Abstract
Study Objectives:
Sleep disturbances have been associated with attention deficit hyperactivity disorder (ADHD), but such relationship is still unclear. The results from the studies conducted do not provide enough evidence to support a sleep physiology inherent to ADHD. This study tries to determine if that sleep physiology really exists by comparing children with ADHD and control children in some sleep parameters.
Methods:
A search was conducted in several databases (Web of Science, Scopus, Pubmed and PsycINFO), and a manual search, to retrieve all the articles available from 1987 until March 2014. Of 8,678 non-duplicate studies retrieved, 11 studies met the inclusion and methodological quality criteria. Two meta-analyses were performed with eight of those studies, depending on data provided by them: polysomnographic or actigraphic. A fixed-effects model, and the standardized mean difference (SMD) as the index of effect size, were used in both meta-analyses.
Results:
Significant differences were found only in the meta-analysis with polysomnography as outcome. Children with ADHD were found to spend more time in stage 1 sleep than controls (pooled SMD = 0.32, 95% CI = 0.08–0.55, p value = 0.009).
Conclusions:
Although few differences in sleep between children with ADHD and controls have been found in this review, further studies are required on this matter. Those studies should consider some variables discussed in this review, in order to obtain useful and reliable conclusions for research and clinical practice. Particularly, the influence of assessment criteria and ADHD subtypes in the sleep characteristics of children with ADHD should be addressed.
Citation:
Díaz-Román A, Hita-Yáñez E, Buela-Casal G. Sleep characteristics in children with attention deficit hyperactivity disorder: systematic review and meta-analyses. J Clin Sleep Med 2016;12(5):747–756.
Keywords: sleep, attention deficit hyperactivity disorder, ADHD, children, systematic review, meta-analysis
INTRODUCTION
Attention deficit hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders in childhood and adolescence, with a worldwide prevalence rate of about 5.3% and 5% in Europe.1,2 The considerable increase in ADHD diagnosis for the last few years (around 24% between 2001 and 2010),3 has made this disorder a topic of great interest for many researchers and clinicians. Mainly because of its numerous effects on the social, emotional, and cognitive functioning. ADHD symptomatology interferes negatively with academic performance, levels of self-esteem and quality life, and social and family relationships of children who suffer from it.4–6 In addition, ADHD is related to numerous comorbid conditions in childhood and adolescence, including bipolar disorder, oppositional defiant disorder, behavioral and substance use disorders, and eating disorders.7–10 It has been also associated with depression and anxiety symptoms and even identified as a major risk factor for suicide.11,12
Other problems related to this disorder have been sleep disturbances. Although rates estimated have varied over the years, it has been reported that up to 55% of children with ADHD may have sleep problems.13 In general, sleep disturbances have negative consequences in different areas of a child's life. For instance, sleep problems have a negative impact on attention and/ or behavior and on daytime sleepiness levels of children.14,15 Given that these factors have repercussions on academic or cognitive performance, which were already affected in children with ADHD, sleep disturbances in these children might be acting as a positive feedback mechanism, exacerbating their symptomatology. Therefore, the relationship between sleep characteristics and ADHD in children needs to be examined for the development of effective intervention or treatment programs for ADHD that could improve their quality of life. Nevertheless, such relationship is not totally determined yet, because the results obtained until now have been contradictory.
Although numerous authors have found differences between children with and without ADHD in several sleep descriptors, such differences have not been consistent. Whereas some authors have found differences on sleep continuity and architecture,16,17 other authors have found them regarding motor activity during sleep,18,19 and others in daytime sleepiness levels.20 However, the discrepancies between the results of the previous studies might be due to the differences between them with regard to: (a) the type of measure (objective or subjective) employed to obtain data, and the little comparison between both information sources; (b) the age ranges covered; (c) the consideration of sex differences in the clinical symptomatology of ADHD; (d) the control of participants' medication and of their comorbid conditions; (e) the distinction made between the three subtypes of ADHD; and (f) the ADHD assessment itself, because there is not a common assessment protocol to all the studies.19,21–24
Besides the limitations resulting from those differences between the studies, another important limitation is the lack of rigorous inclusion and exclusion criteria for participants in several studies. For instance, participants with primary sleep disorders, like apnea or restless legs syndrome, were not excluded in some studies.25–30 This limitation makes it difficult to conclude if sleep disturbances in those children with ADHD were actually due to ADHD symptomatology, or if their primary sleep disorders might be biasing the results; for instance, regarding sleep physiology. Given that those primary sleep disorders suffered from children with ADHD may be changing their sleep architecture regardless their ADHD symptoms, it is not possible to ensure that the sleep architecture found in such studies is a distinctive feature of ADHD. This question was not taken into account either in the reviews and/or meta-analyses conducted until now.23,31,32 Therefore, the results of these reviews should be also interpreted with a certain caution.
Considering these aspects, the main goal of this study is to determine the relationship between sleep and ADHD, taking into account the limitations of earlier studies. Particularly, we analyze if there are differences in sleep characteristics between children with and without ADHD. Furthermore, we study if the possible differences between them might be influenced by variables inherent to participants or methodology followed in the studies included: sex, subtypes, medication use, comorbidities, assessment measures and inclusion criteria for participants.
METHODS
This systematic review was conducted according to a previously established protocol drawn up following the recommendations of the MOOSE statement.33
Search Strategy
A search was conducted in Pubmed, Web of Knowledge, PsycINFO and Scopus, entering the following search terms in Spanish or in English depending on the database: < < ADHD OR “attention deficit” OR hyperactivity AND sleep* > > . Search fields were title, abstract and keywords. No search limit was established by language, but by publication year, in or after 1987. This is the year in which the third revised edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) was published and sleep disturbances stopped being one of the diagnostic criteria of ADHD.34
Subsequently, the literature search was completed with a manual search, reviewing the references included in the selected articles, and the citations that they had received.
We employed the RefWorks bibliographic management program to manage the references found.
Selection Criteria
Studies available from 1987 until March 2014 were selected if they: (a) included children with ADHD, according to the diagnostic criteria of DSM or any other diagnostic manual, in which sleep disturbances were not one of the symptoms of the disorder; (b) were comparative studies (randomized or non-randomized) in which the control group was composed of children without ADHD and the evaluation had been performed simultaneously in both groups by the research team itself (what guarantees an identical and less biased assessment for both groups); (c) did not include children with primary sleep disorders; (d) assessed differences in sleep between children with and without ADHD; (e) provided data in relation to age, sex, medication use, and comorbid diseases of participants; and (f) were not just abstracts or conference papers.
Titles and abstracts of all the articles retrieved, after excluding duplicates, were examined to check if they fulfilled the inclusion criteria previously described; those in which there were some doubts were assessed in full text length.
Selected studies were assessed in terms of risk of bias or methodological quality through the Scottish intercollegiate guidelines network (SIGN 50) scale designed for cohort studies that has a wide acceptance.35,36 The assessment was performed blindly, as a mean of guaranteeing the preciseness of this process. This scale enables three assessment categories—high quality, medium quality, and low quality—on the basis of risk of bias. Due to the fact that some items of the scale were not applicable to the type of studies selected (1.3–1.6 and 1.12), we decided to obtain a weighted score by subtracting one degree of quality from each of the studies. Thus, we made sure that the assessment was not biased due to the loss of items.37 Only those studies that, after subtracting that degree of quality, belonged to the second category (medium quality) were included in the review.
From each study included, the following data were collected: first author and publication year of the article, country in which the study was performed, number of participants in each group (along with age, sex, medication use, subtypes, and comorbidities), study design, assessment measures employed, and main results obtained.
Studies were assessed for inclusion criteria and methodological quality, and the data extracted, by two of the three authors independently, and discrepancies between them were resolved by a third author.
Data Analysis
Two meta-analyses were performed following the steps proposed by Botella and Gambara38—one of them with polysomnographic data and the other with actigraphic data. The most common variables among studies were selected as dependent variables: total sleep time, sleep latency, sleep efficiency, wake time, stage 1 NREM sleep, stage 2 NREM sleep, slow wave sleep, REM sleep, and REM latency. The independent variable was always the presence or absence of ADHD.
Both meta-analyses were carried out using Review Manager 5.3. software, with a fixed-effects model and a 95% confidence interval (CI). The index of effect size used was the standardized mean difference (SMD), applying the correction proposed by Hedges39 to avoid bias due to sample size. The weighted mean effect size (pooled SMD) was obtained through the inverse variance method, and its statistical significance by the Z statistic. Heterogeneity between studies was also analyzed by means of the χ2 and I2 statistics,40 interpreting the percent value of this last one according to the levels suggested by Higgins et al.41: low (I2 < 25%), medium (25% < I2 < 50%), and high heterogeneity (I2 > 50%).
Sensibility and publication bias analyses could not be performed because the number of studies included was not enough.42 Such circumstance did not allow us to carry out any other analysis according to the variables of interest mentioned in our goals (age, sex, ADHD subtypes, medication use, comorbidities and assessment measures employed), being only possible to describe them by means of a narrative synthesis.
RESULTS
Studies Included
We retrieved 12,495 studies through databases (Figure 1). From 8,678 non-duplicate studies, only 11 were included in the review, after removing those that did not meet the inclusion criteria or presented overlapping data. Those 11 studies18,22,43–51 passed the assessment of risk of bias, obtaining a medium methodological quality level. No new study was retrieved through the manual search.
Figure 1. Results of the search and selection of studies.
The main characteristics of the studies included and their participants are shown in Tables 1 and 2. In all the studies, a cross-sectional assessment of participants had been performed, 6 performed it with objective measures of sleep uniquely, one study used subjective measures, while 4 employed both.
Table 1.
Characteristics of the included studies.
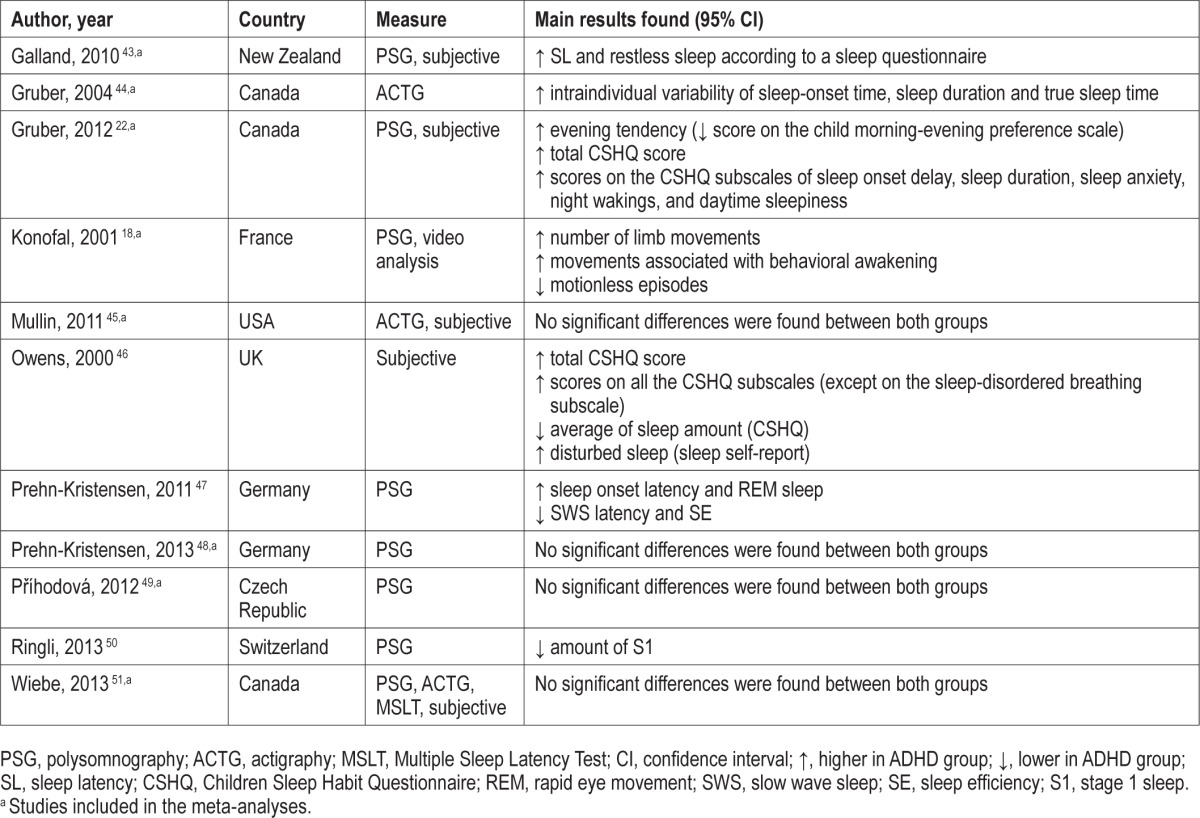
Table 2.
Participant characteristics of the included studies.
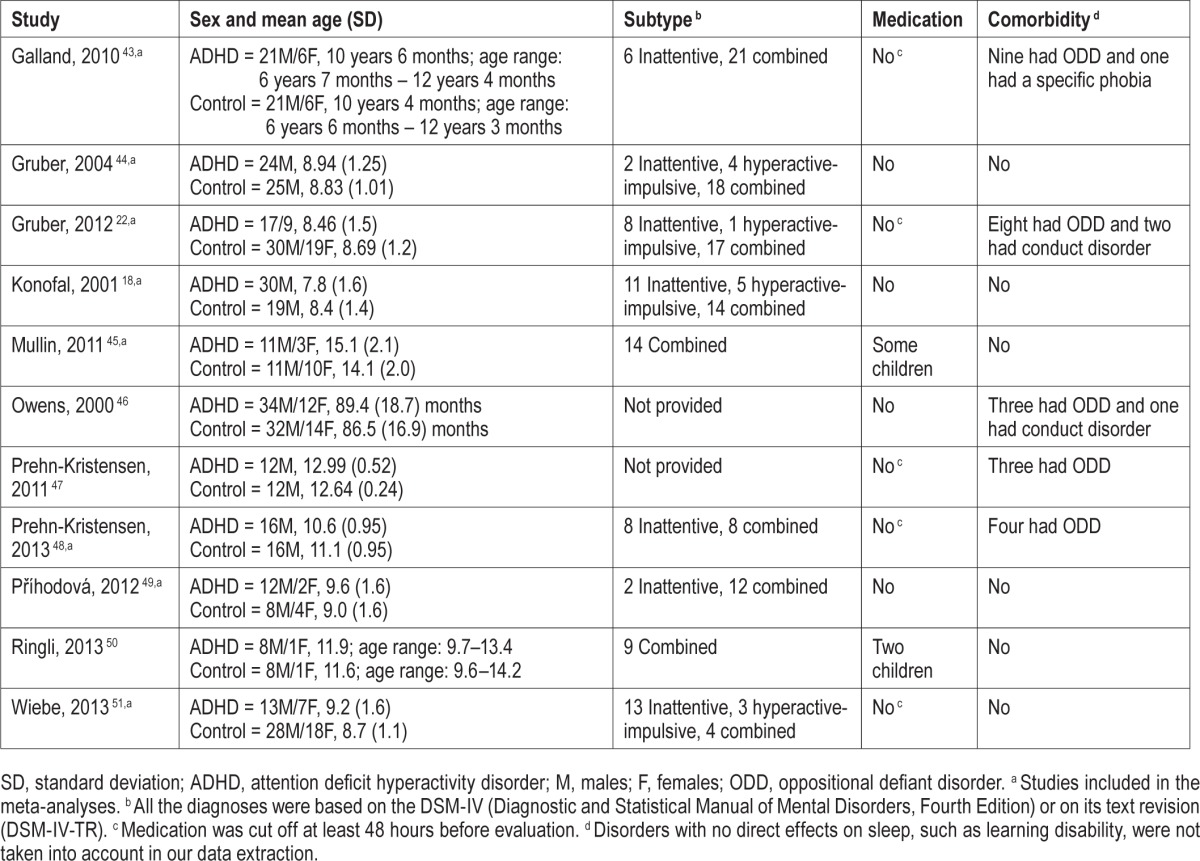
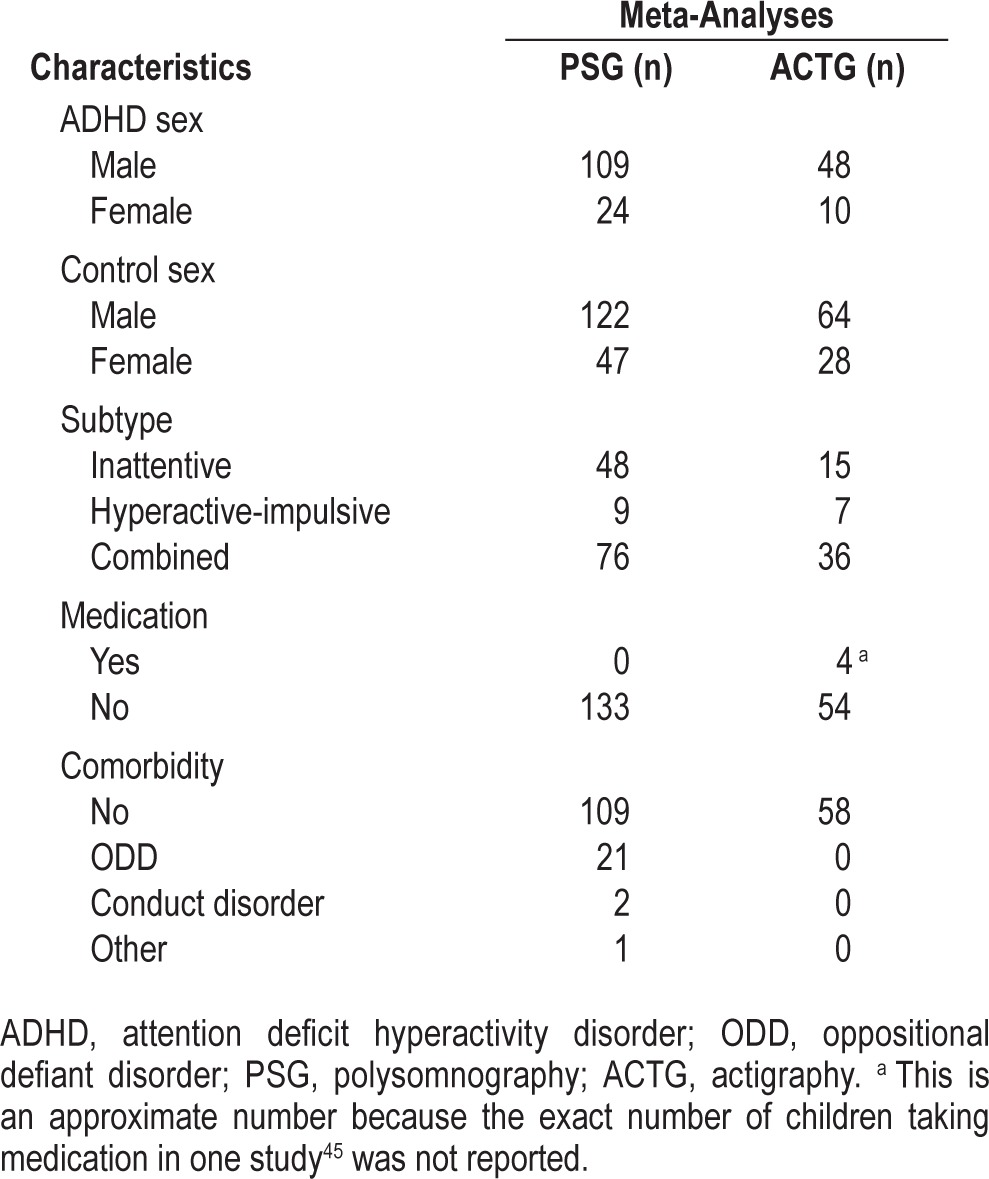
For the meta-analyses, studies were considered according to the measure employed for sleep assessment. At first time, 8 studies were included in the first meta-analysis that performed a sleep assessment through polysomnography (PSG), and 3 studies in the second meta-analysis that used actigraphy to assess sleep. One study employed both objective measures to assess to the participants, so it was included in both meta-analyses.51 On the contrary, the study that only provided subjective measures46 was not included in any meta-analysis, because no meta-analysis was carried out on the basis of subjective measures, since subjective measures were too varied between studies to be summarized in a meta-analysis. Thus, only 10 of the 11 studies included in the review were included in the meta-analyses. However, from those 10 studies included initially, 2 studies were excluded from the meta-analysis with PSG as outcome,47,50 because they increased significantly the heterogeneity between the studies. In particular, when those studies were included, the percent values of heterogeneity according to the I2 statistic ranged between 53% and 76% in 5 of the 9 sleep variables considered. The decision of excluding those studies was taken because it was not possible to employ a random-effects model or to perform a meta-regression because of the sparse number of studies included.42
The final sample of each meta-analysis was composed of 133 (PSG) and 58 (actigraphy) children with ADHD, and 169 (PSG) and 92 (actigraphy) controls, whose most relevant characteristics are shown in Table 3. Regarding the meta-analysis with PSG as outcome, the Rechtschaffen and Kales criteria52 were applied as scoring rules in all the studies included, except for one of the studies22 in which the American Academy of Sleep Medicine criteria53 were applied. A difference between both scoring rules that could have affected our results is the consideration of stage 3 and stage 4 sleep as the stage of slow wave sleep as a whole, but this last variable was also provided by the studies in which the Rechtschaffen and Kales criteria had been applied. In addition, although some significant differences have been pointed out between both scoring systems in sleep data,54 there are no reasons to think that such differences might have affected our results. Mainly because, besides the fact a different system criterion was applied only in one study of the meta-analysis at issue,22 the same procedure of scoring was also followed in all the studies for both children with ADHD and control children. Differences in sleep data depending on scoring criteria would have affected both groups of children equally, with no repercussion on the differences found between them in sleep parameters.
Table 3.
Main characteristics of children included in the meta-analyses.
In all the studies, the proper procedure was carried out in order not to include children with primary sleep disorders (even snoring or sleep-disordered breathing). Both in the studies with PSG and in the studies with actigraphy, children with ADHD and controls were excluded if they displayed some sleep disorder or if this disorder was known before taking part in the study. Even in the study in which only subjective measures were employed to obtain sleep data,46 parents of children were interviewed on this matter prior to their participation.
Meta-Analyses
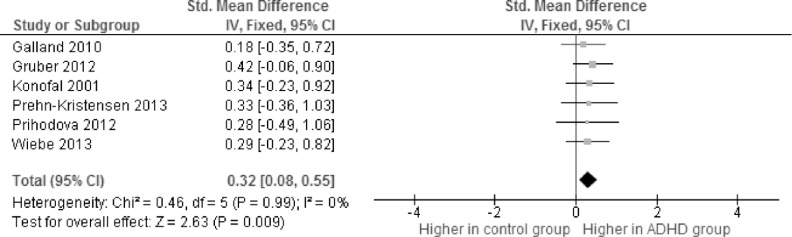
In the meta-analysis with PSG as outcome, only 1 of the 9 variables assessed approached statistical significance, the stage 1 sleep (pooled SMD = 0.32, 95% CI = 0.08–0.55, p value = 0.009). Children with ADHD spend more time in that sleep stage than control children (Table 4, Figure 2). In the rest of the variables, although the differences between both groups were not significant, that tendency is also observed, primarily in the case of sleep latency, so a higher sleep latency is observed in children with ADHD compared with the control group (pooled SMD = 0.23, 95% CI = −0.01–0.46, p = 0.06). The heterogeneity percent between the studies was zero in all the variables, except for the wake time (I2 = 3%, p = 0.38), slow wave sleep (I2 = 13%, p = 0.33), and sleep efficiency (I2 = 54%, p = 0.05) variables. Although the heterogeneity found in those sleep parameters could be supposed to affect to the proportion of stage 1 sleep, the I2 values obtained are into the limits considered for low heterogeneity.41 Only the heterogeneity percent found in sleep efficiency is considered high.41 This high heterogeneity, although requires the results in sleep efficiency to be interpreted with extreme caution, cannot affect to the proportion of stage 1 sleep. Basically, because sleep efficiency is a parameter obtained as the result of (TST/TIB) × 100, considering all sleep stages (1, 2, 3, 4, and REM) in TST as a whole.53
Table 4.
Results of the meta-analysis with polysomnography as outcome (n = 302).
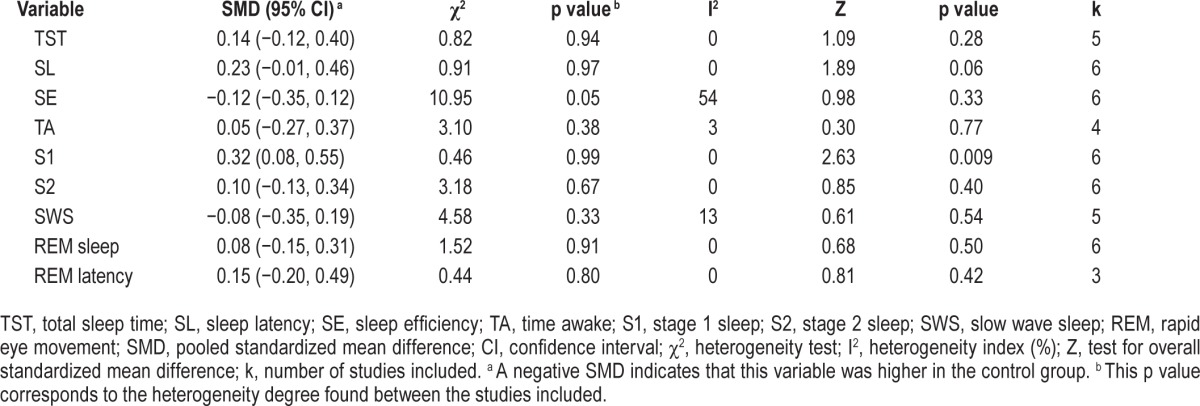
Figure 2. Forest plot of the standardized mean differences (SMD) obtained in the meta-analysis with polysomnography as outcome for stage 1 sleep.
IV, inverse variance method; Fixed, fixed-effects model; CI, confidence interval; Chi2, heterogeneity test; df, degrees of freedom; I2, heterogeneity index; Z, test for overall standardized mean difference; ADHD, attention deficit hyperactivity disorder.
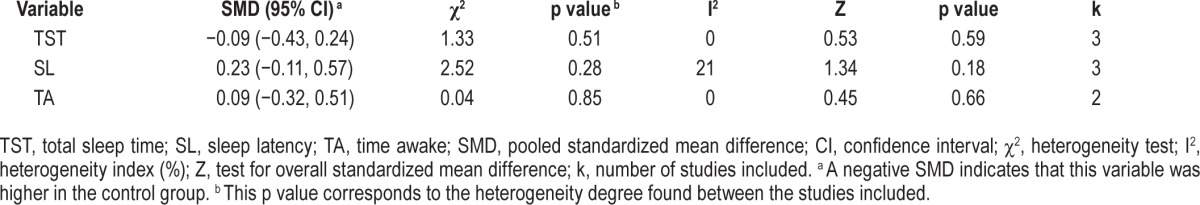
Otherwise, in the meta-analysis with actigraphy as outcome, significant differences between children with ADHD and controls were not observed in any variable (Table 5). The heterogeneity degree between the studies of this meta-analysis was always within the acceptable limits (I2 = 0%–21%, p > 0.05).
Table 5.
Results of the meta-analysis with actigraphy as outcome (n = 150).
DISCUSSION
This study aimed at determining the relationship between sleep characteristics and ADHD in children, analyzing the differences in sleep physiology between children with and without ADHD through the meta-analysis, and defining strict inclusion and exclusion criteria that considered the limitations from preceding studies previously mentioned. In particular, we intended to compare children with ADHD and control children in sleep, excluding of them those who suffered from primary sleep disorders. This is a novel criterion in this study, in comparison with previous systematic reviews and meta-analyses, and that was adopted to determine the sleep architecture of ADHD itself, distinguishing it from the sleep architecture inherent to primary sleep disorders.
In this regard, it is observed that just the percent of stage 1 sleep approaches the statistical significance when the assessment is performed by PSG. Thus, these results enable to conclude that children with ADHD spend more time in stage 1 NREM sleep than children without this pathology. It means that children with ADHD show a lighter sleep than controls. These results are not consistent with the results corresponding to the 2 studies that were not included in the meta-analyses (because of heterogeneity) but they were in this review.47,50 In one of those studies,47 differences in stages of NREM sleep between children with ADHD and controls were not found. Moreover, in that study, children with ADHD, besides a higher sleep onset latency and a lower sleep efficiency, spent more time in stage REM sleep than controls.47 According to that study, children with ADHD would have a deeper sleep that controls and not the opposite. In the other study included,50 children with ADHD were found to spend less time in stage 1 NREM sleep than controls. Definitely, results from both studies were contrary to what we have found. However, these inconsistencies between our results and the results from those 2 studies mentioned may be due to some aspects that are discussed below.
We also wanted to determine if other variables might be having an impact on sleep characteristics, such as age, sex, ADHD subtypes, medication use, comorbidities, and assessment measures employed. In this sense, a certain similarity was observed between the studies included in the meta-analyses regarding age, medication use (children who were taking medication stopped taking it at least 48 hours before evaluation, with the exception of 4 children in one study45), comorbidities of participants, and the type of objective assessment employed (PSG-actigraphy) (Tables 1, 2, and 3). In addition, even though a greater number of boys than girls is observed in all the studies included in the meta-analyses, this superiority of masculine sex is found both in children with ADHD and in control children (Table 3). Therefore, it is just possible to discuss the influence of ADHD subtypes in sleep disturbances.
In fact, although few studies have analyzed the differences between the ADHD subtypes regarding sleep patterns, the results found indicate that sleep disturbances are different depending on the subtype or the predominant symptomatology in ADHD. Children with the inattentive subtype appear to have fewer sleep problems, being those children with the hyperactivity-impulsivity subtype who show more problems in this area.55,56 In this regard, the distribution of ADHD subtypes between the participants of the studies included in the 2 meta-analyses of this review was not homogeneous. The number of children with ADHD with the inattentive subtype was higher than the number of children with the hyperactivity-impulsivity subtype (Table 3), mainly in the meta-analysis with PSG as outcome. Therefore, if children with the inattentive subtype predominate, who show fewer sleep problems, the results might be under the influence of this variable. With regard to the other 2 studies that did not distinguish between subtypes,46,47 these were not included in the meta-analyses, so they cannot have influenced our results.
In summary, on the basis of all the above, it seems plausible that the differences in sleep found in this review between control children and children with ADHD were affected by the ADHD subtypes of the children included. Or, moreover, that the absence of greater significant differences in sleep between both groups has been conditioned by this variable.
Other variable that may have had an influence in the results obtained in the meta-analysis is the sample size in each study. Although the total sample of each meta-analysis was composed of an acceptable number of participants in each group (Table 3), undoubtedly the sample sizes of each study included were not too high (Table 2). Noteworthy, above all, the studies of Mullin,45 Prehn-Kristensen,48 and Prihodova,49 with 14, 16, and 14 participants with ADHD, respectively. This low sample size might have determined the lack of statistical significance in other variables, because although not significant, some tendencies are appreciated in the rest of the variables (Tables 4 and 5).
In addition, there are other variables also related to sleep that have not been taken into account in our meta-analyses. In this sense, some of the studies included in this review provided subjective sleep data. Due to the lack of analogy between those studies with regard to the sleep variables considered and the subjective assessment measures employed, no meta-analysis could be performed with subjective sleep measures. Nevertheless, significant differences were found in those studies included between children with ADHD and controls in some subjective sleep variables that are important to be noted. For instance, one of these variables is daytime sleepiness. Children with ADHD showed a higher daytime sleepiness than controls in 2 of the studies,22,46 according to their scores in the Children Sleep Habit Questionnaire (CSHQ). Conversely, daytime sleepiness was not found to be affected by ADHD in 2 other studies included, according to a sleep questionnaire43 or a modified Epworth Sleepiness Scale.51 Such discrepancies, even in this subjective variable, deserves a deeper analysis in future studies. For that reason, although both meta-analyses presented in this review were performed focused on nocturnal sleep characteristics, further research is needed to pay attention to some other sleep variables, such as daytime sleepiness, that might be also affected by ADHD symptomatology.
Finally, although ADHD is currently a topic of great interest, there is a debate in relation to the disorder, leading some authors even to question its own existence.57 Other authors suggest that the big problem might be an overdiagnosis of the disorder58,59 that would be the responsible for the increase in the number of children diagnosed with ADHD, increasing the number of false positives. Although the latter is not totally clear,60 in that case, this could be a factor that impacts on the controversy about the existence of sleep disturbances in children with ADHD. Since a high number of false positives in the group with ADHD would lead the differences between the groups with regard to sleep disturbances to disappear. This requires that the future studies include an assessment of the child by a specialist that covers different areas (school, social, and family), to corroborate the diagnosis. In this sense, there were not enough data provided in all the studies included in this review in order to confirm that the diagnosis of children with ADHD had been appropriately corroborated (example, Mullin et al.45), and in the cases in which it was corroborated, nor was a common assessment protocol.
In general, this systematic review has several limitations; among them, the small sample size of the studies, like the sparse number of studies included in the review and in the meta-analyses. The other limitation is the unequal distribution of ADHD subtypes between the participants of those studies. These limitations do not enable to generalize the results, not even make possible to obtain convincing conclusions. On the contrary, such limitations highlight the importance of further studies on this topic.
This review has also some strengths to be noted. In the first place, the development of a previous protocol guaranteed the methodological rigor of the following review. Secondly, a very complete search of all the studies available in the literature was carried out, avoiding bias by publication language. In the way, the blind assessment of the quality of the studies avoided the presence of methodological bias in them and in the evaluation itself. Also, rigorous inclusion criteria were followed, which enabled to obtain valid and feasible results. For instance, those studies in which some participants showed primary sleep disorders were excluded, along with those in which a control group composed of children with no disorders was not included. These two criteria meant that if differences in sleep between children with ADHD and controls were found, these could not be attributed to other factors different from the pathology studied itself. Finally, when meta-analyses were performed, the opportune corrective measures were taken in order to avoid that the results obtained were conditioned by the heterogeneity between the studies or the different assessment measures of sleep parameters.
CONCLUSIONS
The results obtained with this systematic review and meta-analyses suggest that children with ADHD show few differences in sleep with regard to children without this pathology. However, such differences might be stressed if some of the limitations previously discussed would be taken into account. For that reason, a higher number of studies on the relationship between sleep and ADHD are still required. Above all, these studies will have to: (a) assess if the predominant sub-type or symptomatology in these children leads to particular sleep patterns; (b) count on an appropriate sample size that enables to generalize the results; (c) consider both objective and subjective sleep variables and perform a comparison between them; (d) avoid the presence in the sample of children with primary sleep disorders, or control children with medical or psychological problems, which affect the results obtained; and (e) confirm the ADHD diagnosis, guaranteeing the absence of false positives in the group with ADHD.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was funded by Grant Number EDU2010-21215 from the Spanish Ministry of Science and Innovation to Dr. Buela-Casal. The authors have indicated no financial conflicts of interest. This study is part of a Thesis Doctoral.
ABBREVIATIONS
- ↑
higher in ADHD group
- ↓
lower in ADHD group
- ACTG
actigraphy
- ADHD
attention deficit hyperactivity disorder
- χ2
heterogeneity test
- CI
confidence interval
- CSHQ
Children Sleep Habit Questionnaire
- df
degrees of freedom
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- DSM-III-R
DSM, Third Edition Revised
- DSM-IV
DSM, Fourth Edition
- DSM-IV-TR
DSM, Fourth Edition Text Revision
- F
females
- Fixed
fixed-effects model
- I2
heterogeneity index (%)
- IV
inverse variance method
- k
number of studies included
- M
males
- MSLT
Multiple Sleep Latency Test
- NREM
non-rapid eye movement
- ODD
oppositional defiant disorder
- PSG
polysomnography
- S1
stage 1 sleep
- S2
stage 2 sleep
- SD
standard deviation
- SE
sleep efficiency
- SIGN-50
Scottish Intercollegiate Guidelines Network
- SL
sleep latency
- SMD
standardized mean difference
- SWS
slow wave sleep
- TA
time awake
- TST
total sleep time
- Z
test for overall standardized mean difference
REFERENCES
- 1.Polanczyk G, Silva M, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–8. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 2.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–79. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Getahun D, Jacobsen SJ, Fassett MJ, Chen W, Demissie K, Rhoads GG. Recent trends in childhood attention-deficit/hyperactivity disorder. JAMA Pediatr. 2013;167:282–8. doi: 10.1001/2013.jamapediatrics.401. [DOI] [PubMed] [Google Scholar]
- 4.Polderman TJ, Boomsma DI, Bartels M, Verhulst FC, Huizink AC. A systematic review of prospective studies on attention problems and academic achievement. Acta Psychiatr Scand. 2010;122:271–84. doi: 10.1111/j.1600-0447.2010.01568.x. [DOI] [PubMed] [Google Scholar]
- 5.Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90(suppl 1):2–7. doi: 10.1136/adc.2004.059006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barkley RA, Fischer M, Smallish L, Fletcher KE. Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- 7.Biederman J, Ball SW, Monuteaux MC, Surman CB, Johnson JL, Zeitlin S. Are girls with ADHD at risk for eating disorders? Results from a controlled, five-year prospective study. J Dev Behav Pediatr. 2007;28:302–7. doi: 10.1097/DBP.0b013e3180327917. [DOI] [PubMed] [Google Scholar]
- 8.Biederman J, Pretty CR, Dolan C, et al. The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: findings from a controlled 10-year prospective longitudinal follow-up study. Psychol Med. 2008;38:1027–36. doi: 10.1017/S0033291707002668. [DOI] [PubMed] [Google Scholar]
- 9.Donfrancesco R, Miano S, Martines F, Ferrante L, Melegari MG, Masi G. Bipolar disorder co-morbidity in children with attention deficit hyperactivity disorder. Psychiatry Res. 2011;186:333–7. doi: 10.1016/j.psychres.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Szobot CM, Rohde LA, Bukstein O, et al. Is attention-deficit/hyperactivity disorder associated with illicit substance use disorders in male adolescents? A community-based case-control study. Addiction. 2007;102:1122–30. doi: 10.1111/j.1360-0443.2007.01850.x. [DOI] [PubMed] [Google Scholar]
- 11.Daviss WB, Diler RS. Suicidal behaviors in adolescents with ADHD: associations with depressive and other comorbidity, parent-child conflict, trauma exposure, and impairment. J Atten Disord. 2012;18:680–90. doi: 10.1177/1087054712451127. [DOI] [PubMed] [Google Scholar]
- 12.Manor I, Gutnik I, Ben-Dor DH, et al. Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents - A pilot study. Eur Psychiatry. 2010;25:146–50. doi: 10.1016/j.eurpsy.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Corkum P, Tannock R, Moldofsky H. Sleep disturbances in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1998;37:637–46. doi: 10.1097/00004583-199806000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Fallone G, Acebo C, Seifer R, Carskadon MA. Experimental restriction of sleep opportunity in children: effects on teacher ratings. Sleep. 2005;28:1561–7. doi: 10.1093/sleep/28.12.1561. [DOI] [PubMed] [Google Scholar]
- 15.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;74:444–5. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 16.Owens J, Sangal RB, Sutton VK, Bakken R, Allen AJ, Kelsey D. Subjective and objective measures of sleep in children with attention-deficit/hyperactivity disorder. Sleep Med. 2009;10:446–56. doi: 10.1016/j.sleep.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Scott N, Blair PS, Emond AM, et al. Sleep patterns in children with ADHD: a population-based cohort study from birth to 11 years. J Sleep Res. 2013;22:121–8. doi: 10.1111/j.1365-2869.2012.01054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Konofal E, Lecendreux M, Bouvard MP, Mouren-Simeoni MC. High levels of nocturnal activity in children with attention-deficit hyperactivity disorder: a video analysis. Psychiatry Clin Neurosci. 2001;55:97–103. doi: 10.1046/j.1440-1819.2001.00808.x. [DOI] [PubMed] [Google Scholar]
- 19.Silvestri R, Gagliano A, Arico I, et al. Sleep disorders in children with attention-deficit/hyperactivity disorder (ADHD) recorded overnight by video-polysomnography. Sleep Med. 2009;10:1132–8. doi: 10.1016/j.sleep.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Hansen BH, Skirbekk B, Oerbeck B, Richter J, Kristensen H. Comparison of sleep problems in children with anxiety and attention deficit/hyperactivity disorders. Eur Child Adolesc Psychiatry. 2011;20:321–30. doi: 10.1007/s00787-011-0179-z. [DOI] [PubMed] [Google Scholar]
- 21.Biederman J, Mick E, Faraone SV, et al. Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry. 2002;159:36–42. doi: 10.1176/appi.ajp.159.1.36. [DOI] [PubMed] [Google Scholar]
- 22.Gruber R, Fontil L, Bergmame L, et al. Contributions of circadian tendencies and behavioral problems to sleep onset problems of children with ADHD. BMC Psychiatry. 2012;12:212. doi: 10.1186/1471-244X-12-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadeh A, Pergamin L, Bar-Haim Y. Sleep in children with attention-deficit hyperactivity disorder: a meta-analysis of polysomnographic studies. Sleep Med Rev. 2006;10:381–98. doi: 10.1016/j.smrv.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Sung V, Hiscock H, Sciberas E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder - Prevalence and the effect on the child and family. Arch Pediatr Adolesc Med. 2008;162:336–42. doi: 10.1001/archpedi.162.4.336. [DOI] [PubMed] [Google Scholar]
- 25.Golan N, Shahar E, Ravid S, Pillar G. Sleep disorders and daytime sleepiness in children with attention-deficit/hyperactive disorder. Sleep. 2004;27:261–6. doi: 10.1093/sleep/27.2.261. [DOI] [PubMed] [Google Scholar]
- 26.Gruber R, Xi T, Frenette S, Robert M, Vannasinh P, Carrier J. Sleep disturbances in prepubertal children with attention deficit hyperactivity disorder: a home polysomnography study. Sleep. 2009;32:343–50. doi: 10.1093/sleep/32.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kirov R, Kinkelbur J, Heipke S, et al. Is there a specific polysomnographic sleep pattern in children with attention deficit/hyperactivity disorder? J Sleep Res. 2004;13:87–93. doi: 10.1111/j.1365-2869.2004.00387.x. [DOI] [PubMed] [Google Scholar]
- 28.Kirov R, Uebel H, Albrecht B, Banaschewski T, Yordanova J, Rothenberger A. Attention-deficit/hyperactivity disorder (ADHD) and adaptation night as determinants of sleep patterns in children. Eur Child Adolesc Psychiatry. 2012;21:681–90. doi: 10.1007/s00787-012-0308-3. [DOI] [PubMed] [Google Scholar]
- 29.Hansen BH, Skirbekk B, Oerbeck B, Wentzel-Larsen T, Kristensen H. Associations between sleep problems and attentional and behavioral functioning in children with anxiety disorders and ADHD. Behav Sleep Med. 2014;12:53–68. doi: 10.1080/15402002.2013.764525. [DOI] [PubMed] [Google Scholar]
- 30.Moreau V, Rouleau N, Morin CM. Sleep of children with attention deficit hyperactivity disorder: actigraphic and parental reports. Behav Sleep Med. 2014;12:69–83. doi: 10.1080/15402002.2013.764526. [DOI] [PubMed] [Google Scholar]
- 31.Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 2009;48:894–908. doi: 10.1097/CHI.0b013e3181ac09c9. [DOI] [PubMed] [Google Scholar]
- 32.Cortese S, Konofal E, Yateman N, Mouren MC, Lecendreux M. Sleep and alertness in children with attention-deficit/hyperactivity disorder: a systematic review of the literature. Sleep. 2006;29:504–11. [PubMed] [Google Scholar]
- 33.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in Epidemiology. A proposal for reporting. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 34.American Psychiatric Association. Washington, DC: American Psychiatric Association; 1987. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. revised. [Google Scholar]
- 35.Scottish Intercollegiate Guidelines Network. SIGN 50. A guideline developer's handbook. 2011. [Accessed Feb 4, 2013]. Available from: http://www.sign.ac.uk/guidelines/fulltext/50/index.html.
- 36.Bai A, Shukla VK, Bak G, Wells G. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2012. Quality assessment tools project report. [Google Scholar]
- 37.Diaz-Roman A, Perestelo-Perez L, Buela-Casal G. Sleep in obsessive-disorder: a systematic review and meta-analysis. Sleep Med. 2015;16:1049–55. doi: 10.1016/j.sleep.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 38.Botella J, Gambara H. Doing and reporting a meta-analysis. Int J Clin Health Psychol. 2006;6:425–40. [Google Scholar]
- 39.Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. J Educ Stat. 1981;6:107–28. [Google Scholar]
- 40.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 41.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0, 2011. [Accessed Jan 29, 2013]. Available from: http://handbook.cochrane.org.
- 43.Galland BC, Tripp EG, Taylor BJ. The sleep of children with attention deficit hyperactivity disorder on and off methylphenidate: a matched case-control study. J Sleep Res. 2010;19:366–73. doi: 10.1111/j.1365-2869.2009.00795.x. [DOI] [PubMed] [Google Scholar]
- 44.Gruber R, Sadeh A. Sleep and neurobehavioral functioning in boys with attention-deficit/hyperactivity disorder and no reported breathing problems. Sleep. 2004;27:267–73. doi: 10.1093/sleep/27.2.267. [DOI] [PubMed] [Google Scholar]
- 45.Mullin BC, Harvey AG, Hinshaw SP. A preliminary study of sleep in adolescents with bipolar disorder, ADHD, and non-patient controls. Bipolar Disord. 2011;13:425–32. doi: 10.1111/j.1399-5618.2011.00933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Owens JA, Maxim R, Nobile C, McGuinn M, Msall M. Parental and self-report of sleep in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2000;154:549–55. doi: 10.1001/archpedi.154.6.549. [DOI] [PubMed] [Google Scholar]
- 47.Prehn-Kristensen A, Goder R, Fischer J, et al. Reduced sleep-associated consolidation of declarative memory in attention-deficit/hyperactivity disorder. Sleep Med. 2011;12:672–9. doi: 10.1016/j.sleep.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 48.Prehn-Kristensen A, Munz M, Molzow I, Wilhelm I, Wiesner CD, Baving L. Sleep promotes consolidation of emotional memory in healthy children but not in children with attention-deficit hyperactivity disorder. PloS One. 2013;8:e65098. doi: 10.1371/journal.pone.0065098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Prihodova I, Paclt I, Kemlink D, Nevsimalova S. Sleep microstructure is not altered in children with attention-deficit/hyperactivity disorder (ADHD) Physiol Res. 2012;61:125–33. doi: 10.33549/physiolres.932225. [DOI] [PubMed] [Google Scholar]
- 50.Ringli M, Souissi S, Kurth S, Brandeis D, Jenni OG, Huber R. Topography of sleep slow wave activity in children with attention-deficit/hyperactivity disorder. Cortex. 2013;49:340–7. doi: 10.1016/j.cortex.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 51.Wiebe S, Carrier J, Frenette S, Gruber R. Sleep and sleepiness in children with attention deficit/hyperactivity disorder and controls. J Sleep Res. 2013;22:41–9. doi: 10.1111/j.1365-2869.2012.01033.x. [DOI] [PubMed] [Google Scholar]
- 52.Rechtschafen A, Kales A, editors. A manual standardized terminology, techniques and scoring system and sleep stages of human subjects. Los Angeles: UCLA Brain Information Service; 1968. [Google Scholar]
- 53.Iber C, Ancoli-Israel S, Chesson AL, Quan SF. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. [Google Scholar]
- 54.Novelli L, Ferri R, Bruni O. Sleep classification according to AASM and Rechtschaffen and Kales: effects on sleep scoring parameters of children and adolescents. J Sleep Res. 2010;19:238–47. doi: 10.1111/j.1365-2869.2009.00785.x. [DOI] [PubMed] [Google Scholar]
- 55.Mayes SD, Calhoun SL, Bixler EO, et al. ADHD subtypes and comorbid anxiety, depression, and oppositional-defiant disorder: differences in sleep problems. J Pediatr Psychol. 2009;34:328–37. doi: 10.1093/jpepsy/jsn083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wagner J, Schlarb AA. Subtypes of ADHD and their association with sleep disturbances in children. Somnologie. 2012;16:118–24. [Google Scholar]
- 57.Garcia F, Gonzalez H, Perez M. Spain: Alianza Ensayo; 2014. Volviendo a la normalidad. La invención del TDAH y del trastorno bipolar infantil. [Google Scholar]
- 58.Bruchmuller K, Margraf J, Schneider S. Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. J Consult Clin Psychol. 2012;80:128–38. doi: 10.1037/a0026582. [DOI] [PubMed] [Google Scholar]
- 59.Thomas R, Mitchell G, Batstra L. Attention-deficit/hyperactivity disorder: are we helping or harming? BMJ. 2013;347:f6172. doi: 10.1136/bmj.f6172. [DOI] [PubMed] [Google Scholar]
- 60.Sciutto MJ, Eisenberg M. Evaluating the evidence for and against the overdiagnosis of ADHD. J Atten Disord. 2007;11:106–13. doi: 10.1177/1087054707300094. [DOI] [PubMed] [Google Scholar]