an AF episode within the three-month blanking period during follow-up, the patient was diagnosed with an early recurrence, and any AF recurrence thereafter was diagnosed with clinical recurrence. | NA | 8 |
| Smit 2012 | Netherland | 100 | Patients were included if they had short-lasting persistent AF, defined as a total AF history of, 2 years, a total persistent AF history of, 6 months, and ≤1 previous electrical cardioversion. | Cohort study | 12 months | The primary endpoint consisted of early AF recurrence, defined as any (a)symptomatic recurrence of AF within the first month after cardioversion lasting ≥30s. Secondary endpoint was progression to permanent AF within 1 year. | 4.2 months | 9 |
| Canpolat 2014 | Turkey | 41 | Lone paroxysmal AF patients who underwent preablation DE-MRI. Lone AF was defined in patients who were <60 years old; without structural heart disease based on patient history, physical examination, and imaging methods including chest X-ray and echocardiography; and no history of coronary artery disease, diabetes mellitus, or hypertension. Paroxysmal AF is defined as self-terminating episode, usually within 48 hours, that may continue for up to 7 days. | Cohort study | 18 months | Recurrence of AF is defined as detection of AF (at least 30 seconds duration when assessed with ECG monitoring) >3 months following AF ablation. | 60 months | 8 |
| Rosenberg 2014 | America | 1538 | Participants were recruited for The Cardiovascular Health Study. | Cohort study | 12 months | The occurrence of AF. (1) Annual outpatient study ECGs were interpreted by the EPICARE ECG reading center, where the diagnoses of AF or atrial flutter were verified; (2) hospital discharge diagnoses that included codes for AF and flutter were also included, although AF or flutter diagnoses that were made during the same hospitalization as coronary artery bypass surgery or heart valve surgery were not counted. | NA | 9 |
AF = atrial fibrillation; RHD = rheumatic heart disease; VHD = valvular heart disease; CHF = congestive heart failure.
Table 2. Patients characteristics of included studies.
| Investigator (year) | Mean age (y) | Male (%) | BMI (kg/m2) | Smoker (%) | HTN (%) | DM (%) | CAD (%) | Mean LAD (mm) | Mean LVEF (%) | Medication | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β-blocker (%) | ACEI/ARB (%) | Statin (%) | Amiodarone (%) | ||||||||||
| Wang 2010 | 45.9 | - | 25.8 | 56.1 | 100 | 0 | 0 | - | - | 0 | 0 | 0 | 0, |
| Wu 2013 | 52.8 | 91.3 | 26.2 | - | 28.3 | 2.2 | 2.2 | 44.6 | 54.6 | - | 23.9 | 4.3 | 26.1 |
| On 2009 | 53.9 | 44.7 | - | 23.7 | 22.4 | 14.5 | - | 60.2 | - | - | - | - | - |
| Xiao 2010 | 41.2 ± 9.1 | - | - | - | 0 | - | 0 | 50.6 | 52.9 | - | 0 | - | - |
| Zhao 2014 | 50.8 | 45 | - | - | - | 0 | - | 50.9 | 54.5 | 65 | 58 | - | - |
| Kim 2009 | 58.6 | 77 | 24.7 | - | 28.4 | - | - | 45.8 | 49.1 | 24.3 | 35.1 | 10.8 | 64.9 |
| Mira 2013 | 49.5 | 57.5 | - | - | - | - | - | 57.3 | 60.5 | - | 0 | - | - |
| Lin 2015 | 67.5 | 62.5 | - | 32.1 | 100 | 21.4 | - | 38.5 | 61.6 | 0 | 0 | 0 | 0 |
| Kimura 2014 | 59 ± 8 | - | 23.2 ± 2.6 | - | - | - | - | 39 ± 6 | 71.9 ± 9.4 | 37.9 | 20.7 | 17.2 | - |
| Shim 2013 | 55.7 ± 10.9 | 77.7 | 24.8 ± 2.8 | - | 44 | 10.3 | - | 41.4 ± 6.2 | 61.3 ± 8.3 | 0 | 0 | 0 | 0 |
| Smit 2012 | 65 ± 9 | 74. | - | 62 | 67 | 14 | 18 | 45 ± 6 | 19 ± 13 | 89 | 74 | 38 | 12 |
| Canpolat 2014 | 49.2 ± 7.6 | 58.5 | 27.1±5.2 | 31.7 | 0 | 0 | 0 | 41.2 | 68.2±4.5 | - | - | - | 31.7 |
| Rosenberg 2014 | 77.8 ± 4.6 | 37.9 | - | 9.2 | 56.3 | 16.8 | - | - | - | - | - | - | - |
BMI = body mass index; HNT = hypertension; DM = diabetes mellitus; CAD = coronary artery disease; LAD = left atrium diameter; LVEF = left ventricular ejectionfraction; ACEI = angiotensin converting enzyme inhibitors; ARB = angiotensin receptor blocker.
Table 3. Confounding factors used in multivariate analysis.
| Investigator (year) | HR/OR | 95%CI | P value | Adjustment |
|---|---|---|---|---|
| Canpolat 2014 | HR:1.013(Univariate model) | 1.010–1.018 | 0.001 | NA |
| Smit 2012 | HR:1.2 | 1.0–1.5 | 0.04 | Left ventricular ejection fraction, and early AF recurrence. |
| Wu 2013 | OR:1.11 | 1.01–1.22 | 0.031 | Age, sex, body mass index, use of angiotensin-converting enzyme inhibitor/ angiotensin II receptor blocker, left atrial diameter. |
| Rosenberg 2014 | HR:1.05 | 0.95–1.17 | 0.36 | Age, sex, race, clinic site, systolic blood pressure, hypertensive medications, body mass index, body mass index -squared, height, smoking status, history of CHF, MI, or prevalent diabetes. |
HR = hazard ratio; OR, odds ratio; CI = confidence interval; NA = not available; AF = atrial fibrillation; CHF = congestive heart failure; MI = myocardial infarction.
Main analysis
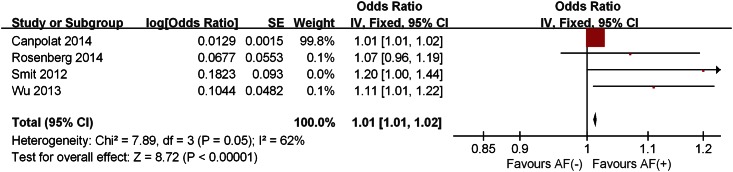
The pooled analysis of included studies showed that plasma TGF-β1 levels in the patients with AF was significantly higher than those without AF in both analyses; continuous variable (SMD 0.67; 95%CI 0.29–1.05) with significant heterogeneity across studies (I² = 91%, P<0.00001) (Fig 2) and categorical variable (OR 1.01, 95% CI 1.01–1.02) with moderate heterogeneity across studies (I² = 62%, P = 0.05) (Fig 3). Patients with persistent AF had higher TGF-β1 levels than that in paroxysmal AF patients (SMD 0.57; 95%CI 0.22–0.92) without significant heterogeneity (I² = 30%, P = 0.23) across studies (Fig 4).
Fig 2. Forest plot of the association between the plasma level of TGF-β1 and AF occurrence depending on different study population in which TGF-β1 levels were analyzed as continuous variable.
AF, atrial fibrillation; CI, confidence interval; SD, standard deviation.
Fig 3. Forest plot of the association between the plasma level of TGF-β1 and AF occurrence in which TGF-β1 levels were analyzed as a categorical variable.
AF, atrial fibrillation; CI, confidence interval; OR, odds ratio.
Fig 4. Forest plot of the association between the plasma level of TGF-β1 and the two different types of AF.
AF, atrial fibrillation; CI, confidence interval; SD, standard deviation.
Sensitivity and subgroup analysis
A subgroup analysis was performed based on the type of AF on 5 studies and it showed a positive correlation between high TGF-β1 plasma levels and the risk of new-onset AF (SMD 1.07; 95%CI 0.26–1.89) with significant heterogeneity (I² = 95%, P<0.00001) across studies. However, there was no clear relationship between plasma TGF-β1 levels and the risk of recurrent AF (SMD 0.38; 95%CI (-0.05–0.81) with significant heterogeneity (I² = 83%, P<0.00001) across studies (Fig 2).
A predefined subgroup analysis was performed to investigate the origin of the heterogeneity between studies. In the subgroups with follow-up <12 months, LVEF <50% and sample size ≥100, there were no significant heterogeneity between studies. Therefore, the follow-up duration, LVEF and sample size are likely the origin of the significant heterogeneity in our meta-analysis (Table 4).
Table 4. Subgroup analyses of the association between the TGF-β plasma levels and incidence of AF.
| Subgroup | Study | Number of studies | Heterogeneity | Meta-analysis | |||
|---|---|---|---|---|---|---|---|
| I2 | p-Value | SMD | 95% CI | p-Value | |||
| Follow-up duration | <12 months | 2 | 0% | 0.49 | 0.48 | [0.04, 0.92] | 0.03 |
| ≥12 months | 5 | 88% | <0.00001 | 0.36 | [-0.19, 0.92] | 0.2 | |
| Study design | Cohort | 7 | 83% | <0.00001 | 0.38 | [-0.05, 0.81] | 0.09 |
| Case control | 5 | 95% | <0.00001 | 1.07 | [0.26, 1.89] | 0.01 | |
| LVEF | <50% | 2 | 0% | 0.61 | 0.07 | [-0.25, 0.39] | 0.67 |
| ≥50% | 8 | 92 | <0.00001 | 0.81 | [0.36, 1.26] | 0.0004 | |
| Sample size | <100 | 8 | 92% | <0.00001 | 1 | [0.24, 1.75] | 0.01 |
| ≥100 | 4 | 48% | 0.12 | 0.17 | [-0.02, 0.35] | 0.07 | |
| Age of patients | ≤50 years | 4 | 97% | <0.00001 | 1.75 | [0.09, 3.41] | 0.04 |
| >50 years | 8 | 57% | 0.02 | 0.25 | [0.01, 0.48] | 0.04 | |
AF = atrial fibrillation; LVEF = left ventricular ejection fraction; CI = confidence interval; SMD = standard mean difference.
Finally, we performed a sensitivity analysis and found that there was no significant difference on the overall heterogeneity regardless of which study was removed. The result of the funnel plot for TGF-β1 in AF patients was asymmetrical, indicating the potential for publication bias (Fig 5). After removing the study with the highest levels of TGF-β1, the result of the funnel plot was symmetrical (Fig 6).
Fig 5. Funnel plot of the meta-analysis.

Fig 6. Funnel plot after removing the study with the highest levels of TGF-β1.

Discussion
The main finding of this comprehensive meta-analysis is that there is an association between high plasma TGF-β1 levels and risk of AF, especially for new-onset AF. To the best of our knowledge, this is the first comprehensive meta-analysis performed to investigate their relationship.
TGF-β1 is a major factor promoting collagen production in cardiac fibroblasts [27]. It is also considered to be a key factor in the signal cascade reaction during the process of tissue fibrosis [28, 29]. Multiple studies have found increased atrial fibrosis on biopsy or autopsy specimens of patients with AF and concurrently elevated plasma level of TGF-β1 [30, 31, 32]. Previous studies have only investigated the plasma level of TGF-β1 in specific subgroups, such as the patients who developed recurrent AF (following surgical maze procedure, electrical cardioversion and catheter ablation) or patients with new-onset AF after cardiac surgery. In our meta-analysis, different groups were analyzed together to identify the potential role of TGF-β1 in promoting AF. We demonstrated that there is a positive correlation between higher plasma TGF-β1 levels and the development of new onset AF and the overall occurrence of AF. However, it is worth noting that there was no clear relationship between plasma TGF-β1 levels and recurrent AF in the subgroup analysis. This finding could be due to the heterogeneity in study population and AF management strategy between studies.
4 studies included information on the type of AF, whether they were persistent or paroxysmal AF. Persistent AF was defined as AF lasting for more than 7 days while paroxysmal AF was defined as AF with spontaneous termination in less than 7 days. To investigate the relationship between TGF-β1 and the type of AF, we analyzed these 4[14, 16–18] studies which included the plasma level of TGF-β1 in both persistent AF and paroxysmal AF patients. TGF-β1 levels were found to be higher in patients with persistent AF compared to paroxysmal AF. The finding was expected as atrial fibrosis is more extensive with longer duration of AF. It also leads us to the hypothesis that TGF-β1 as an index of atrial fibrosis may inform us of the chronicity of AF.
Despite being the most common sustained arrhythmia, the mechanism of AF is poorly understood. Systemic inflammatory response appear to be the contributing factor to the occurrence and recurrence of AF. A meta-analysis performed by Wu et al [33] demonstrated that high levels of circulating inflammatory factors especially CRP and IL-6 are associated with greater risk of AF in the general population, occurrence of AF after coronary artery bypass grafting and AF recurrence after electrical cardioversion or catheter ablation. In our analysis, we found that elevated levels of plasma TGF-β1 was associated with the occurrence of new onset AF. Our findings provide important insight into the mechanisms of AF.
Study Limitations
The present meta-analysis has several limitations. First, AF duration and methods of AF detection were different among the studies which account for the heterogeneity between the individual studies. Second, the sample size of the meta-analysis was relatively small. Finally, the asymmetrical funnel plot suggests that there may be publication bias.
Conclusions
In conclusion, this meta-analysis suggests an association between high plasma TGF-β1 and the occurrence of new onset AF. Additional studies with larger sample sizes are needed to further investigate the relationship between plasma TGF-β1 and the occurrence of AF.
Supporting Information
(DOC)
(DOC)
Acknowledgments
This work was supported by grants (81270245, 81570298 to T.L. and 81370300, to G.L.) from the National Natural Science Foundation of China and the Specialized Research Fund for the Doctoral Program of Higher Education (20121202110004 to G.L.).
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by grants (81270245, 81570298 to Tong Liu, and 81370300 to Guangping Li) from the National Natural Science Foundation of China and the Specialized Research Fund for the Doctoral Program of Higher Education (20121202110004 to Guangping Li). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Tan AY, Zimetbaum P. Atrial fibrillation and atrial fibrosis. J Cardiovasc Pharmacol 2011; 57:625–9. 10.1097/FJC.0b013e3182073c78 [DOI] [PubMed] [Google Scholar]
- 2.Kostin S, Klein G, Szalay Z, Hein S, Bauer EP, Schaper J. Structural correlate of atrial fibrillation in human patients. Cardiovasc Res 2002; 54:361–79. [DOI] [PubMed] [Google Scholar]
- 3.Beyerbach DM, Zipes DP. Mortality as an endpoint in atrial fibrillation. Heart Rhythm 2004; 1:B8–19. [DOI] [PubMed] [Google Scholar]
- 4.Abed HS, Samuel CS, Lau DH, Kelly DJ, Royce SG, Alasady M, et al. Obesity results in progressive atrial structural and electrical remodeling: implications for atrial fibrillation. Heart Rhythm 2013; 10:90–100. 10.1016/j.hrthm.2012.08.043 [DOI] [PubMed] [Google Scholar]
- 5.Everett TH, Olgin JE. Atrial fibrosis and the mechanisms of atrial fibrillation. Heart Rhythm 2007; 4:S24–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gramley F, Lorenzen J, Koellensperger E, Kettering K, Weiss C, Munzel T. Atrial fibrosis and atrial fibrillation: the role of the TGF-beta1 signaling pathway. Int J Cardiol 2010; 143:405–413. 10.1016/j.ijcard.2009.03.110 [DOI] [PubMed] [Google Scholar]
- 7.Redondo S, Navarro-Dorado J, Ramajo M, Medina U, Tejerina T. The complex regulation of TGF-beta in cardiovascular disease. Vasc Health Risk Manag 2012; 8:533–539. 10.2147/VHRM.S28041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan R, Sheppard R. Fibrosis in heart disease: understanding the role of transforming growth factor-β in cardiomyopathy, valvular disease and arrhythmia. Immunology 2006; 118:10–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verheule S, Sato T, Everett T, Engle SK, Otten D, Rubart-von der Lohe M, et al. Increased vulnerability to atrial fibrillation in transgenic mice with selective atrial fibrosis caused by overexpression of TGF-beta1. Circ Res 2004; 94:1458–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bunch TJ, Mahapatra S, Bruce GK, Johnson SB, Miller DV, Horne BD, et al. Impact of transforming growth factor-beta1 on atrioventricular node conduction modification by injected autologous fibroblasts in the canine heart. Circulation 2006; 113:2485–94. [DOI] [PubMed] [Google Scholar]
- 11.Levine M, Walter S, Lee H, Haines T, Holbrook A, Moyer V. Users' guides to the medical literature. IV. How to use an article about harm. Evidence-Based Medicine Working Group. JAMA 1994; 271:1615–1619. [DOI] [PubMed] [Google Scholar]
- 12.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 2001; 20:21–35. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin X, Wu N, Shi Y, Wang S, Tan K, Shen Y, et al. Association between transforming growth factor β1 and atrial fibrillation in essential hypertensive patients. Clin Exp Hypertens 2015; 37:82–87. 10.3109/10641963.2014.913600 [DOI] [PubMed] [Google Scholar]
- 15.Wu CH, Hu YF, Chou CY, Lin YJ, Chang SL, Lo LW, et al. Transforming growth factor-β1 level and outcome after catheter ablation for nonparoxysmal atrial fibrillation. Heart Rhythm 2013; 10:10–5. 10.1016/j.hrthm.2012.09.016 [DOI] [PubMed] [Google Scholar]
- 16.Xiao H, Lei H, Qin S, Ma K, Wang X. TGF-beta1 expression and atrial myocardium fibrosis increase in atrial fibrillation secondary to rheumatic heart disease. Clin Cardiol 2010; 33:149–156. 10.1002/clc.20713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao F, Zhang S, Chen Y, Gu W, Ni B, Shao Y, et al. Increased expression of NF-AT3 and NF-AT4 in the atria correlates with procollagen I carboxyl terminal peptide and TGF-β1 levels in serum of patients with atrial fibrillation. BMC Cardiovasc Disord 2014; 14:167 10.1186/1471-2261-14-167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mira YE, Muhuyati, Lu WH, He PY, Liu ZQ, Yang YC. TGF-β1 signal pathway in the regulation of inflammation in patients with atrial fibrillation. Asian Pac J Trop Med 2013; 6:999–1003. 10.1016/S1995-7645(13)60180-7 [DOI] [PubMed] [Google Scholar]
- 19.Canpolat U, Oto A, Hazirolan T, Sunman H, Yorgun H, Sahiner L, et al. A prospective DE-MRI study evaluating the role of TGF-β1 in left atrial fibrosis and implications for outcomes of cryoballoon-based catheter ablation: new insights into primary fibrotic atriocardiomyopathy. J Cardiovasc Electrophysiol 2015; 26:251–9. 10.1111/jce.12578 [DOI] [PubMed] [Google Scholar]
- 20.On YK, Jeon ES, Lee SY, Shin DH, Choi JO, Sung J, et al. Plasma transforming growth factor beta1 as a biochemical marker to predict the persistence of atrial fibrillation after the surgical maze procedure. J Thorac Cardiovasc Surg 2009; 137:1515–1520. 10.1016/j.jtcvs.2008.10.022 [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Hou X, Li Y. Association between transforming growth factor beta1 polymorphisms and atrial fibrillation in essential hypertensive subjects. J Biomed Sci 2010; 17:23 10.1186/1423-0127-17-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim SK, Pak HN, Park JH, Ko KJ, Lee JS, Choi JI, et al. Clinical and serological predictors for the recurrence of atrial fibrillation after electrical cardioversion. Europace 2009; 11:1632–1638. 10.1093/europace/eup321 [DOI] [PubMed] [Google Scholar]
- 23.Kimura T, Takatsuki S, Inagawa K, Katsumata Y, Nishiyama T, Nishiyama N, et al. Serum Inflammation Markers Predicting Successful Initial Catheter Ablation for Atrial Fibrillation. Heart Lung Circ 2014; 23:636–643. 10.1016/j.hlc.2014.02.003 [DOI] [PubMed] [Google Scholar]
- 24.Shim J, Joung B, Park JH, Uhm JS, Lee MH, Pak HN. Long duration of radiofrequency energy delivery is an independent predictor of clinical recurrence after catheter ablation of atrial fibrillation: Over 500 cases experience. Int J Cardiol 2013; 167:2667–2672. 10.1016/j.ijcard.2012.06.120 [DOI] [PubMed] [Google Scholar]
- 25.Smit MD, Maass AH, De Jong AM, Muller Kobold AC, Van Veldhuisen DJ, Van Gelder IC. Role of inflammation in early atrial fibrillation recurrence. Europace 2012; 14:810–817. 10.1093/europace/eur402 [DOI] [PubMed] [Google Scholar]
- 26.Rosenberg MA, Maziarz M, Tan AY, Glazer NL, Zieman SJ, Kizer JR, et al. Circulating fibrosis biomarkers and risk of atrial fibrillation: The Cardiovascular Health Study (CHS). Am Heart J 2014; 16:723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Biernacka A, Dobaczewski M, Frangogiannis NG. TGF-beta signaling in fibrosis. Growth Factors 2011; 29:196–202. 10.3109/08977194.2011.595714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim SK, Park JH, Kim JY, Choi JI, Joung B, Lee MH, et al. High plasma concentrations of transforming growth factor-β and tissue inhibitor of metalloproteinase-1: potential non-invasive predictors for electroanatomical remodeling of atrium in patients with non-valvular atrial fibrillation. Circ J 2011; 75:557–564. [DOI] [PubMed] [Google Scholar]
- 29.Arujuna A, Karim R, Caulfield D, Knowles B, Rhode K, Schaeffter T, et al. Acute pulmonary vein isolation is achieved by a combination of reversible and irreversible atrial injury after catheter ablation: evidence from magnetic resonance imaging. Circ Arrhythm Electrophysiol 2012; 5:691–700. 10.1161/CIRCEP.111.966523 [DOI] [PubMed] [Google Scholar]
- 30.Rahmutula D, Marcus GM, Wilson EE, Ding CH, Xiao Y, Paquet AC, et al. Molecular basis of selective atrial fibrosis due to overexpression of transforming growth factor-b1. Cardiovasc Res 2013; 99:769–779. 10.1093/cvr/cvt074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao F, Zhang S, Shao Y, Wu Y, Qin J, Chen Y, et al. Calreticulin overexpression correlates with integrin-α5 and transforming growth factor-β1 expression in the atria of patients with rheumatic valvular disease and atrial fibrillation. Int J Cardiol 2013; 168:2177–2185. 10.1016/j.ijcard.2013.01.239 [DOI] [PubMed] [Google Scholar]
- 32.Zhang YJ, Ma N, Su F, Liu H, Mei J. Increased TRPM6 expression in atrial fibrillation patients contribute to atrial fibrosis. Exp Mol Pathol 2015; 98:486–490. 10.1016/j.yexmp.2015.03.025 [DOI] [PubMed] [Google Scholar]
- 33.Wu N, Xu B, Xiang Y, Wu L, Zhang Y, Ma X, et al. Association of inflammatory factors with occurrence and recurrence of atrial fibrillation: a meta-analysis. Int J Cardiol 2013; 25; 169:62–72. 10.1016/j.ijcard.2013.08.078 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.