Abstract
Background
American Indian children have high rates of emergency department (ED) use and face potential discrimination in health care settings.
Objective
Our goal was to assess both implicit and explicit racial bias and examine their relationship with clinical care.
Research Design
We performed a cross-sectional survey of care providers at five hospitals in the Upper Midwest. Questions included American Indian stereotypes (explicit attitudes), clinical vignettes and the Implicit Association Test (IAT). Two IATs were created to assess implicit bias toward the child or the parent/caregiver. Differences were assessed using linear and logistic regression models with a random effect for study site.
Results
A total of 154 care providers completed the survey. Agreement with negative American Indian stereotypes was 22–32%. Overall, 84% of providers had an implicit preference for non-Hispanic white adults or children. Older providers (≥ 50 years) had lower implicit bias than those middle aged (30–49 years), (p = 0.01). American Indian children were seen as increasingly challenging (p = 0.04) and parents/caregivers less compliant (p = 0.002) as the proportion of American Indian children seen in the ED increased. Responses to the vignettes were not related to implicit or explicit bias.
Conclusions
The majority of ED care providers had an implicit preference for non-Hispanic white children or adults compared to those who were American Indian. Provider agreement with negative American Indian stereotypes differed by practice and respondents’ characteristics. These findings require additional study to determine how these implicit and explicit biases influence healthcare or outcomes disparities.
Keywords: American Indian Health, Bias, Emergency Medicine, Pediatrics
Introduction
Care for children in the emergency department (ED) should be high quality and free from differential treatment based on race and ethnicity. However, given the unique, time-stressed environment of EDs, providers may have increased reliance on classification and cognitive short-cuts leading to greater use of stereotypes.1–3 In addition, given their “safety-net” role, EDs are often used for non-urgent reasons.4–6 Utilization by parents for concerns that are perceived as non-urgent may reduce empathy toward disadvantaged groups.7–10 This environment could play a role in increasing bias against racial and ethnic minority children and their caregivers through subtle, non-verbal cues, bias in triage assignment and differences in clinical care provided throughout the visit.11
Many factors affect health care use and access by American Indian children, including low insurance rates, lack of access to quality primary care and higher prevalence of diabetes, asthma, mental health issues, and injuries.12–16 American Indian children often rely on the ED to access necessary medical care instead of a medical home.13, 14, 17 Additionally, many American Indian parents perceive that they are discriminated against when they seek care at the ED or elsewhere. In one study, American Indian parents were 25 times more likely to perceive racial discrimination in health care for their child compared to non-Hispanic white parents and often felt that providers did not understand their culture or respect their religious beliefs.18 Other research suggests differences in ED treatment and outcomes for American Indian children, but no studies have fully explained the reasons for these differences.19, 20
The theoretical framework for this study is based in intergroup relations and bias. Intergroup bias is usually seen as a mild form of in-group favoritism sometimes including out-group derogation.21 This type of bias can either be explicit (e.g. stereotypes, blatant prejudice) or implicit (e.g. unintentional or unconscious bias).21 Major, et. al. suggest that both implicit and explicit bias influence the quality of health care interactions and can contribute to health disparities.22 Previous studies have found high levels of implicit bias with a preference for non-Hispanic whites in physicians and medical students, but low levels of explicit bias.23–31 Although differences in clinical care and decision making could arise based solely on implicit attitudes,23, 24, 27, 29 not all studies have consistently found this association.25, 26, 31, 32 This inconsistency could be based on population differences, clinical measurements, or type of provider studied. Even without differences in treatments or outcomes, implicit or explicit bias may degrade the patient’s or family’s perception of clinical care during ED encounters.
This study explored implicit and explicit bias against American Indian children and their parents/caregivers. Tests were created to determine if implicit bias was associated with the child or the parent/caregiver accompanying the child to the ED. We hypothesized that 1) we would observe high levels of implicit preference for non-Hispanic white adults and low levels of explicit bias against American Indian children and parents/caregivers, 2) levels of implicit bias against American Indian adults would be higher than levels of implicit bias against American Indian children, 3) levels of implicit and explicit bias would be lower for nurses and among those with greater familiarity with American Indian children, and 4) that implicit and explicit bias would be related to the child’s race and responses on clinical vignettes including increased agreement with biased treatment options for non-Hispanic white children.
Methods
Study Sites
Five EDs were included in this study. Two were in large cities (population ≥ 250,000), one was in a mid-sized city (population ≥ 150,000), and two were in rural towns (population <20,000). Urban sites primarily served American Indians living in those cities while rural sites primarily served American Indians living on nearby reservations. The American Indian population ranged from 2.6%–3.5% for urban sites and from 16.3%–19.0% for rural sites.33 The percent of pediatric ED visits by American Indian children ranged from 33.1%–68.0% at rural sites and 2.3%–8.7% at urban sites based on data for visits between June 2011 and May 2012.
Differences by study site were assessed by hospital characteristics including rural/urban location and the % of AI children seen on a typical shift at the ED.
Survey Development
We developed and administered a survey to a cross-sectional sample of physicians, nurses and advanced practice provider at five EDs in the Upper Midwest. The study was approved by the relevant institutional review boards for each ED. Providers were recruited via email and posters. Each potential participant received one initial email and three weekly follow-up emails. Survey responses were anonymous with no individual identifiers collected.
The survey included demographic and practice information, explicit bias questions, case vignettes and implicit bias measures in that order. The survey was piloted at a site that did not participate in the final survey.
Implicit Bias Measures
The Implicit Association Test (IAT) is an established measure of implicit bias with good internal consistency and test-retest reliability.34 Predictive validity of the IAT was found to be good in a meta-analysis of 103 studies with the IAT predicting prejudicial bias and stereotyping behaviors more accurately than self-report.34 The IAT measures implicit bias through response time in categorizing pictures of those of various races with value concepts (e.g. good/bad). Scoring depends on differences in response times, not the choice of a positive or negative value concept.35 For example, a faster response grouping American Indian pictures with positive values compared to grouping non-Hispanic whites with such values would suggest a preference for American Indian individuals.
We created new versions of the race IAT36 using pictures of adults and children from American Indians from the Northern Plains and from non-Hispanic whites through a partnership with Project Implicit (a non-profit organization created by the original developers of the IAT, Boston, MA). Pictures were taken of American Indian and non-Hispanic white adults and children living in the study area. For children’s pictures, photos were age, gender, lighting, and background-matched. Children were between 4 and 8 years old. Adult photos included those aged 30–45 years and were similarly matched between American Indian and non-Hispanic white subjects. Parents and adults signed a picture release form for use of the photos for the research project. To ensure validity, staff at Project Implicit guided the development and assessed all pictures for consistency between groups. We piloted the two IATs at a separate ED. Based on this testing; survey participants were randomly assigned to either the adult or child IAT to shorten the length of the test. Pictures were used in conjunction with words categorized as “good” (joy, love, wonderful, pleasant, laughter, happy) and “bad” (terrible, nasty, evil, awful, agony, hurt), (see figures S1 and S2, supplemental digital content 1, which provide the IAT introduction screens).36
Continuous IAT scores range from −2 to 2. These scores are standardized and controlled for respondents’ average response speed.35 Scores near zero (between −0.15 and 0.15) indicate no preference. Increasingly negative or positive scores indicate increasing strength of preference. For our IATs, negative values indicated a preference for American Indian individuals and positive values indicated a preference for non-Hispanic white individuals. Values between 0.16 and 0.35 or −0.16 and −0.35 suggest slight preference, between 0.36 and 0.65 or −0.36 and −0.65 suggest moderate preference and values greater than 0.65 or lower than −0.65 suggest a strong preference.35
Explicit Bias Measures
Three statements were used to identify explicit bias by rating the respondents’ agreement with common stereotypes of American Indian children and their caregivers. The three statements were: 1. Treating American Indian children often is more challenging than treating white children in the ED; 2. American Indian children seem to present at the ED with less urgent complaints than white children; 3. The parents/caregivers of American Indian children often are less compliant than parents/caregivers of white children. A five-point Likert scale was used to measure agreement from strongly agree, agree, neither agree nor disagree, disagree, and strongly disagree.
Case Vignettes
Four clinical vignettes were developed; modeled after the vignettes used in Sabin et. al.32 We focused on two areas in pediatric emergency medicine: asthma care and pain management. Two vignettes were created for each area and, for each vignette, two treatment/management options were presented. Both options represented appropriate care; however, one option provided an approach that may be related to bias (e.g. choice of opioid analgesic vs. ibuprofen and acetaminophen). Agreement with the options was based on a five-item scale (1. I strongly disagree. This is clearly the wrong treatment/management option.; 2. I disagree. This is the wrong treatment/management option.; 3. I neither agree nor disagree with this treatment/management option.; 4. I agree. This is a good treatment/management option.; 5. I strongly agree. This is clearly a good treatment/management option.). Race was randomly assigned for each vignette with each respondent receiving two vignettes describing American Indian children and two describing non-Hispanic white children. Separate vignettes were designed for physicians/advanced practice providers and nurses to reflect differences in clinical decision making (see Table S1, Supplemental Digital Content 2, which provides the vignettes).
Statistical Analysis
Descriptive statistics were calculated as mean and standard deviation for continuous variables and frequency and percent for categorical variables. Differences in demographic variables for those with valid IAT scores were compared to those without valid scores using a chi-squared test. To test differences in the IAT score based on demographic variables, type of IAT, provider type, explicit bias, and practice characteristics, we used a linear mixed effects regression model with a random effect for the study location. Differences in explicit bias were similarly assessed using mixed effects logistic regression models with a dichotomized version of our explicit bias questions (agree vs. disagree or neither).
Vignettes were analyzed by contrasting a more biased and less biased approach. Responses from both options were combined for each vignette, and models included a random subject effect. The five-level categorical responses were treated as continuous and used in a linear mixed effects regression model. The model included race of the child in the vignette, type of recommendation (i.e. more biased or not) and their interaction. An interactive effect between implicit or explicit bias and race was also examined.
Results
The survey was sent to e-mail addresses of 402 ED providers. The overall response rate was 38.3%. The sample matched the population of providers in the ED at the time of the survey well in terms of demographic characteristics (Table 1). Valid IAT scores (complete IAT and error rate <0.3) were obtained for 101 surveys. Demographic factors did not differ between those who started the survey and those with valid IAT scores, except that fewer nurses and other care providers completed the survey compared to physicians/advanced practice providers (p = 0.01). Demographic information for the respondents is presented in Table 1. The sample was racially homogeneous with over 90% of respondents identifying as white and non-Hispanic. Over half of the respondents were nurses (62%) and over three-fourths of the sample was female (76.1%).
Table 1.
Comparison between the population and survey respondents
| Variable | Category | Populationa % |
Overall (n = 154) N (%)b |
With Valid IAT (n = 101) N (%)b |
|---|---|---|---|---|
| Role in ED | Physician/Advanced Practice Provider | 32.9% | 48 (31%) | 38 (38%) |
| Nurse/Other | 67.1% | 106 (69%) | 63 (62%) | |
| Years in practicec | <6 | 43 (30%) | 26 (28%) | |
| 6–10 | 31 (22%) | 19 (20%) | ||
| >10 | 68 (48%) | 48 (52%) | ||
| Missing | 12 | 9 | ||
| Race | White | 93.8% | 134 (95%) | 86 (93%) |
| Other | 6.3% | 7 (5%) | 6 (7%) | |
| Missing | 12 | 9 | ||
| Ethnicity | Non-Hispanic | 98.7% | 138 (98%) | 91 (99%) |
| Hispanic | 1.3% | 3 (2%) | 1 (1%) | |
| Missing | 12 | 9 | ||
| Sex | Female | 73.0% | 108 (76%) | 70 (76%) |
| Male | 27.0% | 34 (24%) | 22 (24%) | |
| Missing | 12 | 9 | ||
| Age | <30 | 14.8% | 24 (17%) | 11 (12%) |
| 30–49 | 59.8% | 82 (59%) | 58 (63%) | |
| ≥50 | 25.4% | 34 (24%) | 23 (25%) | |
| Missing | 12 | 9 | ||
| Location | Rural | 20.1% | 26 (17%) | 15 (15%) |
| Urban | 79.9% | 128 (83%) | 86 (85%) | |
| % of American Indian children on a typical shift | 0%–10% | 54.7%d | 84 (58%) | 57 (57%) |
| 11% –25% | 24.6%d | 30 (21%) | 23 (23%) | |
| More than 25% | 20.7%d | 31 (21%) | 20 (20%) |
Population refers to providers employed in the EDs at the time of the survey
No demographic information apart from role in the ED was collected from one site due to small numbers of providers (n = 11 overall and n = 9 with a valid IAT)
No population data available
Based on overall proportion of American Indian children seen in the EDs
Implicit Bias
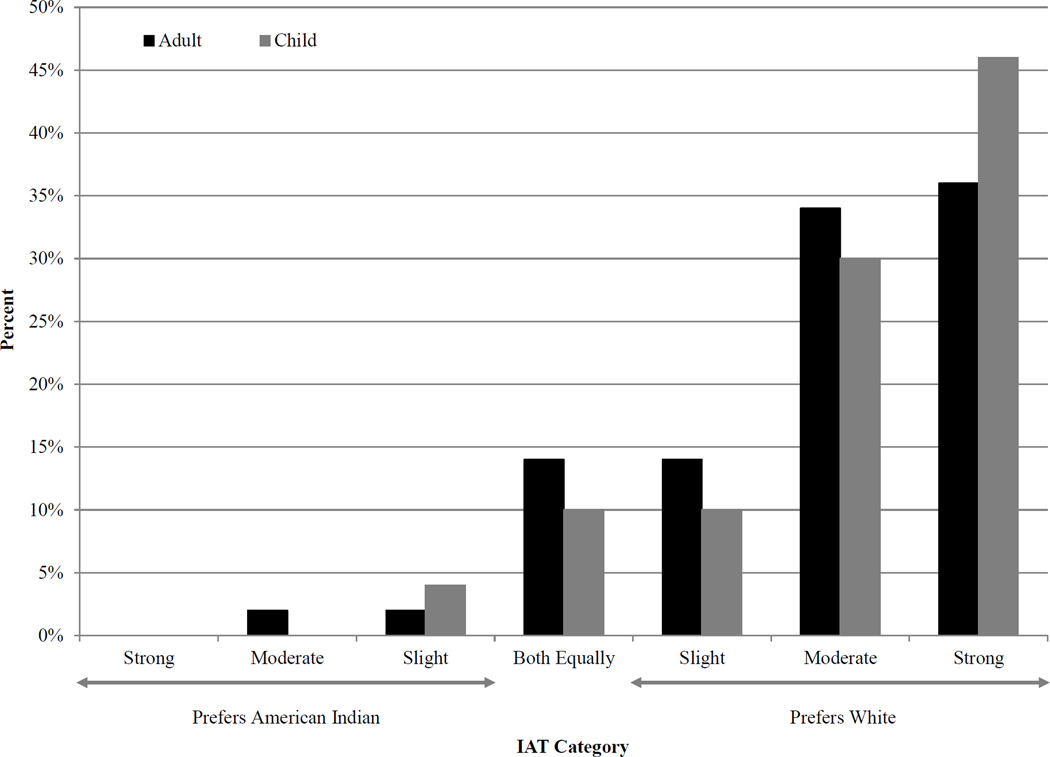
We found a high level of implicit preference for non-Hispanic white individuals, with 84% of those surveyed indicating some implicit preference for non-Hispanic whites (average IAT score = 0.54, 95% confidence interval (CI) = 0.47, 0.62). Contrary to our hypothesis, we did not find a reduction in implicit bias using the child IAT compared to the adult IAT (mean difference = −0.12, 95% CI = −0.27, 0.03, p = 0.12) (Figure 1). In fact, the mean IAT score for the child IAT was higher than for the adult IAT (Table 2).
Figure 1.
Categorized responses to the IAT by type: Adult: IAT with pictures of adults, Child: IAT with pictures of children.
Table 2.
Associations between Demographic Variables and the Implicit Association Test (IAT) Score
| Variable | Category | N (101 Total) |
IAT score mean |
95% CI | pa |
|---|---|---|---|---|---|
| Role in ED | Physician/APC | 38 | 0.56 | (0.45, 0.68) | 0.73 |
| Nurse/Other | 63 | 0.53 | (0.43, 0.64) | ||
| Years in practice | <6 | 26 | 0.60 | (0.48, 0.72) | 0.25 |
| 6–10 | 19 | 0.57 | (0.39, 0.74) | ||
| >10 | 48 | 0.52 | (0.39, 0.64) | ||
| Missing | 9 | ||||
| Race | White | 86 | 0.56 | (0.48, 0.64) | 0.41 |
| Other | 6 | 0.43 | (−0.25, 1.10) | ||
| Missing | 9 | ||||
| Ethnicity | Non-Hispanic | 91 | 0.55 | (0.47, 0.63) | NA |
| Hispanic | 1 | NA | NA | ||
| Missing | 9 | ||||
| Sex | Female | 70 | 0.55 | (0.46, 0.64) | 0.94 |
| Male | 22 | 0.55 | (0.36, 0.73) | ||
| Missing | 9 | ||||
| Age | <30 | 11 | 0.59 | (0.37, 0.81) | 0.04 |
| 30–49 | 58 | 0.62 | (0.52, 0.71) | ||
| ≥50 | 23 | 0.37 | (0.20, 0.55) | ||
| Missing | 9 | ||||
| Location | Rural | 15 | 0.48 | (0.32, 0.63) | 0.47 |
| Urban | 86 | 0.56 | (0.47, 0.64) | ||
| IAT Type | Adult | 51 | 0.49 | (0.39, 0.59) | 0.12 |
| Child | 50 | 0.60 | (0.49, 0.72) | ||
| % of AI children on a typical shift | 0%–5% | 35 | 0.52 | (0.37, 0.67) | 0.90 |
| 6%–10% | 22 | 0.57 | (0.39, 0.74) | ||
| 11% –25% | 23 | 0.57 | (0.40, 0.73) | ||
| More than 25% | 20 | 0.53 | (0.40, 0.66) |
P-value for unadjusted models, similar results were obtained for models adjusted for all other demographic variables (data not shown).
Based on the similarity in responses, we combined results for the child IAT and adult IAT as a measure of implicit bias. IAT scores were not statistically different based on any demographic variables with the exception of age (Table 2). Those over the age of 50 years had a significantly lower IAT score than those middle aged (30–49 years) (mean difference = 0.25, 95% CI = 0.06, 0.42, p = 0.01). IAT scores were not statistically different by provider type, ED location (rural/urban), or % of children who are American Indian seen during a typical shift (Table 2).
Explicit Bias
Agreement with explicit bias questions ranged from 22%-32% with 145 complete responses (Table 3). American Indian children were seen as increasingly challenging and parents/caregivers less compliant as the proportion of American Indian children seen during a typical shift increased (p = 0.04 and 0.02 respectively). Results were similar when limited to those with a valid IAT. Those with more years in practice had lower agreement with statements about American Indian children being more challenging and having less urgent complaints (p = 0.01). IAT scores were not a significant predictor of agreement with explicit bias questions.
Table 3.
Associations between Demographic Variables and Agreement with Explicit Bias Questions
| Variable | Category | More Challenging N = 145 |
Less Urgent N = 145 |
Less Compliant N = 145 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N (%) Agree |
Odds Ratioa |
95% CI | N (%) Agree |
Odds Ratioa |
95% CI | N (%) Agree |
Odds Ratioa |
95% CI | ||
| Overall | 33 (22%) | 38 (33%) | 48 (33%) | |||||||
| Role in ED | Physician or Advanced Practice Provider |
9 (19%) | 1.0 | 13 (27%) | 1.0 | 9 (19%) | 1.0 | |||
| Nurse or Other |
24 (24%) | 1.4 | (0.5, 3.8) | 35 (35%) | 1.2 | (0.5, 2.7) | 39 (39%) | 1.8 | (0.7, 4.4) | |
| Years in practice | <6 | 14 (33%) | 6.4** | (1.8, 22.4) | 18 (42%) | 3.5** | (1.4, 8.7) | 16 (37%) | 1.6 | (0.6, 4.0) |
| 6–10 | 8 (28%) | 5.6** | (1.5, 21.2) | 11 (38%) | 3.0* | (1.1, 8.2) | 10 (34%) | 1.6 | (0.6, 4.4) | |
| >10 | 4 (6%) | 1.0 | 11 (17%) | 1.0 | 15 (23%) | 1.0 | ||||
| Race | White | 24 (19%) | 1.0 | 38 (29%) | 1.0 | 38 (29%) | 1.0 | |||
| Other | 2 (29%) | 3.8 | (0.6, 23.2) | 2 (29%) | 1.1 | (0.3, 6.1) | 2 (29%) | 1.9 | (0.3, 10.9) | |
| Sex | Female | 24 (23%) | 1.0 | 32 (31%) | 1.0 | 33 (32%) | 1.0 | |||
| Male | 2 (6%) | 0.2 | (0.05, 1.1) | 8 (24%) | 0.7 | (0.3, 1.8) | 7 (21%) | 0.7 | (0.3, 1.8) | |
| Age | <30 | 8 (33%) | 2.3 | (0.5, 10.0) | 11 (46%) | 4.6* | (1.3, 16.1) | 11 (46%) | 2.2 | (0.6, 8.2) |
| 30–49 | 13 (16%) | 1.3 | (0.4, 4.6) | 23 (29%) | 2.2 | (0.8, 6.5) | 21 (27%) | 1.3 | (0.5, 3.8) | |
| ≥50 | 4 (13%) | 1.0 | 5 (16%) | 1.0 | 7 (22%) | 1.0 | ||||
| Location | Rural | 11 (46%) | 3.7 | (0.5, 29.5) | 12 (50%) | 2.4 | (0.5, 11.7) | 14 (58%) | 3.3 | (0.6, 19.2) |
| Urban | 22 (18%) | 1.0 | 36 (29%) | 1.0 | 34 (27%) | 1.0 | ||||
| % of American Indian children on a typical shift | 0%–5% | 5 (10%) | 0.2* | (0.1, 0.9) | 11(22%) | 0.3* | (0.1, 0.9) | 7 (14%) | 0.1** | (0.03, 0.4) |
| 6%–10% | 4 (12%) | 0.3 | (0.1, 1.2) | 11 (32%) | 0.6 | (0.2, 1.7) | 9 (26%) | 0.2* | (0.1, 0.8) | |
| 11% –25% | 10 (33%) | 0.9 | (0.3, 2.8) | 10 (33%) | 0.5 | (0.2, 1.5) | 11 (37%) | 0.3* | (0.1, 1.0) | |
| More than 25% | 14 (45%) | 1.0 | 16 (52%) | 1.0 | 21 (68%) | 1.0 | ||||
Odds ratios and 95% CIs based on an unadjusted logistic regression model with a random site effect. Similar results were obtained for models adjusted for other demographic variables (data not shown).
P-value <0.05
P-value <0.01
Vignette Response
There was little difference in responses to vignettes based on race of the child described (Table 4). The only statistically significant difference was for nurses who were more likely to agree with what we considered to be the more biased recommendation to provide a work note to a mother of an asthmatic child presenting with a cough for a child described as American Indian. For a child described as non-Hispanic white, nurses were more likely to agree with the less biased recommendation to decline a work note and refer the mother to follow-up with the child’s primary care provider (p = 0.03). Neither IAT scores nor agreement with explicit bias questions were a significant predictor of vignette response based on the child’s race.
Table 4.
Associations with Vignette Responses and Race of the Child Presented
| Question Category | Treatment recommendationa | Physicians/Advanced Practice Providers | ||||||
| American Indian | White | Pb | ||||||
| N | Mean | SD | N | Mean | SD | |||
| (1) Asthma Control | Work note + Acetaminophen | 30 | 3.6 | 0.9 | 24 | 3.2 | 1.2 | 0.21 |
| Decline + Follow-up PCP | 25 | 2.8 | 1.1 | 18 | 3.2 | 1.2 | ||
| (2) Pain Control | Ibuprofen | 26 | 3.7 | 1.1 | 27 | 4.0 | 0.6 | 0.53 |
| Intra-nasal fentanyl | 24 | 3.2 | 1.3 | 26 | 3.2 | 1.1 | ||
| (3) Pain Control | Oxycodone | 24 | 3.7 | 1.1 | 30 | 4.1 | 0.8 | 0.68 |
| Ibuprofen | 22 | 2.7 | 1.1 | 29 | 3.0 | 1.0 | ||
| (4) Asthma Control | Refer to pulmonary | 28 | 3.8 | 0.9 | 24 | 3.3 | 0.9 | 0.12 |
| Refer back to PCP | 26 | 3.6 | 1.1 | 25 | 3.6 | 1.0 | ||
| Question Category | Treatment recommendationa | Nurses | ||||||
| American Indian | White | |||||||
| N | Mean | SD | N | Mean | SD | |||
| (1) Asthma Control | Work note | 47 | 3.1 | 1.1 | 36 | 2.8 | 1.0 | 0.03 |
| Decline + Follow-up PCP | 40 | 3.0 | 1.2 | 34 | 3.4 | 1.2 | ||
| (2) Pain Control | None | 37 | 2.7 | 1.3 | 36 | 2.7 | 1.3 | 0.91 |
| Ibuprofen | 40 | 3.8 | 1.3 | 39 | 3.7 | 1.1 | ||
| (3) Pain Control | Recommend Oxycodone | 32 | 3.3 | 1.1 | 46 | 3.7 | 1.0 | 0.23 |
| Recommend Ibuprofen | 32 | 3.0 | 1.1 | 39 | 2.9 | 1.2 | ||
| (4) Asthma Control | No treatment, Triage 4 on ESI | 36 | 3.9 | 0.9 | 41 | 3.8 | 0.9 | 0.74 |
| Albuterol, Triage 3 on ESI | 33 | 2.2 | 1.0 | 36 | 2.2 | 1.0 | ||
More empathetic treatment option presented in italics.
P-value for interaction between race and type of recommendation with a random effect for study site
Discussion
We found a high level of implicit bias favoring non-Hispanic whites among ED providers and relatively high levels of explicit bias compared to other studies.23, 24, 26, 29–32
Contrary to our hypotheses, implicit bias was similar against both American Indian children and American Indian adults. While no differences were detected between type of care provider or rural/urban location, we did find differences in explicit bias based on the proportion of American Indian children seen during a typical ED shift. Little difference was seen in the agreement with responses in the vignettes based on the race of the child described. In fact, the only significant difference we found in the vignettes was an increased agreement with one response for American Indian children by nurses. Implicit bias appeared to be more common than explicit bias.
We found higher levels of implicit bias in our study than other studies using the race IAT in medical care providers or medical students.23, 24, 26, 29–32 Other studies have used different measures of explicit bias so our results are difficult to compare. However, Sabin, et. al. found that 45% of pediatricians perceived African Americans to be more likely to be more compliant compared to Non-Hispanic Whites which is in stark contrast to our findings.32 Lower levels of implicit bias were seen in older providers in our data, which is also different than some studies32, 37, yet consistent with others.23, 26 Interestingly, we also found that those with longer years of service had lower agreement with two of three explicit bias questions. This is different than the positive association found by Sabin et. al.32 Overall, it may be that, in ED care providers, older individuals with greater clinical experience have lower levels of bias. Additional exploration of the effect of age on bias is needed.
While we expected to see lower levels of implicit bias for the child IAT, we saw levels of bias that were similar to the adult IAT. While we would like to believe that health professionals generally find racial bias unacceptable and deny being biased when caring for children of different races, studies suggest differential care of children by race.38, 39 Thus our finding of little difference in implicit bias when viewing pictures of children or adults may not be so surprising.
Increasing proportion of visits involving American Indian children was associated with higher agreement with explicit bias questions. Some studies suggest that increasing inter-group contact reduces bias. However, this reduction may be tempered by the equality of the groups involved.40 In our sites, high poverty and low numbers of American Indian providers suggest possible inequality. This trend, only present for explicit bias, may also relate more to true perceptions of care for American Indian children rather than representing broad stereotypes.
Although one study found an association between race, implicit bias, and treatment recommendations29, similar to many other studies, we did not find an association between explicit bias or clinical vignettes and implicit bias.25, 26, 32 Some research has suggested that explicit and implicit biases are conceptually different constructs and might not be associated.34 Implicit bias may be more likely to influence subtle cues and patient perceptions of care rather than actual care. For example, Cooper, et. al. found an association between physician IAT score with negative perceptions of their physician by African American patients.23 Even in cases when clinical care is equivalent, implicit bias could alter the interaction with patients. Another explanation for our finding is that providers may be less truthful in answering explicit bias questions and responding to clinical vignettes.34 It is possible that providers differentially responded to the vignettes after answering explicit bias questions. In the ED, caregivers might be unwilling to acknowledge their bias in an environment that stresses equal treatment and where diversity training has been regularly provided. Surveys designed to identify explicit bias could show lower levels of bias because caregivers feel it is in their best interest not to express their bias or feel that no such bias exists and that they treat all patients equally. Additionally, vignettes may not be a good measure of how providers would actually respond in a clinical setting.
Interventions to mitigate implicit bias or its impact have been explored. Some interventions have shown a short term effect on reducing levels of implicit bias through perspective taking and thinking about counter-stereotypical examples.41–43 Other interventions have shown a more lasting change in implicit attitudes using similar strategies over time.44 However, debate continues about whether or not implicit bias is changeable and, if so, whether this change is enduring.45, 46 This has led some researchers to suggest that simply recognizing implicit bias might be a more appropriate strategy than trying to change the bias itself.47
Limitations
This study has several limitations. We had limited sample size and relatively low response rates compared to published surveys including both ED physicians and nurses48–53, but feel that our responses are representative of the population given the similarity between our sample and the demographics of the population as a whole (Table 1). Some research also suggests reduced non-response bias in physician surveys.54, 55 Our generalizability is also possibly limited to the Upper Midwest. Another limitation is the possible difference between sites in exposure to diversity training. Diversity training was done at all of our sites, but actual content differed and may influence responses. To account for this, we controlled for site as a random factor in all of our analysis. We were unable to separate bias due to race or due to socio-economic status. In our study sites poverty was 4 to 7 times greater for American Indians than non-Hispanic whites.56 Thus stereotypes were likely confounded low socio-economic status.
Since we developed novel IATs for this study, additional studies should validate these IATs. However, working with the experienced Project Implicit staff provided a high likelihood of validity for our new IATs. Finally, our vignettes only covered two areas of care. We tried to balance the length of the survey and felt that these two areas represented commonly seen visits within the ED.
Our study makes several unique contributions to the literature. No other studies have developed a photo-based IAT to examine differences in implicit bias against American Indian children or adults, giving us the ability to assess how this bias may apply to children or the child’s parent/caregiver. We also included multiple sites with different characteristics representing a range of typical EDs that serve the Northern Plains American Indian populations. We found similar rates of implicit bias at all sites. This reinforces the idea that implicit bias is pervasive in many different types of settings serving American Indian children. We are also the first to use the IAT in a combined sample of physicians, advanced practice providers and nurses, finding that implicit bias may be similar across different types of care providers.
Overall, a majority of ED care providers had an implicit preference for non-Hispanic white children or adults. Many ED providers, 22%–32%, agreed with explicit American Indian stereotypes and this differed by practice characteristics. Implicit and explicit biases did not relate to differences in responses to clinical vignettes. Although we did not find a link between implicit bias and agreement with vignette treatment options, the high levels of implicit bias could be associated with the perception of discrimination in health care, documented in other studies, leading to lower access of care by American Indians.18, 57 Addressing implicit bias in the ED setting is challenging, but may be best approached using a combination of interventions that include standardization in triage determination and treatment regimens, direct observation of ED encounters to assess subtle differential treatment, and training providers and staff about implicit bias in health care.
Supplementary Material
Acknowledgments
Funding Source: National Institute on Minority Health and Health Disparities of the National Institutes of Health, Award Number U54MD008164. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to thank Emily Umansky who is a project manager at Project Implicit (a non-profit organization and international collaborative network of researchers investigating implicit social cognition). Ms. Umansky provided assistance with the development of the two IATs, web-based implementation and technical support.
Footnotes
Conflict of Interest: The authors have no potential conflicts of interest to disclose.
This data was presented as a poster at the Pediatric Academic Society Meeting, San Diego, CA, April 26, 2015.
References
- 1.Kovacs G, Croskerry P. Clinical decision making: an emergency medicine perspective. Acad Emerg Med. 1999;6:947–952. doi: 10.1111/j.1553-2712.1999.tb01246.x. [DOI] [PubMed] [Google Scholar]
- 2.Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med. 2002;9:1184–1204. doi: 10.1111/j.1553-2712.2002.tb01574.x. [DOI] [PubMed] [Google Scholar]
- 3.Croskerry P. Diagnostic Failure: A Cognitive and Affective Approach. In: Henriksen K, Battles JB, Marks ES, et al., editors. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology) Rockville (MD): Agency for Healthcare Research and Quality; 2005. [PubMed] [Google Scholar]
- 4.Pomerantz WJ, Schubert CJ, Atherton HD, et al. Characteristics of nonurgent emergency department use in the first 3 months of life. Pediatr Emerg Care. 2002;18:403–408. doi: 10.1097/00006565-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Sharma V, Simon SD, Bakewell JM, et al. Factors influencing infant visits to emergency departments. Pediatrics. 2000;106:1031–1039. doi: 10.1542/peds.106.5.1031. [DOI] [PubMed] [Google Scholar]
- 6.Zimmer KP, Walker A, Minkovitz CS. Epidemiology of pediatric emergency department use at an urban medical center. Pediatr Emerg Care. 2005;21:84–89. doi: 10.1097/01.pec.0000159050.19188.23. [DOI] [PubMed] [Google Scholar]
- 7.Salami O, Salvador J, Vega R. Reasons for nonurgent pediatric emergency department visits: perceptions of health care providers and caregivers. Pediatr Emerg Care. 2012;28:43–46. doi: 10.1097/PEC.0b013e31823f2412. [DOI] [PubMed] [Google Scholar]
- 8.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115:e310–e315. doi: 10.1542/peds.2004-1541. [DOI] [PubMed] [Google Scholar]
- 9.Morrison AK, Chanmugathas R, Schapira MM, et al. Caregiver low health literacy and nonurgent use of the pediatric emergency department for febrile illness. Acad Pediatr. 2014;14:505–509. doi: 10.1016/j.acap.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang U, Weber EJ, Richardson LD, et al. A research agenda to assure equity during periods of emergency department crowding. Acad Emerg Med. 2011;18:1318–1323. doi: 10.1111/j.1553-2712.2011.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zook HG, Kharbanda AB, Flood A, et al. Racial Differences in Pediatric Emergency Department Triage Scores. Journal of Emergency Medicine. 2015 doi: 10.1016/j.jemermed.2015.02.056. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schubot DB. South Dakota Youth Risk Behavior Survey 2011. Pierre, SD: Coordinated School Health; 2011. [Google Scholar]
- 13.Barradas DT, Kroelinger CD, Kogan MD. Medical home access among American Indian and Alaska Native children in 7 states: National Survey of Children's Health. Matern Child Health J. 2012;16(Suppl 1):S6–S13. doi: 10.1007/s10995-012-0990-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121:e286–e298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- 15.Acton KJ, Burrows NR, Moore K, et al. Trends in diabetes prevalence among American Indian and Alaska native children, adolescents, and young adults. Am J Public Health. 2002;92:1485–1490. doi: 10.2105/ajph.92.9.1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brim SN, Rudd RA, Funk RH, et al. Asthma prevalence among US children in underrepresented minority populations: American Indian/Alaska Native, Chinese, Filipino, and Asian Indian. Pediatrics. 2008;122:e217–e222. doi: 10.1542/peds.2007-3825. [DOI] [PubMed] [Google Scholar]
- 17.Alpern ER, Clark AE, Alessandrini EA, et al. Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21:365–373. doi: 10.1111/acem.12347. [DOI] [PubMed] [Google Scholar]
- 18.Call KT, McAlpine DD, Johnson PJ, et al. Barriers to care among American Indians in public health care programs. Medical care. 2006;44:595–600. doi: 10.1097/01.mlr.0000215901.37144.94. [DOI] [PubMed] [Google Scholar]
- 19.Harrison B, Finkelstein M, Puumala S, et al. The complex association of race and leaving the pediatric emergency department without being seen by a physician. Pediatr Emerg Care. 2012;28:1136–1145. doi: 10.1097/PEC.0b013e31827134db. [DOI] [PubMed] [Google Scholar]
- 20.Payne NR, Puumala SE. Racial disparities in ordering laboratory and radiology tests for pediatric patients in the emergency department. Pediatr Emerg Care. 2013;29:598–606. doi: 10.1097/PEC.0b013e31828e6489. [DOI] [PubMed] [Google Scholar]
- 21.Hewstone M, Rubin M, Willis H. Intergroup bias. Annu Rev Psychol. 2002;53:575–604. doi: 10.1146/annurev.psych.53.100901.135109. [DOI] [PubMed] [Google Scholar]
- 22.Major B, Mendes WB, Dovidio JF. Intergroup relations and health disparities: a social psychological perspective. Health Psychol. 2013;32:514–524. doi: 10.1037/a0030358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper LA, Roter DL, Carson KA, et al. The Associations of Clinicians’ Implicit Attitudes About Race With Medical Visit Communication and Patient Ratings of Interpersonal Care. American journal of public health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. Journal of general internal medicine. 2007;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haider AH, Schneider EB, Sriram N, et al. Unconscious race and class bias: its association with decision making by trauma and acute care surgeons. The journal of trauma and acute care surgery. 2014;77:409–416. doi: 10.1097/TA.0000000000000392. [DOI] [PubMed] [Google Scholar]
- 26.Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306:942–951. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Penner LA, Dovidio JF, West TV, et al. Aversive Racism and Medical Interactions with Black Patients: A Field Study. Journal of experimental social psychology. 2010;46:436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sabin J, Nosek BA, Greenwald A, et al. Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20:896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. American journal of public health. 2012;102:988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White-Means S, Zhiyong D, Hufstader M, et al. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students: implications for addressing health disparities. Medical care research and review : MCRR. 2009;66:436–455. doi: 10.1177/1077558709333995. [DOI] [PubMed] [Google Scholar]
- 31.Sabin JA, Moore K, Noonan C, et al. Clinicians' Implicit and Explicit Attitudes about Weight and Race and Treatment Approaches to Overweight for American Indian Children. Child Obes. 2015;11:456–465. doi: 10.1089/chi.2014.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Medical care. 2008;46:678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 33.U.S. Census Bureau. [Accessed December 7, 2015];2010–2014 American Community Survey 5-year Estimates. 2015 Available at: http://factfinder.census.gov.
- 34.Greenwald AG, Poehlman TA, Uhlmann EL, et al. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97:17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 35.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- 36.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74:1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 37.Stewart BD, von Hippel W, Radvansky GA. Age, race, and implicit prejudice: using process dissociation to separate the underlying components. Psychol Sci. 2009;20:164–168. doi: 10.1111/j.1467-9280.2009.02274.x. [DOI] [PubMed] [Google Scholar]
- 38.Berdahl T, Owens PL, Dougherty D, et al. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children's health care quality. Acad Pediatr. 2010;10:95–118. doi: 10.1016/j.acap.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 39.Flores G, Committee On Pediatric R Technical report--racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125:e979–e1020. doi: 10.1542/peds.2010-0188. [DOI] [PubMed] [Google Scholar]
- 40.Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. J Pers Soc Psychol. 2006;90:751–783. doi: 10.1037/0022-3514.90.5.751. [DOI] [PubMed] [Google Scholar]
- 41.Blair IV. The Malleability of Automatic Stereotypes and Prejudice. Pers Soc Psychol Rev. 2002;6:242–261. [Google Scholar]
- 42.Dasgupta N, Greenwald AG. On the malleability of automatic attitudes: combating automatic prejudice with images of admired and disliked individuals. J Pers Soc Psychol. 2001;81:800–814. doi: 10.1037//0022-3514.81.5.800. [DOI] [PubMed] [Google Scholar]
- 43.Galinsky AD, Moskowitz GB. Perspective-taking: decreasing stereotype expression, stereotype accessibility, and in-group favoritism. J Pers Soc Psychol. 2000;78:708–724. doi: 10.1037//0022-3514.78.4.708. [DOI] [PubMed] [Google Scholar]
- 44.Devine PG, Forscher PS, Austin AJ, et al. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of experimental social psychology. 2012;48:1267–1278. doi: 10.1016/j.jesp.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rudman LA, Ashmore RD, Gary ML. "Unlearning" automatic biases: the malleability of implicit prejudice and stereotypes. J Pers Soc Psychol. 2001;81:856–868. doi: 10.1037//0022-3514.81.5.856. [DOI] [PubMed] [Google Scholar]
- 46.Joy-Gaba JA, Nosek BA. The Surprisingly Limited Malleability of Implicit Racial Evaluations. Soc Psychol. 2010;41:137–146. [Google Scholar]
- 47.Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. American journal of public health. 2012;102:945–952. doi: 10.2105/AJPH.2011.300601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Betz ME, Arias SA, Miller M, et al. Change in emergency department providers' beliefs and practices after use of new protocols for suicidal patients. Psychiatr Serv. 2015;66:625–631. doi: 10.1176/appi.ps.201400244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kene MV, Ballard DW, Vinson DR, et al. Emergency Physician Attitudes, Preferences, and Risk Tolerance for Stroke as a Potential Cause of Dizziness Symptoms. West J Emerg Med. 2015;16:768–776. doi: 10.5811/westjem.2015.7.26158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kotora JG. An assessment of Chemical, Biological, Radiologic, Nuclear, and Explosive preparedness among emergency department healthcare providers in an inner city emergency department. J Emerg Manag. 2015;13:431–446. doi: 10.5055/jem.2015.0253. [DOI] [PubMed] [Google Scholar]
- 51.Reed JL, Vaughn LM, Pomerantz WJ. Attitudes and knowledge regarding emergency contraception among emergency department adolescents and providers. Pediatr Emerg Care. 2012;28:775–779. doi: 10.1097/PEC.0b013e3182627d14. [DOI] [PubMed] [Google Scholar]
- 52.Walters EL, Reibling ET, Wilber ST, et al. Emergency department provider preferences related to clinical practice guidelines for tobacco cessation: a multicenter survey. Acad Emerg Med. 2014;21:785–793. doi: 10.1111/acem.12421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Freiermuth CE, Haywood C, Jr, Silva S, et al. Attitudes toward patients with sickle cell disease in a multicenter sample of emergency department providers. Advanced emergency nursing journal. 2014;36:335–347. doi: 10.1097/TME.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Keeter S, Miller C, Kohut A, et al. Consequences of reducing nonresponse in a national telephone survey. Public Opin Q. 2000;64:125–148. doi: 10.1086/317759. [DOI] [PubMed] [Google Scholar]
- 55.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20:61–67. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 56.U.S. Census Bureau. [Accessed December 7, 2015];American FactFinder: Poverty Status in the Past 12 Months by Sex by Age, 2006–2010. 2010 Available at: http://factfinder.census.gov.
- 57.Gonzales KL, Lambert WE, Fu R, et al. Perceived racial discrimination in health care, completion of standard diabetes services, and diabetes control among a sample of American Indian women. Diabetes Educ. 2014;40:747–755. doi: 10.1177/0145721714551422. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.