Abstract
Endometrial cancer (EC) is a complex disease involving multiple gene-gene and gene–environment interactions. TGF-β signaling plays pivotal roles in EC development. This study aimed to investigate whether the genetic polymorphisms of TGF-β signaling related genes TGFB1, TGFBR1, SNAI1 and TWIST1 contribute to EC susceptibility. Using the TaqMan Genotyping Assay, 19 tagging-SNPs of these four genes were genotyped in 516 EC cases and 707 controls among Chinese Han women. Logistic regression (LR) showed that the genetic variants of TGFB1 rs1800469, TGFBR1 rs6478974 and rs10733710, TWIST1 rs4721745 were associated with decreased EC risk, and these four loci showed a dose-dependent effect (Ptrend < 0.0001). Classification and regression tree (CART) demonstrated that women carrying both the genotypes of TGFBR1 rs6478974 TT and rs10512263 TC/CC had the highest risk of EC (aOR = 7.86, 95% CI = 3.42–18.07, P<0.0001). Multifactor dimensionality reduction (MDR) revealed that TGFB1 rs1800469 plus TGFBR1 rs6478974 was the best interactional model to detect EC risk. LR, CART and MDR all revealed that TGFBR1 rs6478974 was the most important protective locus for EC. In haplotype association study, TGFBR1 haplotype CACGA carrier showed the lowest EC risk among women with longer menarche-first full term pregnancy intervals (˃11 years) and BMI˂24 (aOR = 0.39, 95% CI = 0.17–0.90, P = 0.0275). These results suggest that polymorphisms in TGFB1, TGFBR1, SNAI1 and TWIST1 may modulate EC susceptibility, both separately and corporately.
Introduction
Endometrial cancer (EC) is one of the most common gynecological malignancies worldwide. According to the National Central Cancer Registry of China, the incidence of EC was about 18.5 per 100,000 urban women in 2011 [1]. Longer lifetime estrogen exposure such as early menarche, late menopause, nulliparity and postmenopausal estrogen use, is related with increased EC risk, which indicates that estrogen can drive endometrial carcinogenesis. Traditionally, there are three subtypes of EC distinguished by biological and clinical courses: hormonally driven Type I with endometrioid histology, Type II with non-endometrioid serous or clear cells, and familial aggregated EC [2]. The increasing EC prevalence in recent years highlights the importance for developing strategies for its risk estimation and prevention [1].
It’s well known that the genetic variants such as single nucleotide polymorphisms (SNPs) play important roles in cancer susceptibility. The contributions of genetic variations or mutations to cancer risk in a population depend on their frequency and penetrance [3]. Although the high-penetrant and low-frequent mutations such as TP53, PTEN confer high risk to rare familial aggregated EC [4, 5], the vast majority of EC are sporadic and involve polygenes, indicating that the common polymorphisms play predominant roles in carcinogenesis because of their high frequency [4].
Genome-wide association study (GWAS) still remains costly, so many association studies on SNPs with EC risk have been performed in the context of candidate genes, including genes regulating DNA damage repair, steroid and carcinogen metabolism, cell-cycle control and apoptosis [2]. The epithelial-to-mesenchymal transition (EMT), a crucial process in tumor progression, promotes tumor cell invasion from the primary foci to surrounding tissues. To date, many molecules have been validated to trigger epithelial dedifferentiation and EMT, such as those involved in TGF-β signaling as well as EMT-related transcriptional factors Snail and Twist [6, 7]. Canonical mediation of TGF-β1 (encoded by TGFB1) signaling is via TβRI (encoded by TGFBR1) and TβRII to form SMAD transcriptional complexes, thus leading to the rapid activation of the transcriptional factors Snail and Twist (encoded by SNAI1 and TWIST1) [8, 9].
Germline mutations in signaling components of TGF-β family have been described to result in malignancies along with other heritable disorders. Polymorphism association studies in genes of this signaling pathway have been mainly focused on the risk of breast cancer [10–12], ovarian cancer [13] or colorectal cancer [14]. Until now, there have been few studies to explore the association of germline variants in TGF-β related genes with EC among Chinese Han population. We hypothesized that common genetic polymorphisms of TGFB1, TGFBR1, SNAI1 and TWIST1 may influence EC susceptibility in Chinese Han women.
Materials and Methods
Ethics statement
This study was approved by the Peking University IRB (reference no. IRB00001052-11029). Written consents were obtained from all control samples. EC patient’s genomic DNAs were extracted from archived formalin-fixed paraffin-embedded normal fallopian tube tissues. Because the contact information of EC patients who were treated in the hospitals before 2011 was not clear, PKU IRB approved our application to waive informed consent for the archived EC samples collected before April 2011. This study only used this part of samples. All the data/samples were used anonymously.
Study population
A total of 516 cases with pathological diagnosed endometrial adenocarcinoma were recruited from Peking University Third Hospital, Beijing Cancer Hospital and Beijing Hospital between 1999 and 2011. Patients with history of cancer, metastasized cancer from other organs, and radiotherapy or chemotherapy history were excluded from our study. The epidemiological information including age, body mass index (BMI), age at menarche/menopause/primiparity, smoking history and family history of cancer in the first-degree relatives was collected. The eligible 707 controls were randomly selected from women who participated in a community-based screening program for non-infectious diseases conducted in Beijing between 2011 and 2012. The selection criteria included no history of cancer, Chinese Han ethnic background and frequency-matched to the cases by 5 year-age. All controls provided the same epidemiological information as that we collected from the cases. The characteristics of the 707 controls and the 516 cases are summarized in S1 Table. This study was approved by the Ethics Committee of Peking University Health Science Center.
SNPs selection
We selected tagging-SNPs (tSNPs) by using Haploview v.4.2 software program based upon Chinese Beijing population (CHB) data from HapMap Project phase I, II and III merged database (http://hapmap.ncbi.nlm.nih.gov/). All tSNPs with a minor allele frequency (MAF) ≥5% were identified and partitioned in bins according to the r2 linkage disequilibrium (LD) statistic (threshold ≥0.8). A maximally informative tSNP was then selected from each bin, and these tSNPs could capture all known common genetic variants within the entire gene [15]. For TGFB1, seven tSNPs spanning 5 kb to each flank were identified, these being rs1800469, rs2241716, rs4803455, rs747857, rs12983047, rs10417924 and rs12981053. For TGFBR1, the minimum set of five tSNPs, rs10988706, rs6478974, rs10512263, rs10733710 and rs334348, ranging from 5 kb upstream to 5 kb downstream, was chosen. For SNAI1, three tSNPs spanning 2kb to each flank were selected, these being rs6125849, rs4647959 and rs6020178. For TWIST1, four common tSNPs covering 2kb flanking sequence were identified, these being rs2285682, rs2285681, rs4721746 and rs4721745.
DNA isolation and genotyping assay
Genomic DNA for controls was isolated from peripheral blood leukocytes, whereas cases’ genomic DNA was extracted from formalin-fixed paraffin-embedded normal fallopian tube tissues. Genotyping was conducted with the ABI 7900HT® Real-Time PCR System (Applied Biosystems, Foster City, California) using TaqMan® Assay in compliance with the manufacturer’s instructions. Primers and probes (FAM- and VIC- labeled) were supplied by ABI incorporation and the PCR reaction system was the same as described previously [16]. Briefly, all assays were carried out in 384-well plates with negative and positive controls. Plates were sealed and heated at 95°C for 5min, then subjected to 45–50 cycles of 92°C for 15s and 60°C for 1min. Data from plates failing in more than 15% samples were excluded from the analysis. At least 1% of the samples were duplicated randomly in each SNP genotyping assay, and the concordance between duplicates was more than 99%.
Statistical analysis
Differences in the distribution of demographic characteristics and selected variables between controls and cases were calculated by two-sided Pearson’s χ2 test or Student’s t test, where appropriate. Hardy-Weinberg equilibrium (HWE) was evaluated in controls using goodness-of-fit χ2 test within each tSNPs. The D’ values of LD plots were produced using the Haploview program. The expectation–maximization (EM) algorithm was used to evaluate the most probable haplotype by maximum-likelihood estimation among current population. A two-sided χ2 test was employed to compare differences in the distribution of genotypes and alleles between cases and controls. Each genotype was assessed in terms of additive (co-dominant), dominant and recessive models of inheritance. Also, Cochran-Armitage trend test was performed to estimate the association between EC risk and allele dose in each tSNP (P trend). Odds ratios (OR) and 95% confidence intervals (CI) were assessed by using univariate and multivariate unconditional logistic regression (LR), with adjustment for BMI, age at menarche/primiparity, menopause status, number of childbearing and family history of cancer. Statistical significance was defined as P<0.05. A Bonferroni-corrected P value was carried out in individual tSNPs and haplotype/diplotype association analysis. The potential gene-environment interactions between TGFBR1 haplotype CACGA and clinical risk factors (estrogen exposure, family history of cancer and BMI) were assessed by LR in stratified population. All statistics were analyzed by SAS software (v.9.1; SAS Institute, Cary, NC).
Classification and regression tree (CART) analysis was performed for high-order gene-gene interactions using SPSS software (v.19.0; SPSS Inc., Chicago, IL, USA) to build a decision tree via recursive partitioning. The decision tree started with a root node which contained the total sample and split into two child nodes. The splitting process continued until the terminal nodes had no subsequent statistically significant splits or reached a pre-supposed minimum size, and then the terminal subgroups were further analyzed. The case rate was calculated for each terminal node and the association of subgroups with EC risk was evaluated by LR analysis, using the subgroup with the least percentage of cases as reference. The ORs and 95% CI were adjusted as mentioned above.
Multifactor dimensionality reduction (MDR) analysis was performed to identify high-order interaction models that were associated with EC risk using open-source MDR software (v.2.0 beta 8.4, http://www.epistasis.org) [17]. Statistical significance was determined using permutation testing in MDRpt (v.1.0 beta 2.0). MDR analysis collapsed multi-dimensional data into a single independent dimensional variable with two levels (high and low risk) using the ratio of the number of cases to the number of controls, and thereby reduced multiple dimensional data into one dimension and permitted detection of interactions in relatively small sample sizes. The new one-dimensional multi-locus genotype variable was evaluated for its ability to classify and examine disease status through cross-validation and permutation test. The best candidate interaction model was regarded as the one with maximal testing accuracy and cross-validation consistency (CVC). To better confirm and visualize the interaction models, we further built an entropy-based interaction dendrogram. This would enable the loci that strongly interact to each other to appear close together at the branches of the tree, and those with weak interaction to appear distant from one another. MDR 1,000-fold permutation results were regarded as statistically significant at P<0.05. The conjoint effect of the variables in the best model was assessed by LR analysis.
Results
Characteristics of study population
The characteristics of population were herein described in S1 Table. The controls and cases seemed to be adequately matched on age (P = 0.7528). The cases, as expected, had higher BMI (P<0.0001), earlier age of menarche (P<0.0001) and later age of menopause (P = 0.0002) compared with the controls. In addition, the percentage of nulliparous women in patients was significantly higher than that in controls (P<0.0001). EC patients were more likely to have family history of cancer in first-degree relatives (P = 0.0464). These variables with significant differences between cases and controls were used in multivariate LR models to further adjust for any possible confounding effect on the association of selected genetic variants with risk of EC.
LD degree between tSNPs
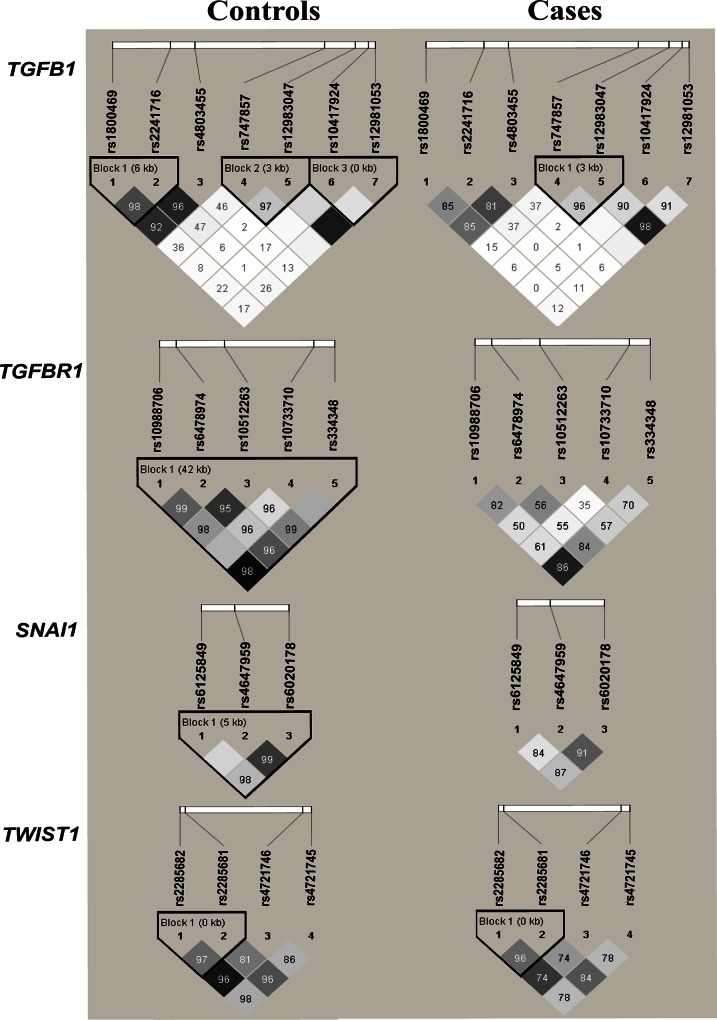
The genotype frequencies for selected 19 tSNPs were all consistently in agreement with those expected by HWE in controls (P˃0.05, S2 Table). For our study, haplotype blocks were reconstructed in cases and controls as well as in HapMap CHB population based on D’ value (Fig 1). There were some differences in SNPs’ pairwise LD between controls and cases. For TGFB1, three LD blocks were reconstructed in disease-free participants. For TGFBR1 as well as SNAI1, all selected tSNPs were reconstructed into one high-LD block in controls. For TWIST1, only one haplotype block was reconstructed, in which the rs4721746 and rs4721745 were excluded from the analysis because their MAFs were lower than 5%.
Fig 1. LD maps of the analyzed 19 tSNPs in controls and cases.
The value in each diamond indicates pairwise LD between tSNPs (measured as D’× 100, 10 means 0.10, 1 means 0.01). The shading with a dark grey-to-white gradient reflects higher to lower LD values.
Association of individual tSNPs in TGFB1, TGFBR1, SNAI1, TWIST1 with EC risk by LR analysis
As shown in Table 1, two-sided χ2 test indicated statistically differences of genotype frequencies between cases and controls in polymorphisms TGFB1 rs1800469 (C˃T), TGFBR1 rs6478974 (T˃A), TGFBR1 rs10512263 (T˃C), TGFBR1 rs10733710 (G˃A), TWIST1 rs4721746 (C˃A) and TWIST1 rs4721745 (C˃G) (P<0.0001, <0.0001, P = 0.0059, 0.0016, 0.0045 and 0.0430, respectively). Also, multivariate LR showed that TGFB1 rs1800469, TGFBR1 rs6478974 and rs10733710, and TWIST1 rs4721745 were protective loci for EC susceptibility under dominant or recessive models, whereas TWIST1 rs4721746 was a risk locus (Table 1). TGFBR1 rs6478974 remains significant under an additive and dominant models after applying the stringent Bonferroni correction (Bonferroni-corrected P<0.05). Other tSNPs did not show statistical significance in the multivariate analysis (S3 Table).
Table 1. Univariate and multivariate analysis of the association of candidate tSNPs with EC risk.
| Gene | SNPs | Genotype | Cases (%) | Controls (%) | Pa | Pb | Ptrend (Pd) | OR (95% CI) | P | aOR (95% CI)c | Pc (Pd) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| TGFB1 | rs1800469 | CC | 189 (36.63) | 170 (24.05) | <0.0001 | 0.0111(0.2109) | Reference | Reference | |||
| CT | 197 (38.18) | 372 (52.62) | 0.48 (0.36–0.62) | <0.0001 | 0.57 (0.41–0.80) | 0.0012 (0.0456)(0.0228) | |||||
| TT | 130 (25.19) | 165 (23.34) | 0.71 (0.52–0.97) | 0.0292 | 0.86 (0.59–1.27) | 0.4463 | |||||
| T allele frequency | 457 (44.28) | 702 (49.65) | 0.0087 | ||||||||
| CT/TT vs. CC (dominant model) | 0.55 (0.43–0.70) | <0.0001 | 0.66 (0.48–0.90) | 0.0093 (0.1767) | |||||||
| TT vs. CC/CT (recessive model) | 1.11 (0.85–1.44) | 0.4538 | 1.27 (0.92–1.75) | 0.1454 | |||||||
| TGFBR1 | rs6478974 | TT | 282 (54.65) | 286 (40.45) | <0.0001 | 0.0006(0.0114) | Reference | Reference | |||
| TA | 163 (31.59) | 326 (46.11) | 0.51 (0.40–0.65) | <0.0001 | 0.55 (0.40–0.75) | 0.0001 (0.0038) | |||||
| AA | 71 (13.76) | 95 (13.44) | 0.76 (0.54–1.07) | 0.1193 | 0.86 (0. 57–1.32) | 0.4903 | |||||
| A allele frequency | 305 (29.55) | 516 (36.49) | 0.0003 | ||||||||
| TA/AA vs. TT (dominant model) | 0.56 (0.45–0.71) | <0.0001 | 0.63 (0.47–0.83) | 0.0010 (0.0190) | |||||||
| AA vs. TT/TA (recessive model) | 1.03 (0.74–1.43) | 0.8706 | 1.13 (0.76–1.69) | 0.5467 | |||||||
| TGFBR1 | rs10512263 | TT | 298 (57.75) | 379 (53.61) | 0.0059 | 0.8535 | Reference | Reference | |||
| TC | 168 (32.56) | 284 (40.17) | 0.75 (0.59–0.96) | 0.0221 | 0.85 (0.63–1.14) | 0.2693 | |||||
| CC | 50 (9.69) | 44 (6.22) | 1.45 (0.94–2.23) | 0.0952 | 1.44 (0.86–2.42) | 0.1631 | |||||
| C allele frequency | 268 (25.97) | 372 (26.31) | 0.8504 | ||||||||
| TC/CC vs. TT (dominant model) | 0.85 (0.67–1.06) | 0.1500 | 0.93 (0.70–1.23) | 0.6240 | |||||||
| CC vs. TT/TC (recessive model) | 1.62 (1.06–2.47) | 0.0257 | 1.54 (0.93–2.55) | 0.0914 | |||||||
| TGFBR1 | rs10733710 | GG | 359 (69.57) | 471 (66.62) | 0.0016 | 0.8505 | Reference | Reference | |||
| GA | 121 (23.45) | 212 (29.99) | 0.75 (0.58–0.97) | 0.0306 | 0.59 (0.42–0.82) | 0.0018 (0.0684) | |||||
| AA | 36 (6.98) | 24 (3.39) | 1.97 (1.15–3.36) | 0.0130 | 1.48 (0.79–2.79) | 0.2206 | |||||
| A allele frequency | 193 (18.70) | 260 (18.39) | 0.8435 | ||||||||
| GA/AA vs. GG (dominant model) | 0.87 (0.68–1.11) | 0.2747 | 0.69 (0.51–0.94) | 0.0176 (0.3344) | |||||||
| AA vs. GG/GA (recessive model) | 2.13 (1.26–3.62) | 0.0050 | 1.78 (0.96–3.32) | 0.0694 | |||||||
| TWIST1 | rs4721746 | CC | 399 (77.33) | 512 (72.42) | 0.0045 | 0.3457 | Reference | Reference | |||
| CA | 92 (17.83) | 175 (24.75) | 0.68 (0.51–0.90) | 0.0067 | 0.70 (0.49–0.99) | 0.0432 (1.6416) | |||||
| AA | 25 (4.84) | 20 (2.83) | 1.60 (0.88–2.93) | 0.1242 | 2.11 (1.05–4.22) | 0.0354 (1.3452) | |||||
| A allele frequency | 142 (13.77) | 215 (15.21) | 0.3220 | ||||||||
| CA/AA vs. CC (dominant model) | 0.77 (0.59–1.00) | 0.0522 | 0.85 (0.61–1.17) | 0.3061 | |||||||
| AA vs. CC/CA (recessive model) | 1.75 (0.96–3.19) | 0.0675 | 2.29 (1.15–4.57) | 0.0188 (0.3572) | |||||||
| TWIST1 | rs4721745 | CC | 193 (37.40) | 216 (30.55) | 0.0430 | 0.0343(0.6517) | Reference | Reference | |||
| CG | 231 (44.77) | 352 (49.79) | 0.73 (0.57–0.95) | 0.0179 | 0.82 (0.60–1.13) | 0.2246 | |||||
| GG | 92 (17.83) | 139 (19.66) | 0.74 (0.53–1.03) | 0.0723 | 0.60 (0.40–0.92) | 0.0173 (0.6574) | |||||
| G allele frequency | 415 (40.25) | 630 (44.55) | 0.0337 | ||||||||
| CG/GG vs. CC (dominant model) | 0.74 (0.58–0.94) | 0.0123 | 0.76 (0.56–1.02) | 0.0642 | |||||||
| GG vs. CC/CG (recessive model) | 0.89 (0.66–1.19) | 0.4193 | 0.68 (0.46–0.98) | 0.0401 (0.7619) | |||||||
tSNPs, tagging single nucleotide polymorphisms; EC, endometrial cancer; OR, odds ratios; CI, confidence intervals.
a Two-sided χ2 test for difference in frequency distribution of genotypes between cases and controls.
b Two-sided χ2 test for difference in frequency distribution of alleles between cases and controls.
c Adjusted for BMI, age at menarche, age at primiparity, number of childbirth, menopause status and family history of cancer in first-degree relatives.
d Bonferroni-corrected P value for multiple testing.
Bold numbers denote a statistical significance at 0.05 level.
We further explored the combination effects between the aforementioned four protective polymorphisms by setting up two binary (1, 0) dummy variables. Firstly, we assessed the relative importance of the four protective tSNPs in their designated models. The adjusted OR value indicated that these four protective tSNPs affected EC susceptibility at a similar level (S4 Table). Then, individuals were categorized into five groups based on the number of protective genotypes they carried, and those without any protective genotypes were defined as the reference group. The analysis of combination effects indicated that the adjusted OR of EC for individuals carrying two protective genotypes was 0.41 (95% CI = 0.23–0.74, P = 0.0029). Co-existing three or four protective genotypes substantially decreased the susceptibility of EC in an almost similar degree (Table 2). Also, the protective genotypes took effect in a dose-dependent manner (Ptrend < 0.0001) (Table 2).
Table 2. Combination effects of rs1800469, rs6478974, rs10733710 in dominant model and rs4721745 in recessive model on EC susceptibility.
| Number of protective genotypesa | Cases (%) | Controls (%) | OR (95% CI) | P | aOR (95% CI) b | Pb |
|---|---|---|---|---|---|---|
| Combinations of rs1800469, rs6478974, rs10733710 and rs4721745 | ||||||
| 0 (Group 1) | 49 (9.50) | 32 (4.53) | Reference | Reference | ||
| 1 (Group 2) | 188 (36.43) | 186 (26.31) | 0.66 (0.41–1.08) | 0.0962 | 0.67 (0.36–1.22) | 0.1880 |
| 2 (Group 3) | 220 (42.64) | 336 (47.52) | 0.43 (0.27–0.69) | 0.0005 | 0.41 (0.23–0.74) | 0.0029 |
| 3 (Group 4) | 54 (10.47) | 137 (19.38) | 0.26 (0.15–0.44) | <0.0001 | 0.24 (0.13–0.48) | <0.0001 |
| 4 (Group 5) | 5 (0.97) | 16 (2.26) | 0.20 (0.07–0.61) | 0.0046 | 0.24 (0.07–0.84) | 0.0255 |
| Ptrend<0.0001 | ||||||
EC, endometrial cancer; OR, odds ratios; CI, confidence intervals.
a The genetic variants of rs1800469, rs6478974, rs10733710 and rs4721745 were considered as protective genotypes. Individuals in group 1 had no protective genotypes; in the next four groups, we pooled all individuals harboring any one protective genotype as group 2, harboring any two protective genotypes as group 3, harboring any three protective genotypes as group 4 and four protective genotypes as group 5.
b Adjusted for BMI, age at menarche, age at primiparity, number of childbirth, menopause status and family history of cancer in first-degree relatives.
Bold numbers denote a statistical significance at 0.05 level.
Association of high-order interactions among genetic variants with EC risk by CART analysis
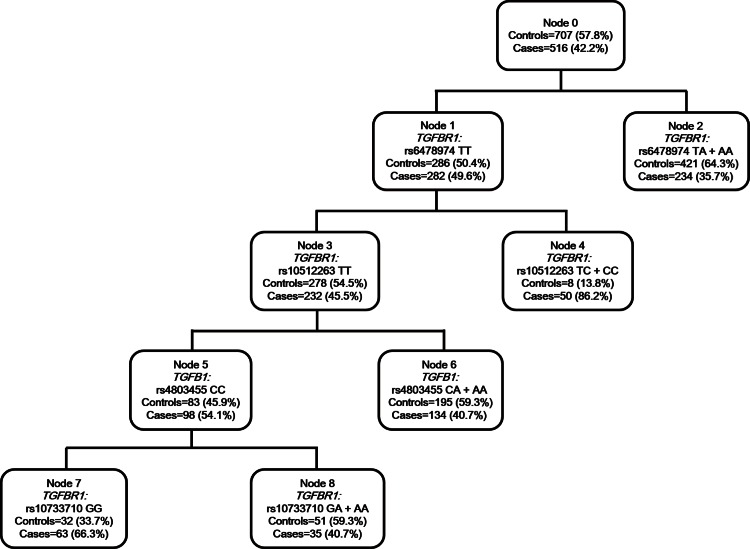
CART is a binary recursive partitioning method that produces a decision tree to identify subgroups of subjects at higher risk [18]. Fig 2 demonstrated the tree structure. The tree initiated from the total study population (node 0) and contained five terminal nodes in the final tree structure. TGFBR1 was singled out in the first splitting node, and TGFBR1 rs6478974 TA/AA genotype carriers had the least percentage of EC cases (35.7%), indicating that rs6478974 locus was the strongest susceptible factor for EC risk among the examined polymorphisms. Then the tree progressed along node 1 with the major allele homozygotes of SNP rs6478974. We designated node 2 as a reference node, because women in this node (with TGFBR1 rs6478974 TA/AA genotypes) had the lowest EC risk. This tree structure revealed that individuals harboring TGFBR1 rs6478974 TT, TGFBR1 rs10512263 TT, TGFB1 rs4803455 CC and TGFBR1 rs10733710 GG genotypes (node 7) had significantly higher risk calculated by multivariate LR analysis (aOR = 3.71, 95% CI = 2.14–6.43, P<0.0001), and women with both the genotypes of TGFBR1 rs6478974 TT and TGFBR1 rs10512263 TC/CC (node 4) imparted the highest predisposition to EC risk in our population (aOR = 7.86, 95% CI = 3.42–18.07, P<0.0001, Table 3).
Fig 2. CART analysis of genetic variants in modulating EC susceptibility.
Table 3. Conjoint analysis of the effects of individual tSNPs on EC risk by CART.
| Terminal nodes | Genotype of participants in each node | Cases (%) | Controls (%) | aOR (95% CI)a | Pa |
|---|---|---|---|---|---|
| 2 | TGFBR1 rs6478974 (TA+AA) | 234 (35.7) | 421 (64.3) | Reference | |
| 6 | TGFBR1 rs6478974 (TT) +TGFBR1 rs10512263 (TT) + | 134 (40.7) | 195 (59.3) | 1.13 (0.81–1.59) | 0.4683 |
| TGFB1 rs4803455 (CA+AA) | |||||
| 8 | TGFBR1 rs6478974 (TT) +TGFBR1 rs10512263 (TT) + | 35 (40.7) | 51 (59.3) | 1.07 (0.61–1.88) | 0.8172 |
| TGFB1 rs4803455 (CC) +TGFBR1 rs10733710 (GA+AA) | |||||
| 7 | TGFBR1 rs6478974 (TT) +TGFBR1 rs10512263 (TT) + | 63 (66.3) | 32 (33.7) | 3.71 (2.14–6.43) | <0.0001 |
| TGFB1 rs4803455 (CC) +TGFBR1 rs10733710 (GG) | |||||
| 4 | TGFBR1 rs6478974 (TT) +TGFBR1 rs10512263 (TC+CC) | 50 (86.2) | 8 (13.8) | 7.86 (3.42–18.07) | <0.0001 |
tSNPs, tagging single nucleotide polymorphisms; EC, endometrial cancer; CART, classification and regression tree; OR, odds ratios; CI, confidence intervals.
a Adjusted for BMI, age at menarche, age at primiparity, number of childbirth, menopause status and family history of cancer in first-degree relatives.
Bold numbers denote a statistical significance at 0.05 level.
Association of high-order interactions among genetic variants with EC risk by MDR analysis
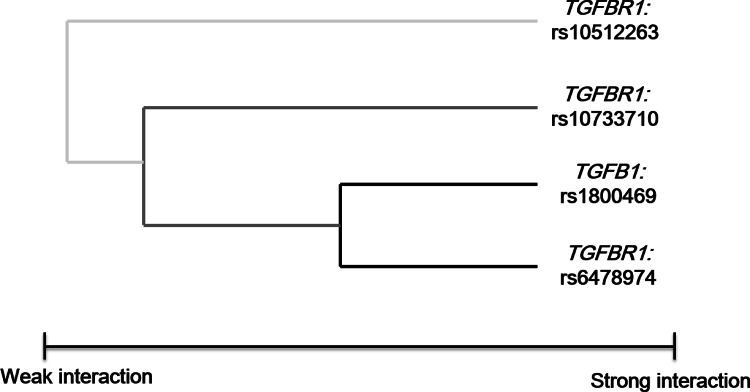
We applied the MDR method, a nonparametric and genetic model–free analysis, to identify interaction models. The best one-factor model generated by MDR for examining EC risk was TGFBR1 rs6478974 (testing accuracy 0.561, CVC 9/10, Table 4), which was consistent with the first splitting node by CART analysis. The two-factor model including both TGFB1 rs1800469 and TGFBR1 rs6478974 was the best interaction model, which yielded the maximal CVC of 10/10 and the highest testing accuracy of 0.589. The best three-factor model including TGFB1 rs1800469, TGFBR1 rs6478974 and TGFBR1 rs10733710 and the four-factor model consisting of TGFB1 rs1800469, TGFBR1 rs6478974, TGFBR1 rs10512263 and TGFBR1 rs10733710 had higher testing accuracy compared with the one-factor model (0.584, 0.575, respectively), but the CVCs were decreased (7/10, 6/10, respectively). All interaction permutation P value was less than 0.05. The interaction dendrogram showed that TGFB1 rs1800469 and TGFBR1 rs6478974 had the strongest synergistic interaction (black line), which also interacted with TGFBR1 rs10733710 (dark grey line). Furthermore, TGFBR1 rs10512263 had weak interaction with TGFBR1 rs10733710, TGFB1 rs1800469 and TGFBR1 rs6478974 (light grey line, Fig 3). For the combined effect of TGFB1 rs1800469 and TGFBR1 rs6478974 in the best interaction model identified above, LR analysis demonstrated that the adjusted OR of EC was 0.43 (95% CI = 0.27–0.69, P = 0.0003, data not shown). The summary of these three approaches for single-locus analysis was shown in S5 Table.
Table 4. Association of high-order gene-gene interactions with EC risk by MDR analysis.
| Number of loci | Best interaction models | Testing accuracy | Cross-validation consistency | P for permutation test |
|---|---|---|---|---|
| 1 | TGFBR1 rs6478974 T>A | 0.561 | 9/10 | <0.05 |
| 2 | TGFB1 rs1800469 C>T, | 0.589 | 10/10 | <0.05 |
| TGFBR1 rs6478974 T>A | ||||
| 3 | TGFB1 rs1800469 C>T, | 0.584 | 7/10 | <0.05 |
| TGFBR1 rs6478974 T>A, | ||||
| TGFBR1 rs10733710 G>A | ||||
| 4 | TGFB1 rs1800469 C>T, | 0.575 | 6/10 | <0.05 |
| TGFBR1 rs6478974 T>A, | ||||
| TGFBR1 rs10512263 T>C, | ||||
| TGFBR1 rs10733710 G>A |
EC, endometrial cancer; MDR, multifactor dimensionality reduction; CVC, cross-validation consistency.
Bold numbers denote a statistical significance at 0.05 level.
Fig 3. Interaction dendrogram for EC.
The loci that strongly interact to each other appear close together at the branches of the tree (black line), whereas the loci with weak interaction appear distant from one another (grey line).
Association of haplotypes and diplotypes in TGFB1, TGFBR1, SNAI1, TWIST1 with EC risk by LR analysis
To further explore the modest etiological effects of polymorphisms on EC susceptibility, haplotype was reconstructed as surrogate to provide higher resolution and potentially greater statistic power [16]. In our study, TGFB1 haplotypes (rs1800469 and rs2241716) with above 1% frequency were tested separately against the most common haplotypes, and the remaining rare haplotypes in the block (frequency < 1%) were not analyzed. The haplotype CG in block 1 was associated with increased EC risk relative to haplotype TG by univariate LR algorithm (OR = 1.60, 95% CI = 1.32–1.95, P˂0.0001, Table 5), and the diplotype CA-CG, carrying at-risk haplotype CG, increased about 62% of EC risk compared to the most common diplotype TG-CA (aOR = 1.62, 95% CI = 1.08–2.43, P = 0.0187). They did not remain significant after the Bonferroni correction. For TGFBR1, CACGA, harboring a protective locus rs6478974, could decrease about 42% of EC risk (aOR = 0.58, 95% CI = 0.43–0.77, P = 0.0003). Even after adjustment for Bonferroni-corrected multiple testing, the haplotype was still significantly associated with EC risk (Bonferroni-corrected P<0.05). Furthermore, the diplotype CACGA-CTTAA, containing a protective haplotype CACGA was also associated with decreased EC risk compared with the most common diplotype TTTGG-CACGA (aOR = 0.35, 95% CI = 0.18–0.66, P = 0.0012), with a Bonferroni corrected P<0.05 (Table 5). Haplotypes in SNAI1 and TWIST1 were not associated with EC susceptibility (S6 Table).
Table 5. Association of haplotypes and diplotypes of TGFB1 and TGFBR1 with EC risk.
| Cases (%) | Controls (%) | OR (95% CI) | P | aOR (95% CI)a | Pa (Pb) | |||
|---|---|---|---|---|---|---|---|---|
| Block1 of TGFB1 (rs1800469 + rs2241716)c | ||||||||
| Haplotype | TG | 441 (42.73) | 699 (49.43) | Reference | Reference | |||
| CA | 306 (29.65) | 457 (32.32) | 0.88 (0.74–1.05) | 0.1596 | 0.80 (0.61–1.06) | 0.1249 | ||
| CG | 269 (26.07) | 255 (18.03) | 1.60 (1.32–1.95) | <0.0001 | 1.06 (0.76–1.48) | 0.7347 | ||
| Diplotype | TG-CA | 119 (23.06) | 242 (34.23) | Reference | Reference | |||
| TG-TG | 118 (22.87) | 162 (22.91) | 1.00 (0.76–1.31) | 0.9851 | 1.15 (0.83–1.59) | 0.4131 | ||
| TG-CG | 78 (15.12) | 130 (18.39) | 0.79 (0.58–1.07) | 0.1332 | 0.84 (0.58–1.21) | 0.3440 | ||
| CA-CG | 85 (16.47) | 81 (11.46) | 1.52 (1.10–2.12) | 0.0118 | 1.62 (1.08–2.43) | 0.0187 (0.5236) | ||
| CA-CA | 51 (9.88) | 67 (9.48) | 1.05 (0.71–1.54) | 0.8113 | 0.83 (0.50–1.38) | 0.4815 | ||
| Block of TGFBR1 (rs10988706 + rs6478974 + rs10512263 + rs10733710 + rs334348)c | ||||||||
| Haplotype | TTTGG | 363 (35.17) | 573 (40.52) | Reference | Reference | |||
| CACGA | 174 (16.86) | 358 (25.32) | 0.60 (0.49–0.73) | <0.0001 | 0.58 (0.43–0.77) | 0.0003 (0.0045) | ||
| CTTAA | 147 (14.24) | 252 (17.82) | 0.77 (0.61–0.96) | 0.0179 | 0.70 (0.48–1.02) | 0.0661 | ||
| CATGA | 91 (8.82) | 144 (10.18) | 0.85 (0.65–1.12) | 0.2556 | 0.83 (0.54–1.27) | 0.3945 | ||
| CTTGG | 48 (4.65) | 53 (3.75) | 1.25 (0.84–1.87) | 0.2701 | 2.01 (0.93–4.32) | 0.0750 | ||
| Diplotype | TTTGG-CACGA | 61 (11.82) | 149 (21.07) | Reference | Reference | |||
| TTTGG-TTTGG | 77 (14.92) | 117 (16.55) | 0.88 (0.65–1.21) | 0.4422 | 0.82 (0.55–1.22) | 0.3336 | ||
| TTTGG-CTTAA | 59 (11.43) | 103 (14.57) | 0.76 (0.54–1.07) | 0.1111 | 0.51 (0.32–0.81) | 0.0045 (0.1260) | ||
| CACGA-CTTAA | 19 (3.68) | 70 (9.90) | 0.35 (0.21–0.59) | <0.0001 | 0.35 (0.18–0.66) | 0.0012 (0.0336) | ||
| TTTGG-CATGA | 29 (5.62) | 53 (7.50) | 0.74 (0.46–1.17) | 0.1966 | 0.78 (0.45–1.36) | 0.3839 | ||
| CACGA-CACGA | 25 (4.84) | 40 (5.66) | 0.85 (0.51–1.42) | 0.5319 | 0.83 (0.45–1.55) | 0.5655 | ||
| CACGA-CATGA | 24 (4.65) | 37 (5.23) | 0.88 (0.52–1.50) | 0.6443 | 1.11 (0.59–2.09) | 0.7550 | ||
| CTTAA-CTTAA | 14 (2.71) | 22 (3.11) | 0.87 (0.44–1.71) | 0.6840 | 1.07 (0.50–2.32) | 0.8550 | ||
EC, endometrial cancer; OR, odds ratios; CI, confidence intervals.
a Adjusted for BMI, age at menarche, age at primiparity, number of childbirth, menopause status and family history of cancer in first-degree relatives.
b Bonferroni-corrected P value for multiple testing.
c Haplotypes and diplotypes with frequency less than 1% were omitted.
Bold numbers denote a statistical significance at 0.05 level.
Association of interactions among genetic variants and environmental factors with EC risk
Given that long-term exposure to estrogen, cancer history in first-degree relatives and overweight are clinical EC risk factors [19], we conducted analysis in stratified population to explore whether the associations of genetic variants with EC risk were modified by these clinical risk factors. Table 6 showed that women harboring TGFBR1 protective haplotype CACGA had an even lower EC risk among those with longer menarche-FFTP intervals (˃11 years [20], aOR = 0.49, 95% CI = 0.31–0.75, P = 0.0012) and without family history of cancer (aOR = 0.49, 95% CI = 0.30–0.80, P = 0.0044). Also, CACGA carriers had a bit lower EC risk in BMI˂24 subgroup than in BMI≥24 subgroup (BMI˂24, aOR = 0.62, 95% CI = 0.40–0.96, P = 0.0323; BMI≥24, aOR = 0.70, 95% CI = 0.51–0.96, P = 0.0255). Moreover, carriers of this haplotype showed the lowest EC risk among women with longer menarche-FFTP intervals and BMI˂24 (aOR = 0.39, 95% CI = 0.17–0.90, P = 0.0275) (Table 6).
Table 6. Stratified analysis between protective haplotype CACGA of TGFBR1 and EC risk by family history of cancer, BMI status and menarche-FFTP intervals.
| All | Menarche-FFTP intervalsa ≤ 11 years | Menarche-FFTP intervalsa ˃ 11 years | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases (%)/Controls (%) | aOR (95% CI)b | Pb | Cases (%)/Controls (%) | aOR (95% CI)b | Pb | Cases (%)/Controls (%) | aOR (95% CI)b | Pb | |
| All | |||||||||
| Other haplotypes | 858 (83.14)/1056 (74.68) | Reference | 477 (81.12)/695 (75.87) | Reference | 381 (85.81)/361 (72.49) | Reference | |||
| CACGA | 174 (16.86)/358 (25.32) | 0.66 (0.51–0.84) | 0.0008 | 111 (18.88)/221 (24.13) | 0.79 (0.58–1.08) | 0.1330 | 63 (14.19)/137 (27.51) | 0.49 (0.31–0.75) | 0.0012 |
| Family history of cancer (yes) | |||||||||
| Other haplotypes | 131 (79.88)/216 (75.00) | Reference | 59 (73.75)/107 (75.35) | Reference | 72 (85.71)/109 (74.66) | Reference | |||
| CACGA | 33 (20.12)/72 (25.00) | 0.88 (0.49–1.56) | 0.6573 | 21 (26.25)/35 (24.65) | 1.28 (0.58–2.84) | 0.5373 | 12 (14.29)/37 (25.34) | 0.70 (0.25–1.98) | 0.5065 |
| Family history of cancer (no) | |||||||||
| Other haplotypes | 727 (83.76)/840 (74.60) | Reference | 418 (82.28)/588 (75.97) | Reference | 309 (85.83)/252 (71.59) | Reference | |||
| CACGA | 141 (16.24)/286 (25.40) | 0.61 (0.46–0.81) | 0.0005 | 90 (17.72)/186 (24.03) | 0.73 (0.52–1.02) | 0.0662 | 51 (14.17)/100 (28.41) | 0.49 (0.30–0.80) | 0.0044 |
| BMI ˂24 | |||||||||
| Other haplotypes | 286 (83.14)/409 (74.91) | Reference | 179 (81.36)/252 (77.78) | Reference | 107 (86.29)/157 (70.72) | Reference | |||
| CACGA | 58 (16.86)/137 (25.09) | 0.62 (0.40–0.96) | 0.0323 | 41 (18.64)/72 (22.22) | 0.75 (0.43–1.31) | 0.3075 | 17 (13.71)/65 (29.28) | 0.39 (0.17–0.90) | 0.0275 |
| BMI ≥24 | |||||||||
| Other haplotypes | 572 (83.14)/647 (74.54) | Reference | 298 (80.98)/443 (74.83) | Reference | 274 (85.63)/204 (73.91) | Reference | |||
| CACGA | 116 (16.86)/221 (25.46) | 0.70 (0.51–0.96) | 0.0255 | 70 (19.02)/149 (25.17) | 0.79 (0.54–1.15) | 0.2227 | 46 (14.38)/72 (26.09) | 0.54 (0.32–0.93) | 0.0269 |
EC, endometrial cancer; BMI, body mass index; FFTP, first full term pregnancy; OR, odds ratios; CI, confidence intervals.
a Both parous and nulliparous women were included. This parameter was measured by age at FFTP minus age at menarche in all parous women, age at menopause minus age at menarche in postmenopausal nulliparous women, and age at EC diagnosed (case) or age at interview (control) minus age at menarche in premenopausal nulliparous women.
b Adjusted for BMI, age at menarche, age at primiparity, number of childbirth, menopause status and family history of cancer in first-degree relatives.
Bold numbers denote a statistical significance at 0.05 level.
Discussion
In this study, we applied multiple strategies including LR, CART and MDR approaches to systematically evaluate the association of EC susceptibility with germline variants in TGF-β signaling related genes TGFB1, TGFBR1, SNAI1 and TWIST1 among Chinese Han women.
In single-locus analysis using multivariate LR, five polymorphisms, rs1800469 in TGFB1, rs6478974 and rs10733710 in TGFBR1, rs4721746 and rs4721745 in TWIST1 showed significant association with EC susceptibility. Although LR has been widely used in multivariate gene-gene or gene-environment interactions, it cannot fully characterize them because of the sparseness of data in high dimensions. Moreover, its statistic power would decrease and type II errors would increase in relatively small sample size [21]. So the non-parametric CART and MDR analysis were employed in high-order gene-gene interactions to examine particular combination effects of genetic variants. In this study, CART analysis indicated that the most important splitting variable was TGFBR1 rs6478974, followed by TGFBR1 rs10512263. The MDR method, which reduces the genotype parameters from multi- dimension to one dimension, demonstrated that TGFB1 rs1800469 and TGFBR1 rs6478974 together were the best interactional polymorphisms to examine EC risk.
All the three approaches in single-locus analysis consistently indicated that the genotype TGFBR1 rs6478974 TA/AA (located in intron 1) had the strongest protective effect on EC susceptibility. Until now, common variants were seldom reported in the exons or functional regions of TGFBR1 to have clear functional relevance. Although the vast majority of SNPs are located in the genomic non-coding regions, new evidence suggests that SNPs, located in gene promoter or regulatory regions, play critical roles in regulating the nature and timing of gene expression [22]. Chen J et al found that rs6478974 was associated with increased risk of gastric cancer in Chinese population (in dominant model: aOR = 1.36, 95% CI = 1.14–1.63; in additive model: aOR = 1.23, 95% CI = 1.08–1.40) [23]. They discovered that rs6478974 was in moderate LD with rs334348 and rs1590 (in the 3’-UTR, both r2 = 0.504) using online software SNPinfo (http://manticore.niehs.nih.gov/cgi-bin/snpinfo/snpfunc.cgi), and these two loci probably regulated miRNAs binding and influenced gastric cancer development. Because TβRI inhibits cell growth during early tumorigenesis [9, 24], we speculate that individuals carrying TGFBR1 rs6478974 TA/AA express higher levels of TβRI than TT genotype carriers, and therefore have lower susceptibility to EC. We also found that individuals with both the genotypes of TGFBR1 rs6478974 TT and TGFBR1 rs10512263 TC/CC had higher susceptibility compared with those harboring the genotype TGFBR1 rs6478974 TA/AA by CART analysis, which indicates that rs10512263 could be a risk locus. A two-stage case-control study of gastric cancer (the first stage of cases/controls = 650/683; the second stage of cases/controls = 484/348) showed that rs10512263 in dominant models (CT/CC vs. TT) was significantly associated with increased risk of gastric cancer in Chinese population [23], which is consistent with our results. But Scollen S et al discovered that the minor allele C of rs10512263 had a protective effect on breast cancer susceptibility (OR = 0.87, 95% CI = 0.81–0.95, P = 0.001) in meta-analysis of the SEARCH and PBCS studies [25]. The discrepancies among these results could be due to the ethnic diversity of populations and complicated environmental factors.
In TGFB1, we observed that the T allele of rs1800469 (C˃T at the 5’UTR region) was associated with decreased EC susceptibility under dominant model, which was consistent with the result in gastric cancer among the same ethnic population (cases/controls = 675/704, aOR = 0.65, 95% CI = 0.52–0.82) [26]. Our MDR analysis demonstrated that the combined genetic variants of TGFB1 rs1800469 and TGFBR1 rs6478974, the best interaction model, decreased the EC risk, which was in accordance with the results analyzed by LR. It was reported that the T allele of rs1800469 could enhance the affinity of its promoter with some transcriptional factors such as Yin Yang 1 (YY1), and increase the expression of TGF-β1 [27, 28]. Moreover, Grainger DJ et al showed that the concentration of TGF-β1 in plasma was extremely higher in T allele carriers than C allele carriers among UK population [29]. The polymorphism TGFB1 rs1800469 may perform its protective function during early tumorigenesis by altering the expression of TGF-β1.
In TWIST1, we discovered that the variant genotypes of rs4721746 and rs4721745, both locating in the 3’ flanking regions, had opposite effects on EC risk in our population. When using web-based functional annotation tool F-SNP (http://compbio.cs.queensu.ca/F-SNP/) [30], these two polymorphisms were both predicted to influence transcriptional regulation by TFSearch and Consite tools (functional significance scores = 0.239; 0.208, respectively). Further studies in other population are needed to verify our findings.
Haplotype-based approach may have greater power than single-locus analysis when SNPs are in strong LD and would provide additional statistical power to detect genes involved in complex trait diseases [31, 32]. In our haplotype-reconstruction association study, we found that TGFB1 haplotype CG and diplotype CA-CG were both associated with increased EC susceptibility. In TGFBR1, haplotype CACGA and diplotype CACGA-CTTAA decreased EC risk. Also, we observed significant joint effects of haplotype CACGA, family history of cancer, BMI status and estrogen exposure in stratified analysis. Haplotype CACGA, harboring a protective allele A of rs6478974, decreased the risk of EC regardless of what the environmental factors were, which further indicated that A allele of rs6478974 might be the most important protective locus in our population. If these haplotypes and diplotypes could be proved in other populations, they can be used as molecular makers for the estimation of EC risk, and can also provide some clues for finding causal SNPs.
There are three main strengths in our study. First, in single-locus analysis, we not only used traditional LR, but also CART and MDR approaches to identify high-order interactions while overcoming LR’s shortcomings, such as inaccurate parameter estimates and low power for detecting interactions. Second, we performed gene-wide analysis of tSNPs that covered all common SNPs of the four genes. Third, we reconstructed haplotype blocks according to our genotyping data in controls, which could guarantee the reasonable division of haplotype blocks. However, our study has several limitations. First, our sample size was relatively small, and the number of individuals was even smaller when the data were stratified. Second, the causal genetic variants hidden behind the association have not been revealed, and a further fine mapping study with high-density SNPs within the target region would be helpful in identifying the causal variants.
Supporting Information
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
This study was supported by the National Natural Science Foundation of China (No. 81171961 and No. 81321003) and the Open Project of Key Laboratory of Genomic and Precision Medicine, Chinese Academy of Sciences.
References
- 1.Zheng R, Zeng H, Zhang S, Chen T, Chen W. National estimates of cancer prevalence in China, 2011. Cancer letters. 2015. October 13 . [DOI] [PubMed] [Google Scholar]
- 2.Meyer LA, Westin SN, Lu KH, Milam MR. Genetic polymorphisms and endometrial cancer risk. Expert review of anticancer therapy. 2008. July;8(7):1159–67. 10.1586/14737140.8.7.1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirshfield KM, Rebbeck TR, Levine AJ. Germline mutations and polymorphisms in the origins of cancers in women. Journal of oncology. 2010;2010(2010):297671–82. . Pubmed Central PMCID: 2810468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cancer Genome Atlas Research N, Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013. May 2;497(7447):67–73. Pubmed Central PMCID: 3704730. 10.1038/nature12113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacey JVJ, Yang H, Gaudet MM, Dunning A, Lissowska J, Sherman ME, et al. Endometrial cancer and genetic variation in PTEN, PIK3CA, AKT1, MLH1, and MSH2 within a population-based case-control study. Gynecologic oncology. 2011. February;120(2):167–73. Pubmed Central PMCID: 3073848. 10.1016/j.ygyno.2010.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moreno-Bueno G, Portillo F, Cano A. Transcriptional regulation of cell polarity in EMT and cancer. Oncogene. 2008. November 24;27(55):6958–69. 10.1038/onc.2008.346 [DOI] [PubMed] [Google Scholar]
- 7.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011. March 4;144(5):646–74. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 8.Siegel PM, Massague J. Cytostatic and apoptotic actions of TGF-beta in homeostasis and cancer. Nature reviews Cancer. 2003. November;3(11):807–21. . [DOI] [PubMed] [Google Scholar]
- 9.Drabsch Y, ten Dijke P. TGF-beta signalling and its role in cancer progression and metastasis. Cancer metastasis reviews. 2012. December;31(3–4):553–68. 10.1007/s10555-012-9375-7 [DOI] [PubMed] [Google Scholar]
- 10.Liao RY, Mao C, Qiu LX, Ding H, Chen Q, Pan HF. TGFBR1*6A/9A polymorphism and cancer risk: a meta-analysis of 13,662 cases and 14,147 controls. Molecular biology reports. 2010. October;37(7):3227–32. 10.1007/s11033-009-9906-7 [DOI] [PubMed] [Google Scholar]
- 11.Dunning AM, Ellis PD, McBride S, Kirschenlohr HL, Healey CS, Kemp PR, et al. A transforming growth factorβ 1 signal peptide variant increases secretion in vitro and is associated with increased incidence of invasive breast cancer. Cancer research. 2003. May 15;63:2610–5. [PubMed] [Google Scholar]
- 12.Ma X, Beeghly-Fadiel A, Lu W, Shi J, Xiang YB, Cai Q, et al. Pathway analyses identify TGFBR2 as potential breast cancer susceptibility gene: results from a consortium study among Asians. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2012. July;21(7):1176–84. . Pubmed Central PMCID: 3810157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yin J, Lu K, Lin J, Wu L, Hildebrandt MAT, Chang DW, et al. Genetic variants in TGF-b pathway are associated with ovarian cancer risk. PloS one. 2011;6(9):e25559 10.1371/journal.pone.0025559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhong R, Liu L, Zou L, Sheng W, Zhu B, Xiang H, et al. Genetic variations in the TGFbeta signaling pathway, smoking and risk of colorectal cancer in a Chinese population. Carcinogenesis. 2013. April;34(4):936–42. 10.1093/carcin/bgs395 [DOI] [PubMed] [Google Scholar]
- 15.Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, et al. The structure of haplotype blocks in the human genome. Science. 2002. June 21;296(5576):2225–9. . [DOI] [PubMed] [Google Scholar]
- 16.Ruan Y, Song AP, Wang H, Xie YT, Han JY, Sajdik C, et al. Genetic polymorphisms in AURKA and BRCA1 are associated with breast cancer susceptibility in a Chinese Han population. The Journal of pathology. 2011. December;225(4):535–43. 10.1002/path.2902 [DOI] [PubMed] [Google Scholar]
- 17.Hahn LW, Ritchie MD, Moore JH. Multifactor dimensionality reduction software for detecting gene-gene and gene-environment interactions. Bioinformatics. 2003. February 12;19(3):376–82. . [DOI] [PubMed] [Google Scholar]
- 18.Muller R, Mockel M. Logistic regression and CART in the analysis of multimarker studies. Clinica chimica acta. 2008. August;394(1–2):1–6. . [DOI] [PubMed] [Google Scholar]
- 19.Amant F, Moerman P, Neven P, Timmerman D, Van Limbergen E, Vergote I. Endometrial cancer. The Lancet. 2005;366(9484):491–505. [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Xie YT, Han JY, Ruan Y, Song AP, Zheng LY, et al. Genetic polymorphisms in centrobin and Nek2 are associated with breast cancer susceptibility in a Chinese Han population. Breast cancer research and treatment. 2012. November;136(1):241–51. 10.1007/s10549-012-2244-9 [DOI] [PubMed] [Google Scholar]
- 21.Conklin JD. Applied Logistic Regression. Technometrics. 2002. February 44(1):81 . English. [Google Scholar]
- 22.Salzman DW, Weidhaas JB. SNPing cancer in the bud: microRNA and microRNA-target site polymorphisms as diagnostic and prognostic biomarkers in cancer. Pharmacology & therapeutics. 2013. January;137(1):55–63. . Pubmed Central PMCID: 3546232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen J, Miao L, Jin G, Ren C, Ke Q, Qian Y, et al. TGFBR1 tagging SNPs and gastric cancer susceptibility: a two-stage case-control study in Chinese population. Molecular carcinogenesis. 2014. February;53(2):109–16. 10.1002/mc.21954 [DOI] [PubMed] [Google Scholar]
- 24.Muinelo-Romay L, Colas E, Barbazan J, Alonso-Alconada L, Alonso-Nocelo M, Bouso M, et al. High-risk endometrial carcinoma profiling identifies TGF-beta1 as a key factor in the initiation of tumor invasion. Molecular cancer therapeutics. 2011. August;10(8):1357–66. 10.1158/1535-7163.MCT-10-1019 [DOI] [PubMed] [Google Scholar]
- 25.Scollen S, Luccarini C, Baynes C, Driver K, Humphreys MK, Garcia-Closas M, et al. TGF-beta signaling pathway and breast cancer susceptibility. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2011. June;20(6):1112–9. . Pubmed Central PMCID: 3112459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jin G, Wang L, Chen W, Hu Z, Zhou Y, Tan Y, et al. Variant alleles of TGFB1 and TGFBR2 are associated with a decreased risk of gastric cancer in a Chinese population. International journal of cancer Journal international du cancer. 2007. March 15;120(6):1330–5. . [DOI] [PubMed] [Google Scholar]
- 27.Silverman ES, Palmer LJ, Subramaniam V, Hallock A, Mathew S, Vallone J, et al. Transforming growth factor-beta1 promoter polymorphism C-509T is associated with asthma. American journal of respiratory and critical care medicine. 2004. January 15;169(2):214–9. . [DOI] [PubMed] [Google Scholar]
- 28.Zheng W, Yan C, Wang X, Luo Z, Chen F, Yang Y, et al. The TGFB1 functional polymorphism rs1800469 and susceptibility to atrial fibrillation in two Chinese Han populations. PloS one. 2013;8(12):e83033 Pubmed Central PMCID: 3861462. 10.1371/journal.pone.0083033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grainger DJ, Heathcote K, Chiano M, Snieder H, Kemp PR, Metcalfe JC, et al. Genetic control of the circulating concentration of transforming growth factor type beta1. Human molecular genetics. 1999. January;8(1):93–7. . [DOI] [PubMed] [Google Scholar]
- 30.Lee PH, Shatkay H. F-SNP: computationally predicted functional SNPs for disease association studies. Nucleic acids research. 2008. January;36(Database issue):820–4. . Pubmed Central PMCID: 2238878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Niu T, Qin ZS, Xu X, Liu JS. Bayesian haplotype inference for multiple linked single-nucleotide polymorphisms. American journal of human genetics. 2002. January;70(1):157–69. . Pubmed Central PMCID: 448439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hsieh AR, Hsiao CL, Chang SW, Wang HM, Fann CS. On the use of multifactor dimensionality reduction (MDR) and classification and regression tree (CART) to identify haplotype-haplotype interactions in genetic studies. Genomics. 2011. February;97(2):77–85. 10.1016/j.ygeno.2010.11.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.