Abstract
Elevated blood pressure in mid-life contributes significantly to the risk of cardiovascular disease. However, patterns of blood pressure increase may differ among individuals and may result in differential risk. Our goal was to examine the contribution of longitudinal patterns of blood pressure change to incidence of heart failure, coronary heart disease, stroke and cardiovascular disease mortality.
Latent class growth models were used to identify patterns of change in blood pressure across 4 clinical examinations (1987–1998) among 9,845 ARIC cohort participants (mean age: 53.7 (SD 5.7) years). Patterns of change in systolic blood pressure included slowly and steeply increasing, a decreasing and a sustained elevated blood pressure. Changes in diastolic and mid blood pressure (½ systolic + ½ diastolic) were less pronounced. The association of blood pressure pattern group membership with incidence of clinical outcomes was examined in follow-up from the fourth clinical examination (1996–1998) through Dec 31, 2011 using Poisson regression models adjusted for demographic and metabolic characteristics, and hypertension medication use. A gradient of rates of all events was observed across the identified patterns. Associations were attenuated after adjustment for covariates.
Cumulative systolic blood pressure load rather than the temporal pattern of change in systolic blood pressure itself, plays a role in determining the risk of cardiovascular disease, in particular of heart failure and cardiovascular disease mortality, independent of blood pressure level measured at one point in time.
Keywords: cardiovascular disease, coronary disease, heart failure, hypertension, stroke
Background
The association of elevated systolic and diastolic blood pressure (BP) with cardiovascular events is well documented. Even below hypertensive levels, a 20 mmHg increase in systolic BP nearly doubles the overall risk of stroke and coronary heart disease mortality.1, 2 Most longitudinal population-based studies examining the association of BP with cardiovascular outcomes rely on BP measured at one point in time and are not able to account for changes in BP occurring in midlife.1–3 Extant research shows that BP increases in midlife for most individuals; however, the pattern of change may differ. 4–7 Three parameters: baseline BP levels, directionality, and rate of change characterize temporal patterns of change in BP. So far, few studies have examined the association of attributes of change in BP with cardiovascular disease (CVD).4–7 It has been suggested that in young adults, cumulative BP exposure may determine cardiovascular risk later in life.4, 8 However, it remains unclear whether it is the cumulative BP load itself or the temporal pattern of that accumulation that determines the risk. Thus, the objective of this study was to apply the longitudinal approach to the examination of the association of BP with clinical outcomes. We aimed to describe patterns of change in blood pressure over a 9-year period in a large biracial cohort of middle-aged men and women, and evaluated the association of those patterns with the incidence of coronary heart disease (CHD), heart failure (HF), stroke, and CVD mortality occurring during an extended follow-up.
Methods
Study population
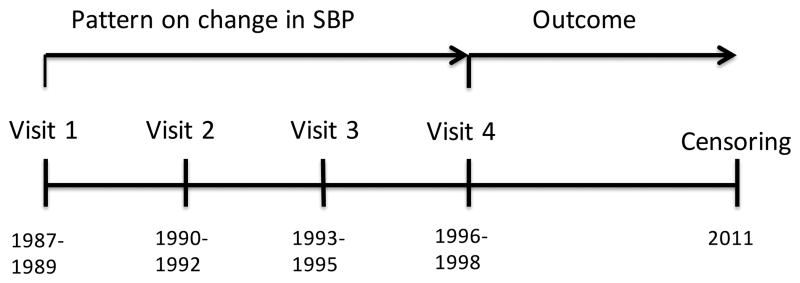
The Atherosclerosis Risk in Communities (ARIC) Study was initiated in 1987 as a prospective cohort of 15,792 men and women, age 45–64 years, selected through probability sampling from four U.S. communities: Washington County, Maryland; Forsyth County, North Carolina; suburbs of Minneapolis, Minnesota; and Jackson, Mississippi. Standardized examinations and interviewer-administered questionnaires were conducted at baseline and at four follow-up examinations. 9 Included in the analyses were ARIC cohort participants with blood pressure measurements at the first four triennial visits (n=11,656) (Figure 1). Excluded were those with prevalent CHD, HF and stroke at visit 4 (n=1233), those with missing data on covariates included in the models (n=541), as well as those self-identifying as of non-white or non-black race (n=30), or as black at the Washington County, and Minneapolis field centers (n=36). The final sample included 9,852 participants.
Figure 1.
Timeline of exposure and follow-up assessment.
Blood Pressure Measurement
Sitting systolic and diastolic BP was measured three times at visits 1–3 and twice at visit 4 using a random zero sphygmomanometer. The average of the second and third measurement (first and second at visit 4) was used in analyses. To account for use of antihypertensive medications, 10mm Hg was added to systolic and diastolic BP measurements. 10–12 Mid arterial BP, a combined measure of systolic and diastolic BP, was calculated as ½ systolic BP+ ½ diastolic BP. 13
Outcomes assessment
Outcomes of interest in this study, HF, stroke, CHD, and CVD mortality, were assessed as incident events during a median 13.2 years of follow-up from visit 4 through December 31, 2011.
Hospitalized cardiovascular events were identified through active surveillance of medical records in study area hospitals and through participants’ self-report of prior hospitalizations provided during the annual telephone follow-up interview. Incident CHD was defined as incident myocardial infarction (MI). MI events were adjudicated by a panel of trained clinicians and identified as definite or probable MI which did not result in a death within 28 days based on ICD-9 codes 410 and 411.0 and information obtained from ECG and laboratory findings available from participants’ medical records. Incident HF events were identified on the basis of the presence of ICD-9 code 428.xx in any position in the inpatient medical record. Incident stroke events were identified based on the presence of ICD-9 codes 430–438 as well as presence of neurological signs and symptoms and adjudicated by a panel of clinicians as ischemic or hemorrhagic stroke. Due to small numbers, we did not differentiate between stroke subtypes. Cardiovascular deaths were identified using ICD-9 codes (390–398, 401–404, 410–429, 430–434, 436–438, 440–448) for deaths occurring through the year 1999 and ICD-10 codes (I00–I78) thereafter.
Covariates
Covariates included in multivariable models were age; race; gender; ARIC Study field center; educational level (<=11 or >11 years of attained education), obtained via interviewer-administered questionnaire at the baseline examination; HDL and LDL cholesterol measured at visit 4; 14 cigarette smoking status, defined as never or ever smoker at any of the 4 clinic visits; obesity, defined as body mass index (BMI) >30 kg/m2 at any of the 4 clinic visits; and diabetes defined as self reported history of a physicians diagnosis, use of diabetes medication, fasting blood glucose level of at least 126 mg/dL, or a nonfasting glucose level of at least 200 mg/dL reported during any of the 4 clinic visits.
Statistical analysis
Descriptive statistics are presented as means (SD) and percentages. Normally distributed continuous values were compared using a t-test. The chi square statistic was used to evaluate categorical values.
We used latent class growth models to identify participants with similar underlying patterns of change in systolic, diastolic and mid arterial BP over a 9-year period (from ARIC visit 1 to visit 4). The models were fit using STATA 13.1 “traj” program (equivalent to PROC TRAJ in SAS).15–18 Based on the Bayesian Information Criterion (BIC), we selected the number and shape of the trajectories that best represented distinct patterns of change. 16 Model adequacy was assessed by comparing estimated with average posterior probabilities of group assignment, by estimating the odds of correct group classification, and examination of the 95% confidence intervals around the trajectories.16
We fit Poisson regression models to estimate the rates of all events in each identified pattern of systolic, diastolic and mid arterial BP change. Incidence rate ratios were calculated with pattern 1 (sustained low BP throughout) as referent. Beginning of follow-up was defined as date of visit 4. End of follow-up was defined as the date of an incident event, death, date of last known status or end of study period (December 31, 2011), whichever came first (Figure 1).
Finally, we performed several sensitivity analyses. To partially account for the exclusion of participants with prevalent events occurring during the exposure period, we shortened the period during which we observed change in BP and modeled BP patterns of change from baseline to ARIC visit 3 (6-year period) in association with cardiovascular outcomes occurring the follow-up through December 31, 2011. We also stratified BP patterns by visit 4 age group (<=64 years or >64 years), race, and sex. We also modeled patterns of BP change, unadjusted by medication use with hypertension medication use as a covariate in regression models.
Results
Descriptive characteristics
Among 9,852 ARIC cohort participants eligible for this study, at ARIC visit 4 the average age was 62.6 years (SD 5.6), 41.4% of the participants were male, 21.4% Black, and 17.4% had less than high school education (Table 1). The average BP at visit 1 was 118 mmHg (SD 16.8) for systolic, and 75 mmHg (SD 12.0) for diastolic BP. By visit 4 the average systolic BP increased to 127 mmHg (SD 18.8), diastolic BP decreased slightly to 74 mmHg (SD 11.7). Over the course of 9 years, from the baseline visit 1 to visit 4, 50.9% of participants reported being ever smokers, 50.4% had ever been diagnosed with hypertension and 18.2% with diabetes, while 39.0% had a BMI >30 kg/m2 during at least one of the four ARIC visits.
Table 1.
Descriptive characteristics of study participants at ARIC visit 4 by systolic BP pattern.
| Variable | Slowly increasing below 140mmHg | Above the 140mmHg throughout | ||||
|---|---|---|---|---|---|---|
| Pattern1 n=1902 | Pattern2 n=3492 | Pattern3 n=2951 | Pattern4 n=586 | Pattern5 n=706 | Pattern6 n=208 | |
| Age, yrs. (SD) | 60.7 (5.3) | 62.1 (5.5) | 63.4 (5.6) | 64.3 (5.6) | 65.1 (5.5) | 66.8 (4.9) |
| Gender, % male | 35.9 | 44.9 | 42.6 | 35.2 | 39.7 | 38.8 |
| Race % Black | 9.9 | 17.3 | 26.5 | 37.9 | 32.1 | 41.6 |
| Ever smokers, % | 54.0 | 52.6 | 49.6 | 50.3 | 43.5 | 42.1 |
| Education <11y, % | 9.9 | 16.0 | 19.2 | 26.3 | 26.0 | 21.4 |
| Obese, % ever | 19.8 | 37.0 | 47.6 | 47.6 | 54.0 | 50.2 |
| Hypertension, % ever | 1.9 | 24.5 | 86.9 | 100 | 100 | 100 |
| SBP, mmHg (SD) | 100 (8) | 113 (8) | 126 (11) | 135 (14) | 146 (13) | 165 (17) |
| DBP, mmHg (SD) | 64 (7) | 70 (8) | 75 (9) | 77 (10) | 81 (10) | 85 (12) |
| Diabetes, % ever | 6.6 | 14.3 | 24.3 | 26.6 | 31.4 | 35.4 |
| Hypert med use, % | 5.4 | 22.3 | 58.2 | 77.3 | 85.5 | 92.3 |
Abbreviations: V4, ARIC visit 4 clinical examination; SBP, systolic blood pressure; DBP, diastolic blood pressure. Obesity defined as body mass index (BMI)>30. Ever smokers include current and past smokers;
p for trend significant (<0.0001) for all covariates except gender.
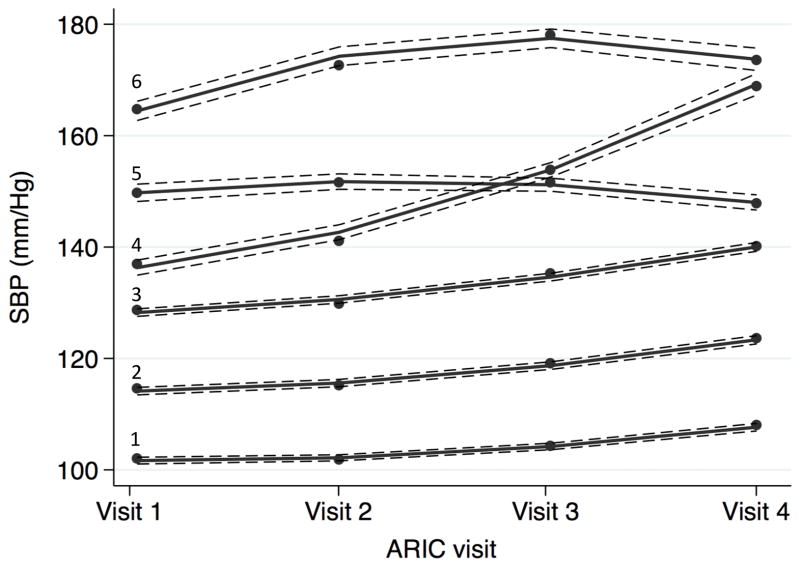
Patterns of change in systolic BP
We identified six distinct patterns of change in systolic BP over the 9-year period (Figure 2). Three patterns (patterns 1–3) were characterized by a slow sustained increase from different baseline systolic BP levels, with the means remaining below the 140 mmHg threshold throughout the exposure period. Majority of study participants (84.2%) fell into one of those three patterns. The average increase in systolic BP over the 9-year period for patterns 1, 2, and 3 was 5.9 mmHg, 9.1 mmHg, and 11.3 mmHg respectively. A steep increase in systolic BP from just under 140 mmHg to 170 mmHg (average 33.8 mm Hg) over the 9-year period (pattern 4) was observed for 6.0% of participants. Participants in the fifth group (pattern 5, 7.2% of study participants) experienced a slight decrease in systolic BP (average 4.0 mmHg), but their average systolic BP remained above the 140 mmHg threshold throughout. Only 2.1% of study participants were classified into the pattern with average systolic BP elevated at above 160 mmHg throughout the period from visit 1 to visit 4 (pattern 6). Participants in this group showed an average increase in BP of 9.4 mmHg over the 9-year period.
Figure 2. Patterns of change in systolic BP over the 9-year period among ARIC study participants.
Confidence intervals represented by dashed lines.
We observed a differential distribution of demographic and metabolic risk factors across the patterns of change in SBP. Those with high levels of systolic BP throughout (systolic BP patterns 4–6) were older than those with patterns of systolic BP consistently below 140 mmHg. Across the six distinct patterns of change in systolic BP (patterns 1 through 6) we observed gradients in the proportion of Blacks (from 9.9% to 41.6%), proportion of participants with BMI>30 kg/m2 at any of the 4 visits (from 19.8% to 50.2%) as well as proportion of those with diabetes (from 6.5% to 35.4%). Use of antihypertensive medications was the highest among participants with BP consistently above 140 mmHg (77.3%–92.3%).
In sensitivity analyses, we observed that the shape and number of patterns of systolic BP change did not differ by race or age group. The number of patterns differed slightly by gender, however the overall patterns of systolic BP change and the distribution of participants across those patterns were similar. We identified three distinct patterns of change in diastolic BP, which differed by baseline levels and suggested no significant change over the 9 years of observation (see appendix).
We observed less variability in mid arterial BP patterns change as compared to patterns of change in systolic BP patterns. We attributed this to the relatively minor change that was observed in diastolic BP over the 9-year period (supplemental Figures S1 and S2).
Incidence rates
Although estimates of the rates of CVD events across distinct patterns of change were examined for systolic, diastolic, and mid arterial BP, we focus on incidence of CVD across patterns of change in systolic BP. Systolic BP is more predictive than diastolic BP of future CVD events and in older age groups, such as that of the ARIC cohort, age-related changes in diastolic BP are less prominent than those observed for systolic BP. 2, 19, 20 Mid arterial BP, although associated with long-term outcomes,21 is not used in clinical settings and, as a composite measure of systolic and diastolic BP, it is less reflective of the underlying physiology.
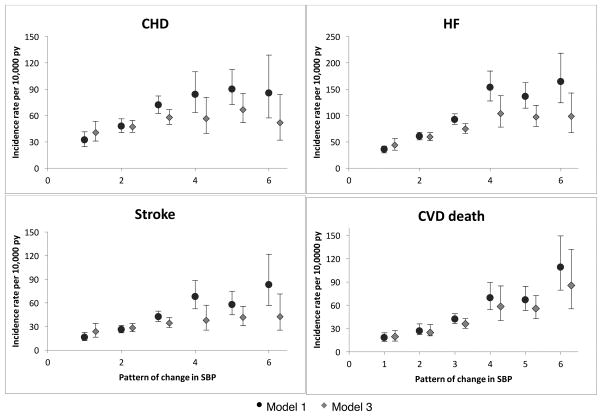
Sequential models estimating rates of CVD incidence across patterns of change in systolic BP were built from an initial model adjusting for baseline age (model 1), to a model that included additional demographic characteristics and comorbidities (model 2), and lastly to a model that also included systolic BP measured at visit 4 (model 3). In age-adjusted models (model 1) we observed steep gradients of the incidence of CHD, HF, stroke, and CVD mortality across systolic BP patterns 1–4 (Table 2, Figure 3). Those gradients were less pronounced in the models that accounted for demographic characteristics and comorbidities (model 2) and were further attenuated after accounting for systolic BP at visit 4 (model 3) for all outcomes, with the exception of CVD mortality. We found no significant difference in the incidence of CHD, HF, and stroke between patterns 4 through 6. The incidence rate for CVD mortality was highest among study participants in pattern 6 systolic BP, as compared to all other patterns.
Table 2.
Incidence rates and incidence rate ratios by pattern of change in systolic BP.
| Outcome | Incidence rates per 10,000 py | Outcome | Incidence rates per 10,000 py | ||||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | ||
| Stroke | CHD | ||||||
| Pattern1 | 16(12, 22) | 18 (13, 24) | 24 (17, 34) | Pattern1 | 32 (26, 40) | 34(27, 43) | 41 (31, 54) |
| Pattern2 | 26 (22, 31) | 26 (21, 31) | 28 (24, 34) | Pattern2 | 48 (42, 55) | 45 (39, 51) | 47 (41, 55) |
| Pattern3 | 43 (37, 50) | 39 (33, 45) | 34 (29, 41) | Pattern3 | 72 (64, 81) | 62 (55, 71) | 58 (50, 67) |
| Pattern4 | 68 (52, 88) | 62 (47, 80) | 38 (25, 57) | Pattern4 | 84 (66, 107) | 78 (61, 100) | 57 (40., 81) |
| Pattern5 | 58 (45, 75) | 51 (39, 66) | 42 (31, 56) | Pattern5 | 90 (73, 112) | 76 (61, 95) | 67 (53, 86) |
| Pattern6 | 83 (57, 122) | 72 (49, 106) | 43 (25, 71) | Pattern6 | 85 (58, 127) | 72 (48, 107) | 51 (32, 83) |
| HF | CVD death | ||||||
| Pattern1 | 36 (29, 45) | 39 (32, 49) | 44 (34, 56) | Pattern1 | 18 (14, 25) | 20 (15, 27) | 19 (14, 27) |
| Pattern2 | 61 (54, 68) | 51 (51, 65) | 59 (52, 68) | Pattern2 | 27 (23, 32) | 25 (21, 30) | 25 (21, 30) |
| Pattern3 | 93 (83, 103) | 78 (70, 87) | 75 (66, 85) | Pattern3 | 42 (36, 49) | 36 (31, 42) | 36 (31, 43) |
| Pattern4 | 154 (128, 185) | 127 (105, 154) | 104 (78, 138) | Pattern4 | 70 (54, 90) | 58 (45, 75) | 58 (40, 85) |
| Pattern5 | 136 (114, 162) | 107 (89, 128) | 97 (80, 119) | Pattern5 | 67 (53, 84) | 55 (43, 70) | 56 (43, 72) |
| Pattern6 | 165 (124, 218) | 129 (97, 172) | 99 (68, 143) | Pattern6 | 109 (80, 149) | 84 (60, 116) | 85 (55, 132) |
Model1: age at visit 4 adjusted;
Model 2: covariate adjusted includes age at visit 4, gender, race, study center, obesity, diabetes, smoking status, and hypertension medication use;
Model 3: full model adjusted for age at visit 4, gender, race, study center, obesity, diabetes, smoking status, hypertension medication use, and systolic BP at visit 4.
Figure 3. Incidence rates per 10,000 person-years by systolic BP pattern.
Model 1: adjustment for age at visit 4;
Model 3: adjustment for age at visit 4, gender, race, study center, obesity, diabetes, smoking status, hypertension medication use, and systolic BP at visit 4.
We examined selected contrasts of systolic BP patterns in order to separate the effect of temporal change in BP from the effect of the level of BP measured at one point in time on the risk of CVD outcomes. We first compared those who had similar systolic BP at visit 4 (mean systolic BP 141.7 mmHg (SD 11.8)), but who arrived at that BP either as a result of a gradual increase from the initial mean 129.1 mmHg (SD 10.7) (pattern 3) or through a decrease from the initial mean 151.1 mmHg (SD 12.4) systolic BP (pattern 5). We observed that age-adjusted rates of all events were higher in participants whose systolic BP was decreasing during the exposure period as compared to those with a gradual increase in systolic BP, although that difference was attenuated for CHD and stroke (and less so for HF and CVD death) after accounting for systolic BP at visit 4, demographic characteristics and comorbidities.
In the second contrast we compared those whose systolic BP increased steeply from pre-hypertensive levels to above 140 mmHg (pattern 4) with those whose systolic BP remained above 140 mmHg throughout the exposure period (pattern 6). For these two group with a mean visit 4 systolic BP of 170 mmHg, we observed no difference in rates for CHD, HF, and stroke. However, CVD mortality rates were lower among the group with shorter exposure to systolic BP levels of ≥140 mmHg (pattern 4).
To examine the effect of cumulative systolic BP exposure, we compared patterns with similar cumulative systolic BP load but with opposite direction of systolic BP change (patterns 4 and 5). We found that among the two groups the rates for all events were similar despite different temporal patterns and different systolic BP levels at baseline and at visit 4.
The trend in the age adjusted incidence rates of all events across patterns of mid arterial BP was similar to the trend observed across systolic BP patterns, however after adjusting for demographic characteristics and other risk factors the trend remained for HF and CHD although it was much attenuated (Table S2).
In a sensitivity analysis in which we modeled the patterns of change in systolic BP from baseline to ARIC visit 3 (a 6-year period), we identified 6 patterns that were very similar to the patterns identified in the main analysis. Associations with outcomes were similar to those observed for trajectories accumulated over a 9-year period (data not shown).
Incidence rate ratios
In age-adjusted models (model 1) we observed a gradient in incidence rate ratios (IRR) of CVD events across systolic BP patterns 2 through 4 relative to pattern 1. This gradient was less pronounced after adjustment for other covariates (model 2) and further attenuated after accounting for systolic BP at visit 4 (model 3). Participants for whom change in systolic BP followed patterns 4 through 6 experienced similar relative rates of CHD, HF, and stroke relative to pattern 1 in all models (Figure S3).
Discussion
In this study of middle-aged men and women we identified 6 patterns of change in systolic BP, 3 patterns of change in diastolic BP, and 5 patterns of change in mid arterial BP occurring over the course of 9 years. The majority of participants experienced a slow increase in systolic BP, however, this increase was not accompanied by similar changes in diastolic BP. Average diastolic BP remained stable or slightly decreased over time for most participants. Consequently, we observed low variability in mid arterial BP, which combined the systolic and diastolic BP measurements. These temporal changes were consistent with previous findings of Willis et al who observed a gentle underlying increase in midlife systolic BP for the majority of the study population.6, 7 Temporal systolic BP patterns of change were associated with different incident rates of HF, CHD, stroke, and CVD mortality in the age adjusted models, however those differences were attenuated after adjustment for demographic characteristics and comorbidities. Our findings suggest that it is the cumulative load of BP during midlife as opposed to the temporal pattern of that accumulation, that plays a role in determining the risk of cardiovascular events, in particular of HF and CVD mortality.
Demographic and metabolic characteristics varied significantly by pattern of change in systolic BP, and a strong gradient in those characteristics across the patterns of systolic BP was observed (Table 1). That gradient was reflected in rates of incidence of CVD events in age-adjusted models (model 1). However, after accounting for participants’ characteristics, the gradient was less pronounced. The associations were significant for parallel patterns of gradual increase in BP in the lower range of BP. This finding is in accordance with extant studies, which suggest that any increase in systolic BP independent of baseline is associated with increased CVD risk. 1, 2 Further, results of our study suggest that a reduction in systolic BP may not fully reverse the effect of sustained hypertension earlier in life which may be due to physiological changes in the vasculature, such as arterial stiffening, fibrosis, and calcification. 22
To this day, estimates of the association of patterns of change in systolic BP with outcomes are sparse. In a recent study of BP trajectories, Allen et al. identified 5 distinct patterns of change in mid BP among young adults over a 25-year period and found that individuals with elevated mid BP and those with increasing mid BP over time were at a greater risk of subclinical disease (measured by coronary artery calcification), concluding that the temporal change is predictive of risk independent of BP measured at one point in time. 4 In another study Wills et al. observed that among middle-aged adults a marked increase in systolic BP as compared to a gradual increase is associated with an increase in the risk of angina. 6, 7 Our study contributes to the existing literature by examining associations with clinical outcomes and comparing cumulative systolic BP load to the patterns of this accumulation (similar cumulative load but opposite direction of longitudinal change).
Strengths and limitations
The strengths of our study include a large community-based population and availability of four measurements over a 9-year period. All BP measurements were taken by trained staff according to standardized ARIC protocols and repeatability of measurements was high. In addition, information was available on many demographic and metabolic characteristics at all ARIC visits and through annual follow up. All events were identified over a long follow-up and were adjudicated by physicians and trained reviewers.
Despite these strengths, we note some limitations of our study that should be taken into consideration. For our estimates of change in BP we relied in on four measurements over a 9-year period which may not have captured more frequent fluctuations in BP. Hypertension medication use may not reflect adherence to medication. To account for medication use we added 10 mmHg to the existent measurements of BP, which may not accurately represent the actual response to medication by some individuals. Due to a high proportion of individuals reporting anti-hypertensive medication use, we could not stratify analyses by medication use status. In a sensitivity analysis we included hypertension medication use as an independent variable in our models. This did not change our results. BP patterns obtained through the statistical procedure “traj/proc traj” are dependent on the user-specified parameters of number and shape of trajectories during modeling. To address this limitation, we adhered to established criteria for model specification examining the BIC, average posterior probabilities of group assignment, and odds of correct classification (OCC). In our final model the average posterior probabilities ranged from 0.79–0.90 (expected to be >0.7) and OCC ranged from 5.6–434.5 (expected to be >5). It is also worth noting that grouping patterns of change in BP may have obscured some of the individual variability in temporal changes in BP and may have resulted in attenuated estimates. In our sensitivity analysis we addressed the issue of attrition by modeling patterns of change in systolic BP over a 6-year period (ARIC visit 1 through visit 3) and including in our analyses incident events happening between visit 3 and visit 4. A small number of group members and events with patterns of systolic BP consistently above the 140 mmHg level resulted in wide confidence intervals and we were unable to detect significant differences in estimates. Similarly, we were unable to conduct analyses stratified by race and gender due to the small number of events in each stratum-pattern group.
Perspectives
In this large population-based study of middle-aged adults, we observed that distinct patterns of change in systolic blood pressure over a period of 9 years differentially influenced the risk of CVD events. However, our results suggest that the cumulative systolic BP load rather than the temporal pattern of change in systolic BP itself plays a role in determining the risk of CVD, independent of BP level measured at one point in time. Our results support previous findings of observational studies, which suggest that any increase in systolic BP is detrimental to health. Our results are also in line with the most recent findings from the clinical trial on BP control,23 which suggest that intensive treatment of elevated BP to below the guideline recommended levels results in lower rates of fatal and non-fatal CVD. In addition, we observed that exposure to elevated systolic BP at any point in midlife results in higher rates of cardiovascular events even if systolic BP is lowered later in life.
Conclusions
Results of this study strongly underscore the importance of maintaining blood pressure below the guideline recommended levels throughout the life course.24, 25 Our results also support clinical efforts aimed at preventing any increase in systolic blood pressure, independent of its absolute value.
Supplementary Material
Novelty and significance.
What is new?
This study describes longitudinal patterns of change in BP over 9 years in a large biracial cohort of men and women and evaluates the association of those patterns with clinical outcomes.
Results of this study suggest that the cumulative load of BP, rather than the longitudinal change itself, determines the risk of CVD events.
What is relevant?
Our results support the findings from previous cohort studies and clinical trials, and implement a life course approach to studying the association of BP with clinical outcomes.
Summary
Results of this study underscore the importance of primary prevention of hypertension as well as the importance of maintaining a BP below the guideline recommended levels throughout the life course.
Acknowledgments
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C).
The authors thank the staff and participants of the ARIC study for their important contributions.
Sources of funding: National Institutes of Health/National Heart, Lung, and Blood Institute.
Footnotes
We have no disclosures.
References
- 1.van den Hoogen PC, Feskens EJ, Nagelkerke NJ, Menotti A, Nissinen A, Kromhout D. The relation between blood pressure and mortality due to coronary heart disease among men in different parts of the world. Seven countries study research group. N Engl J Med. 2000;342:1–8. doi: 10.1056/NEJM200001063420101. [DOI] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 3.Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, Peto R. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol. 1999;150:341–353. doi: 10.1093/oxfordjournals.aje.a010013. [DOI] [PubMed] [Google Scholar]
- 4.Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, Jacobs DR, Jr, Liu K, Lloyd-Jones D. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA. 2014;311:490–497. doi: 10.1001/jama.2013.285122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tielemans SM, Geleijnse JM, Menotti A, Boshuizen HC, Soedamah-Muthu SS, Jacobs DR, Jr, Blackburn H, Kromhout D. Ten-year blood pressure trajectories, cardiovascular mortality, and life years lost in 2 extinction cohorts: The minnesota business and professional men study and the zutphen study. J Am Heart Assoc. 2015;4:e001378. doi: 10.1161/JAHA.114.001378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wills AK, Lawlor DA, Matthews FE, Sayer AA, Bakra E, Ben-Shlomo Y, Benzeval M, Brunner E, Cooper R, Kivimaki M, Kuh D, Muniz-Terrera G, Hardy R. Life course trajectories of systolic blood pressure using longitudinal data from eight uk cohorts. PLoS Med. 2011;8:e1000440. doi: 10.1371/journal.pmed.1000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wills AK, Lawlor DA, Muniz-Terrera G, Matthews F, Cooper R, Ghosh AK, Kuh D, Hardy R. Population heterogeneity in trajectories of midlife blood pressure. Epidemiology. 2012;23:203–211. doi: 10.1097/EDE.0b013e3182456567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warnick GR, Benderson J, Albers JJ. Dextran sulfate-mg2+ precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–1388. [PubMed] [Google Scholar]
- 9.The atherosclerosis risk in communities (aric) study: Design and objectives. The aric investigators. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 10.Tobin MD, Sheehan NA, Scurrah KJ, Burton PR. Adjusting for treatment effects in studies of quantitative traits: Antihypertensive therapy and systolic blood pressure. Stat Med. 2005;24:2911–2935. doi: 10.1002/sim.2165. [DOI] [PubMed] [Google Scholar]
- 11.Wu J, Kraja AT, Oberman A, Lewis CE, Ellison RC, Arnett DK, Heiss G, Lalouel JM, Turner ST, Hunt SC, Province MA, Rao DC. A summary of the effects of antihypertensive medications on measured blood pressure. Am J Hypertens. 2005;18:935–942. doi: 10.1016/j.amjhyper.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 12.Rana BK, Dhamija A, Panizzon MS, Spoon KM, Vasilopoulos T, Franz CE, Grant MD, Jacobson KC, Kim K, Lyons MJ, McCaffery JM, Stein PK, Xian H, O’Connor DT, Kremen WS. Imputing observed blood pressure for antihypertensive treatment: Impact on population and genetic analyses. Am J Hypertens. 2014;27:828–837. doi: 10.1093/ajh/hpt271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenman RH, Sholtz RI, Brand RJ. A study of comparative blood pressure measures in predicting risk of coronary heart disease. Circulation. 1976;54:51–58. doi: 10.1161/01.cir.54.1.51. [DOI] [PubMed] [Google Scholar]
- 14.Warnick GR, Mayfield C, Benderson J, Chen JS, Albers JJ. Hdl cholesterol quantitation by phosphotungstate-mg2+ and by dextran sulfate-mn2+-polyethylene glycol precipitation, both with enzymic cholesterol assay compared with the lipid research method. Am J Clin Pathol. 1982;78:718–723. doi: 10.1093/ajcp/78.5.718. [DOI] [PubMed] [Google Scholar]
- 15.Nagin DS, Odgers CL. Group-based trajectory modeling (nearly) two decades later. J Quant Criminol. 2010;26:445–453. doi: 10.1007/s10940-010-9113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 17.Jones BL, Nagin DS. A note on a stata plugin for estimating group-based trajectory models. Sociological Methods and Reasearch. 2013 [Google Scholar]
- 18.Jones BL, Nagin DS, Roeder K. A sas procedure based on mixture models for estimating developmental trajectories. Sociological Methods and Reasearch. 2001;29:374. [Google Scholar]
- 19.Mosley WJ, 2nd, Greenland P, Garside DB, Lloyd-Jones DM. Predictive utility of pulse pressure and other blood pressure measures for cardiovascular outcomes. Hypertension. 2007;49:1256–1264. doi: 10.1161/HYPERTENSIONAHA.106.083592. [DOI] [PubMed] [Google Scholar]
- 20.Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, Levy D. Does the relation of blood pressure to coronary heart disease risk change with aging? The framingham heart study. Circulation. 2001;103:1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 21.Carlsson AC, Johansson SE, Theobald H, Wandell PE. Blood pressure measures and their predictive ability of cardiovascular mortality: A 26-year follow-up. Blood Press Monit. 2013;18:72–77. doi: 10.1097/MBP.0b013e32835ea233. [DOI] [PubMed] [Google Scholar]
- 22.Harvey A, Montezano AC, Touyz RM. Vascular biology of ageing-implications in hypertension. J Mol Cell Cardiol. 2015;83:112–121. doi: 10.1016/j.yjmcc.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chomistek AK, Chiuve SE, Eliassen AH, Mukamal KJ, Willett WC, Rimm EB. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol. 2015;65:43–51. doi: 10.1016/j.jacc.2014.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gillman MW. Primordial prevention of cardiovascular disease. Circulation. 2015;131:599–601. doi: 10.1161/CIRCULATIONAHA.115.014849. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.